PT-622 Cardio-Pulm Final
1/799
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
800 Terms
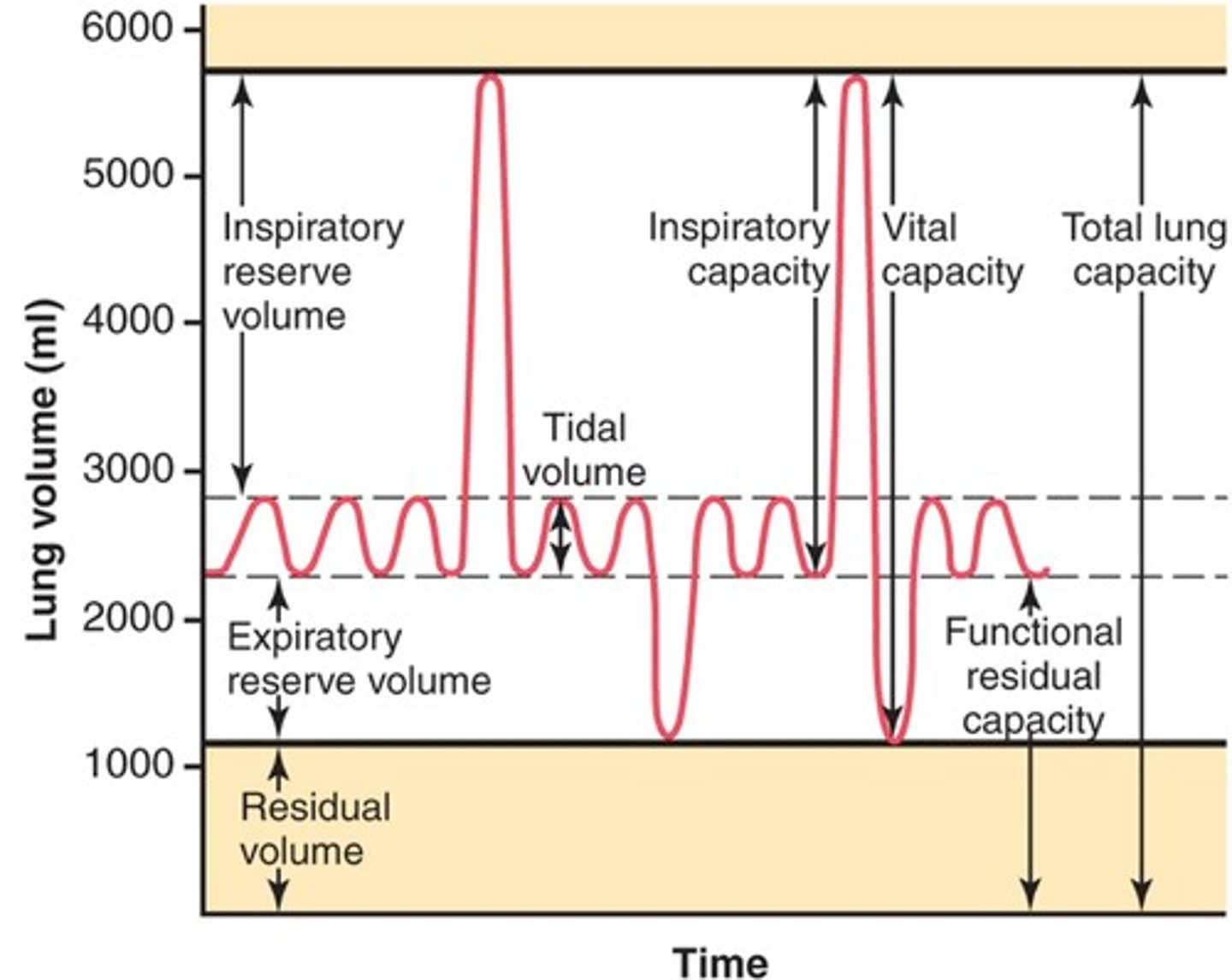
Tidal Volume (TV)
Air inhaled/exhaled at rest w/ each breath
Normal: approx. 350-500 mL
Defibrillator
VT w/ a pulse
V-Fib
SVT = Urgent
VT = Emergency
V-Fib
Code Blue
Lingula location
Between 4th and 6th IC space
Arterial Doppler =
Ankle-Brachial Index (PAD)
4 factors of BNP
-LV Systolic dysfunction
-LV Diastolic dysfunction
-RV dysfunction
-Valvular dysfunction
S2 = Atria >>> Ventricle (SL valves closing)
S1 = Ventricle >>> Out (AV valves closing)
S2 = Ventricular filling
Longer than S1
Ventilatory rate / Respiratory rate
Breathes per minute at rest
Normal: 10-15 breaths
Expiratory reserve volume (ERV)
Additional volume of air that can be let out beyond the normal tidal exhalation
Inspiratory reserve volume (IRV)
Additional volume of air that can be taken into the lungs beyond normal tidal inhalation
Total lung capacity (TLC)
Maximum volume to which the lungs can be expanded
sum of all pulmonary volumes
Residual volume (RV)
Volume of air that remains in the lungs after forceful expiration
Inspiratory capacity (IC)
Maximum amount of air that can be inhaled after a normal tidal expiration
Sum of the TV + IRV
Functional residual capacity (FRC)
The amount of air remaining in the lungs at the end of a normal tidal exhalation
Sum of ERV + RV
Vital capacity (VC)
Maximum amount of air that can be exhaled following a maximum inhalation
Sum of IRV + TV + ERV
What effects ventilation and perfusion matching?
-
Lung capacities diagram
Pulmonary ventilation
movement of air into and out of the lungs
Pulmonary respiration
the exchange of oxygen and carbon dioxide between the alveoli and circulating blood in the pulmonary capillaries
Majority of oxygen is transported to peripheral tissue bound to hemoglobin within RBC's
Very small portion (2%) is dissolved in plasma within blood
Oxygen-carrying capacity
Concentration of hemoglobin
Normal:
12-16 (women)
13-18 (men)
What causes acidemia (pH < 7.4)
1) Low HCO3 produces metabolic acidosis
2) High CO2 produces respiratory acidosis
What causes alkalemia (pH > 7.4)
1) High HCO3 causes metabolic alkalosis
2) Low CO2 causes respiratory alkalosis
If a disease causes decreased HCO3 (metabolic) the body would respond by...
Decreasing the CO2 (respiratory) to return pH to normal
Preload
Volume of blood returning to the heart
or
Amount of stretch on the myocardial wall before contraction
Correlated w/ End-Diastolic Volume (EDV)
Directly proportional to Stroke Volume (SV)
End Diastolic Volume (EDV)
Maximum amount of blood that can be in the ventricles immediately before contraction
Contractility
Myocardial contractility is influenced by intrinsic and extrinsic factors
Intrinsic control of contraction strength is a result of the degree of myocardial stretch caused by changes in the EDV
The extrinsic control of contractility depends on the activity of the sympathoadrenal system
Epinephrine from the adrenal medulla and norepinephrine from the sympathetic nerve endings produce a positive ionotropic effect, or increase myocardial contractility,
Conversely, a reduction in sympathetic stimulation and reduction in heart rate results in reduced myocardial contractility.
