MICR 270 Mod 2 - Branches of the Immune System
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
innate immune system - physical barriers
made of every structure located at the interface between the inside and outside of the body
ie. cilia, skin, bodily secretions
innate immune system - cellular barriers
made of the various cells ie. neutrophils, macrophages, dendritic cells, and NK cells, which play a role in the innate immune response
innate immune system - soluble barriers
made of macromolecules which contribute to the mediation of an innate immune response
ie. complement and cytokines
Physical components of physical barriers
the skin creates a barrier pathogens cannot cross unless it is breached
mucous membranes cover the cavities of the body including the respiratory, GI, urinary, and reproductive tracts. These specialized membranes contain specialized structures ie. mucous, cilia, which sweep pathogens away
chemical components of physical barriers
tears and saliva are mucous membrane secretions which contain antimicrobial substances such as lysozyme (catalyzes cell wall destruction)
another example is gastric acid in the stomach
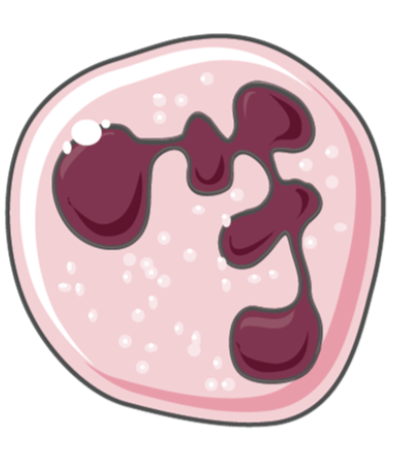
cellular barriers - neutrophils
most common leukocyte found in blood of mammals (45-70%)
phagocytes that patrol the body to find, engulf, and destroy pathogens
circulate in the blood for approx 12 hours before entering tissues by diapedesis
recruited to a site of infection by residdent macrophages that have encountered pathogens
lifespan of 1-3 days after entering the tissues
cellular barriers - macrophages
phagocytes that patrol the body to find, engulf, and destroy pathogens
can either take up residence in a specific tissue or move freely/patrol throughout a larger area of tissues
contribute to tissue repair and present antigens to other immune cells such as T cells
become activated after phagocytosing pathogens or in response to cytokine signalling
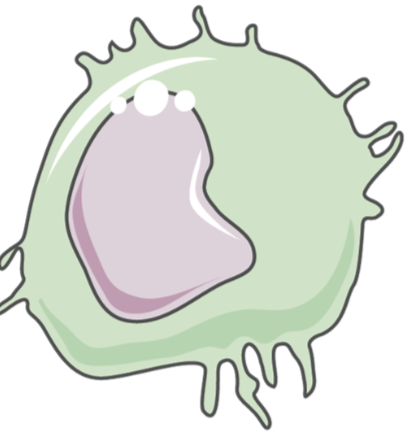
cellular barriers - dendritic cells
phagocytes that are often in contact with the external environment (specifically Langerhans DC)
engulf foreign antigens that have evaded the initial barriers of the innate immune system
present antigens on their cell surface through peptide MHC complexes, which can be recognized by helper T cells
major link between the innate and adaptive immune systems
cellular barriers - Natural Killer Cells
recognize abnormal cells lacking antigen-specific receptors
destroy abnormal cells of the body, which include tumours and virus infected cells
bind to cell surface of target cells and release chemicals causing pores to form in the cell membrane, leading to their lysis
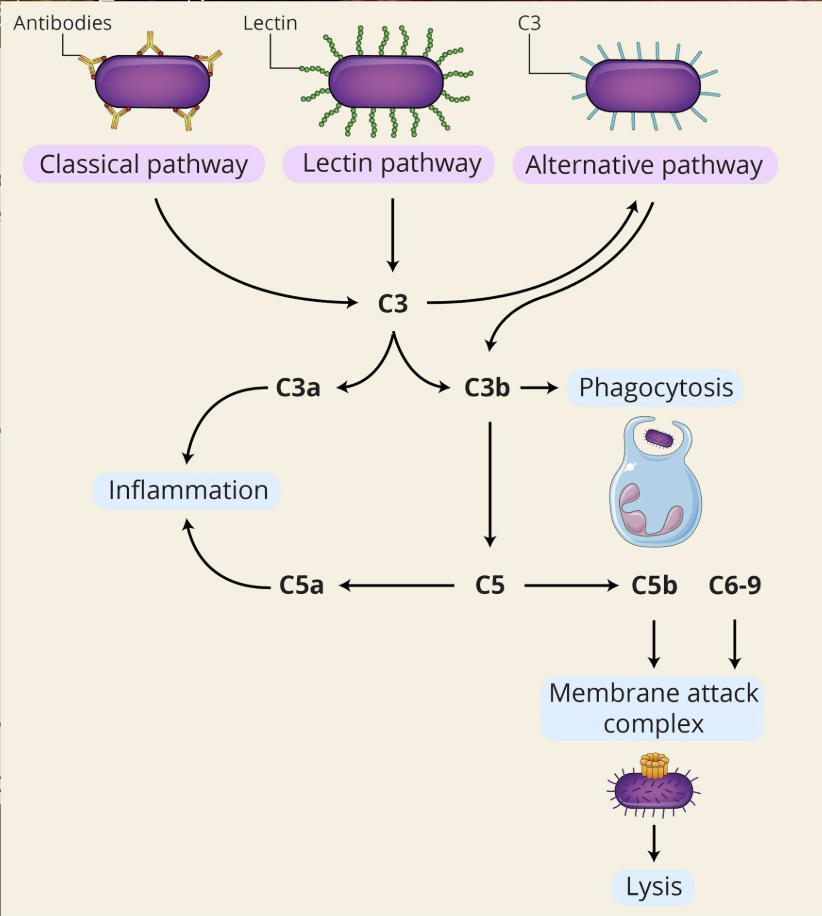
Soluble barrier - Complement system
the complement system is made up of over 30 proteins
complement proteins circulate in the blood, normally in an inactive form
the complement system can be directly activated in the presence of extracellular pathogens or indirectly by pathogen-bound antibodies
activation includes a cascade of reactions between various complement proteins, leading to the formation of a Membrane Attack Complex (MAC) and, in parallel, enhances the efficiency of other immune functions such as inflammation and phagocytosis
soluble barrier complement system - functions
the complement system can be activated through three major pathways: classical, alternative, and lectin pathways.
When activation of the complement system is initiated, it leads to a series of interactions between complement proteins, releasing activated forms of these proteins which together carry out a number of basic functions.
