HP: Lec 16- Cardiac Cycle, electrical activity of heart & EKG
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
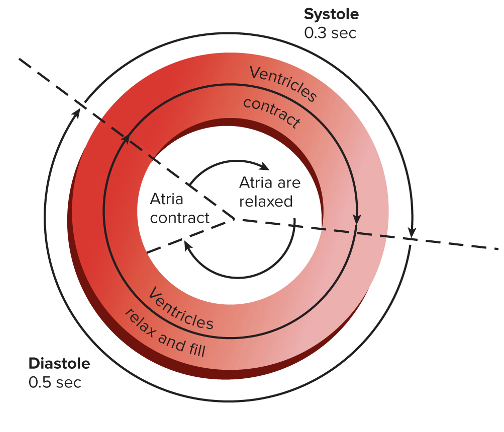
What is the Cardiac Cycle?
repeating pattern of contraction and relaxation of the heart
What does the Cardiac Cycle consist of?
Systole: contraction of Ventricles
Diastole: relaxation of heart muscles (except for the end of diastole when atrium contracts)
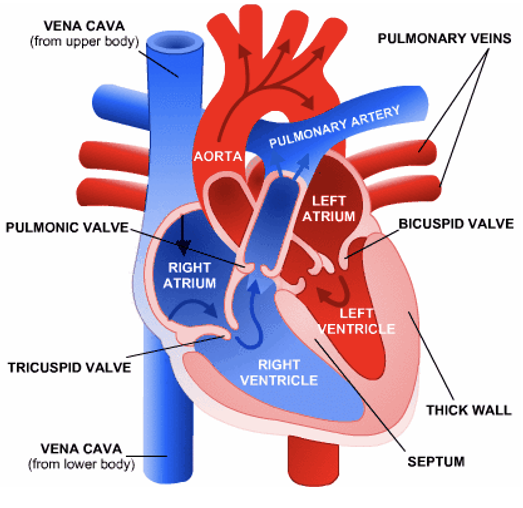
Atrioventricular Valves
where are AV valves located
what does it consist of
where are these factors located
Atrioventricular (AV) valves: located between the atria and the ventricles
a) Tricuspid: between RIGHT atrium & ventricle
b) Bicuspid or mitral: between LEFT atrium & ventricle
c) Papillary Muscles & Chordae Tendinea: prevent inversion or prolapse of these valves on systole (or ventricular contraction)
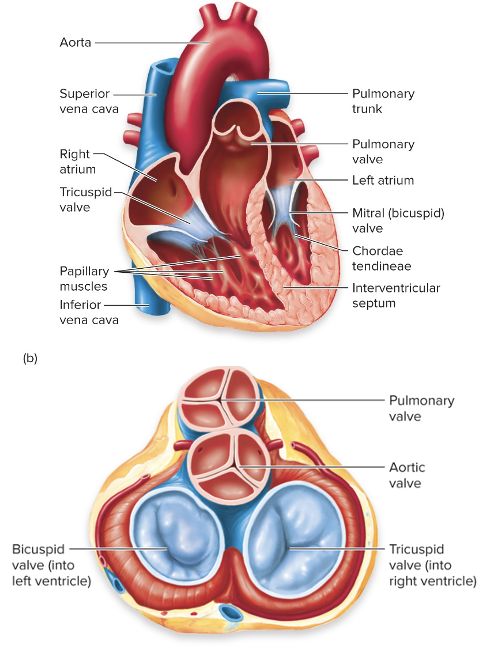
Semilunar Valves
Semilunar Valves: located between the ventricles & arteries leaving the heart
a) Pulmonary: between right ventricle & pulmonary trunk
b) Aortic: between left ventricle & aorta
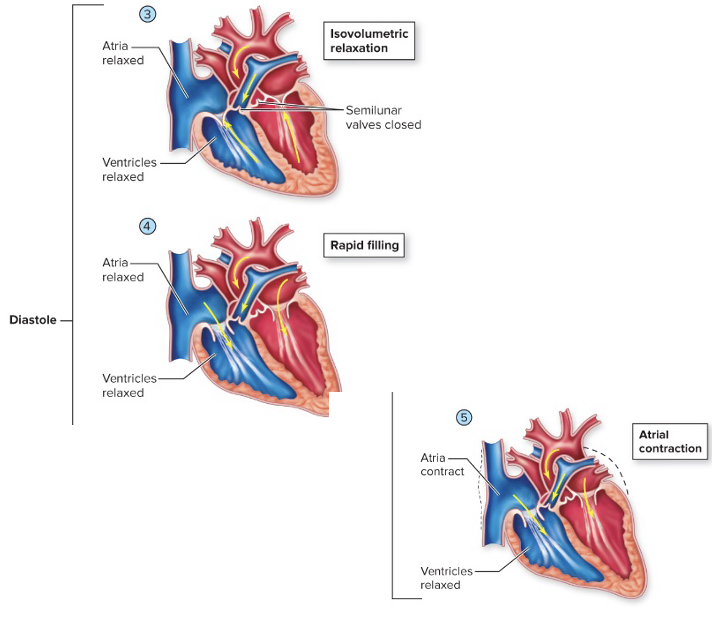
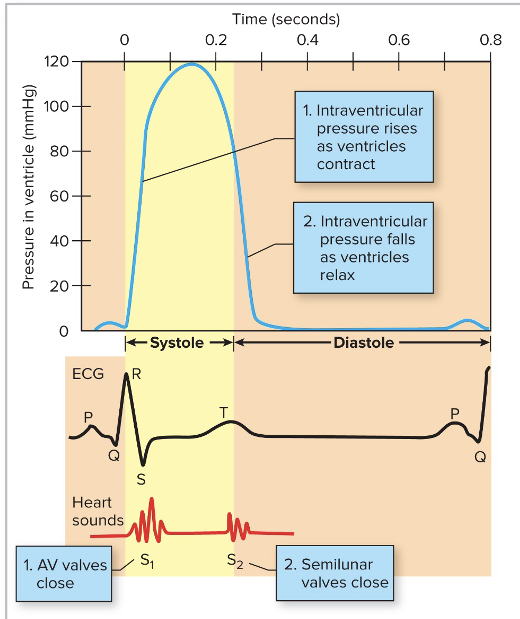
Cardiac Cycle: systole
Ventricles begin contraction, pressure rises, and AV valves close(lub); isovolumetric contraction
Pressure builds, semilunar valves open, and blood is ejected into arteries
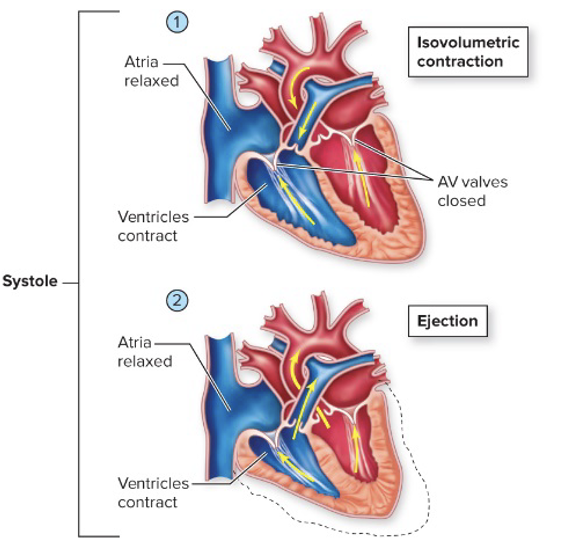
Cardiac cycle: Diastole