Afterload
Pressure at which the heart has to overcome to pump blood into the aorta
Afterload is inversely proportional to Stroke Volume (SV)
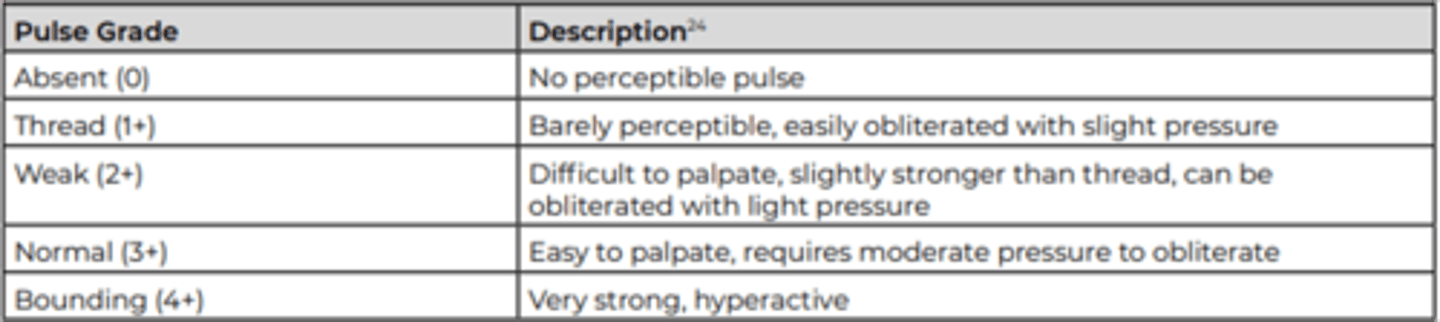
Pulse classification
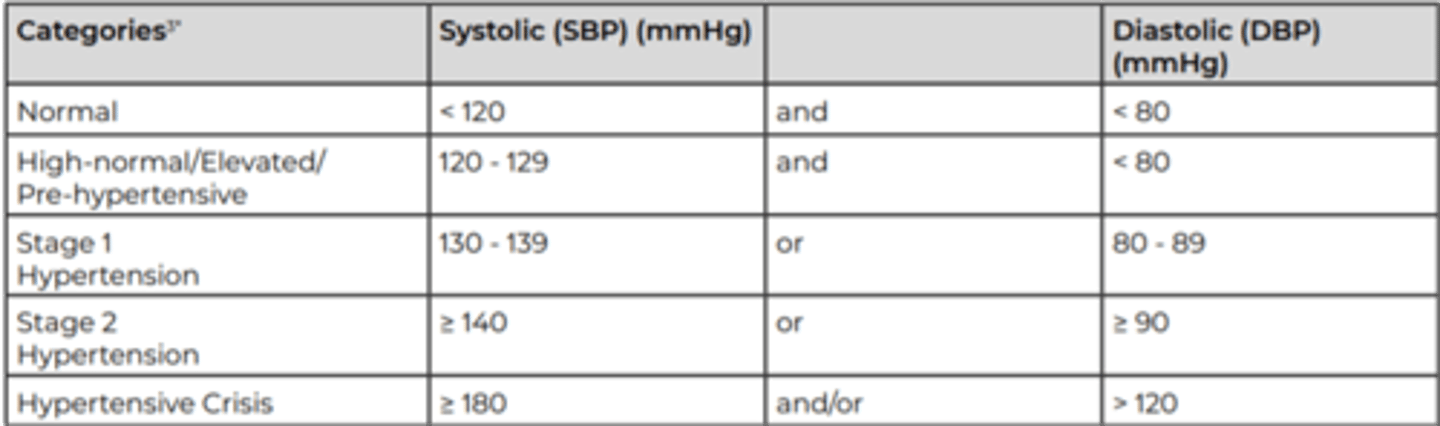
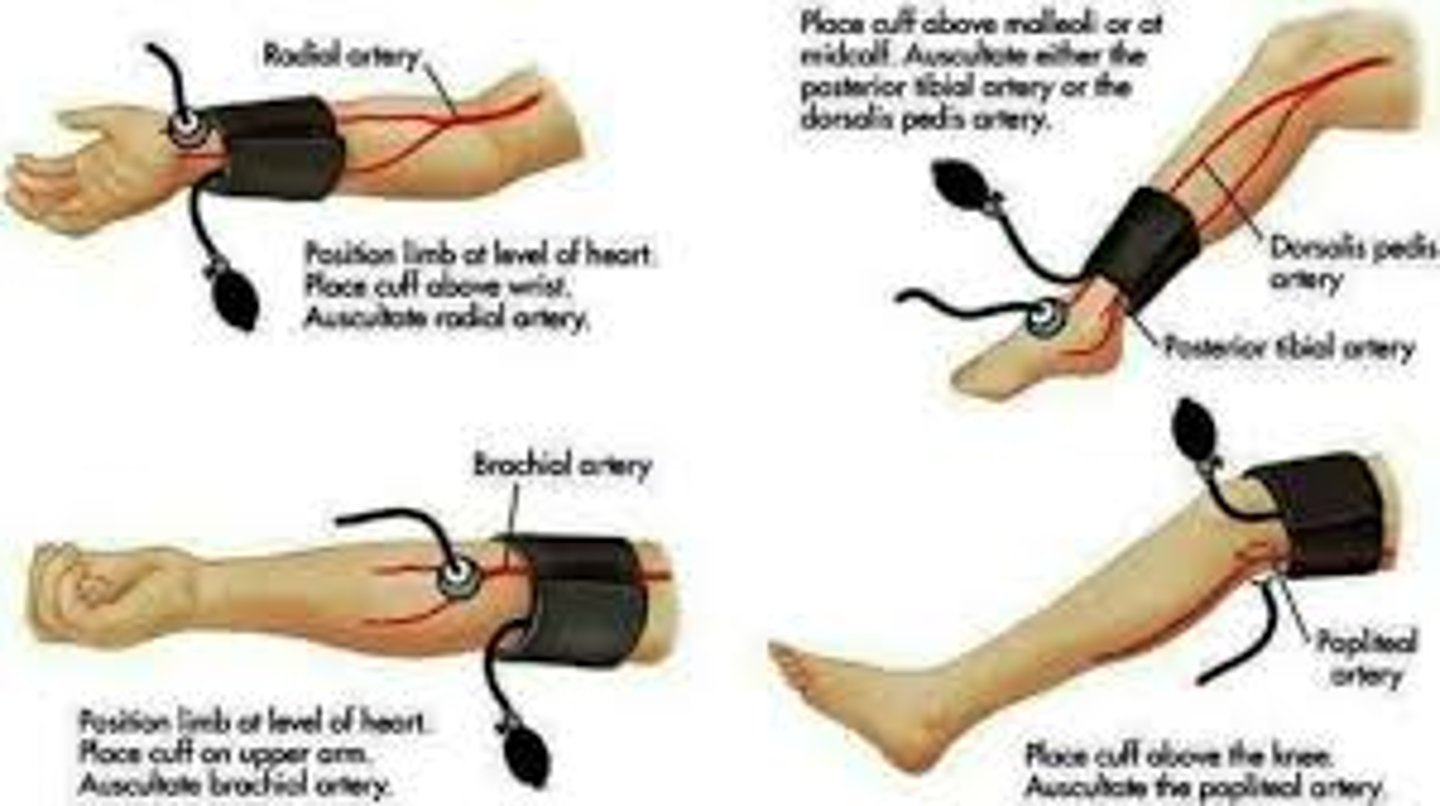
Blood pressure
Measurement of force exerted against the arterial walls during ventricular systole (SBP) and ventricular diastole (DBP)
ALWAYS CHECK FOR POSTED SIGNS FIRST!!
