Health and Medical Psychology
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
115 Terms
What are lay perceptions of health (Blaxter, 1990)?
Health as not ill: no visits to doctor
Health as reserve/resources: strong family, recover quickly
Health as behaviour: look after myself
Health as physical fitness and vitality: energetic
Health as psychological well-being: in harmony, balance, proud, enjoyment
Health as function: to do what I want/have to do
What is the definition of health according to WHO (1948) and what is the criticism?
A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
Criticism: black and white: two people with same symptoms can have a different health
How does the biomedical model understand health and illness and what is the criticism?
As underlying pathology, neural and/or biochemical activity (exposure to contagious agents, insufficient immune response)
Criticism: you can only become ill if a bodily process is affected, not always the case (also health behaviour, stress and emotions, social relations)
What are other predictors of health and illness?
Health behaviour
Stress/emotions
Social relations
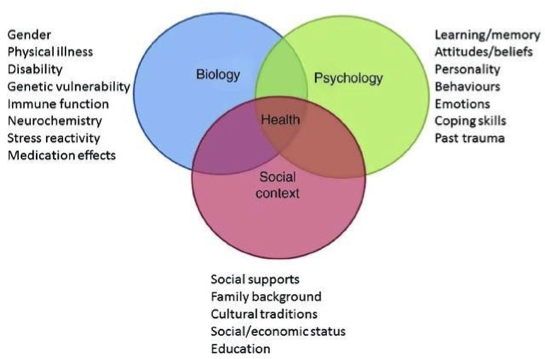
How does the biopsychosocial model understand health and illness?
Body and mind interaction
Consequences of interplay biological, psychological and social
Systems influence each other
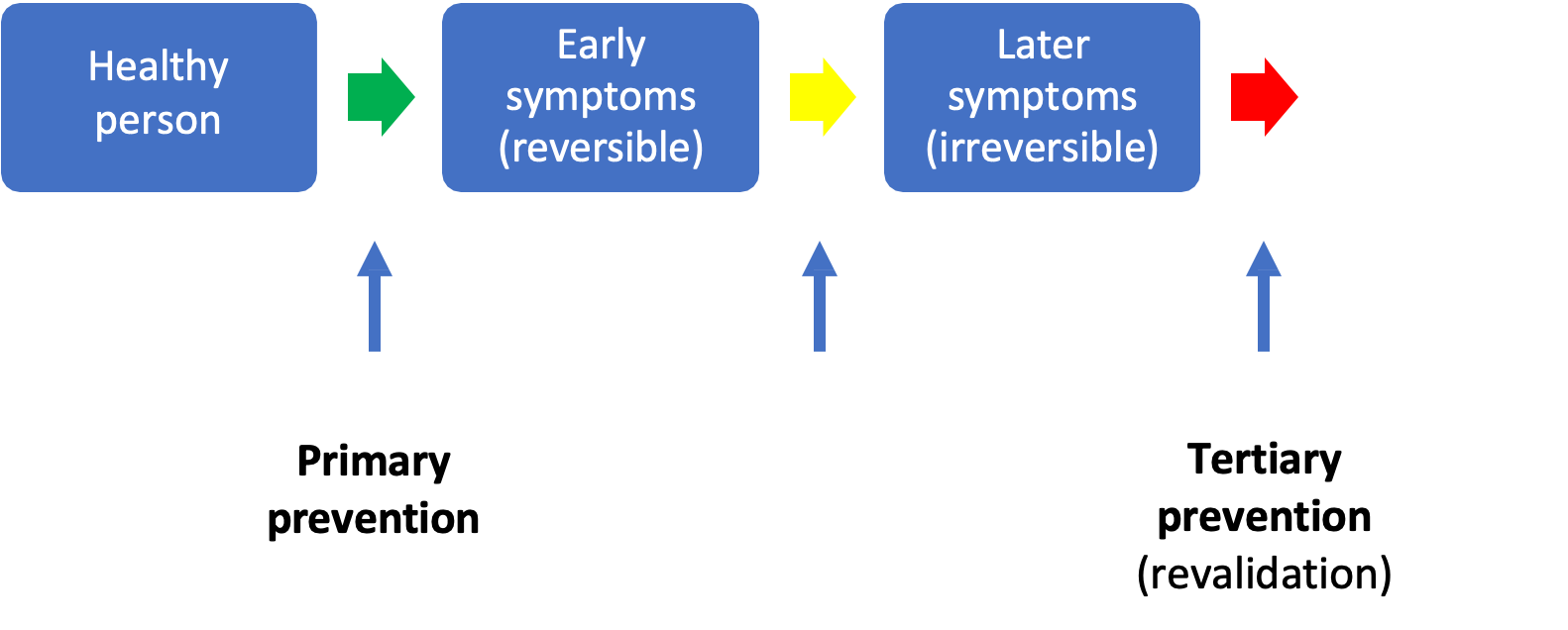
What kind of prevention are there?
Primary: prevention of problem, illness or casualty
Target group: healthy people
Secondary: tracing illness in an early phase, for early treatment or for prevention of more serious complaints
Target group: (healthy) people with increased risk for disease
Tertiary: revalidation/ living life to decrease symptoms or learning to live with it
Target group: ill people
What is the Alameda 7 for longevity?
Exercising
Drinking less than five drinks in one sitting
Sleeping 7-8 hours a night
Not smoking
Maintaining desirable weight for height
Avoid snacks
Eating breakfast
What kind of health behaviours are there (Matarazzo, 1984)
Behavioral pathogens (health risk behavior): smoking, alcohol etc.
Behavioral immunogens (health protective behaviour): exercising, sun protection etc.
Why would you influence health behaviour?
Health behavior is related to morbidity and mortality
The prevalence of risk behaviors is high
Socio-economic differences in health and health behavior
Health behavior is not always an informed choice
What diseases and their medications reduced mortality?
Measles: vaccine
Scarlet fever: penicillin
Tuberculosis: izoniazid
Typhoid: chloramphenicol
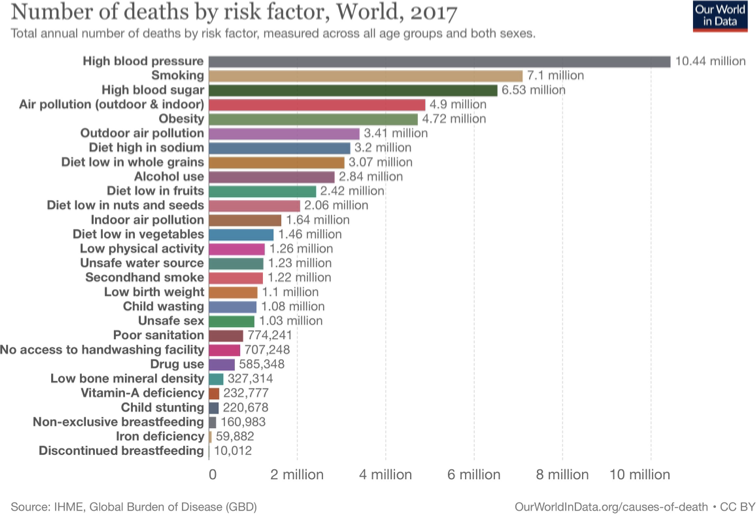
What are the top 3 main causes of death worldwide?
High blood pressure
Smoking
High blood sugar
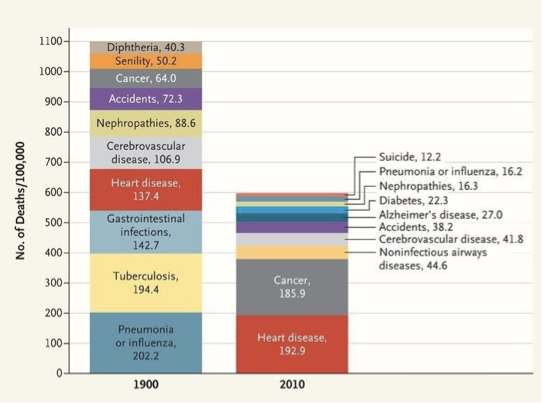
What are the main causes of death in the USA in 1900 compared to 2010? (Jones, Podolsky & Greene, 2012)
1900
Pneumonia or influenza
Tubercolosis
Gastrointestinal infections
2010
Heart disease
Cancer
Noninfectious airways disease
What adverse effects may occur in health interventions?
The interventions only reach the higher part in SES and generate inequalities
Hardening: people lose trust in the government
Stigmatizing: people who have conditions and blaming them for this
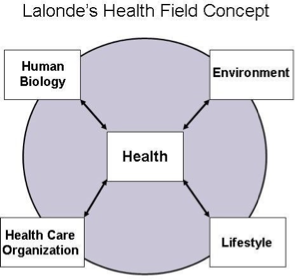
What are determinants of health according to Lalonde’s Health Field Concept?
Health risk behavior
Health promoting behavior
What are behavioural determinants of health behaviour?
Things that have been proven to influence behavior change. Effective interventions work by addressing a set of determinants (determinants —> behaviours, (CDC, 2024))
OR
The underluing factors why someone does (not) engage in health behavior
What health theories are about getting motivated?