Pressure in ventricles falls; semilunar valves close (dub); isovolumetric relaxation
pressure in ventricles falls below that of the atria, and AV valve opens
Atria contracts, sending last of blood to ventricles, ventricles fill
Heart sounds: Lub & Dub
what are they produced by?
what causes them?
Produced by closing valves
Lub: closing of the AV valves; caused by the closure of the atrioventricular valves (mitral and tricuspid) at the beginning of ventricular contraction or systole
Dub: closing of semilunar valves; caused by the closure of the aortic valve & pulmonary valve at the END of ventricular systole
Heart Sounds: What is a Heart Murmur?, what causes it?
a sound made by backflow of blood through either set of valves that cannot close or open properly
many heart murmurs are caused by defective heart valves
Heart Sounds: Mitral Stenosis
Mitral Stenosis: Mitral (bicuspid) valve calcifies and impairs flow between left atrium & ventricle
reduced blood flow through the narrowed valve opening from the left atrium to the left ventricle
the volume of blood bringing oxygen from the lungs is reduced, can make you feel tired and short of breath
the volume & pressure from blood remaining in the left atrium increases which causes the left atrium to enlarge & fluid to build up in the lungs
Intro: Electrical Activity of the Heart
what are cardiac muscle cells interconnected by?
what happens once stimulation is applied?
