RENAL ANATOMY & Introduction and History (PDF 1 & 2) - AUBF - MLS 112 LECTURE PRELIM
1/26
Earn XP
Description and Tags
"For You formed my inward parts; You wove me in my mother’s womb." — Psalm 139:13 (LSB)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What are the four main organs of the urinary system?
Kidneys, Ureters, Bladder, and Urethra.
What are the 7 functions of the kidneys? (Hint: The acronym is A WET BED).
A - controlling Acid-base balance
W - controlling Water balance
E - maintaining Electrolyte balance
T - removing Toxins and waste products from the body
B - controlling Blood pressure
E - producing the hormone Erythropoietin
D - activating vitamin D
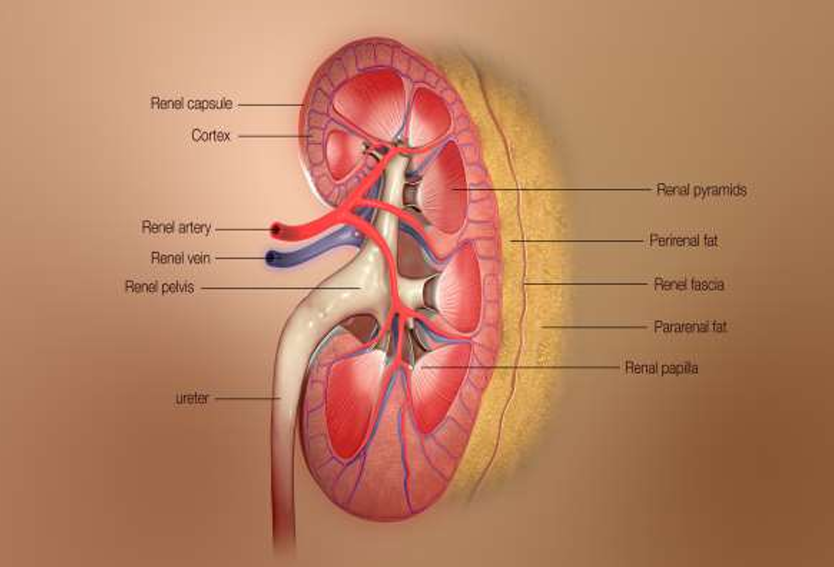
What are the three main regions of the kidney?
Renal cortex (outer region), Renal medulla (inside the cortex), and Renal pelvis (inner collecting tube).
What are the three layers that cover the kidneys, from innermost to outermost?
Renal capsule: The fibrous innermost layer that directly surrounds each kidney.
Adipose capsule: The middle layer that provides protection and helps keep the kidney in place.
Renal fascia: The double-layered outermost layer that anchors the kidney to surrounding structures.
What is the structural and functional unit of the kidneys?
The nephron.
What are the two main structures of a nephron?
The Glomerulus and the Renal tubule
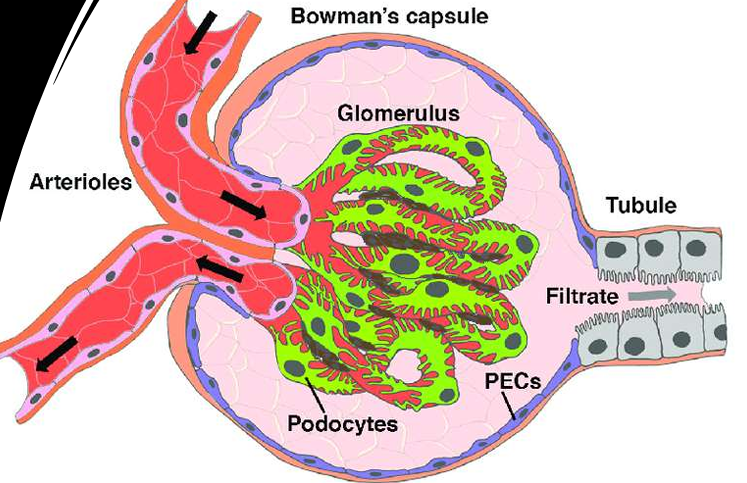
Describe the glomerulus.
The glomerulus is a specialized capillary bed that sits within a glomerular capsule. It is attached to arterioles on both sides (a large afferent arteriole and a narrow efferent arteriole), which helps maintain high pressure. The capillaries are covered with podocytes from the renal tubule.
What are podocytes and what is their function?
Podocytes are highly specialized epithelial cells that cover the outside of the glomerular capillary. They have foot processes (primary, secondary, and tertiary extensions). The primary function of podocytes is to form a crucial part of the glomerular filtration barrier.
