Regional anatomy 11 -- the abdomen & pelvis 1
1/139
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
140 Terms
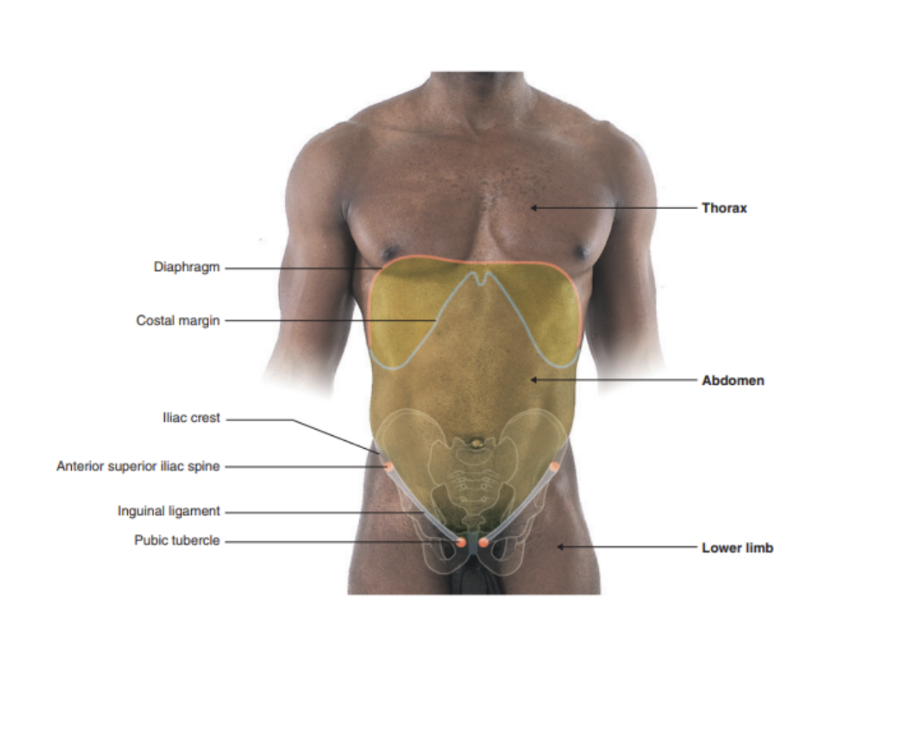
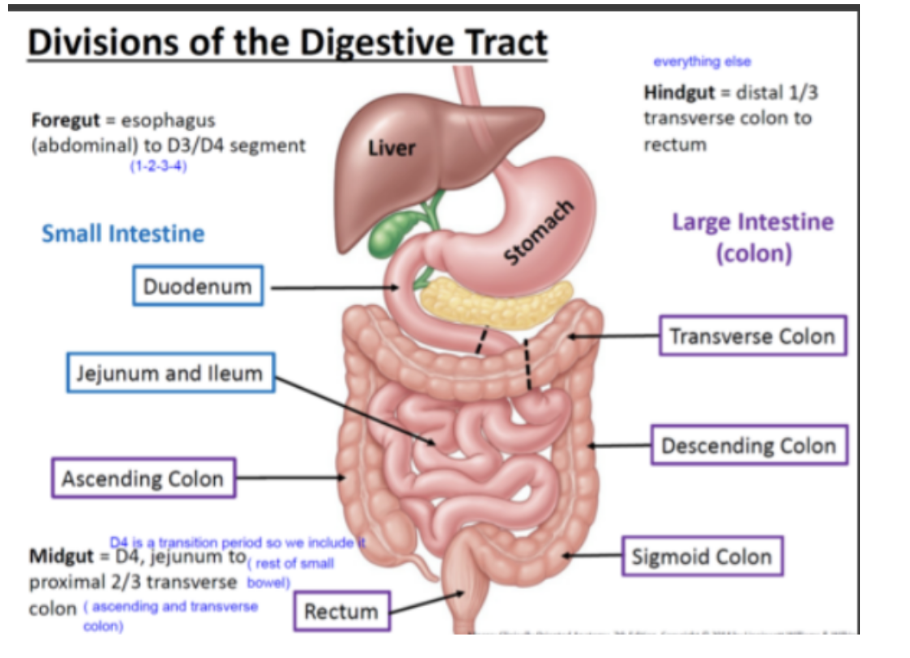
The abdomen
Roughly cylindrical chamber extending from inferior margin of thorax to superior margin of pelvis & lower limb
Upper boundary — diaphragm
Inferior thoracic aperture forms superior opening & is closed by diaphragm
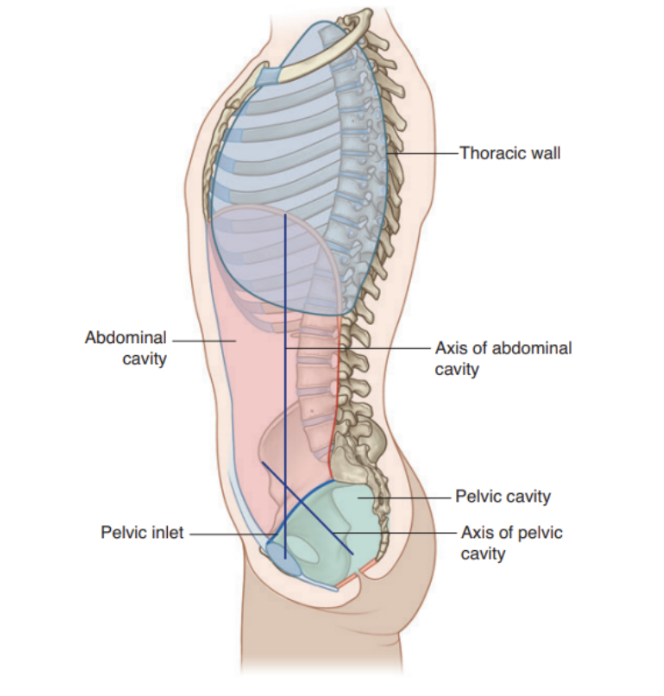
Lower boundary — upper plane of pelvic cavity
Deep abdominal wall is continuous with pelvic wall at pelvic inlet
Vertically — enclosed by vertebral column, adbominal muscles, & other muscles
Superficially — inferior limit of abdominal wall is superior margin of lower limb
Chamber enclosed by abdominal wall contains a single large peritoneal cavity that freely communicates with the pelvic cavity
Functions of the abdomen
Protection of viscera
Breathing
Control of intraabdominal pressure
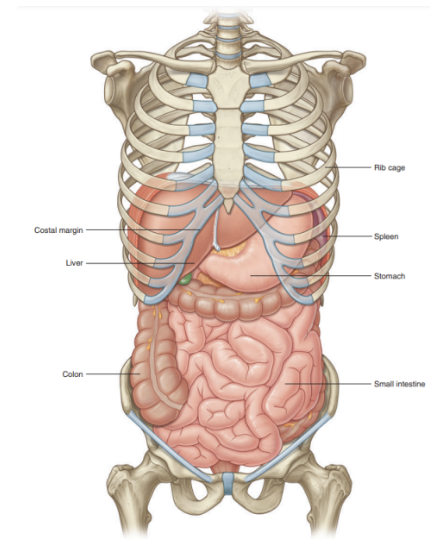
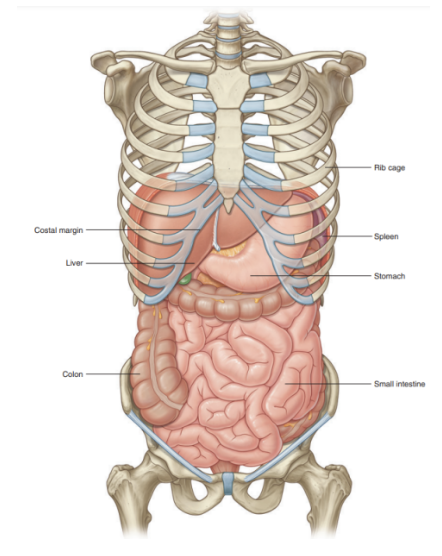
Abdominal function — protection of viscera
Holds major elements of GI system, spleen, & parts of urinary system
Additionally — much of liver, gallbladder, stomach, spleen, & parts of colon are under domes of diaphragm (project superiorly above costal margin of thoracic wall) — thus these abdominal viscera are protected by the thoracic wall
Superior poles of kidneys are deep to lower ribs
Viscera not under domes of diaphragm are supported & protected primarily by the muscular walls of the abdomen
Abdominal function — breathing
During inspiration —
Relaxes to accommodate expansion of the thoracic cavity and the inferior displacement of abdominal viscera during contraction of the diaphragm.
During expiration —
Contracts to assist in elevating the domes of the diaphragm, thus reducing thoracic volume.
It is to be noted that material can be expelled from the airway by forced expiration using the abdominal muscles, as in coughing or sneezing
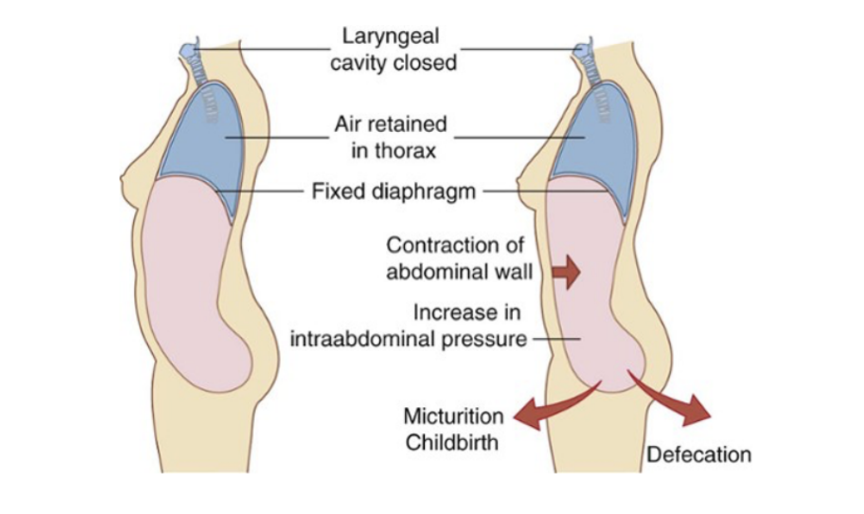
Abdominal function — control of intraabdominal pressure
Can be controlled by contraction & relaxation of the abdominal wall —
Ex. — contraction dramatically increases intraintraabdominal pressure when the diaphragm is in a fixed position, as air will be retained in the lungs by closing valves in the larynx in the neck (and can provide the counteracting pressure preventing expansion of the abdominal wall.
Increased intraabdominal pressure assists in voiding the contents of the bladder and rectum and in giving birth
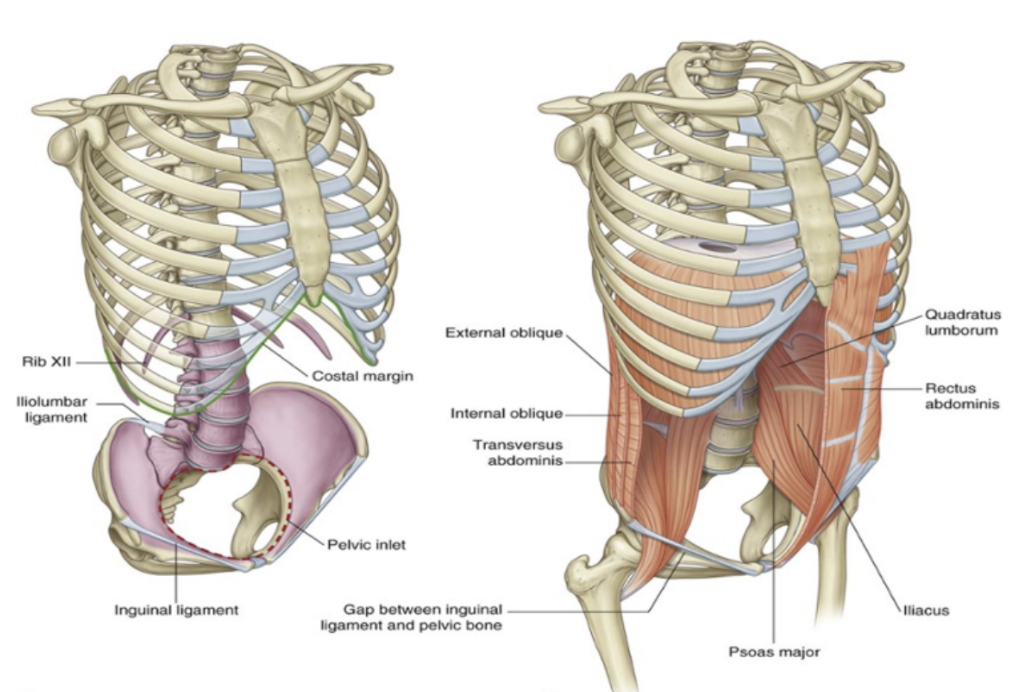
The abdominal wall makeup
Skeletal elements —
5 lumbar vertebrae & their interveneing intervertebral discs
Superior expanded parts of the pelvic bones
Bony components of inferior thoracic wall (costal margin, rib XII, end of rib XI, & xiphoid process)
Muscles —
Lateral to vertebral column —
Quatratus lumborus, Psoas major, & Iliacus muscles — reinforce posterior aspect of the wall
Distal ends of Psoas major & iliacus muscles pass into thigh — major flexors of hip joint
Lateral parts of abdominal wall are mainly formed by 3 layers of muscle (similar orientation to intercostal muscles of thora) —
Transversus abdominis
Internal oblique
External oblique
Anteriorly — rectus abdominas present on each side, spanning distance between inferior thoracic wall & pelvis
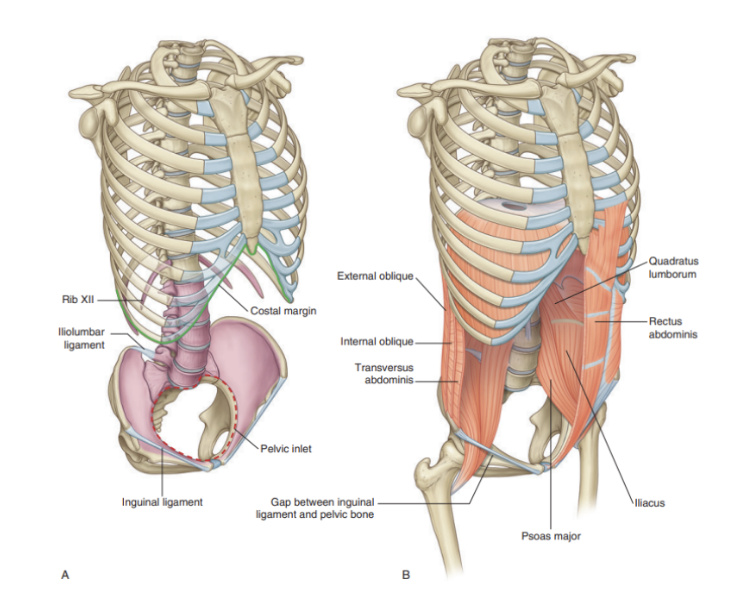
Boundaries of the abdomen
Superior aperture —
Corresponds to the thoracic inferior aperture which corresponds to the diaphragm — margin consists of
Vertebra TXII, rib XII, distal end of rib XI, costal margin, & xiphoid process of sternum
Inferior boundary —
Level of pelvic inlet — abdominal wall/cavity continuous with pelvic wall/cavity
Circular margin formed entirely by bone —
Posteriorly by the sacrum, anteruorly by pubic symphysis, & laterally (on each side) by a distinct bony rim on the pelvic bone
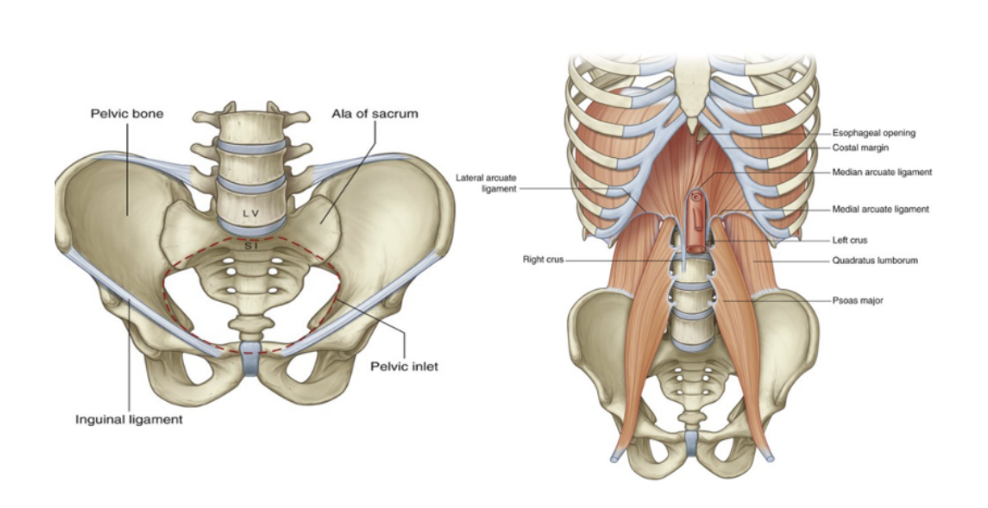
Different orientation of pelvic & abdominal cavity
Because of how sacrum & attached pelvic bones are angled posteriorly, the pelvic cavity is not oriented on same vertical plane as abdominal cavity — instead projects posteriorly, with inlet opening anteriorly & somewhat superiorly
Surface projection of abdomen —
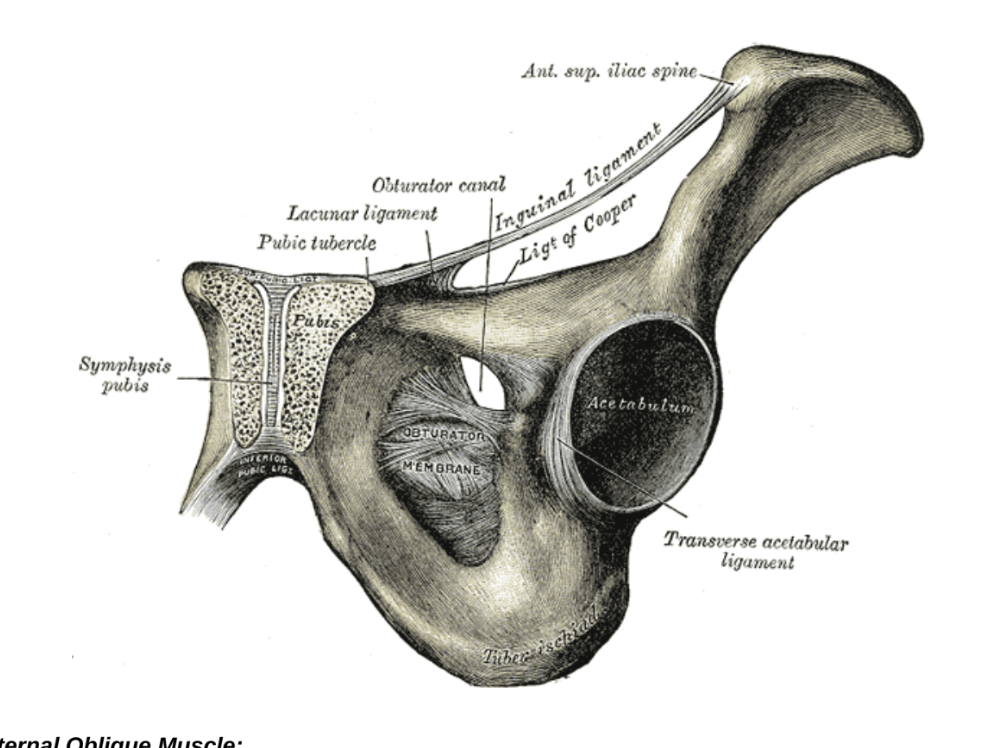
Specific landmarks to recognize regions on surface — easily palpable
Above — costal margin
Below — pubic tubercle, anterior superior iliac spine, & iliac crest
Line between anterior superior iliac spine & pubic tubercle — inguinal ligament
Separates anterior abdominal wall above from thigh of lower limb below
Iliac crest separates posterolateral abdominal wall from gluteal region of the lower limb
Upper part of abdominal cavity projects above costal margin to the diaphragm — thus abdominal viscera in this region are protected by thoracic wall
Level of diaphragm varies during breathing cycle —
Right dome of diaphragm can reach as high as fourth costal cartilage during orced expiration
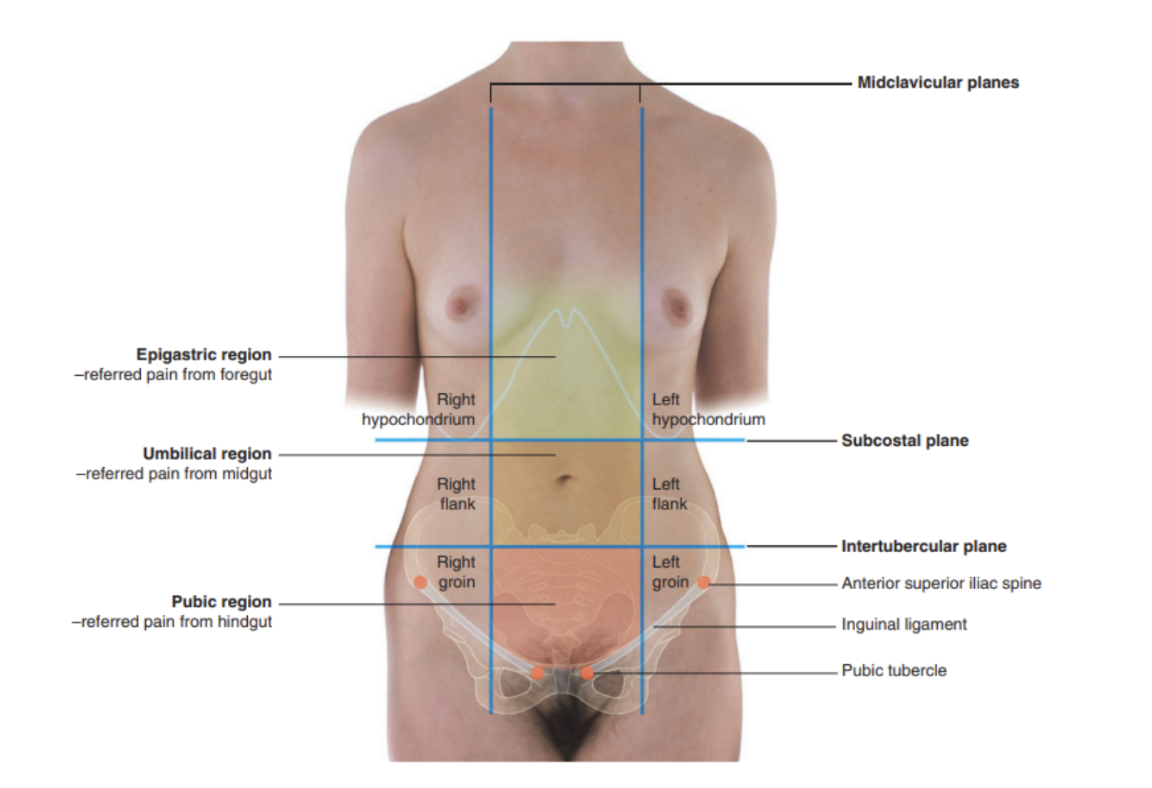
Planes & regions of the abdomen (+ importance)
Divided into 9 regions by a midclavicular sagittal plane on each side, & by subcostal & intertubercular planes (passing through the body transversely) —
3 central regions
Epigastric, umbilical, pubic
3 lateral regions
Hypochondrium, flank, groin
These regions — important when discussing referred pain
Pain from abdominal part of foregut — epigastric region
Pain from midgut — umbilical region
Pain from hindgut — pubic region
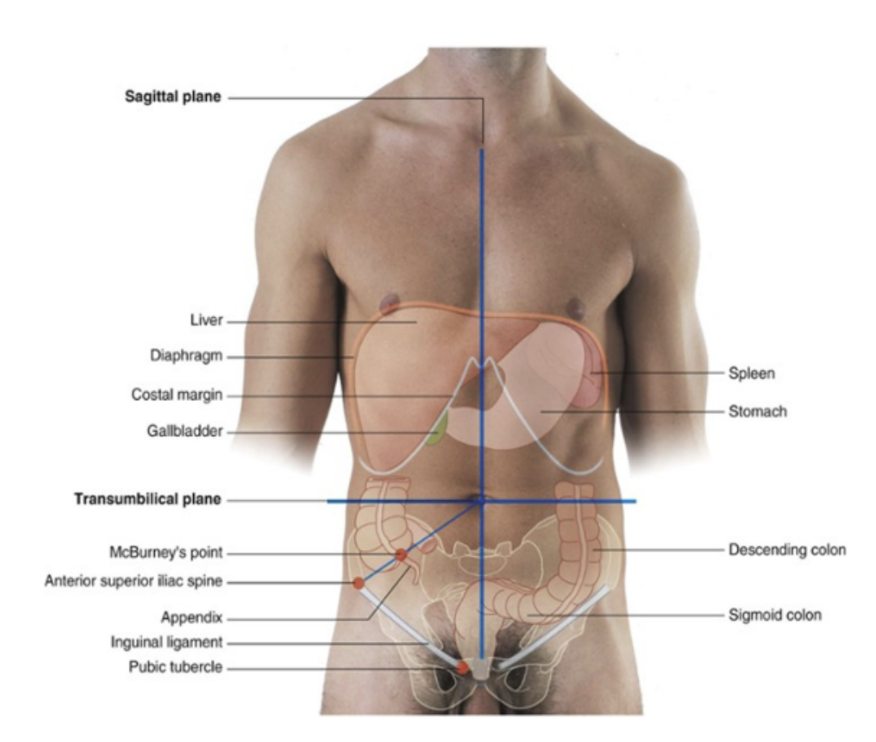
Quadrants of abdomen
We can also divide the abdomen into 4 different quadrants, by forming a vertical plane and a horizontal plane (horizontal transumbilcial plane) that coincides at the level of the umbilicus.