Cardiac muscle cells are interconnected by gap junctions called intercalated discs
Once stimulation is applied, the impulse flows from cell to cell
Electrical Activity of the Heart
what is automaticity?
what is the sinoatrial node?
Automaticity- automatic nature of the heartbeat
Sinoatrial node (SA node)- “pacemaker”; located in the right atrium
AV node & Purkinje fibers are secondary pacemakers of ectopic pacemakers, normally they are inhibited by the SA node
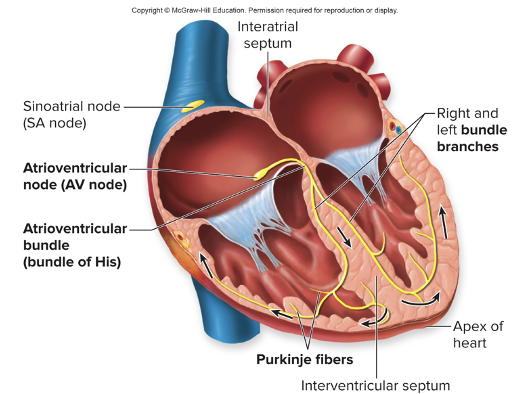
Process: Conduction of electrical activity of the heart
Action potentials spread via gap junctions
SA node to AV node to stimulate atrial contraction
AV node at base of right atrium and bundle of His conduct stimulation to ventricles
in the interventricular septum, the bundle of His, divides into right & left bundle branches
Branch bundles become purkinje fibers, which stimulate ventricular contraction
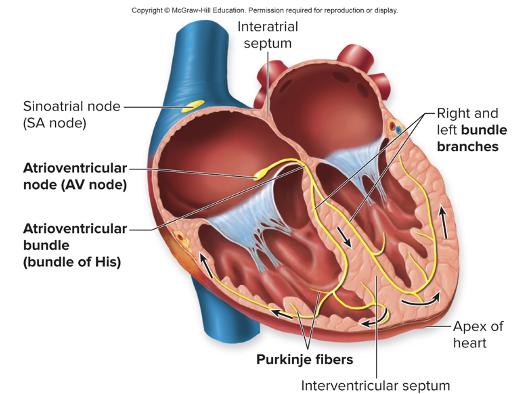
Electrical Activity of the Heart: conduction of impulses, time
how to action potentials spread in the SA node, AV node, and bundle of His?
1) action potentials from the SA spread rapidly
0.8 to 1.0 meter/second
2) at the AV node, things slow down
0.03 to 0.05 meter/sec
this accounts for HALF of the time delay between atrial & ventricular contraction
the speed of conduction picks up in the bundle of His, reaching 5 meter/seconds
Ventricles contract 0.1 to 0.2 second after atria
Dont get confused between what the action potentials in the Cardiac uscle cells of the SA node and the rest of the cardiac muscle cells
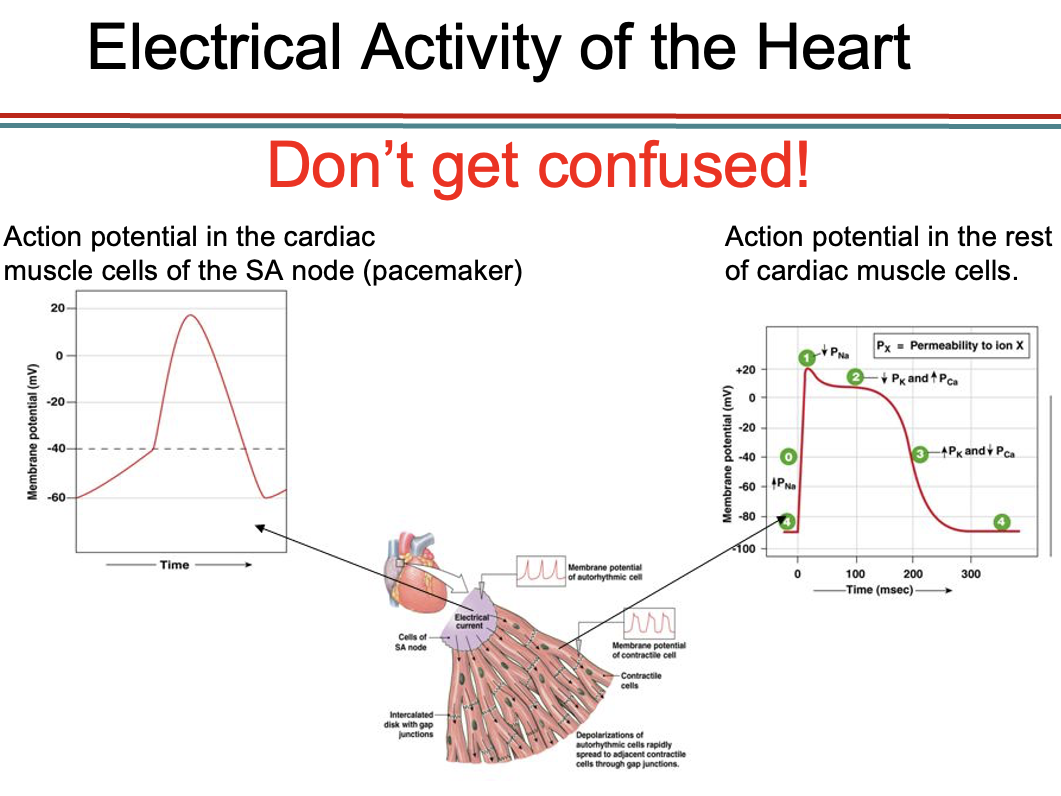
