Lecture 3 - Disorders featuring Somatic symptoms
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
What are 5 Somatic symptom and related disorders (SSRD) based on the DSM-5?
Somatic symptom disorder
Illness anxiety disorder
Conversion disorders / Functional Neurologic Disorders (FND)
Factitious disorder (less prevalent than somatic symptom disorders)
Psychological factors affecting other medical conditions
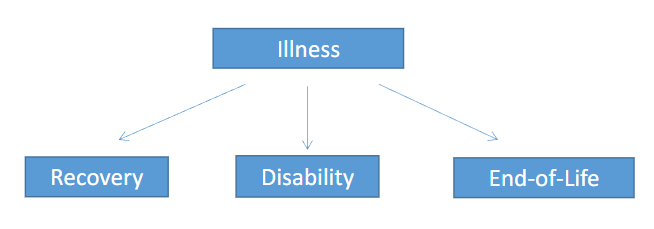
What is an illness?
Cluster of symptoms or complaints.
It has a specific (organic) cause.
A defined course.
A specific outcome.
What are 4 things a symptom can be a part of? What do they entail?
Disease : biological / medical substrate.
Disorder : disturbances, typically with a known biomedical underpinning, but not necessarily (e.g. depression).
Illness : the feeling of being ill (self-report).
Sickness : not fulfilling social roles, calls sick at work, limited functioning, patient role.
What is the prevalence of syndromes?
Research suggests that 17% of patients under the care of general
physicians (family physician) display physical symptoms that have no
apparent physical cause.
This estimate is consistent with other literature in this field, indicating a prevalence of approximately 20% (“persistent somatic symptoms”)
What is a syndrome?
Cluster of symptoms (and signs) that co-occur more often than expected by change (not ‘at random’); often without a clear cause / pathology.
Represents non-normal behavior or experiences, the symptoms belong together.
Clusters are clearly defined (recognizable) and saliently different from other clusters.
Purely descriptive, the (somatic) cause is not necessarily known.
What are the notions of Pathology of Somatic symptoms?
Somatic pathology → Somatic symptom
Psychopathology → Somatic symptom
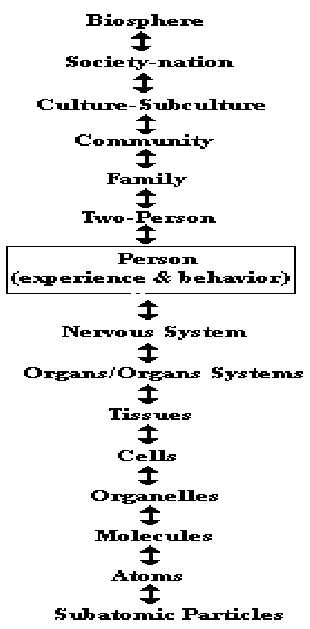
What is Engel’s Hierarchy of Natural systems?
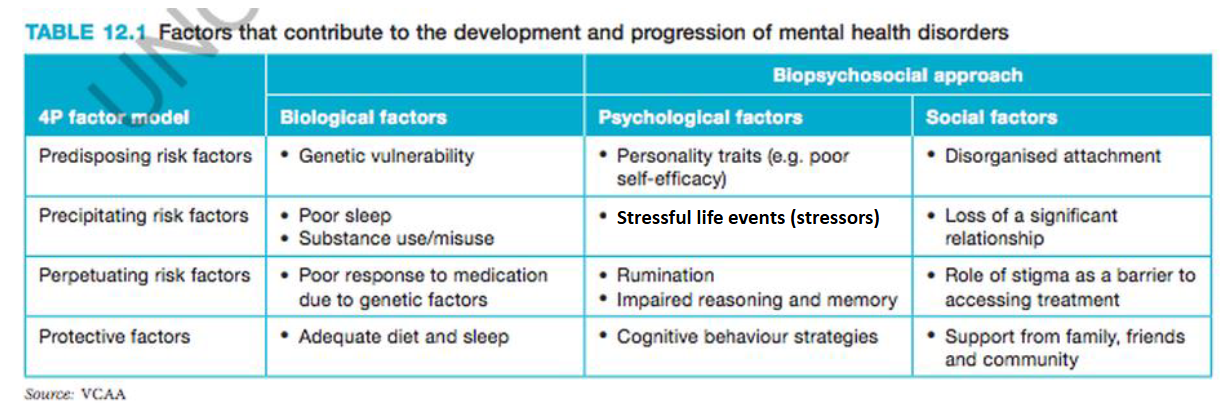
What are the differences between predisposing, precipitating and perpetuating factors?
Predisposing = Conditions and activities that can lead to the development of disease; factors that put a child at risk of developing a problem.
“Why me?”
Precipitating = Specific event of trigger to the onset of the current problem.
“Why now?”
Perpetuating = Behaviors or environmental factors that maintain or worsen a mental illness.
“Why still?”
(Protective factors) = Influences that make it less likely that individuals will develop a mental health problem.
