6. Corneal Development and Structure
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
68 Terms
What are the layers of the cornea?
Epithelium
Superficial
Wing cells
Basal
Bowman’s
Stroma
Descemet’s
Endothelium
What embryonic tissue is the cornea made from?
All tissues are derived from ectoderm.
Surface ectoderm → corneal epithelium
Neural crest → Corneal stroma, corneal endothelium, descemet’s membrane, sclera and trabecular meshwork
When does the cornea develop?
Immediately after the formation of the lens (27-36 days)
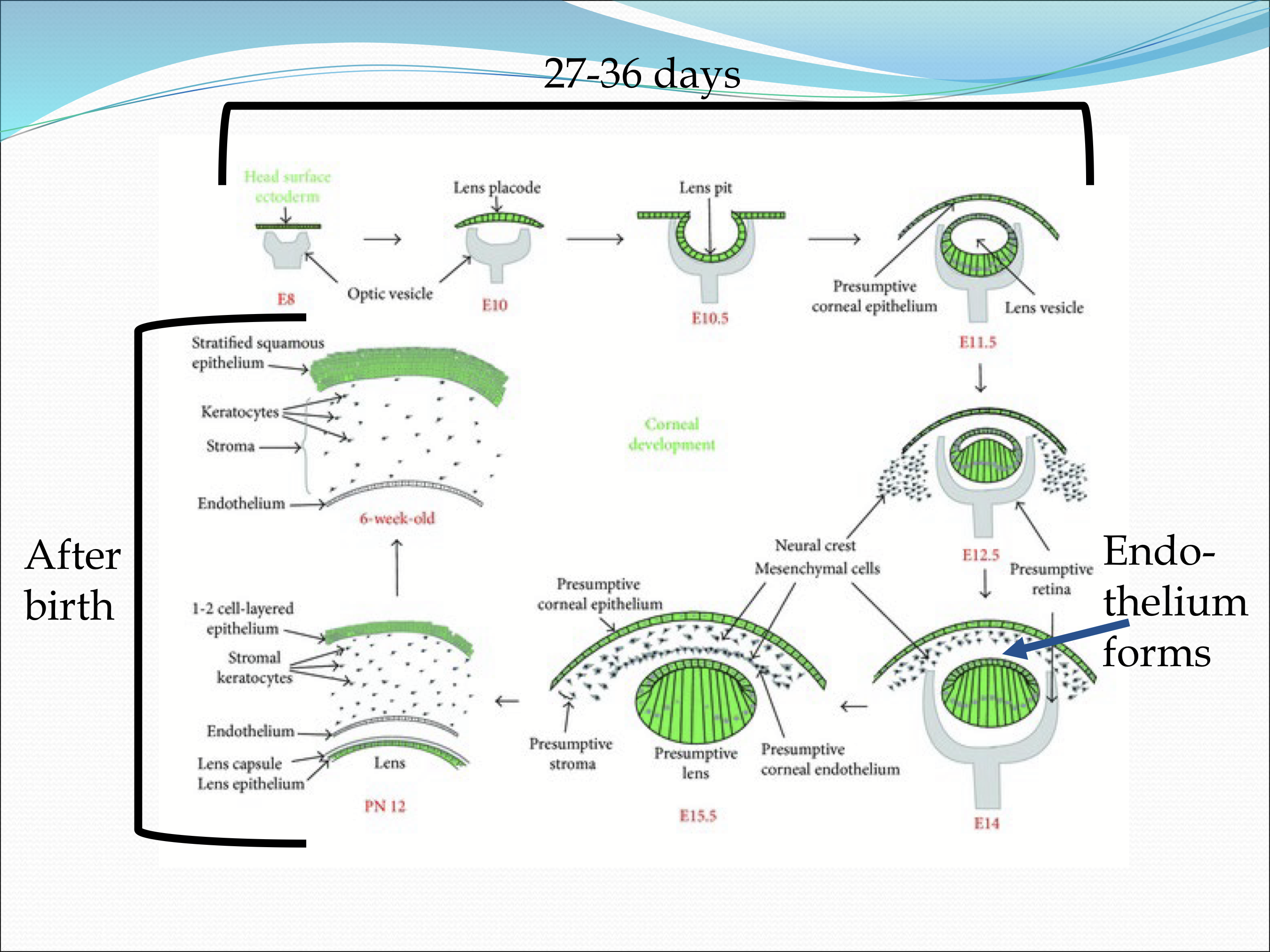
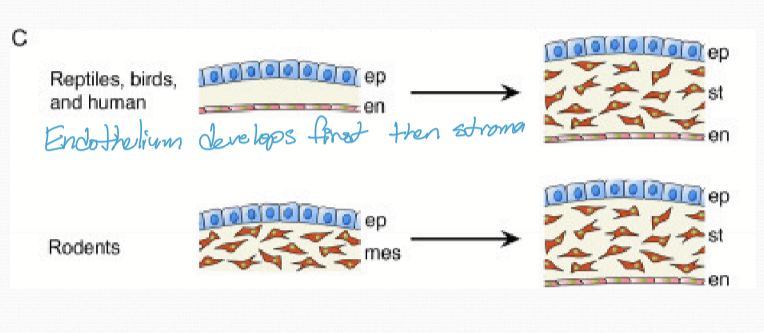
In humans, what develops first? The endothelium or stroma?
The endothelium
When does the cornea epithelial thicken?
The epithelial thickness increases twice. Once after the eye lids open, gaining ~4 cells and with the production of basement membrane and anchoring complexes; and again after birth by 4-6 cells.
What happens to the cornea after birth?
It shrinks, decreasing in thickness as the hyaluronic rick ECM is replaced with collagen fibril rich ECM.
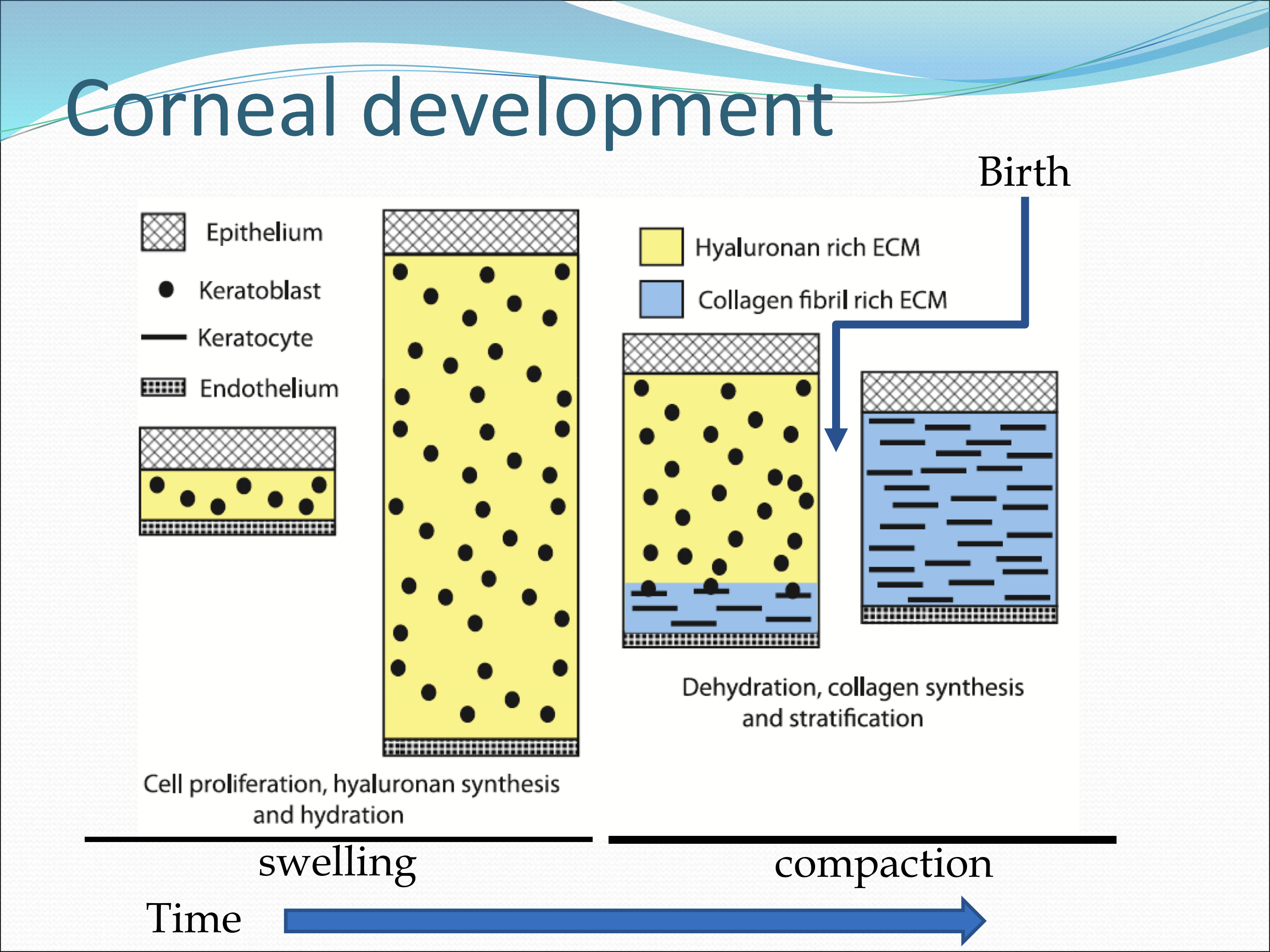
Where is Hyaluronic acid/hyaluronan synthesized?
It is synthesized in large amounts by primitive corneal endothelium and keratoblasts.
What properties does hyaluronic acid/hyaluronan have?
They have a high negative charge and that draw water in, causing the stroma to swell. It also provides a substrate for further cell migration into the stroma.
Why does the corneal thickness decrease?
It decreases due to the removal of hyaluronans and stromal dehydration from endothelial pump function.
How is hyaluronan removed?
Keratocytes change their secretion, producing hyaluronidase, to break down hyaluronan. It also synthesiszes collagens and other GAGs to form lamellae
When the endothelium matures, what happens?