-May be contraindicated to take BP in upper extremity (lymphedema, neglect, dialysis access, PICC line, etc)
Use appropriate fitting cuff
Width=40%
Length=80%
Blood pressure procedure
1) Cuff should be 2.5 cm above antecubital space
2)Rest arm at level of the heart
3) Place bell of stethoscope over brachial artery
4) Inflate to 30-40 mmHg above SBP
5) Slowly deflate (rate of 2-3 mmHg per second)
6) Listen for onset of tapping sounds
-Systolic BP—blood starts to flow through artery
7) Listen of disappearance of tapping
-Diastolic BP—normal blood flow & no compression on artery
BP classification
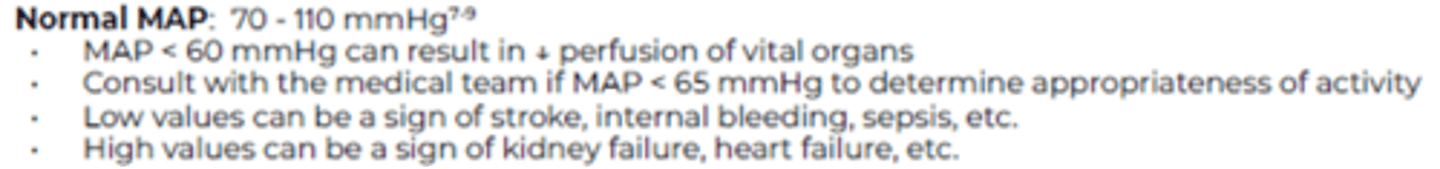
Mean Arterial Pressure (MAP)
SBP + DBP + DBP
3
Average pressure during a single cardiac cycle
Tells us that perfusion is adequate to the end organs
MAP values
Blood oxygen levels Pulse Oximeter
85-90 during exercise = stop

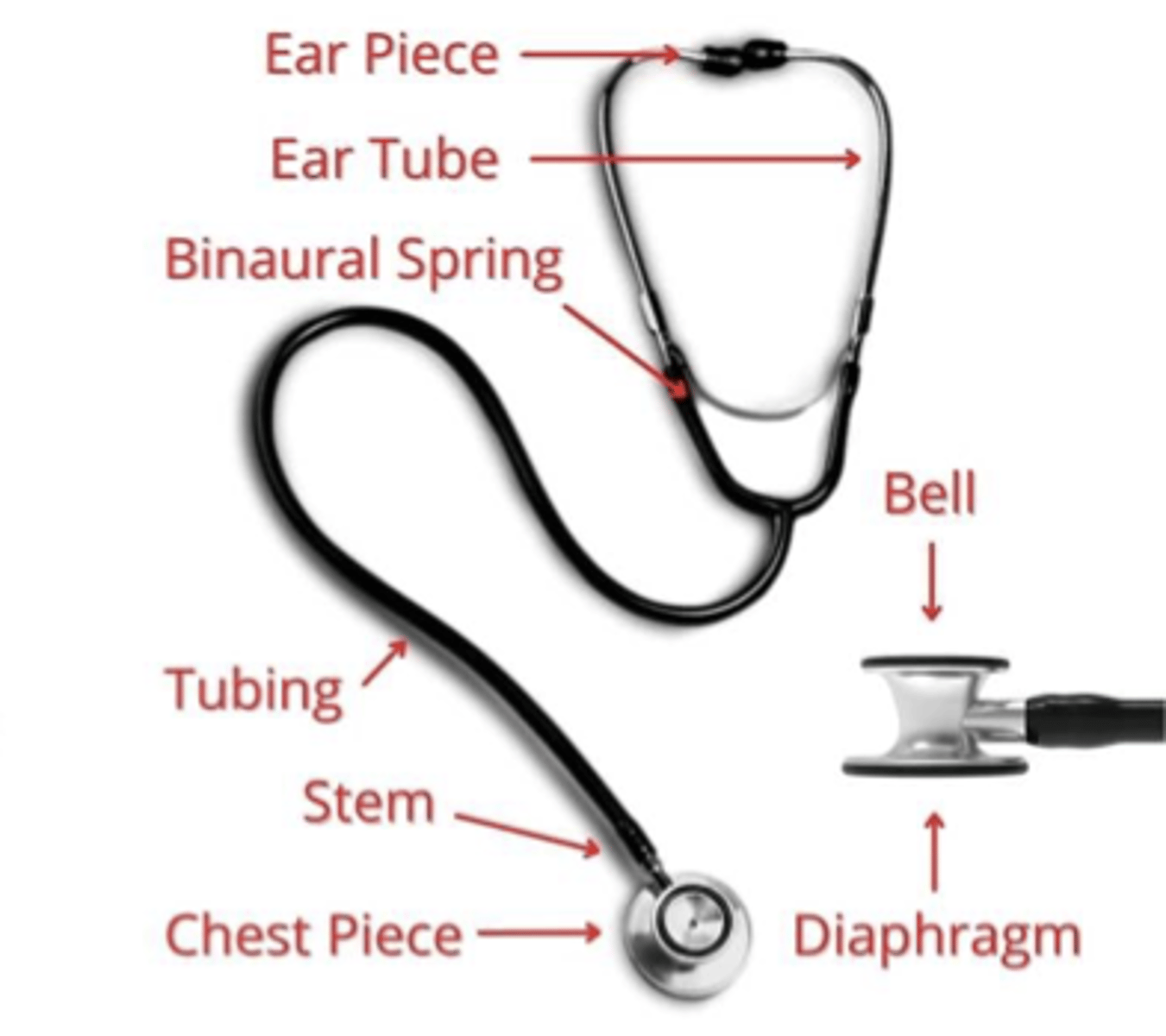
Stethoscope diagram