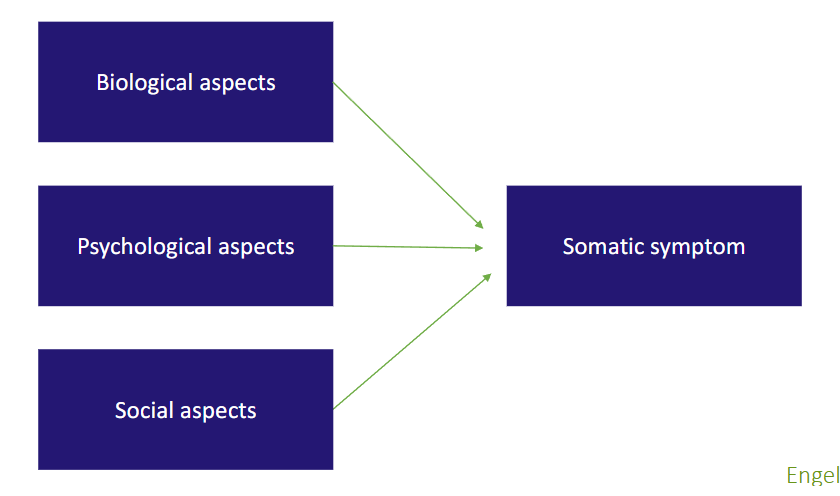
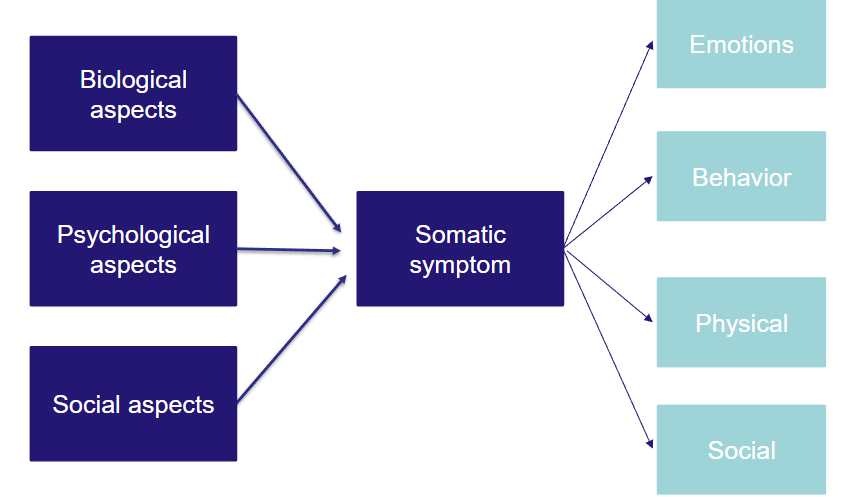
What does the Biopsychosocial model of factors that contribute to the development and progression of mental health disorders look like?
What are the 4 types of Somatic symptom disorder (SSD) and Related disorders (SSRD)?
• Somatic symptom disorder (SSD)
• Illness anxiety disorder (in DSM-IV: hypochondriasis)
• Conversion disorder / Functional Neurological (symptom)
Disorder)
• Factitious disorder (imposed on self versus imposed on
another)
• Other specified somatic symptom and related disorder
• Unspecified somatic symptom and related disorder
What is a Critical symptom in SSRD?
Fatigue and Pain.
What are the Classifications of Somatic symptom disorder (SSD) according to the DSM-5?
A. One or more somatic symptoms that are distressing or result in
significant disruption of daily life.
B. Excessive thoughts, feelings, or behaviors related to the somatic
symptoms
Disproportionate and persistent thoughts about the seriousness of one’s symptoms (cognitions).
Persistently high level of anxiety about health or symptoms (affect).
Excessive time and energy devoted to these symptoms or health concerns (behavior).
C. Complaints present more than 6 months.
What are the 3 Specifications of Somatic symptom disorder (SSD)?
Specify if
With predominant pain (previously “pain disorder”): This specifier is for individuals whose somatic symptoms predominantly involve pain.
Specify if:
Persistent: a persistent course is characterized by severe symptoms, marked impairment, and long duration (more than 6 months).
Specify if:
Mild: Only one of the symptoms specified in Criterion B is fulfilled.
Moderate: Two or more of the symptoms specified in Criterion B are fulfilled.
Severe: Two or more of the symptoms specified in Criterion B are fulfilled, plus there are multiple somatic complaints (or one very severe somatic symptom).
How prevalent is SSD?
• Estimated: 5-7% (exact % still unknown)
• Expectation: higher than thaf for somatization disorder (<1%)
• Lower than that of the undifferentiated somatoform disorder (19%)
• More common in women than men
• Possibly more common in people with medical disorders
Explained or unexplained is not relevant for SSRD anymore.
True or False?
True.