Inflammation:
the inflammation process includes the attraction of various immune cells to the site of infection through the release of chemotactic molecules, such as histamine and cytokines
activated compliment proteins bind to complement receptors on immune cells, such as mast cells and basophils, inducing the release of these substances, which enhance the inflammatory response
Phagocytosis:
activated complement proteins, predominantly C3b, opsonize (bind and mark for destruction) pathogens thereby targeting them for destruction by phagocytes
Membrane Attack Complex (MAC):
one of the ultimate complement system functions is to destroy extracellular foreign invaders through the formation of MACs
the MAC structures create holes in the pathogen which leads to its lysis and death
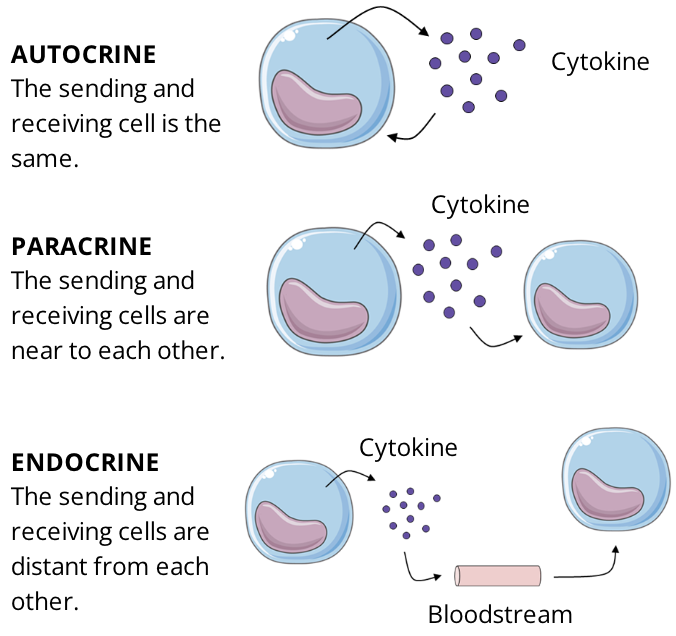
soluble barrier - cytokines
cytokines are small proteins secreted by various immune cells in response to number of different stimuli
they are chemical mediators that play a key role in cell-cell communication
a large variety of cytokines exist and they each have a strong affinity for a specific type of cytokine receptor
the cytokine receptors are expressed on the cell surface of various immune cells depending on their needs/functions
the function of cytokine signalling is to regulate immune processes such as immune responses, inflammation, and hematopoiesis
soluble barrier - characteristics of cytokines
Autocrine vs Paracrine vs Endocrine:
characterize the location of action depending on the site of secretion of cytokines. The majority of cytokines act locally, having autocrine or paracrine effects
Autocrine: the sending and receiving cell is the same
Paracrine: the sending and receiving cells are close to eachother
Endocrine: the sending and receiving cells are distant from eachother
Specificity and Affinity:
cytokines bind to specific receptors on the membrane of their target cells
cytokines and their receptors exhibit very high affinity for each other
Alter Gene Expression:
cytokine binding to its receptor initiates a series of reactions that ultimately alter gene expression, which may affect cell growth and maturation, and have a role in the hosts response to infection and disease
Pro-inflammatory vs Anti-inflammatory cytokines:
pro-inflammatory cytokines are made by most immune cells. When secreted, these cytokines will induce an inflammatory response
anti-inflammatory cytokines are made by several immune cells and work to limit the inflammatory response within the body. They do so by inhibiting pro-inflammatory cytokine production and activating the immune cells that promote healing
Inflammation (overview)
when a pathogen evades the physical barriers of the innate immune system, the surrounding cells work to induce an inflammatory response
inflammation can be described as a series of biological reactions in response to the invasion of a harmful infectious agent
inflammation occurs as a localized tissue response to injury or invasion and has local and systemic effects in the body
Characteristics:
redness, heat, pain, swelling
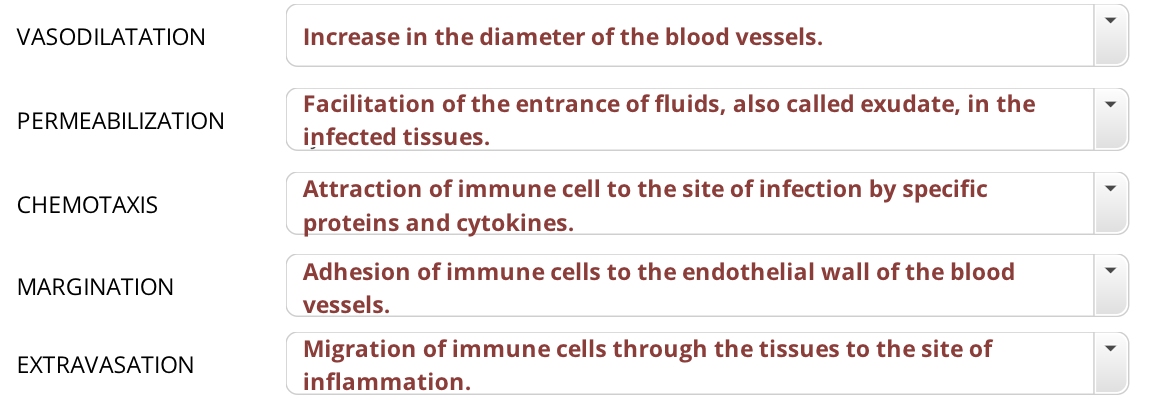
Events:
alteration of blood flow to the injured area
influx of phagocytic and other immune cells
removal of foreign antigens
healing of damaged tissues
the physical responses during inflammation can result in a loss of function, another common characteristic of inflammation