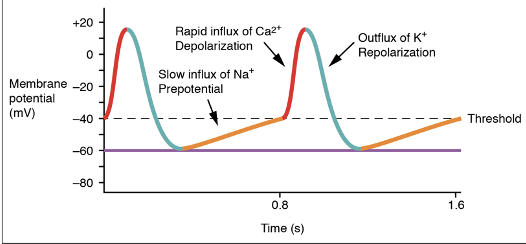
Pacemaker potential: action potential in SA node
a slow, spontaneous depolarization; also called diastolic depolarization- between heartbeats, triggered by hyperpolarization (via HCN channels- hyperpolarization- activated cyclic nucleotide-gated channel
small conductance, small driving force, mixed ion selectivity Na+ and K+
At -40mV, voltage gated Ca2+ channels open, triggering action potential and contraction (within the pacemaker cardiac cells)
Repolarization occurs with the opening of voltage-gated K+ channels
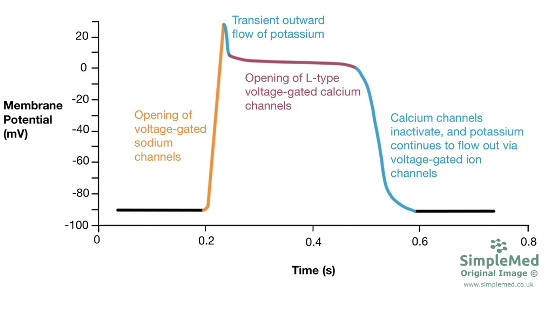
Process: Action Potential in the rest of the muscle cardiac cells
Non-pacemaker cardiac muscle cells have a resting potential of -85mV
they are depolarized to threshold (-70mV) by action potentials from the SA node
voltage-gated Na+ channels (fast Na+) open, and membrane potential plateau at -15mV for 200 to 300 msec
due to balance between slow influx of Ca2+ and efflux of K+
more K+ are opened, and repolarization occurs
long plateau prevents summation and tetanus
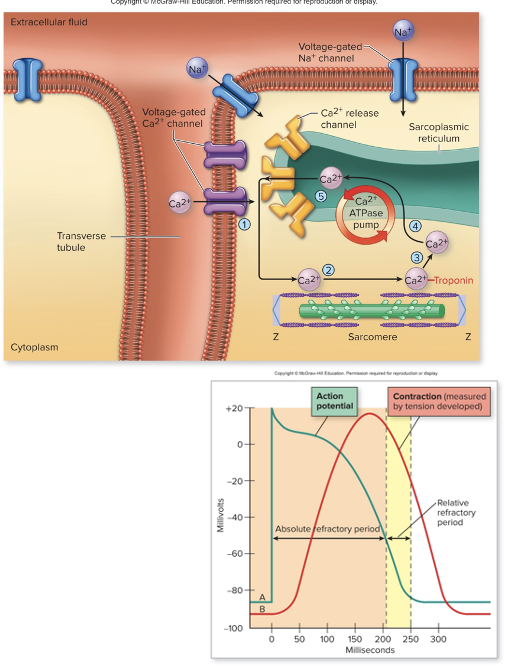
Process: Excitation-Contraction coupling in cardiac muscle cells
the wave of depolarization spreads along the sarcolemma and T-tubule
voltage-gated Ca2+ channels open: Ca2+ enters the cardiac cell, this Ca2+ influx only counts for about 10% of the Ca2+ needed for contraction
this influx of extracellular Ca2+ is detected by RyR2 (ryanodine) receptors on the SR; this stimulates the opening of Ca2+ release channel on the SR and more calcium will flow in the cytoplasm