TJ form in epithelial cells to limit paracellular water transport
Production/activation of endothelial pump proteins
Stroma decreases water content and cornea becomes transparent
What steps does the corneal stroma undergo to reach full maturity?
Mesenchymal cells migrate from limbal region beneath corneal epithelium after lens invagaination to form primitive endothelium and keratoblasts
After primary migration, smoe collagen is deposited, keratoblasts produce HA and primary stroma, and primitive endothelium begins producing descemet’s membrane
Second wave of mesenchymal cells migrate from limbus and become keratoblasts
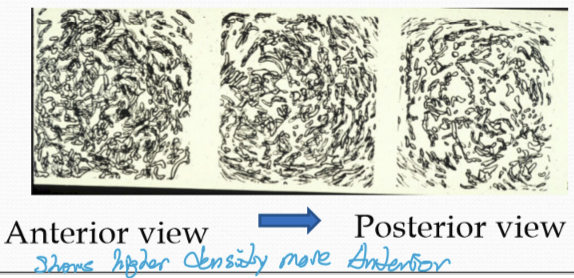
Dehydration/compaction/organization occurring in a posterior to anterior direction
How long does the cornea continue to grow?
It grows for 2 years to reach adult size, affecting the optic power
As the cornea ages, what happens to it?
Decrease in keratocyte number
Decrease in corneal nerve fibers
Decrease in endothelial cell density
Increase in epithelial basement membrane thickness
Increase in stiffness of stroma
Increase in descemet’s membrane
Impaired wound healing
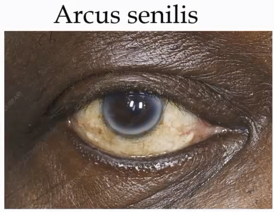
What is arcus senilis
Deposits of cholestryl ester-rich lipid particles
Doesn’t typically affect vision
Mainly derived from low-density lipoproteins
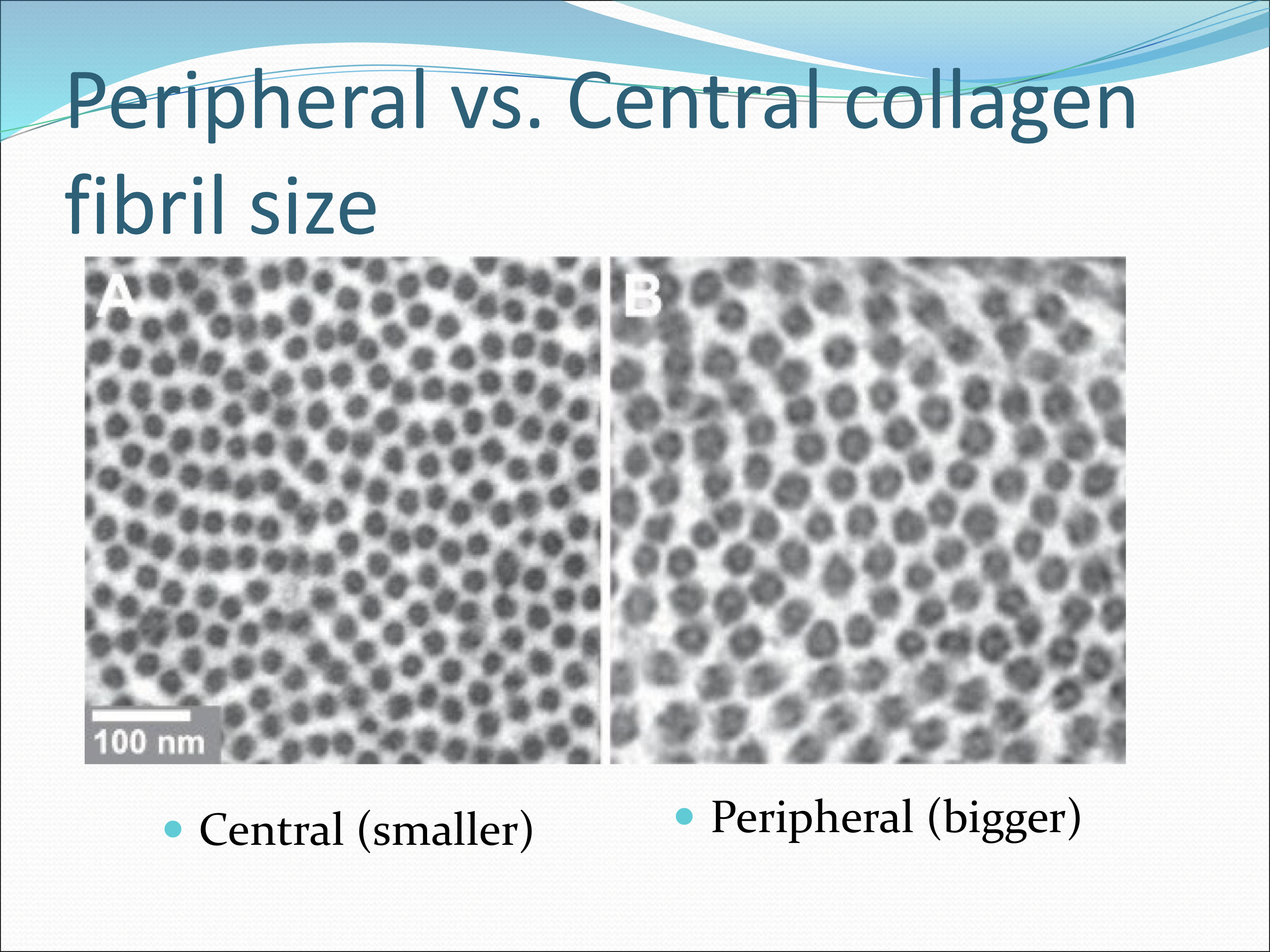
Which collagen fibrils is thicker, stroma or bowman’s?
Stroma is thicker at 25nm vs bowman’s 22nm, with an increase in width from central to peripheral cornea
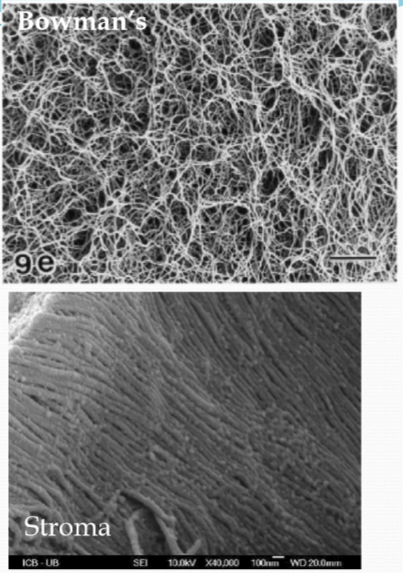
How big is the interfibrillar space?
20 nm, and increases in spacing from central to peripheral cornea
Which aspect of the stroma is more mechanically stronger?
The anterior aspect has more mechanical strength than the posterior from the interweaving collagen lamella.
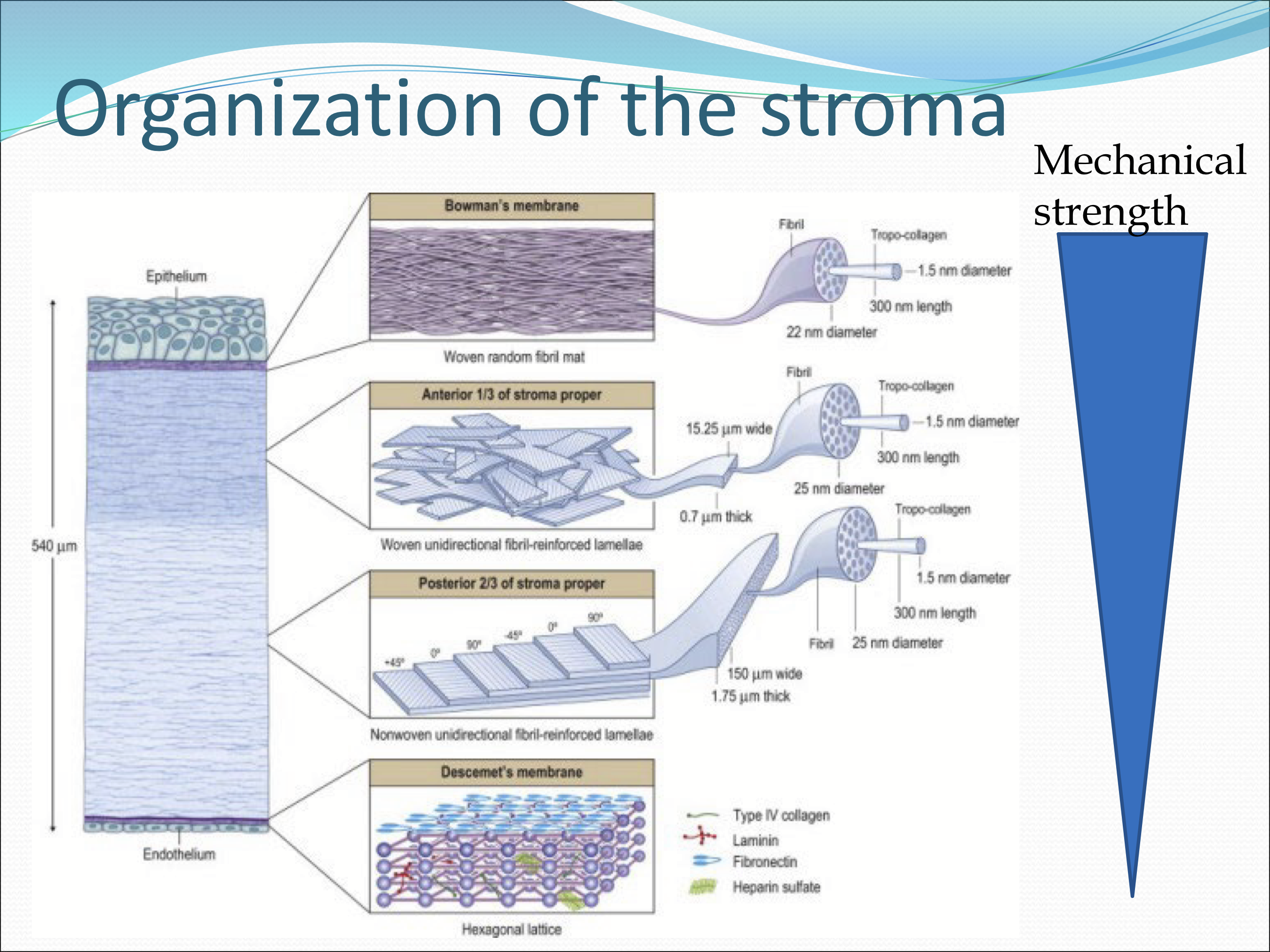
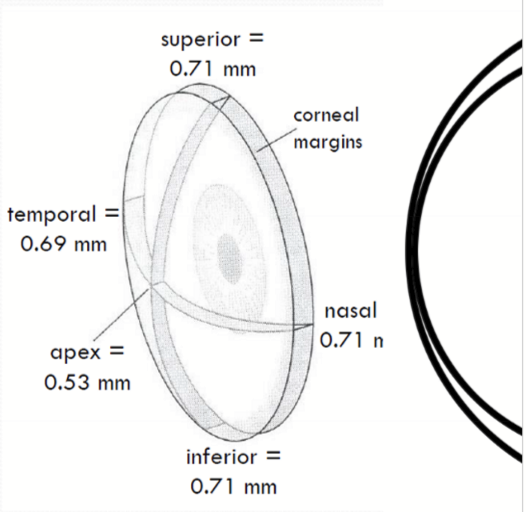
Where is the corneal lamellae thickness the thinnest, thickest?