Purpose:
inflammation is the body’s attempt at self protection by removing barmful stimuli, including damaged cells, irritants, or pathogens
the purpose of inflammation is to localize and eliminate the invading pathogen, in an effort to stop it from spreading and remove damaged tissue
Inflammation step 1 - Breach
because the physical barrier is sealed, pathogens need to find a breach in order to be able to enter the body
this can happen in various ways, ie. a wound created by a nail or a piece of glass
an injury such as this will damage cells and give an opportunity for pathogens to break through the physical barrier
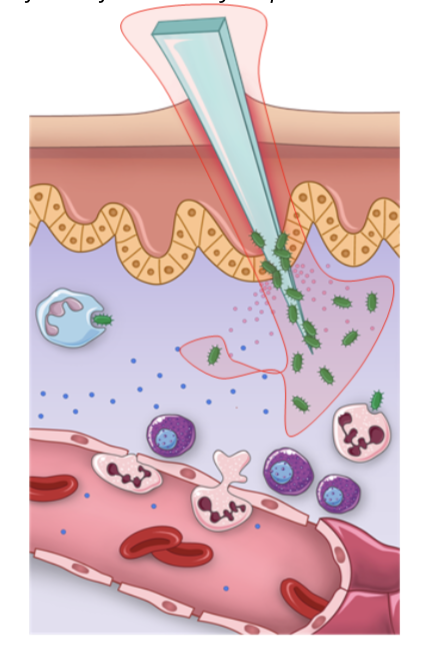
Inflammation step 2 - Vasodialation
vasodilation, an increase in the diameter of blood vessels and permeabilization of the capillaries near the affected area is the first major step in inflammation
these changes are induced by vasoactive and chemotactic factors secreted by damaged tissues and activated immune cels ie. macrophages and mast cells
the redness and heat are a consequence of the vasodilation inducing a higher blood volume around the infected area
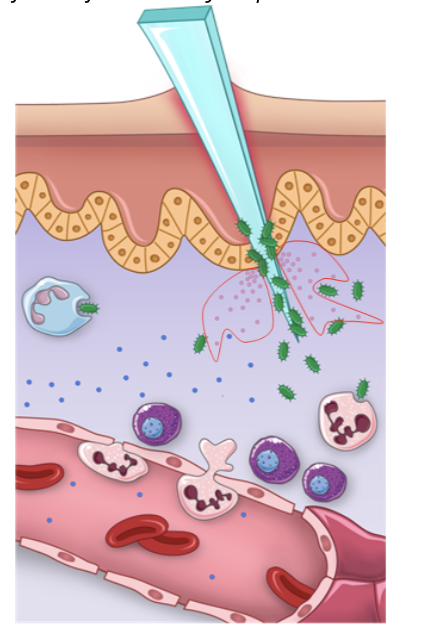
Inflammation step 3 - permeabilization
vasodilation, coupled with vasoconstriction of vessels carrying blood away, allows for accumulation of excess fluid at the site of infection, called exudate
the exudate fluid contains proteins that contribute to the mediation of the inflammatory response. It includes both pro-inflammatory cytokines, specifically a group called chemokines, and complement proteins that will be activated in the presence of extracellular pathogens
the function of these proteins is to attract the cellular barrier key players to the side of infection
the swelling characteristic of inflammation is a consequence of accumulation of fluids at the infection site, forming an edema
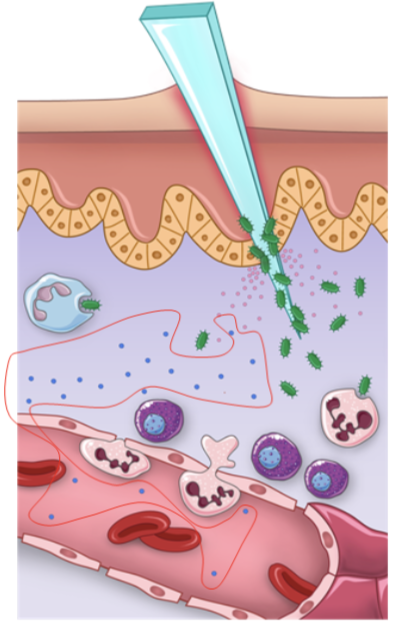
Inflammation step 4 - extravasation
the chemotactic factors released by cells during the vasodilation and permeabilization steps induce the recruitment of more immune cells to the site of infection
the first type of cells to arrive by chemotaxis to the site of infection are neutrophils
when neutrophils are circulating in the blood arrive to an infection site, they adhere to the endothelial cell walls via a process called margination and migrate between the capillary-endothelial cells into the infected tissue by a process called extravasation or diapedesis
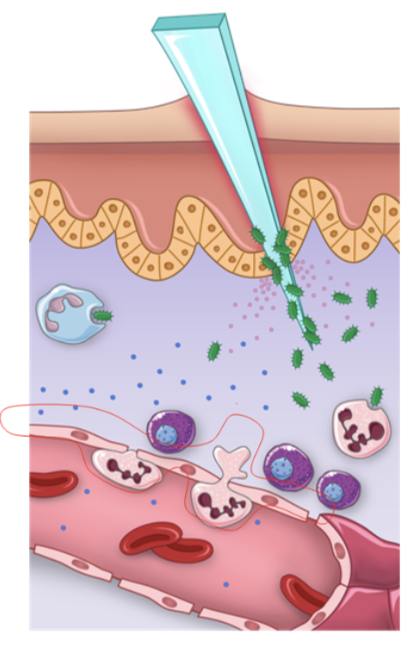
Inflammation step 5 - Phagocytosis
at the infection site, neutrophils and other phagocytes ie. macrophages and dendritic cells, engulf the pathogens
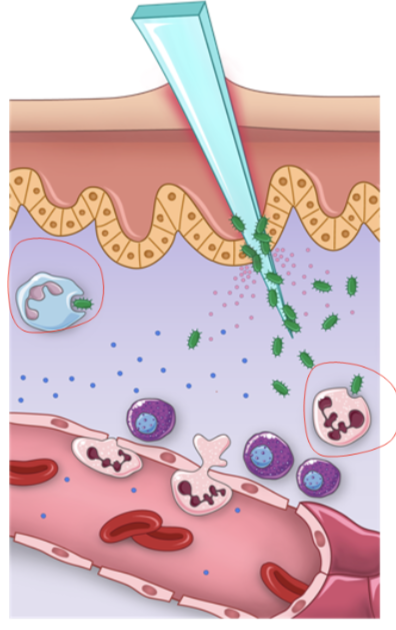
Inflammation summary graphic
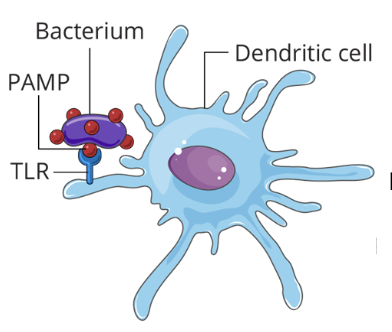
Pattern recognition receptors (PRRs)
innate immune cells have PRRs that are capable of recognizing repeated molecular patterns of pathogens
there are various families of PRRs, we will focus on Toll-Like Receptors (TLRs)
Molecular Patterns
the repeated molecular patterns recognized by PRRs are conserved motifs and certain subsets can be found in various groups of pathogens, where they are called pathogen associated molecular patterns (PAMPs)
PAMPs are molecular structures either expressed on the surface or found inside pathogens ie.