Bell of stethoscope may be better for low-pitched sound (heart)
Diaphragm may be better for high-pitched sounds (lungs)
Auscultation—Heart
Aortic - Aortic valve heard during S2
Tricuspid - Tricuspid valve is heard during S1
Mitral - Mitral valve is heard during S1
Pulmonary - Pulmonary valve is heard during S2
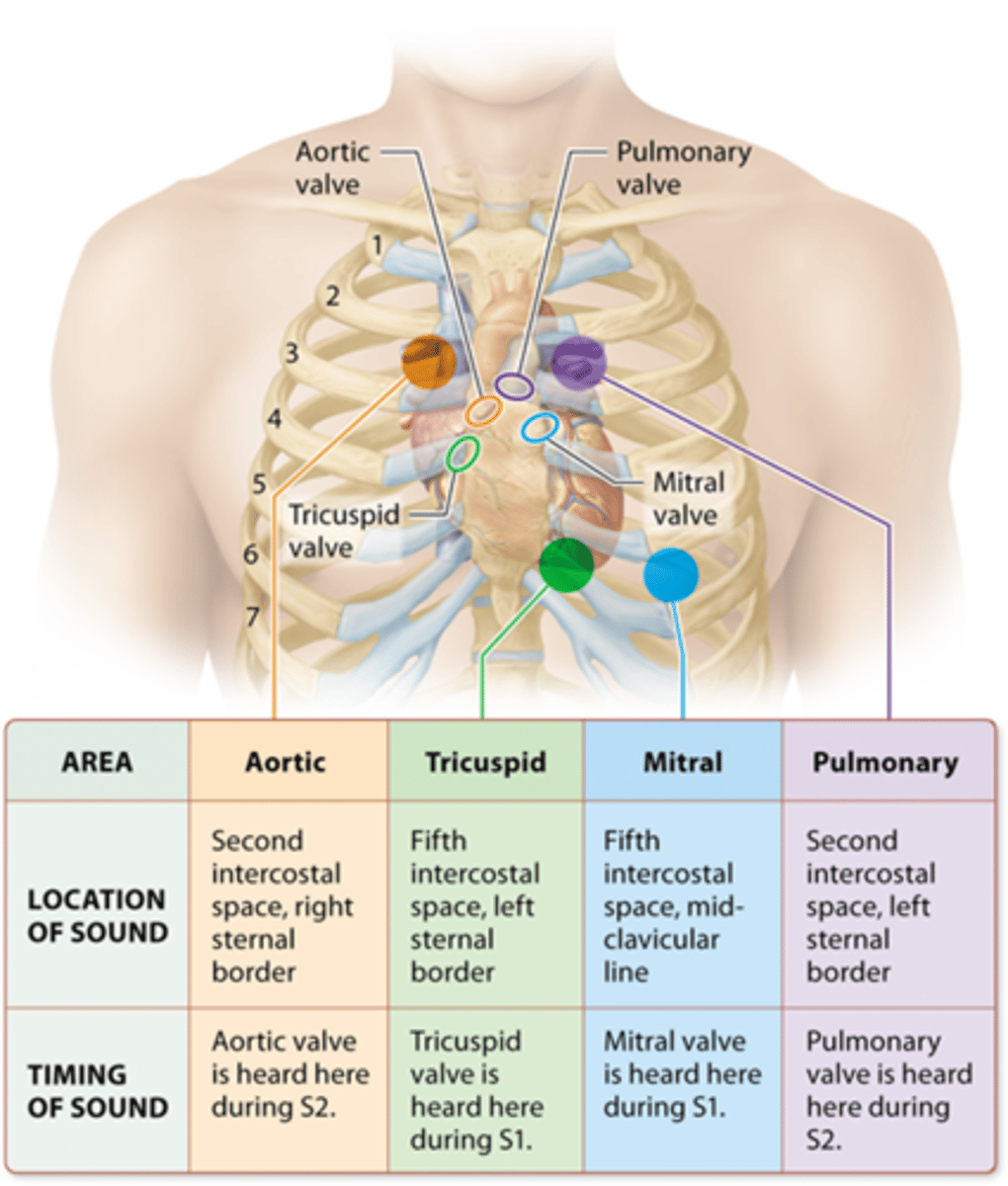
Aortic valve auscultation location
2nd intercostal space
Right sternal border
Pulmonary valve auscultation location
Second intercostal space
Left sternal border
Mitral valve auscultation location
Fifth intercostal space
Mid-clavicular line
Tricuspid valve auscultation location
Fifth intercostal space
Left sternal border
S1 >> S2 = Systole
S2 >> S1 = Diastole
Abnormal heart sounds occur during
Diastole
Just after S2 (S3)
or
Just before S1 (S4)
Mitral valve prolapse sounds
clicking noted in middle of ventricular systole
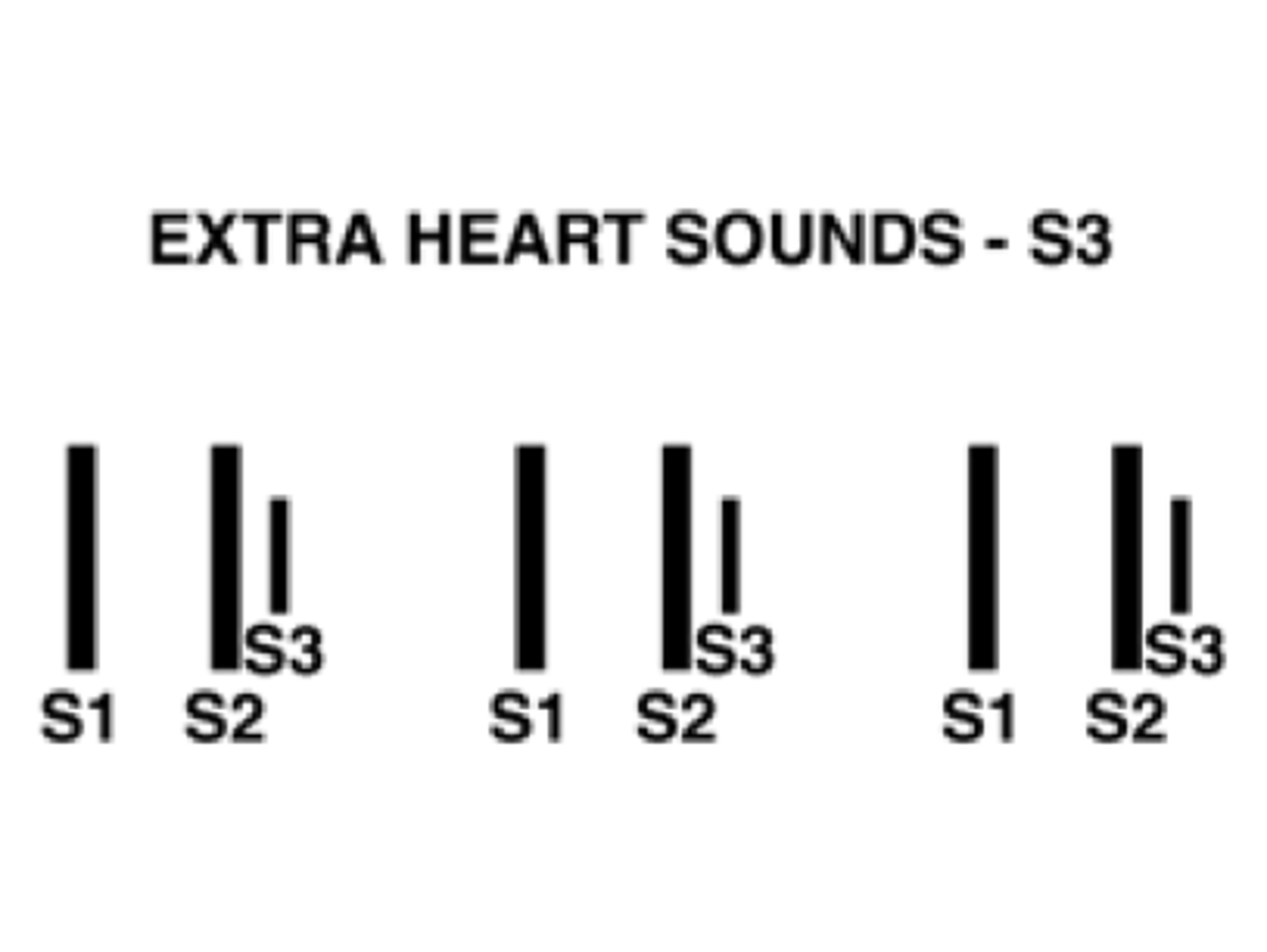
Extra heart sounds - S3