It is thinner at the central cornea (250-300 lamellae) vs the peripheral cornea (500 lamellae)
What is the difference between posterior vs anterior lammelae?
The posterior lammelae are wider.
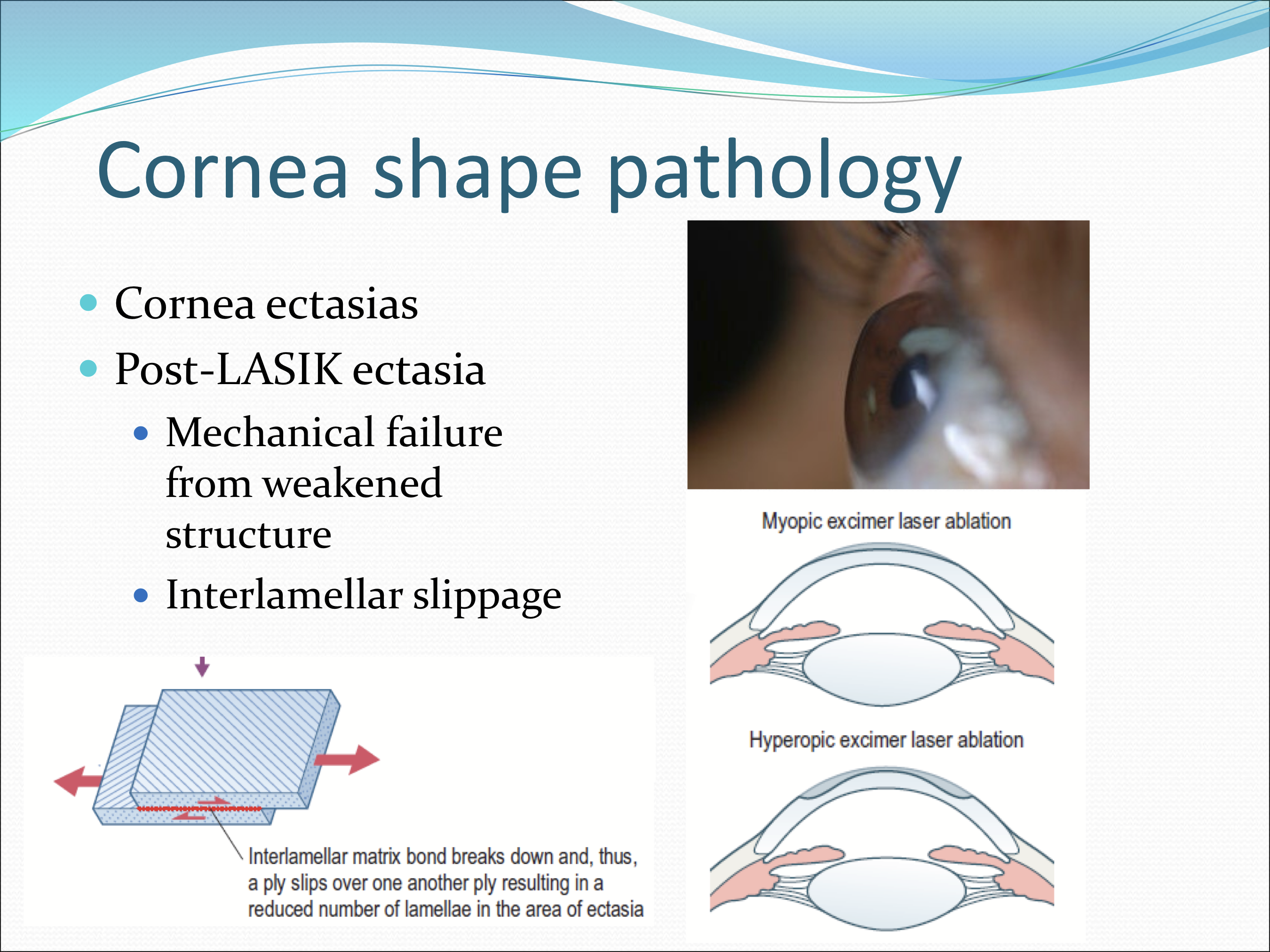
What is cornea ectasias?
A broad term that refers to a group of progressive thinning and bulging disorders of the cornea
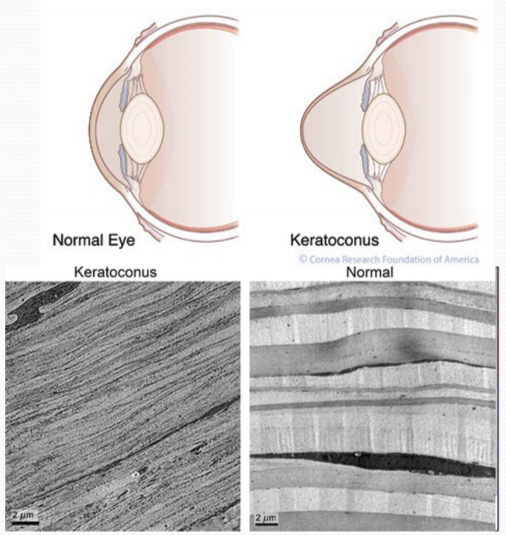
What is Keratoconus?
A bilateral, progressive thinning and ectasia of the cornea that results in blurred vision from irregular astigmatism
What is post-LASIK ectasia?
The intrerlamellar slippage from mechanical failure of the cornea due to a weakened structure
How is the lamellae oriented in the cornea?
Nasal/temporal (horizontal) and inferior/superior (vertical), but adjacent lamellae are not necessarily orthognal to each other
How is the peripheral collagen arranged?
Collagen fibrils thoroughout width of stroma stretch across the cornea and turn 90 degrees to form a circumferential annulus to maintain curvature. It is 1.0-2.5 mm wide
What are the types of collagen in the cornea?
Type I, V, VI, and XII and XIV for FACIT (fibril associated collagens with interrupted triple helicies)
What collagen types form fibrils?
Type I and V and is the majority of the collagen found in the cornea
What collage are non-fibril forming?
Collagen type VI, and FACIT: XII and XIV
What role does type V collage have?
It limits the diameter of collagen fibrils by introducing small mismatches in the alignment between type I and V collagen segments. It also prevents binding of additional segments due to weaker non-covalent bonds.
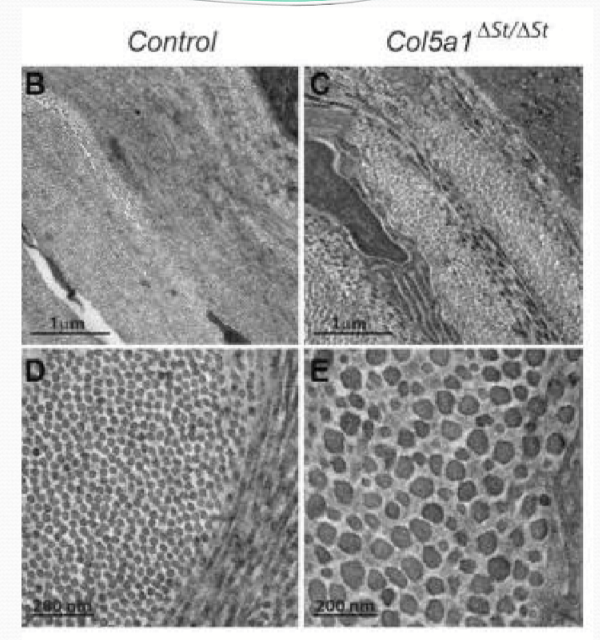
What is Ehlers-Danlos syndrome?
An inherited disorder with disruptions in CT proteins, affecting collagen I/V genes. Genes encoding noncollagenous ECM proteins and intracellular processes can be also affected
What are some symptoms of Ehlers-Danlos syndrome?
Skin hyper-extensibility
Delayed wound healing
Joint hypermobility
Corneal complications: thinner, stromal folding, keratoconus
What function does Type VI collagen have?
It binds corneal lamellae together by bridging other types of collagen together. They are non-banded and beaded filaments
What are the functions of a keratocyte?
Production of collagen fibrils and ECM of stroma
Control turnover of stromal ECM
Source of ECM during injury
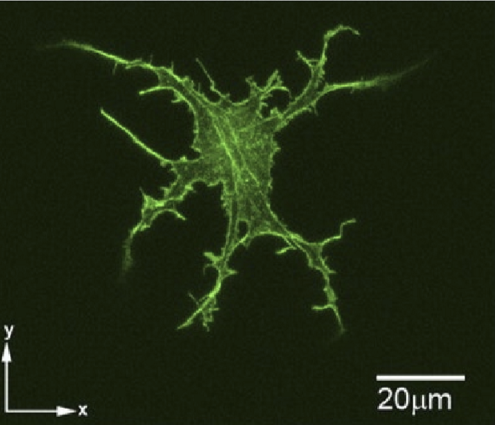
How much corneal volume does keratocytes take up?
