structure and function of the colon
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
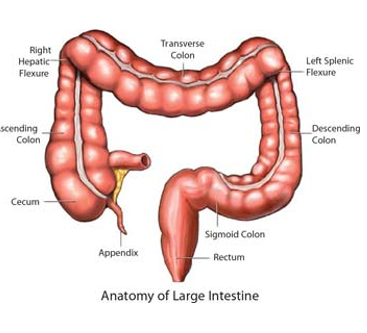
structure of the large intestine
approx. 1.5m long
arranged into haustra which gives the colon its segmented appearance
comprise of the caecum, colon (ascending, transverse, descending), rectum, anal canal
functions: absorb remaining nutrients, absorb water, store and eliminate stool
organization of the colonic mucosa
colonic epithelial cells arise from stem cells within the crypt
transporting enterocytes
goblet cells
enteroendocrine cells
Paneth cells - less numerous than in the SI.
Lamina propria contains nerves and immune cells that regulate epithelial function
Peyer patches are less numerous than in the small intestine
colonic mucosa functions
absorption and secretion
form a barrier
communication with bacteria
colonic enteroendocrine cells
EEC population of the large bowel in generally less diverse than in the small intestine
I cells, S cells, G cells, M cells are absent
enteroendocrine cells - enterochromaffin cells
largest population of EEC cells in the colon
store and release 5-HT (serotonin)
primarily function as sensors of the luminal content
are activated by stretch and nutrients as a food bolus moves through the lumen
released 5-HT stimulates motility and increases local fluid secretion
not to be confused with enterochromaffin-like cells (ECL) in the stomach
enteroendocrine cells - L cells
sense nutrients (e.g. glucose) in the lumen
release glucagon-like peptide 1 (GLP-1)
GLP-1 stimulates insulin secretion from the pancreas
GLP-1 also sends satiety signals to the brain
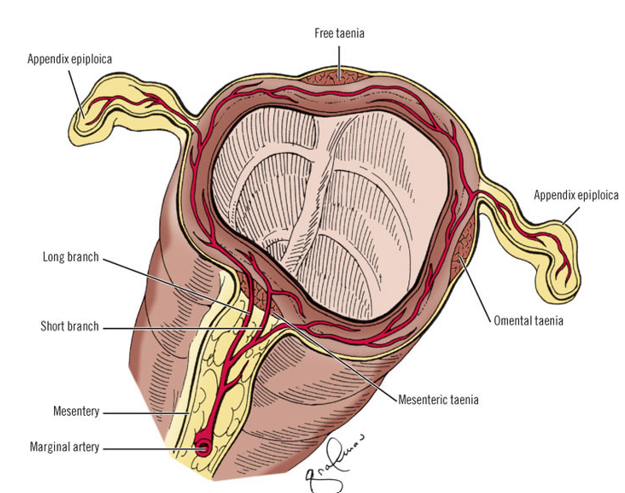
organization of the colonic muscle
colonic muscularis consist of an inner circular layer and outer longitudinal layer of smooth muscle
However, the longitudinal layer is organized into 3 discontinuous longitudinal bands, known as taeniae coli (bands of the colon)
the bands of the taeniae coli are lightly shorter than the underlying circular layer causing the intestinal wall to bunch up into its haustral appearance
types of colonic motility
haustral movements
slow segmenting movements occurring every 25 mins
serve to mix/churn the contents and increase exposure to the epithelium
Peristalsis
propels the bolus forward towards the sigmoid colon and rectum
occurs slowly in the large intestine to allow maximal absorption
mass movements
specialized peristaltic contraction occurring only in the colon
occur 3-4 times a day (after meals)
clears the colon by forcing material towards the rectum