this mechanism is called calcium-induced calcium release (CaInd-CaRel)
The resulting rise in intracellular Ca2+ concentration (for the most part from the SR via the CaInd-CaRel) activates the contractile machinery
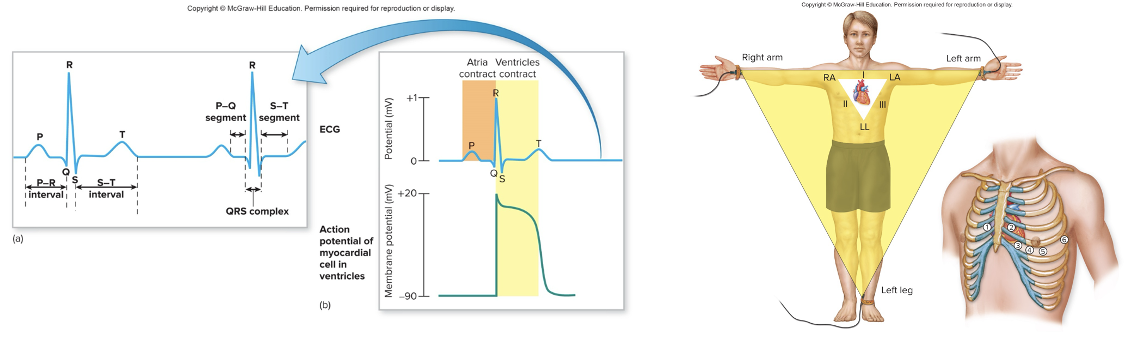
Electrocardiogram (ECG or EKG)
what does the electrocardiograph do?
what does it NOT record?
what does it record?
when do electrical potential differences arise?
the electrocardiograph records the electrical activity of the heart by picking up the movement of charged ions in body tissues in response to this activity
does not record action potentials, but it does record results from waves of depolarization
does not record contraction or relaxation, but it does record the electrical events leading to contraction & relaxation
electrical potential differences arise as the electrical impulse travels through the heart
since the entire human body acts as an electrical conductor, these electrical impulses are conducted all the way to the skin where they can be detected by two or more electrodes
EKG image
Electrodes & Leads
an electrode: is a conductive pad that is attached to the skin and enables recording of the electrical current
an ECG lead is a graphical description of the electrical activity of the heart, and it is created analyzing several electrodes
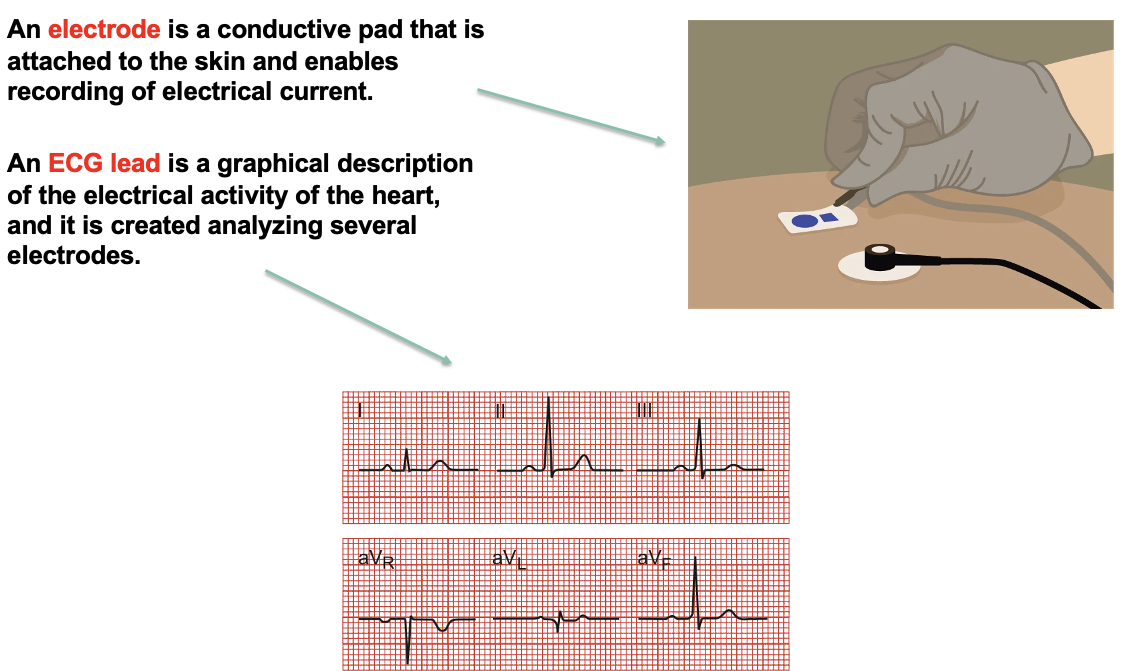
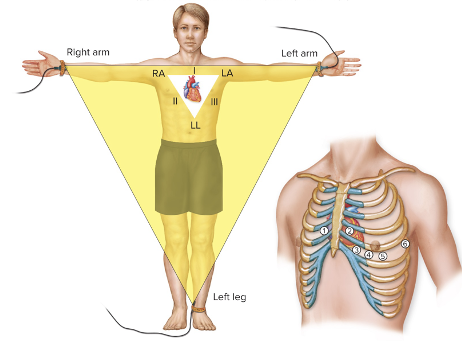
Electrocardiograph
electrocardiograph (normally 12 leads from the combination of 12 electrodes)
two types of leads:
Bipolar Limb Leads
Unipolar Leads
Bipolar Limb Leads
Bipolar limb leads: record voltage between electrodes placed on wrists and legs
