Kidney Pathology
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Signs & Symptoms: Renal Cystic Disease:
–Flank pain
– Hematuria
– Proteinuria
– White blood cells in urine
– ↑ Protein
–Inflammatory or necrotic cysts
Signs & Symptoms: Renal subcapsular hematoma:
– Hematuria
– ↓ Hematocrit
–Renal Inflammatory Processes
Signs & Symptoms: Abscess
– Acute onset of symptoms
– Fever
– Palpable mass
– ↑ White blood cell count
– Pyuria
Signs & Symptoms: Acute focal bacterial nephritis:
–Fever
– Flank pain
– Pyuria
– ↑ Blood urea nitrogen
– ↑ Albumin
– ↑ Total plasma proteins
Signs & Symptoms: Acute tubular necrosis:
– Moderate to severe intermittent flank pain (caused by renal calculi)
– Vomiting (caused by renal calculi)
– Hematuria
– Infection
– Leukocytosis with infection
Signs & Symptoms: Chronic renal failure:
–↑ Concentration of urea in blood
– High urine protein excretion
– ↑ Creatinine
– Presence of granulocytes
Signs & Symptoms: Renal cell carcinoma:
– Erythrocytosis may occur
– Leukocytosis
– Red blood cells in urine
– Pyuria
– ↑ Lactic acid dehydrogenase
Renal Cystic Disease
•Simple renal cystic disease encompasses a wide range of disease processes, which may be typical, complicated, or atypical. (rounded, acoustic enhancement)
Simple Renal Cyst
•The most common renal mass lesion is a simple cortical renal cyst.
•Solitary or multiple, involving one or both kidneys.
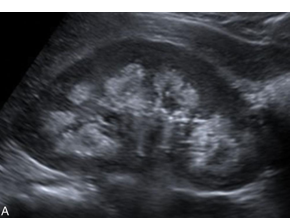
Sonographic Findings - Simple Renal Cyst
•A round or oval shape, anechoic, thin walls, and posterior acoustic enhancement.

Simple Renal Cyst
•Most common mass.
•Arises from the cortex
•Patient will be asymptomatic
•May be single or multiple involving one or both kidneys.
•Local pain and hematuria may be caused by the distention of the cyst wall or spontaneous bleeding in the cyst.
•Classical sonographic criteria to diagnose simple real cyst is it is round or oval, anechoic, thin walls, and posterior enhancement.
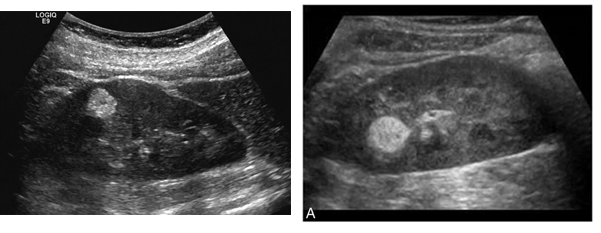
Complex Cyst
•May be considered as a malignant until proven otherwise
•It may contain septations, thick walls, calcifications, internal echoes, and mural nodularity
•Sonographic Findings: thick wall, with internal echoes due to hemorrhage or infection.(anechoic with debris)
•Contains thin septa
•If irregularity of septa seen showing vascularity on color Doppler or Power Doppler, should be considered as malignant
Sonographic Considerations for Renal Mass
• Evaluate the renal vein and inferior vena cava into the right atrium to look for thrombus/tumor.
Von Hippel-Lindau
•: is an autosomal dominant condition.
•Several areas of the body may be affected, which include Retinal angiomas, Cerebellar hemangioblastoma, and a variety of abdominal cysts and tumors, including Renal and pancreatic cysts, Renal adenomas, and bilateral renal adenocarcinomas. Renal cell carcinoma in patients with this disease is multifocal and bilateral. A high incidence of renal cysts is found in patients with Von Hippel–Lindau disease, usually of cortical origin.
Tuberous Sclerosis:
•an autosomal dominant condition characterized by mental retardation, seizures, and adenoma
Acquired Cystic Kidney Disease
•Found in the native kidneys of patients with Renal Failure and who needs dialysis (atrophic kidneys – smaller kidney, look for the cortex)
•Patient will have an increased incidence of renal cysts, adenomas, and renal carcinoma. (on dialysis)
•Renal cyst shows spontaneous bleeding and hemorrhage, causing flank pain and discomfort.