We can use these 4 quadrants in order to localise the specific organs:
The liver and gallbladder are in the right upper quadrant.
The stomach and spleen are in the left upper quadrant.
The cecum and appendix are in the right lower quadrant.
The end of the descending colon and sigmoid colon arein the left lower quadrant.Anterolateral wall
Anterolateral wall
The abdominal wall covers a large area.
It is bounded superiorly by the xiphoid process and costal margins, posteriorly by the vertebral column, and inferiorly by the upper parts of the pelvic bones.
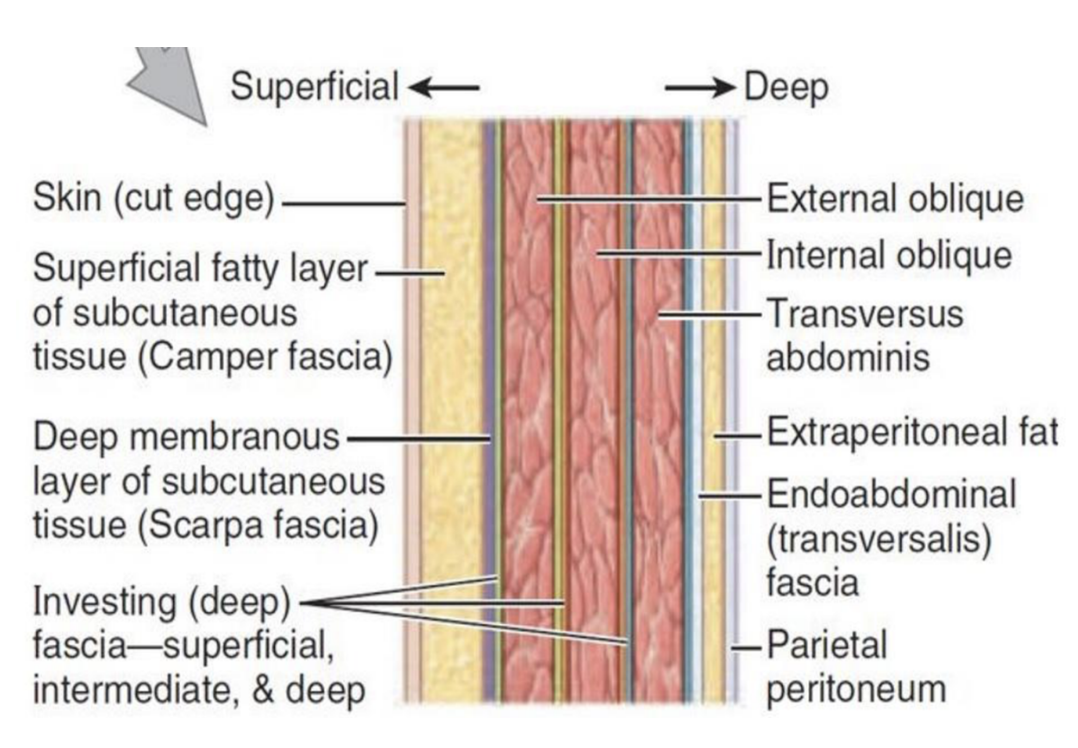
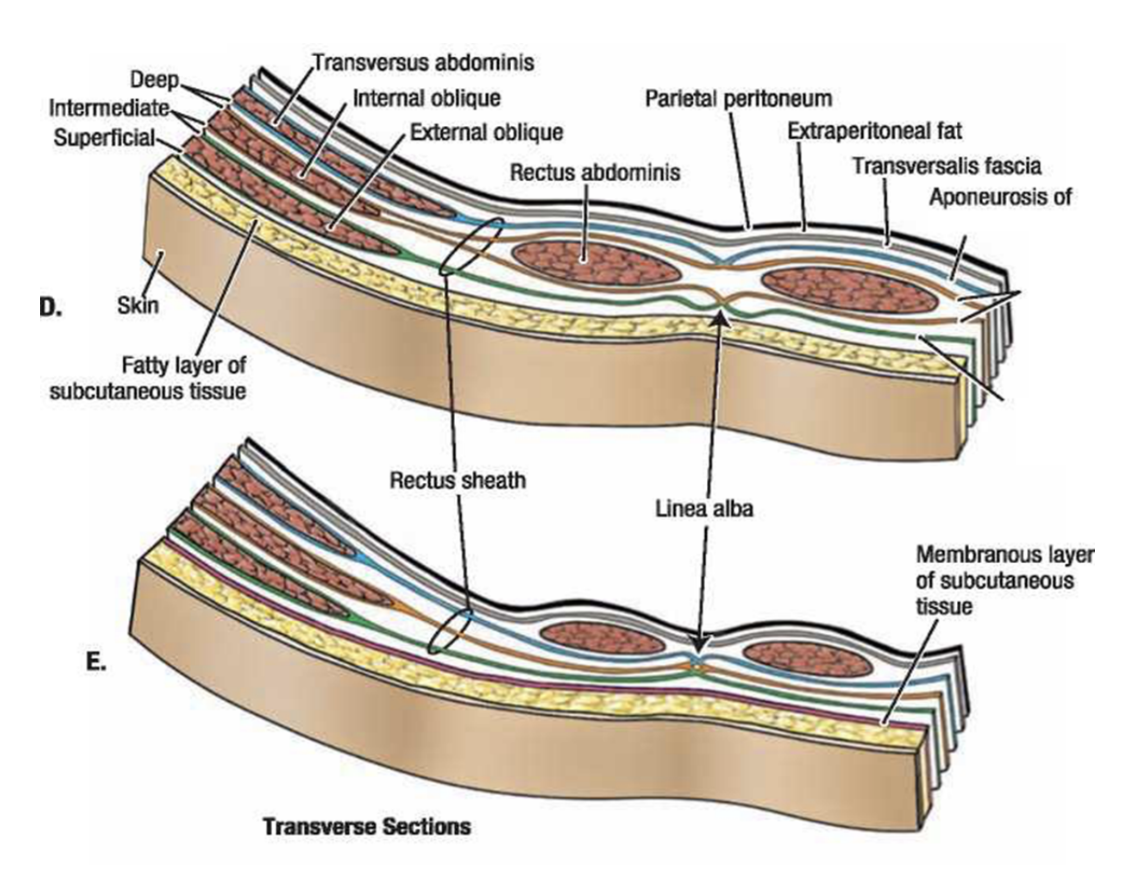
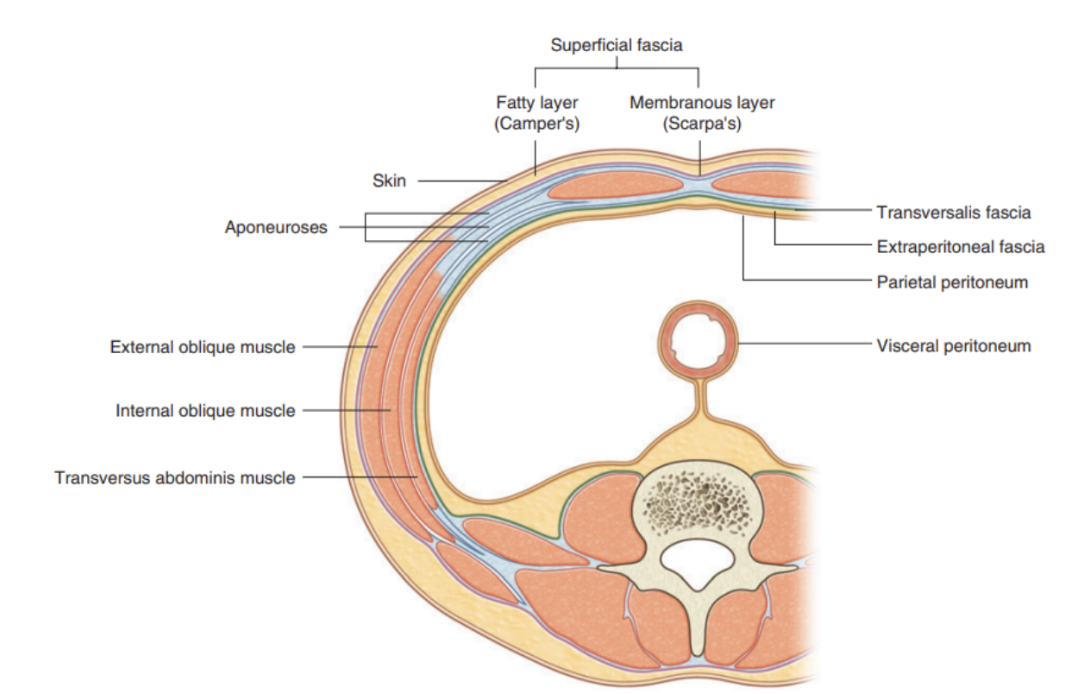
Its layers consist of skin, superficial fascia (subcutaneous tissue), muscles and their associated deep fascias, extraperitoneal fascia, and parietal peritoneum
Superficial fascia
Superficial fascia —
Subcutaneous tissue of abdomen — a layer of fatty connective tissue that usually is similar to & continuous with the fascia in other body regions
However, in the lower region of anterior part of abdominal wall, below the umbilicus, it forms 2 layers —
Superficial Camper’s fascia —
Thicker fatty layer with variable thickness — ex. greatly increased in obese individuals & thin in people with low body fat
Deep Scarpa’s fascia —
Thinner & denser membranous layer overlying muscle layer of abdominal wall, firmly attached to the linea alba & pubic symphysis and fuses with fascia lata (thigh deep fascia) right below the inguinal ligament
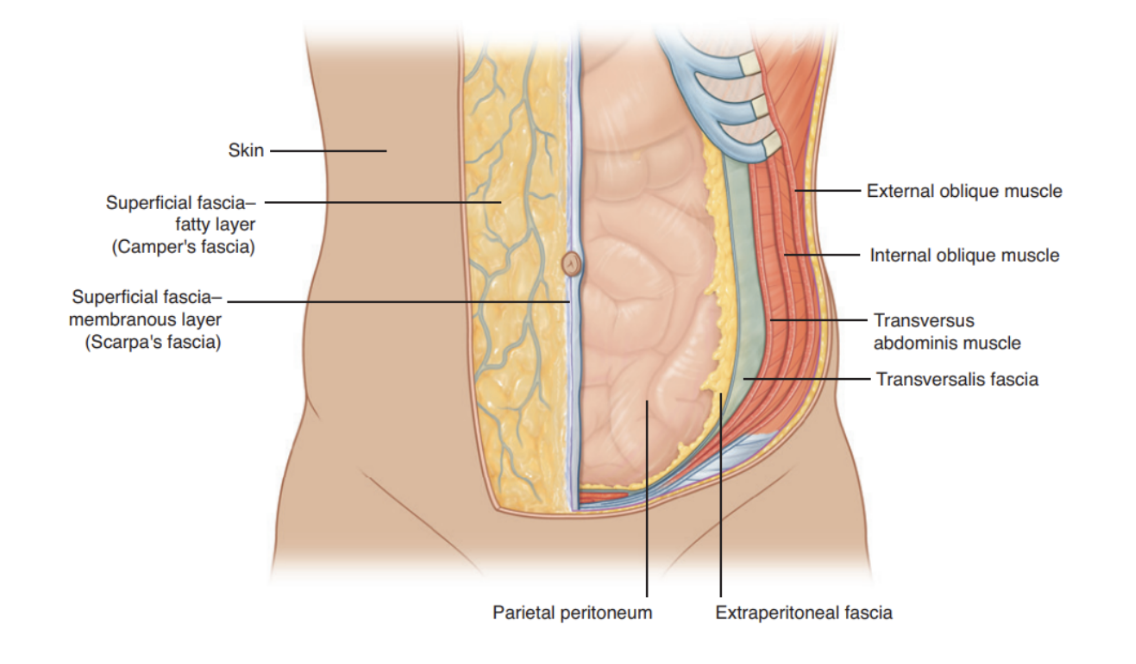
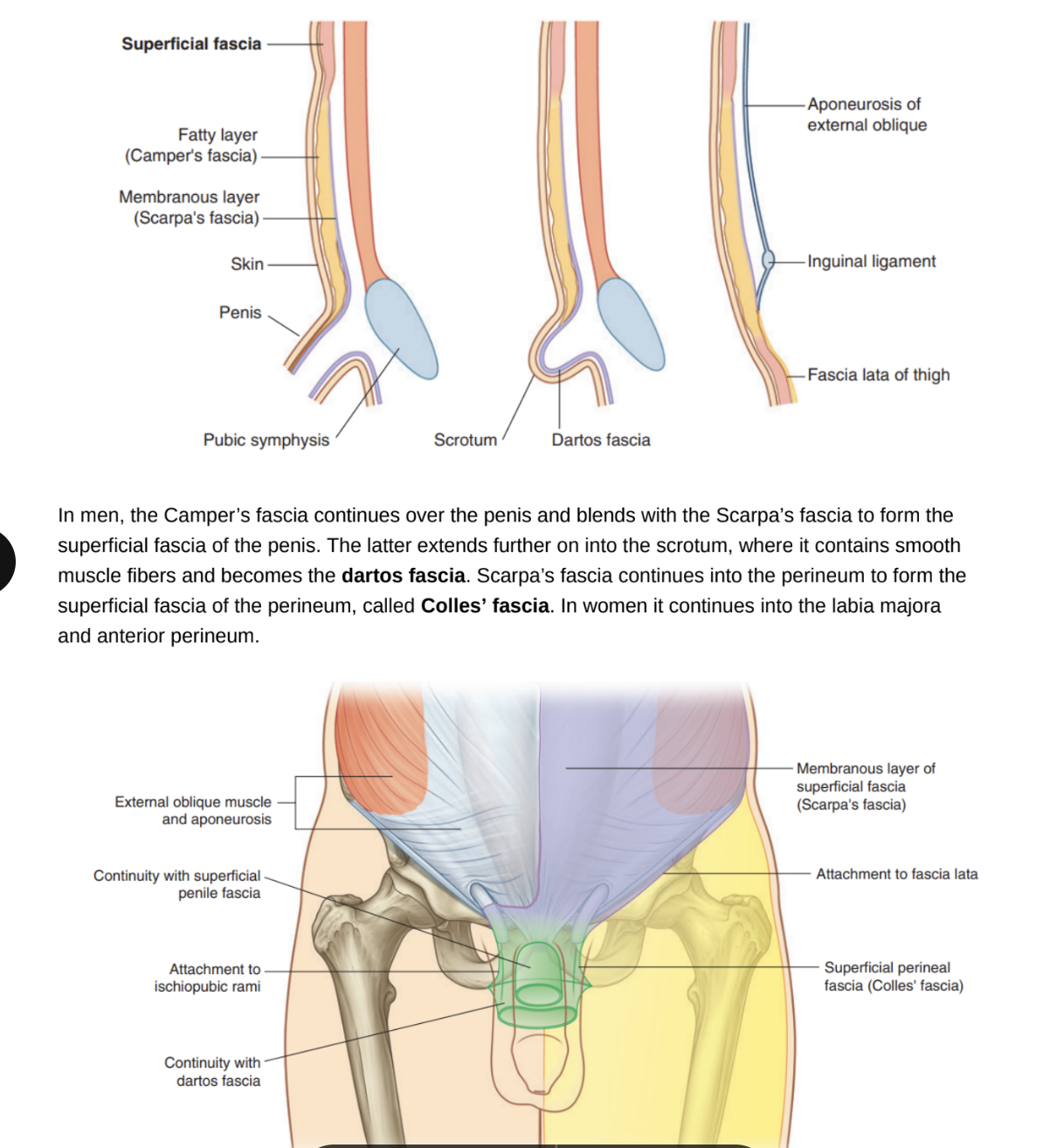
Continuation of fascia — blending of fascia & new fascias
In men, Camper’s fascia continues over penis & blends with Scarpa’s fascia to form superficial fascia of the penis
Scarpa’s fascia extends further into the scrotum, where it contains smooth muscle fibers, becoming — dartos fascia
Scarpa’s fascia also continues into the perineum to form the superficial fascia of the perineum — called Colles’ fascia
In women continues into labia majora & anterior perineum `
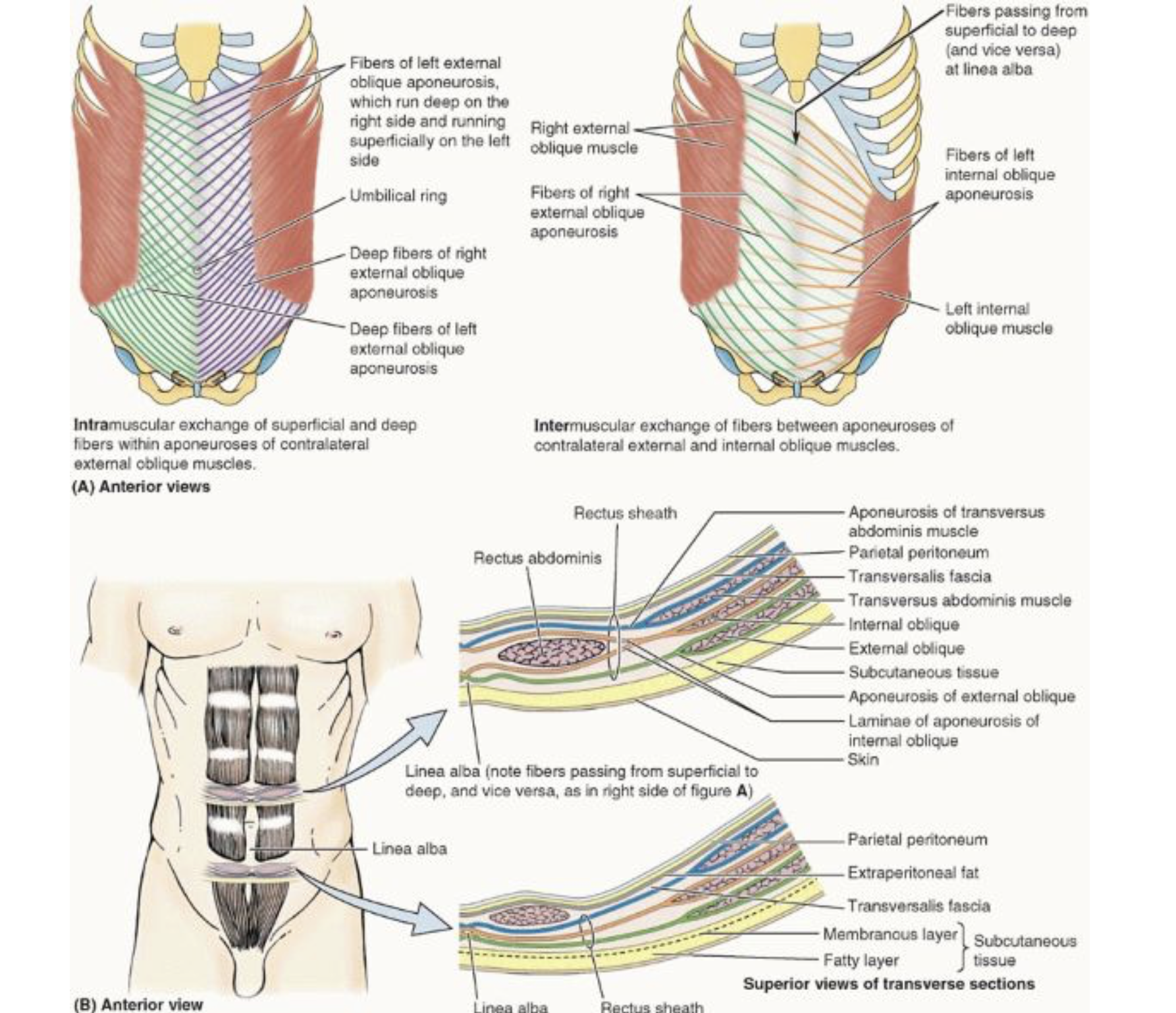
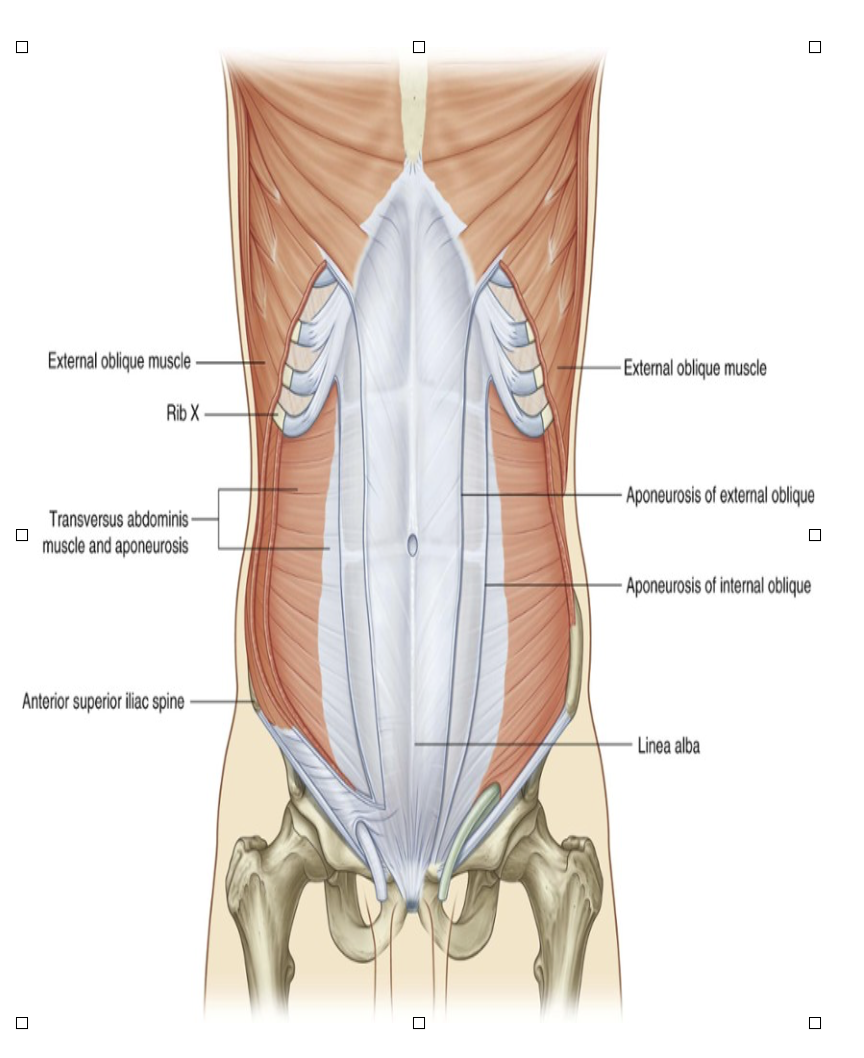
Layers of abdominal wall (image)
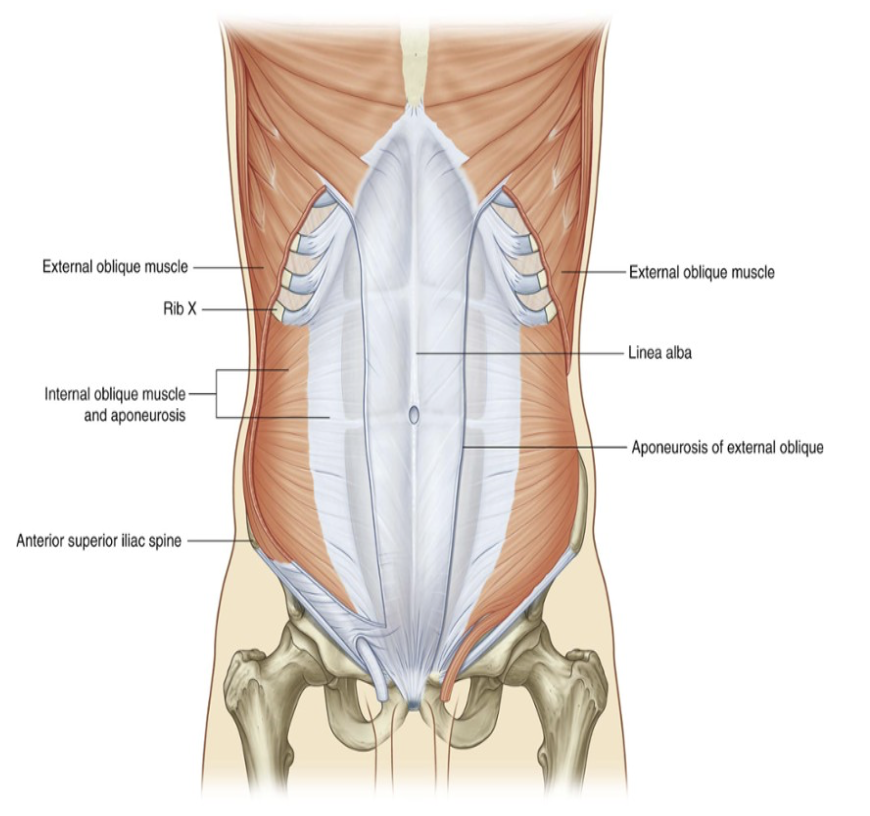
Anterolateral muscles
5 muscles in anterolateral group of abdominal wall muscles —
3 flat muscles whose fibers begin posterolaterally, pass anteriorly, & are replaced by an aponeurosis as the muscle continues towards the midline —
The external oblique, internal oblique, & transversus abdominis muscles
2 vertical muscles near the midline that are enclosed in a tendinous sheath formed by the aponeuroses of the flat muscles —
Rectus abdominis & pyamidalis muscles
These muscles form a firm but flexible wall keepng abdominal viscera in their cavity & protected from injury
They are also very important in any action increasing intraabdominal pressure —
Ex. parturition (childbirth), micturition (urination), defecation, coughing, & even breathing
Mnemonic — Tire pump
Transversus abdominis
Internal bolique
Rectus abdominis
External oblique
Pyramidalis
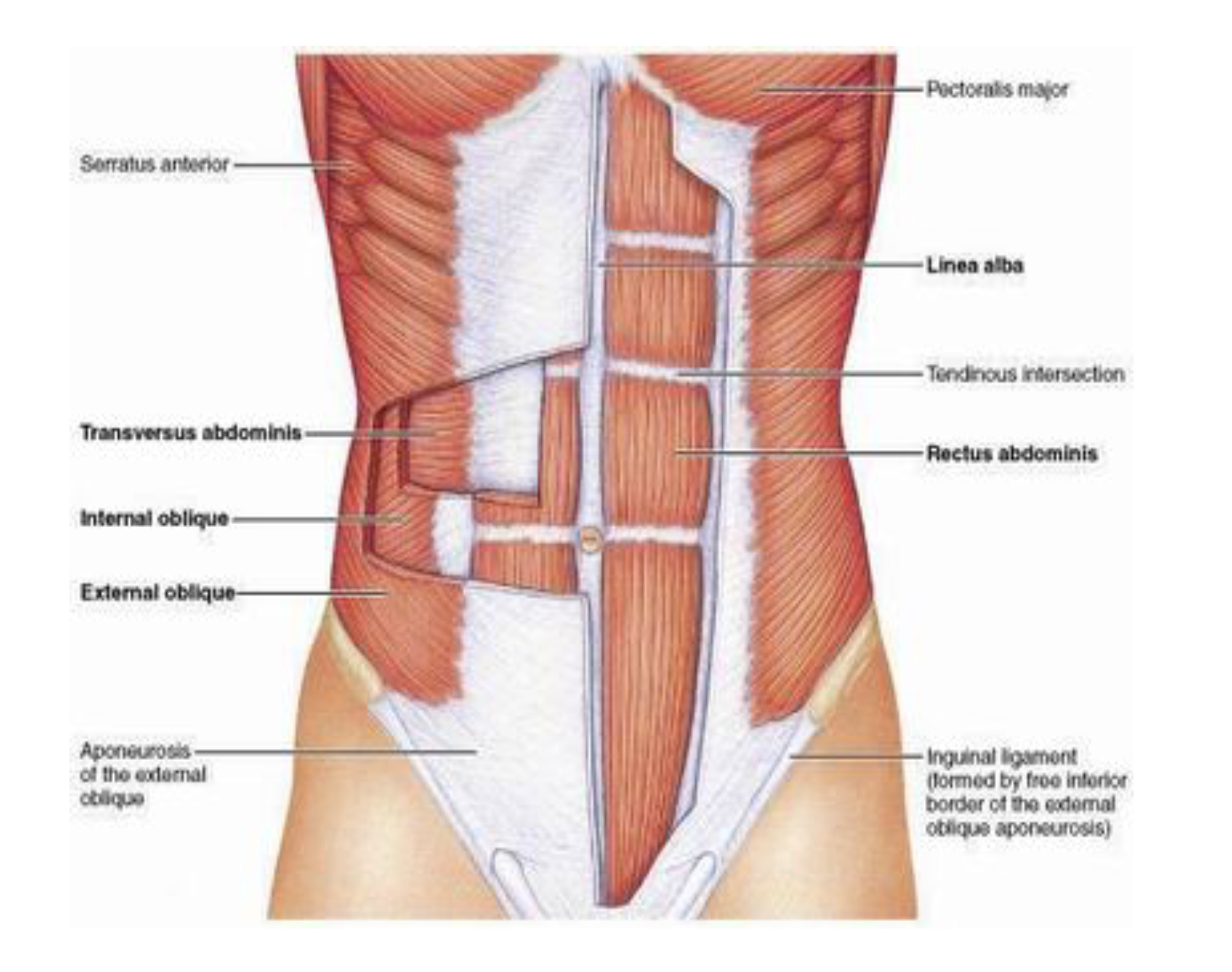
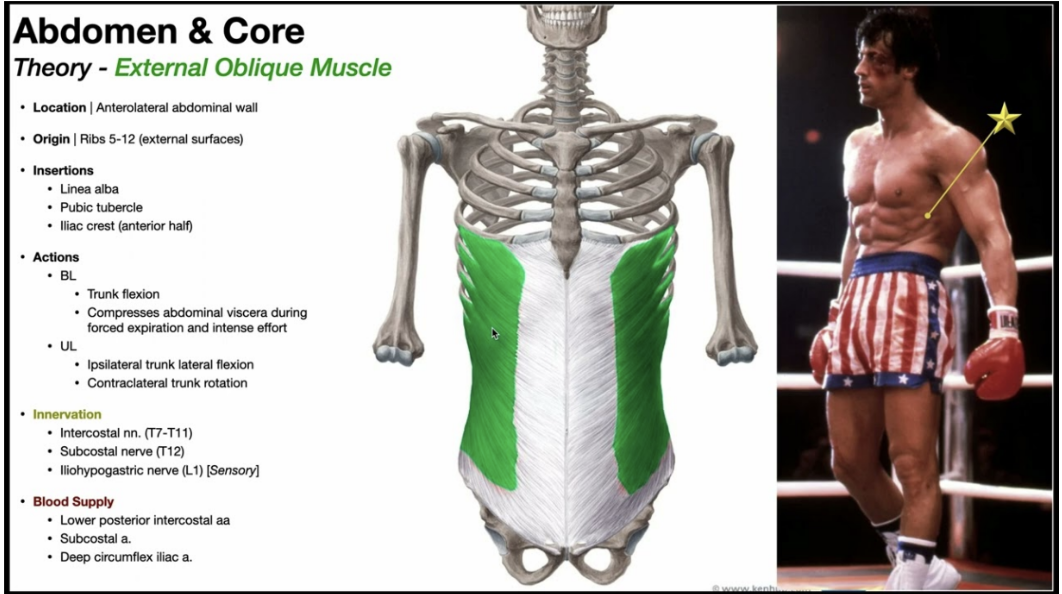
External oblique muscle
Most superficial of 3 flat muscles — immediately deep to superficial fascia
Fibers run inferiomedially
Courses from 5th to 12th rib ventromedially until the anterior layer of the rectus sheath
Originates at serratus anterior & latissimus dorsi muscles
Ventrally builds a large aponeurosis extending medially to form the linea alba, which extends from the xiphoid process to the pubic symphysis — inferior margin forms inguinal ligament
Innervation —
Anterior rami of lower six thoracic spinal nerves (T7 to T12)
Function —
Compress abdominal contents; both muscles flex trunk; each muscle bends trunk to same side, turning anterior part of abdomen to opposite side
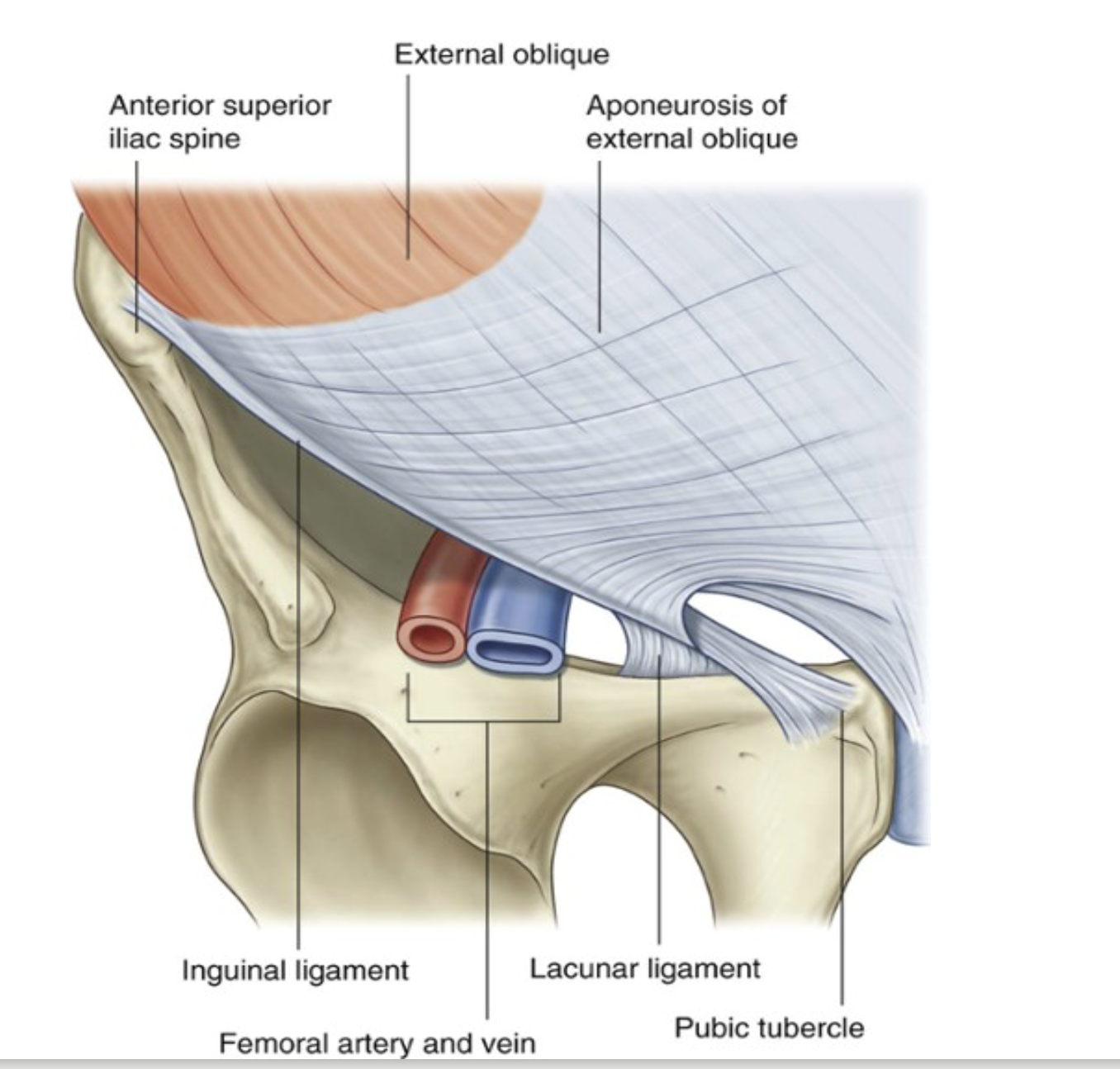
Ligaments that are extensions of fibers at medial end of inguinal canal (associated abdominal ligaments)
Inguinal ligament folds over itself creating a trough, playing an important role in the formation of the inguinal canal — several other ligaments also formed from extensions of fibers at medial end of inguinal ligament
Lacunar ligament —
Crescent shaped extension of fibers at medial end of inguinal ligament that passes backwards to attach to pecten pubic on the superior ramus of the pubic bone
Pectineal(Cooper’s) ligament —
Formed by additional fibers that extend from the lacunar ligament along the pecten pubis of the pelvic brim
Internal oblique muscle
Deep to the external oblique muscle — 2nd of 3 flat muscles
Smaller & thinner than external oblique, with most muscles fibers passing in a supromedial direction
Lateral muscular components end anteriorly as an aponeurosis blending into the linea alba at the midline
Origin — thoracolumbar fascia, iliac crest, & ileopectineal arch
Insertion — cranially at lower costal cartilages & ventrally at linea alba
Caudal fibers extend to spermatic cord & merge to form the cremaster muscle (male)
Semilunar lines (linea semilunaris) — formed by the divisions of the internal oblique aponeurosis & correspond with lateral margins of rectus abdominis muscle
Extend from tip of the 9th costal cartilage to the pubic tubercle
Innervation —
Anterior rami of lower six thoracic spinal nerves (T7 to T12) and L1
Function —
Compress abdominal contents; both muscles flex trunk; each muscle bends trunk and turns anterior part of abdomen to same side
Transversus abdominis
Deep to internal oblique muscle — named because of direction of most of its muscle fibers
Ends in an anterior aponeurosis — blends with linea alba at midline
Caudal fibers involved in formation of cremaster muscle
Innervation —
Anterior rami of lower six thoracic spinal nerves (T7 to T12) and L1
Function —
Compress abdominal contents
Transversalis fascia
Separates anterior abdominal wall from extra-peritoneal fat