10%, and are the second major component of the corneal stroma’s dry weight. It increases in density with age and have a radial organization.
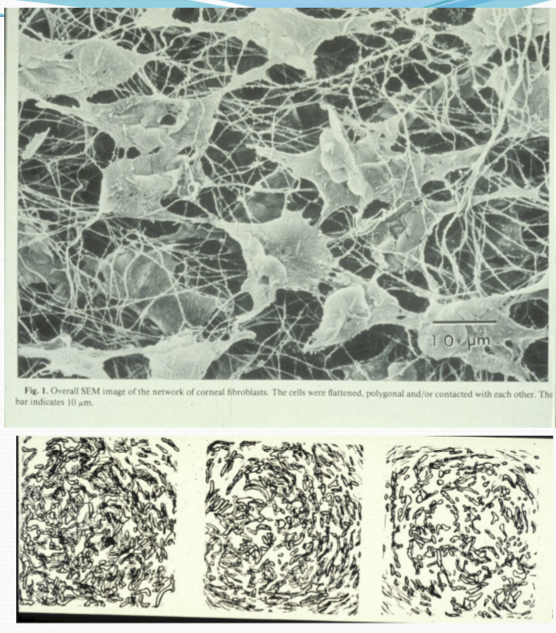
Where are keratocytes localized?
More anteriorly vs posteriorly
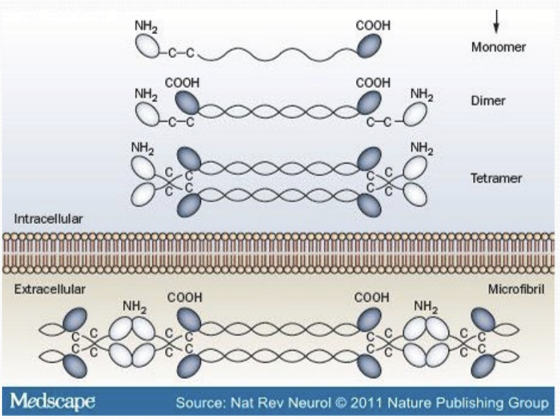
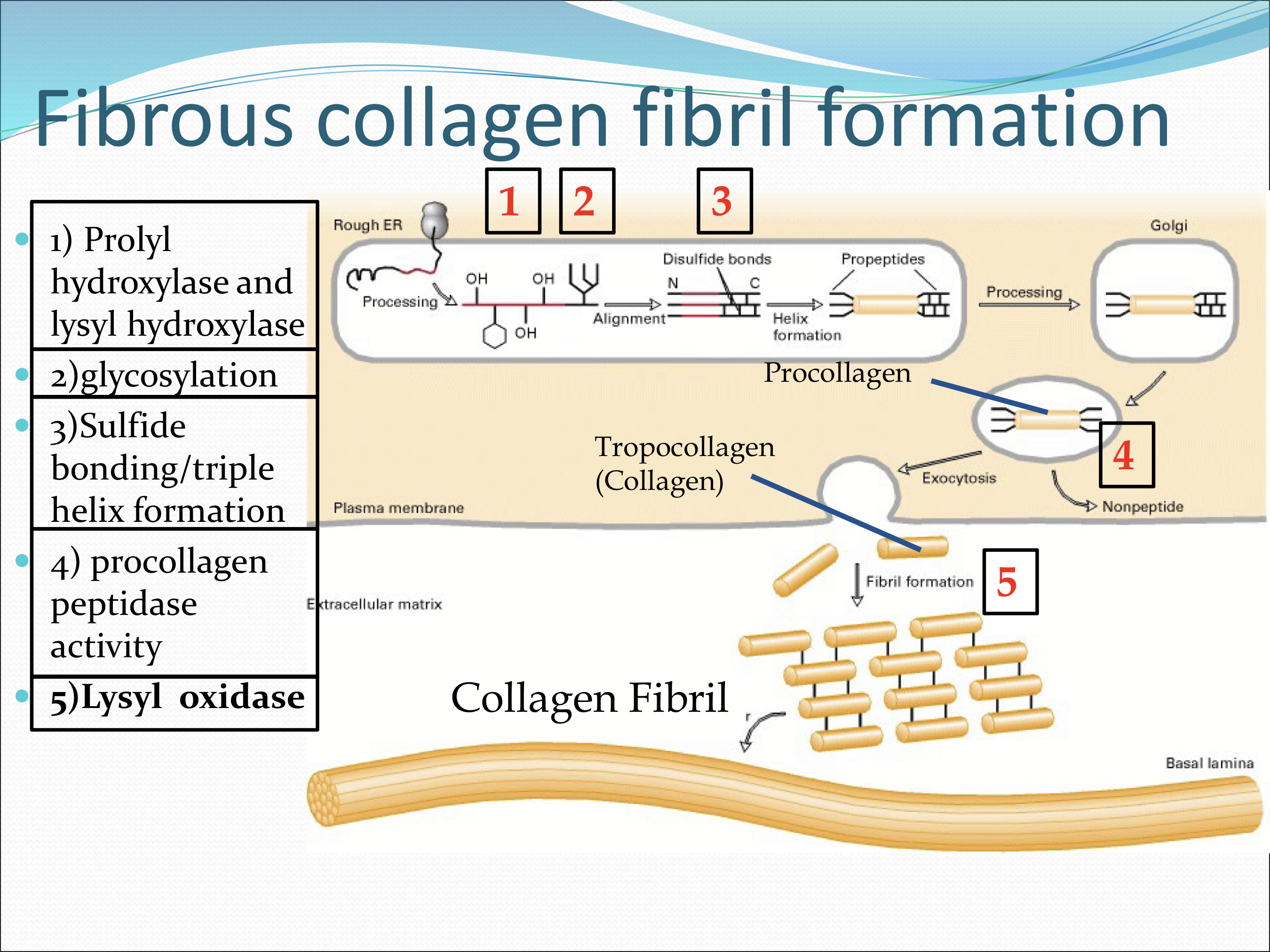
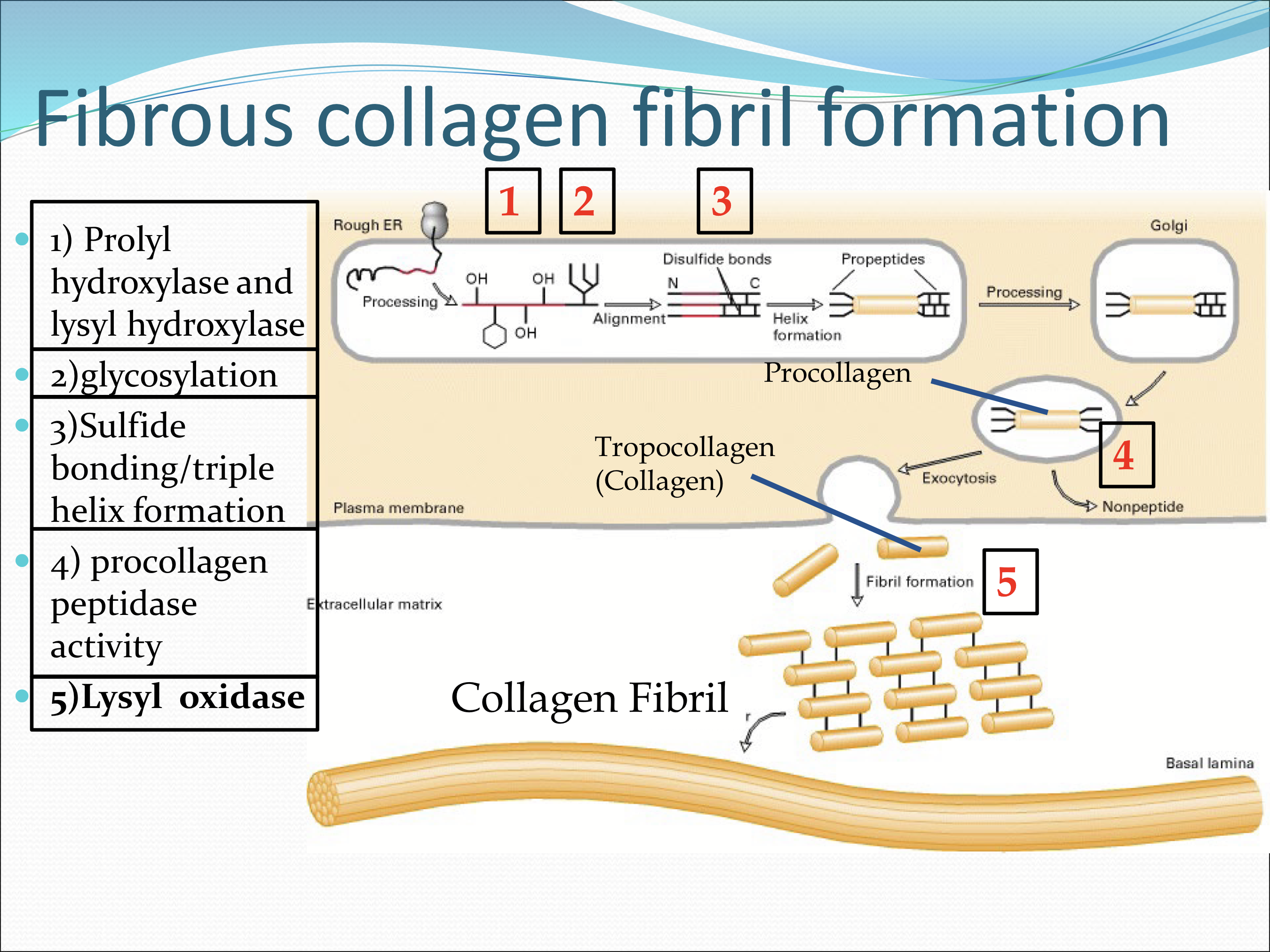
What are the enzymes used during fibrous collagen fibril formation?
