Abnormal ocular conditions- L13 and L14 Part 4 Peripheral Retina Disorders Likely to Affect Vision
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
Peripheral retinal conditions that are
likely to affect vision
Retinoschisis
• Degenerative
• Juvenile
• Lattice degeneration
• Snail-track degeneration
• Cystic Tuft
• Atrophic retinal hole (retinal break)
• Operculated retinal hole (retinal break)
• Retinal tears
• Rhegmatogenous retinal detachment
• Retinitis Pigmentosa
• Albinism
• Malignant melanoma
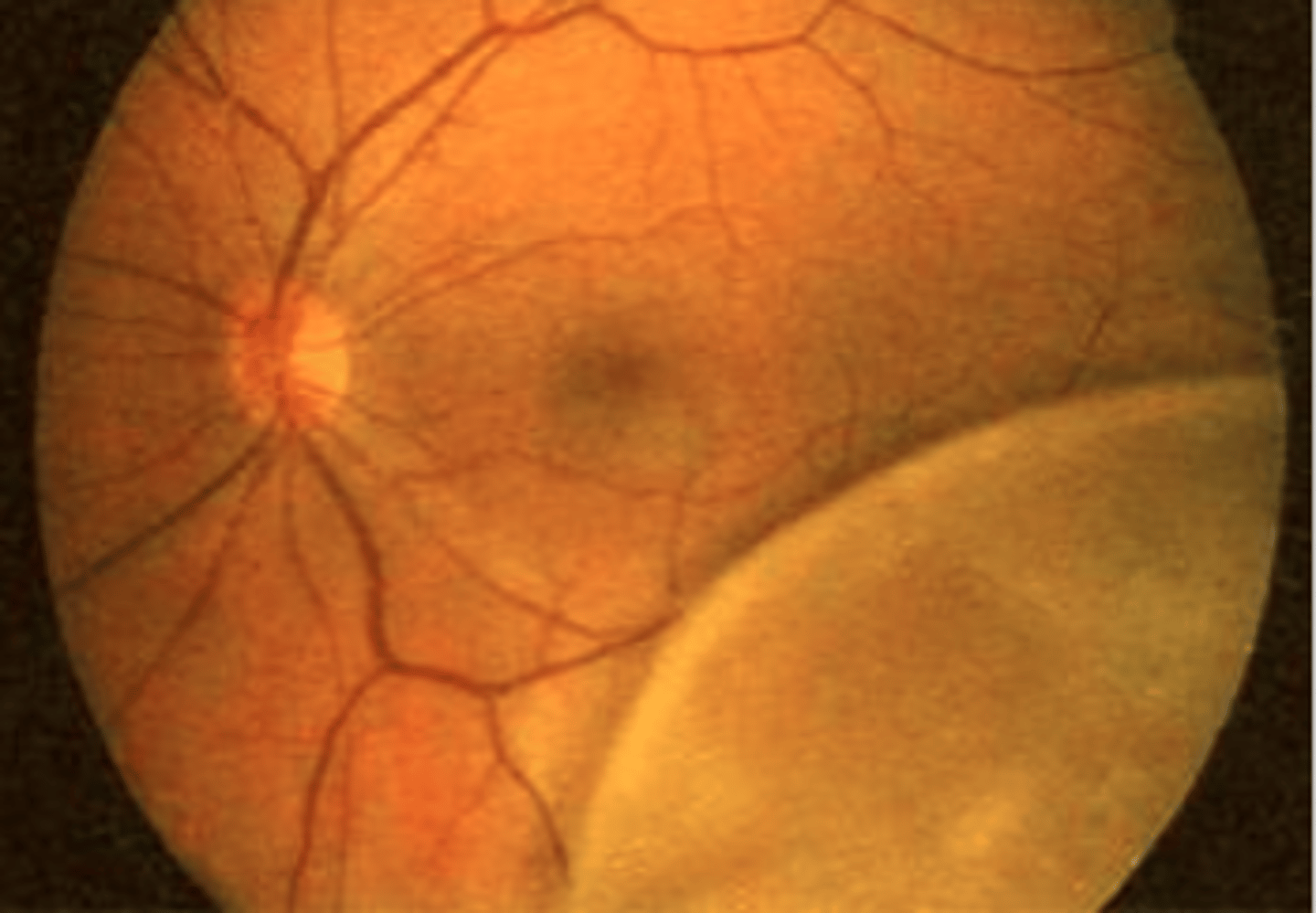
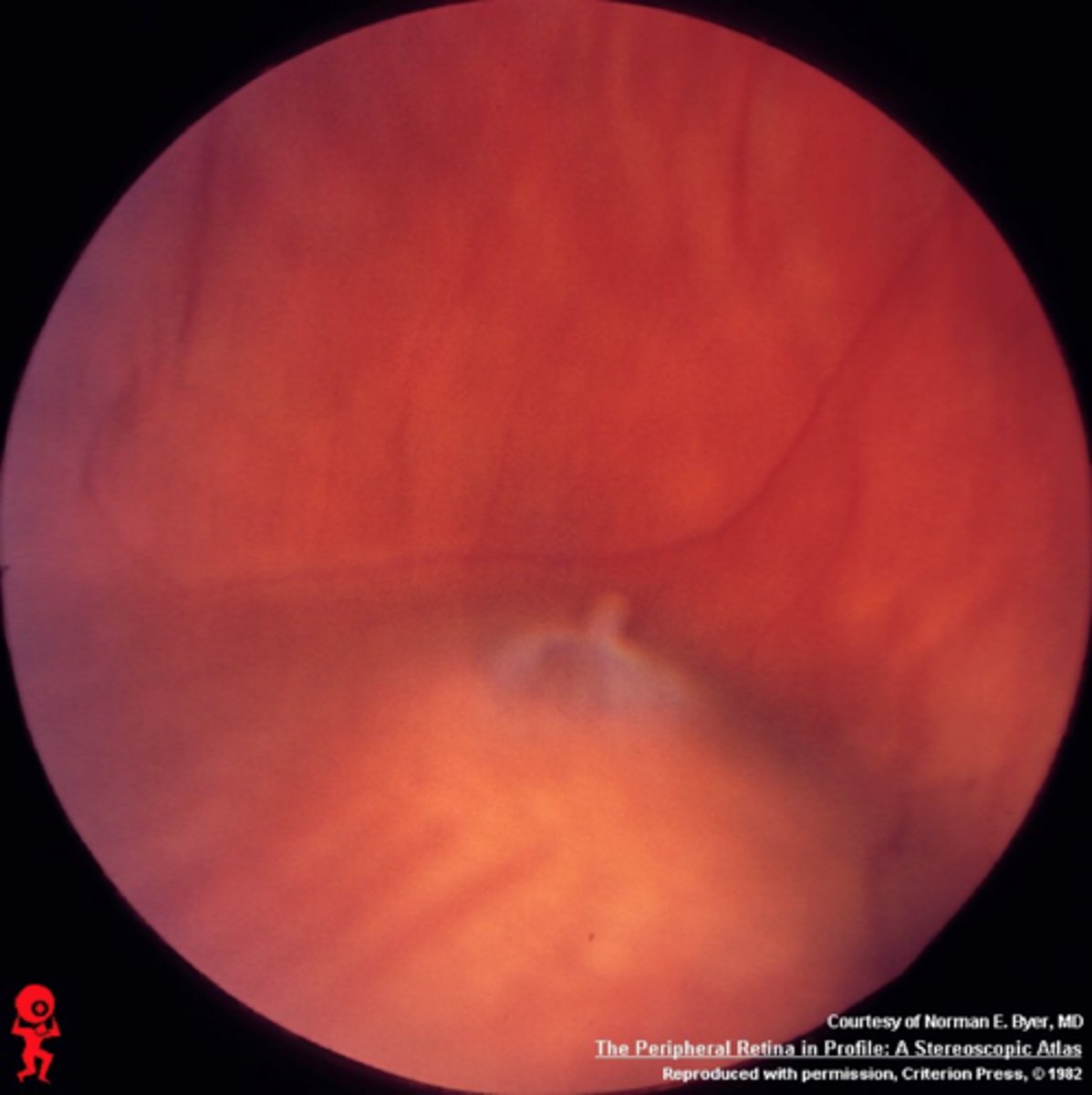
Degenerative Retinoschisis aetiology
Splitting of the neurosensory retina (schisis =splitting), usually between the inner nuclear and outer plexiform layers
Degenerative Retinoschisis prevalence
1.5 to 7% of patients over 40 yrs old
Degenerative Retinoschisis symptoms
Usually asymptomatic as peripheral,
absolute scotoma on field testing
Degenerative Retinoschisis signs
Bilateral in up to 80%
• Usually inferotemporal location
• Smooth, immobile dome-shaped elevation of the retina (like a blister)