Health Belief Model
Social Cognitive Theory
Theory of Planned Behavior/Reasoned Action Approach
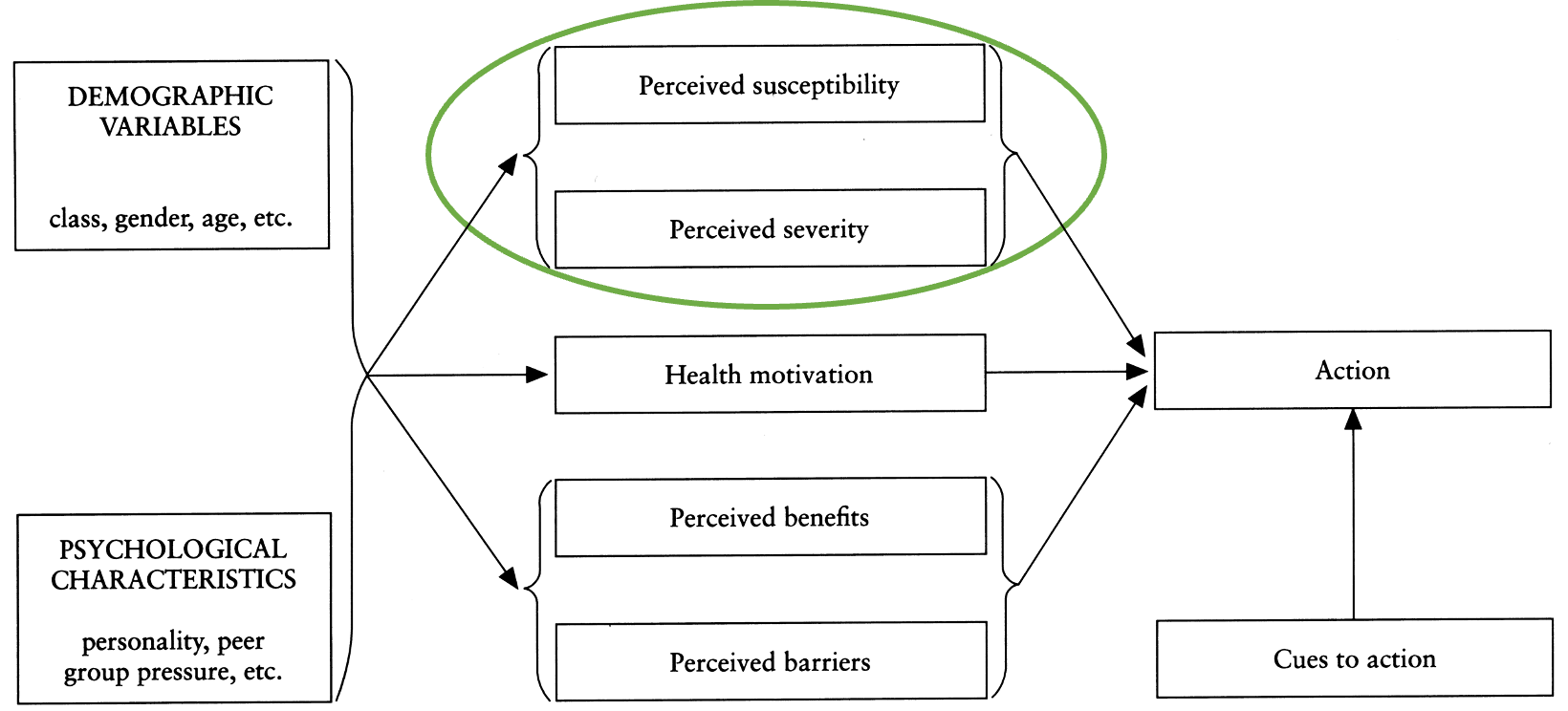
What is the Health Belief Model (Becker, 1974)?
Perceived susceptibility: how likely am I to get the disease?
Perceived severity: how bad would it be if I got the disease?
Perceived benefits: if I get the vaccine I can see my friends and family
Perceived barriers: what side-effects do you expect?
Health motivation: how motivated are you to live a healthy life in general?
Cues to action: how often are you prompted to engage in the behaviour?
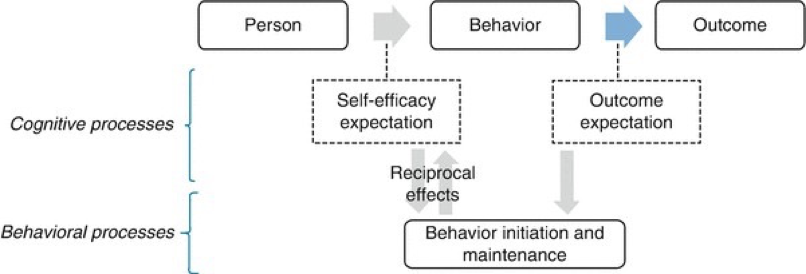
What is the basic concept of the Social Cognitive Theory (Bandura, 1977, 1989)?
Three observable elements: person, behavior, outcome
Self-efficacy: your expectation that you can engage in health behaviour and that it will help you
Outcome expectation: if I engage in this health behaviour, will it lead to the desired outcome?
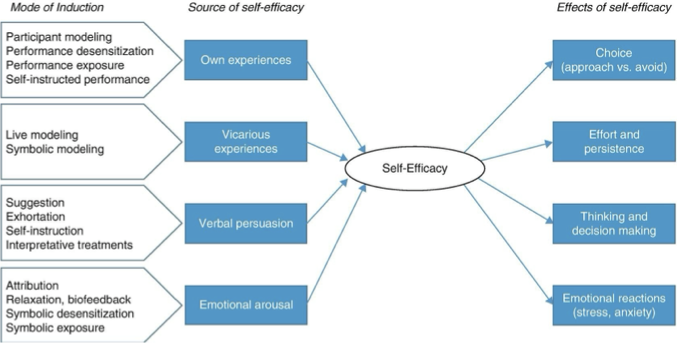
What is the Social Cognitive Theory, and then specifically self-efficacy? (Bandura, 1977, 1989)
Own experiences: if you have tried it and it did not work
Vicarious: someone else’s experiences
Verbal persuasion: someone can tell you
Emotional arousal: how you feel after doing something
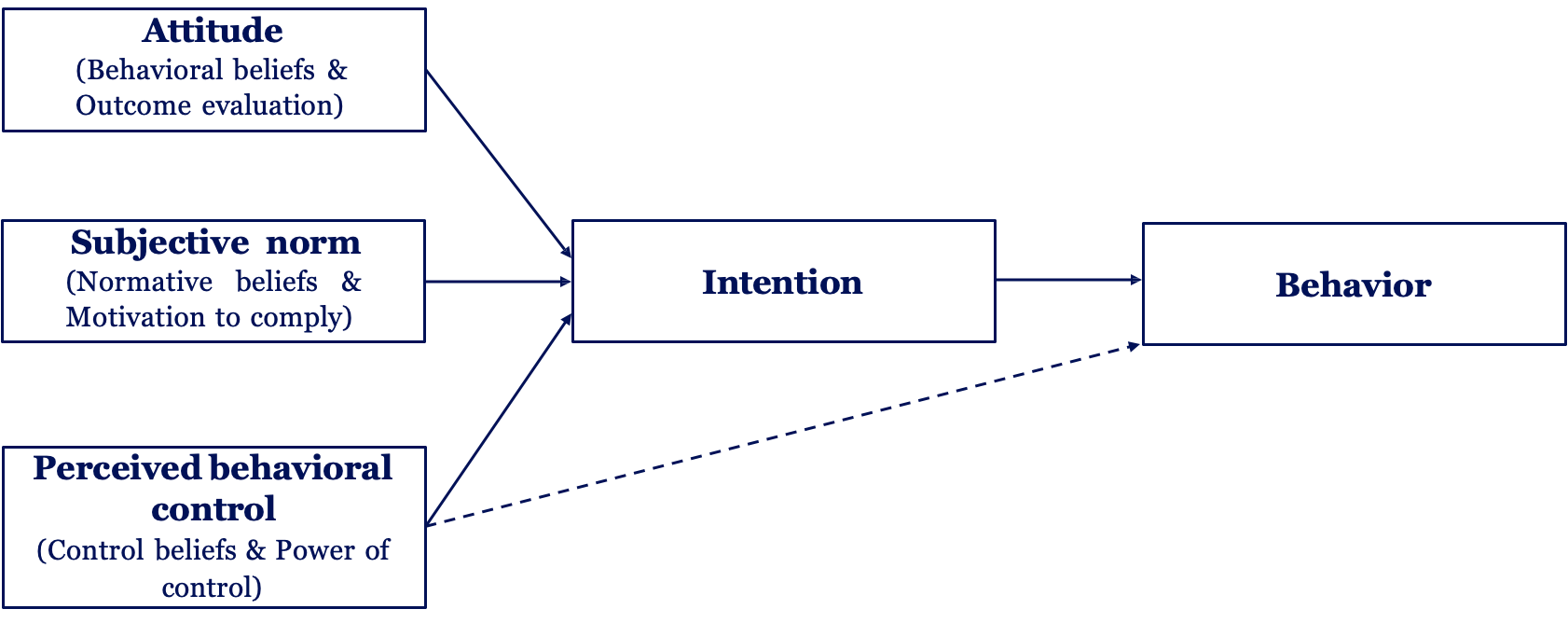
What is the Theory of Planned Behaviour (Ajzen, 1991)
Intention is the most important for engaging in health behaviour (determined by: relevance, valence, evaluation)
Attitude: your evaluations of what it will lead to (similar to outcome expectations)
Subjective norm: what others do (descriptive: what they do, injunctive: what people think is right)
Perceived: related to self-efficacy, trust in own ability
Normative beliefs: what do you think others think?