(lub-dub-dub)—ventricular filling; early in diastole
Considered normal in healthy children and young adults*
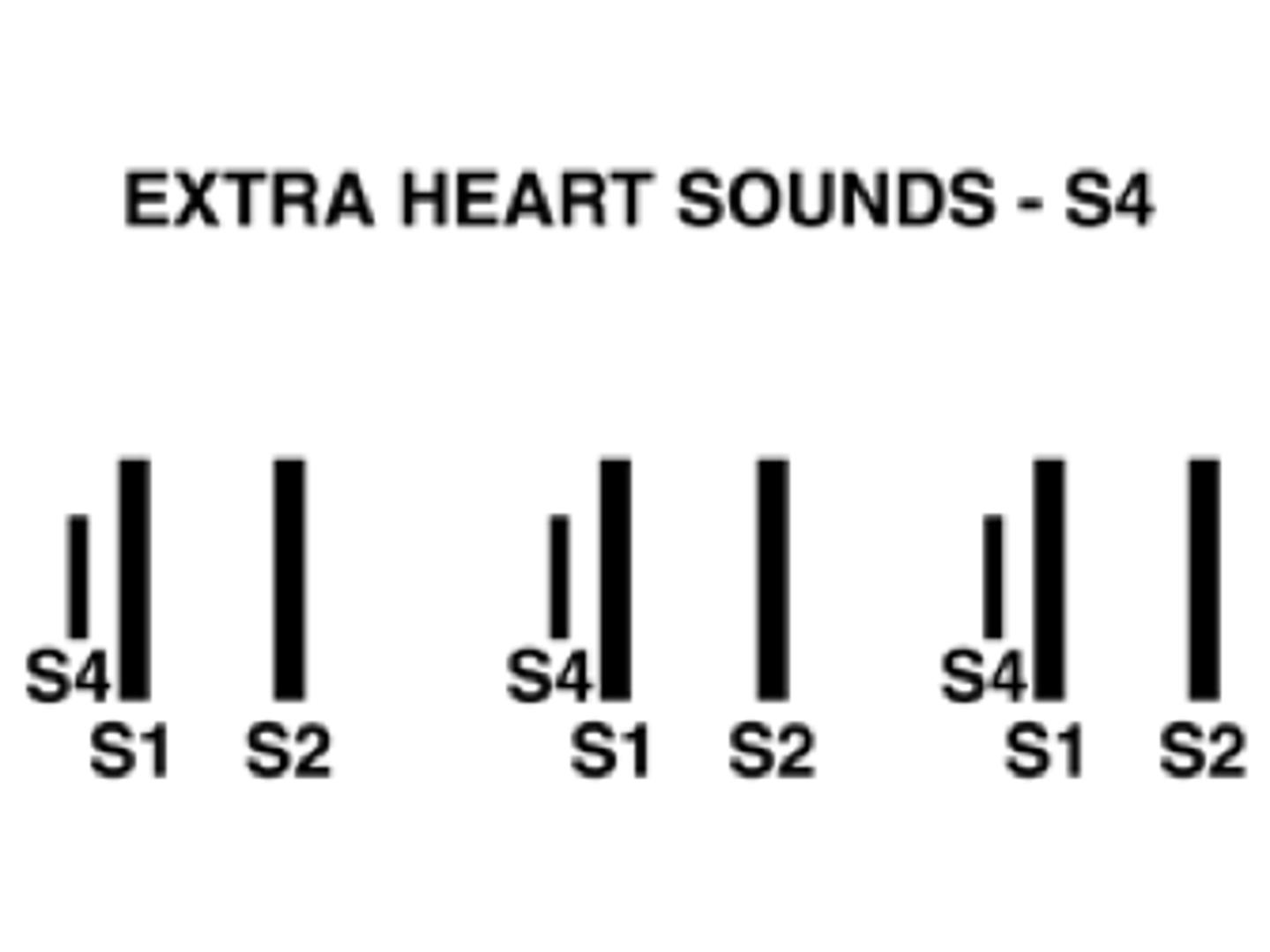
Extra heart sounds - S4
(la-lub-dub)—atrial contraction; late in diastole
“atrial gallop”—not normal; associated with increased resistance to ventricular filing
-Hypertension
-Ventricular hypertrophy
-Stenosis
Distension
Increased RA pressure
Heart murmurs
1) High rates of flow through normal or abnormal valves
2) Forward flow through a constricted (stenotic) or deformed valve; or by flow into a dilated vessel or chamber
3) Backward flow through a valve (regurgitation)
-Systolic most common, usually heard between S1 and S2
-Diastolic are rare and usually heard immediately following S2
-Mitral valve prolapse—clicking sound noted in the middle of ventricular systole
ANTERIOR LUNG LANDMARKS
SUPERIOR LOBE—above first rib/clavicle to rib 4 (right)
-above first rib/clavicle to rib 6 (left side)