Lead I: between right arm and right leg
Lead II: between right arm and left leg
Lead III: between left arm and left leg
Unipolar Leads
Unipolar Leads: record voltage between a single electrode on the body and one built into the machine (ground)
Limb leads go on the right arm (AVR). left arm (AVL), and left leg (AVF)
there are six chest leads
What is an electrocardiogram made up of?
waves
segments
intervals
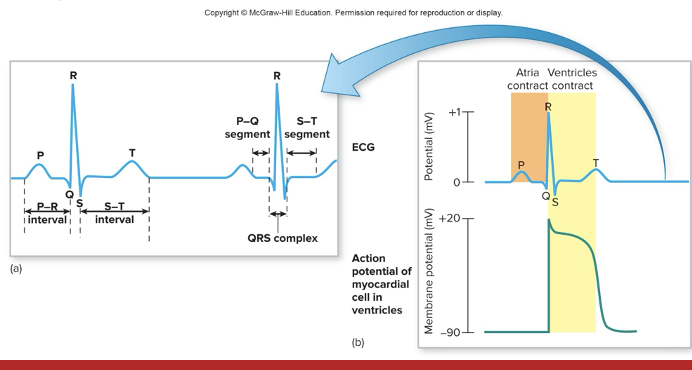
Segments in an EKG
the region between two waves
when analyzing segments, we talk about morphology: elevation or progression of segments
Intervals in an EKG
duration of time that includes one segment and one or more waves
when analyzing duration, we talk about time (duration) and so we cannot talk about the morphology or depression or elevation of an interval
Electrocardiogram: Wave, segments, and intervals order
P wave: atrial depolarization
P-R interval: electrical activity leading to atrial systole
QRS wave: ventricular depolarization
S-T segment: plateau phase, electrical activity ventricular systole
T-wave: ventricular repolarization
ECG Graph
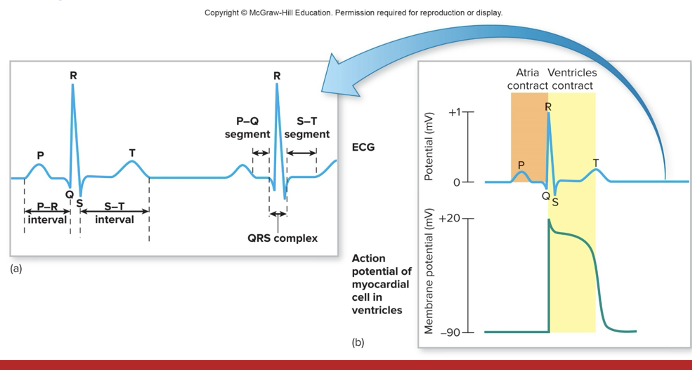
ECG and Heart Sounds
“Lub” occurs after the QRS wave as the AV valves close
“Dub” occurs at the beginning of the T wave as the SL valves close
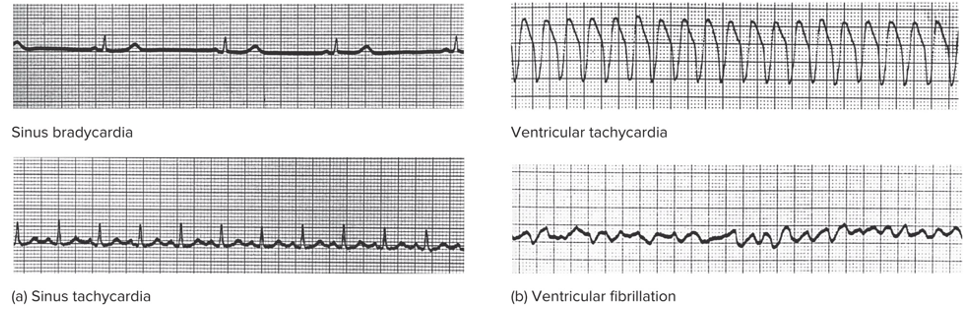
Heart Arrhythmias Detected by ECG (3 Types)
Abnormal Heart Rhythms
Bradycardia: slow heart rate, below 60 bpm
Trachycardia: fast heart rate, above 100bpm
this heart rhythm can be considered normal if the person is highly active, but not at rest