Sonographic Findings for Acquired Cystic Kidney Disease:
–The native kidney is small and echogenic with several small cysts
Autosomal Recessive Polycystic Kidney Disease AKA Infantile Polycystic Kidney Disease
•Autosomal recessive polycystic kidney disease (ARPKD) was previously called infantile polycystic disease and is a rare genetic disorder. (multiple cysts on the infants kidneys)
•The juvenile form may present with hypertension, renal insufficiency, nephromegaly, hepatic cysts, bile duct proliferation, and Caroli disease, which may be associated with periportal fibrosis.
•In older children, the kidneys are enlarged with an echogenic cortex and medulla and lack of corticomedullary differentiation.
The difference between Recessive and Dominant Autosomal Polycystic Kidney Disease:
Recessive - found in infant to 39 yrs old
Dominant - found in 40 and over
Autosomal Dominant (adult) Polycystic Kidney Disease (ADPKD)
•Doesn’t manifest until 40yrs old
•Associated abnormalities include cysts in the liver, spleen, pancreas, thyroid, ovary, testes, or breast; cerebral berry aneurysm; and abdominal aortic aneurysm. Patients who are on renal dialysis have an increased incidence of renal cell carcinoma.
•Usually bilateral but not fatal.
•On ultrasound bilateral renal enlargement with multiple asymmetric cysts of varying size in both cortex and medulla.
•The walls may be calcified, and renal stones may form.
Multicystic Dysplastic Kidney Disease
•Most common cause of an abdominal mass in newborns.
•Usually unilateral, may be bilateral.
•Fatal if bilateral
• Cysts of varying size and shape with the absence of renal parenchyma
•Associated renal anomalies include:
- Contralateral UPJ obstruction
-Horseshoe kidney
Medullary Cystic Kidney Disease and Nephronophthisis:
•Inherited disorders that eventually lead to End-stage renal disease (ESRD).
•They are grouped together because they share many features. Pathologically, they cause cysts restricted to the renal medulla or corticomedullary border.
Medullary nephrocalcinosis
Renal Angiomyolipoma
•Most common benign renal tumor
•Composed of varying proportions of fat, muscle and blood vessels.
•Hyperechoic benign renal tumor. Its echogenicity is greater than or equal to that of the renal sinus.
Renal Adenomatous Tumors:
- Patients are usually asymptomatic
- these tumors may cause hematuria
Sonographic findings for Renal Adenomatous Tumors:
–These tumors appear as solid masses on sonography, are hyperechoic to hypoechoic in echotexture, and are hypovascular on color Doppler.
Renal Cell Carcinoma (Hypernephroma):
- Most common renal mass in adults.
- Usually unilateral encapsulated mass.
Sonographically, it is hypoechoic relative to the normal adjacent renal parenchyma.
-Treated with nephrectomy and wedge resection
- Patient presents with hematuria (blood in urine), pain, and palpable mass.
-Tumor extension into the renal vein and IVC is common
-The lungs are the most common site for distant metastases. Lymph nodes, liver, bone, adrenal glands, and contralateral kidney are also metastatic sites.
Increased incidence associated with Renal Cell Carcinoma (Hypernephroma):
-Acquired cystic disease (chronic dialysis)
-Von Hippel Lindau Syndrome
-Tuberous sclerosis
-ADPKD
Renal Cell Carcinoma (Hypernephroma):
•Most RCC are isoechoic but may also present as hyperechoic
•Color Doppler is used to detect the vascularity of tumor.
•The most common vascular patterns include a “basket sign” and/or “vessel within the tumor”
Sonographic Characteristics of a Malignant Renal:
• Renal cell carcinomas (RCCs) less than 2–3 cm in diameter are always hyperechoic.
• The bigger the tumor, the more heterogeneous is its echotexture.
• Hypoechoic rim represents a vascular pseudo capsule.
•In Cases with Cystic Appearance with Malignant Renal:
– Thick wall >1 mm
– Irregularity at the base of the cyst
– Septations
– Calcifications
– Presence of vascularity in the septa and/or cystic wall
Transitional Cell Carcinoma:
•This tumor involve the renal pelvis, ureter and bladder.
•They are low grade malignancies and tend to have benign course.
•The typical appearance is that of a hypoechoic mass within the collecting system, with low vascularity on color Doppler and, extremely rarely, calcifications.
•TCC may invade adjacent renal parenchyma and form an infiltrating mass, which usually preserves the renal contour.
Renal Metastasis
•Renal metastases occur late in course disease.