Motivation to comply: how much you care about someone’s opinion
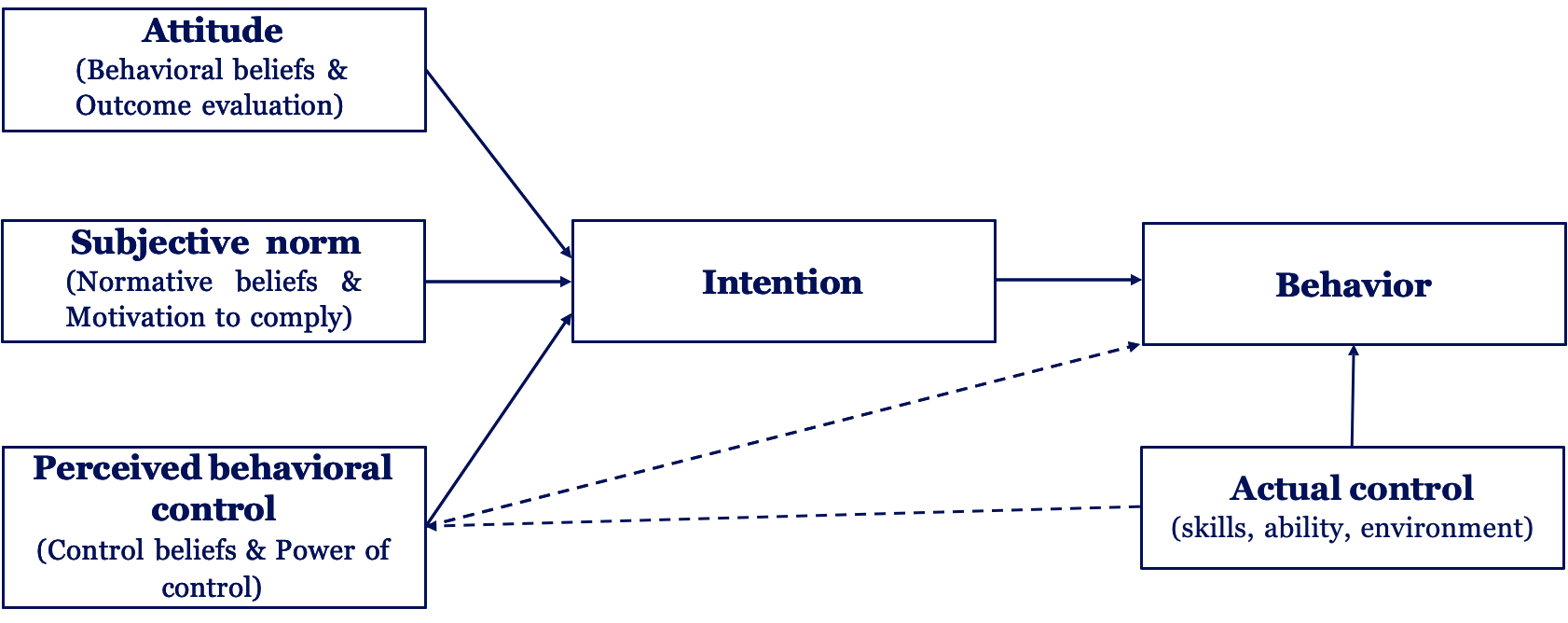
What is the Reasoned Action Approach? (Fishbein & Ajzen, 2010)
+ Actual control (skills, ability, environment)
This makes intentions turn into behaviour
What health theories are about preparing for action and starting to change?
Self-Determination Theory
Health Action Process Approach
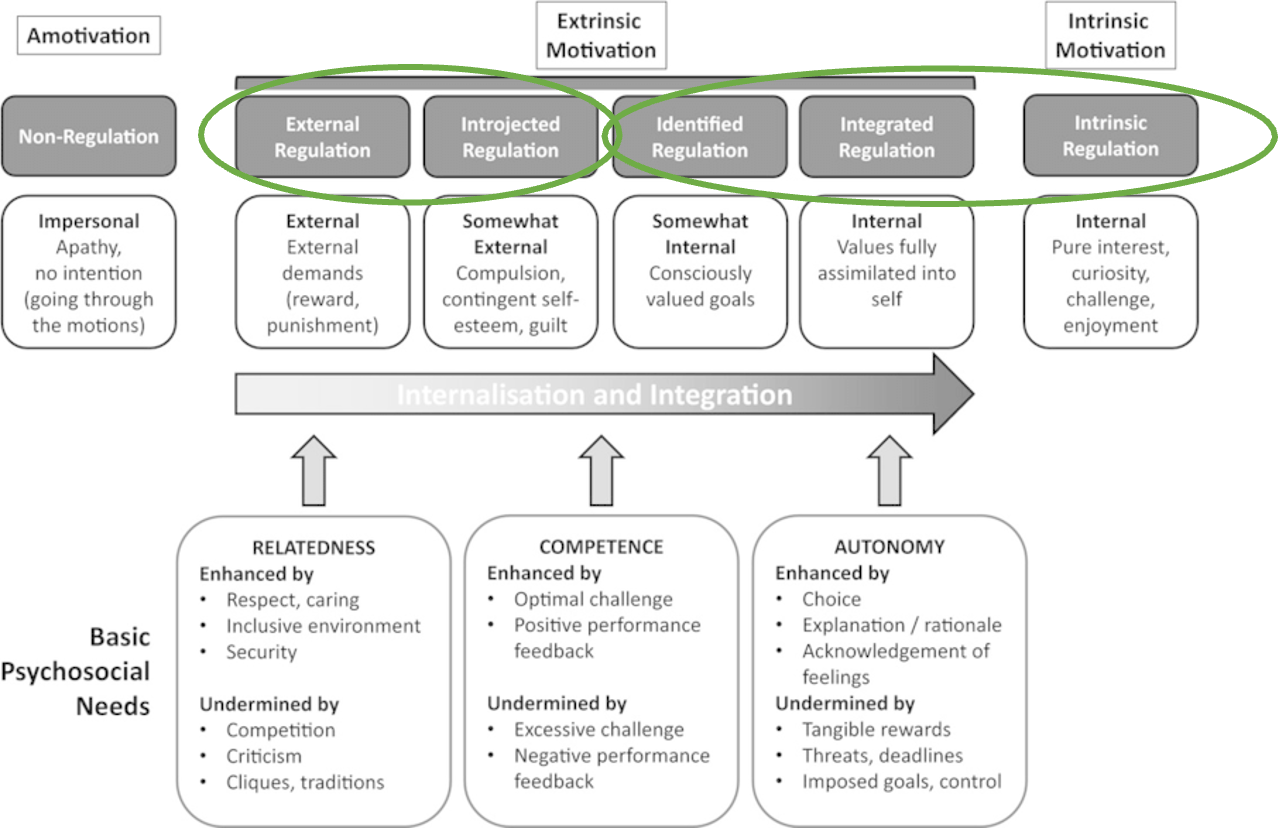
What is the Self-Determination Theory? (Deci & Ryan, 1985, 2000)
Quality of motivation: what kind of motivation drives behaviour
Amotivation: you do not know why you should engage in health behaviour
Autonomous: values that you have
Understands content of motivation
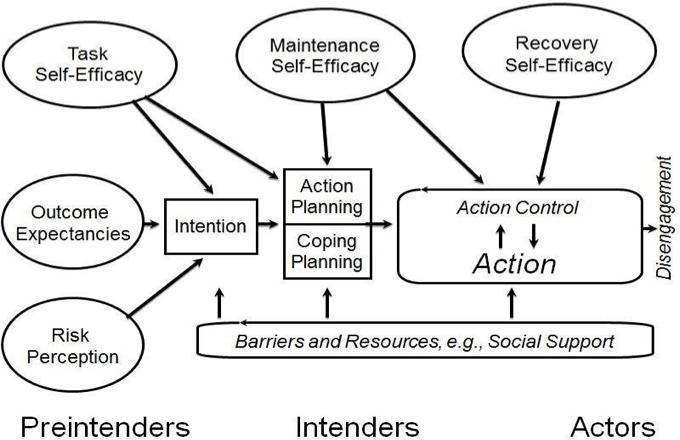
What is the Health Action Approach (Schwarzer, 1992)?
What is between intention and action
Volitional phase: how you translate intention into action
Action planning: what are you going to do about your intention?
Coping planning: how are you going to cope if things are not going according to plan?
Moves beyond motivation and highlights importance of volition
Stage model
What are dual process theories?
Theories that assume we to not always make reasoned decisions
Two systems: reflective/intuitive
We can also have reasoning (type 2) to engage in unhealthy behaviours (‘I worked hard so I deserve this chocolate)
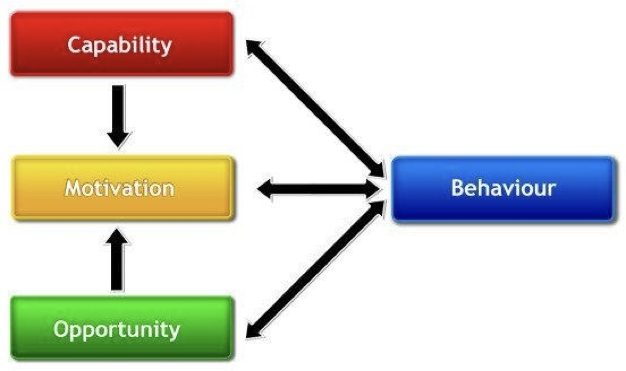
What is the COM-B model?
