A&P Quiz 8 (Ch 24 pt 2)
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
93 Terms
Oral Cavity
mouth, lined by nonkeratinized stratified squamous epithelium
2 Regions of Oral Cavity
vestibule
oral cavity proper
Vestibule
space between the lips/cheeks and teeth
Oral Cavity Proper
space medial to the teeth
Lips (Labia)
form anterior boundary of the vestibule, important for mastication and speech, formed by the orbicularis oris muscle and connective tissue, outer skin is not highly keratinized making it more transparent
Labial Frenulum
central mucosal fold that attaches each lip to the gingiva within the vestibule
Cheeks
form the lateral walls of the oral cavity, lined with nonkeratinized stratified squamous epithelium and covered by skin
Buccinator Muscle
flattens cheek against the teeth
Buccal Fat Pad
act as a gliding pad for muscles of mastication
Palate
forms the roof of the oral cavity to prevent food from passing into the nasal cavity during chewing and swallowing
2 Regions of Palate
hard
soft
Hard Palate
anterior bony portion
Soft Palate
posterior nonbony portion composed of skeletal muscle and connective tissue
Uvula
posterior projection of the soft palate
Fauces
posterior boundary of the oral cavity, opening to the pharynx, palatine tonsils are located on the lateral wall
Tongue
large muscular organ, occupies most of the oral cavity proper when the mouth is closed
3 Features of Tongue
terminal sulcus
body
root
Terminal Sulcus
divides the tongue into the body and root
Body of Tongue
anterior portion found in the oral cavity, relatively free except at the attachment to the lingual frenulum, covered by nonkeratinized stratified squamous epithelium and papillae
Root of Tongue
posterior portion in the oropharynx, contains a few scattered taste buds and the lingual tonsil
2 Muscle Groups of Tongue
intrinsic
extrinsic
Intrinsic Tongue Muscles
within the tongue itself, responsible for the changing shape of the tongue (flattening, elevating)
Extrinsic Tongue Muscles
outside the tongue but attached to it, protrude and retract the tongue, move the tongue from side to side, change the tongues shape
5 Functions of the Tongue
moves the food in the mouth
hold food in place during mastication
major role in swallowing
location of taste buds
functions in speech
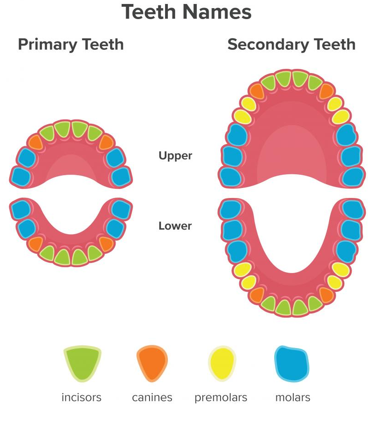
Teeth
dentition, function in mastication of food and assist in speech, 32 permanent (secondary) teeth that are in 2 dental arches (maxillary arch and mandibular arch)
Permanent Teeth
32, secondary, replace deciduous teeth staring at about 6 until 11 years, divided into four quadrants
Deciduous Teeth
primary, milk, lost during childhood, erupt between 6 months and 24 months of age
4 Quadrants of Permanent Teeth
right upper
left upper
right lower
left lower
Each Quadrant of Permanent Teeth Contains
one central and one lateral incisor
one canine
first and second premolars
first, second and third molars
3 Main Regions of Teeth
crown
neck
root
Crown
region of tooth exposed in the oral cavity and covered with enamel, can have one or more cusps
Neck
small region of tooth between crown and root
Root
largest region of tooth that anchors it to the bone
4 Structures of Teeth
pulp cavity
dentin
enamel
cementum
Pulp Cavity of Tooth
region in the center of the neck and root of the tooth, contains pulp, includes root canal and apical foramen
Tooth Pulp
collection of blood vessels, nerves, and connective tissue
Root Canal
portion of pulp cavity within root
Apical Foramen of Tooth
opening that allows nerves and blood vessels to enter and exit the pulp
Dentin of Tooth
living, cellular, calcified tissue that surrounds the root canal
Enamel of Tooth
hard, nonliving, acellular substance covering the dentin of the tooth crown, protects from abrasion and acids produced by bacteria in the mouth
Cementum of Tooth
bonelike structure that covers the surface of the dentin in the root, helps anchor the tooth to the periodontal ligament
3 Connective Structures of Tooth
alveoli (sockets)
gingiva
periodontal ligaments
Alveoli (Sockets) of Tooth
anchor site along the alveolar process of the mandible and maxilla
Gingiva of Tooth
dense fibrous connective tissue and stratified squamous epithelium covering the alveolar process
Periodontal Ligaments of Tooth
secure the teeth in the alveoli
Mastication
chewing of food by the teeth, anterior teeth (incisors and canines) primarily cut and tear food, posterior teeth (premolars and molars) crush and grind food, breaks down large food particles to increase surface area
4 Muscles of Mastication
temporalis m
masseter m
medial pterygoid m
lateral pterygoid m
Temporalis m Role in Mastication
closes jaw, retracts jaw
Masseter & Medial Pterygoid m Role in Mastication
closes jaw, protraction and lateral and medial excursion of the jaw
Lateral Pterygoid m Role in Mastication
opens jaw, protraction and lateral and medial excursion of the jaw
Mastication (Chewing) Reflex
integrated in the medulla oblongata, controls basic movements of chewing, stimulated by activation of presence of food in the mouth (relaxes muscles), muscles are stretched as mandible is lowered (activates a reflex that causes muscles of mastication to contract), descending pathways from cerebrum influence the mastication reflex to allow conscious control of chewing
Salivary Glands
scattered throughout the oral cavity, major salivary glands are compound (branching) acinar glands, can produce thin serous secretions or thicker mucous secretions
Saliva (simple)
combination from various salivary glands
2 Sizes of Salivary Glands
three pairs of large, multicellular glands
many small, coiled, tubular salivary glands
