Examination and Evaluation of the Airway
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
Why examine and evaluate a patient's airway preoperatively?
1. Determine ease or difficulty of airway manipulation (intubation, mask ventilation)
2. To prepare the anesthetist
→ Selection of airway devices, techniques, and procedures
3. Minimize harm during subsequent airway management
4. Determine airway-related risks in order to
→ Discuss them with patients
→ Avoid risk-related problems
What are the three main mechanisms of injury that account for most serious airway complications?
1. Esophageal intubation
2. Failure to ventilate
3. Difficult intubation
Which airway issue can contribute to esophageal intubation, failure to ventilate, and other complications?
Difficult intubation
What is the key to anticipating difficult intubation in most cases?
Performing a thorough airway evaluation in advance
True or False: Most difficult intubations occur without warning and cannot be predicted
False
→ 98% or more can be anticipated with proper airway evaluation
Why is airway evaluation important for anesthetists?
It helps determine the anticipated ease or difficulty of airway management techniques
Types of airway management techniques
1. Bag-mask ventilation
2. Direct laryngoscopy (for tracheal intubation)
3. Blind airway techniques
4. Fiberoptic bronchoscopy
5. Cricothyrotomy/cricothyroidotomy
6. Tracheostomy
What are examples of blind airway techniques?
LMA and Combitube
What key questions should you ask a patient during airway evaluation?
History
→ Any problems with intubation before?
→ Have you been told you have a difficult airway?
Mouth
→ Any crowns, loose, chipped, or removable teeth
→ OSA, snore, or smoke
→ Anything removable in the mouth?
Conditions
→ Acid reflux or GERD
→ Diabetes
→ Clotting abnormalities
→ Congenital syndromes and abnormalities
Neck
→ Neck radiation
→ Arthritis
→ Circumference
Which types of joint issues can affect airway management?
1. TMJ disease → Limits mouth opening
2. Ankylosing spondylitis → Restricts neck and spine movement
3. Rheumatoid arthritis (RA)
4. Osteoarthritis (OA)
Clotting abnormalities should be asked about prior to what airway intervention?
Nasal airway
What two things should be evaluated separately based on history, examination, and diagnostic tests?
1. Ability to ventilate
2. Ability to intubate
What should you confirm before giving muscle relaxants during airway management?
Make sure you can intubate
What body position should the patient tolerate for a normal airway?
Ability to lie supine
What part of a patient's history is most reassuring for predicting easy intubation?
Past history of easy intubation
What mouth opening measurement suggests a normal airway?
Three finger-breadths
≥ 3-4 cm
What Mallampati class is associated with a normal airway?
Class I or II
What thyromental distance suggests a normal airway?
Three finger-breadths
→ From chin to thyroid notch with neck fully extended
→ Greater than 6 cm
What neck features suggest a normal airway?
→ Full range of motion
→ Slender neck without masses
What is the normal extension angle of the atlanto-occipital joint for airway assessment?
35 degrees
What are the airway assessment risk features for difficult intubation related to:
1. Mouth opening
2. Thyromental distance
3. Mallampati score
4. Neck movement
5. Mandible movement
6. Neck anatomy
7. Past intubation history
BE ABLE TO DISTINGUISH SIGNS OF DIFFICULT MASK VENTILATION FROM SIGNS OF DIFFICULT INTUBATION
1. < 4 cm
2. < 6 cm
3. Class III or IV
4. < 80% range of motion
5. Inability to advance mandible (poor prognathism)
6. Obese or thick neck
7. Positive history of difficult intubation
What percentage of the general adult population has difficult mask ventilation (DMV)?
5%
What are the main goals of face-mask ventilation?
1. Maintain airway patency
2. Oxygenation
How is difficult mask ventilation (DMV) defined?
Inability of an unassisted anesthesiologist to:
1. Keep SpO₂ > 92%
2. Prevent or reverse signs of inadequate ventilation during positive pressure mask ventilation under GA
Predictors of difficult mask/bag mask ventilation
BE ABLE TO DISTINGUISH SIGNS OF DIFFICULT MASK VENTILATION FROM SIGNS OF DIFFICULT INTUBATION
OBESE
1. Obese → BMI > 30
2. Beard
3. Elderly → > 57
4. Snores/OSA
5. Edentulous
In addition:
→ Mallampati class III or IV
→ Severely limited mandibular protrusion
→ Neck radiation
What condition can make mask ventilation severely difficult due to stiff tissues and limited mobility?