• Dutch: “Somatisch Onvoldoende verklaarde Lichamelijke
Klachten (SOLK)”
• Since 2021 referred to as: “Aanhoudende lichamelijke
klachten (ALK)” = “Persistent Physical Symptoms”
Other terms: Medical Unexplained Somatic / Physical
Symptoms (MUSS / MUPS); substantial overlap with SSD,
but DSM-5 criterion B essential difference
What are “Medically Unexplained” Somatic Symptoms (MUSS)?
Somatic symptoms that persist for > a couple of weeks while there is no medical or biological substrate or deficit to sufficiently explain the complaints.
MUSS is considered a ‘working hypothesis’ based on the (demonstrable) premise that somatic or psychological pathology has been ruled out.
Similar to: “Functional Somatic Disorder” (FSD)), “Functional Somatic Symptoms”
Examples: Non-cardiac chest pain, fibromyalgia, chronic fatigue syndrome, irritable bowel syndrome.
People with these conditions often do not appreciate a psychological explanation of (part of) their symptoms; often prefer a somatic causal explanation.
Continued debated about terminology / names: currently preferred: Persistent Physical symptoms (PPS).
How prevalent are MUSS / FSD / PPS?
Prevalence somatic symptoms::
• General population: 85-95%2
Prevalence MUSS:
• General population: 20-26%3,4
• Primary care: 25-84%5-9
• Secondary care: 35-53%4
What are the 6 Most common symptoms of MUSS / FSD / PPS?
Headache
Backache
Pain in joints
Stomach ache
Fatigue
Nausea
What are 4 Functional somatic disorders (MUSS / PPS) and their main complaints?
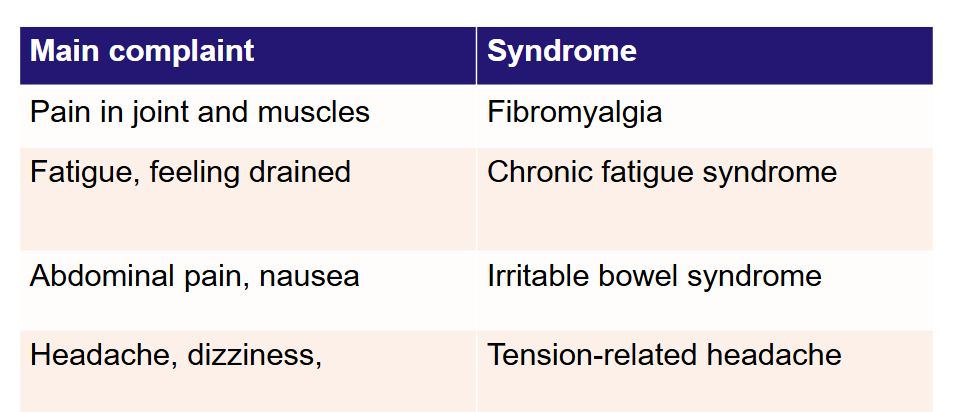
What is Comorbidity in Somatic disorders?
Both psychological as physical symptoms are present.
More somatic disorders → Higher prevalence of anxiety and depressive disorders.
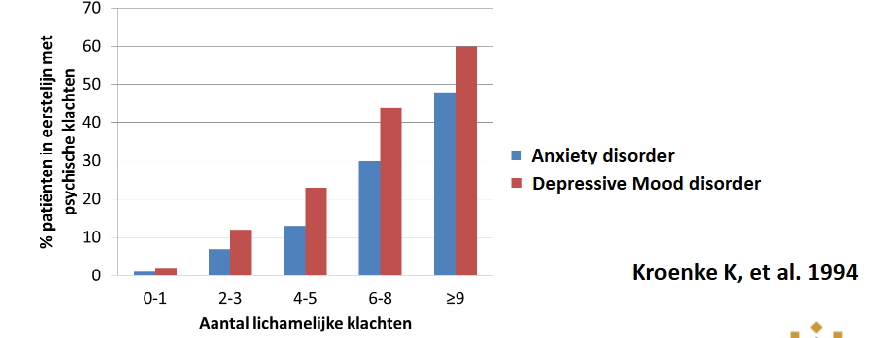
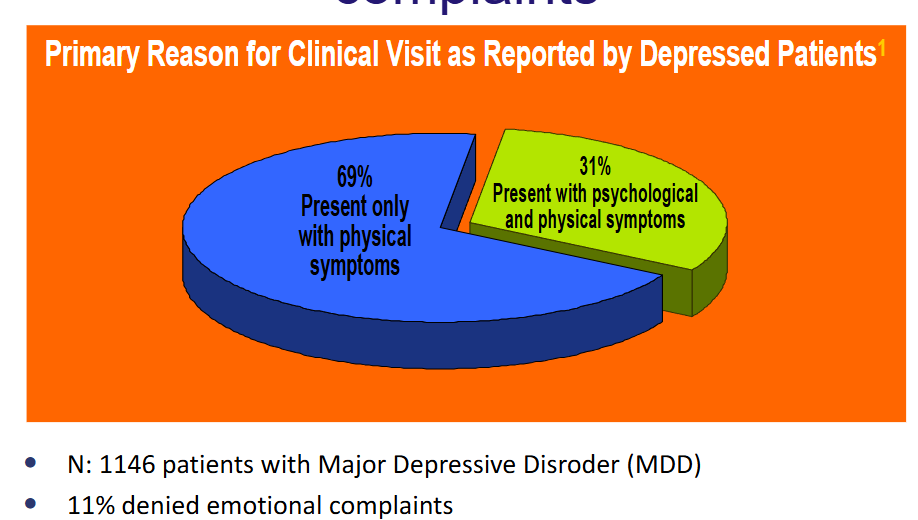
What is remarkable about Patients with psychological disorders?