can cause rectal distension and trigger the defecation reflex
gastrolienal and gastrocolic reflexes
before food arrives into the large intestine, it has been readied
presence of food in the stomach induces neural (cholinergic) and hormonal (gastrin and CCK) stimuli that induce
Gastrolienal reflex
peristalsis of the terminal ileum
relaxation of the ileocecal valve
Gastrocolic reflex
mass movement along the colon
induces the urge to defecate soon after a meal
serve to prepare the lower intestine for the arrival of a new meal
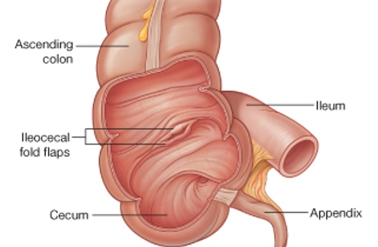
Ileocecal junction
when food reaches the end of the ileum, it enters the large intestine through the ileocecal valve
peristaltic contraction of terminal ileum forces chyme through the valve into the caecum
contraction of the caecum causes the ileocecal valve to close - prevents reflux of colonic contents into ileum
approx. 2L of material pass into caecum/day
at this point the chyme contains mostly water, indigestible food particles (fiber), and bile acids
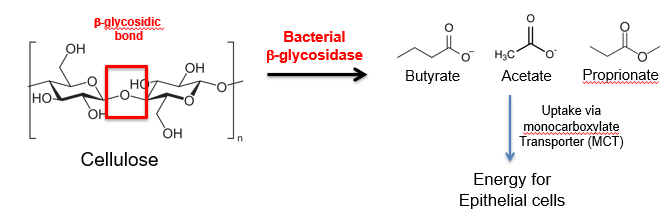
bacteria and digestion - fiber
dietary fiber cannot be metabolized by digestive enzymes
fiber can be fermented by gut bacteria to short chain fatty acids (SCFAs) e.g. acetate, propionate, butyrate
SCFAs are not found at high concentrations in the caecum (70-140mM) and decrease along the colon - are primary determinants of pH along the colon
Enter epithelial cells by active and passive transport and are used as the primary source of fuel for epithelial cells (60-70%)
bacteria and digestion - vitamins
vitamins are organic compounds required of life - must be taken in the diet because humans do synthesize enough
some vitamins are produced through bacterial metabolism in the large intestine
vitamin K - required for blood coagulation and bone metabolism. deficiencies include bleeding disorders, osteoporosis
Vitamin B12 (cobalamin) - required for hematopoiesis and healthy nerves. deficiencies cause anemia and damage to nervous system (fatigue, depression, memory loss)
vitamin B-7 (biotin) - required for cell growth, production of fatty acids an fat/amino acid metabolism,. Deficiencies cause neurological symptoms, hair loss, conjunctivitis and dermatitis.
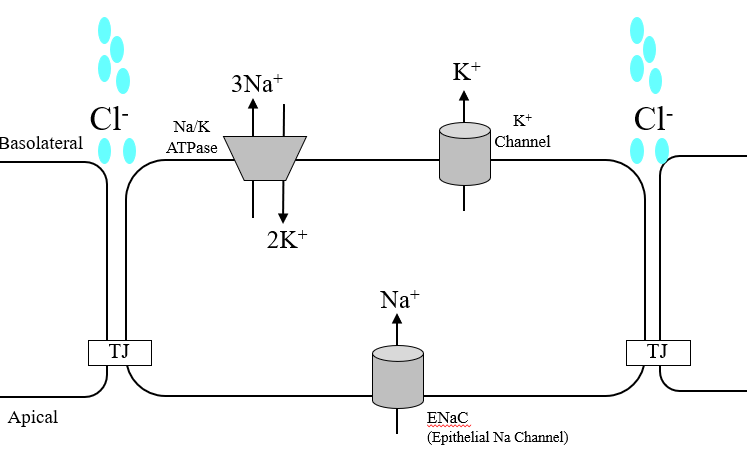
colonic absorption - water
water movement in the intestine occurs along osmotic gradients
driven by electrogenic Na+ absorption
the rectum
final segment of the intestinal tract (15cm) from the end of the sigmoid colon to the anal canal
mucosa largely resembles the colon, but the crypts and lined almost entirely with goblet cells.