Prolyl hydroxylase and lysyl hydroxylase
Glycosylation
Sulfide bonding/triple helix formation
Procollagen peptidase activity
Lysyl Oxidase (an extracellular enzyme secreted by keratocytes)
Where is lysyl oxidase found?
Extracellularly, and is an enzyme secreted by keratocytes.
What is the importance of prolyl hydroxylase and lysyl hydroxylase
They help stabilize the collagen triple helix by modifing select proline/lysine amino acids and changing them to hydroxyproline/hydroxylysine by adding a hydroxyl group in the ER
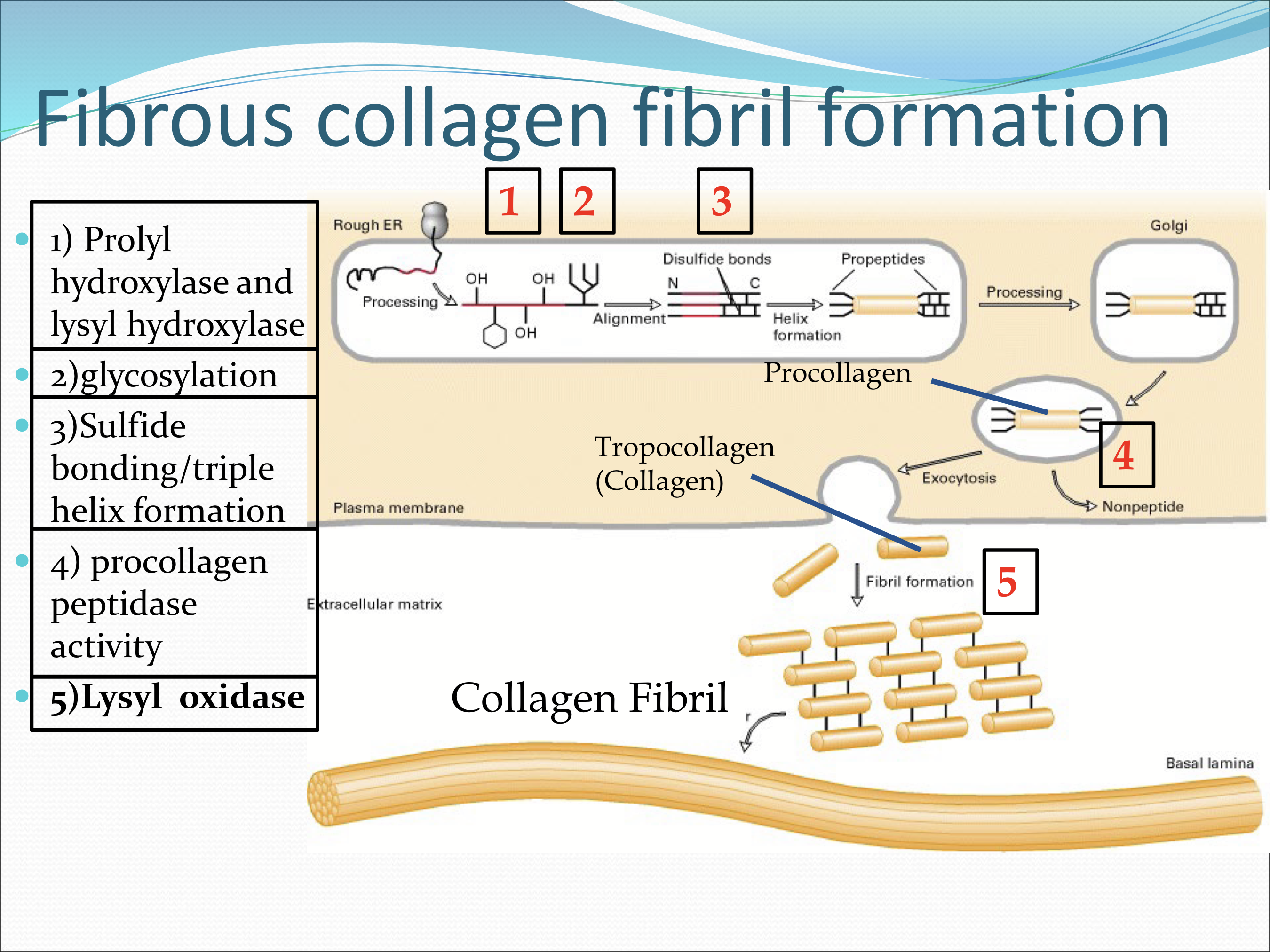
What do prolyl hydroxylase and lysyl hydroxylase require to function?
Vitamin C/ascorbic acid
What allows the alignment and formation of triple helix formation?
The intrapeptide disulfide bonds forming between propeptide sequences to align the 3 collagen chains
What does lysyl oxidase do?
It catalyzes the linkage between tropocollagen units after the procollagen is exocytosed
What are fibripositors?
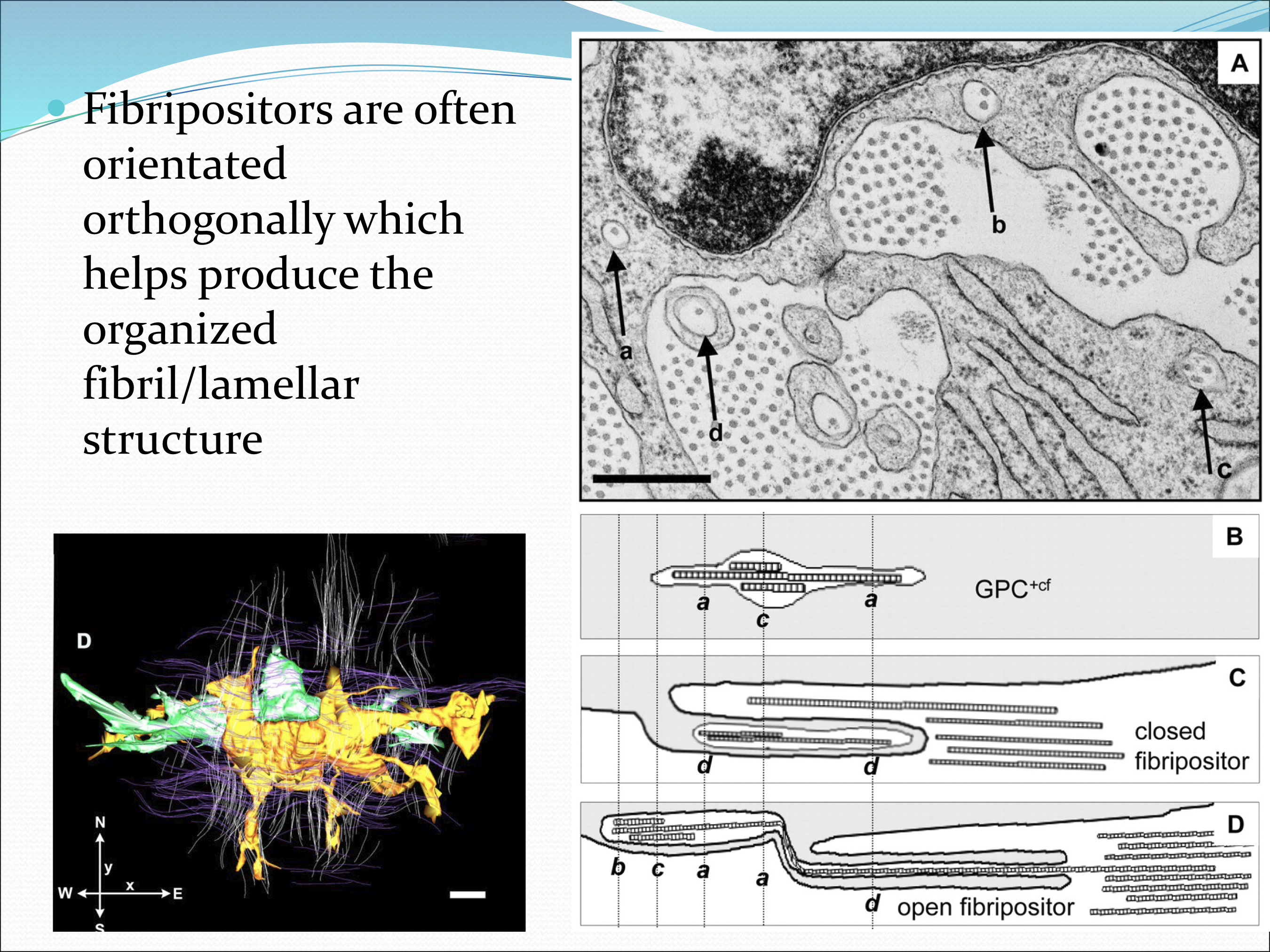
The are long cytoplasmic extensions of keratocytes that surround nascent fibrils and deposit them into forming lamellae
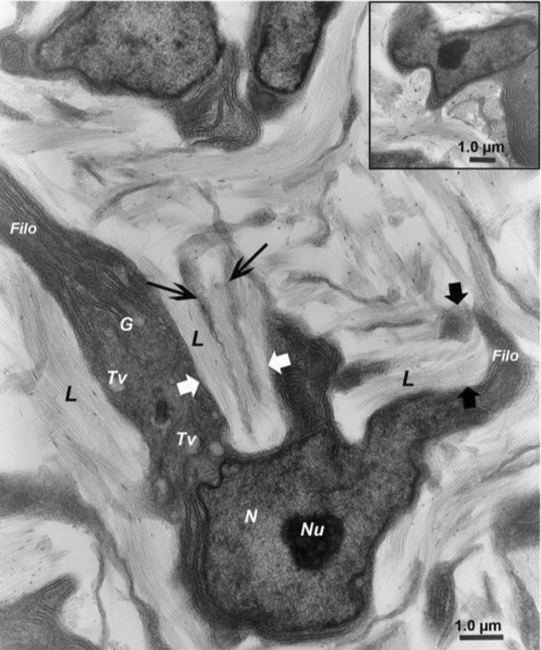
How are fibripositors orientated?