They report more somatic symptoms than healthy controls.
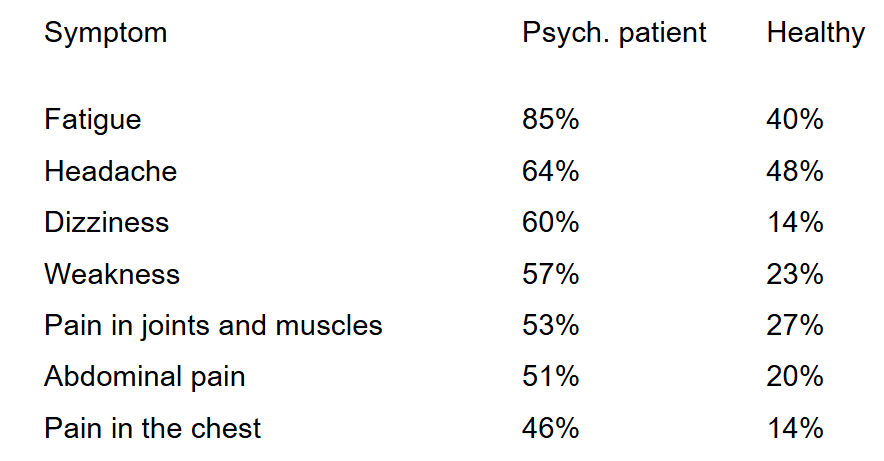
What do Patients with Major depressive disorder (MDD) report as main complaints?
MUSS.
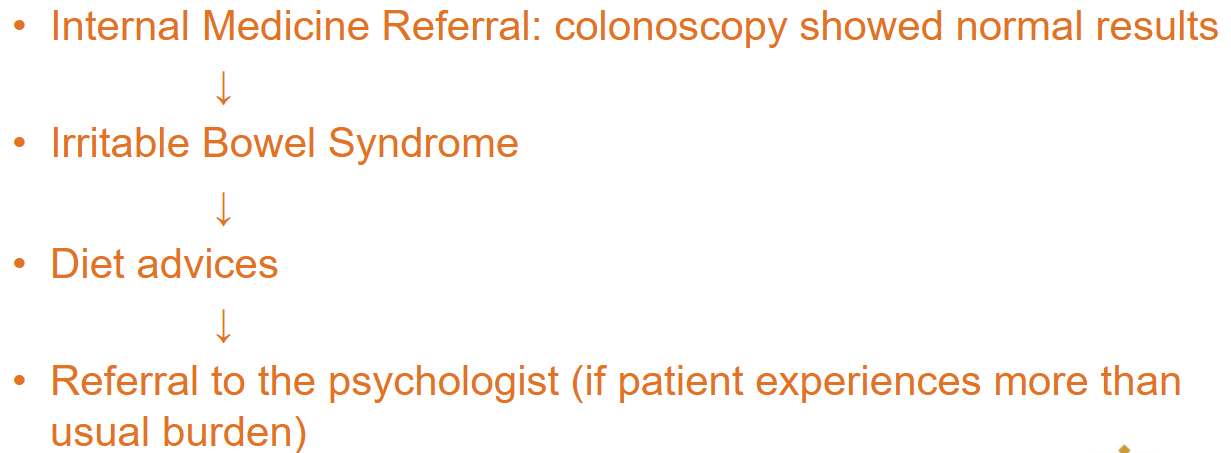
What are 4 Vignettes — Differential Diagnosis?
Colorectal cancer
Irritable Bowel syndrome (i.e. a functional disorder)
There must be something else physical going on
Illness anxiety disorder
What is the General Practitioner’s Perspective on Vignette — Differential diagnosis?
What are the Classifications for Illness anxiety disorder according to the DSM-5?
A. Preoccupation with having or acquiring a serious illness.
B. Somatic symptoms are not present or if present, are only mild in intensity. If another medical condition is present or there is a high risk for developing a medical condition (e.g., strong family history is present), the preoccupation is clearly excessive or disproportionate.
C. There is a high level of anxiety about health, and the individual is easily alarmed about personal health status.
D. The individual performs excessive health-related behaviours (e.g., repeatedly checks his or her body for signs of illness) or exhibits maladaptive avoidance (e.g, avoids doctor appointments and hospitals).