A model that collects all theories and simplifies it
Actual control (RAA)
Automatic & reflective processes (dual process theories), self-efficacy & outcome expectations (SCT)
Cues to action (HBM), perceived norms and behavioral control, actual control (RAA)
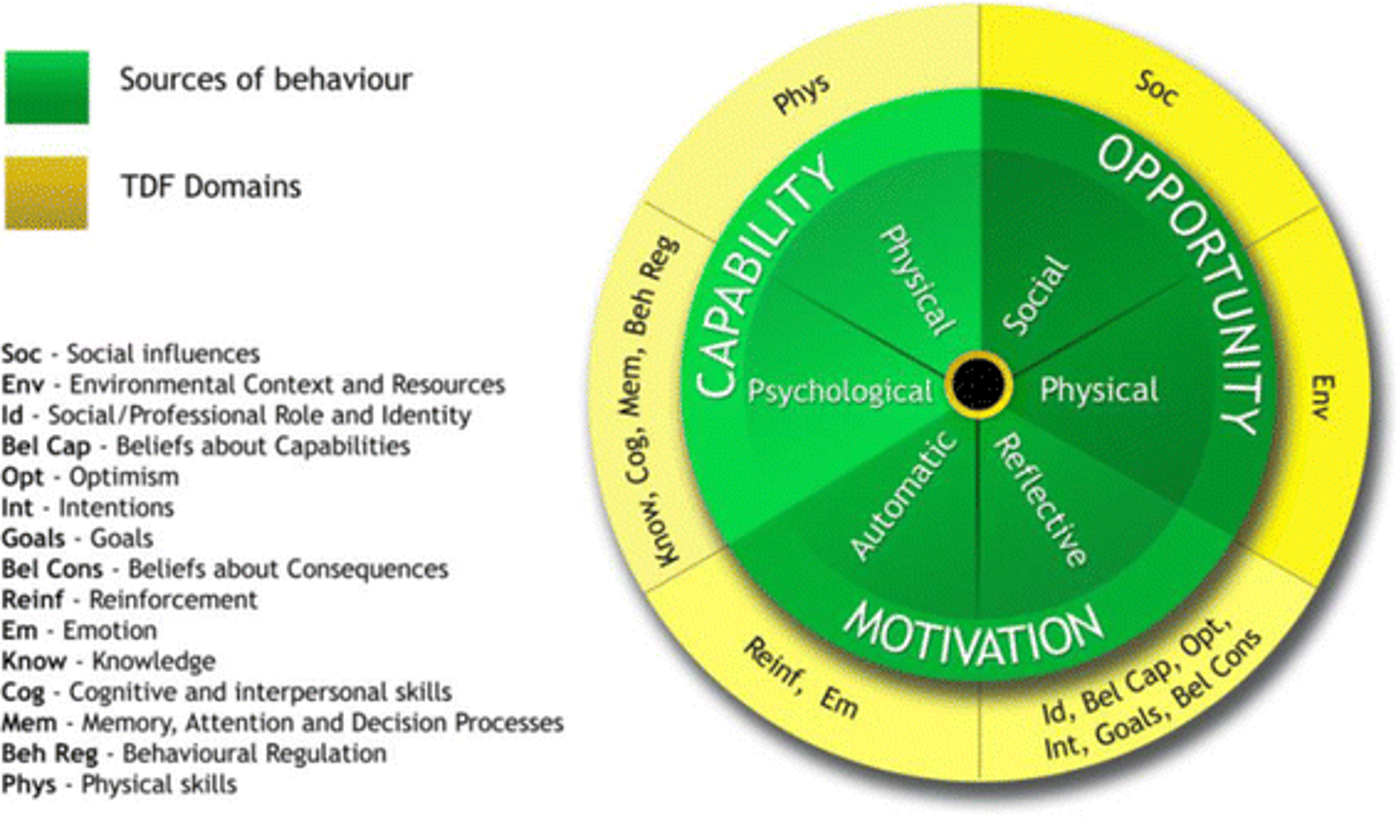
What is the Theoretical Domains Framework?
Green: COM-B
Motivation has automatic and reflective components (sources of behaviour)
Integrative model for understanding health behaviour
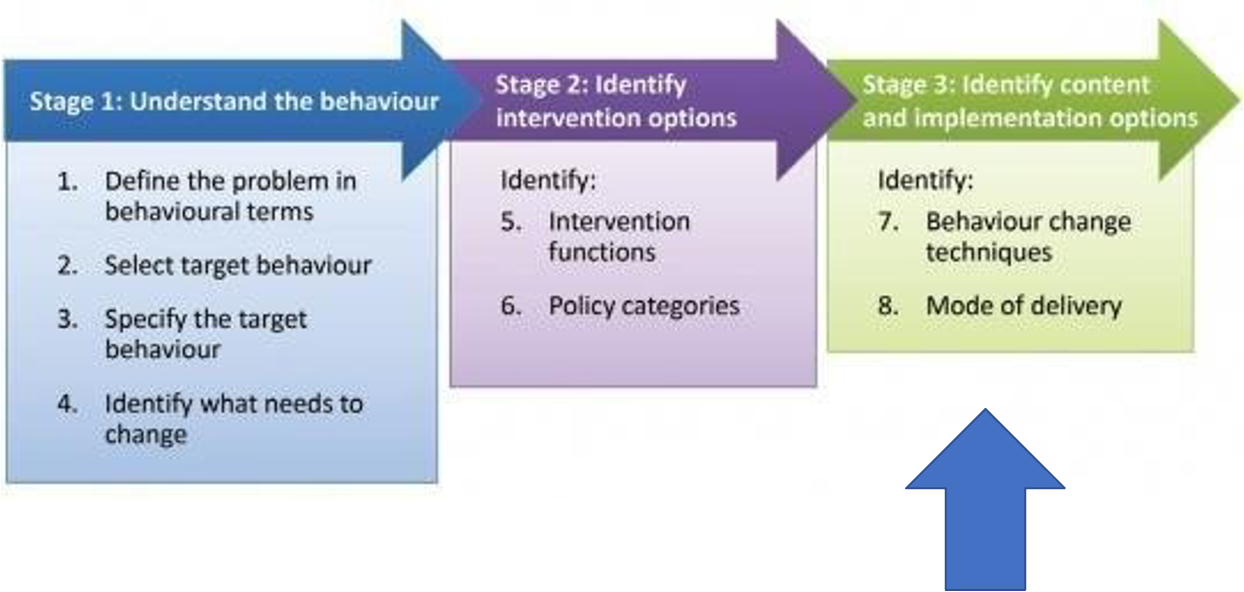
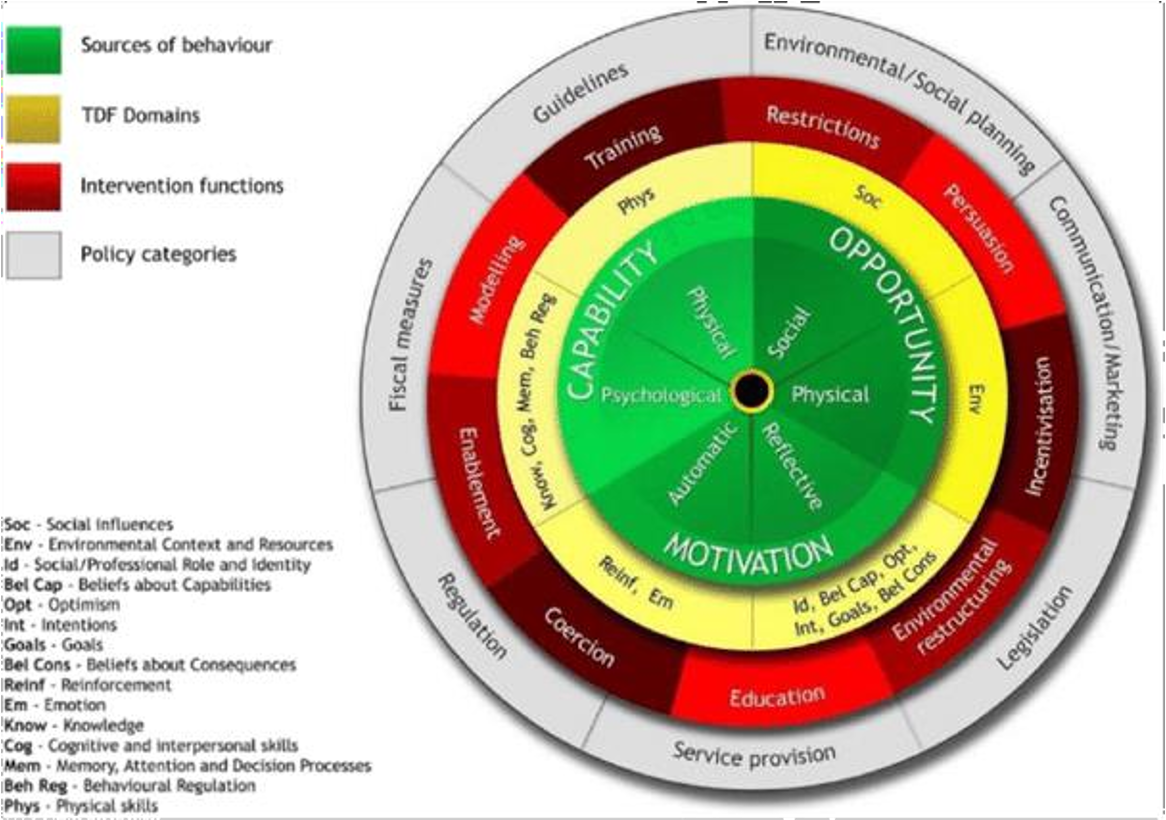
What is the Behaviour Change Wheel?
Method to guide intervention development
Red wheel: COM-B model first to characterize factors that underlie
Integrative model for understanding health behaviour
What fields do health and medical psychologists work in?
Health care: primary (huisarts), secondary (mental health organizations, rehab) en medical psychology department in hospital (multidisciplinary)
Primary prevention, policy and training
Research and policy
Self-efficacy (Bandura)
het geloof in je eigen vermogen om een specifieke taak of gedrag succesvol uit te voeren en de gewenste uitkomst te bereiken
Habit
A mental association between a cue and a goal-directed response
Behavior —> habit when frequently performed in a stable situation until context automatically triggers the behavior
Efficient
Problematic
Difficult to change despite strong intentions
Different interventions: competing with excising habits
What is the Reflective Impulse Model (Strack & Deutsch, 2004)?
Reflective system
Impulsive system
Parallel but asymmetry
What are the information provision NICE guidelines (2014)
Outcome expectancies
Personal relevance
Positive attitude
Self-efficacy
Descriptive norms
Subjective norms
Personal and moral norms
How can you motivate change?