The are orthogonal to help produce the organized fibril/lamellar structure
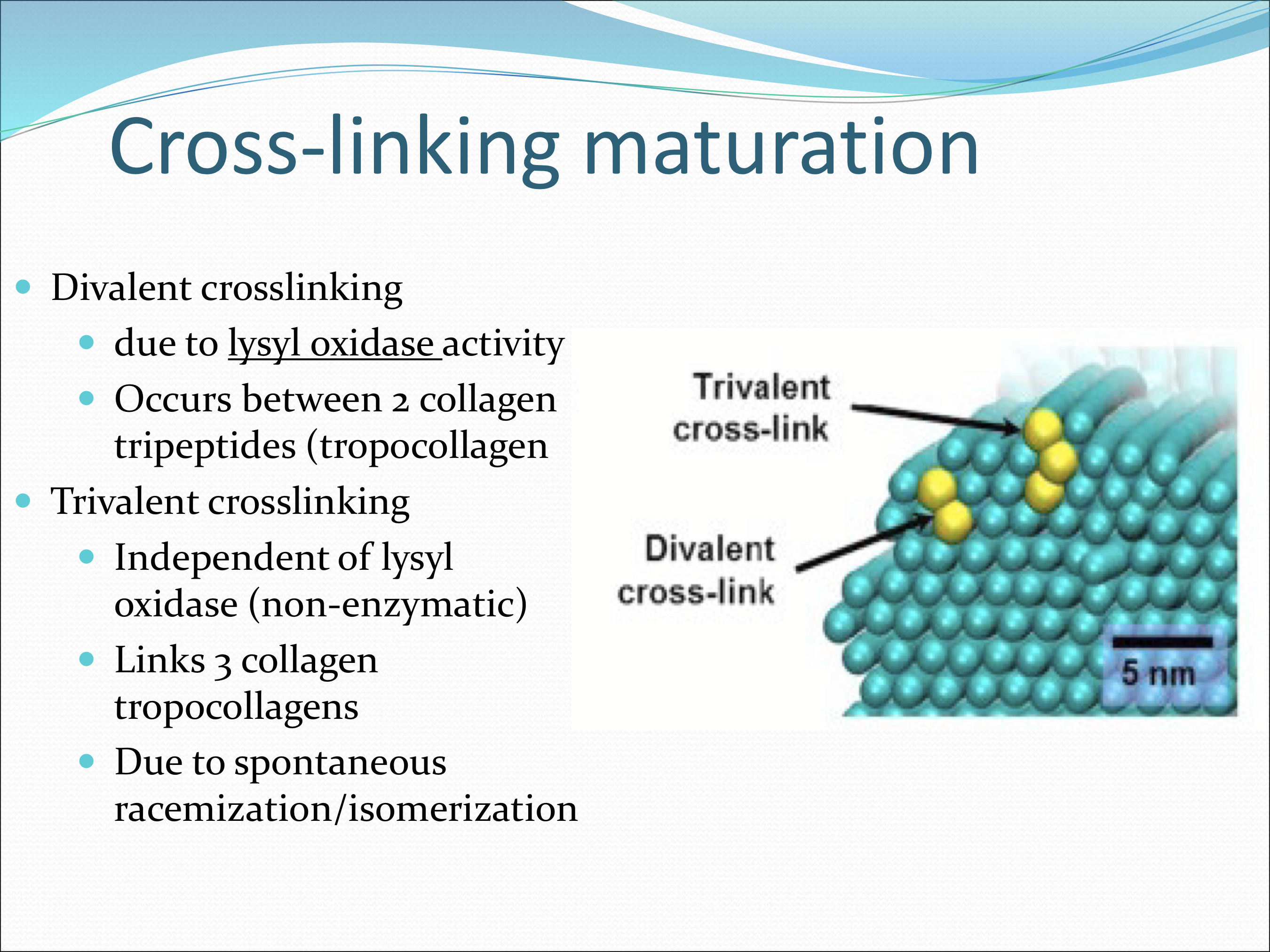
What are the 2 categories of collagen fibril maturation?
Cross-link maturation via:
Enzymatic (divalent cross-linking)
Non-enzymatic (trivalent cross-linking)
Glycation
What happens to the collagen as it matures?
It increases in stiffness= strong/tougher fibirls, but can be overdone, forming a brittle cornea.
What is the difference divalent vs trivalent crosslinking?
Divalent corsslinking is due to lysyl oxidase altering lysines to form covalent bonds. It is between 2 collagen tripeptides.
Trivalent crosslinking is independent of lysyl oxidase. Links 3 collagen tropocollagnes from spontaeous racemization/isomerization of aspartic acid and glycine amino acid
What is glycation?
A non-enzymatic process in which sugar molecules bind to proteins, lipids, or nucleic acids. They are reversible.
Where does glycation occur between?
Different tropocollagnes
Within the same tropocollagen
Different fibrils
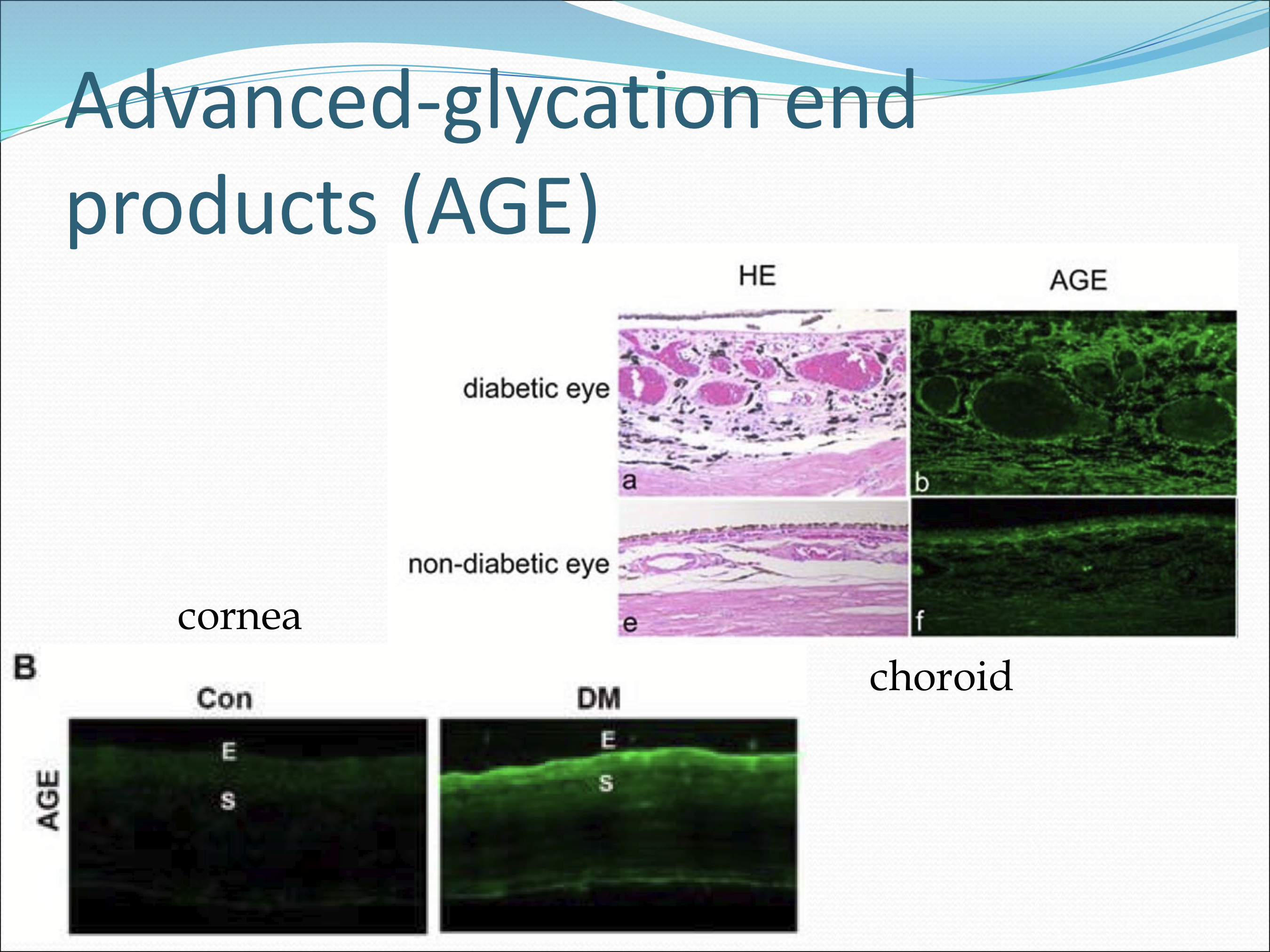
What are Advanced-glycation end products (AGE)?
They are glycation reactions with biological molecules.
Why are AGE’s potentially problematic?
They accumulate with age, and increase the stiffness of the tissue, making it brittle and prone to injury.
What tissues to AGE affect?
Vasculature
Lens
Vitreous
Outer retina
trabecular meshwork
What pathology can increase the accumulation of AGE?
Hyperglycemia
What is UVA-Riboflavin (ultraviolet A light with riboflavin) do?
It cross links corneal collagen, and increases the mechanical strength of the cornea.
