W28 L1&2 - Circulation and Respiration
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
62 Terms
what is the systemic circulation
left side of heart → tissues → right side heart
arterial system: left ventricle → aorta → arteries → arterioles → branch capillaries
what is pulmonary circulation
right ventricle → lungs → left ventricle
where does the blood go once it has reached the capillaries
venus system: small vessels → venules → veins → Vena cava → RHS
what is cardiac output
total blood flow
where does exchange of material take place, why
capillaries
because they have a leaky epithelium which allows the exchange of materials
what can’t capillaries control, why
can’t control blood flow because they don’t have much smooth muscle in their walls
what allows arteriole movement
smooth muscle in their wall allows them to constrict and dilate
means they can have variable resistance to blood flow
can distribute blood across different tissues by selectively constricting and dilating
which end connects capillaries to the venus system
at the distal end of capillaries, blood flows into the venous side of circulation
what important function do veins have
act as a volume reservoir
if blood pressure falls to low, allow blood to be sent to arterial side to increase bp
describe the composition of 5 blood vessels
Artery
diameter 0.1 -10+ mm
mean wall thickness - 1mm
composition - small amount of endothelium, lots elastic tissue and more smooth muscle, some fibrous tissue
Arteriole
diameter 10-100 micrometers
mean wall thickness - 6 micrometers
composition - small amount of endothelium, no elastic tissue, some smooth muscle, no fibrous tissue
Capillary
diameter 4 -10 micrometers
mean wall thickness - 0.5 micrometers
composition - small amount of endothelium
Venule
diameter 10 - 100 micrometers
mean wall thickness - 1 micrometer
composition - small amount of endothelium, some fibrous tissue
Vein
diameter 0.1 -100+ mm
mean wall thickness - 0.5mm
composition - small amount of endothelium, some elastic tissue and more smooth muscle, some fibrous tissue
what is the composition of blood vessels like generally
inner lining is a thin layer of endothelial cells that secrete paracrine signals
walls
elastic tissue - connective tissue elasticity (endothelial layer + adjacent elastic tissue = tunica intima)
vascular smooth muscle - arranged in circular or spiral layers. contractions depends on Ca2+ entry. most bv smooth muscles maintain partial state of contraction - muscle tone influenced by signal molecules (hormones, neurotransmitters)
fibrous tissue - connective tissue, stiffness
how is the pressure maintained in the circulatory system
pressure stored in the elastic walls of the arteries and contained by stiffness of fibrous tissue
what can the arteriole walls do, under the influence of what
arteriole walls can contract and relax under the influence of chemical signals
what are capillaries made from, because of this what do they have
consist of one flat layer of endothelium, one cell thick, so are supported on an extracellular matrix - the basal lamina
what are pericytes
highly branched contractile cells wrapped around the capillaries which contribute to the tightness/leakiness of capillaries
which cells help to control the blood flow through capillaries
pericytes - contractile cells which wrap around the capillaries
how does blood flow back from microcirculation and the venus system
blood flows from capillaries into venules
they are distinguished from capillaries by their convergent pattern of flow
blood flows from venules to veins
some veins have one way valves to prevent backflow
veins have thinner walls than arteries, with less elastic tissue and expand easily
veins more numerous than arteries, larger diameter, hold more blood, lie close to body surface
skeletal muscle pressure on veins can help force blood up and valves then stop it from going back
cellular vs external respiration
cellular - intracellular reaction
external - movement of gasses between the environment and the body’s cells