Boosting self-efficacy (SCT)
Social norms (TPB, RAA): majority norms instead of minority norms, identification with norm referent group
Injunctive norms: what we think should be done
Descriptive norms: what people actually do (more effective than injunctive)
Fear appeals (HBM) (if too extreme, cognitive dissonance and defensive responses, so important to recommend healthy alternatives)
Self-monitoring (HAPA)
Implementation intentions/Action planning
Motivational phase= setting goals
Volitional phase= translating intentions into behavior (assumption: sufficient motivation, but it actually has to do with volitional phase)
Changing habits
By removing/avoiding cue (changing environment)
Implementation intentions (alternatives)
Promoting health-protective behaviour and decreasing habits
Nudging= strategic use of mental shortcuts (dual process models)
We do what most people do (social norms), we favour the status quo (loss aversion, inertia)
Motivational interviewing: individual approach
Fear appeal
A persuasive communication that tries to scare people into changing their attitudes by conjuring up negative consequences that will occur if they do not comply with the message recommendations (motivational technique)
Consider information inaccurate
Sensitivity to counter-information
Estimate low personal risk
Spending less time on the information
Suppressing threat-related thoughts
Making up excuses for the behaviour
Increased commitment to/intensity of the risk behaviour
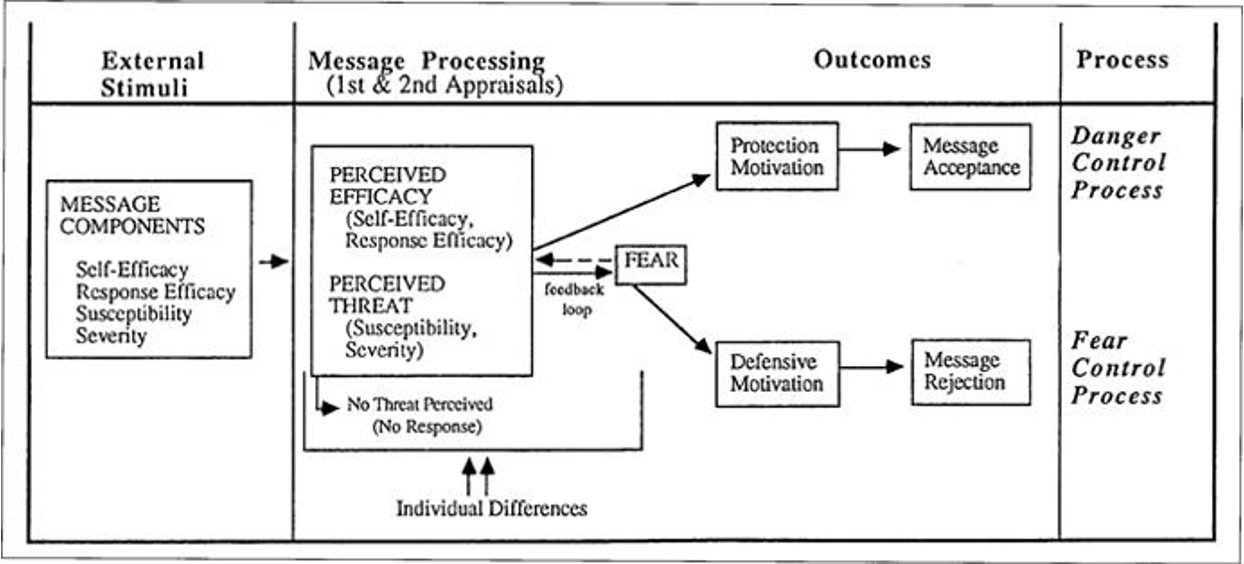
What is the Extended Parallel Process Model?
You need perceived threat and perceived efficacy to have an effective fear appeal
Protection motivation= accepting the message and using a danger control process
Defensive communication= rejecting the message and using a fear control process
What is self-monitoring?
Evaluating ongoing performance relative to the standard
Periodically noting qualities of target behaviour
Identify discrepancies between current state and desired state
Effective, especially when public/recorded
What is the behaviour-intention gap?
Intentional control of behaviour is limited, thus people can have intentions but not act upon them (there are many other influences on our behaviour)
'A medium-to-large change in intention —> small-to-medium change in behaviour’
Implementation intentions can help translating intentions into behaviour (If X, then Y), effective because:
Increased activation of specified cue
Automatic activation of specified response
Libertarian Paternalism (nudging)
The idea that it is both possible and legitimate for private and public institutions to affect behavior while also respecting freedom of choice
What are examples of nudges?
Salience (opvallendheid): fruit bij de kassa neerleggen
Social proof: 85% of guests in this room reuse their towels
Defaults
What are the pros and cons of nudges?
+no need for cognitive resources/strong motivation/highly acceptable
-one shot localized intervention: very specific and target one choice
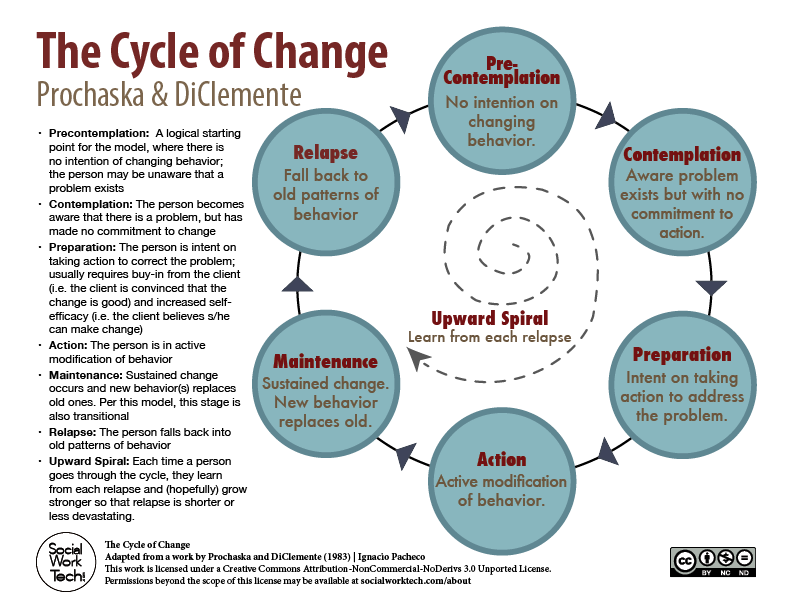
What is the Model of Stage of Change (Prochanska, DiClemente, Norcross)
Lapses= little slipups
Relapses= completely falling back into old behaviour
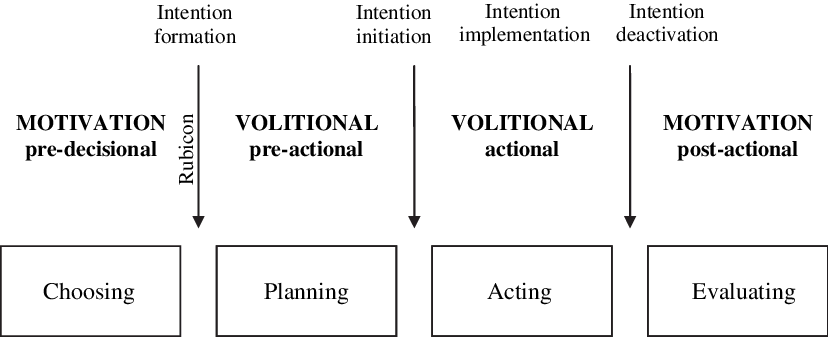
What is the Rubicon Model of Action Phases? (Heckhausen & Gollwitser)
What development was there in Work Health Psychology?
Safety and quality of products
Top management
Medical risk factors
Health Behaviour
Health wellness programmes
Why Health Promotion at the worksite?
Lifestyles connected with mortality, morbidity, absenteeism, health care corsts, productivity
Worksite specific advantages
Why do organisations introduce Work Health Psychology?
•keep employees healthy
•part of the business culture
•reduces indirect costs of health failure
•moral responsibility towards employees
•in response to employee requests
•desire to project a favorable corporate image
•belief that WHP is an important benefit that improves employee recruitment and retention
•as a means for improving employee morale and job satisfaction
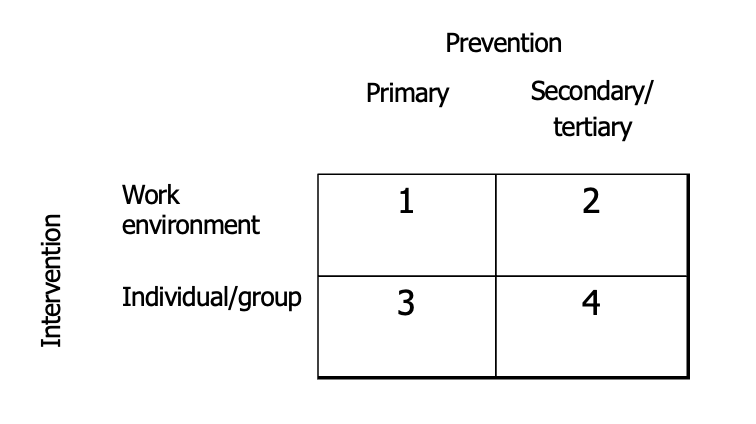
What kind of preventions are there in the workplace?
Prevention | Response type | Orientation | Focus |
Primary | Proactive | Prevention or promotion | All employees and/or the organisation |
Secondary | Pro-active, potentially reactive | Primarily prevention | Employees at risk and/or organizational risk factors |
Tertiary | Reactive | Reduction consequences | Employees with ill health / in need of assistance |
What are advantages as the worksite as a setting for Health Psychology?
•large population adults (also the ‘’difficult to reach’’)
•convenience for target population
•stability of population
•social context
•availability organisational structure
•possibility to intervene at different levels (individual, organisational, environmental)
What are health-wellness programmes?
Focus on employee wellness next to physical health/absence of disease (and positive outcomes)
Work is important determinant of employee health, stress management (individual)
What is the criticism toward individual-focues intervention?
-Often low participation
-Often not attracting the target (stressed) population
-Focus on employees not coping adequately (‘blaming the victim’)
-Avoids employers having to modify any work-related causes of stress
What is the model of Tetrick & Winslow, based on the Job Demands-Resources model?