abnormal tachycardia can occur due to drugs or fast ectopic pacemakers
Ventricular tachycardia: occurs when pacemakers in the ventricles make them contract out of synch with the atria
this condition is very dangerous and can lead to ventricular fibrillation
Abnormal heart rythms image
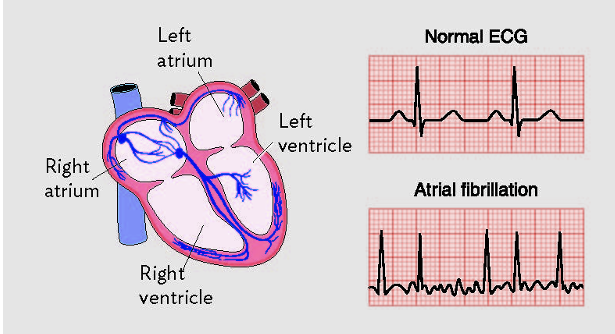
Heart Arrhythmias detected by ECG: Flutter & Fibrillation
Flutter: extremely fast (200 to 300bpm) but coordinated contractions
Fibrillation: uncoordinated pumping between the atria and ventricles
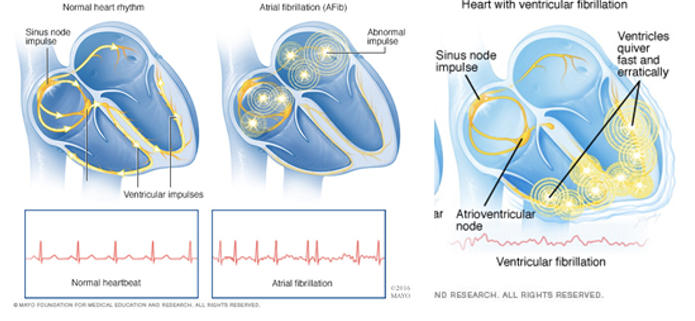
Heart Arrhythmias detected by ECG: Atrial Fibrillation
what can is it caused by?
what happens to the atrial muscles?
how is the AV node affected?
cardiac output?
increased risk of what?
Atrial fibrillation is the most common type of tachycardia
can result from atrial flutter
atrial muscles cannot effectively contract
AV node can’t keep pace with speed of atrial contractions but some stimulation is passed on
only reduced cardiac output by 15%
associated with increased risk of thrombi, stroke, and heart failure
Heart Arrhythmias detected by ECG: Ventricular Fibrillation
what happens when a person experiences ventricular fibrillation
what is it caused by
what does it prevent
ventricles cant pump blood, and victim dies without CPR and/or electrical defibrillation to reset the heart rhythm
caused by circus rhythms: continuous cycling of electrical waves
prevents the refractory period
sudden death progresses from ventricular tachycardia, through ventricular fibrillation, ending straight-line ECG
Ventricular Fibrillation image