what is the respiratory tract divided into
upper and lower regions
lower tract also called the thoracic portion
Upper
mouth
nasal cavity
pharynx
larynx
Lower
trachea
2 primary bronchi
their branches
lungs
what does pleural fluid do and where is it
lowers friction between membranes
holds lungs tight against thoracic wall
found between pleural membranes
what is pleurisy
inflammation of the pleura
makes breathing laboured
usually caused by another condition e.g infection
what is pleural effusion
when pleural fluid accumulates
e.g TB, also when body fluid volumes are disturbed
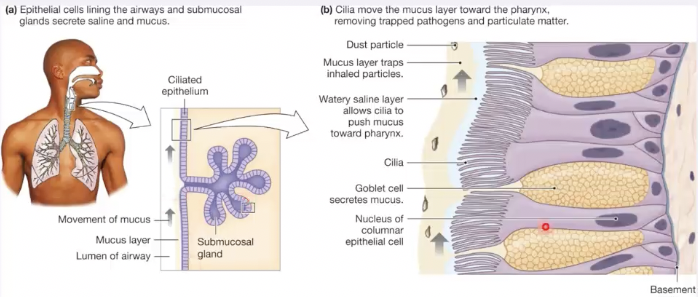
importance of ciliated epithelium cells in the airway
allow movement of mucus (secreted by goblet cells) up towards the pharynx and remove any trapped pathogens or any trapped particulate
what can occur within ciliated epithelium cells
sub mucosal glands
what are the types of alveolar cells and what do they do
type I - gas exchange
type II - produce surfactant
what condition can lead to a change in mucus consistency
cystic fibrosis
a failure of the CFTR receptor leads to thick, sticky mucus that causes the deep diseases pathology seen in CF
what are the two types of breathing
quiet (passive) breathing
normal breathing requires very little muscle contraction
diaphragm is the dominant muscle involved in quiet respiration
forced (active) breathing
deeper breathing due to increased physical activity
also deliberate breath control (singing, inflating a balloon)
several muscles involved in forced inspiration and expiration
what is the inner lining of the blood vessels called
endothelium
which muscles are used for quiet expiration
diaphragm
what are anatomical aspects which impact lung function/breathing
lungs (bronchi, bronchioles, alveoli)
chest cavity (ribs, intercostal muscles) and the diaphragm muscle
pleural membranes (pleural fluids and pleural pressure)
what are functional aspects which impact lung function/breathing
passive (shallow) breathing - lung elasticity (recoil), pressure gradients
active (deep) breathing - different muscles involved larger tidal volumes up to vital capacity (maximum)
when does inspiration occur
when alveolar pressure decreases
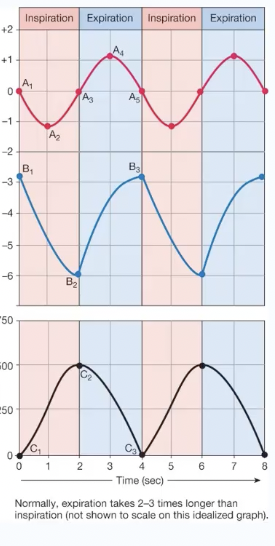
explain what is occuring in this image
ventilation
time 0 - when pressures are equal there is no air flow
time 0-2 - inspiration
time 2-4 - expiration (occurs when alveolar pressure increases)
time 4 - passive vs active respiration
is pulmonary ventilation or alveolar ventilation great
which one is a better indication of how much fresh air reaches the alveoli
pulmonary ventilation is greater because of dead space
alveolar ventilation is better because fresh air remaining in the dead space does not get to the alveoli
what is dead space
Dead space (Vd) is the portion of each tidal volume that does not take part in gas exchange and includes:
anatomical dead space (Vdaw), that is the part of airways that do not contribute to gas exchange (nose, pharynx, conduction airways
(Vdalv) alveoli which are well-ventilated but poorly perfused
how can lung function be measured
using a spirometer
when patient breathes in, air moves into the lungs, the volume of the bell decreases, the pen rises on the tracing
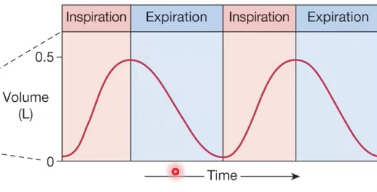
define tidal volume
the amount of air moved in or out of the lungs at rest (i.e. quiet/passive/shallow breathing)
~500ml
define expiratory reserve volume (ERV)
the extra volume of air that can be forcibly blow out of the lungs, additional to that exhaled in the tidal volume
what is inspiratory reserve volume (IRV)
the extra volume of air that can be forcibly sucked into the lungs, additional to that normally inhaled in tidal volume
what is vital capacity
the total volume of air that can be breathed in and out of the lungs
TV+ERV+IRV
how to measure capacities
inspiratory capacity
vital capacity
total lung capacity
functional residual capacity
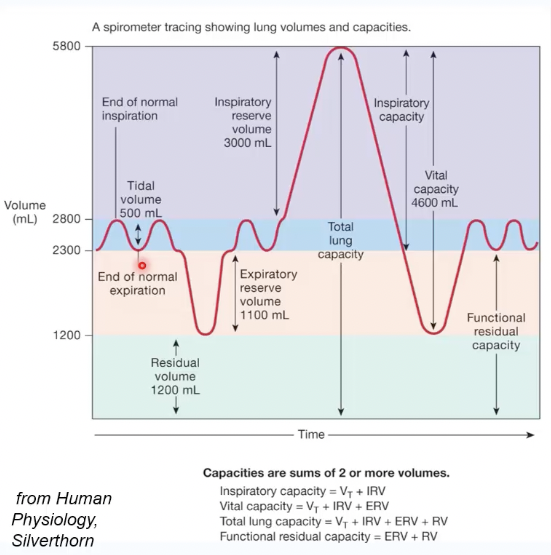
lung values of men and women
IRV
TV
ERV
VC
RV
TLC
IRV