Posteriorly coninuous with thorocolumbar fascia
Anteriorly crosses midline & associates with transversalis fascia of opposite side
Also in continuoation with fascia on inferior surface of diaphragm
Formed from a layer of deep fascia originating from the transversus abdominis muscle
After attaching to crest of ilium, it blends with fascia covering muscles assocated with upper regions of pelvic bones & with similar fascia covering pelvis muscles — at this point referred to as the parietal pelvic/endopelvic fascia —
Therefore presence of a continuous layer of deep fascia surrounding abdominal cavity thick in some areas, thin in others, attached or free, & participates in the formation of specialized structures
Rectus abdominus
Vertical, long, flat muscle that extends the length of the anterior abdominal wall
Paired, separated in midline by linea alba, & widens as it ascends from pubic symphysis to costal margin
Along its course intersected by 3 or 4 transverse fibrous bands/tendinous intersection
Easily visible on individuals with well developed rectus abdominis muscles (6 pack)
Innervation —
Anterior rami of lower seven thoracic spinal nerves (T7 to T12)
Function —
Compress abdominal contents; flex vertebral column; tense abdominal wall
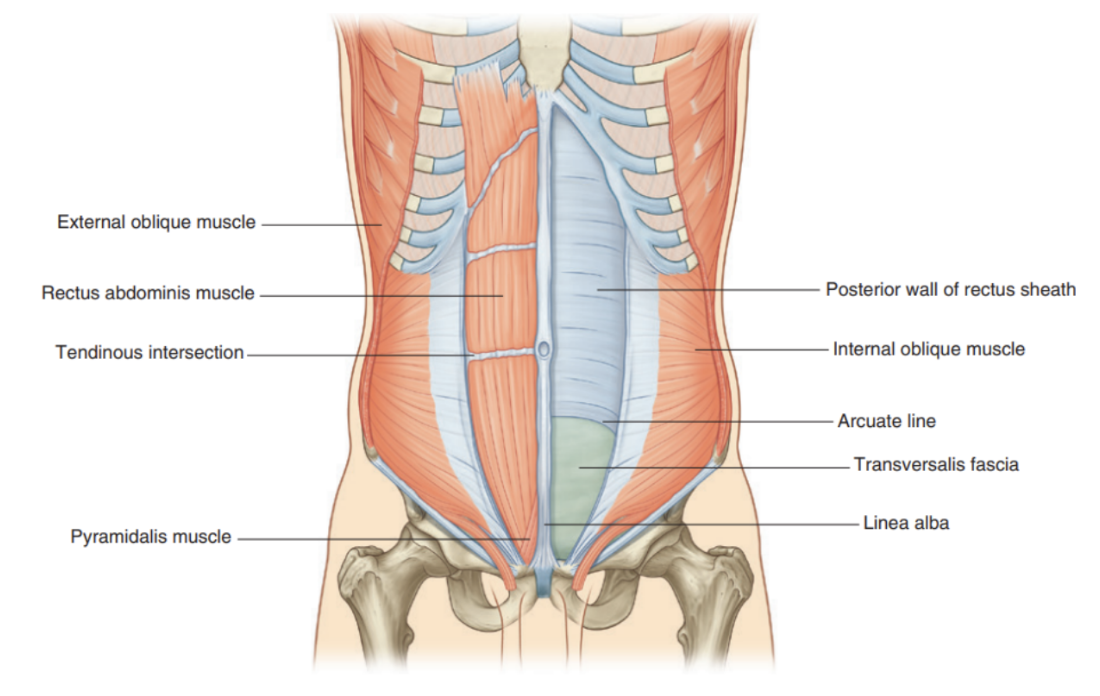
Pyramidalis muscle
Vertical, small triangular muscle lying anterior to rectus abdominis muscle
Can be absent in around 20% of the population
Contained in rectus sheath & originates from bony pelvis, where it is attached to the pubic symphysis & pubic crest through tendinous fibers —
The fibers run superiorly & medially to inert into the linea alba, tensing it during muscular contractions
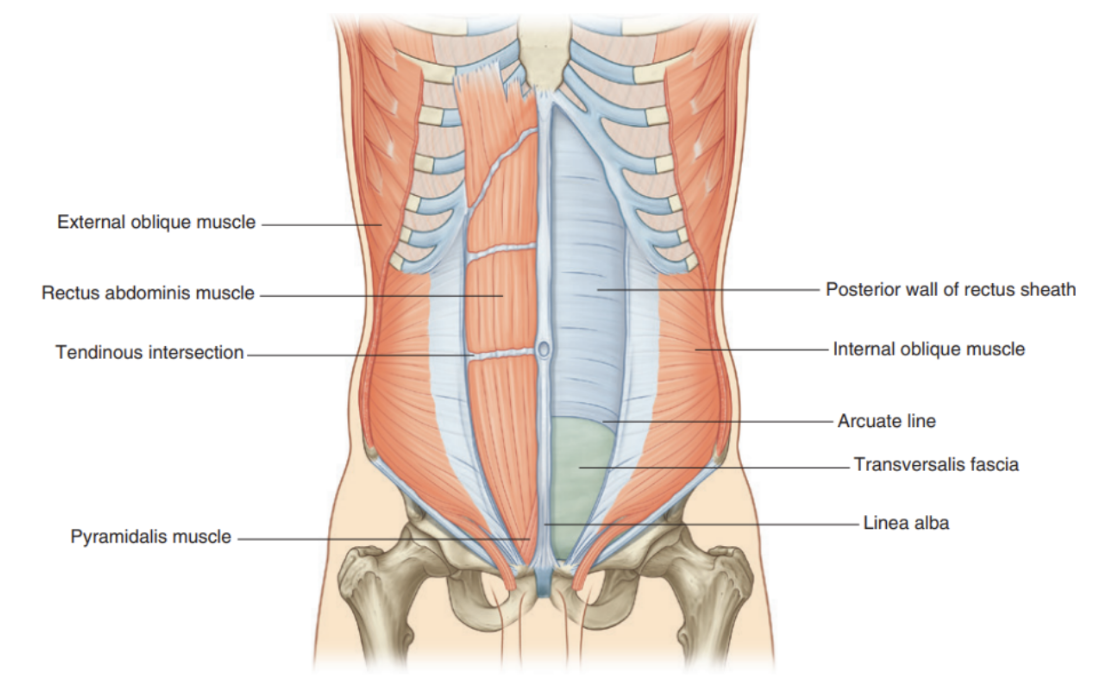
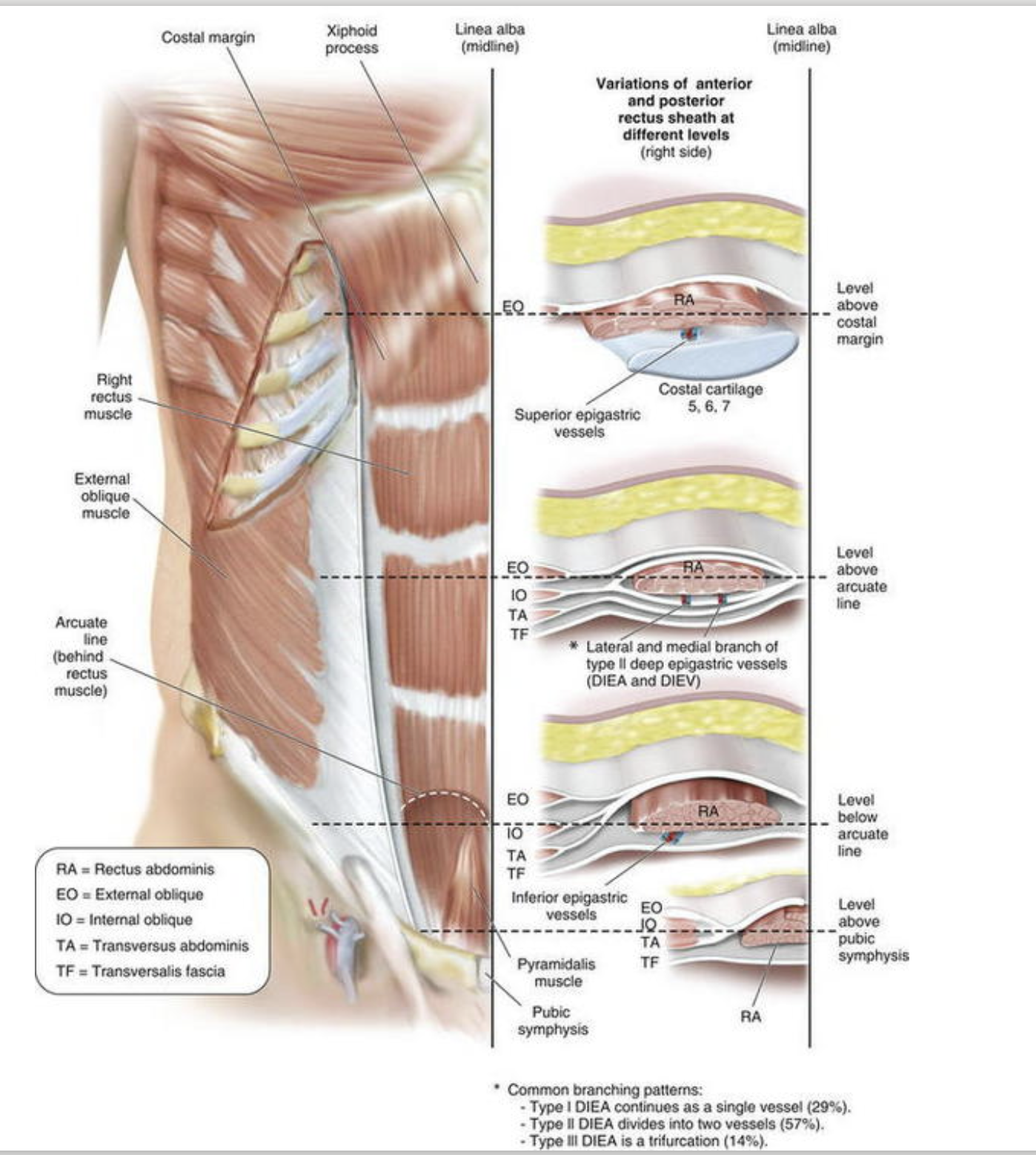
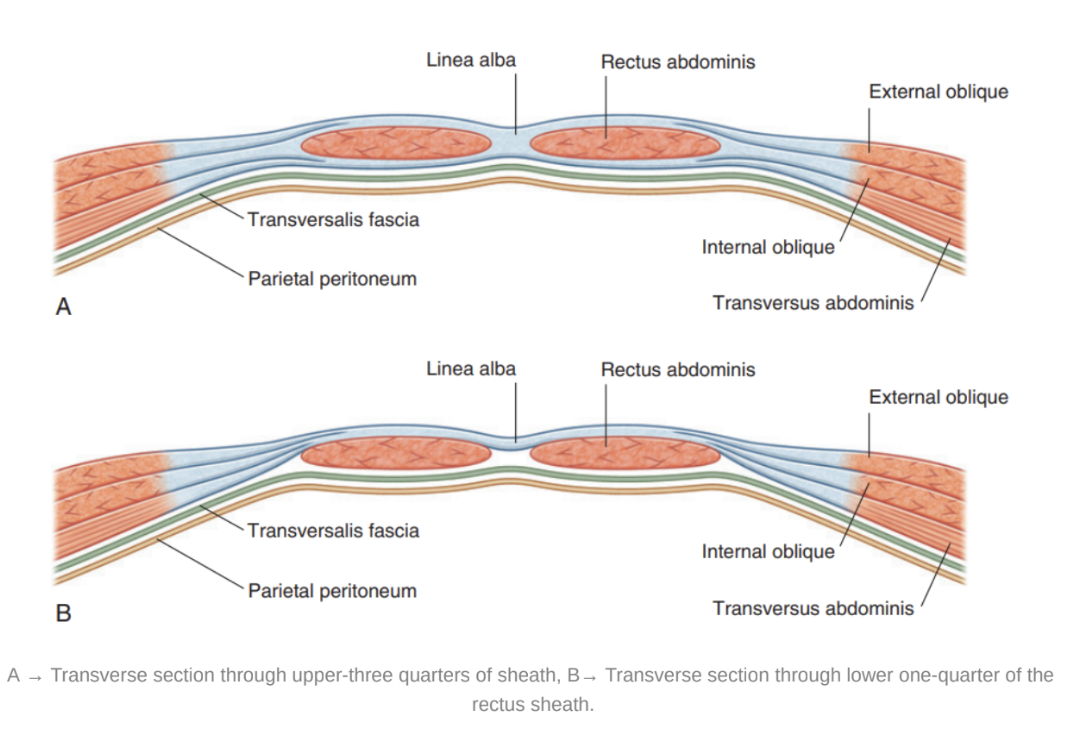
The rectus sheath
Covers both the rectus abominus & pyramidalis and formed by the layering of aponeurosis originating from the 3 flat muscles
Completely encloses the upper 3 quarters of the rectus abdominus & the anterior surface of the lower one quarter of the muscle, at posterior surface muscle is instead contacted by transversalis fascia
Sheath enclosing upper 3/4s has following pattern —
Anterior wall — aponeurosis of external oblique & half of aponeurosis of internal oblique (splits at lateral margin of rectus abdominis)
Posterior wall — other half of aponeurosis of internal oblique & aponeurosis of transversus abdominis
Point of transition between aponeurosis covering both anterior & posterior parts to the only anterior parts is marked by an arch of fibers known as the arcuate line —
Essentially the inferior limit of the posterior layer of rectus sheath is demerated by the horizontal arcuate line
Where the inferior epigastric artery & vein perforate the rectus abdominus
Extraperitoneal fascia
Deep to the transversalis fascia — separates it from the peritoneum
Not only lines the abdominal cavity but also continuous with similar layer lining pelvic cavity
Abundant on posterior abdominal wall (especially around kidneys), continuous over organs covered by peritoneal reflections, and (as vasculature is located in this layer) extends into mesenteries with the blood vessels
Viscera located in the extraperitoneal fascia are referred to as retroperitoneal
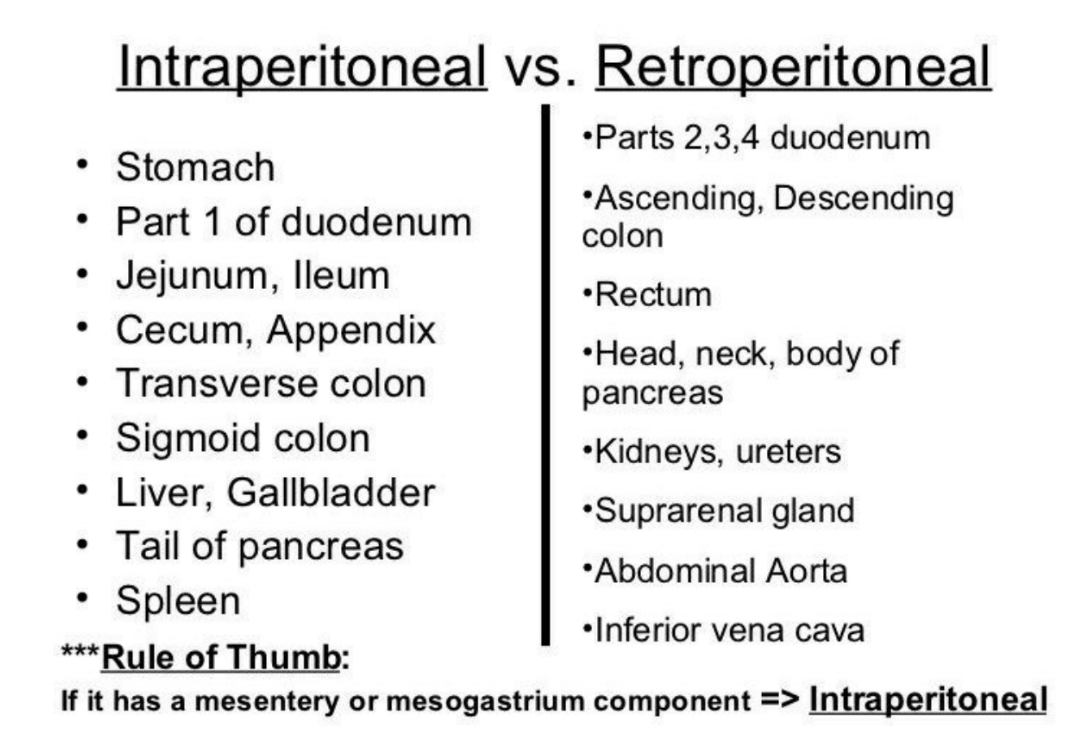
Intraperitoneal vs Retroperitoneal
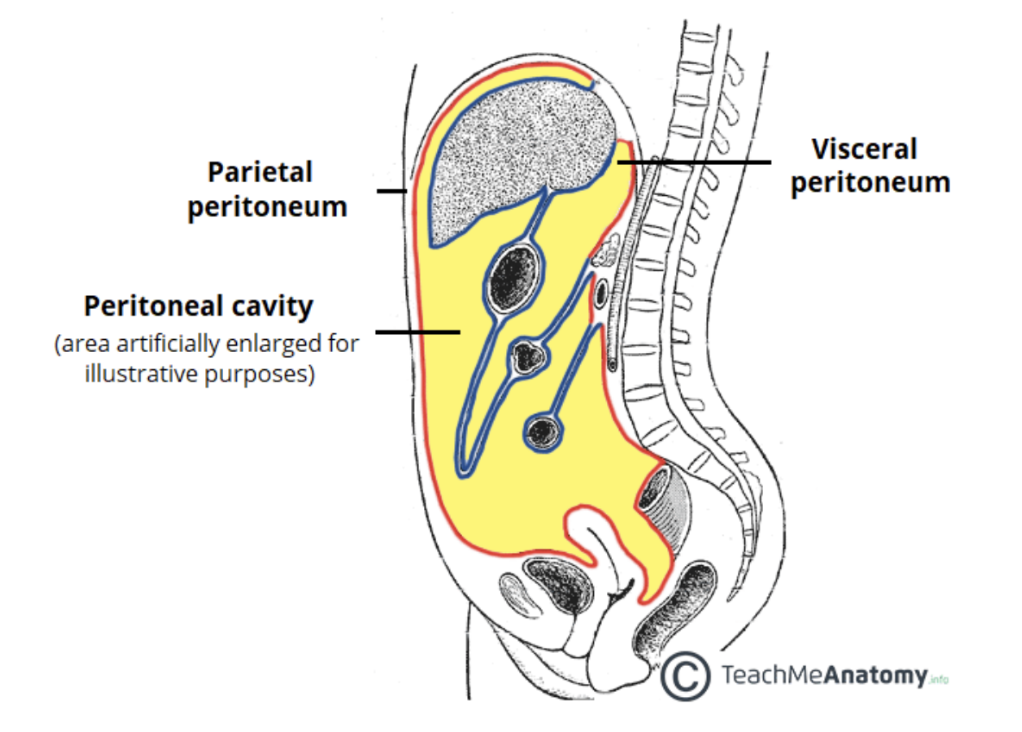
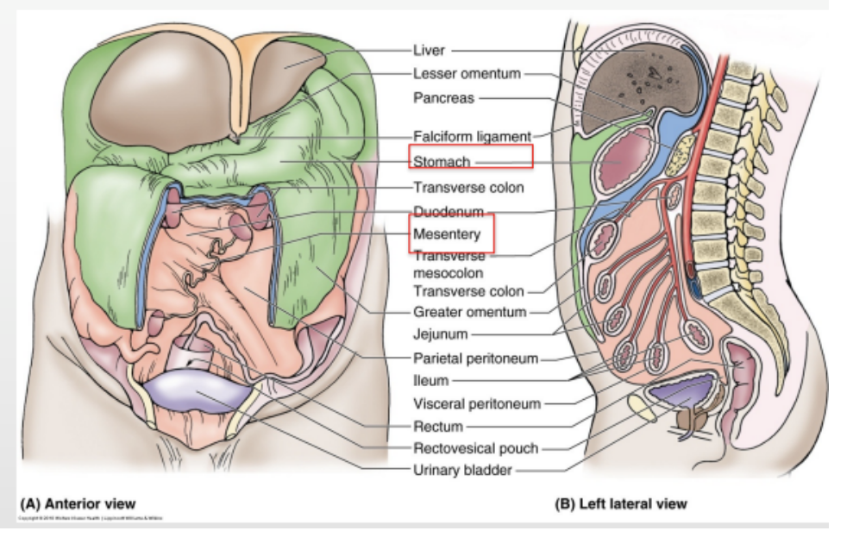
Peritoneum
Deep to extraperitoneal fascia — thin serous membrane that lines the walls of the abdominal cavity & at verious points, reflects onto abdominal viscera in either a complete or partial covering
2 main parts —
Lining walls — parietal peritoneum
Lining viscera — visceral peritoneum
Continuous lining of abdominal walls forms a sac — closed in men but 2 openings in women (where uterine tubes pass outside) — closed sac is called the peritoneal cavity — holds abdominal viscera
Subperitoneal — tissue deep to the peritoneum — includes…
Extraperitoneal space, the ligaments, the mesenteries & their suspended organs
Innervation of peritoneum
Paritetal peritoneum in abdominal wall —
Innervated by somatic afferents carried in branches of the associated spinal nerves
Thus sensitive to well-localized pain
Visceral peritoneum —
Innervated by visceral afferents that accompany autonomic nerves (both sympathetic & parasympathetic) back to the CNS
Activation of these fibers can cause referred & poorly localized feelings of discomfort, and to reflex visceral motor activity
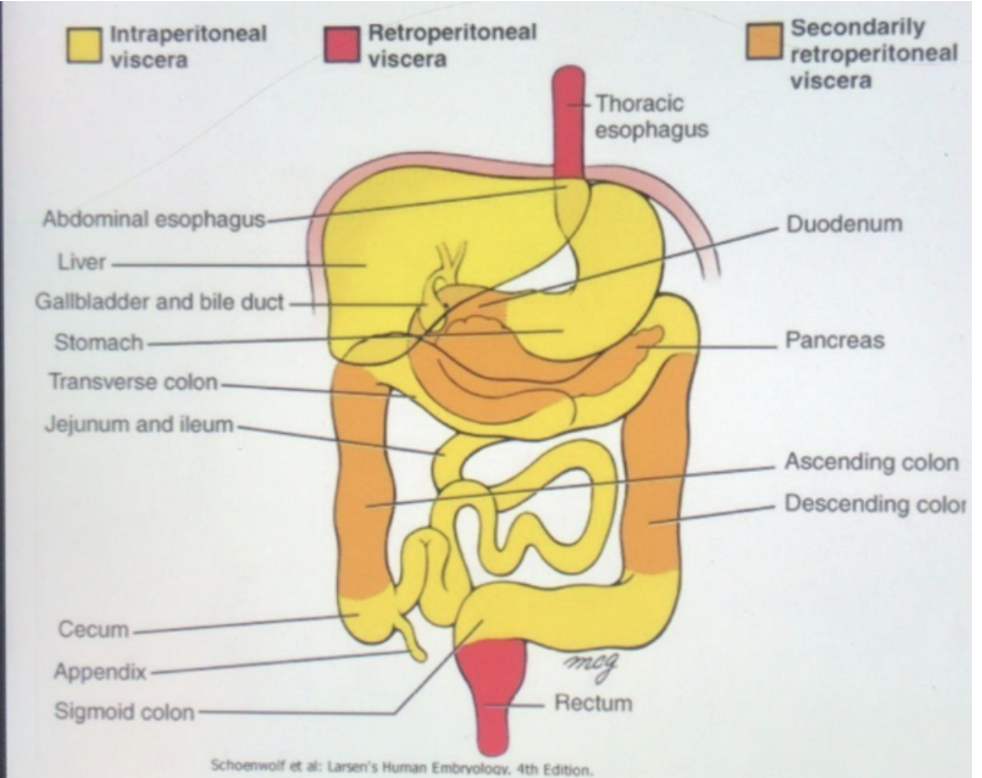
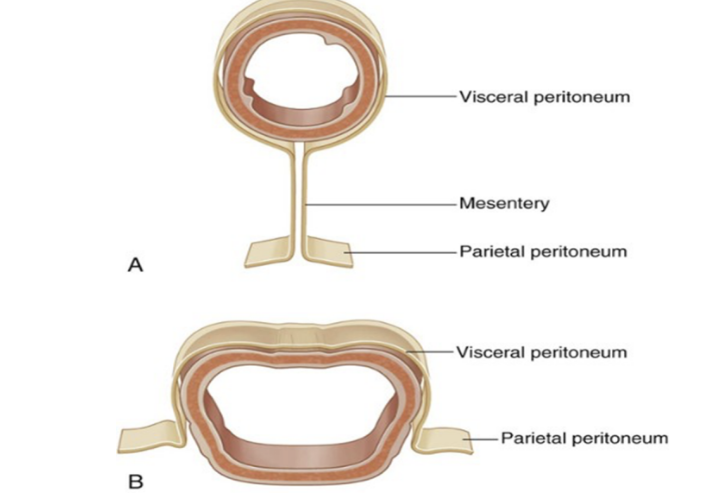
Relation between peritoneum & viscera
Abdominal viscera can be anatomically divided based on their relationship to the peritoneum —
Intraperitoneal organs
Covered by visceral peritoneum, both anteriorly & posteriorly
Ex. stomach, liver, spleen
Usually more mobile, while retroperitoneal are attached to posterior abdominal wall
Retroperitoneal organs
Not associated with visceral peritoneum, only covered in parietal peritoneum on their anterior surface — can be further subdivided -
Primarily retroperitoneal —
Developed & remain outside parietal peritoneum
Ex. esophagus, rectum, & kidneys
Secondarily retroperitoneal
Initially intraperitoneal, suspended by mesentery
During embryogenesis, they became retroperitoneal as their mesentery fused with posterior abdominal wall
Thus, in adults, only their anterior surface is covered with peritoneum
Ex. ascending & descending colon
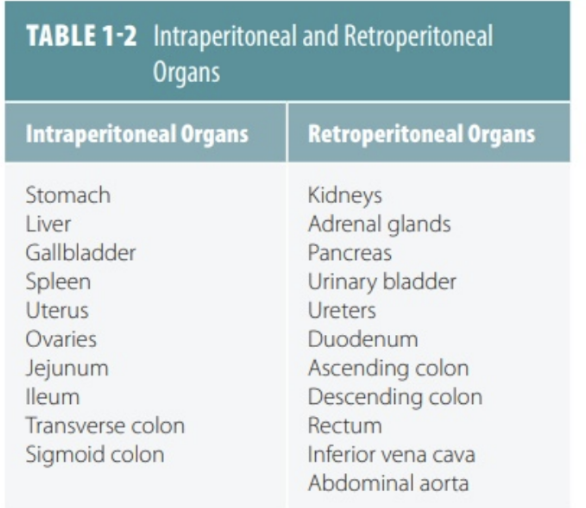
Mnemonic for retroperitoneal organs —
SAD PUCKER —
S = Suprarenal (adrenal) Glands
A = Aorta/IVC
D =Duodenum (except the proximal 2cm, the duodenal cap)
P = Pancreas (except the tail)
U = Ureters
C = Colon (ascending and descending)
K = Kidneys
E = Esophagus
R = Rectum
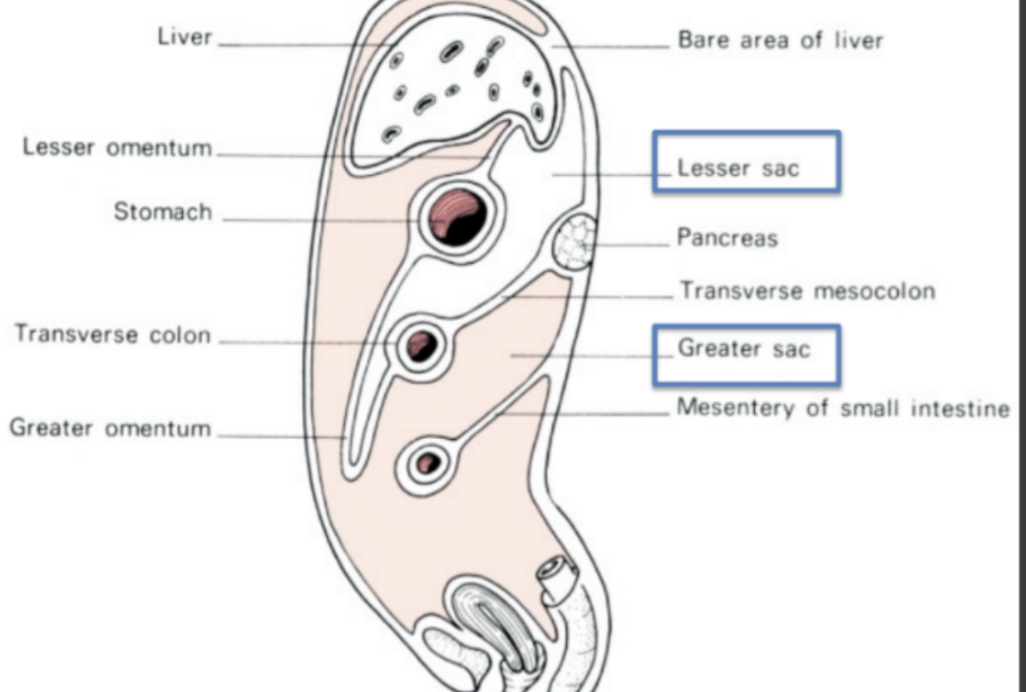
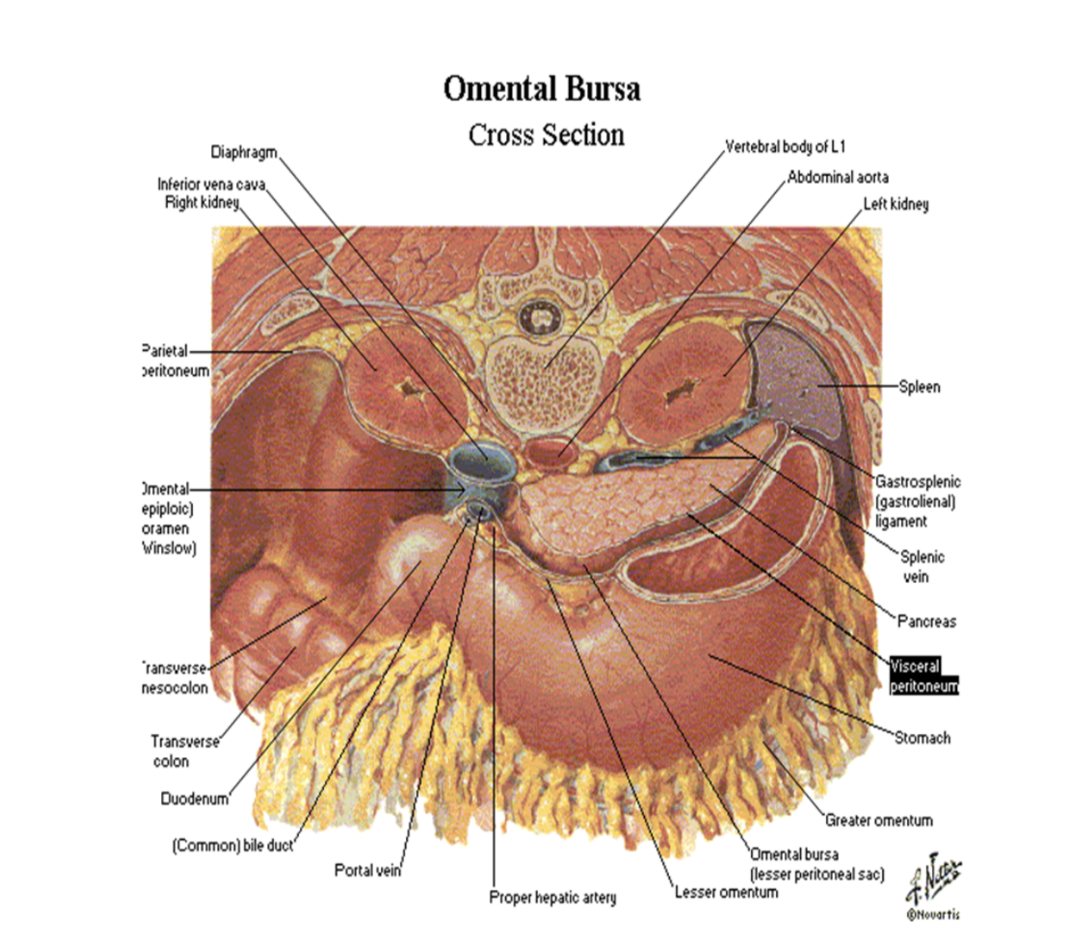
Peritoneal cavity