Approximately how much blood perfuses the kidneys each minute?
About 1200 mL of blood per minute, which is roughly 25% of the cardiac output.
What is the first step in urine formation?
The glomeruli receive blood through afferent arterioles, and an ultrafiltrate of the plasma passes through each glomerulus into Bowman's space.
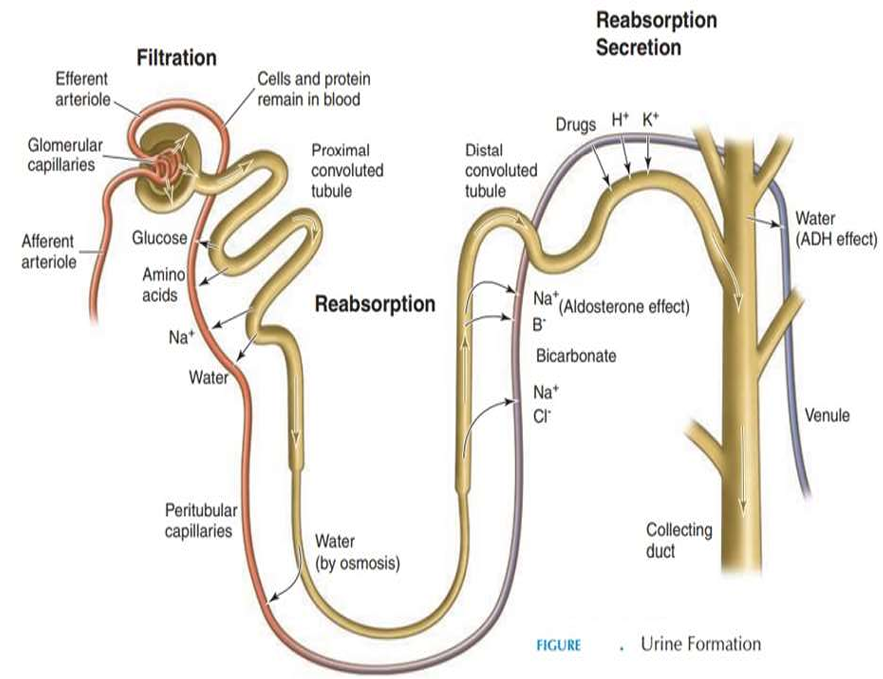
What is the fate of the glomerular filtrate after it leaves Bowman's space?
The filtrate passes through the tubules and collecting ducts, where reabsorption or secretion of various substances and the concentration of urine can occur.
How is the original glomerular filtrate volume reduced to its final urine volume?
The original glomerular filtrate volume of about 180 L in 24 hours is reduced to about 1–2 L, depending on the status of hydration.
What is the pathway of urine after it is formed in the kidneys until it is voided? (Hint: The acronym is CRUBU).
The urine passes from the Collecting ducts, into the Renal pelvis, Ureters, Bladder, and Urethra to be voided.
What was the beginning of laboratory medicine?
Analyzing urine (urinalysis).
What ancient evidence shows urinalysis was practiced?
Drawings of cavemen and Egyptian hieroglyphics such as the Edwin Smith Surgical Papyrus.
What basic observations of urine did early physicians use for diagnosis?
Color, turbidity, odor, volume, viscosity, and sweetness.
What major advancement in the Middle Ages improved urine study?
Instruction in uroscopy and development of color charts (20 different colors by 1140 CE).
What crude tests were used to detect glucose in urine before modern methods?
“Ant testing” and “taste testing.”
Frederik Dekkers’ contribution in 1694.
He discovered albuminuria by boiling urine.
Zacharias Janssen’s Contribution.
Invention of the microscope in 17th century that allowed the examination of urinary sediment.
Thomas Addis’s Contribution.
He developed methods to quantitate microscopic urinary sediment.
Richard Bright’s Contribution in 1827.
He introduced urinalysis as part of routine patient exams.
Why did urinalysis decline in the 1930s?
The number and complexity of tests made it impractical.
What rescued urinalysis as a routine exam tool?
Development of modern testing techniques.
What are the two unique characteristics of urine that make urinalysis valuable?
1) Readily available and easily collected
2) Provides inexpensive information on major metabolic functions.
How does the Clinical and Laboratory Standards Institute (CLSI) define urinalysis?
Testing urine in an expeditious, reliable, accurate, safe, and cost-effective manner.
What are the three main reasons to perform urinalysis according to CLSI?
(a) Aid diagnosis of disease
(b) Screen asymptomatic populations
(c) Monitor disease progress and therapy effectiveness.