Lipopolysaccharides (LPS) found on the cell surface of gram-negative bacteria
Double stranded RNA found inside dsRNA viruses
these patterns are specific for pathogens and not found in host cells, which gives the ability to innate cells to distinguish non self from self
PAMPs
Pathogen-Associated Molecular Pattern
molecules associated with groups of pathogens that are recognized by immune cells. These include:
* functional structures of a pathogen
* repeated sequences of protein, glycoprotein, lipoprotein, and amino acids that are conserved across specific groups of microbes
this allows to initiate a quick response to infection by inducing an innate immune response
Examples of PAMPs include:
lipopolysaccharide
peptidoglycan
flagellin
viral nucleic acids
DAMPs
Damage-Associated Molecular Pattern
DAMPs are molecules released by stressed cells undergoing necrosis
these are host molecules, indicate damage to the body, initiate an inflammatory response
Examples:
abnormal location of cell structures ie. DNA found outside mitochondria or the nucleus
cell stress indicator molecules ie. heat-shock proteins
Toll-Like Receptors (TLRs)
TLRs are a class of PRRs whose signalling plays an essential role in the innate immune response
depending on the type of PAMP or DAMP it recognizes, TLRs are either expressed on the plasma membrane on endosomal/lysosomal membranes of mammalian cells
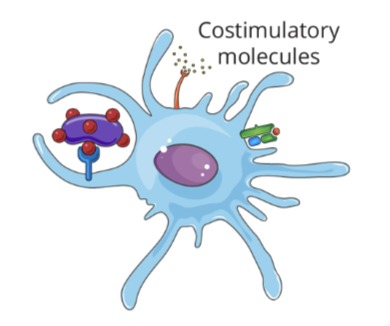
upon activation, these receptors initiate the transcription of genes encoding for
* inflammatory cytokines
* Chemkines
* Costimulatory molecules
these molecules contribute to the activation of innate immune cells, which increase the ability of phagocytes to engulf pathogens and enhance their ability to present antigens to the adaptive immune system
2 major roles of TLRs
recognize PAMPs and/or DAMPs
induce expression of signalling molecules to activate T cells
TLR signalling step 1
TLRs sense the presence of infection through recognition of PAMPs and/or DAMPs
The bacterium will be engulfed through phagocytosis by the phagocytic cell
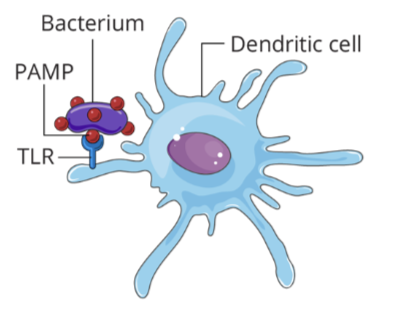
TLR signalling step 2
after engulfing the bacterium, the immune cell (AKA the antigen presenting cell), will present pieces of the antigens on its cell surface through the peptide:MHC complex