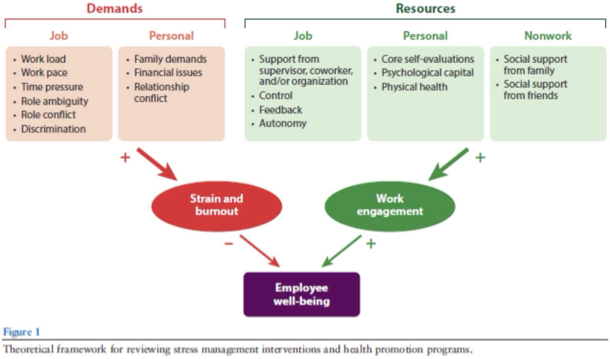
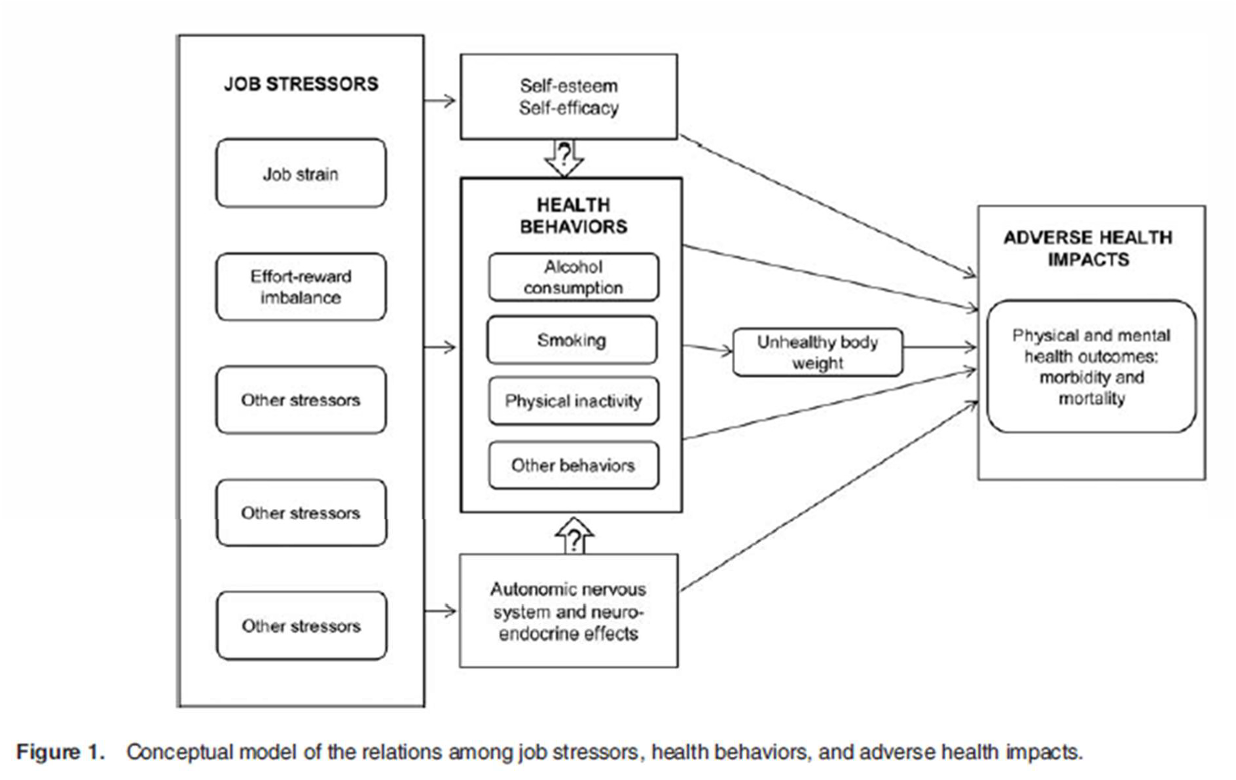
How do job stressors influence physical and mental health? (LaMontagne)
What is the Participative Action Research Program?
involves employees in a cyclic process participating in:
(a)defining issues or problems,
(b)developing methodology and collecting data to inform the problem,
(c)making sense of the data,
(d)defining the interventions,
(e)helping to implement these interventions,
(f)evaluating the results
What is the effectiveness of stress-management programmes (LaMontagne)?
Combining individual + organisational is more effective
What are two important aspects of WHP programs?
Reach/participation rate (important to the employee, match interest, supported by top management, culture integrated within culture, incentives)
Effectiveness in creating behavior change (individual goal setting, social support, low costs/barriers for healthy behaviour, sufficient intensity and duration, environmental cues)
What were the results of the Assessment of Health Risks with Feedback (Goetzel & Pronk)?
Tobaccy use, dietary fat, seat belt use, high blood pressure, cholesterol, high-risk drinkers, absenteeism, physical activity, overall health, health care use —> useful gateway activity for WHP interventions
Insufficient evidence: fruit, BMI, overall phyisical
Stressor
Event with possible threat to the attainment of psychobiological goals
Stress response
Adaptive psychobiological reaction to a stressor
What are the differences between stress and anxiety?
Stress (short-term)
Typically caused by a demanding situation/external trigger
Anxiety (lingering)
Caused by persistent, excessive worries
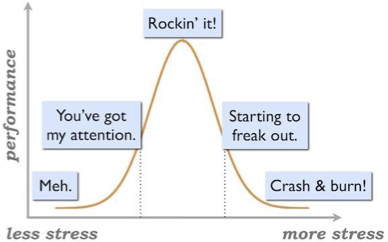
What is the Yekes-Dodson law?
Performance increases with mental arousal (stress) but only up to a point: when an individuals' level of stress is too low or too high, their performance deteriorates
What are positive aspects of stress?
Helps adjusting
Concentration
Avoiding danger
Flexibility
Boosts immunity
Protects DNA
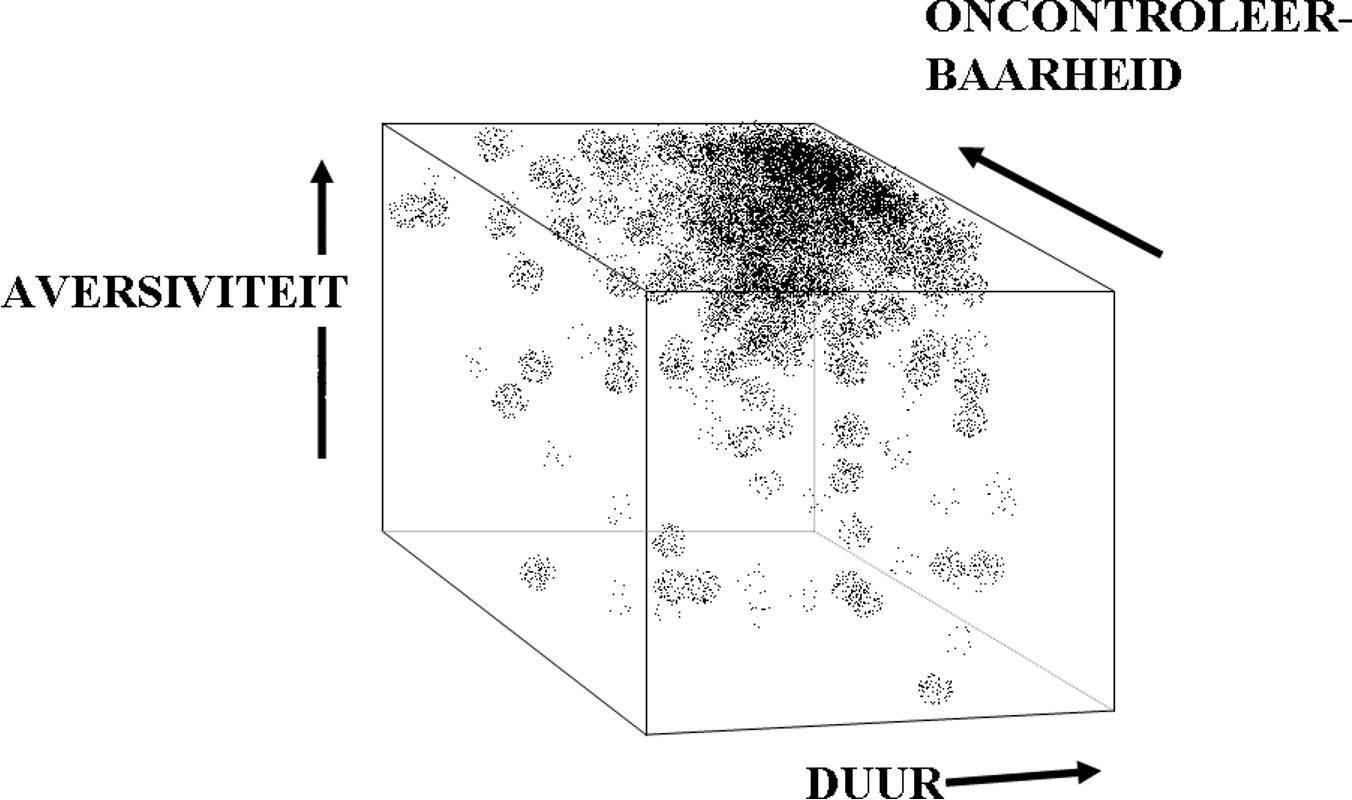
What are the key factors in stress?
Duration
Impact/intensity (adversity)
Predictability/controllability
Why is stress a secondary prevention?
Aims to reduce its harmful effects
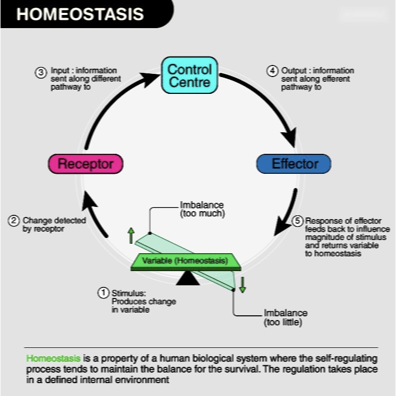
What is homeostasis?