MIDDLE LOBE—from base of rib 4 - 6 (right side only)
LOWER LOBE—laterally from rib 6 - 8
POSTERIOR LUNG LANDMARKS
SUPERIOR LOBE—T1-T4 vertebral bodies
MIDDLE LOBE—not present posteriorly
LOWER LOBE—T4-T10 (with inhalation, can extend to T12)
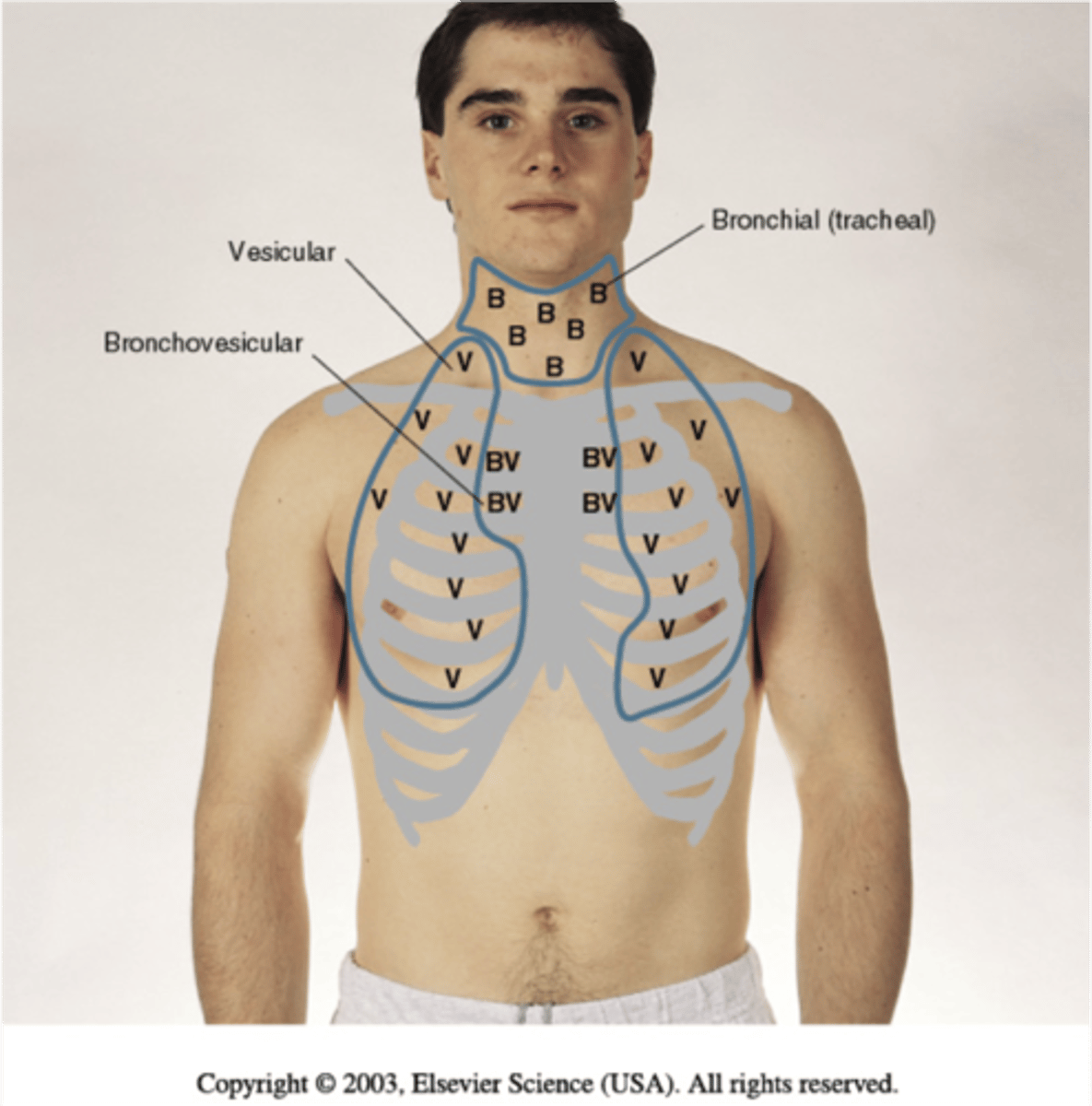
Anterior auscultations
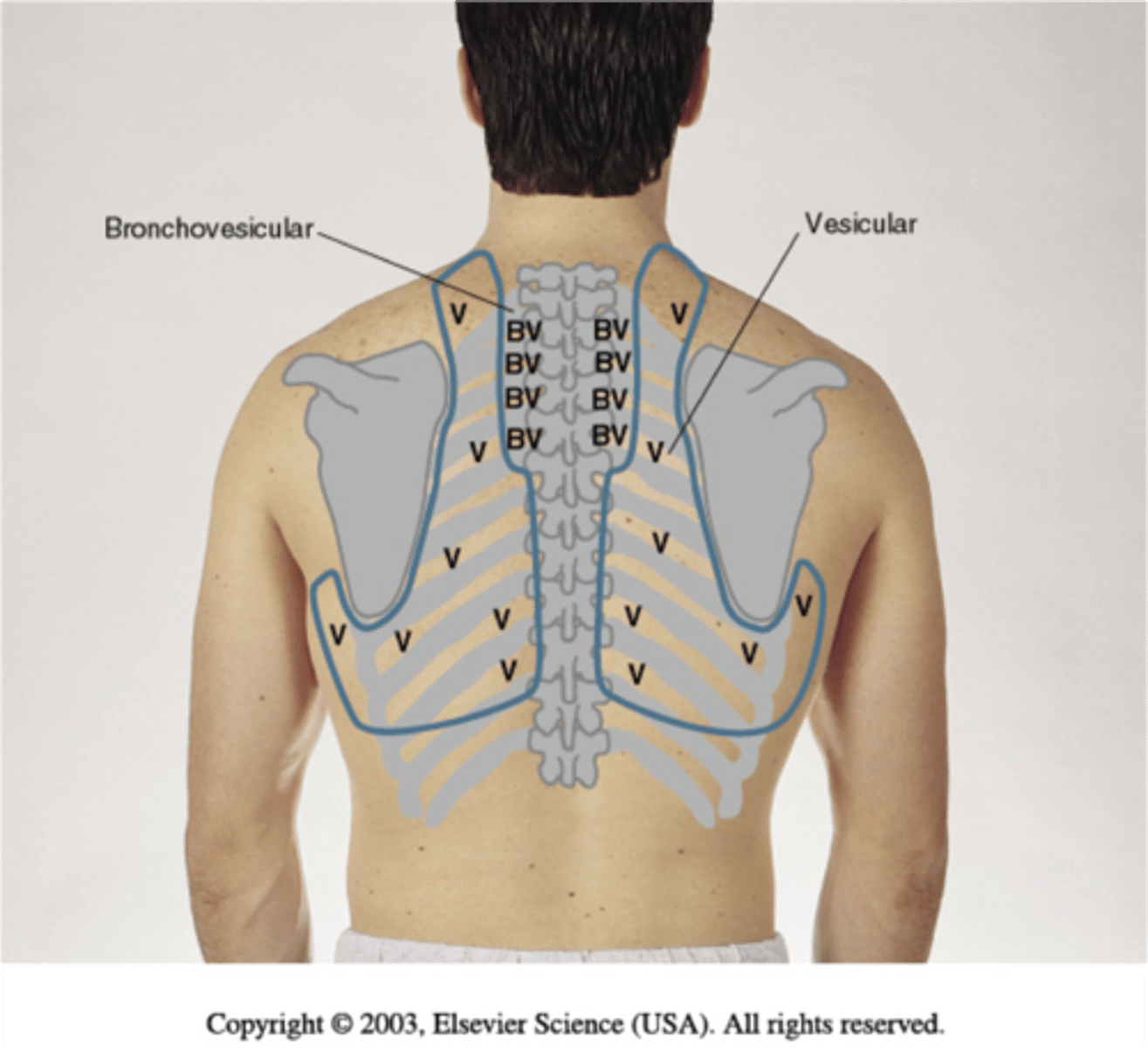
Posterior auscultations
Normal breath sounds - Bronchial
Loud, high pitched
hollow quality
Expiration > Inspiration
distinct pause between in/out
Normal breath sounds - Bronchovesicular
I:E = 1:1
Intercostal space #1 & #2
Normal breath sounds - Vesicular
Soft
low pitched
no pause between in/out
Inspiration > Expiration
Normal breath sounds - Tracheal
Similar to bronchial, but louder
pause between in/out
Crackles
movement of secretions during inspiration (if wet);
sudden closing of airways—atelectasis/fibrosis/pulm edema/pleural effusion (dry)—
usually lung bases.