TLR signalling step 3
the antigen presenting cell will also increase its production of costimulatory molecules, which are involved in the strength and stability of the antigen presenting process
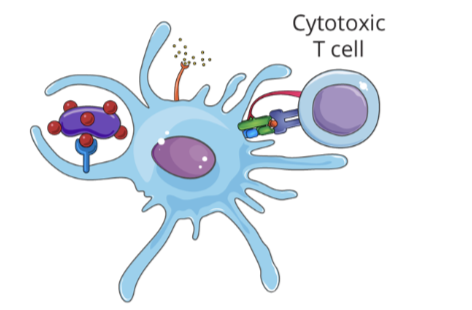
TLR signalling step 4
an immunocompetent naive T cell specific for the antigen presented by the dendritic cell will bind to the peptide:MHC complex through its TCR
this interaction will activate the T cell and initiate an adaptive immune response
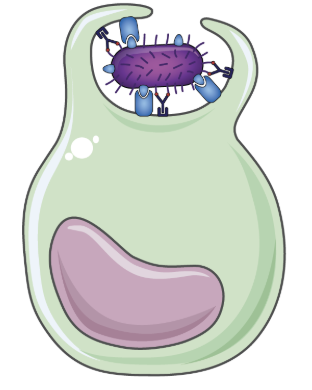
What is phagocytosis
phagocytosis is a type of endocytosis, in which a cell takes up particulate material from its environment by invaginating its membrane to form a vacuole
the recognition of a PAMP by a phagocyte through its PRR is one of the ways phagocytosis can be induced, or through pathogen opsonizatoin
Phagocytosis by neutrophils
the first cells to arrive from the blood to the site of infection
perform early phagocytosis, eliminating the pathogen quickly
can initiate an inflammatory response
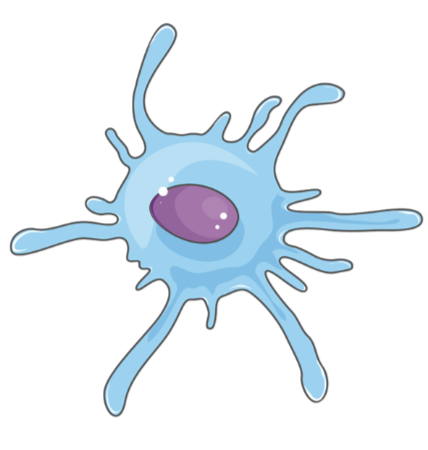
phagocytosis by macrophages
monocytes migrate from the blood to the tissues to become macrophages
perform phagocytosis most efficiently. (called “big eaters” lol)
release cytokines that stimulate inflammation and recruit other immune cells
Phagocytosis by dendritic cells
recognize microbes and initiate phagocytosis
the most efficient antigen presenting cell
play a major role in the adaptive immune response
Phagocytosis - attachment
the pathogen becomes attached to the membrane evaginations called pseudopodia
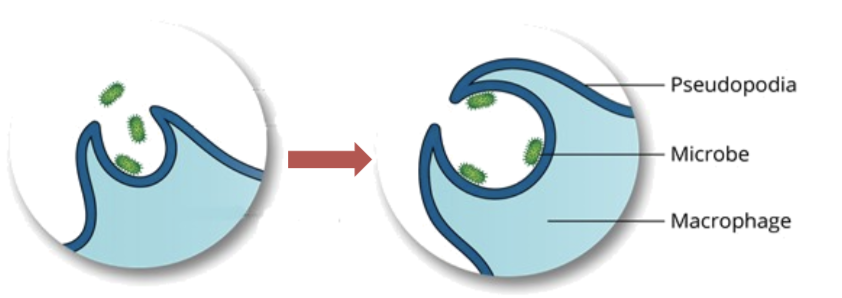
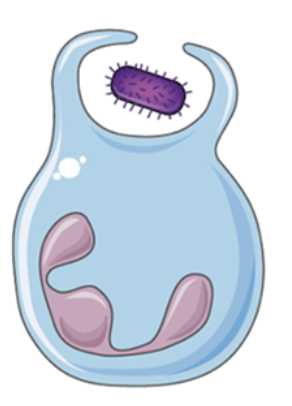
phagocytosis - ingestion
The pathogen is ingested, forming a vacuole, called a phagosome, within the cell
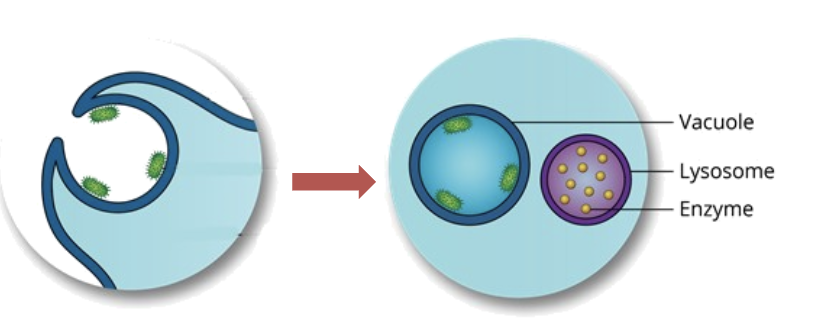
phagocytosis - fusion
The phagosome fuses with a lysosome, releasing lysosomal enzymes that degrade macromolecules and other materials such as bacteria
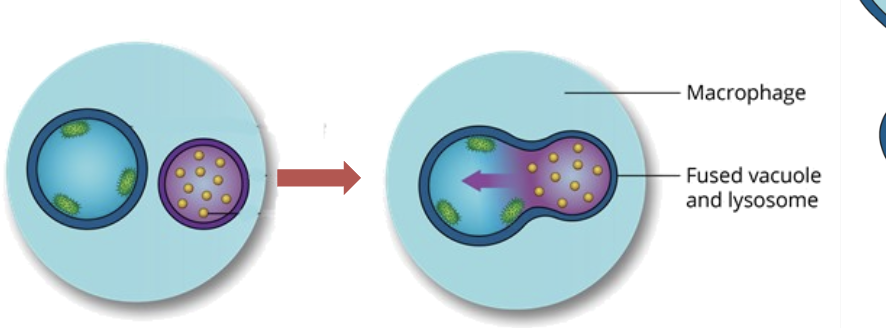
Phagocytosis - digestion
the pathogen is destroyed and digested by the lysosomal enzymes
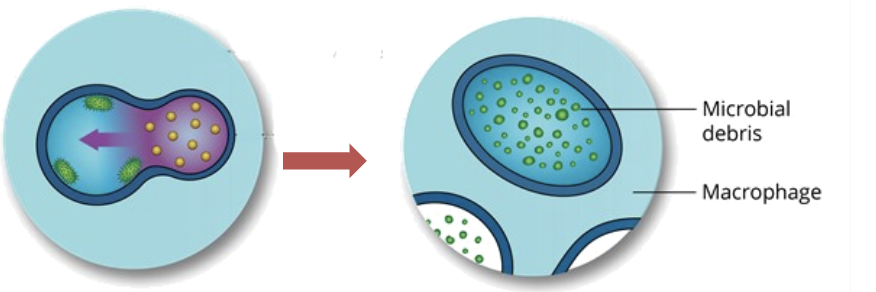
phagocytosis - release
the digestion products are released from the cell via exocytosis, the process in which the vacuole membrane fuses with the cell membrane