• Does not move with eye movements
• May have sclerotic vessels on surface
• May have snow-flake bodies on surface
• May have associated retinal holes
Degenerative Retinoschisis differential diagnosis
Chronic retinal detachment (opaque and corrugated appearance)
Degenerative Retinoschisis complications
Only occasionally leads to retinal detachment
• Foveal involvement is very rare
Degenerative Retinoschisis management
If no associated retinal holes can review in 6 months for progression
• ENSURE that patient is educated correctly regarding symptoms of retinal
detachment
• If in any doubt refer
Juvenile Retinoschisis aetiology
Rare inherited condition (X-linked recessive)
• Defect in Muller cells → Splitting of RNFL from the rest of the NS retina
• Bilateral maculopathy, with peripheral retinoschisis 50%
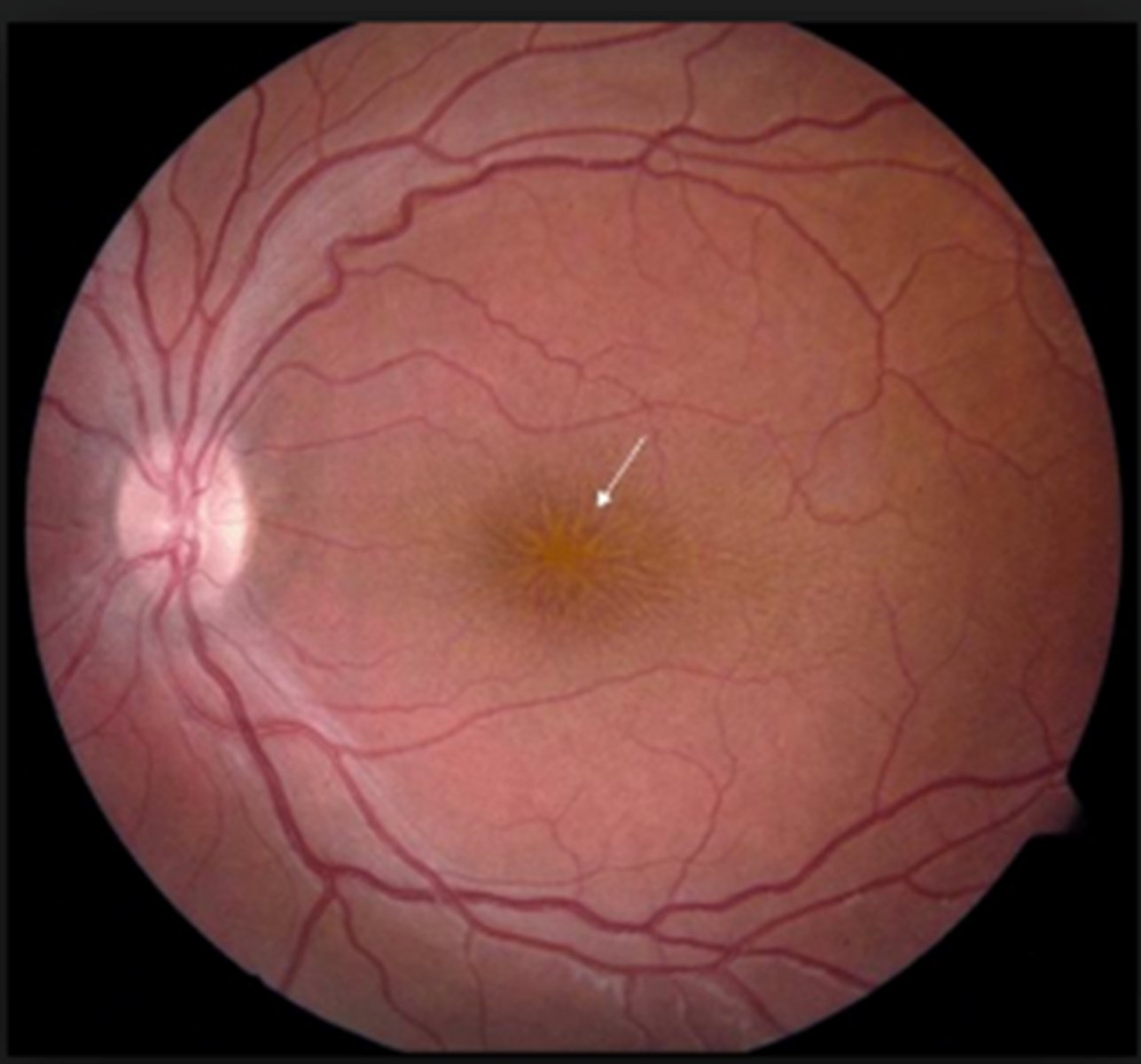
Juvenile Retinoschisis signs and symptoms
Presents in males aged 5-10 years
• Difficulty with near vision
• Macular - cystoid changes appear stellate
• Peripheral schisis - infero-temporal quadrant
Juvenile Retinoschisis complications
Vitreous and intra-schisis haemorrhages in 40%