Subdivided into greater sac & lesser sac (omental bursa)
Greater sac —
Accounts for most of the space — begins superiorly at diaphragm & continues inferiorly into pelvis cavity
Entered by penetrating parietal peritoneaum
Omental bursa (lesser sac) —
Smaller subdivision of the cavity, posterior to stomach & liver
The two are continuous via the omental foramen/foramen of winslow
This foramen is surrounded by numerous structures covered by peritoneum —
Portal vein, hepatic artery proper, & bile duct anteriorly
Inferior vena cava posteriorly
Caudate lobe of liver superiorly
First part of duodenum inferiorly
Peritoneal cavity can also be divided into a supramesocolic & inframesocolic region based on the transverse colon
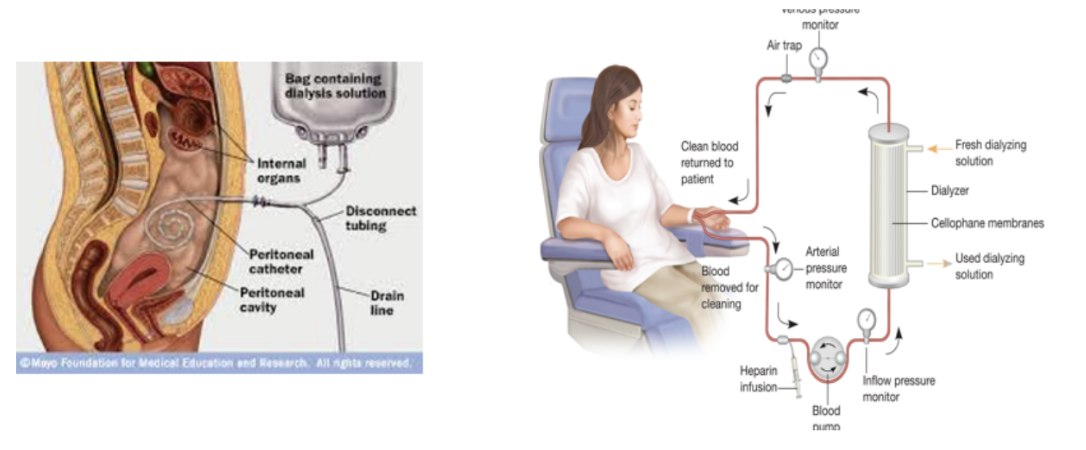
Clinical drop — dialysis
Needed for survival for people with renal failure (kidneys won’t filter blood) — 2 methods —
Hemodialysis —
Blood is taken from the circulation, dialyzed through a complex artificial membrane, & returned to the body
A high blood flow rate is needed to remove excess body fluid, exchange electrolytes, & remove noxious metabolites, which is accomplished by either —
Arteriovenous fistula is established surgically (connecting artery to vein, usually in upper limb (needs 6 weeks to ‘mature’, cannulated each time patient returns for dialysis)
Peritoneal dialysis —
Peritoneum is used as dialysis membrane — large surface area of peritoneal cavity is an ideal dialysis
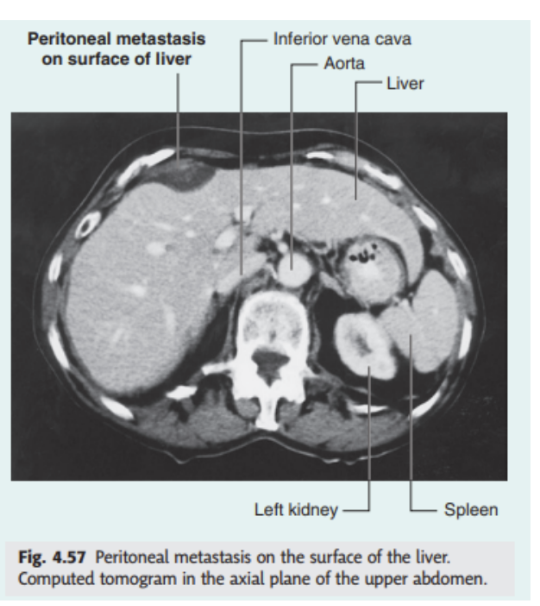
Clinical drop — peritoneal spread of disease
Large surface area of peritoneal cavity allows easy abdominal spread of infection & malignant disease
If malignant cells enter the cavity via direct invasion (ex. from colon or ovarian cancer), spread can be rapid. Similarly, a surgeon excising a malignant tumor & releasing malignant cells into peritoneal cavity can cause a worsening of the patient’s conditions
However, the cavity can also act as a barrier & container for disease — intraabdominal infection tends to remain below the diaphragm rather than spread into other body cavities
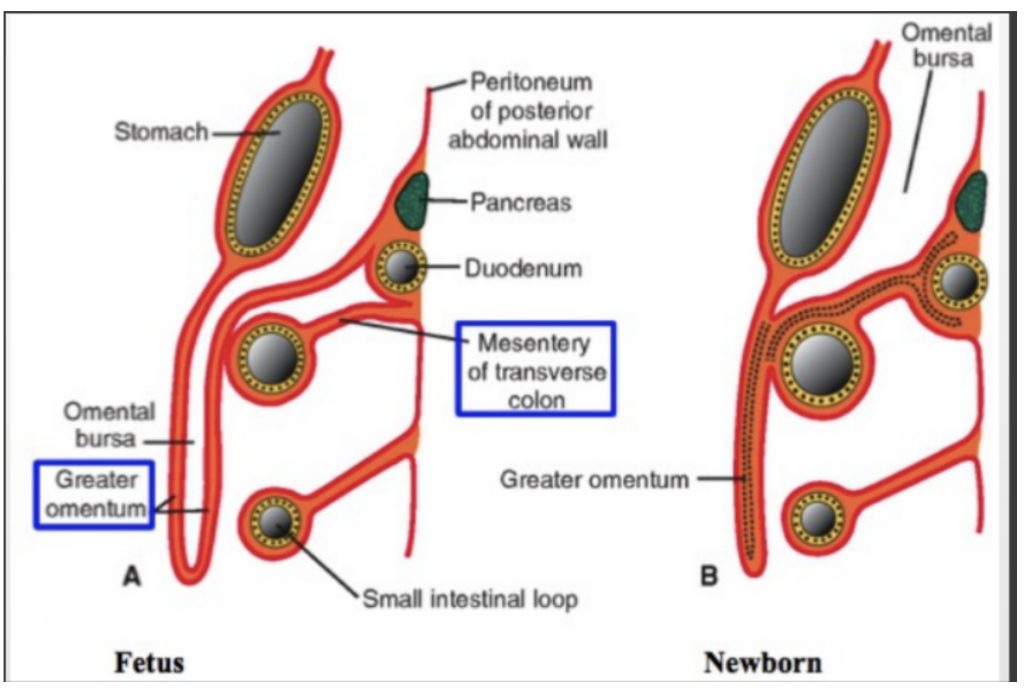
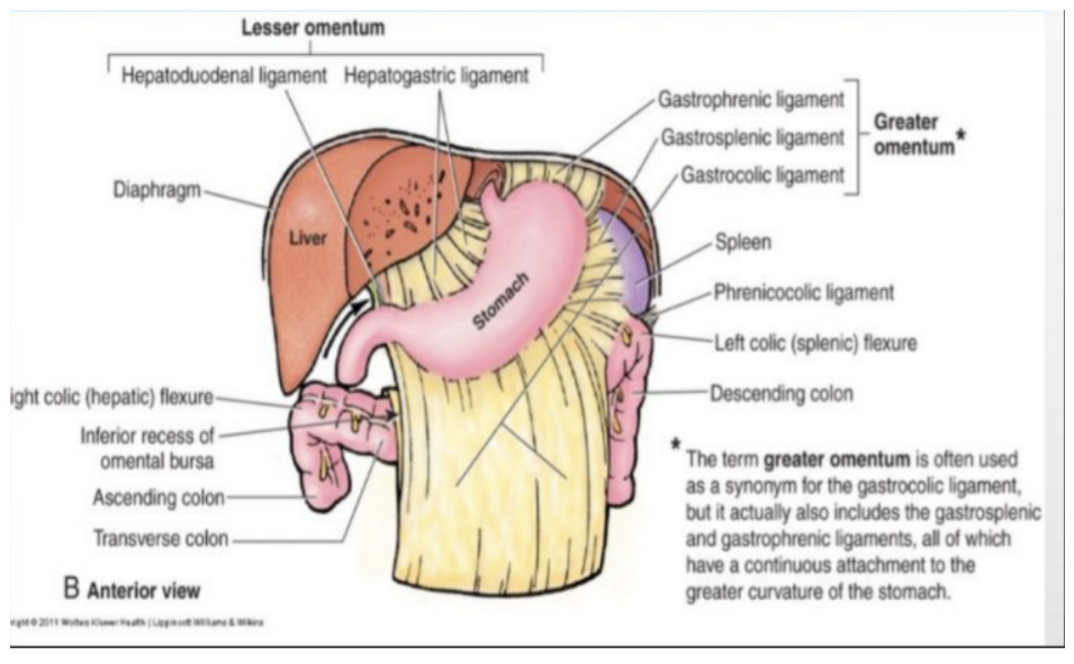
Omenta
2 layers of peritoneum passing from stomach & first part of duodenum to other viscera —
Greater omentum
Large, apron-like peritoneal fold attaching to greater stomach curvature & first part of duodenum. From there it drapes inferiorly over transverse colon, jejunum, & ileum, where it then goes posteriorly to ascend & adhere to the peritoneum on the superior surface of the transverse colon & anterior layer of transverse mesocolon before arriving at posterior abdominal wall
Usually a thin membrane but always contains an accumulation of fat, which can become substantial in some individuals
2 arteries & veins — right & left gastro-omental vessels — between double-layered peritoneal apron just inferior to greater curvature of stomach
Gastrophrenic, gastrosplenic, gastrocolic ligaments
Lesser omentum
Thin membrane that extends from lesser stomach curvature & first part of duodenum to inferior liver surface
Divided into —
Medial hepatogastric ligament
Passes between stomach & liver, ends laterally as a free margin & serves anterior border of omental foramen
Holds the hepatic artery proper, bile duct, & portal vein
Lateral hepatoduodenal ligament — passes between duodenum & liver
Right & left gastric vessels are between layers of lesser omentum near the lesser curvature of the stomach
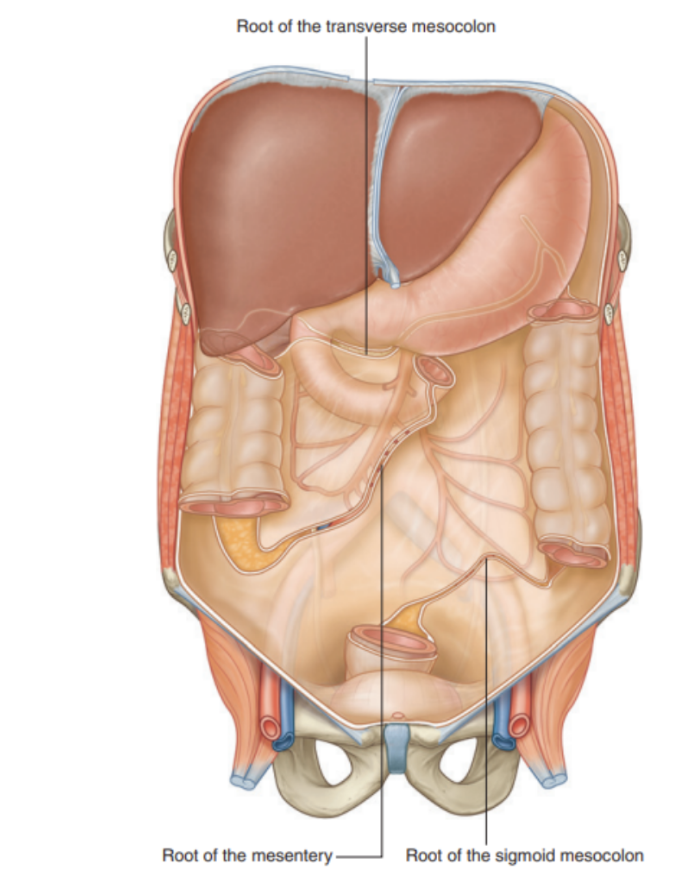
Mesenteries
Peritoneal folds attaching viscera to the posterior abdominal wall
Allow some movement & provide a conduit for vessels, nerves, and lymphatics to reach the viscera
Include —
Mesentery Proper —
Associated with parts of small intestine
Transverse mesocolon —
Associated with transverse colon
Sigmoid mesocolon —
Associated with the sigmoid colon
All of these are derivatives of the dorsal mesentery
Mesentery proper
Mesentery of the small intestine — broad & large fan-shaped mesentery attaching jejunum & ileum to posterior abdominal wall
Superiorly attached to the duodenojejunal junction, just to the left of L2
Runs obliquely down to terminate & attaches to ileocecal junction, by the right sacro-iliac joint
The blood vessels, lymphatics, & nerves required to supply the jejunum & ileum are found between the 2 layers of the peritoneum that make up the mesentery of the small intestine
Transverse mesocolon
Fold of peritoneum that connects the transverse colon to the posterior abdominal wall
2 layers of peritoneum leave the posterior abdominal wall across anterior surface of head & body of pancreas and pass outward to surround the transverse colon
Between its layers are arteries, veins, nerves, & lymphatics related to transverse colon
Anterior layer of transverse mesocolon is adherent to the posterior layer of the greater omentum
Sigmoid mesocolon
An inverted, V-shaped peritoneal fold attaching sigmoid colon to abdominal wall
Apex of the V is near the division of the left common iliac artery into its internal & external branches, with the left limb of the descending V along the medial border of the left psoas major muscle & the right limb descending into the pelvis to end at SIII
Sigmoid & superior rctal vessels, along with nerves & lymphatics associated with sigmoid colon, pass through this peritoneal fold
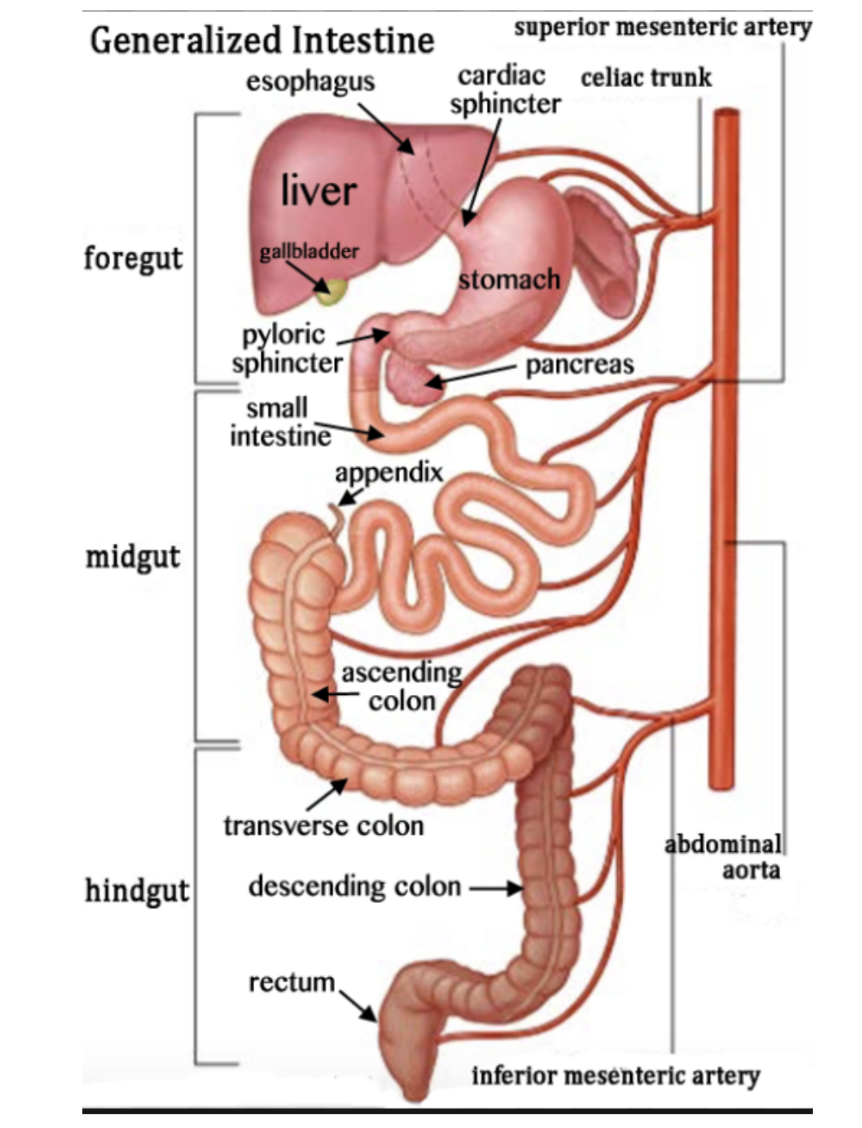
Note on vascularization of abdomen
Each is vascularized by distinct branches of aorta (vessels can be paired or single)
Foregut — Celiac artery (CNX)
Midgut — Superior mesenteric artery (CNX)
Hindgut — Inferior mesenteric artery (Pelvis Splanchnic)
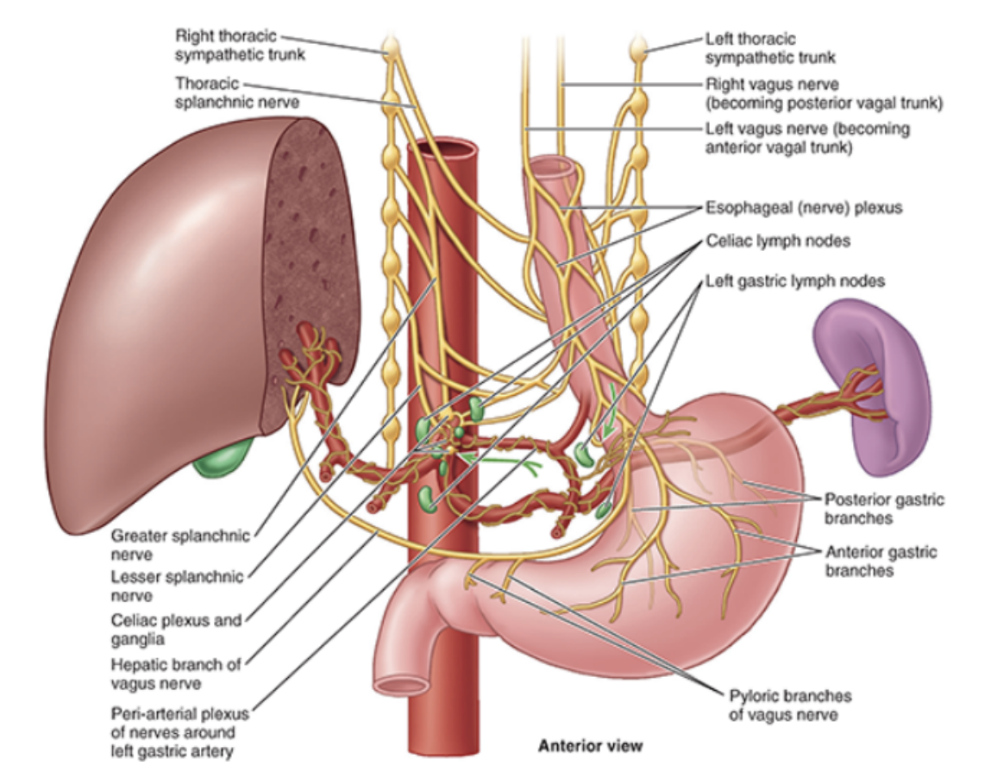
Abdominal esophagus (+ vagal trunks + vascularization)
Short distal part of esophagus in abdominal cavity
Emerges through right crus of diaphragm, usually around T10, passing from esophageal hiatus to cardial orifice of the stomach just left of the midline