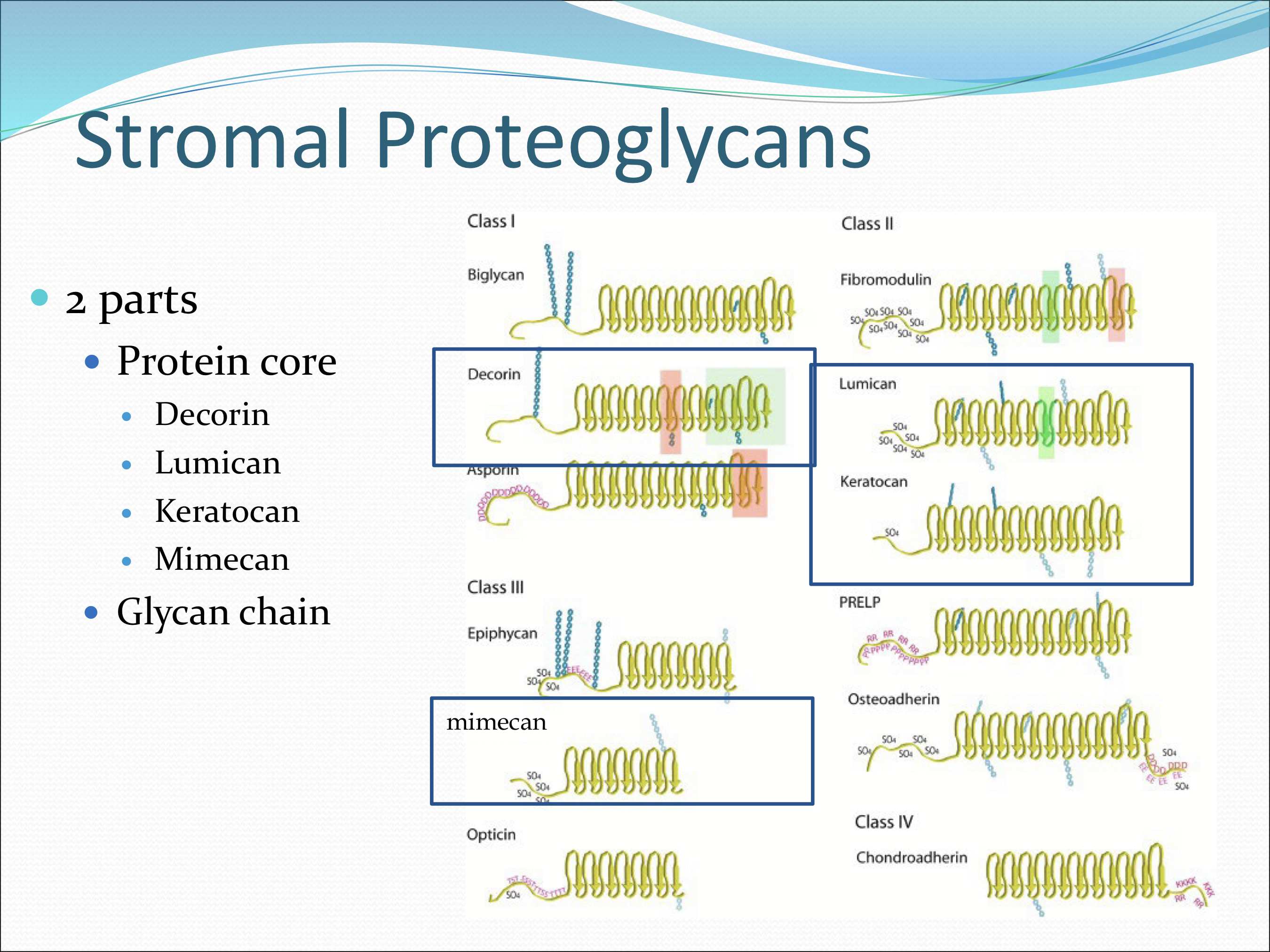
What are stromal proteoglycans composed of?
2 parts:
Protein core: decorin, lumican, keratocan, mimecan
Glycan chain
What charge do GAGs have?
A highly negative charge
What are the functions of stromal proteoglycans?
Function as spacer molecules between collagen fibrils, control fibril diameter growth, assembly, caliber, resist compressive forces, grant viscoelastic properties of cornea, and assist transparency
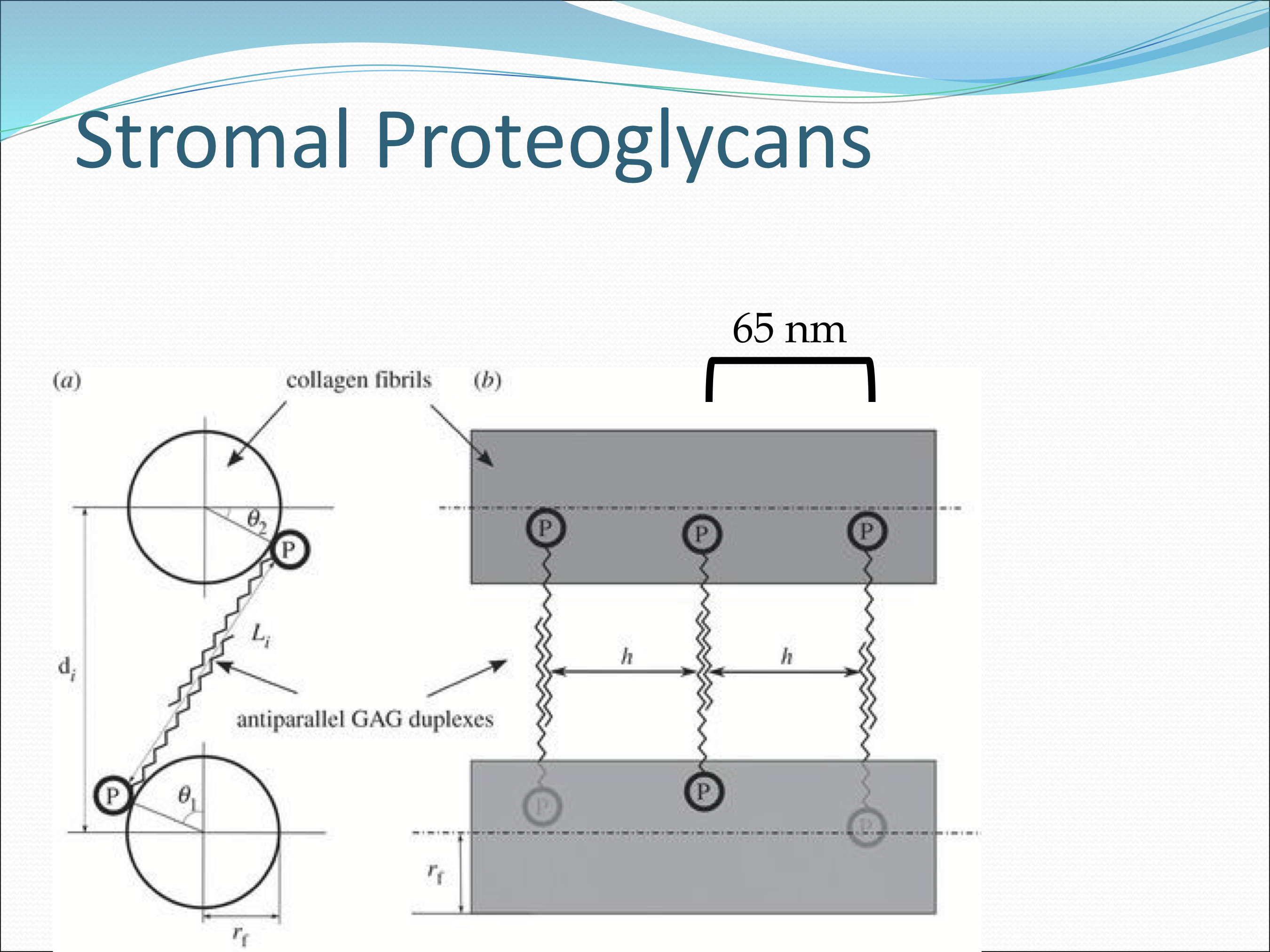
How are fibrils and proteoglycans attached to eachtoher?
They are non-covalently attached to each other
What are the 2 types of glycan chains that stromal proteoglycans use?
Keratan sulfate
Dermatan sulfate
What are keratan sulface glycan chains made of?
Lumican, keratocan, mimecan
Disaccaride made up of galactose and N-acetylgucosamine
What are dermatan sulface glycan chains made of?
Decorin only
Disaccaride made up of iduornic acid and N-acetylgalactosamine
Which glycan chain is more common.
Keratan sulfate > Dermatan sulfate
How much of the total GAGs are Keratan sulfate?
60%
Where is Keratan sulfate more abundant in the stroma?
The posterior aspect
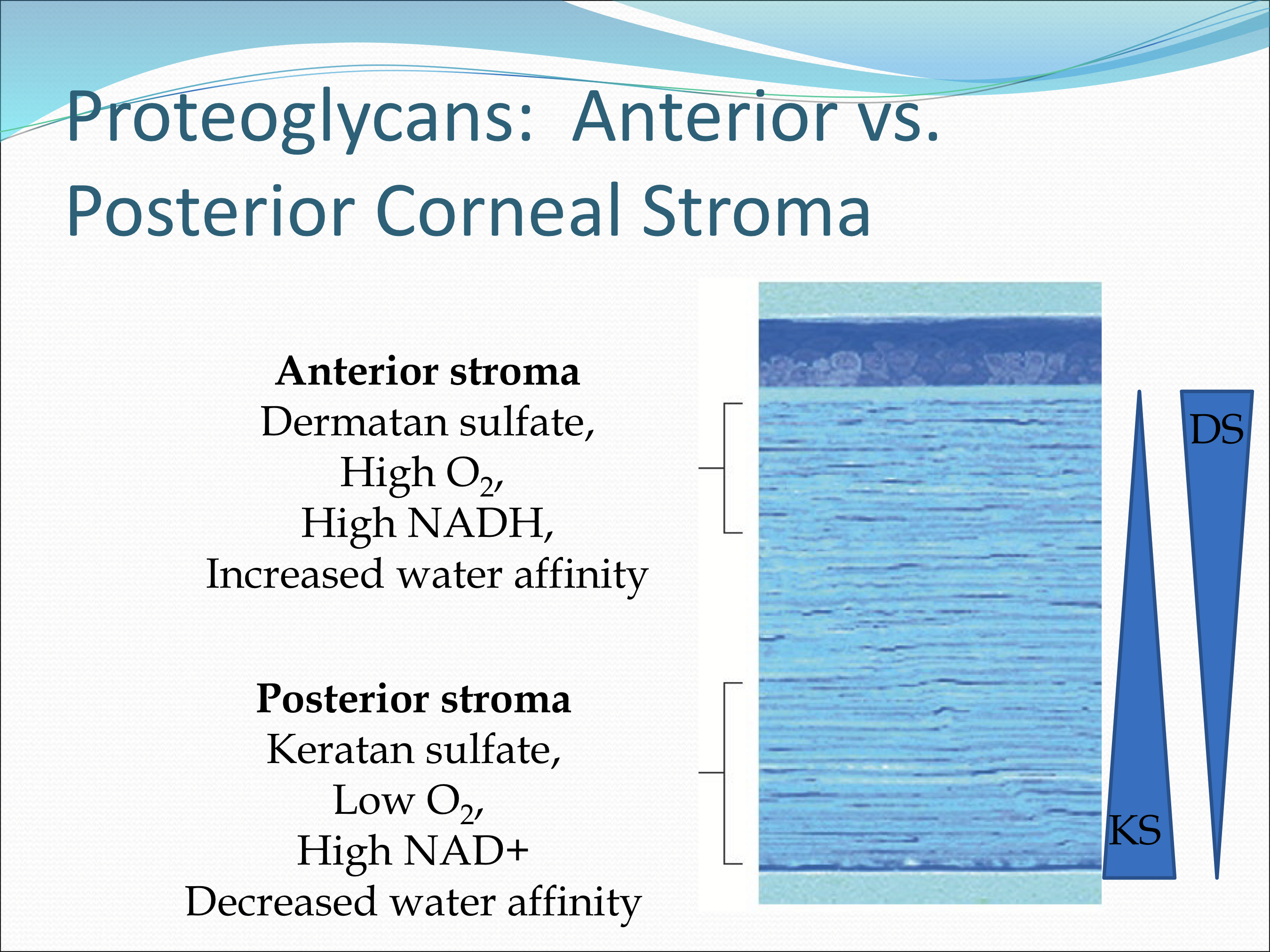
What does keratin sulfate do?