• Neovascularisation
• Predisposes to retinal detachment (25% of cases)
Juvenile Retinoschisis prognosis
Poor due to progressive maculopathy
Management
Refer
• No good treatment - monitor for retinal detachment
• Low vision service
Lattice degeneration prevalence
6-10%
• Peak incidence 2nd-3rd decade
• More common in moderate myopes
Lattice degeneration- aetiology
Retinal thinning with discontinuation of the ILM and variable atrophy of the neurosensory retina
• Overlying area of vitreous liquefies
• Strong attachment at the margins
Lattice degeneration symptoms
asymptomatic
Lattice Degeneration: Signs
Appears as a linear track circumferentially
• Usually bilateral, temporal and superior location
• Between the equator and ora serrata/posterior vitreous base
• Sclerosed vessels ('lattice-like')
• +/- 'snowflakes' (Muller cell remnants)
• Associated RPE hyperplasia
• Chorioretinal atrophy may be present
• Small holes are common
Lattice degeneration: Complications
• Rare
• Risk of retinal detachment 0.05 to 0.1% (decreases with age)
• Tears 2° to PVD (strong adhesion)
• Atrophic holes rarely (2%)
• Found in 30% or eyes with RD
Lattice degeneration: management
No retinal breaks or symptoms - review in 6 to 12 months
- ENSURE that patient is educated correctly regarding symptoms of retinal detachment
• If in any doubt refer
Snailtrack Degeneration aetiology
Precursor to lattice degeneration
• Sharply demarcated bands of tightly packed 'snowflakes'
• Give the peripheral retina a white frost-like appearance
• Prophylactic treatment for snailtrack and lattice degeneration not widely
considered necessary
Cystic Tuft aetiology
Congenital abnormality
• Up to 5% of the population (seen more with widefield imaging)
• Round or oval, discrete, elevated whitishlesion
• Located equatorial or peripheral retina
• Glial tissue
Cystic Tuft associations
Strong vitreoretinal adhesion and small round holes
Cystic Tuft predisposes what
Horse shoe tears and retinal detachment (<1%)
Atrophic retinal holes aetiology
2-3% of the population
• Asymptomatic - incidental finding
• Full or partial thickness
• Pinpoint to 2DD, round, red lesions
• May be surrounded by cuff of whitish oedema or pigment (PRE hyperplasia)