Inflammatory response summary
Vasodilation: facilitates the accumulation of blood, containing immune cells and soluble components, close to the site of infection
Permeabilization: facilitates the entrance of fluids (exudate) containing soluble components to the site of infection
Extravasation: migration of immune cells from the blood to the site of infection
Phagocytosis: destruction of pathogens by phagocytes
Adaptive immunity graphic
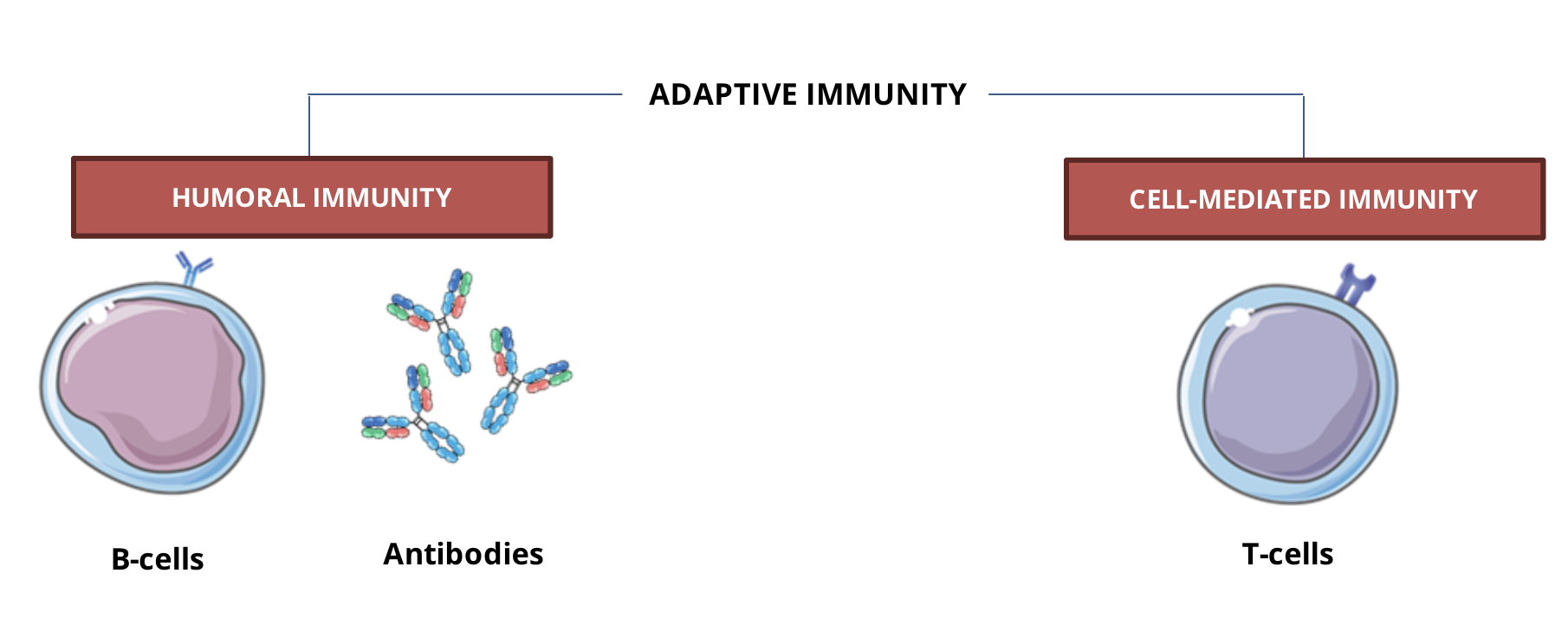
B cell characteristics
key component of the humoral response
mature in the bone marrow
surface receptor: B cell receptor (BCR)
function: antibody factory
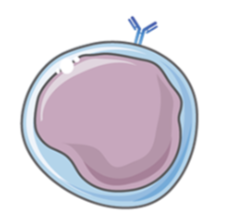
Plasmocyte
B cell subset
Effector B cell
Produce large quantities of antibodies
Memory B cell
memory cell
express BCR on their surface
T cell characteristics
Specificity
key component of the cell mediated response
mature in the thymus
surface receptor: T cell receptors (TCR)
function: cytotoxic activity OR help the activation of the immune response

CD4 Helper T cell
Effector T cell
help the activation of the adaptive immune response
CD8 Cytotoxic T cell
Effector T cell
kill infected cells
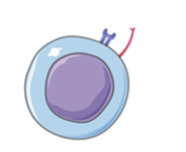
Memory T cells
Memory T cells
Express TCR and CD4 or CD8 on their cell surface
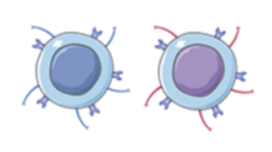
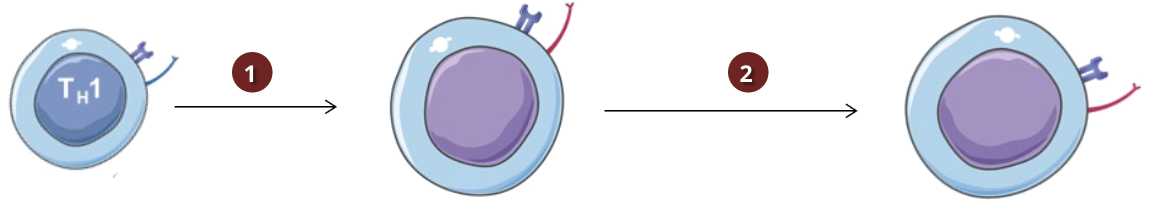
Humoral vs Cell Mediated Immunity (activation & differentiation)
Activation
Antigen presenting cells (ACPs), such as dendritic cells, that have engulfed pathogens by phagocytosis can present the antigens to naive CD4 helper T cells (Th)
Differentiation
depending on the type of antigen it encounters, Th cells can differentiate into 2 subsets:
To induce cell mediated immunity, activated Th cells will differentiate into a subset called Th1
To induce humoral immunity, activated Th cells will differentiate into a subset called Th2
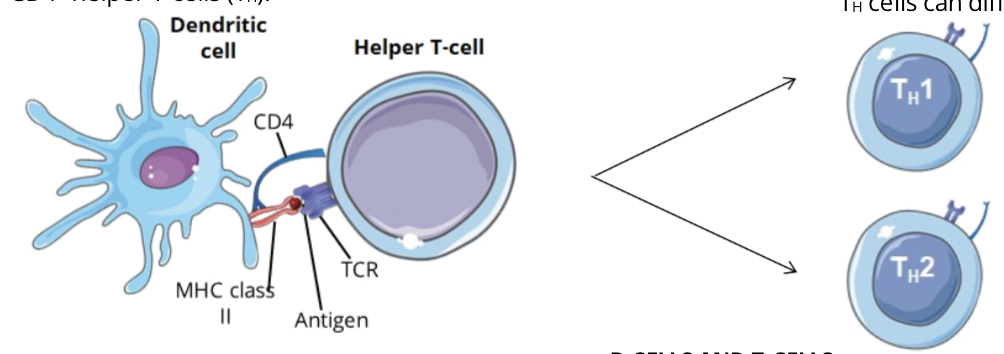
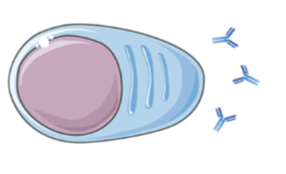
Humoral immunity and Th2 cells
Humoral immunity is characterized by B cells and is an antibody mediated response
Activated and differentiated Th2 cells activate B cells and induce their differentiation into plasmocytes
plasmocytes produce antibodies specific for the invading antigen