Associated with the esophagus, as it enters the abdominal cavity, are the anterior & posterior vagal trunks —
Anterior vagal trunk — Consists of several smaller trunks whose fibers mostly come from the left vagus nerve — rotation of gut during development moves these trunks to the anterior esophageal surface
Posterior vagal trunk — A single trunk whose fibers mostly come from right vagus nerve, with rotational changes during development moving it to posterior esophageal surface
Arterial supply —
Esophageal branches from left gastric artery, from celiac trunk
Esophageal branches from left inferior phrenic artery, from aorta
Venous drainage — 2 routes
To hepatic portal venous system through left gastric vein
To systemic venous system through esophageal veins entering azygos vein
Esophagogastric Junction
Lies left of T11 on horizontal plane passing through tip of xiphoid process
Surgeons & endoscopists designate the Z-line a jagged line where mucosa abruptly changes from esophageal to gastric — thus junction
Immediately superior, musculature of right crus of diaphragm forming esophageal hiatus functions as an extrinsic physiological inferior esophageal sphincter that contracts/relaxes, along with a variabely thickened muscular coat around cardial orifice of stomach
Radiologic studies shows that food moemntarily stops here with sphincter mechanism preventing reflux of gastric contents into esophagus — when one is not eating, lumen of esophagus is normally collapsed superior to this level to prevent food or stomach juices from regurgitating into esophagus
This region is very clinically relevant as it is a very common site of tumors/metaplasia — barrett’s esophagus
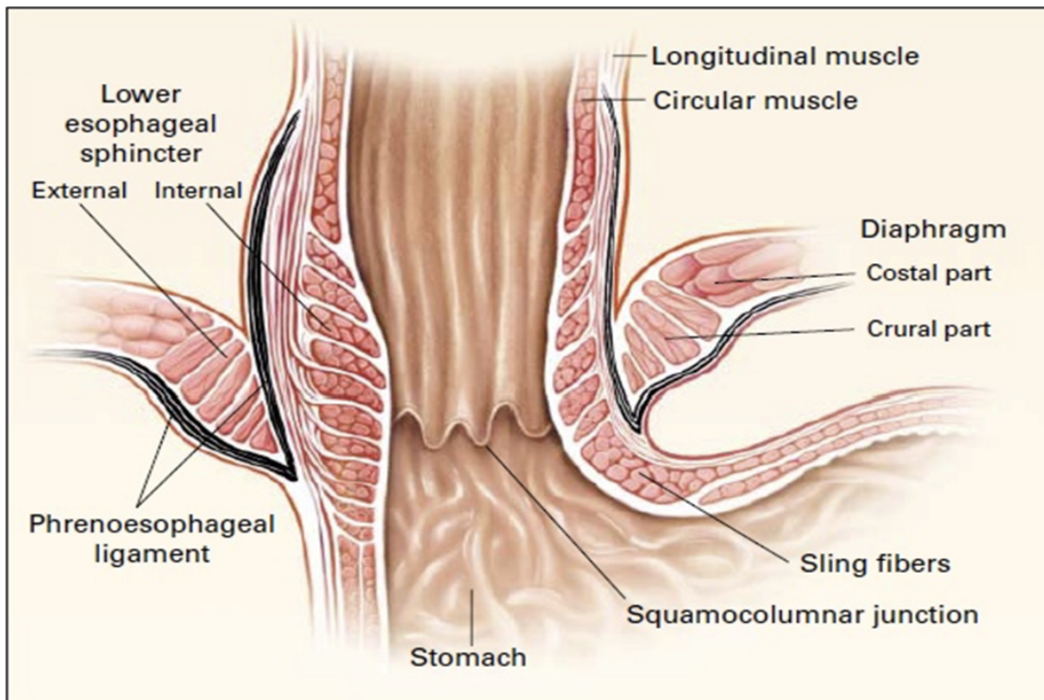
Clinical drop — Barrett’s esophagus
In certain conditions, like gastroesophageal reflux, the stratified squamous epithelium in the esophagus can undergo metaplasia & epithelium in lower esophagus is replaced by columnar epithelium — Barrett’s esophagus
This condition predisposes these people to the development of esophageal malignancy (adenocarcinoma)
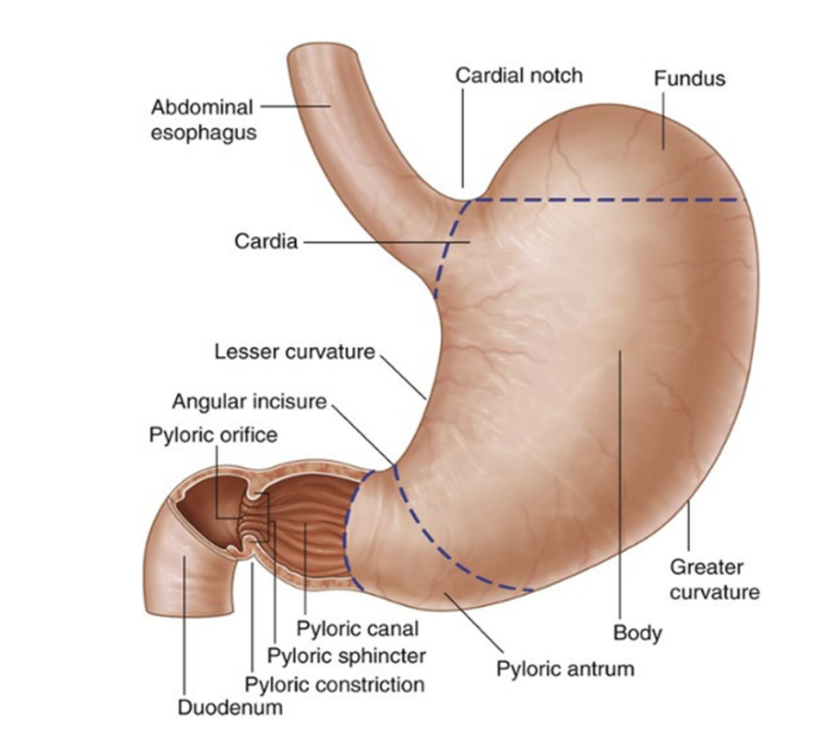
The stomach
Most dilated part of GI tract — J-like shape
Positioned between abdominal esophagus & small intestine, in the epigastric, umbilical, & left hypochondrium regions of the abdomen
Divided into 4 regions —
Cardia (opening of esophagus), fundus (area above cardial orifice), body (largest), and pyloric (further divided into pyloric antrum & canal — distal end)
Most distal portion of pyloric part — pyloris
Marked on surface of organ by pyloric constriction with a thickened ring of gastric circular muscle — pyloric sphincter — surrounding distal opening of the stomach — pyloric orifice (just right of midline at level L1 (transpyloric plane))
Curvatures —
Greater — attachment for gastrosplenic ligament & greater omentum
Lesser — attachment for lesser omentum
Other features —
Cardiac notch — superior angle created where esophagus enters stomach
Angular incisure — bend on lesser curvature
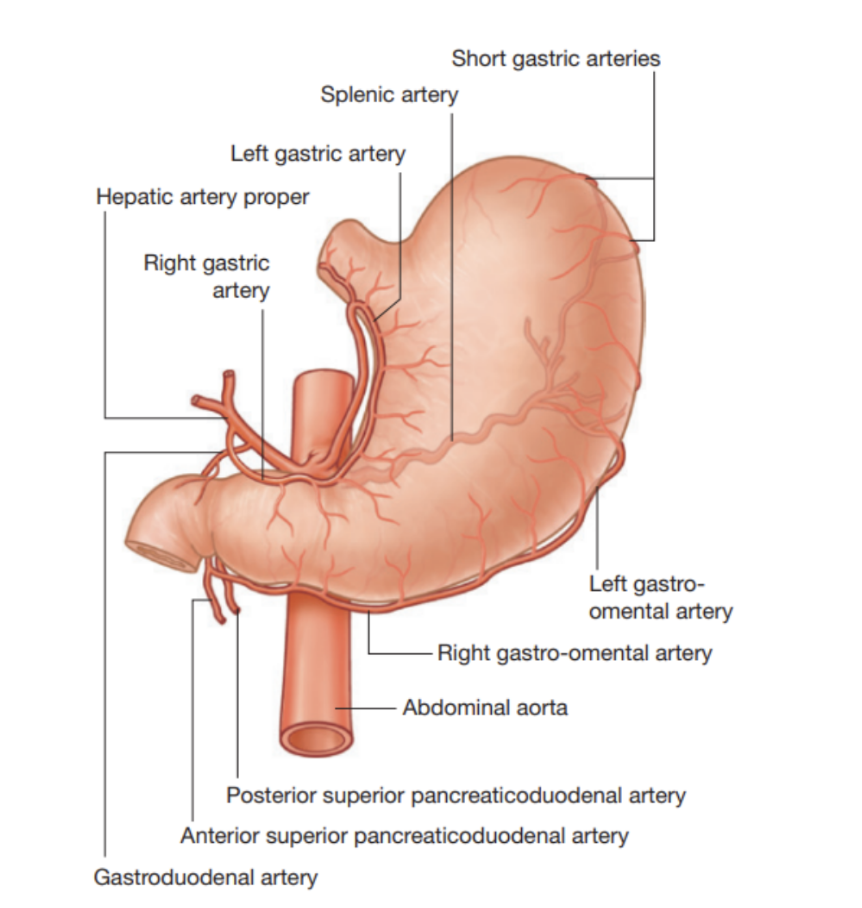
Arterial supply to stomach
Mostly supplied by anastomoses formed along lesser curvature by the right & left gastric arteries, and along greater curvature by right & left gastro-omental (gastroepiploic) arteries, with fundus & upper body receiving blood from short & posterior gastric arteries
Specifically —
Left gastric artery from celiac trunk
Right gastric artery, often from hepatic artery proper
Right gastro-omental artery from gastroduodenal artery
Left gastro-omental artery from splenic artery
Posterior gastric artery from splenic artery (variant)
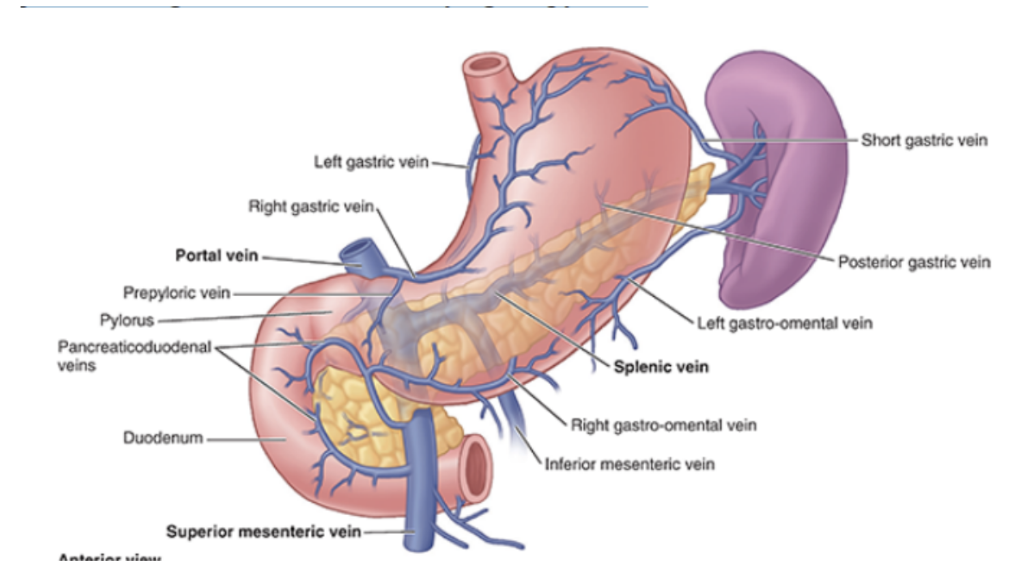
Venous drainage of stomach
Parallel arteries in position & course —
Right & left gastric veins drain into hepatic vein
Short gastric & left gastro-omental veins drain into splenic vein (which joins superior mesenteric vein (SMV) to from hepatic portal vein)
Right gastro-omental vein empties into SMV
Prepyloric vein ascends over pylorus to right gastric vein
Important vein — surgeons use to identify the pylorus
Relations of the stomach
Stomach is covered by visceral peritoneum everywhere except where blood vessels run along its curvatures & in a small area posterior to the cardial orifice
The 2 layers of lesser omentum extend around stomach & leave its greater curvature as the greater omentum
Anteriorly, stomach is related to diaphragm, left lobe of liver, & anterior abdominal wall
Posteriorly, stomach is related to omental bursa & pancreas —
Posterior surface of stomach forms majority of anterior wall of omental bursa (lesser sac)
Transverse colon is related inferiorly & laterally to stomach as it courses along the greater curvature of the stomach to the left colic flexure
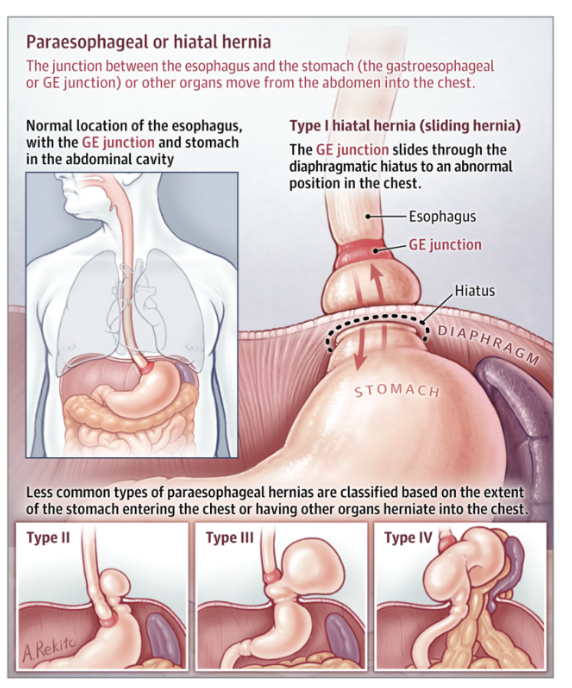
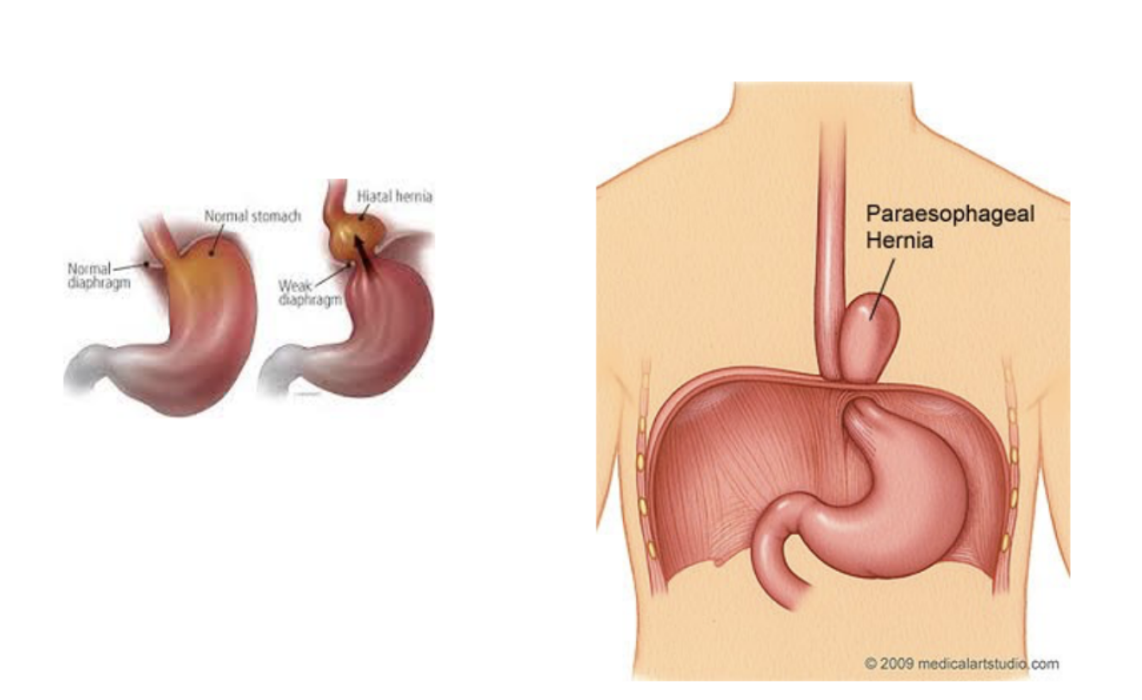
Clinical drop — Hiatal hernia & paraesophageal hernia
Occurs when part of the stomach slides through esophageal hiatus (opening of diaphgram) — 2 types —
Paraesophageal —
Fundus of stomach herniates — no reflux (cardia remains in normal position)
Sliding hital —
Reflux — esophagus & cardia slide through hiatus
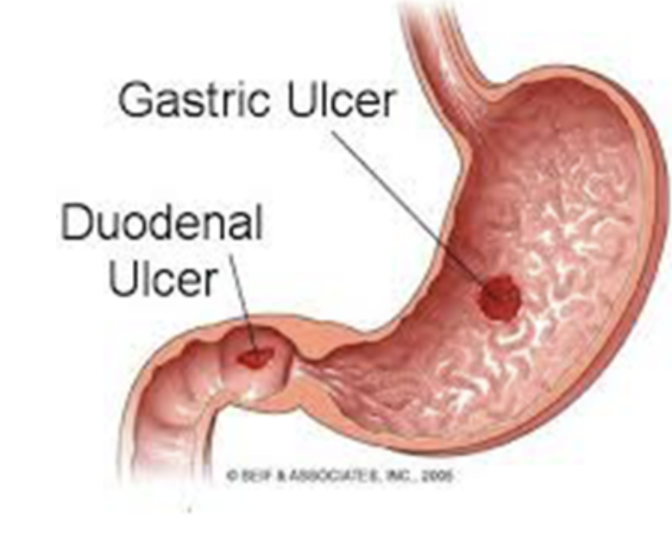
Clinical drop — peptic ulcurs
Involve mucosal lining of stomach/duodenum (first layer of inner lining)
In chronic condition can reach submucosal layer & sometimes even serosa
Commonst cause — Helicobacter Pylori infection, but also due to gastric acid overproduction
Duodenal ulcers can either be anterior or posterior
Posterior duodenal ulcers —
Erode either directly onto gastroduodenal artery or, more commonly, onto posterior pancreaticoduodenal artery (can produce torrential hemorrhage — can be fatal)
Treatment — extensive upper abdominal surgery with ligation of vessels or endovascular means (radiologist places very fine catheter retrogradely from femoral artery into celiac artery