Neck radiation
Acronym used for airway evaluation
MOUTHS
M → Mandible: length and ability to sublux
O → Opening: measure mouth opening
U → Uvula: check visibility (Mallampati)
T → Teeth: check for loose, chipped, or cracked teeth
H → Head: assess neck flexion, extension, and rotation
S → Silhouette: look for upper body issues like kyphosis or large breasts
What mandibular issues can make direct laryngoscopy difficult?
1. Temporomandibular diseases like arthritis
2. Mandibular hypoplasia (small chin)
3. Overjet and overbite
4. Maxilla/mandible prognathism
5. Mandible retrognathism
What airway challenges can acromegaly cause?
1. Difficult laryngoscopy (DL)
2. Difficult mask ventilation (DMV)
3. Difficult intubation (DI)
Why is acromegaly associated with difficult DMV, DL, and DI?
1. TMJ arthritis
→ Limited range of motion
2. Small mouth opening
3. Large nose and tongue
4. Thick mandible
5. Overgrowth of soft tissues
→ Pharynx, larynx, and vocal cords
6. Central apnea or OSA
What congenital issues can make direct laryngoscopy difficult?
1. Torus palatinus
2. Cleft palate
3. Cleft lip
4. Micrognathia
What congenital abnormalities are most common in pediatrics?
Cleft palate and cleft lip
What should you check for when inspecting the lips during airway evaluation?
1. Chapped skin
2. Open sores
3. Scars
4. Abrasion
Why is poor dentition a concern during airway management?
Loose or damaged teeth can fall out, get lodged in the airway or bronchial tree, and lead to complications like abscess formation
Upper lip bite test is a modification of
Mandibular protrusion test
What finding on the upper lip bite test predicts a likely adequate laryngoscopic view?
The lower teeth can bite the upper lip at or above the vermilion border
What joint movement does the upper lip bite test help assess?
TMJ glide
What does a mouth opening < 3 cm suggest?
TMJ dysfunction
What does a mouth opening < 2.5 cm indicate?
May preclude normal direct laryngoscopy
What does a mouth opening < 2 cm indicate?
Limits laryngoscopic equipment
When mouth opening is limited, what should you rule out?
Pain vs mechanical cause
What are two main reasons for limited mouth opening at the TMJ?
Pain limitation and mechanical limitation
What should you assess when palpating the TMJ?
1. Movement
2. Pain
3. Crepitus
4. Clicking
What neck range of motion is considered normal for airway assessment?
More than 90° of flexion and extension
What does neck mobility < 80° indicate?
Triples the risk of a poor laryngoscopic view
To obtain a direct line of sight during intubation, the patient is positioned in the __________, which involves flexing the __________ and extending at the __________
1. Sniffing position
2. Lower cervical spine (flexing)
3. Atlanto-occipital joint (extending)
Why can't patients in a cervical collar be placed in the sniffing position?
Because the collar restricts neck flexion and extension
What is used to estimate the atlanto-occipital gap during airway assessment?