I > E
Restrictive & Obstructive
"pop"
Pulmonary friction rub
inflamed visceral and parietal pleurae rub together—usually over site of pain
Both I & E
"crackling"
Rhonchi
air passing through an obstructed airway
Both I & E
Obstructive
Bronchi/Bronchioles
"Gurgling"
Stridor
Upper airway obstruction
Both I & E
Obstructive
Severe asthma attack
"wheeze"
Wheeze
Variable may be heard one breath and not another,
vibrations of the walls of small airways d/t bronchospasm,
airway collapse of foreign object
Obstructive
typical asthma attack
"whistle"
Bronchophony
Pt says "99"
If you hear muffled noises = normal
If you hear "99" = abnormal
Egophony
Have pt say "E"
If you hear "A" sound = abnormal
Whispered pectoriloquy
Have pt whisper "1, 2, 3"
If you can hear "1, 2, 3" = abnormal
Percussion - Resonant
normal air-filled lung
Percussion - Hyper-resonant
overinflated but not hollow
Percussion - Tympanic
loud, long and hollow
Percussion - Dull or flat
increased density (“thud”)
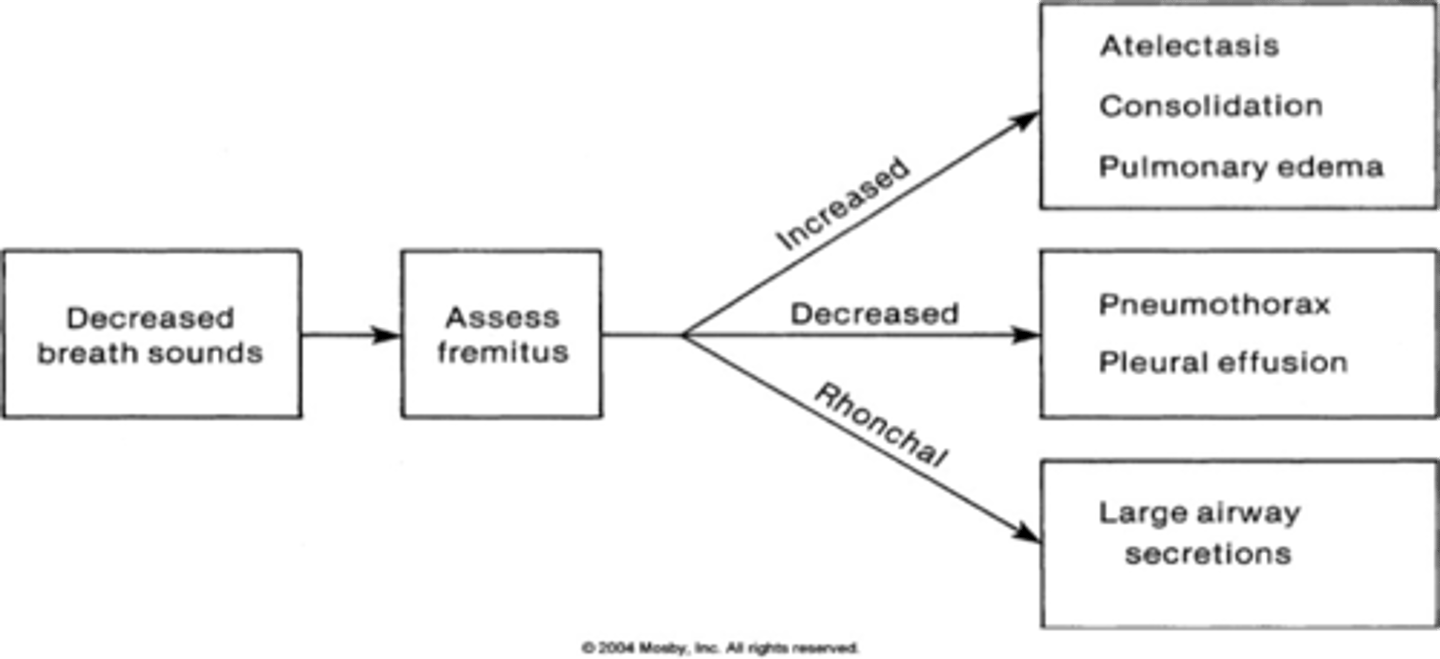
Palpation—Tactile fremitus
Hands flat on thorax, or ulnar border of hands on thorax
Patient speaks quietly, 1-2-3, 99, etc.
Feel vibration of chest
Increased with consolidation, decreased with more air
CI's for taking BP on UE
Dialysis access
Lymphedema
Central lines
Neglect
-No sensation to sense pressure
Alternate BP locations
Must hear pulse before inflating cuff in foot
Decreased breathing sounds >>> Assess fremitus
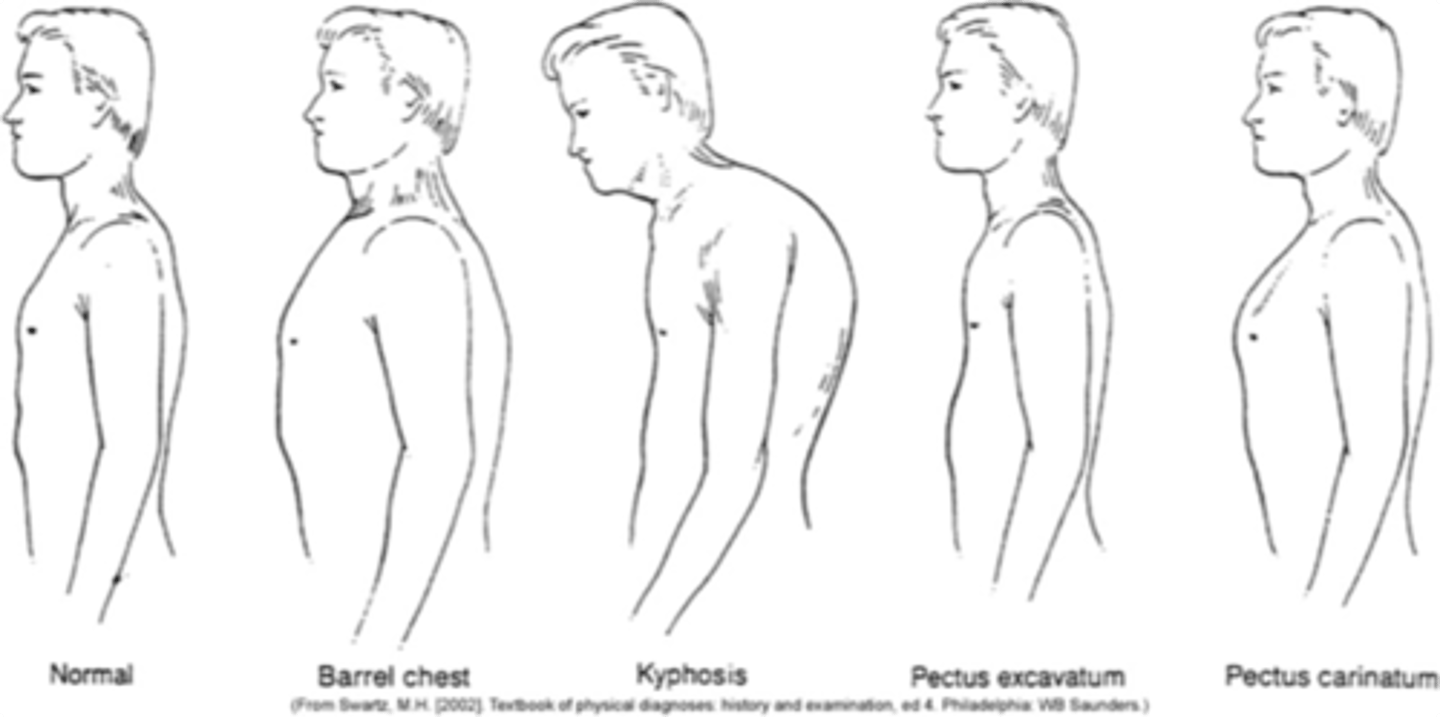
Posture
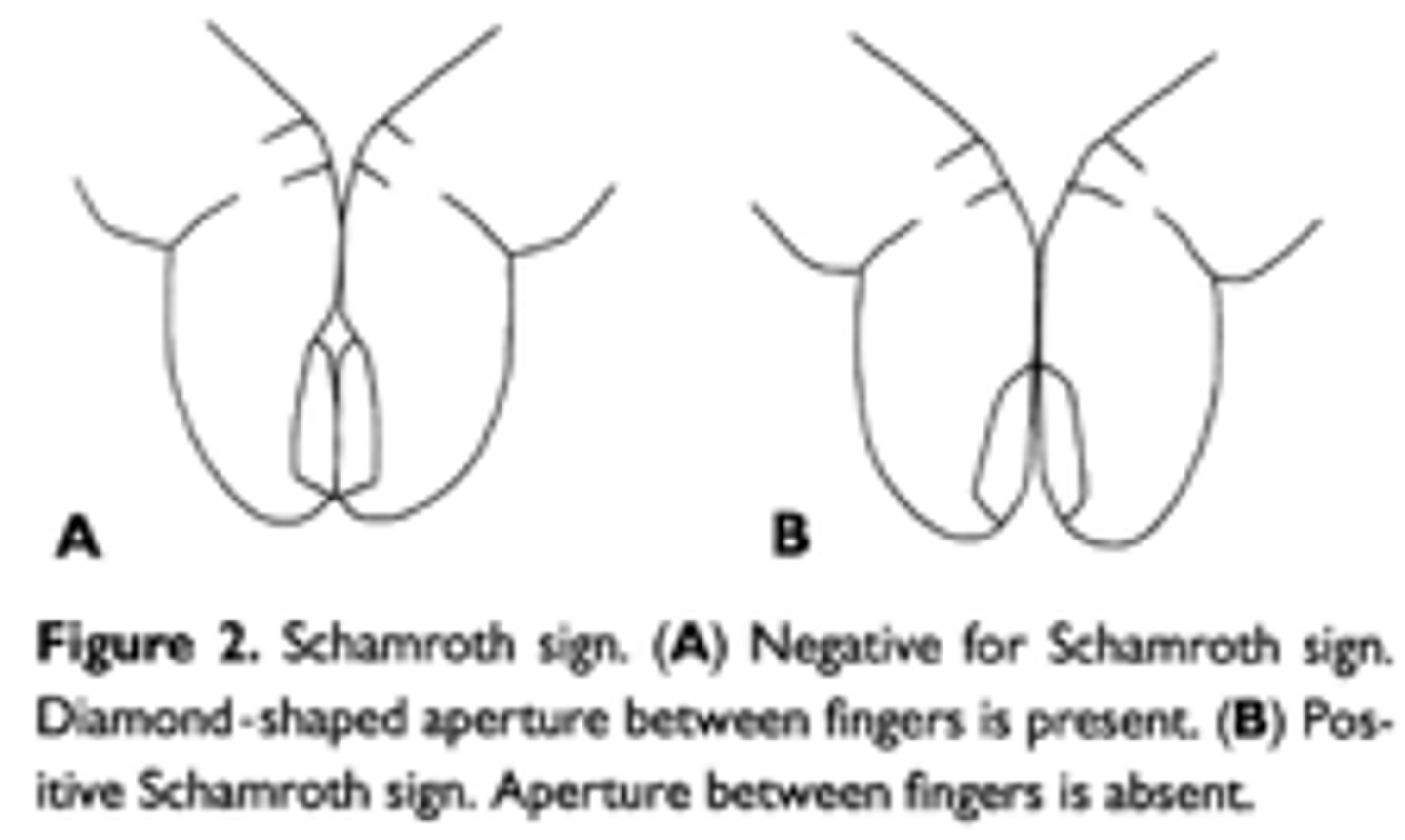
Schamroth's sign
Inspiration:Expiration is 1:2
Respiratory Rate Norms: Newborns
33-45
Respiratory Rate Norms: 1 year
25-35
Respiratory Rate Norms: 10 years
15-20
Respiratory Rate Norms: Adult
12 -20
Hemoglobin molecule consists of 4 iron-containing hemes.
This allows hemoglobin to carry 4 O2 molecules to peripheral tissue
Deoxyhemoglobin = Released its O2
Oxyhemoglobin = Contains O2
Carboxyhemoglobin = Carbon monoxide instead of O2
Percent hemoglobin in systemic arteries = 97%
Gold standard to measure = analysis of arterial blood gases
Can also use pulse oximeter
Meaning that 97% of hemoglobin molecules in blood are bound to O2