function: to temporarily store feces
is normally empty but fills up when a mass movement pushes stool from the sigmoid colon
defecation reflex
defecation involves both involuntary and voluntary reflexes
Peristalsis and mass movement force feces into the rectum, triggering stretch receptors
stretch receptors activate a spinal reflex that stimulates peristalsis and relaxes the internal anal sphincter while contracting the external sphincter
increased pressure in the rectum sends a signal to the brain and we feel the urge to defecate
defecation reflex - delay & defecation
if the urge is not acted on, continued voluntary contraction of the external sphincter and high pressure triggers reverse peristalsis - feces are returned to the sigmoid colon. More water is absorbed to decrease fecal volume until the next mass movement triggers the reflex again
if a voluntary signal volume is sent back along the pudendal nerve, the external anal sphincter relaxes, the rectum contracts, and material exits through the anal canal
Anal canal has stratified squamous epithelium to pretect against abrasion.
feces - composition
70% water and 30% solid
30% of the solid matter consists of bacteria
30% consists of indigestible food matter
10-20% is cholesterol and other fats
10-20% is inorganic substances (e.g. calcium phosphate and iron phosphate)
2-3% protein
cell debris shed from the mucosa (epithelial cells and leukocytes)
bile components (e.g. bile acids; bilirubin)
diarrhea
an illness that causes you to pass waste from your body very frequently an in liquid rather than a solid form
=> 3 loose or liquid stools per day for 3 days
classified as acute (<14 days) or chronic (>14days)
constipation
the condition of being unable to easily pass waster from your body
=< 3 bowel movements a week
associated with hard lumpy stools and straining
causes of diarrhea
diarrhea occurs when there is too much fluid in the stool.
amount of fluid depends on rate of fluid absorption vs. rate of secretion
diarrhea occurs when too little absorption or too much secretion or increased peristalsis
treatment of diarrhea
ensure hydration and use medication if necessary:
anti-motility agents e.g. loperamide
antimicrobials e.g. rifaxamin
anti-inflammatory drugs
alternative medicines e.g. charcoal, probiotics
constipation symptoms
< 3 stools/week
hard/dry, small stools
abdominal pain/swelling
bight blood on the stool
hemorrhoids
long term constipation symptoms
affects quality of life - stress, diminishes overall sense of wellbeing
leads to cardiovascular, endocrine and immune problems
in elderly people, chronic damage to the mucosal membrane can lead to development of colon/rectal cancer
causes of constipation
usually occurs when peristaltic action is diminished - stool mooves too slowly and becomes hard and dry
diet: insufficient intake of dietary fiber, insufficient H2O intake
medication: diuretics, opioids
obstructions: strictures, tumors
neurological/hormonal conditions: hypothyroidism, multiple sclerosis, parkinson’s disease
psychosomatic constipation: based on anxiety e.g. new job, exams
IBS: 1/3 IBS patients have IBS-C
treatment of constipation
change of lifestyle - change of diet ( more fiber), increased levels of exercise
laxatives - bulk forming (fiber), osmotic (lactulose), stimulant (senna, Psyllium)
drug therapy - amitiza (softens stool by stimulating fluid secretion)
role of the colon in drug absorption
the colon does not have the capacity of the small intestine for drug absorption
is equally as permeable to lipophilic drugs in ascending colon
also has several carrier-mediated transport systems that can act as targets for hydrophilic drugs
both locally-targeted (ulcerative colitis) and systemic (protein and peptidase drugs) delivery of drugs can be achieved
colonic delivery strategies
prodrugs: inactive drugs are metabolized by bacteria in the colon
colon specific biodegradable delivery systems - encapsulate a drug in polymer matrices which can only be degraded be bacterial enzymes
times release systems
pH sensitive coatings - polymers breaks down basic Ph in ileum, thus providing targeted drug delivery to the colon
factors affecting colonic drug absorption
pH: basic drugs are better absorbed from the distal than proximal colon
viscosity of contents: only the ascending colon is fluid enough for diffusion of drugs to occur
first pass effect: drugs absorbed from the colon will enter the EHC and pass through the liver
transit time: slow transit gives more time for absorption
bacterial metabolism: can increase or decrease metabolism
rectal route of delivery advantages
relatively large dosage form can be accommodated
safe and convenient for elderly and young patients
drug dilution is minimized as the residual fluid volume is low
relatively empty
degradative enzymes are practically absent
first pass elimination by the liver is avoided
useful if there is nausea, vomiting in unconscious patients, if there is upper GI disease, if there is an unpleasant taste