• Pigment is a sign of relative stability hole present for at least 2-3 months

Atrophic retinal holes where it is found and what it is associated with
Usually found between the ora serrata and equator
• Often associated with lattice degeneration
Atrophic retinal holes: Complications
Full thickness hole can allow transmission of fluid → retinal detachment
• Fewer than 7% of atrophic holes develop into retinal detachment
Atrophic retinal holes: management
Management
• An isolated, asymptomatic atrophic retinal hole with no associated cuff of oedema - review 12 months
• Any atrophic hole with cuff of oedema or symptoms should be referred (same day)
• ENSURE that patient is educated correctly regarding symptoms of retinal detachment
• If in any doubt refer
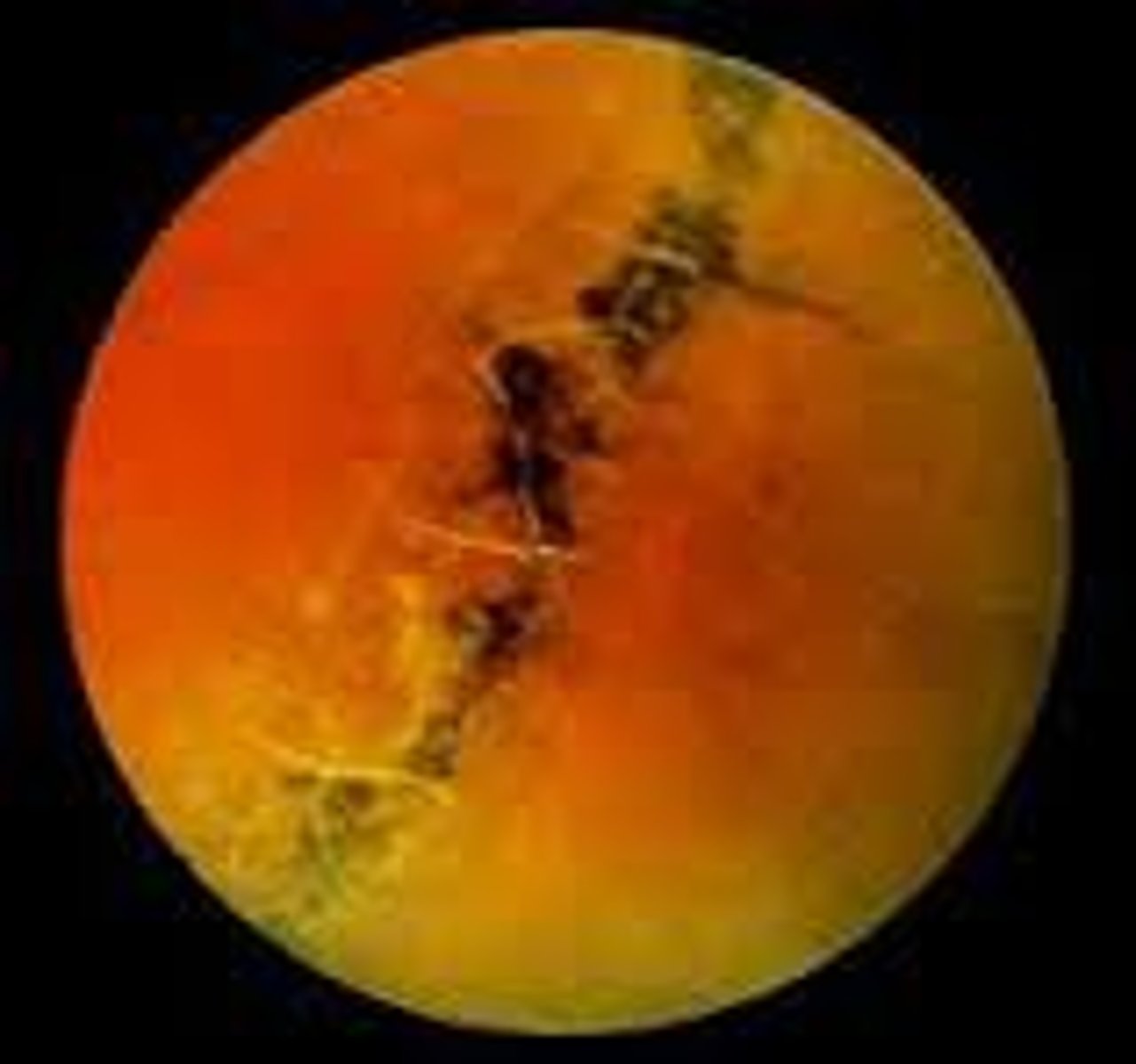
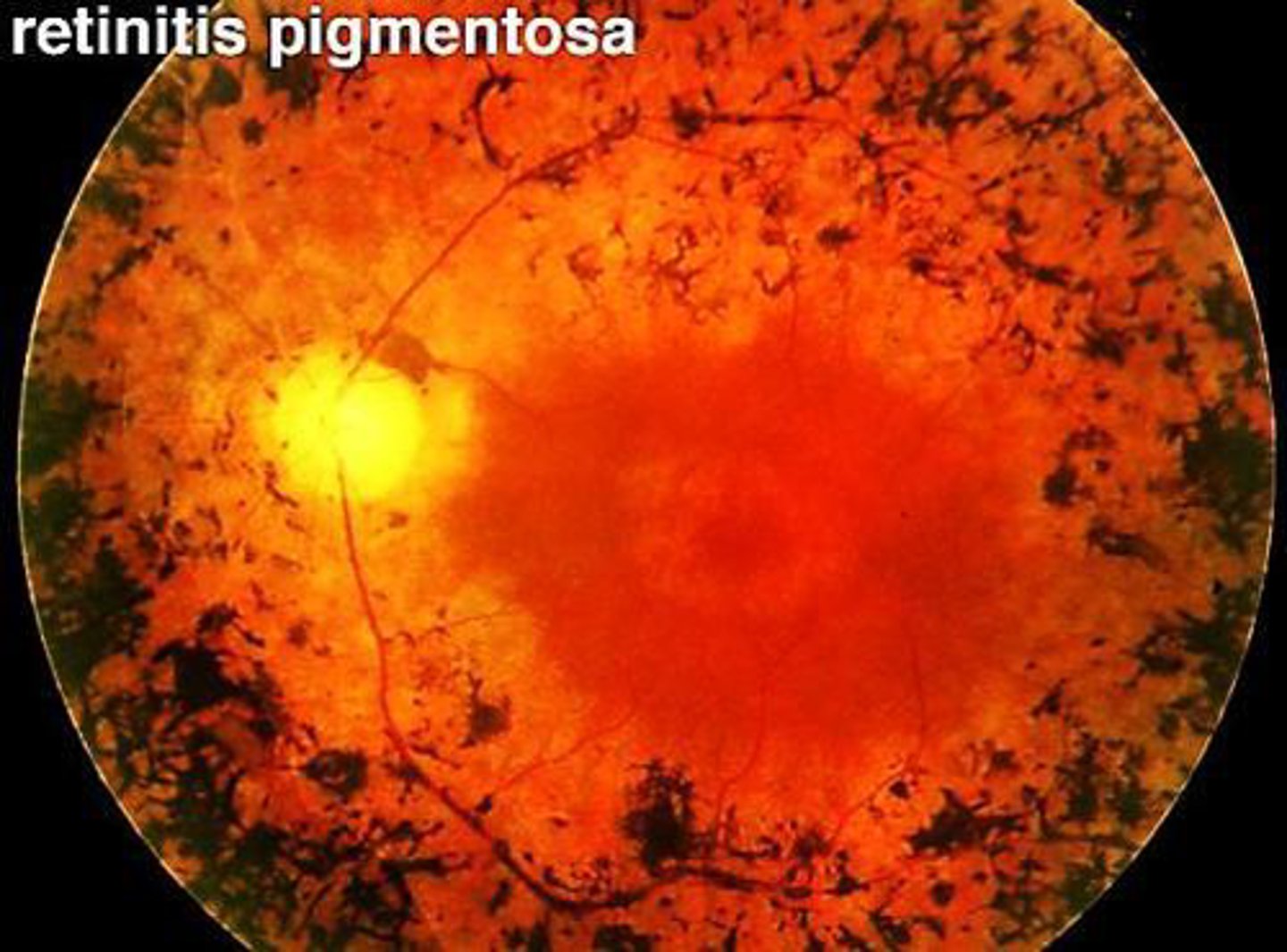
Retinitis Pigmentosa (RP): aetiology
Group of inherited degenerative diseases preferentially affecting rod function
• Prevalence 1 in 5,000
• Age of onset, rate of progression, eventual vision loss and associated ocular features depend on the mode of inheritance
Retinitis Pigmentosa (RP): symptoms
Usually start in childhood or adolescence
• Nyctalopia
• Dark adaptation difficulties
• Photopsia
• Loss of peripheral vision
• Often severely sight impaired by 40 years old
Retinitis Pigmentosa (RP): Signs
Bilateral mid-peripheral 'bone-spicule' pigmentary changes
• RPE atrophy (choroidal vessel visibility)
• Waxy disc pallor
• Blood vessel attenuation
• Midperipheral VF loss → tunnel vision
• Central vision loss in late stages (difficult reading and seeing detail)
Retinitis Pigmentosa (RP): complications
Posterior subcapsular cataract
• Retinal detachment
• Interference with daily activities - driving
Retinitis Pigmentosa (RP): further investigations
Electroretinogram (ERG) to assess retinal function
• Genetic testing
Retinitis Pigmentosa (RP): prognosis
Some people with RP eventually go blind,
most people maintain some vision
Retinitis Pigmentosa (RP): treatment
Conservative, no known cure
• Amber tints - glare
• Supplement e.g. Vitamin A may help to slow progression
• Gene therapy (clinical trials)
What is albinism?