E. Illness preoccupation has been present for at least 6 months, but the specific illness that is feared may change over that period of time.
F. The illness-related preoccupation is not better explained by another mental disorder (such as somatic symptom disorder, panic disorder, generalized anxiety disorder, body dysmorphic isorder, obsessive-compulsive disorder, or delusional disorder, somatic type).
What are the 2 specifications of Illness anxiety disorder?
Specify whether:
Care-seeking type : medical care, including physician visits or undergoing tests and procedures, is frequently used.
Care-avoidant type : Medical care is rarely used.
What are the classifications of Conversion disorder / Functional Neurological Disorder (FND) according to the DSM-5?
A. One or more symptoms of altered voluntary motor or sensory function (some also include cognitive symptoms – e.g., memory loss).
B. Clinical findings provide evidence of incompatibility between the symptom and recognized neurological or medical conditions.
C. The symptom or deficit is not better explained by another medical or mental disorder.
D. The symptom or deficit causes clinically significant distress or impairment in social, occupational, or other important areas of functioning or warrants medical evaluation.
What are the specifications for Conversion disorder / Functional Neurological Disorder (FND)?
Specify symptom type:
With weakness or paralysis
With attacks or seizures
With abnormal movement
With anesthesia or sensory loss
With swallowing symptoms
With special sensory symptom
With speech symptom
With mixed symptom
Often triggered by emotional event (trauma).
People with conversion disorder do not consciously want or purposely produce their symptoms (different from factitious disorder).
Stress-experience assumed to be ‘converted’ into somatic symptoms — FND is probably more precise.
What are the Classifications of Factitious disorder according to the DSM-5?
(Munchausen syndrome).
A. Falsification of physical or psychological symptoms, or induction of injury or disease, associated with identified deception.
B. The individual presents herself or himself to others as ill, impaired, or injured.
C. The deceptive behavior is evident EVEN in the absence of obvious external rewards.
D. The behavior is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder.
What are the 2 types of Factitious disorder?
Imposed on self (Munchausen syndrome)
Imposed on another (Munchausen syndrome by proxy)
What are 3 remarkable things about Patients with Factitious disorder?
Client often knowledgeable about medicine.
Willing to endure substantial pain or medical procedures.
Recurrent use of different medical care facilities / doctors.
What is Factitious disorder by proxy?
Not the person himself, but a dependent (often a child) is injured or poisoned to get medical attention.
Caregiver often “protective” and common with some medical background.
Reasons for engaging in this behavior is similar as self-induced factitious consequences of disorder.
What is the difference between factitious disorder and simulation/malingering?
It is difficult to distinguish between both.
Simulation (falsification) is part of the definition of factitious disorder.
Malingering is not mentioned separately in the DSM-5 anymore, as it is not a ‘Psychiatric or Psychological Disorder’.
The motivation for falsification is to become a ‘patient’ → Factitious disorder.
External rewards motivates the behavior → Malingering
What are the DSM-5 Classifications of Psychological factors affecting other medical conditions?
A. A medical symptom or condition (other than a mental disorder) is present.
B. Psychological or behavioral factors adversely affect the medical condition in one of the following ways:
The factors have influenced the course of the medical condition as shown by a close temporal association between the psychological factors and the development or exacerbation of, or delayed recovery from, the medical condition.
The factors interfere with the treatment of the medical condition (e.g., poor adherence).
The factors constitute additional well-established health risks for the individual.
The factors influence the underlying pathophysiology, precipitating or exacerbating symptoms or necessitating medical attention.
C. The psychological and behavioural factors in Criterion B are not better explained by another mental disorder (e.g., panic disorder, major depressive disorder, posttraumatic stress disorder).
What are the 4 types of Severity?
Light: Increases medical risk (e.g., inconsistent adherence with antihypertension treatment).
Mild: Aggravates underlying medical condition (e.g., anxiety aggravating asthma).
Moderate: Results in medical hospitalization or emergency room visit.