Remaining 3% reflects deoxyhemoglobin, methemoglobin, carboxyhemoglobin
Secondary polycythemia
Increase in RBC's
Where can you auscultate heart murmurs?
3rd left IC space
Troponin
Leakage of the protein into the blood indicates damage to the heart muscle
Normal Troponin levels
Cardiac Troponin I (cTnI)— < 0.03 ng/mL
Cardiac Troponin T (cTnT)— < 0.1 ng/mL
high sensitivity Troponin T (hsTnT)—: women < 14 ng/L, men < 22 ng/L
Creatinine Kinase-MB
Commonly elevated in myocardial infarction within 3-6 hours of cardiac injury and then returns to normal within 2-3 days
(peaks 18-24 hours).
Useful for diagnosing re-infarction.
Might be elevated in cases of carbon monoxide poisoning, pulmonary embolism, hypothyroidism, crush injuries, and muscular dystrophy.
Brain Natriuretic Peptide (BNP)
Released in association with a stretch on the ventricular wall
>400 pg/mL is consistent with Heart Failure diagnosis
Helps determine severity of treatment and effectiveness of treatment
Has a precursor called NT-pro-BNP measured at some facilities
< 300 pg/mL is normal
Normal values for Brain Natriuretic Peptide (BNP)
Normal: < 300 pg/mL
Heart failure: > 400 pg/mL
BNP < 100 pg/mL
Indicates no heart failure.
100–300 pg/mL Class I
Cardiac disease, but no symptoms and no limitation in ordinary physical activity, e.g. no shortness of breath when walking, climbing stairs etc.
Symptoms-based approach when determining appropriateness for activity.
> 300 pg/mL Class II
Mild symptoms
slight limitation during ordinary activity.
> 600 pg/mL Class III
Marked limitation in activity due to symptoms, even during less-than-ordinary activity, e.g. walking short distances (20–100 m).
Comfortable only at rest.
> 900 pg/mL Class IV
Severe limitations.
Experiences symptoms even while at rest.
Cholesterol
main lipid associated with cardiovascular disease.
Desirable: 140-199
Borderline high: 240-239
High: >240
Triglycerides
Assesses the body’s ability to metabolize fat and cardiovascular disease risk
Desirable: < 150
Borderline high: 150-199
High: 200-499
Very high: > 500
Lipoproteins HDL
remove excess cholesterol deposits from the arterial lining.
Higher levels can reduce the incidence of cardiovascular disease