Cell mediated immunity and Th1 cells
Cell mediated immunity is characterized by T cells and is a cytotoxic mediated response
activated and differentiated Th1 cells activate CD8 cytotoxic T cells and induce their differentiation into cytotoxic T lymphocytes (CTLs)
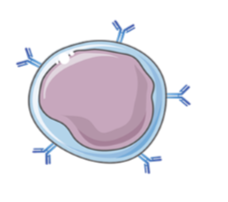
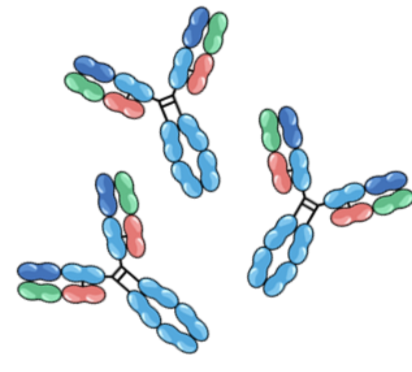
What are antibodies
an antibody, also called immunoglobulin or Ab, is a large, Y shaped protein
each antibody is highly specific and recognizes one epitope
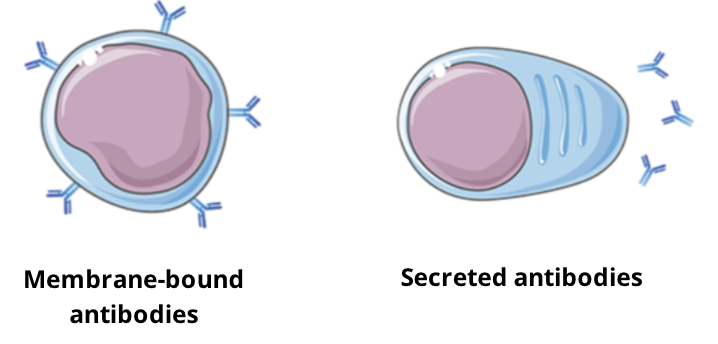
Where do antibodies come from
antibodies are produced by B cells and exist in 2 forms:
Surface antibodies: membrane bound on B cells, forming part of the B cell receptor (BCR)
soluble antibodies:secreted by B cells (plasmocytes) and circulate freely in the blood
one B cell will produce one specific antibody for one specific epitope
What are the functions of antibodies
antibodies play a key role in humoral immunity. They help eliminate a pathogen through various processes
Neutralization
neutralize the biological effect of a pathogen or toxin
Opsonization
mark foreign invaders for phagocytosis
Complement activation
induce the formation of membrane attack complexes (MACs) and opsonization
Effector cell activation
recognized by immune cells when bound to antigen and activate the cell’s effector functions
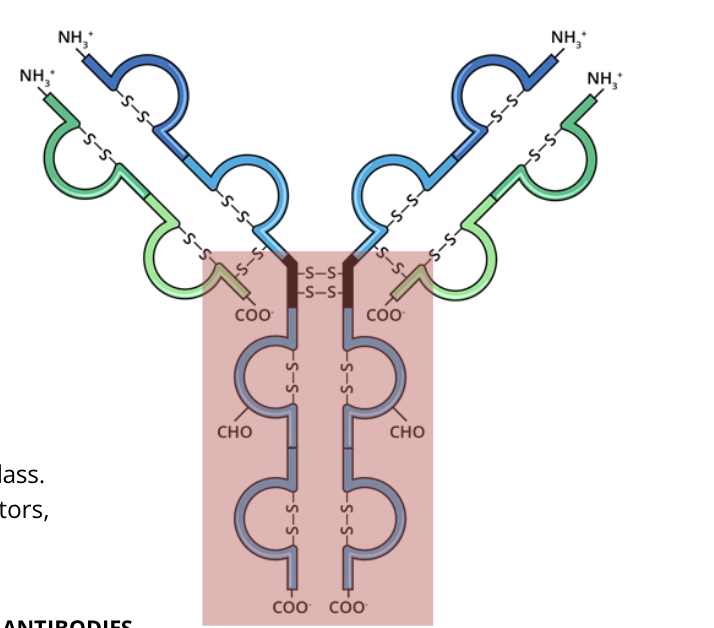
Basic structure of immunoglobulins
immunoglobulins are two heterodimeric (protein made of 2 different polypeptide chains) proteins that are held together by disulfide bonds
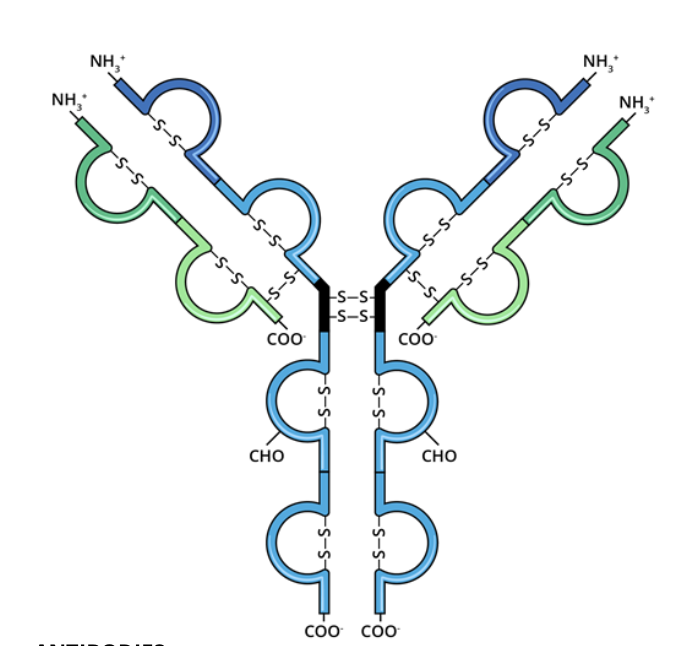
Basic structure of immunoglobulins: Light chains
the light chain is a protein subunit that, as one of a pair, forms part of the main antigen binding region of an antibody
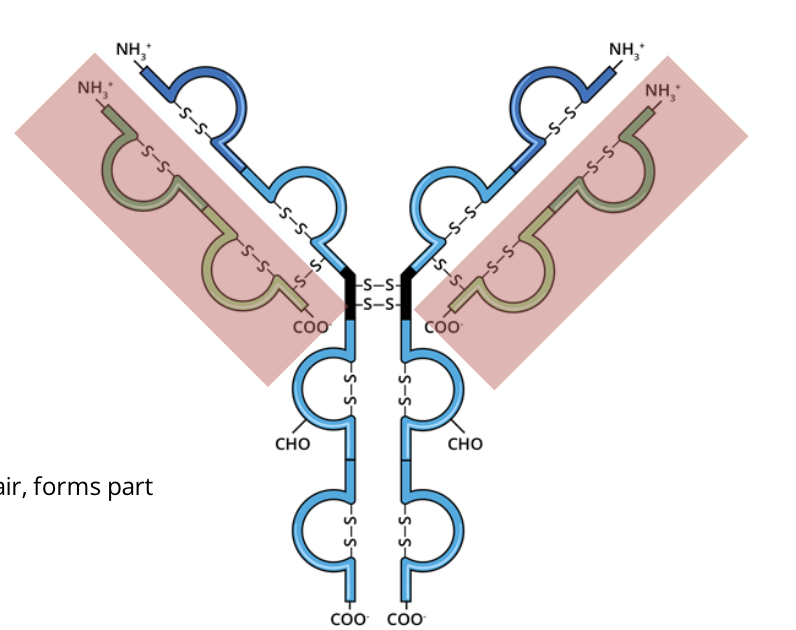
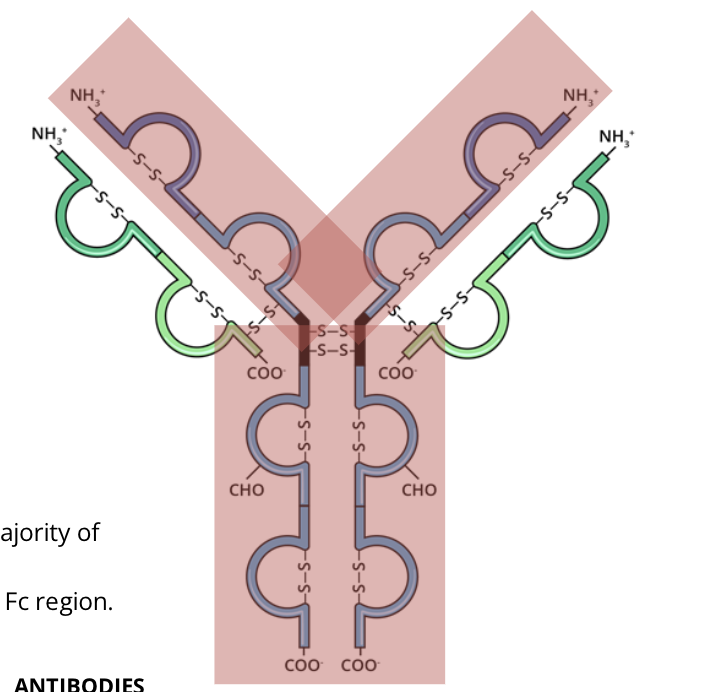
Basic structure of immunoglobulins: heavy chains
the heavy chain is a protein subunit that makes up the majority of the structure of the antibody. It forms part of the antigen binding region and forms the FC region
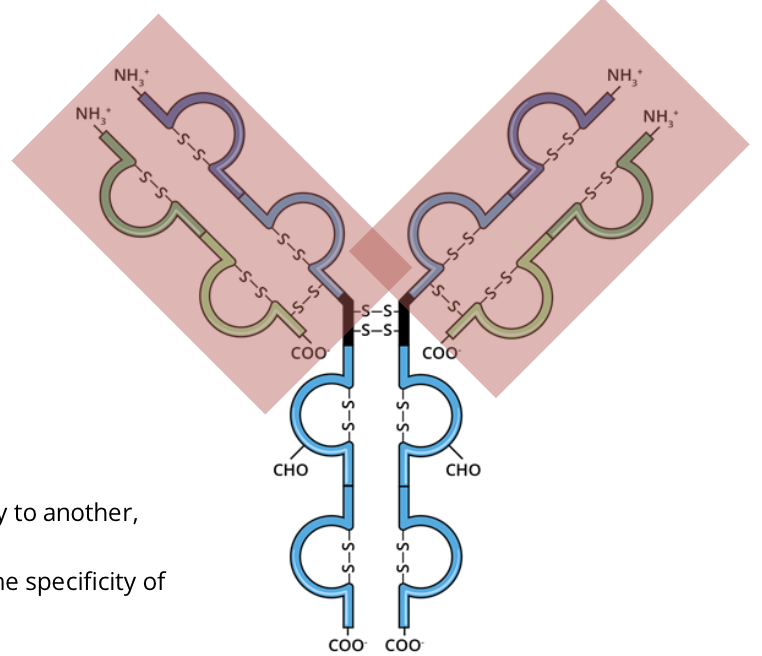
Basic structure of immunoglobulins: antigen binding regions
the antigen binding region is variable and changes from one antibody to another, but remain the same on one antibody.