Your body’s tendency to maintain a stable internal environment
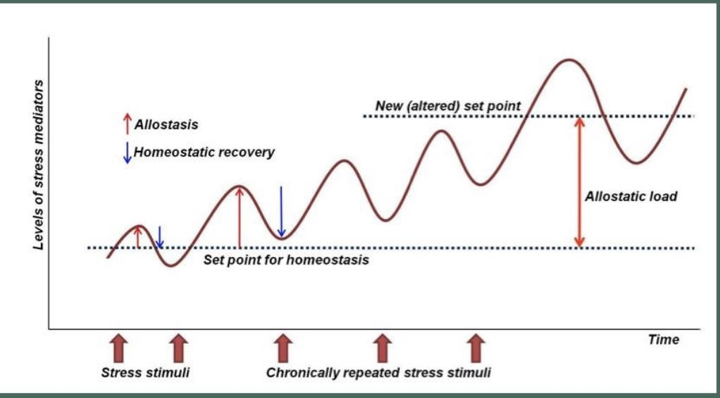
What is the difference between allostasis and allostatic (over)load?
Allostasis: process of achieving homogeneity (stability) through physiological and behavioral adaptation in response to a challenge
Allostatic (over)load: demands exceed energy supplies: kind of balance may be achieved but system needs to work too hard and slowly breaks down
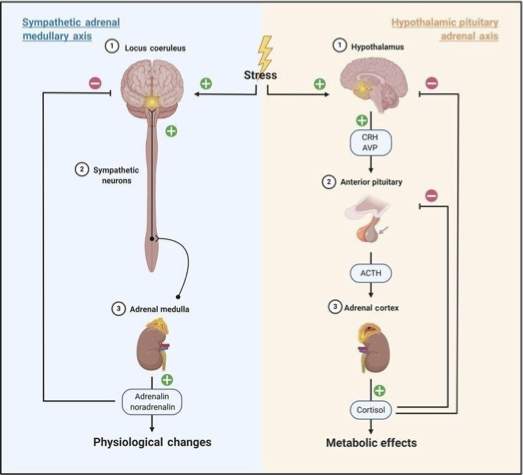
What two important stress systems are there?
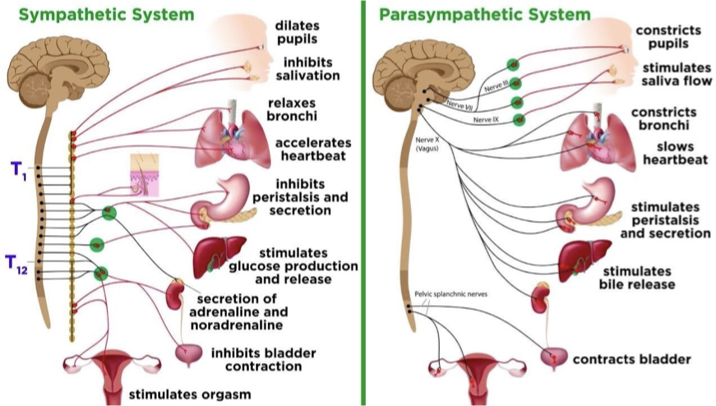
Sympatho-adrenomedulary (SAM) axis: acts via sympathethic (activation) nervous system & adrenal glands
Neurotransmitters: catecholamines (nor)adrenaline —> short-lived arousal
increased heart rate and blood pressure, local constriction of peripheral blood vessels: more blood to muscles, less to viscera (guts): preparation for action!
more glucose in blood: ‘fuel’… preparation for action!
more sweating: ‘cooling’
Hypothalamic Pituitary Adrenal (HPA)
Hormones: glucocorticoids (cortisol) —> longer term arousal
suppressing immune activity and other ‘non-essential’ activity (digestion, growth etc.): save energy (fuel: glucose & simple proteins/fats) to support fight/flight action
buffering against SAM induced tissue damage
suppressing pain (via endorphins): no interference of pain- experience with action
returning to steady state
What are the differences between the sympathetic and the parasympathetic system?
Stress reactivity/recovery
The tendency/capacity to respond to a stressor
Cortisol pros and cons
+regulating immune response
+increased energy and inhibition of inflammation
-decreased energy
-brain damage and cognitive declines (memory and attention)
-reduced ability to adapt
What is psychoneuroimmunology?
Bi-directional relationship between psychological stress and physiological immune responses
What types of stressors are there (related to specific events)?
Transient
Acute time-limiting
Traumatic events
Life events
Repeated
Daily hassles
work-related
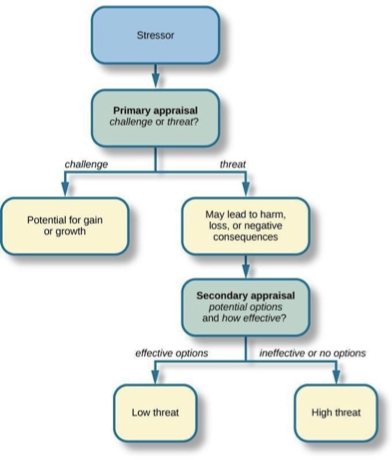
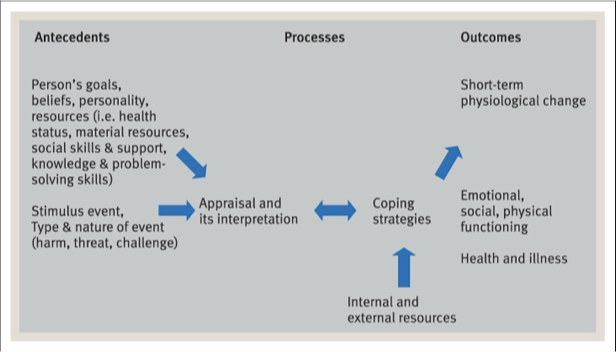
What is the cognitive transactional model of stress (Lazarus)?
Stress is a subjective experience
Cognitive appraisal + thoughts/interpretations
Primary appraisal: perceived demands
Harm-loss: damage that already occured
Threat: future harm/loss
challenge
Secondary appraisal: resources (coping potential)
Stress= mismatch between perceived demands and resources
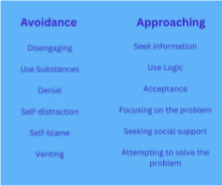
Coping
Anything a person does to reduce the impact of a perceived or actual stressor
Dynamic process involving constellation of cognitions and behaviour that arise
Can operate/alter/reduce negative emotions or target stressor
Concerned by adaptation
Coping style
Trait
Approach/avoid
Coping strategy
Varies according to event/context
Situation-specific coping
Problem-focused coping
Passive coping
Coping taxonomies
Problem-focused/emotion-focused: reduce demands (emotion when control is low)
Approach-oriented/avoidance: attending to the source or distracting yourself
What is the Coping Process (Lazarus)?
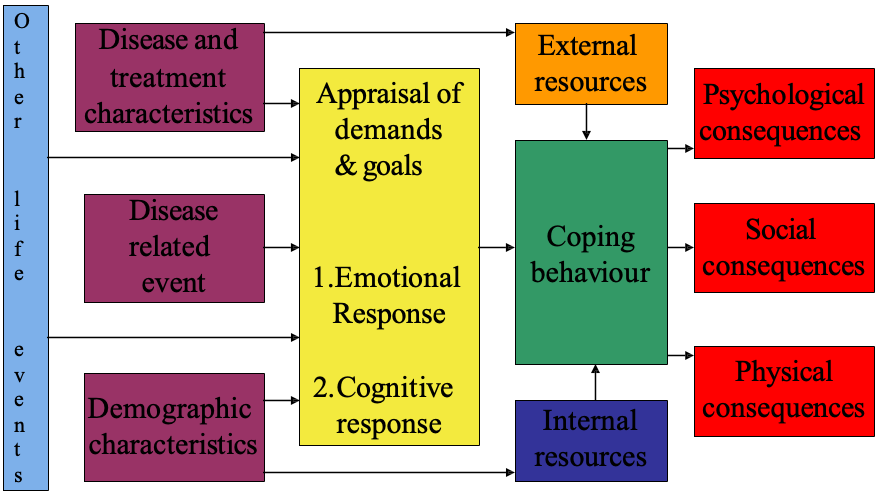
What is the Stress-Coping Model (Maes, Leventhal & De Ridder)
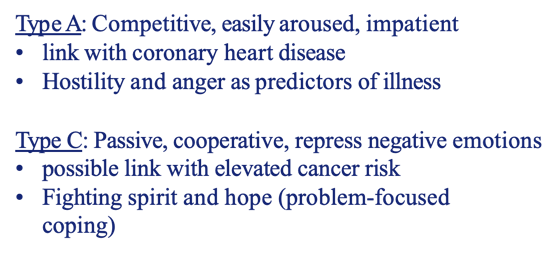
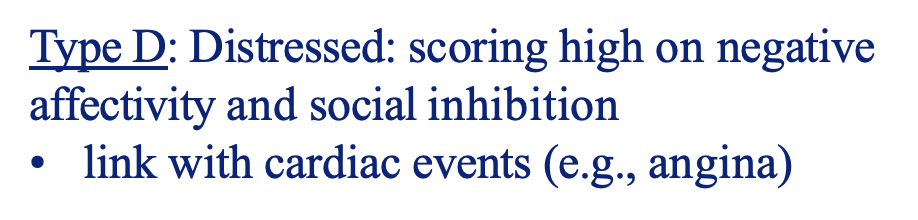
What kind of personalities are there?
What is the difference between worry and rumination?