Severe: Results in severe, life-threatening risk (e.g., ignoring heart attack symptoms)
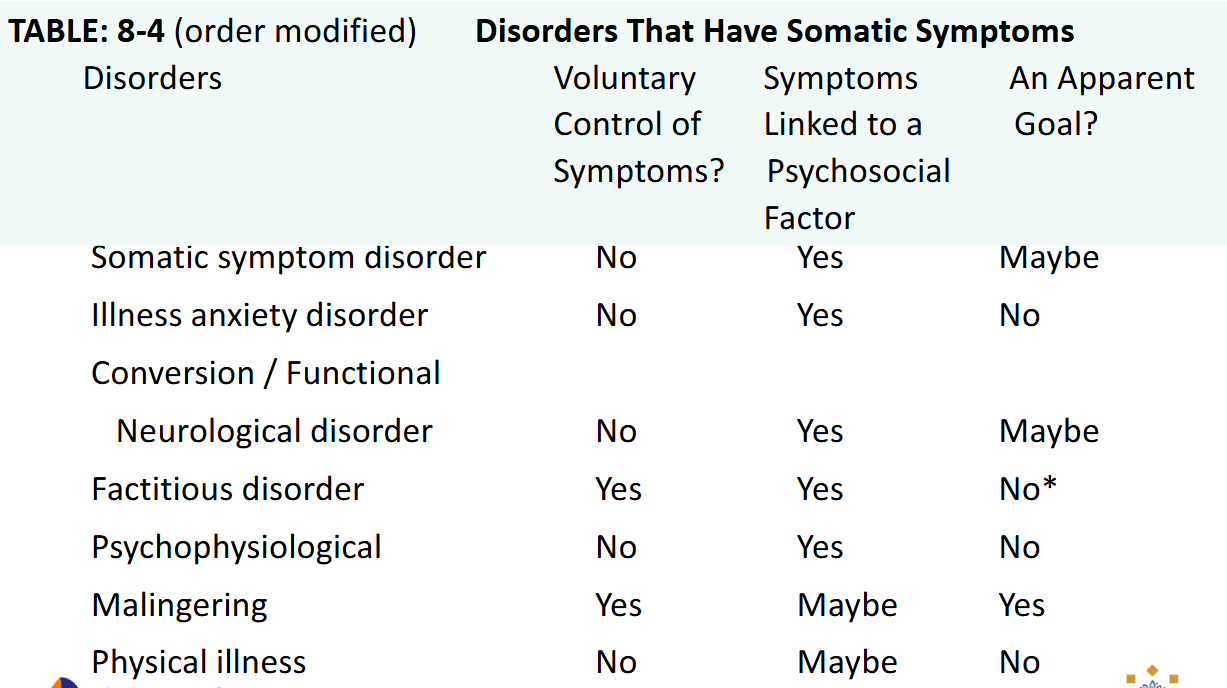
Disorders that have Somatic Symptoms Disorder table.
*except for medical attention.
What does a Typical SSRD patient look like? What are 7 qualities?
Long history of searching an answer, endlessly in assessment.
Little trust in health care and clinicians
Highly (self) critical, perfectionist, competitive
More often women
Low SES, smaller social network network
Often traumatic experiences in the past
Difficulties with mentalization
What is Mentalization?
The ability to understand the mental state — of oneself or others — that underlies behavior.
What is Bodily focused mentalization?
Deducing emotions from bodily sensations.
What could Mentalization mean for the Therapeutic interaction?
• Complain, reject treatment
• Feels rejected
• Misunderstandings
• Difficult to structure all the information
• Rejects psychological perspective
What does the Psychodynamic theory say about SSRD?
In general: Psychological factors (either within awareness or unaware) affect experiences of somatic symptoms.
There is little direct evidence for the psychodynamic explanation of SSRD, including functional neurological disorder (e.g., repressed sexual desires or repressed anger). “
Note: textbook” is insufficiently critical of this outdated view of FND developed in the Victorian era – hence reluctance for the term conversion disorder.
There are, however, substantial indications that emotion regulation is disturbed in FND, and that interventions such as hypnosis can be helpful
What does the Cognitive Behavioral theory say about SSRD?
Reward-related onset or maintenance of physical symptoms.
However, the research does not strongly support the ‘reward’ component of symptoms.
Secondary gain is part of both psychodynamic and cognitive behavioral theory — although the place this construct plays differs.
An alternative view is that symptoms have a communication function.
What does the Culture-Oriented theory say about SSRD?
Cultures differ in ‘psychopathologizing’ the expression of emotions as somatic symptoms: Industrialized countries typically pathologize somatic expression of emotion.
e.g. In Chinese culture, the expression of sadness is often stigmatized more than somatization.
e.g. in South America, the expression of emotion in terms of physical symptoms is relatively more common than other parts of the world.
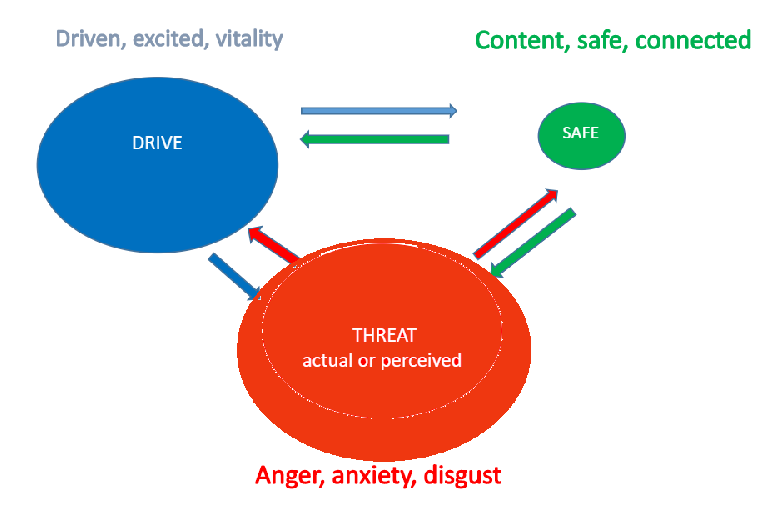
What are 3 Emotional regulation systems?