Abnormalities in the synthesis of melanin
• Ocular albinism: Eye alone
• Oculocutaneous albinism: eye, skin and hair
• VA generally reduced due to foveal hypoplasia
ocular albinism features
↓VA, photophobia
• Nystagmus, strabismus, ametropia, iris hypopigmentation/transillumination, foveal hypoplasia, fundus hypopigmentation
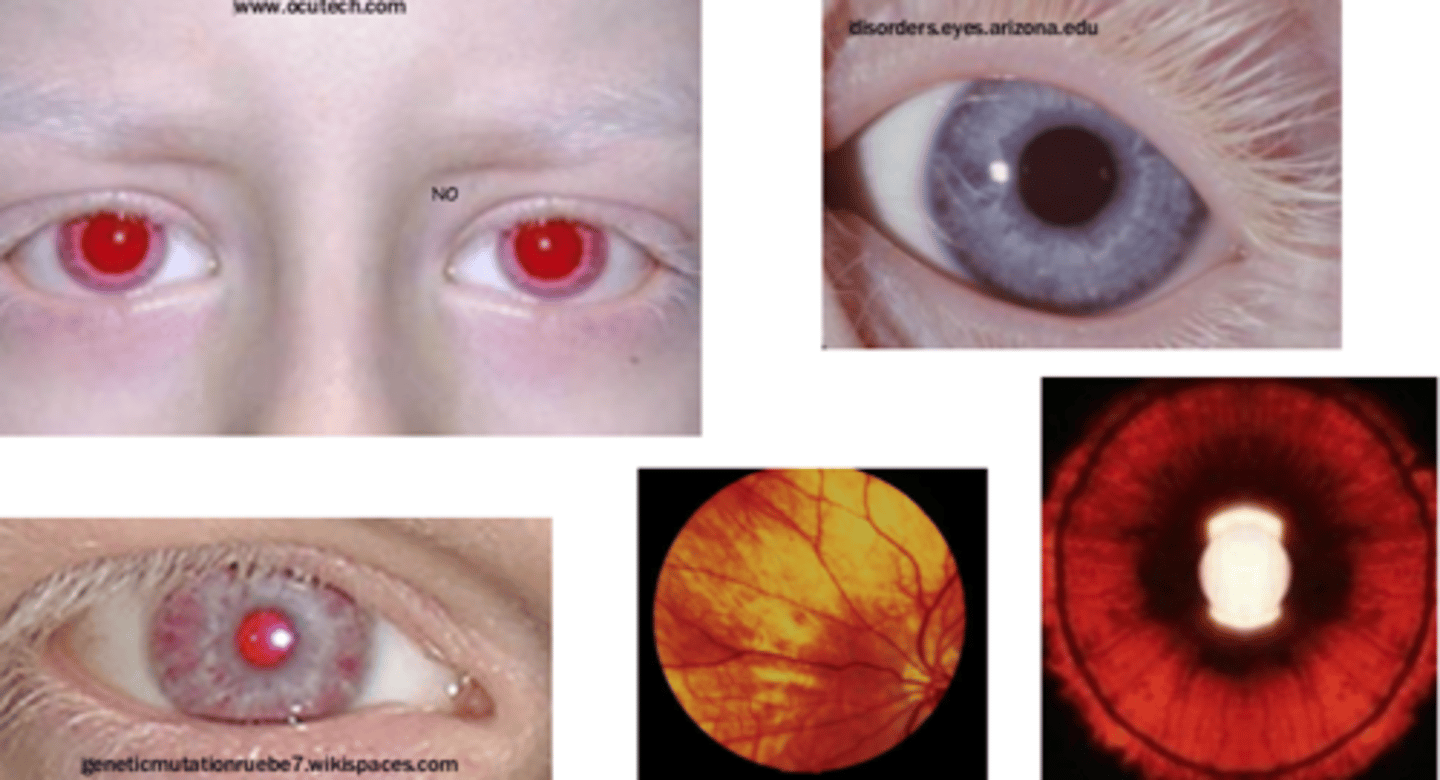
ocular albinism : management
Glasses, surgery for strabismus
Oculocutaneous Albinism
As for Ocular albinism
• Hypopigmentation of skin and hair
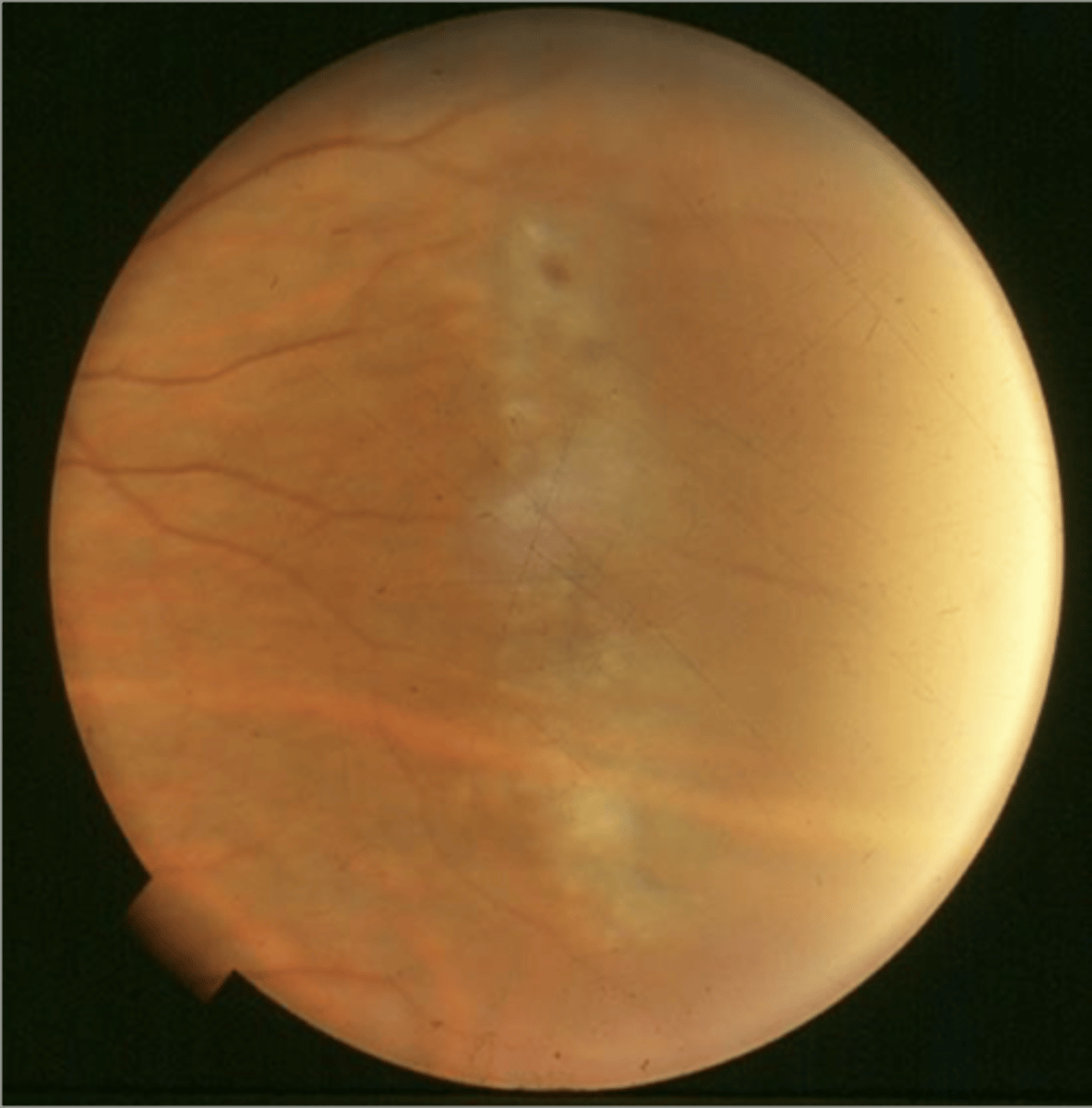
Malignant choroidal melanoma: aetiology
Rare (6 per million Caucasian individuals)
• Life threatening metastasis
• Risk depends on the size, location and cell type
Early detection & treatment improves prognosis
• Occur in isolation for from pre-existing choroidal naevus

Malignant choroidal melanoma: risk factors
Light coloured iridies
• Fair skin
• Congenital ocular melanocytosis
• Mean age at presentation 60 years
Malignant choroidal melanoma: symptoms
Frequently asymptomatic (30% detected before symptoms develop)
• Photopsia, blurred and distorted vision, floaters,VF loss
Malignant choroidal melanoma: Signs
• Slight to dramatic dome-shaped elevation ('collar stud' may protrude
into vitreous)
• Slate grey to greyish/green to white (amelanotic)
• Generally mottled, clumps of orange pigment (lipofuscin) frequently present
• Round to very irregular
• Indistinct margins
• Generally will display a scotoma (may be larger than size of lesion)
• Secondary retinal detachment often present (SRF seen on OCT)