•Most commonly from contralateral kidney, lung, colon, melanoma, breast.
•Malignant cells from leukemia and lymphoma can metastasize to the kidney.
Wilm’s Tumor
(Nephroblastoma)
•Most common tumor in children 1-8 yrs.
•Unilateral
•Homogeneous and echogenic
•May extend into the perirenal area, renal vein and IVC.
•Metastasis can be seen to the lungs, liver, bone, lymph nodes, and retroperitoneum.
•Wilm’s tumor destroy the renal contour.
Sonographic Findings for Wilm’s Tumor (Nephroblastoma)
•The mass varies from hypoechoic to moderately echogenic.
•Patients with Wilms tumor have renal vein thrombosis and/or vena cava or atrial thrombus by the time of diagnosis.
•Venous obstruction may result, with findings of leg edema, Varicocele, or Budd-Chiari syndrome.
Acute Glomerulonephritis:
•In acute glomerulonephritis, necrosis or proliferation of cellular elements (or both)
•the end result is enlarged, poorly functioning kidneys.
•Acute glomerulonephritis is an inflammatory response resulting in glomerular damage caused by an autoimmune reaction, infection or exposure to toxins.
Presenting symptoms for Acute Glomerulonephritis include:
–Sudden onset of hematuria
–Proteinuria
–Azotemia red blood cell casts in urine.
Sonographic findings for Acute Glomerulonephritis:
•Increased cortical echoes probably result from changes within the glomerular, interstitial, tubular, and vascular structures.
Acute Interstitial Nephritis
•May be a manifestation of an allergic reaction to certain drugs.
•Patient present with uremia, proteinuria, hematuria, rash, fever, and eosinophilia.
Sonographic Findings for Acute Interstitial Nephritis:
•the kidneys are enlarged and mottled
•Renal cortical echogenicity is increased.
Causes of Renal Failure: •Prerenal
–Hypoperfusion
–Hypotension
–Congestive heart failure
Causes of Renal Failure: •Renal
–Infection
–Nephrotoxicity
–Renal artery occlusion
–Renal mass or cyst
Causes of Renal Failure: •Postrenal
–Lower urinary tract obstruction (ureter, bladder)
–Retroperitoneal fibrosis
Acute Renal Failure
(ARF)
•A sudden decrease in renal filtration marked by an increase in serum creatinine or blood urea nitrogen (azotemia).
•Immediately after kidney injury the only sign of ARF may be a decrease in urine production.
•Prompt intervention prevents losses of renal parenchyma.
Sonographic Findings for Acute Renal Failure:
•The kidneys may appear normal in size or enlarged and may be hypoechoic with parenchymal disease.
Laboratory studies used to evaluate ARF:
–Urine output
–Urine analysis
–Blood urea nitrogen
–Serum creatinine.
–Changes in serum creatinine reflecting changes in glomerular filtration rate, is the most accurate method of determining ARF.
Acute Tubular Necrosis
•Most common cause of acute renal failure (intra renal failure)
•ATN results from prolonged ischemia or nephrotoxins (drugs and contrast agents) causing damage to the tubular epithelium of the nephron leading to ARF.
•Bilateral enlarged kidneys with hyperechoic renal pyramids
•Seen in renal transplants.
•Most common cause for renal transplant failure. Can be reversible.
Sonographic findings for Acute Tubular Necrosis:
–Bilateral Renal enlargement with hyperechoic pyramids
Chronic Kidney Disease
•It is the loss of renal function as a result of parenchymal disease.
Signs and Symptoms of Chronic Kidney Disease:
–Increase concentration of urea in blood
–High urine protein excretion
–Increase in creatinine
–Presence of granulocytes
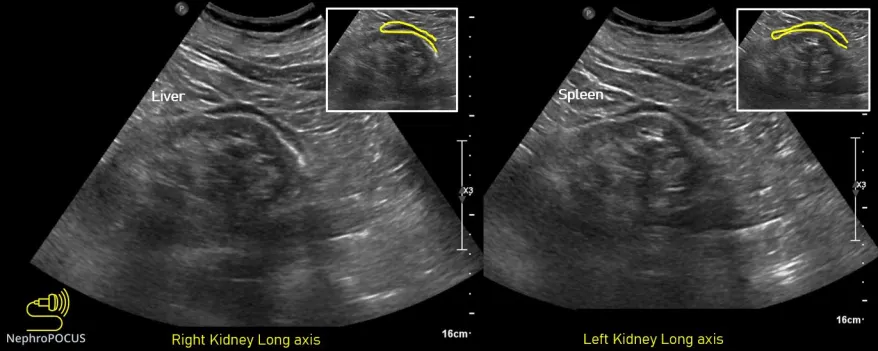
Sonographic Findings of Chronic Kidney Disease:
–CKD is a diffusely echogenic kidney with loss of normal anatomy.