Drive system
Purpose: to motivate us towards resources.
Nuclus accumbens, Dopamine
Feelings: wanting, pursuing, achieving, progressing, focused.
Soothing system
Purpose: to manage distress & promote bonding.
Prefrontal cortex, Opiates Oxytocin.
Feelings: contented, safe, protected, cared-for, trust.
Threat system
Purpose: threat decisions & protection ‘better safe than sorry’.
Amygdala, Adrenaline, corticsol
Feelings: anxiety, anger, disgust.
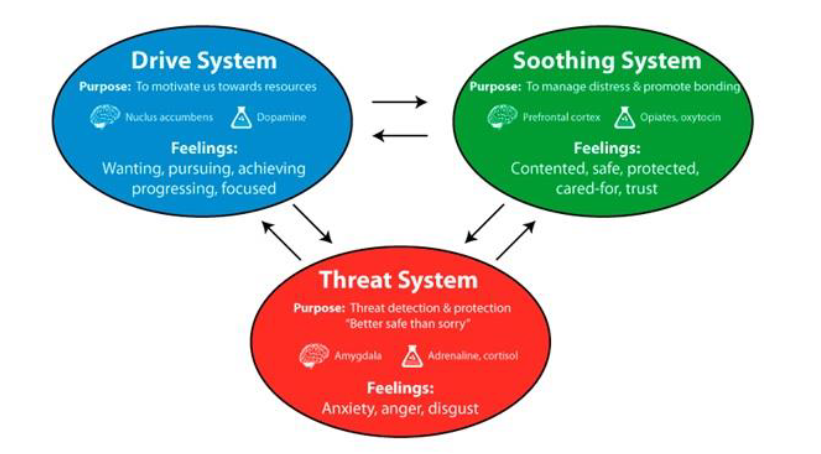
What are the main feelings of the 3 Emotional regulation systems?
What is the Center for Body, Mind and Health (“Centrum voor Lichaam, Geest en Gezondheid” (CLGG)?
Excellence Center for Tertiary care.
National level
People with somatic and psychological symptoms
Explained or unexplained
Psychological symptoms as a result of main somatic conditions or symptoms
Already received secondary care, but did not help
Qualities of Patients with SSRD at the CLGG Excellence Center
Average duration of somatic symptoms
8,5 years (range 1-34 years)
Average duration of ealier treatments
6,9 years without effect (range 1-34 years)
Conflics with previous therapists / clinicians are common
Psychological and physical comorbidity
Social limitations similar to those of severe psychological disorders.
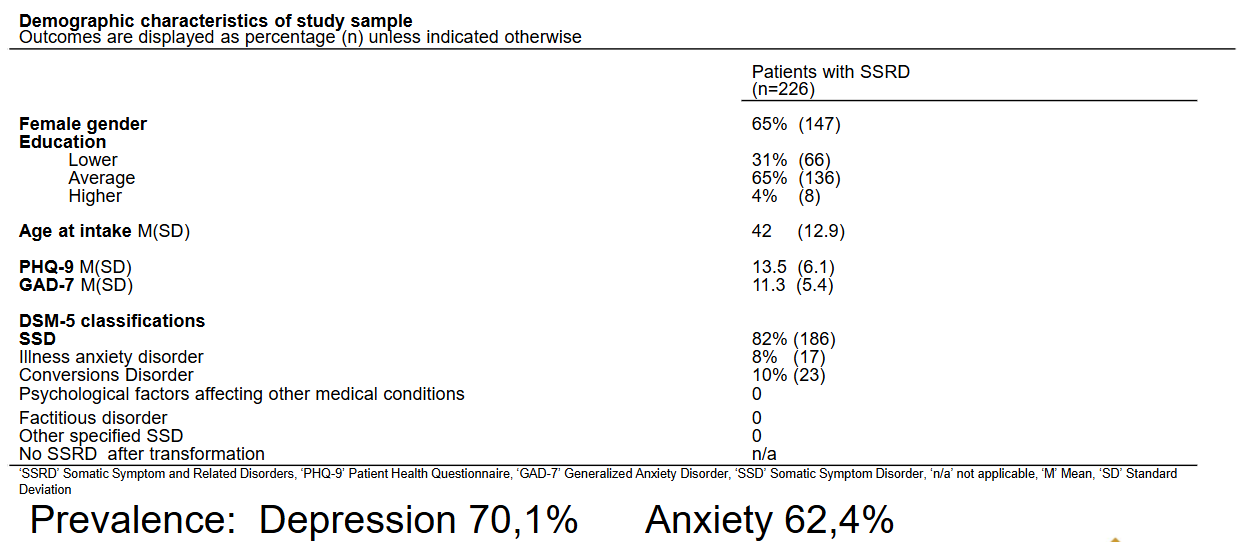
Study sample Center for Body, Mind and Health
Prevalence
Depression 70.1%
Anxiety 62.4%
What happens in the Excellence Center for Body, Mind and Health?