Common hepatic & gastroduodenal artery are cannulated & bleeding area may be blocked using small coils, stemming blood flow
Anterior duodenal ulcurs —
Erode into peritoneal cavity, causing perionitis — this intense inflammatory reaction along with local ileus promote ahesion of the greater omentum, which attempts to seal off the perforation
Stomach & duodenum usually contain gas, which will enter the peritoneal cavity (can be observed on chest radiograph of an erect patient as subdiaphragmatic gas)
In most instances, treatment is surgical
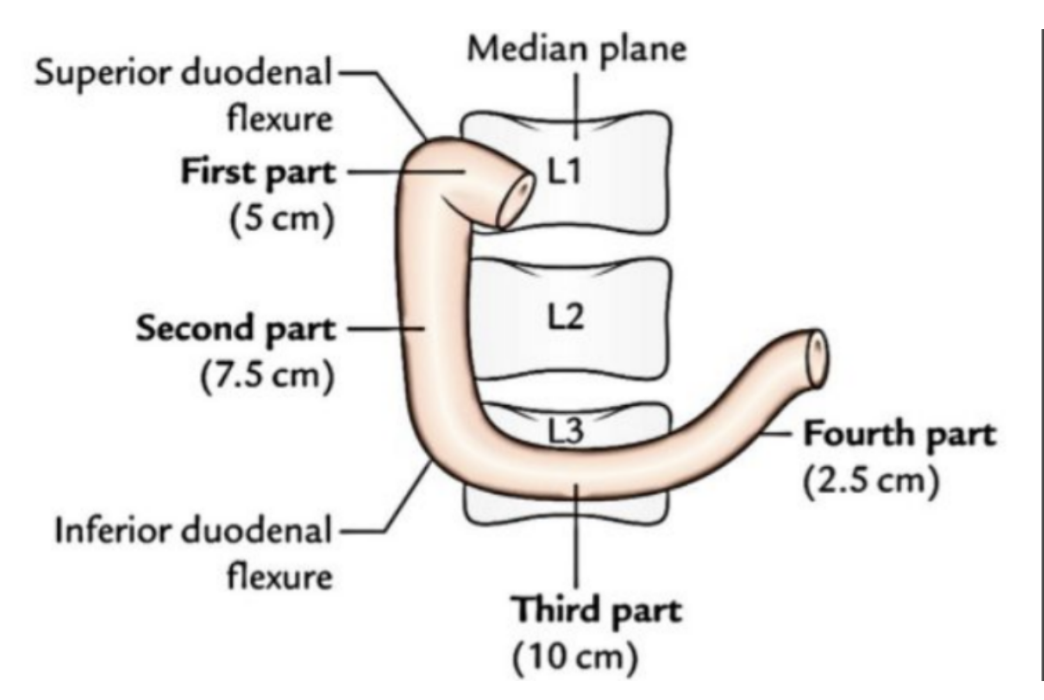
Duodenum
First part of small intestine — C-shaped structure, adjacent to head of pancreas, 20-25cm length, above head of umbilicus
Lumen is widest of all small intestine and it is retroperitoneal, except its beginning — connected to liver via hepatoduodenal ligament (part of lesser omentum)
Can be divided into 4 parts —
Superior (spinal level L1) —
Ascends upwards from pylorus of stomach, connected to liver via hepatoduodenal ligament — most common site f duodenal ulceration
The initial 3 cm of superior duodenum is covered both anteriorly & posteiorly by visceral peritoneam, with the remainder retroperitoneal (only covered anteriorly)
Descending (L1-L3) —
Curves inferiorly around head of pancreas, lying posteriorly to transverse colon & anterior to right kidney
Internlly marked by major duodenal papilla — where bile & pancreatic secretions enter from ampulla of Vater
Inferior (L3) —
Travels laterally to the left, crossing over inferior vena cava & abdominal aorta — inferiorly to the pancreas & posteriorly to superior mesenteric artery/vein
Ascending (L3-L2) —
After crossing aorta, it ascends & curves anteriorly to join jejunum at a sharp turn — duodenojejunal flexure
Located at duodenojejunal junction — suspensory muscle of duodenum
Widens angle of flexure & aids movement of intestinal contents into jejunum
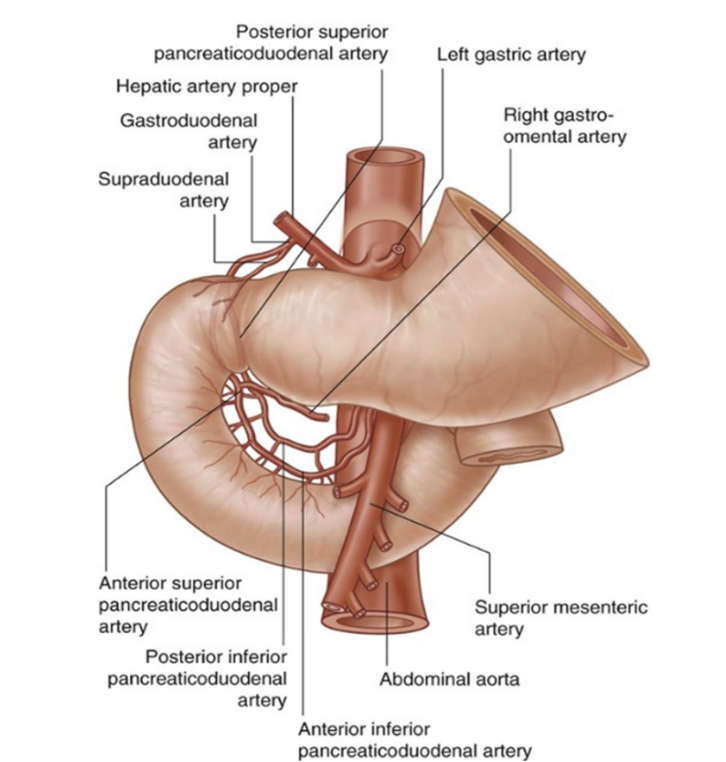
Vascularization of duodenum
Arterial supply —
Supplied proximally by a branch of common hepatic artery — gastroduodenal artery — stems from celiac trunk & gives off anterior & posterior superior pancreaticoduodenal arteries
Also receives blood distally from anterior & posterior inferior pancreaticoduodenal arteries — branches of superior mesenteric artery
Terminal branches of duodenal arteries form important anastomoses between celiac trunk & superior mesenteric artery
Venous drainage —
Duodenal veins — drain directly from duodenum into pancreaticoduodenal veins
From here, they merge back into the superior mesenteric vein & common hepatic vein
(ant & post sup. coming from hepatic, ant & post inf. coming from SMV
Generally follow arteries in this region and all drain either directly or indirectly into the portal vein
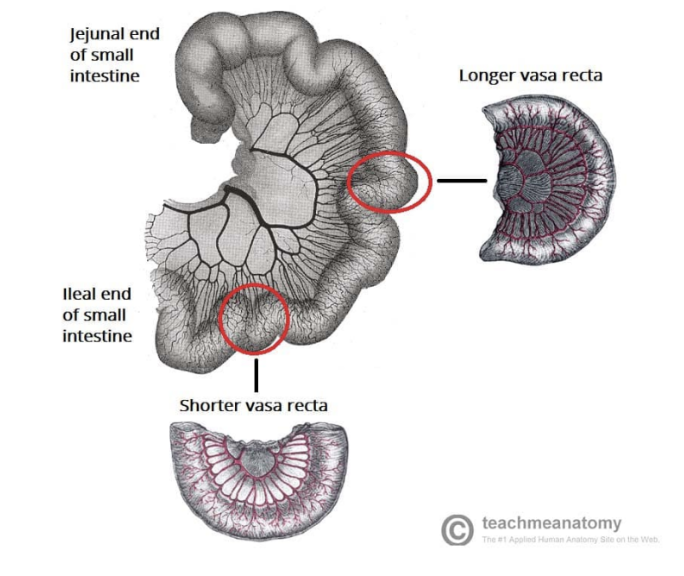
Jejunum —
Makes up proximal 2/5ths of last 2 sections of small intestine — mostly in left upper quadrant in abdomen, with a larger diameter & thicker wall than ileum
Additionally, inner mucosal lining is characterized by numerous prominent folds circling the lumen — plicae circulares
Has less prominent arterial arcades and longer vasa recta (straight arteries) compared to those of the ileum
Vascularixation —
Jejunal arteries from SMA
Jejunal veins to SMV
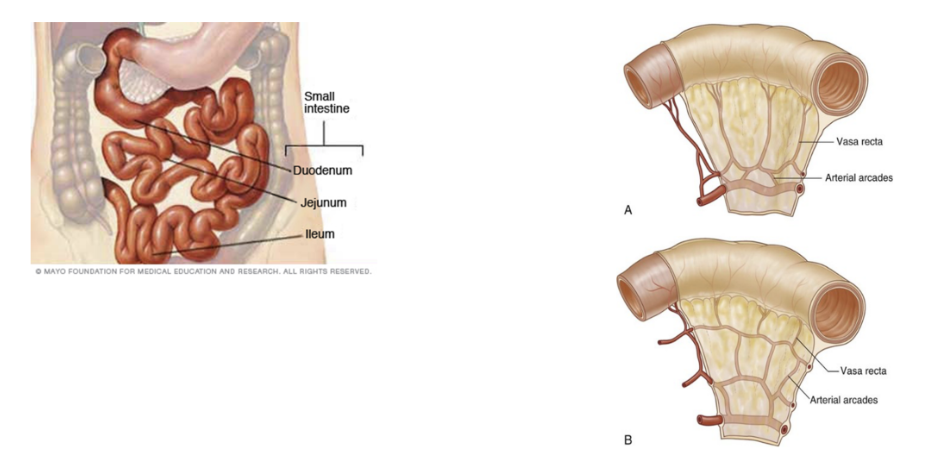
Ileum —
Makes up distal 3/5ths of small intestine — mostly in lower right quadrant
Thinner walls, fewer/less prominent plicae circulares, shorter vasa recta, more mesenteric fat, and more arterial arcades as compared to jejunum
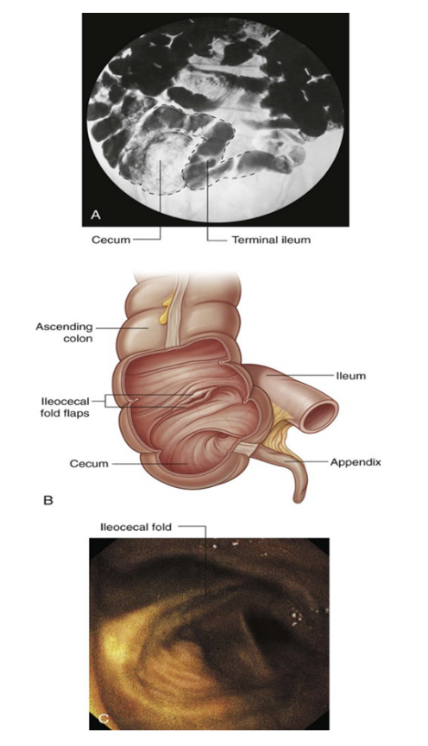
Opens into large intestine, where cecum & ascending colon join together, with the ileocecal fold (2 flaps projecting into large intestine lumen) surrounding the opening — Ileocecal valve
The flaps of the ileocecal fold come together at their end, forming ridges, with musculature from the ileum continues into each flapp — forming a sphincter
Functions to prevent reflex from cecum to ileum (during peristalsis), and regulating passage of contents from ileum to cecum
Thought to function passively, as opposed to a defined muscular sphincter
Vascularization —
Arterial —
Ileal arteries from SMA
Ileal branch from ileocolic artery, from SMA
Venous —
SMV formed by small terminal veins small terminal veins that drain the ileum, cecum, & vermiform appendix
SMV runs superomedially, traversing mesentery of small intestine
Large intestine
Extends from distal end of ileum to anus — 1.5m in adults
Absorbs fluids & salts from gut contents, thus forming feces
Consists of cecum, appendix, colon, rectum, & anal canal
Begins in right groin as cecum along with its associated appendix. Continues upwards as ascending colon into right hypochondrium, and bends to the left just below liver, forming right colic (hepatic) flexure, crossing abdomen as transverse colon into left hypochondrium. Just below spleen, bends downwards, forming left colic (splenic) flexure, continuing as descending colon into left groin
Enters upper part of pelvic cavity as sigmoid colon, continuing on posterior wall as rectum, and terminates as anal canal
General features —
Large internal diameter as compared to small intestine
Peritoneal-covered accumulations of fat (omental appendices) associated with the colon
Segregation of longitudinal muscle in its walls into 3 narrow bands (teniae coli) — primarily observed in cecum & colon, less visible in rectum
Sacculations (haustra) of the colon
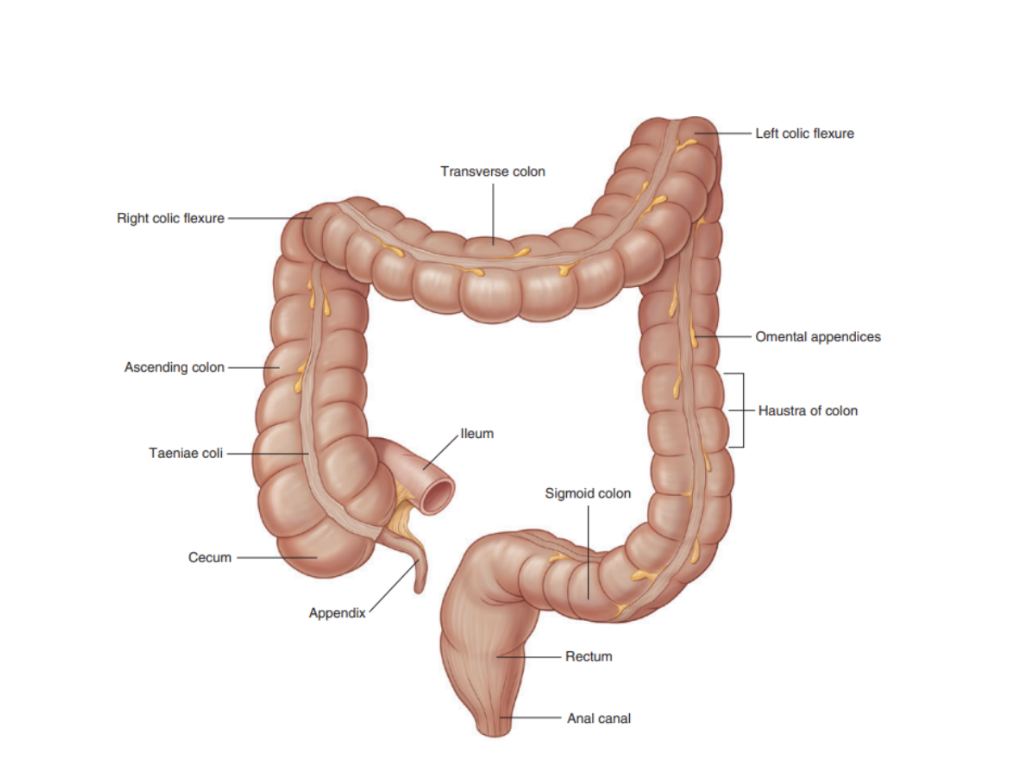
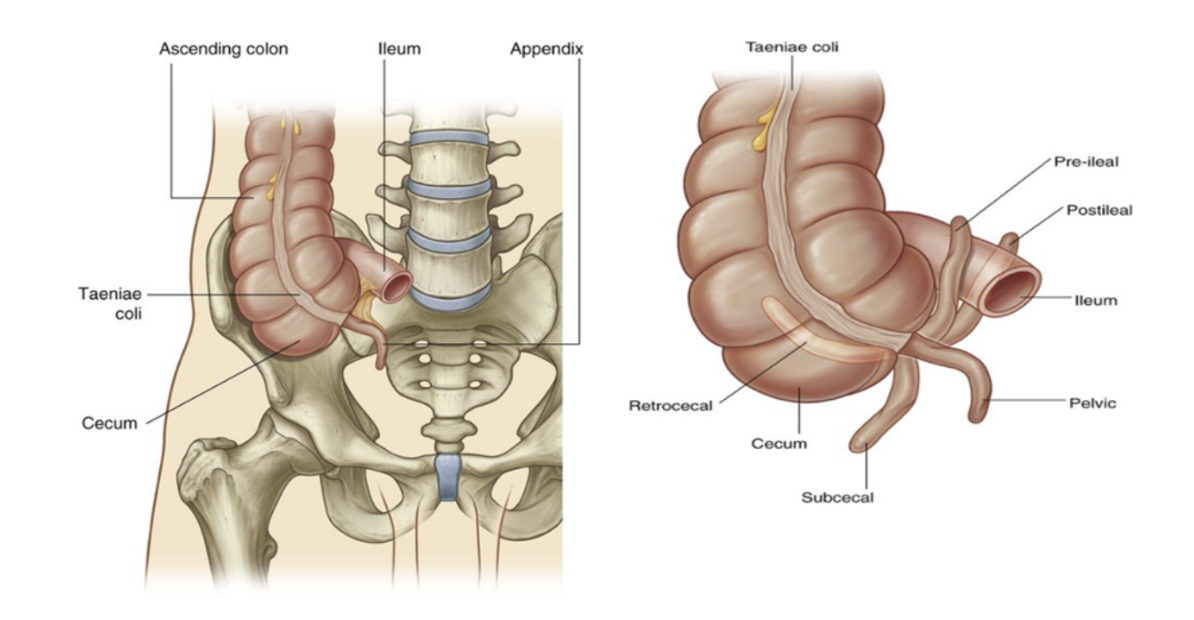
Cecum & appendix
Cecum —
First part of large intestine, inferior to ileocecal opening in the right iliac fossa
Generally considered intrapertitoneal due to its mobility, although normally not suspended by a mesentery
Continuous with ascending colon at enterance of ileum & usually in contact with anterior abdominal wall
May cross pelvic brim to lie in true pelvis
