AMI - Lecture 4 - T cell priming in relation to Covid
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
15 Terms
explain the 3 signals by which the DC activates the naive T cell
ag presentation → ag-MHC/TCR
co-stimulation → upregulation by PRR, CD80/86 molecules are upregulated. these bind to CD28. essential for proliferation and survival
cytokines → these determine the effector cell subset
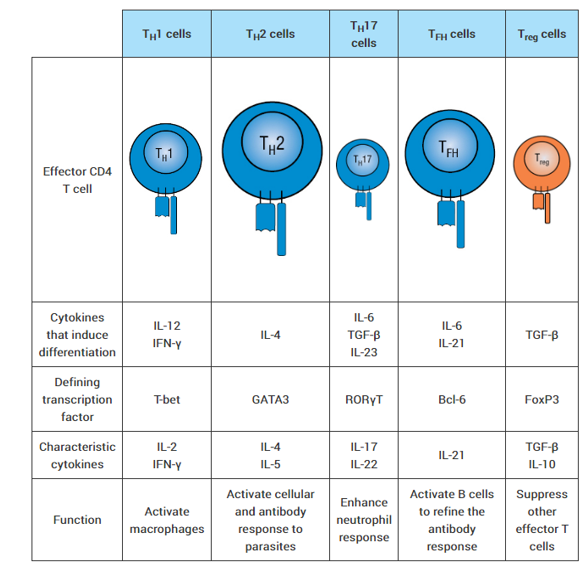
What are the different T cell subsets and which cytokines are involved
Explain T cell exhaustion
happens when there is chronic exposure to ag (viral infection, cancer)
exhausted T cell express high levels of PD1 (programmed cell death protein 1)
PD1 → inhibitory receptor that dampen immune response and T cell activity
T cell exhaustion results in T cells that;
can’t proliferate well
can’t produce cytokines
can’t kill as much
not responsive to cytokines
Solution → immune checkpoint therapy. they block the checkpoints and inhibitory signals
Characteristics of naïve, effector and memory T cells
Naive cells recirculate between lymphoid
organs and have NO effector functions.
Numbers too low to detect.Effector cells migrate to tissues
and have strong/fast effector functions (already differentiated).
Numbers high, can be detected ex vivoMemory cells migrate to lymphoid organs or
tissues and have effector functions
Numbers low, can be detected with sensitive assays
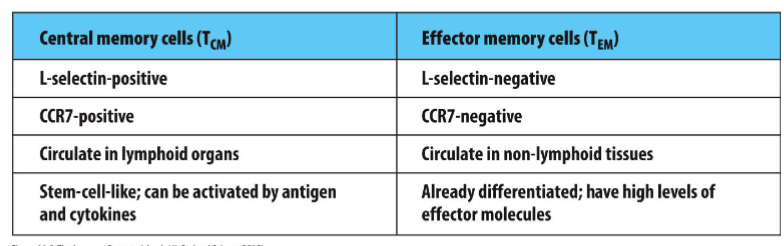
Difference central and effector memory t cells
Tissue resident memory cell
stay in the tissue and provide local protection.
First responder in tissue > local memory responses.
Attraction of other immune cells
Up- and downregulate surface molecule receptors (EXPRESSION OF DIFFERENT RECEPTORS by which they stay in the tissue)
Down: what enters the blood circulation/avoid exit cues.
The presence of Trm has been shown in mice and humans via multiple methods
sew 2 mice together, looked at where the cells went to through blood stream, stayed at the same place.
Explain MHC polymorphism + peptide binding groove
the peptide binding groove is polymorphic for MHC 1+2
6 different for MHC1
6 different for MHC2 → peptide binding groove is bigger here
polymorphism important → recognize wide range of pathogens, defense against evolving pathogens
MHC molecules has revealed peptide motifs for each MHC molecule. The peptide motifs enables prediction of MHC binding peptides from proteins
Every HLA binds multiple peptides.
Different MHC alleles bind different peptide sets
Techniques to measure ag specific T cells; CFSE/CTV
label T cells with dyes that don’t kill the cell > track division with flow cytometry = count cell divisions.
Can combine with markers
Techniques to measure ag specific T cells; elispot assay
sensitive kind of ELISA. intracellular cytokine staining),
ELIspot: coat the well with an antibody against the cytokine. → Then you put the cells on top of it with the antigen. → Only the cells that respond to the antigen will start making Interferon gamma. → The t cells will be washed away and then the ELISA will be done and spots will show the responding cells.
Techniques to measure ag specific T cells; intracellular cytokine assay
stimulate T cells with antigen → the T cells will start to produce cytokines and then a drug is given so the secretion of the cytokines is blocked. → With a detergent the cell can be permeabilized → Then the antibodies inside the cell will be stained. This determines the number of cytokine-producing cells
analyzed by flow cytometry
Activation induced marker assay (AIM)
stain for surface markers!!
the cells that are activated express cytokines and surface markers. Cells are incubated with antigen, then they start to express surface markers. These can be stained.
MHC/ag tetramer staining
quantification of antigen specific T cell responses.
Use the MHC to stain. However, the affinity of TCR and MHC is not as high as antibodies. So tetramer is used;→ The 4 MHC molecules can bind, 4 because the affinity is higher than 1.
Determines the number of antigen, specific T cell
Additional markers by flow cytometry
Quantification directly ex vivo
No culture necessary
Peptide needs to be identified
Works best for MHC-I
Why is covid more serious than normal endemic virus
have spike proteins, are critical to enter host cells
have nucleocapsids (surround + protects viral RNA)
infect respiratory cells, binds ace2 receptors
Explain the persistence of covid in B ant T cells
after 6-8 months following cells still persistent;
memory B and plasma cells → low levels if ab response = secretion
memory B cells + ab are used to target the spike protein + nucleocapsid proteins
CD4/8 T cells are also still in the body after 6-8 months
CD4/8 cells are specific to multiple proteins on virus → spike protein + non structural proteins
Explain the 2 different covid vaccines
cross reactivity → people who have never been infected with Covid still recognize parts of protein. Regions of the virus share homology between common cold and Covid. → may explain why some people get less sick.
RNA (moderna) → very expensive, stored at -18
israel developed this, death rates dropped after 50% was vaccinated
viral vector vaccines (astrazeneca) → modified, non replicating virus, easier to produce and distribute.