Assessment of domains that are problematic (Medical intake, physical examination, psychological and neuropsychological assessment, psychiatric examinations, questionnaires).
Personalized treatment: based on analysis of the risk and protective factors for the somatic symptom.
Psychiatrists, general and internal medicine physicians, psychologists (GZ-psychologists, clinical (neuro)psychologists), psychologists, psychomotor therapist, work together with psychosomatic physiotherapy.
Pharmacotherapy, CBT,, and other psychotherapeutic approaches (trauma therapy, ACT, PST, schema therapy,, cognitive rehabilitation therapy) consultation with the referring primary and secondary care physicians.
Routine Outcome Measurements and Shared Decision Making
Integration of feedback from monitoring the treatment with questionnaires measuring somatic, psychological symptoms and social functioning.
Personalized treatment “Consequences model”
The interpretation, explanation of a somatic symptom, the emotional, behavioral, physical, social consequences have perpetuating roles.

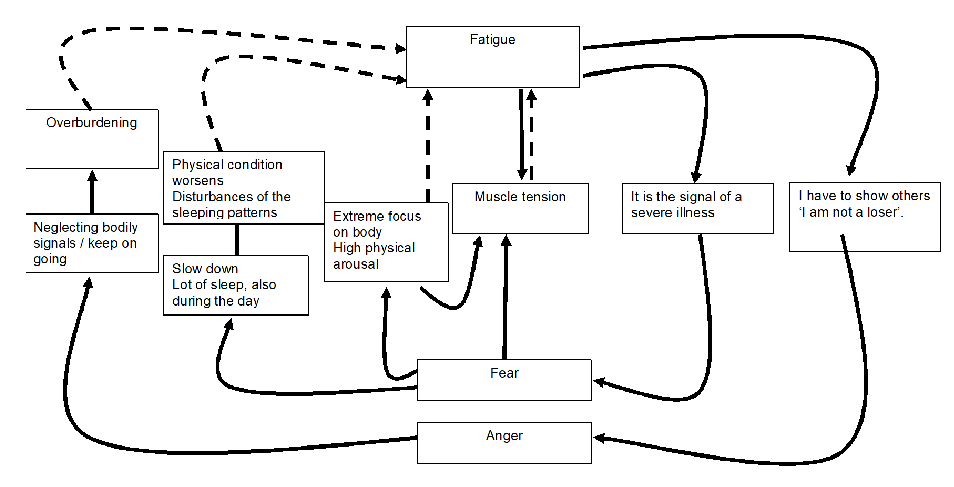
What does the Gevolgenmodel (consequences model) look like with the example of Fatigue?
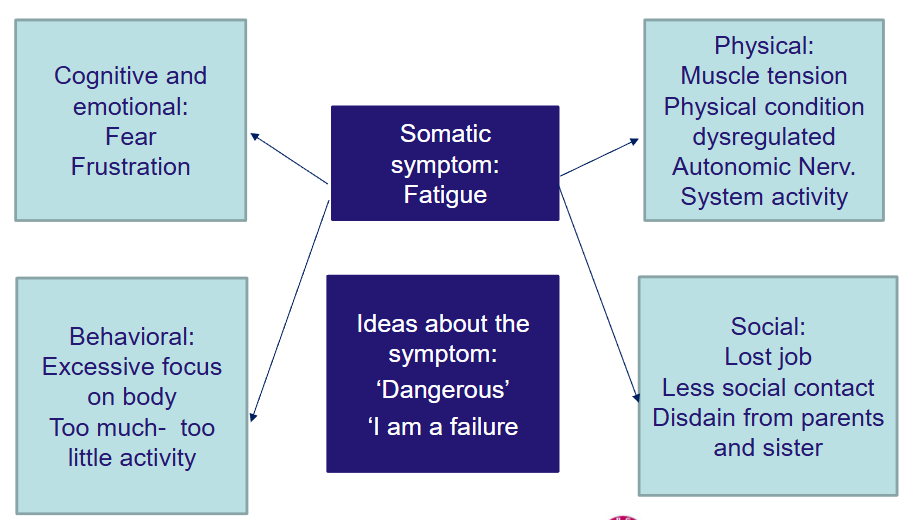
Negative circle
What are 6 types of Treatment interventions?
• Cognitive behavioral therapy
• Psychopharmacology, primarily for comorbid depression or anxiety disorder – effects on SSRD variable
• Graded Physical Activity
• Relaxation training (bv. jacobson, biofeedback)
• Concentration training (e.g., mindfulness meditation)
• PMT for bodily focused mentalization
Summary lecture 3