–If chronic renal disease is bilateral, small kidneys are identified. This may result in hypertension, chronic inflammation, or chronic ischemia.
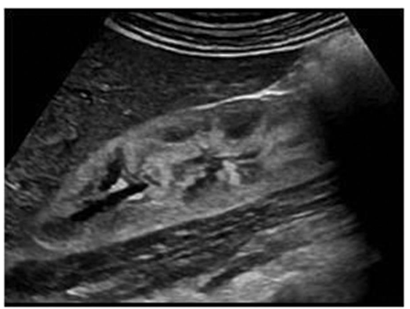
Hydronephrosis

Acquired Causes of Hydronephrosis:
•Bladder tumors
•Carcinoma of the cervix
•Calculi
•Neurogenic bladder
•Normal pregnancy
•Pelvic mass
•Prostatic enlargement
•Retroperitoneal fibrosis
Intrinsic Causes of Hydronephrosis:
•Calculus
•Stricture
•Inflammation
•Pyelonephritis
•Congenital
•Bladder neck obstruction
•Posterior urethral valves
•Ureterocele
•Ureteropelvic junction (UPJ) obstruction
Sonographic Findings of Hydronephrosis:
•At the level of obstruction sweep the transducer back and forth in two planes to see if mass or stone can be distinguished.
•In evaluating the patient for hydronephrosis, look for a dilated ureter, an enlarged prostate, or an enlarged bladder.
•Bladder carcinoma may obstruct the pathway of the urethra.
•A ureterocele may also blocks urine output. The ureter turn inside out and obstruct the orifice.
Renal infection - Pyonephrosis
•occurs when pus is found within the collecting system
•It requires urgent intravenous antibiotic therapy and/or percutaneous drainage.
Sonographic Findings of Pyonephrosis:
•presence of low-level echoes with fluid–debris level
Renal Infection- Emphysematous Pyelonephritis
•occurs when air is present in the parenchyma.
•Caused by E coli
•Generally found unilaterally and may cause for an emergency nephrectomy.
Urinary Tract Calcifications- Renal Calcifications:
• may be seen as localized parenchymal calcifications, resulting from scar tissue caused by bacterial infection, renal abscess, infected hematoma, urinoma, lymphocele, tuberculosis, or infarction, or post-percutaneous renal procedures.
Urinary Tract Calcifications - Medullary Sponge Kidney:
•or intralobular renal calcification, is a developmental anomaly that occurs in the medullary pyramids and consists of cystic or fusiform dilation of the distal collecting ducts. It may be unilateral or segmental. The cause is unknown.
•Many patients remain asymptomatic, but patients with hematuria, infection, and renal stones should be evaluated for MSK.
Sonographic findings for Medullary Sponge Kidney:
• appears as hyperechoic calyces, with or without stones
Nephrocalcinosis:
•Parenchymal calcification occurs.
•Affects both kidneys.
Kidney Stone
•A stone located in the urinary system is called urolithiasis.
•Kidney stones are one of the most common kidney problems that can occur; they may cause obstruction, and this obstruction can be extremely painful.
•Majority of stones formed in the kidney and course down the urinary tract
•Made up of a combination of chemicals that precipitate out of urine
•Most are small and can travel through the urinary system with increased hydration and without treatment.
•Large stones that fill the renal collecting system, called staghorn calculi
•Some kidney stones may obstruct the ureter in the constricted areas.
•Treatment for stones that cause obstruction varies depending on the size and location of the stone.