Worry: anticipation of future events
Rumination: dwelling on past events
—> these are perseverative cognitions (passive, repetitive and self-focused thinking about negative emotional states and implications/consequences of these states)
What is the perceived locus of control?
Appraisal of control over the outcome; distinguish between internal versus external locus of control
What kind of perceived control types are there?
•Behavioral (e.g., breathing techniques)
•Cognitive (e.g., distraction)
•Decisional (e.g., opportunity to choose between options)
•Informational (e.g., opportunity to find out more about stressor)
•Retrospective (e.g., searching for meaning)
What kind of social support is there (Lazarus)?
Instrumental (practical aid)
Emotional
Informational
What are negative moderators of stress?
•Neuroticism
•Negative affectivity
•Social inhibition
•Hostility and anger
•Perseverative cognitions
What are positive moderators of stress?
Social support
Optimism
Hardiness – belief of control, feeling involved and challenged: buffering effect
Self-efficacy - one's belief in one's own ability to complete
tasks and reach goals
Perceived locus of control
Fighting spirit, hope
What is the stress model according to Selye and which phases does it have?
Alarm stage: initial response, increased arousal
Resistance stage: adaptation to the stressor
Exhaustion stage: depletion
Criticism: physiological response can differ depending on type of stressor (specific response)
He defines general adaption syndrome (stress response is innate drive to maintain homeostasis)
What factors contribute to an increased likelihood of perception of symptoms?
Painful or disruptive
Novel (or rare)
Persistent
Pre-existing chronic disease
What is the Symptom Perception Model? (Kolk et al.)
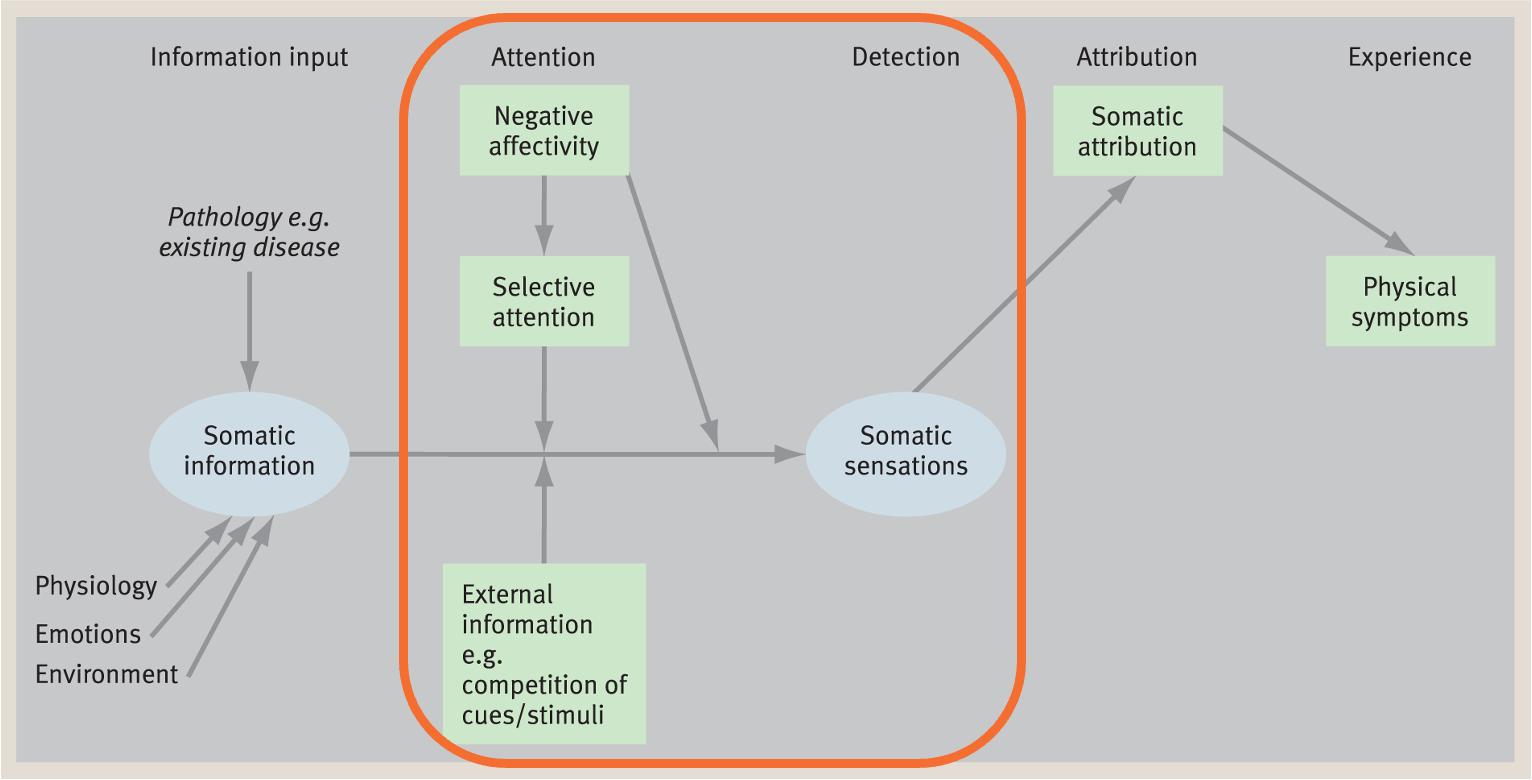
What are factors in Symptom Perception?
Current emotions
Personality traits: neuroticism, negative affectivity
Attention (increased knowledge, distractions)
Social situations
Perceptions of vulnerability
Gender
Coping style
Cognitions
Placebo/nocebo
Favorable / unfavorable treatment effects that cannot be ascribed to mechanisms of treatment itself but due to positive/negative expectation
How are expectations formed?
Instructions
Conditioning
Observation
What are pros and cons of placebos?
+Reduced pain perception
-Reduced trust
-Disappointment
What influences Symptom Interpretation?
Culture
Individual differences
Self identity
Illness experiences
Causal attributions
What is the Common-Sense Model of Illness (Leventhal &Diefenbach)
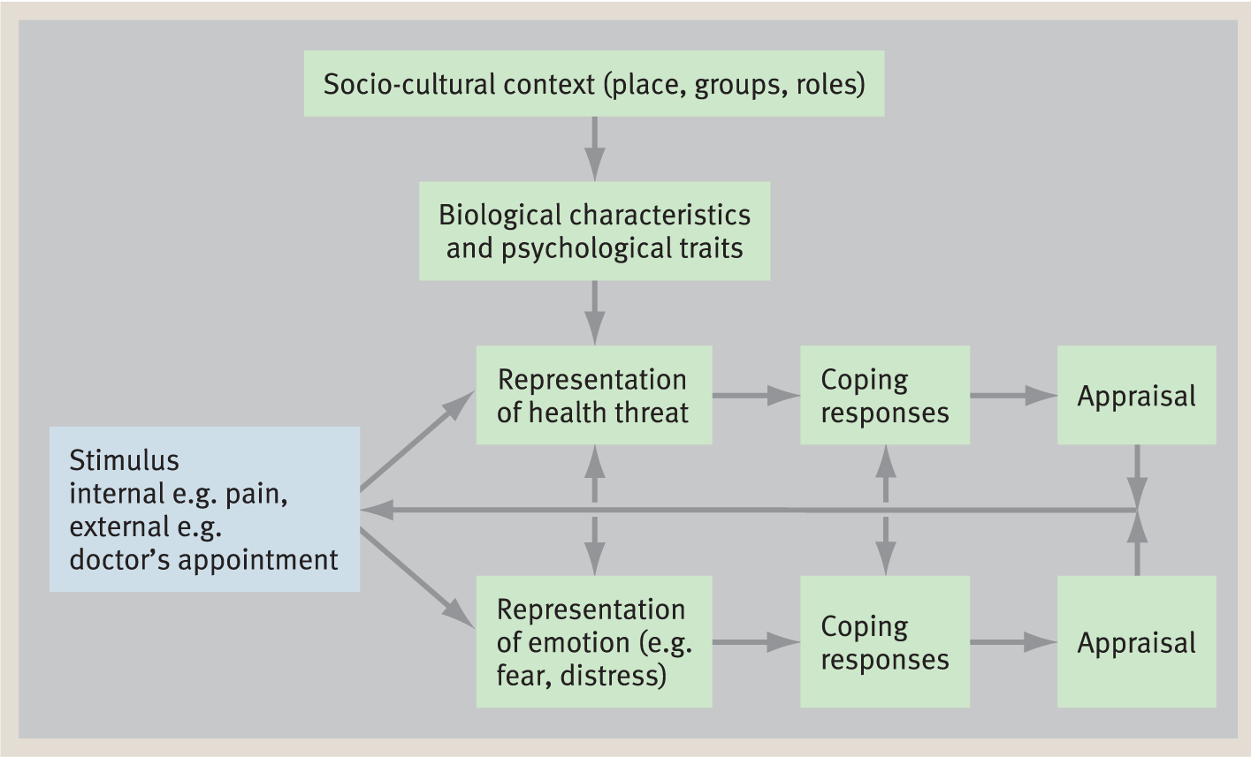
What are the 5 themes in illness representations?
Identity
Consequences
Cause
Timeline
Curability/controllability
Direct effects on seeking treatment, engaging self-care, attitudes towards use brand-specific, return to work, caregiver anxiety, quality of lide
What are reasons for delay in seeking health advice?
Appraisal delay
Illness delay
Utilization/Behavioural delay
Scheduling delay
Treatment delay
What are factors that determine a good medical consultation?
Qualifiers
Shared decision making
Language
Relationship
What 4 steps are involved in Shared Decision-Making?
Choice
Options
Preferences
Decision
Poor adherence predictors
Social factors
Psychological factors
Treatment factors
How to improve adherence during the consultation?
Achieving concordance
Maximising understanding
Maximising memory