these regions are responsible for the diversity and specificity of immunoglobulins
Basic structure of immunoglobulins: FC region (fragment crystallizable)
the FC region is constant for every antibody of the same class,
it is the part that interacts with immune cell surface receptors, called FC receptors
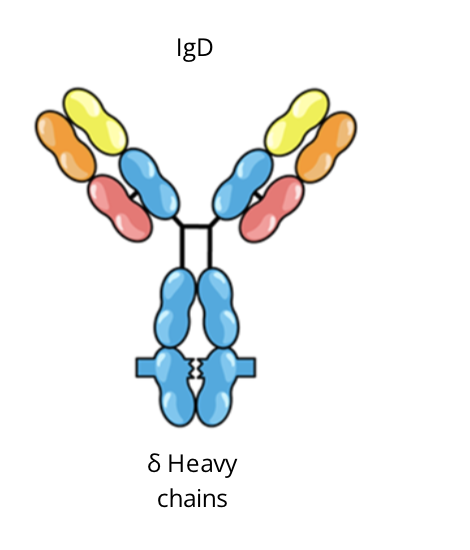
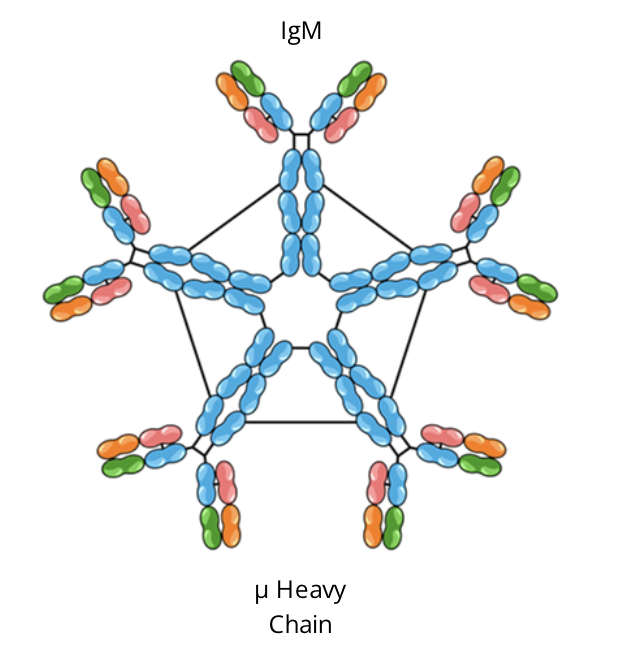
Classes of immunoglobulins
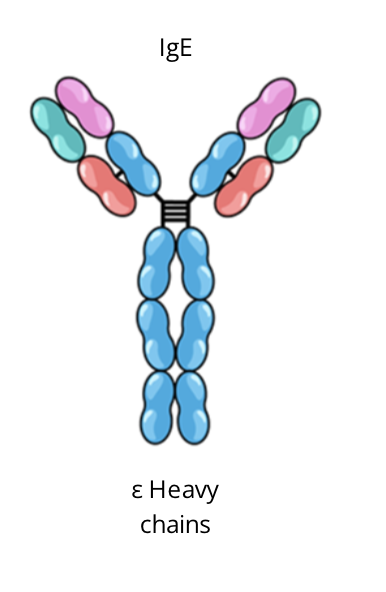
there are 5 classes of immunoglobulins, distinguished by the type of heavy chain in their structure
the unique heavy chain is what allows differentiation between classes
the variation in heavy chain polypeptides allows each immunoglobulin class to function in a different type of immune response or during a different stage of the body’s defence response
the specific amino acid sequences that confer these functional differences are located mainly within the FC domain
IgM immunoglobulins
form a pentameter from IgM monomers when secreted by B cells
first antibody to be formed in an immune response
activates the complement which then amplifies the inflammatory and adaptive immune response
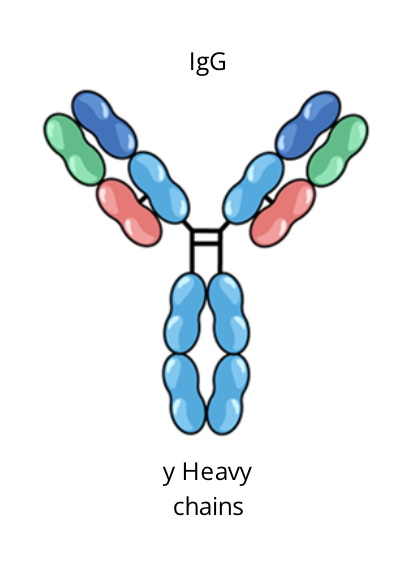
IgG immunoglobulins
monomer when secreted by B cells
coats pathogens to promote phagocytosis and immune cell recruitment
only class that can cross the placental barrier
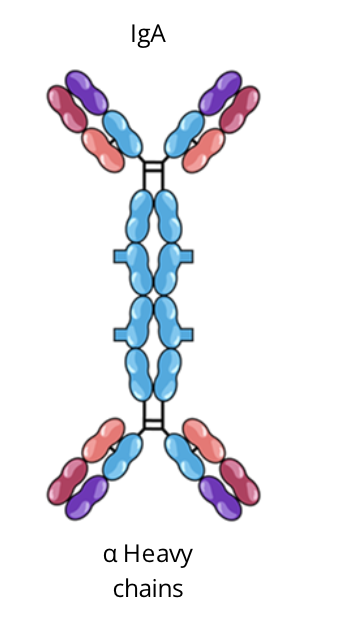
IgA immunoglobulins
generally forms a dimer from IgA monomers when secreted by B cells
first line of defence and predominant antibody class located in the body’s mucosal membranes
IgE immunoglobulin
monomer when secreted by B cells
produced in excess during allergic reactions
has a role in immunity agains certain parasites ie. helminths
IgD immunoglobulins
monomer when secreted by B cells
found in large quantity on the surfaces of mature B cells
function or importance is unclear, still under investigation; though to have a role in B cell development