3 Pairs of Large Salivary Glands
parotid
submadibular
sublingual
4 Small Coiled Salivary Glands
lingual
palatine
buccal
labial
Lingual Glands
deep to the epithelium of the tongue
Palatine Glands
in the palate
Buccal Glands
in the cheeks
Labial Glands
in the lips
Parotid Glands
largest, located anterior to the ears, contain serous glands that secrete mostly watery saliva, includes parotid duct
Parotid Duct
exits the gland on its anterior margin, crosses the lateral surface of the masseter muscle, pierces the buccinator muscle, enters oral cavity adjacent to the second upper molar
Submandibular Glands
mixed glands, more serous then mucous acini, felt as a soft lump along the inferior border of the posterior half of the mandible, submandibular duct exits
Submandibular Duct
exits each submandibular gland, passes anteriorly deep to the mucous membrane on the floor of the oral cavity, opens into the oral cavity beside the frenulum of the tongue
Sublingual Glands
smallest of the paired salivary glands, mixed glands (contain mostly mucous acini), lie immediately below the mucous membrane in the floor of the oral cavity, have multiple openings (10-12 ducts) into the floor of the oral cavity
Saliva
composed of fluid and proteins, 1-1.5 L/day, three main roles
2 Portions of Saliva
serous
mucous
Serous Portion of Saliva
provides moisten function, produced by parotid and submandibular glands
Mucous Portion of Saliva
contains mucin that provides lubrication, produced by submandibular and sublingual glands
3 Main Roles of Saliva
helps keep oral cavity moist (important for normal speech and tasting food)
protective function
begins the process of digestion
Protective Function of Saliva
large volume of saliva continually wash oral surface, bicarbonate ions act as a buffer to neutralize acids produced by the oral bacteria and protect tooth enamel, contains lysosome (weak antibacterial action), and immunoglobulin A (helps prevent bacterial infection), mucous in saliva helps protect digestive tract from physical irritation and enzymatic digestion
Digestive Function of Saliva
relatively minor, salivary amylase, lingual lipase
Salivary Amylase
digestive enzyme that breaks bonds betwee glucose molecules in starch and other polysaccharides to produce disaccharides (maltose and isomaltose), contributes to the sweet taste of sugar, only about 2-5% of total carbs are digested here
Why is such a small amount of carbohydrate digested in the mouth?
limited amount of time in the oral cavity, cellulose covering of plants products (most starchy foods)
Lingual Lipase
digest small amount of lipid digestion
Regulation of Salivary Glands is Stimulated By
stimulated by both parasympathetic and sympathetic nervous systems, parasympathetic stimulation is more prevalent
Nerves Involved in Regulation of Salivary Glands
salivary nuclei in brainstem increases salivary secretion via parasympathetic fibers of facial (vii) and glossopharyngeal (ix) nerves, stimulated by tactile stimulation in oral cavity and certain tastes (sour)
More Regulation of Salivary Glands
can be affected by higher centers of the brain, odors can trigger thoughts of food or sensations of hunger can stimulate saliva secretion
Swallowing: Pharynx
three parts but only two normally transmit food
Nasopharynx Role in Swallowing
not a normal passageway for food
Oropharynx Role in Swallowing
superior opening to nasopharynx, inferior opening to laryngopharynx, anterior opening to posterior larynx
Laryngopharynx Role in Swallowing
extends from oropharynx to esophagus posterior to larynx
Oro & Laryngopharynx Role in Swallowing
lined with nonkeratinized stratified squamous epithelium, three muscles in posterior wall (superior, middle, and inferior pharyngeal constrictors that are arranged stacked inside each other)
Swallowing: Esophagus
extends between pharynx and stomach, 25 cm long, has the four tunics, upper esophageal sphincter and lower esophageal sphincter regulate movement of materials into and out of the esophagus, lined with nonkeratinized stratified squamous epithelium, many mucous glands in submucosal layer that secrete thick lubricating mucus
Esophageal Hiatus
opening of the diaphragm
Modifications of Esophageal Muscularis
superior 1/3 contains skeletal muscle fibers
middle 1/3 contains a mixture of skeletal and smooth muscle
inferior 1/3 contain smooth muscle fibers
3 Phases of Swallowing
voluntary
pharyngeal
esophageal
Voluntary Phase of Swallowing
first phase, bolus of food formed in oral cavity, tongue pushes against hard palate and moves toward and into oropharynx
Pharyngeal Phase of Swallowing
involuntary, 1-2 seconds, reflex initiated by stimulation of tactile receptors in oropharynx, soft palate and pharynx elevates, pharyngeal constrictor muscles contract moving food down, upper esophageal sphincter realxes
Sensory Movement in Pharyngeal Swallowing Phase
action potentials travel trigeminal (v) and glossopharyngeal (ix) nerves to swallowing center in medulla oblongata
Motor Movement in Pharyngeal Swallowing Phase
carried via trigeminal (v), glossopharyngeal (ix), vagus (x), and accessory (xi) nerves to the soft palate and pharynx
Esophageal Phase of Swallowing
5-8 seconds, responsible for moving food from pharynx to stomach, peristaltic waves of contraction, gravity assists with liquids and watery food, bolus approaches the stomach and the lower esophageal sphincter relaxes
Neural Innervation of Esophageal Phase of Swallowing
food stimulates myenteric plexus to control peristaltic waves, tactile stimuli sends impulse via the vagus nerve to the medulla oblongata, motor impulses pass along vagal efferent fiber to skeletal and smooth muscles in esophagus