men - 3000
women - 1900
Tidal Volume
men - 500
women - 500
ERV
men - 1100
women - 700
Vital Capacity
men - 4600
women - 3100
Residual volume
men - 1200
women - 1100
Total lung capacity
men - 5800mL average 70kg man 28yr
women - 4200mL average 50kg woman 28yr
what two important measures are used to monitor lung function
forced vital capacity (FVC)
the total amount of air that you blow out in one deep breath
FVC varies with age, weight, sex, etc but most significantly can be reduced in disease
forced expiratory volume in 1 sec (FEV1)
the amount of air you can blow out within one second
what is the diversity in lung capacity like
well documented that there are differences by ethnicity and geographic location
much debate as to reasons for this
it changes even more in children
within India (well cited example) can be significant differences between ethnicities
for this reason hard to give one set of standards
COVID-19 highlighted issue of diversity h
which lung volume cannot be directly measured
residual volume
what is hypoxia
too little oxygen
what is hypercania
increased conc in CO2
how can the body avoid hypoxia and hypercania
regulate
oxygen
carbon dioxide
pH
give a brief overview of gas exchange
oxygen enters blood at alveolar-capillary interface
oxygen is transported in blood dissolved in plasma or bound to haemoglobin inside RBCs
oxygen diffuses into cells
CO2 diffuses out of cells
CO2 is transported as dissolved, bound to haemoglobin, or as HCO3-
CO2 enters alveoli at alveolar-capillary interface
what do individual gases diffuse along during ventilation
what does the total pressure of mixed gas equal to
they diffuse along partial pressure gradients until equilibrium
total pressure of mixed gas = sum of particle pressures of individual gases
gas exchange between alveoli and blood
what is the partial pressure like of alveolar air compared to that of blood
what does this mean
PO2 of alveolar air is higher than the PO2 of blood
means diffusion will occur towards the blood
gas exchange between blood and tissues
what is the partial pressure like of the blood compared to the tissues
what does this mean
PO2 of blood is higher than PO2 of tissues
means diffusion will occur towards the tissues
How does gas solubility affect oxygen and carbon dioxide transport between alveoli and blood?
Oxygen has low solubility in water, so at equilibrium, its concentration in liquid remains much lower despite equal partial pressures.
Carbon dioxide is more soluble, meaning more CO₂ dissolves in liquid at the same partial pressure.
Unlike solids, gases like oxygen are more soluble in cold water than in warm water.
Since blood is warm, oxygen's lower solubility and CO₂'s higher solubility impact how they are transported in the bloodstream.
Oxygen (O₂) Transport:
Poorly soluble in plasma → only ~2% dissolves.
~98% binds to haemoglobin in red blood cells for transport.
Carbon Dioxide (CO₂) Transport:
More soluble than O₂ → ~7-10% dissolves in plasma.
~20-30% binds to hemoglobin as carbaminohemoglobin.
~60-70% is converted to bicarbonate (HCO₃⁻) for transport.
Impact on Gas Exchange:
In the lungs, O₂ binds to haemoglobin, and CO₂ is released for exhalation.
In the tissues, O₂ is released, and CO₂ is picked up for transport back to the lungs.
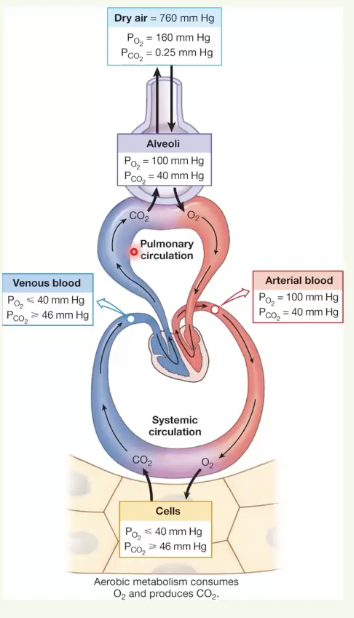
what is the partial pressure of oxygen and carbon dioxide throughout gas exchange
Dry Air
PO2 ≈ 160 mmHg
PCO2 ≈ 0.25 mmHg
Inhaled air (Alveoli):
PO2 ≈ 100 mmHg
PCO2 ≈ 40 mmHg
Arterial Blood (Leaving Lungs):
PO2 ≈ 100 mmHg (matches alveoli, fully oxygenated)
PCO2 ≈ 40 mmHg
Tissues (Oxygen Delivery & CO₂ Pickup):
PO2 ≈ 40 mmHg (lower due to cellular respiration)
PCO2 ≈ 45 mmHg (higher due to metabolism)
Venous Blood (Returning to Lungs):
PO2 ≈ 40 mmHg (deoxygenated)
PCO2 ≈ 45 mmHg
if plasma pH increases from 7.40 to 7.48m haemoglobin’s affinity for oxygen will … so … oxygen will be released to the tissue
increased, less
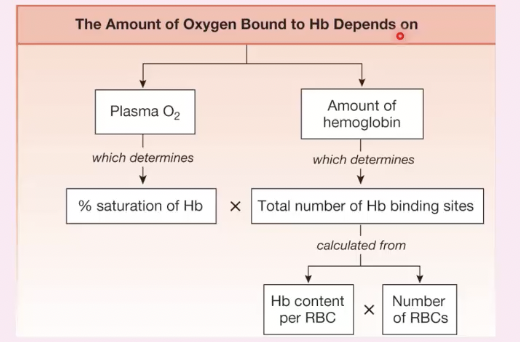
How does haemoglobin help transport oxygen in the blood?