regulates consistency of fibril diameter and spacing
promotes cell migration during development
water binding capability is less than dermatan sulfate, allowing water to exit across the endothelium more freely
How much of the total GAGs are Dermatan sulfate?
40% of total GAGs
What does dermatan suflate do?
Facilitates correct fibril spacing,
binds water with greater affinity than keratan sulfate to facilitate a resistance to evaporation and water loss.
Where is Dermatan sulfate found?
In the anterior cornea and in high oxygen environments
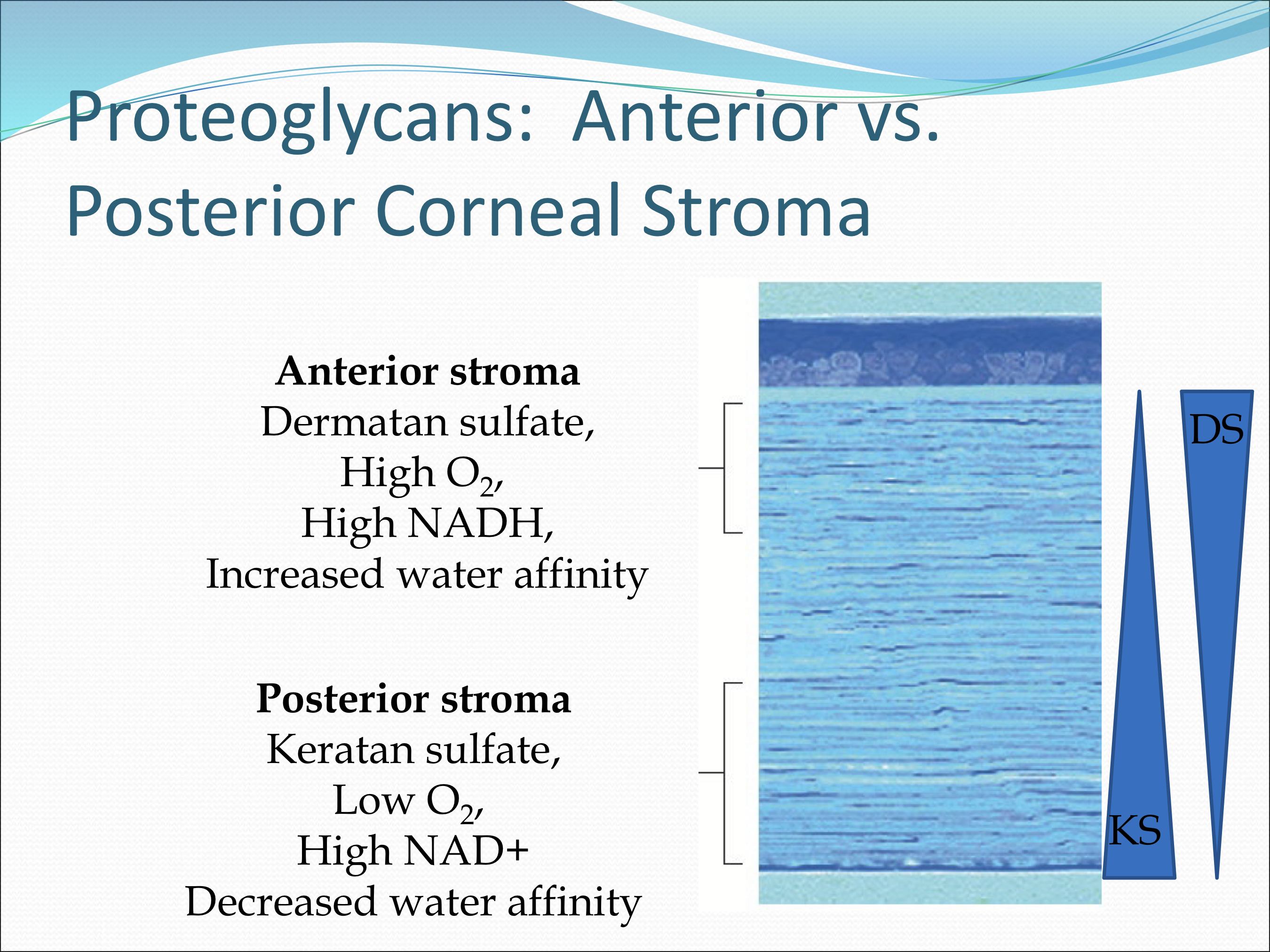
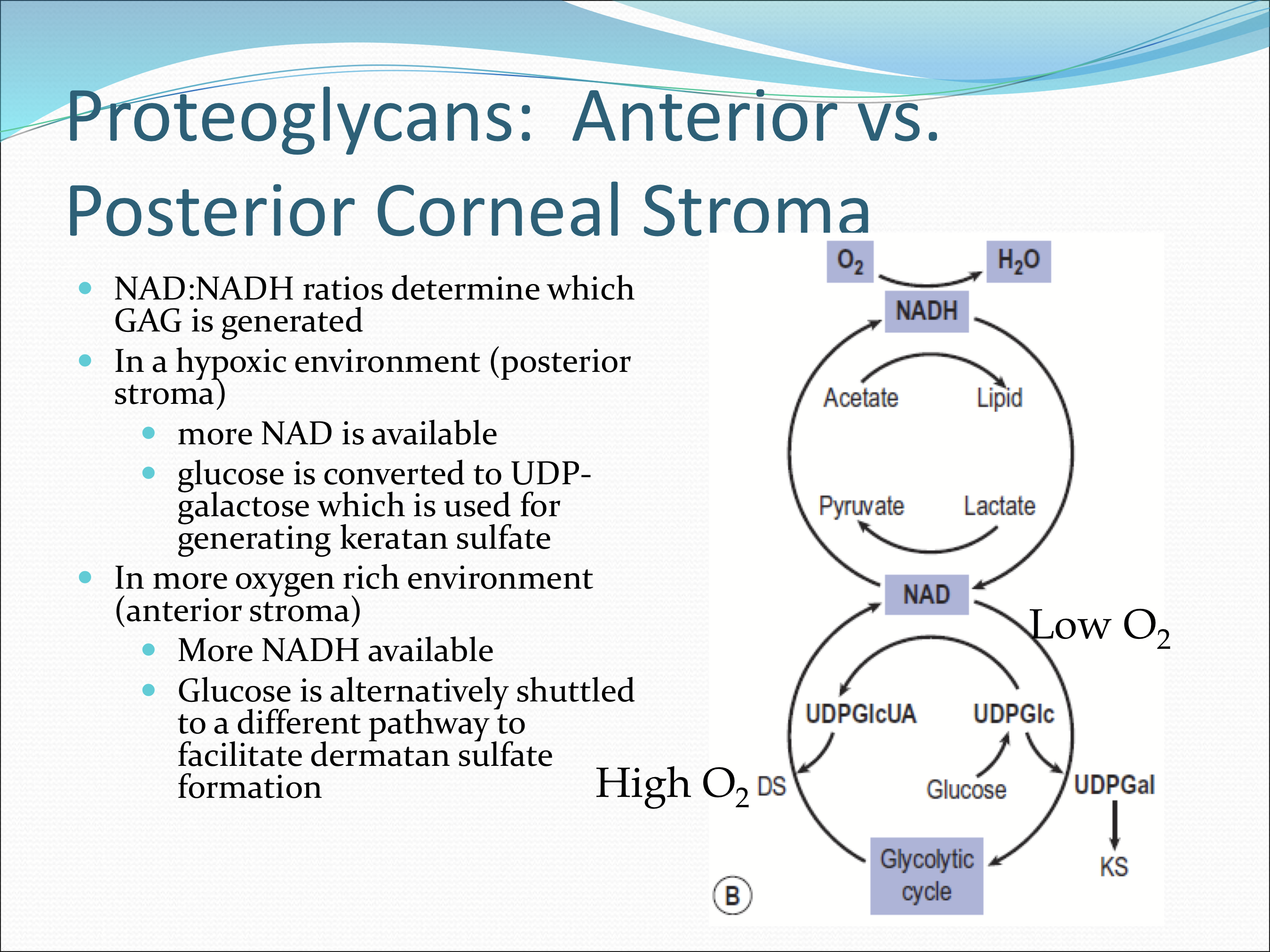
What factor determines which GAG is generated?
NAD:NADH ratio
In a hypoxic environment, more NAD is more abundant and glucose is converted to UDP-galactose which is used for generating keratan sulfate
In a more oxygen rich environment, more NADH is available, and glucose is shuttled to a different pathway to facilitate dermatan suflate formation