Upper-lower dental angle
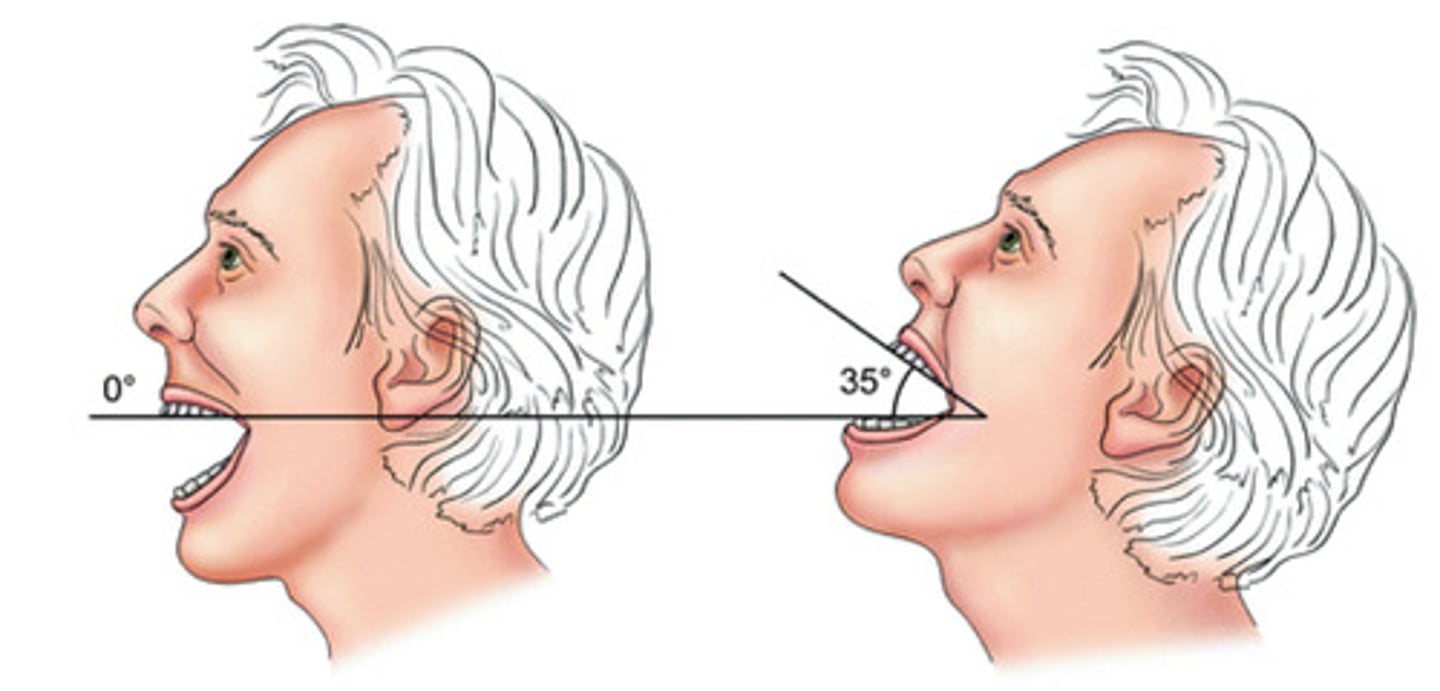
What is the normal angle for the atlanto-occipital gap?
≥ 35°
Why is the atlanto-occipital gap important for direct laryngoscopy?
Reduced angle = Improper axial alignment
→ DL more difficult
What physical sign in diabetics may indicate limited joint mobility?
Prayer sign (interphalangeal joint gap)
What does a positive prayer sign indicate in airway evaluation?
Limited joint mobility
→ Can also affect the cervical spine, TMJ, and larynx
How much more likely are long-term type 1 diabetics to have intubation difficulty?
10 times more likely
What is the gold standard for oropharyngeal examination (OPE)?
Mallampati classification
What is the Mallampati classification based on?
Structures seen with maximal mouth opening and tongue protrusion
→ Without phonation
Mallampati classes
I: Soft palate, fauces, uvula, tonsillar pillars
II: Soft palate, fauces, and uvula
III: Soft palate and base of the uvula
IV: Only the hard palate is visible
What does a false positive mean in Mallampati Class IV?
The airway looks difficult on exam, but intubation ends up being easy
Cormack-Lehane classification
Grade I: Full view of the glottis
Grade II: Only the posterior commissure is visible, partial view of the glottis
Grade III: Only the epiglottis is seen
Grade IV: No epiglottis or glottic structure visible, only soft palate
True or false: One indicator by itself does not predict difficult airway
True
Three minimum requirements for successful direct laryngoscopy (DL)
1. The mouth must open (at least a little)
2. The three axes — oral, pharyngeal, and tracheal — must be at least somewhat aligned in the sniffing position
3. There must be space to displace the tongue and see the glottis
The amount of the _________ you can visualize correlates with the difficulty of intubation
Posterior pharynx
What anatomical feature can obscure the view of the pharynx and larynx during intubation?
A large tongue relative to the size of the mouth
A relatively large tongue that limits pharyngeal and laryngeal visualization is a common airway challenge in which condition?
Down syndrome
What are five predictive risk factors for difficult direct laryngoscopy?
1. Limited jaw movement
2. Poor head and neck movement
3. Receding chin (small mandible)
4. Buck teeth (prominent maxillary incisors)
5. Obesity
Which commonly cited risk factor for difficult laryngoscopy is not considered an independent predictor?
Obesity