Appendix —
Attached to posteromedial wall of cecum, just inferior to end of ileum
A narrow, hollow, blind-ended tube connected to cecum with large aggregations of lymphoid tissue in its walls
Suspending by mesoappendix, containing appendicular vessels
Its point of attachment to the cecum is consistent with the highly visible free taeniae leading directly to the base of the appendix, but the location of the rest of the appendix varies heavily — can be —
Posterior to cecum or lower ascending colon (or both) in a retrocecal or retrocolic position
Suspended over pelvis brim in a pelvic or descending position
Below the cecum in a subcecal position
Anterior to the terminal ileum, possible contacting body wall, in a pre-ileal position or posterior to terminal ileum in a post-ileal position
Surface projection of its base is at the junction of lateral & middle 1/3 of a line from anterior superior iliac spine to umbilicus — McBurney’s point — people with appendicular issues may have pain here
Arterial supply —
Anterior cecal artery from ileocolic artery from SMA
Posterior cecal artery from ileocolic artery from SMA
Appendicular artery from ileocolic artery from SMA
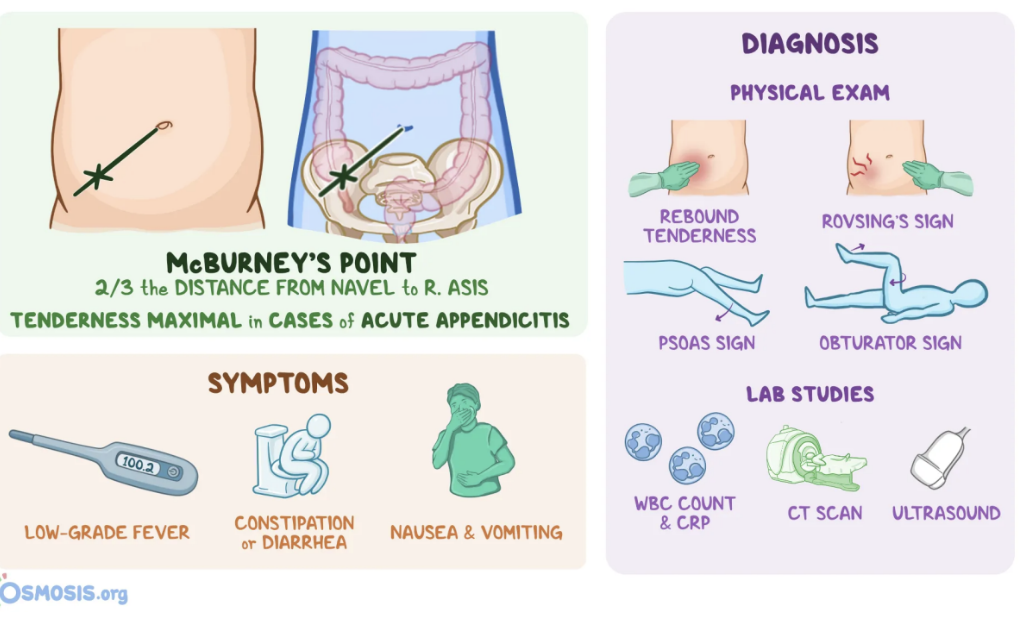
Clinical drop — Appendicitis
An abdominal emergency — appendix is obstructed by either a fecalish or enlargement of lymphoid nodules
In the obstructed appendix, bacteria proliferate & invade the appendicular wall, which becomes damaged by pressure necrosis
In some instances, this may resolve spontaneously — in other cases, inflammatory changes continue & perforation ensures, leading to localized or generalized peritonitis
Clinical drop — Meckel’s diverticulum
An ileal/Meckel’s diverticulum — congenital anomaly occuring in 1-2% of population
Caused by remanant of proximal part of embryonic omphalo-enteric duct (yolk stalk), diverticulum usually appears as a finger-like pouch
Always site of attachment of omphalo-enteric duct on the antimesenteric border (opposite the mesentetic attachment) of the ileum
Usually located 30-60 cm from ileocecal junction in infants & 50 cm in adults
May be free (75%) or attached to the umbilicus (25%)
Although mucosa is mostly ileal in type, may also include areas of acid-producing gastric tissue, pancreatic tissue, or jejunal or colonic mucosa (sometimes even endometrial)
An ileal diverticulum can become inflamed & produce pain mimicking appendicitis (differential diagnosis)
Colon
The distal part of the GI tract, extending from cecum to anal canal. Receives digested food from small intestine, from which it absorbs water & electrolytes to form faeces
Can be anatomically divided into 4 parts, which form an arch encircling the small intestine —
Ascending colon —
A retroperitoneal structure ascending superiorly from the cecum
Once at the right lobe of the liver, it turns at the right colic (hepatic) flexure 90°, marking start of transverse colon
Transverse colon —
Extends from right colic flexure to the left colic (splenic) flexure at the spleen, where it turns another 90° to point inferiorly. Here, the colon is attached to the diaphragm via the phrenicocolic ligament
The least fixed part of the colon & variable (can dip into the pelvis in tall thin people) — unlike ascending & descending colon, it is intraperitoneal & enclosed by transverse mesocolon
Descending colon —
After left colic flexure, moves inferiorly towards the pelvis
Retroperitoneal in most individuals, located anteriorly to the left kidney, passing over its lateral border. Once it turns medially, it becomes the sigmoid colon
Sigmoid colon —
40cm long — located in lower left quadrant of abdomen, extending from left iliac fossa to S3 vertebrae, thus giving its characteristic “S” shape
Attached to the posterior pelvic wall by the sigmoid mesocolon, with this mesentery’s long length allowing this part of the colon to be especially mobile
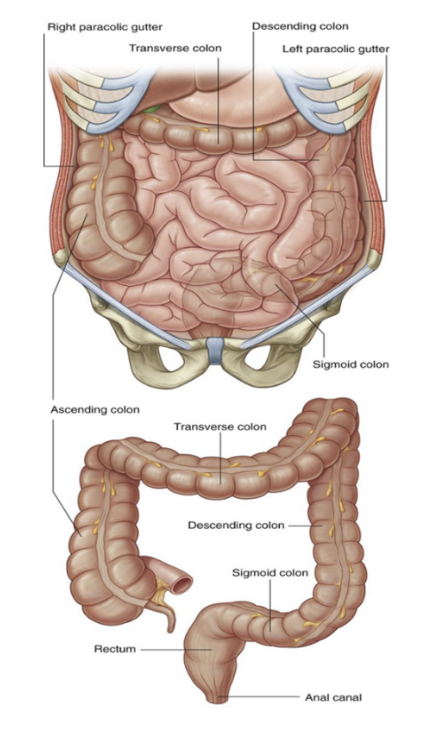
Paracolic gutters
2 spaces between ascending/descending colon & posterolateral abdominal wall
Clinically important — alow material released from inflamed/infected abdominal organs to accumulate elsewhere in the abdomen
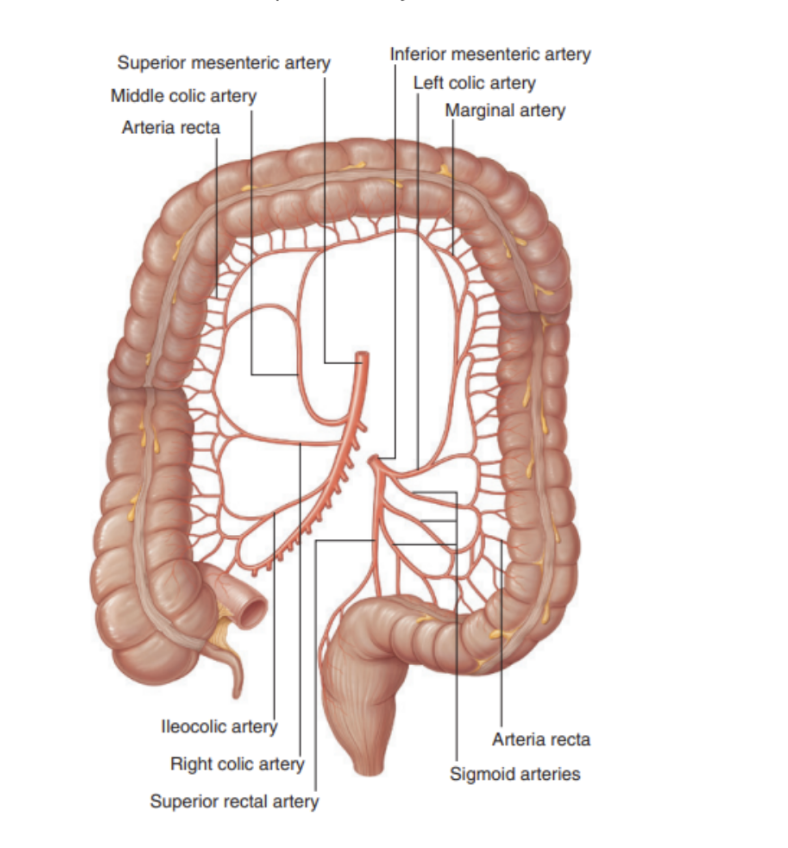
Arterial supply to colon
Ascending colon —
Colic branch from ileocolic artery from SMA
Anterior cecal artery from ileocolic artery from SMA
Posterior cecal artery from ileocolic artery from SMA
Right colic artery from SMA
Transverse colon —
Right colic artery from SMA
Middle colic artery from SMA
Left colic artery from IMA
Descending colon —
Left colic artery from IMA
Sigmoid colon —
Sigmoidal arteries from inferior mesenteric artery
Anastomotic connections between arteries supplying the colon can result in a marginal artery coursing along ascending, transverse, & descending parts of the large bowel
Venous drainage to colon
Similar to arterial supply —
Ascending colon —
Ileocolic & right colic veins — SMV
Transverse colon —
Middle colic vein — SMV
Descending colon —
Left colic vein — IMV
Sigmoid colon —
Sigmoid veins into IMV
Superior mesenteric & inferior mesenteric veins ultimately empty into the hepatic portal veins — allowing toxins absorbed from the colon to be processed by the liver for detoxification
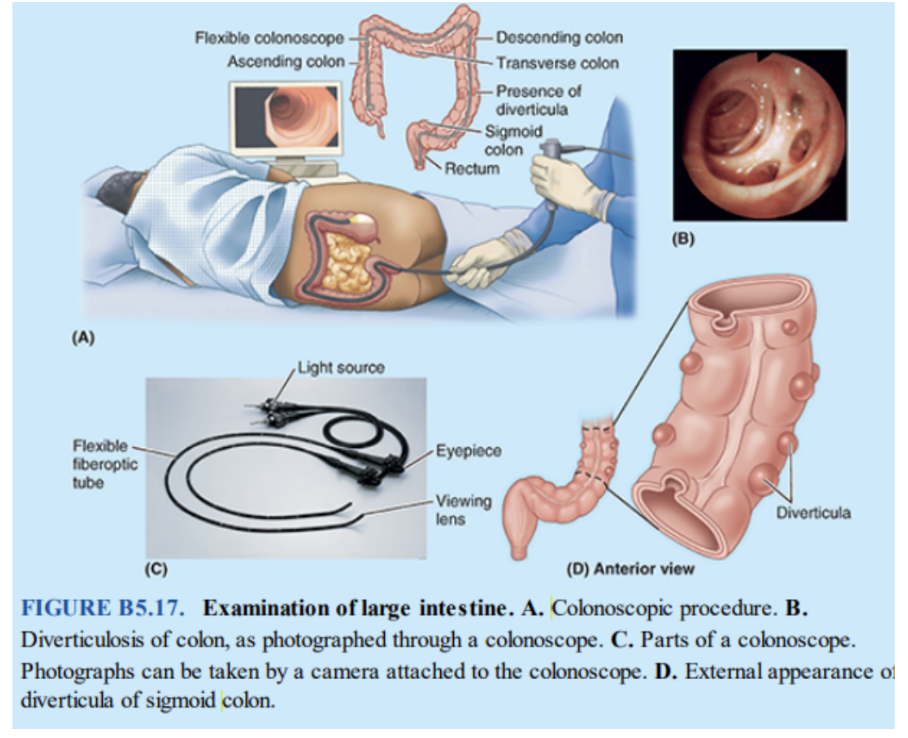
Clinical drop — Colonoscopy
Procedure observing & photographing the interior of the colon using a long, flexible fiberoptic endoscope (colonscope), inserted into the colon through the anus & rectum
The interior of the sigmoid colon is observed with a sigmoidoscope — a shorter endoscope — in sigmoidoscopy
Small instruments can be passed through both instruments & used to facilitate minor operative procedures — ex. biopsies or polyps removal
Most tumors of the large intestine occur in sigmoid colon & rectum (often near rectosigmoid junction), or ascending colon
Colorectal cancers have different characteristics based on where they are in the colon or rectum —