Oxygen (O₂) first dissolves in plasma but accounts for <2% of total O₂ in blood
O2 not good at dissolving in liquids so haemoglobin helps transport around body
Haemoglobin (Hb) binds O₂ to form oxyhemoglobin (HbO₂).
Reaction: Hb + O₂ ⇌ HbO₂ (oxyhemoglobin).
Each haemoglobin molecule has 4 heme groups, allowing it to bind 4 O₂ molecules.
>98% of O₂ is transported by haemoglobin to tissues.
what protein helps increase movement of O2 into plasma
haemoglobin essentially sequesters O2 out of the plasma so that more can move from the alveoli into the plasma
wouldn’t get enough oxygen to our tissues if it was left to just being in the plasma
How does haemoglobin increase oxygen-carrying capacity in the blood?
Without haemoglobin:
O₂ dissolves in plasma, carrying only 3 mL O₂/L blood.
no O2 in RBC
With haemoglobin (at normal PO2):
Haemoglobin binds 98% of O₂, increasing total O₂ transport to 200 mL O₂/L blood.
3mL O2/L in blood in plasma
197mL O2/L in blood in RBC
At reduced PO2 (e.g., in tissues):
Haemoglobin releases some O₂, reducing carrying capacity to 100.3 mL O₂/L blood.
0.8mL O2/L in blood in plasma
99.5mL O2/L in blood in RBC
Key Concept: Hemoglobin vastly increases O₂ transport beyond plasma solubility limits and releases O₂ where needed.
what factors affect the binding of haemoglobin to oxygen
Partial Pressure of Oxygen ( PO2 ):
Higher PO2 (lungs) → More O₂ binds to hemoglobin (HbO₂ formation).
Lower PO2 (tissues) → O₂ is released for cellular use.
pH (Bohr Effect):
Low pH (acidic, ↑CO₂, ↑H⁺) → O₂ unloads more easily (right shift in curve).
High pH (alkaline) → Hb holds onto O₂ more tightly (left shift).
Carbon Dioxide (CO₂) Levels:
↑ CO₂ lowers pH and promotes O₂ release.
↓ CO₂ raises pH, increasing O₂ binding.
Temperature:
↑ Temperature (active tissues) → More O₂ is released (right shift).
↓ Temperature (lungs) → More O₂ binds (left shift).
what is cooperative binding
what happens in the reverse of this
The binding of the first oxygen molecule results in a conformational change in the structure of the haemoglobin molecule, making it easier for each successive oxygen molecule to bind
4 polypeptides in Hb
s shape curve of graph shows cooperativity - not linear
The reverse of this process happens when oxygen dissociates in the tissues
compared with other ways for this protein to work, the cooperative binding allows release of more oxygen at tissues and good binding in the lungs
give a brief overview of carbon dioxide transport
CO2 diffuses out of cells into systemic capillaries
only 7% of the CO2 remains dissolved in the plasma
nearly a fourth of the CO2 binds to haemoglobin, forming carbaminohaemoglobin
70% of the CO2 is converted to bicarbonate and H+
Haemoglobin buffers H+
HCO3- enters the plasma in exchange for the Cl- (the chloride shift)
at the lungs, dissolved CO2 diffuses out of the plasma
by the law of mass action, CO2 unbinds from haemoglobin and diffuses out of the RBC
the carbonic acid reaction reverses, pulling HCO3- back into theRBC and converting it back to CO2
the oxygen-Hb dissociation curve shifts to the right in response to
↓ pH (Bohr Effect) → More H⁺ ions (acidic conditions) reduce Hb's O₂ affinity.
↑ CO₂ Levels → Forms carbonic acid, lowering pH and promoting O₂ unloading.
↑ Temperature → Metabolically active tissues need more O₂.
A right shift means better O₂ delivery to tissues under conditions of high demand.