Keratoconjunctivitis Sicca = Dry Eye Disease
1/10
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
11 Terms
Dry Eye Disease Overview
keratoconjunctivitis sicca, dry eye syndrome, and dysfunction tear syndrome.
Keratoconjunctivitis sicca is dryness of the conjunctiva and cornea.
Dry Eye Disease and Ocular Surface Disease (OSD)
ocular surface disease which indicates damage to the surface layers of the eye, namely the cornea and conjunctiva.
The most common causes of OSD are:
Dry eye
Blepharitis (inflammation of the eyelids)
Meibomianitis
Severe OSD may precipitate secondary keratitis and conjunctivitis, corneal ulceration and scarring, and permanent vision loss.
TFOS DEWS II Definition: Dry Eye
tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities
is evaporation induced tear hyperosmolarity resulting in ocular surface damage and inflammation.
Key etiologies include tear hyperosmolarity, tear film instability, ocular surface inflammation and damage, and neurosensory abnormalities.
All forms of dry eye disease have an evaporative component.
Classification of Dry Eye Disease (DED)
Two Forms of Dry Eye (non-mutually exclusive = continuum)
Aqueous Deficient Dry Eye (ADDE): reduced tear secretion
decreased tear volume disorder of lacrimal gland function
Sjögren syndrome dry eye (NSDE)
A chronic autoimmune disease characterized by immune cell infiltration of exocrine glands
Evaporative Dry Eye (EDE): excessive tear evaporation
Meibomian gland dysfunction or increased palpebral fissure width (the opening between the eyelids) leads to increased evaporation or an anomaly of tear distribution.
Normal lacrimal function
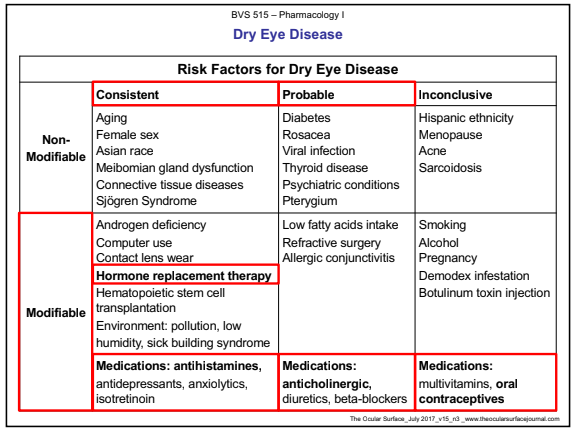
Risk Factors for Dry Eye Disease
1st generation antihistamines (anti-cholinergic)
Oral contraceptives (hormone therapy)
Tear Supplementation: Artificial Tears - General Components
• Preservatives: Prevent the growth of microorganisms.
• Viscosity-Increasing Agents: Prolong contact time by slowing drainage from the eye.
• Demulcents: Water soluble polymers that are used to protect and lubricate the ocular surface.
• Emollients: Fat-based or oil-based products that seek to replicate the lipid layer of the eye.
• Antioxidants: Prevent or delay deterioration by oxygen.
• Wetting Agents: Reduce surface tension, allowing the drug solution to spread across ocular surface.
• Buffers: Maintain ophthalmic products in the pH range of 6 to 8.
• Tonicity Agents: Maintain isotonicity with preocular tear film (0.6%-1.8%).
Tear Supplementation: Artificial Tears -- Preservatives
Three main categories of preservatives in ophthalmic preparations
– Chemical
– Oxidizing agents (less toxic than chemical)
– Ionic buffered (less toxic than chemical)
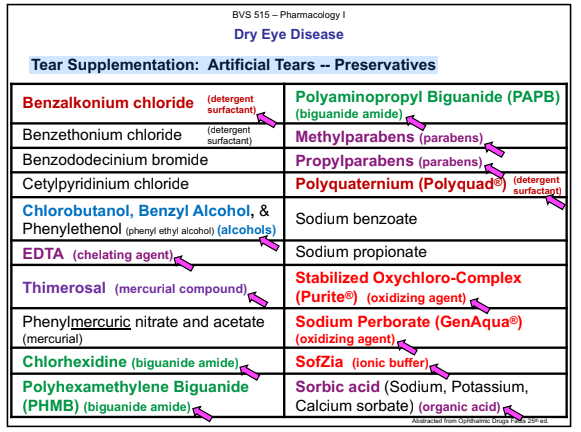
Tear Supplementation: Artificial Tears -- Chemical Preservatives
Detergents:
Benzalkonium Chloride (BAK, BZAK) , Benzethonium chloride, Polyquaternium-1 (Polyquad).
MOA: Disruption of bacterial cell membranes (bactericidal).
Benzalkonium Chloride toxic to corneal epithelium and tear film.
Polyquaternium-1 (Polyquad®) is less toxic
Mercurial derivatives: thimerosal,
MOA: Inhibits microbial metabolism.
Thimerosal is responsible for contact sensitivity
Biguanides or Amides: : polyhexamethylene biguanide (PHMB), chlorhexidine, polyaminopropyl biguanide (PAPB).
MOA: Disruption of bacterial cell membranes (bactericidal).
Known for activity against Acanthamoeba
Used in multipurpose contact lens solutions.
Alcohols: chlorobutanol (detergent), benzyl alcohol, phenylethenol
MOA: Disruption of bacterial cell membranes (bactericidal).
Benzyl alcohol is responsible for hypersensitivity reactions.
Miscellaneous:
Sorbic Acid
MOA: Is an antioxidant.
An organic acid
Methylparaben and Propylparaben (Parabens esters as a class)
MOA: Inhibits microbial metabolism.
Responsible for contact dermatitis (sensitivity) allergic reactions
Disodium EDTA (ethylenediaminetetraacetic acid)
MOA: Has antioxidant properties and is also chelating agent that binds divalent cations (unique action) which disrupts cell membranes.
Responsible for contact dermatitis.
Sodium bisulfite and metabisulfite (“sulfites”)
MOA: Is an antioxidant
Tear Supplementation: Artificial Tears -- Oxidizing Preservatives
Stabilized Oxychloro-Complex (Purite®) and Sodium Perborate (GenAqua®)
MOA: Oxidative preservative systems.
Tear Supplementation: Artificial Tears -- Ionic Buffered Preservatives
SofZia®
MOA: Ionic buffered preservative system.
When exposed to cations in the tear film of the eye, SofZia® breaks up into innate ingredients.
The SofZia® preservative system is used in Travatan Z® (travoprost).
Tear Supplementation: Artificial Tears -- Viscosity-Increasing Agents
Viscosity-Increasing Agents: Prolong contact time by slowing drainage from the eye.
Polymers are used in artificial tear solutions or tear substitute solutions as viscosity increasing agents.
The most common viscoelastic or pseudoplastic polymers are:
Polysaccharides/Cellulose Ethers
Vinyl derivatives (water soluble polymers)
Viscoelastic agents exhibit both viscous and elastic characteristics when undergoing deformation (e.g., stretchability, adaptability, ability to change). Viscosity decreases with increasing shear rate (blinking) for greater patient acceptance.