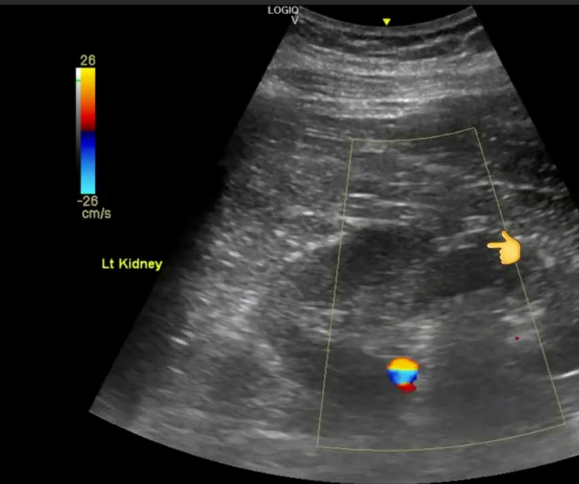
Sonographic Findings for Kidney Stones:
•Very echogenic foci with posterior acoustic shadowing
•Color and power Doppler have increased the sensitivity of confirming the presence of stones. Color and power Doppler cause a twinkling artifact posterior to the stone. This artifact is referred to as the twinkling sign and is imaged as a rapidly changing mixture of red and blue colors posterior to the stone.
Bladder Diverticulum
•Herniation of the bladder wall occurs.
•Outpouchings may be singular or multiple and are thinner than the normal bladder wall.
•The diverticulum lacks a muscular layer and has a neck.
•The diverticulum may still be filled with fluid after the patient empties the bladder
•Urine stasis leads to recurrent infection and stone formation.
Bladder inflammation
•AKA Cystitis
•Inflammation of the bladder has several infectious and non-infectious causes.
•Cystitis is usually secondary to the causes that cause stasis of urine in the bladder
Bladder Tumors
•Majority (95%) of bladder tumors in adults are TCCs.
•Usually not detected until they have become advanced
•Patients typically have gross hematuria, dysuria, urinary frequency, or urinary urgency.
•A cystoscopy or biopsy may allow to differentiate between a benign and a malignant neoplasm.
The bladder may be a secondary site of malignancy. The most common site is prostate.
Sonographic findings of Bladder Tumors:
•Appearance of bladder masses vary
•Benign tumors are typically hypoechoic compared with malignant bladder tumors

Dromedary Hump
•Found in the mid-kidney portion.
•prominent focal bulges on the lateral border of the left kidney
•They are normal variants of the renal contour, caused by the splenic impression onto the superolateral left kidney.
•Dromedary humps are important because they may mimic a renal mass, and as such are considered a renal pseudotumor.

Parapelvic cyst
•are fluid-filled sacs that develop near the renal sinus, the cavity that contains blood vessels and urine-collecting tubes in the kidney.
•These are simple renal cysts that plunge into the renal sinus from the adjacent renal parenchyma
Junctional parenchymal defect:
•are a normal variant that results from the incomplete embryonic fusion of renunculi.
•These defects appear as triangular echogenic cortical defects, often observed in the upper lobe parenchyma of the kidney.
•Specifically, they extend from the sinus fat into the cortex, typically near the border of the upper pole and interpolar region of the kidney.
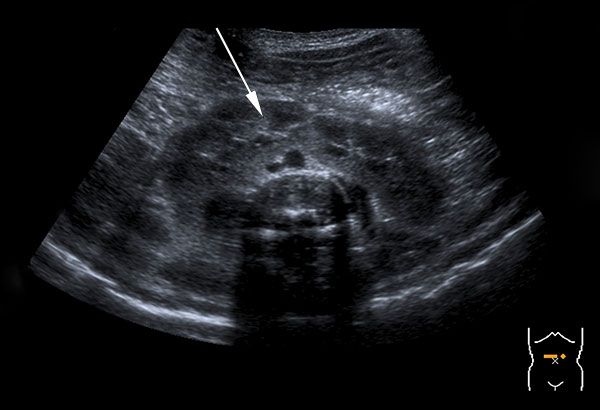
Horseshoe Kidney:
•also known as renal fusion, is a congenital urological anomaly where the two kidneys join together during fetal development, forming a shape resembling a horseshoe or the letter U.
•Instead of moving into their typical position around the spine, the kidneys attach at their lower end and sit lower in the pelvis, closer to the front of the body.
Perinephric fat
•Located outside of the renal capsule.
•The perirenal fat body (a.k.a. perinephric fat) The renal fascia which besides the kidneys also encloses the suprarenal gland and its surrounding fat.
•Outside the fascia is the most superficial layer – a layer of fat tissue called the pararenal (/paranephric) fat body.

Oncocytoma
•is a benign (noncancerous) growth that occurs in one or both of the kidneys.
• “Oncocytoma” refers to a tumor composed of oncocytes, which are cells characterized by an abnormally large number of mitochondria—the energy-producing organelles within the cell.
•They can mimic those of renal cell carcinoma, a type of kidney cancer.