Ex. tumors in ascending colon are more common among women & older patients, whereas rectosigmoidal tumors are more common among men & younger patients. Cancers of transverse or descending colon are less common
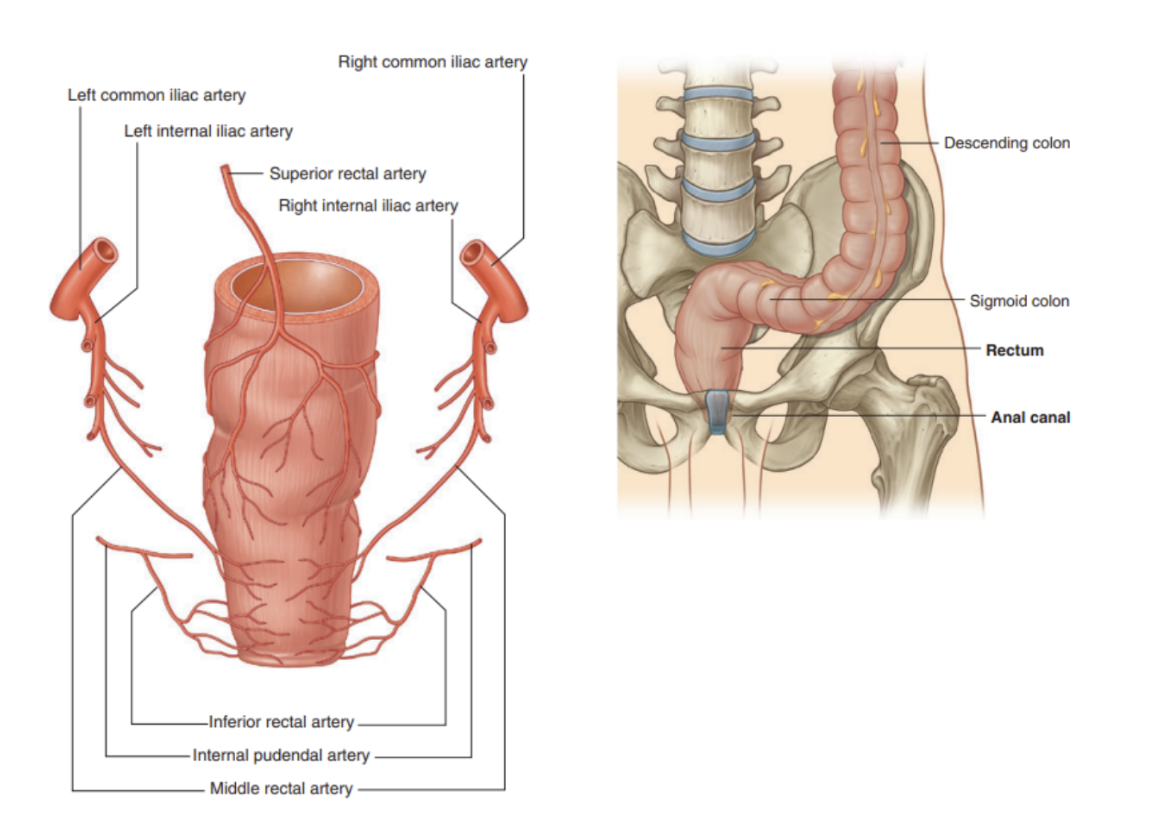
Rectum & anal canal (+vascularization)
Rectum —
Extends from sigmoid colon, with rectosigmoid junction at S3 level or end of sigmoid mesocolon — rectum = retroperitoneal
Anal canal —
Continuation of large intestine inferior to rectum
Arterial supply —
Superior anorectal artery from inferior mesenteric artery (IMA)
Middle rectal artery from anterior branch of internal iliac artery
Inferior rectal artery from internal pudendal artery (from anterior internal iliac artery)
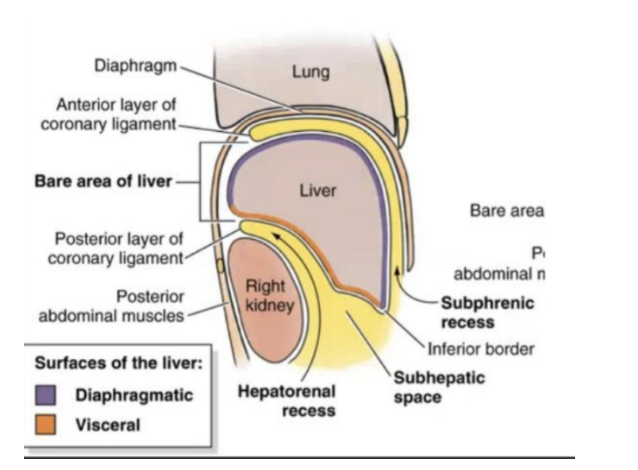
The liver (overall)
Largest visceral organ in the body — primarily in right hypochondrium & epigastric region, extending into left hypochondrium
Surfaces —
Diaphragmatic surface anteriorly, superiorly, & posteriorly
Visceral surface in inferior direction
Diaphragmatic surface of the liver
Smooth & domed, against inferior surface of diaphragm
Associated with suphrenic & hepatorenal recesses —
Subphrenic recess — separates diaphragmatic surface of liver from diaphragm & is divided into right & left areas by the falciform ligament — a structure derived from ventral mesentery in the embryo
Hepatorenal recess — part of peritoneal cavity on right side between liver & right kidney & right suprarenal gland
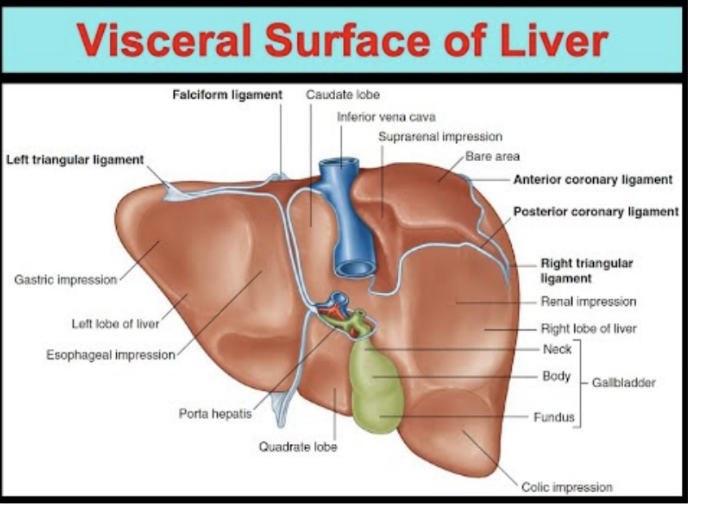
Visceral surface of liver
Covered by visceral peritoneum except in the fossa for gallbladder and at the porta hepatis, aswell as bare area
Structures related to it —
Esophagus, right anterior part of stomach, superior part of duodenum, lesser omentum, gallbladder, & kidney
Porta hepatis — serves a point of entry into liver for hepatic arteries & portal vein, and the exit point for the hepatic ducts
Associated ligaments to the liver
Attached to anterior abdominal wall by the falciform ligament
Except for a small area of liver against the diaphragm (the bare area), the liver is almost completely surrounded by visceral peritoneum — the bare area —
No intervening peritoneum between liver & diaphragm
Anterior boundary of bare area is indicated by a reflection of peritoneum — the anterior coronary ligament
Posterior boundary aswell — posterior coronary ligament
Where the coronary ligaments come together laterally, they form the right & left triangular ligaments
Additional folds of peritoneum connect the liver to —
The stomach — hepatogastric ligament
The duodenum — hepatuduodenal ligament
The diaphragm — right & left triangular ligaments and anterior & posterior coronary ligaments
Lobes of the liver
Divided into right & left lobes by the falciform ligament anterosuperiorly and the fissure for the ligamentum venosum & ligamentum teres on the visceral surface
The right lobe of the liver is the largest lobe, whereas the left is smaller
The quadrate & caudate lobes are described as arising from the right lobe of the liver, but are functionally distinct
The quadrate lobe is visible on the anterior part of the visceral surface of the liver & is bounded on the left by the fissure for the ligamentum teres & on the right by the fossa for the gallbladder
Functionally related to left lobe
Caudate lobe — visible on posterior part of visceral surface of liver
Bounded on left by fissure for ligamentum venosum & on right by groove for inferior vena cava
Functionally separate from both right & left lobes
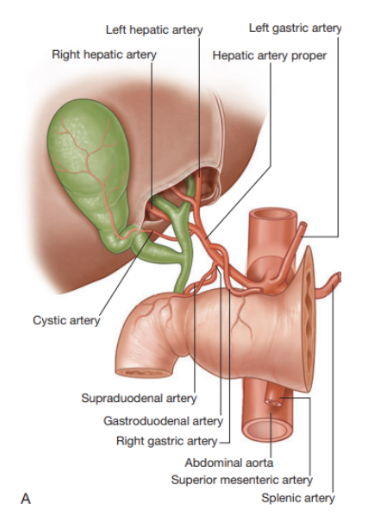
Vascularization of liver
Arterial supply —
Right hepatic artery from hepatic artery proper from common hepatic artery from celiac trunk
Left hepatic artery from (same as above)
Venous drainage —
Right, intermediate, & left hepatic veins — drain into inferior vena cava
Several smaller & somewhat inconsistent caudate lobe veins (from hepatic portal vein)
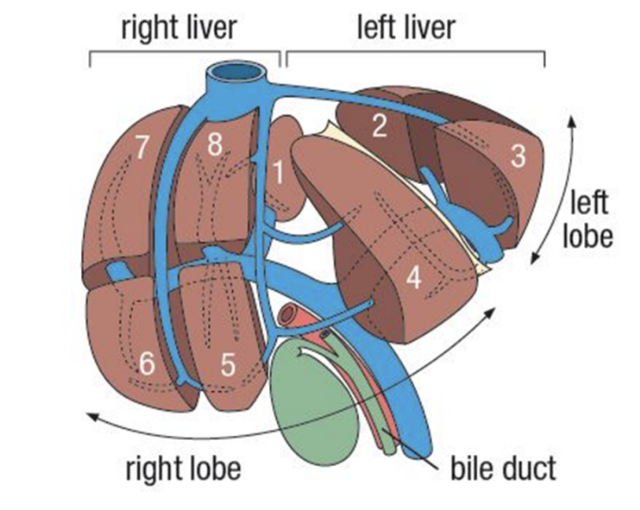
Surgical segmentation of the liver
Based on identification of portal vein bifurcation & origin of hepatic veins
Widely used clinically — better suited for surgery & more accurate in localizing & monitoring various intra parenchymal lesions
8 different recognized segments relevant surgically
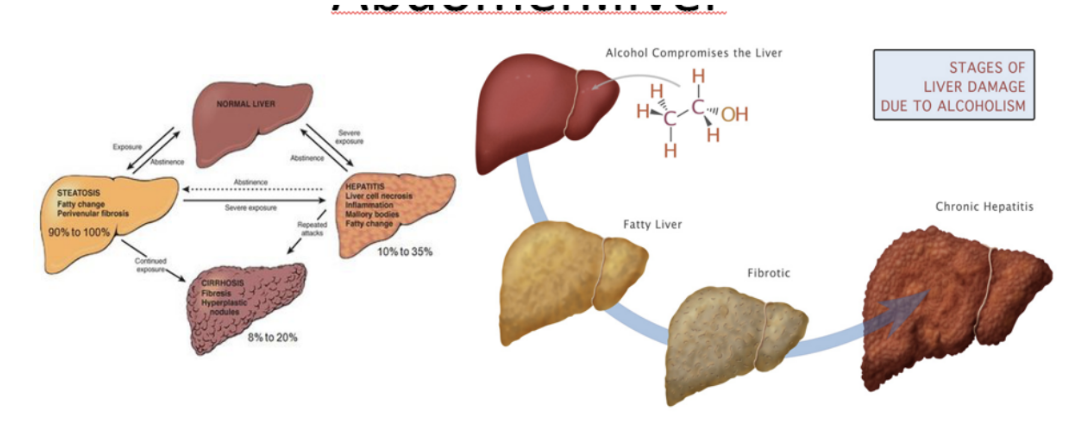
Effect of alcohol on the liver (image)
Gallbladder (+vascularization)
Pear-shaped sac lying on visceral surface of right lobe of liver in a fossa between right & quadrate lobes
Sectioned into —
Rounded end (fundus), projecting from inferior border of liver
Major part in fossa (body), against transverse colon & superior part of duodenum
Narrow part (neck), with mucosal folds forming spiral fold
Arterial supply —
Cystic artery from right hepatic artery (branch of hepatic artery proper)
Receives, concentrates, & stores bile from the liver
Clinical drop — Gallstones
Hard deposits formed in gallbladder, known as cholethiasis
Made of cholesterol, bilirubin, or both
Can cause no symptoms, but if lodged in a duct causing a blockage, can cause —
Sudden & rapid intensifying pain in upper right portion of abdomen
Sudden & rapidly intensifying pain in center of abdomen
Back pain in between shoulder blades
Pain in right shoulder (due to original embryological innervation — was rostral to septum transversum, thus innervated by phrenic nerve, with this maintained after migration)
Nausea or vomiting
Pancreas
Lies mostly posterior to the stomach, extending across posterior abdominal wall from duodenum on the right, and the spleen on the left
Parts —
Projecting from lower part of head is the uncinate process, passing posteriorly to superior mesenteric vessels
Neck — anterior to superior mesenteric vessels
Posterior to neck, superior mesenteric & splenic veins join to form portal vein
Body of pancreas is elongated & extends from neck to tail
Tail passes between layers of splenorenal ligament
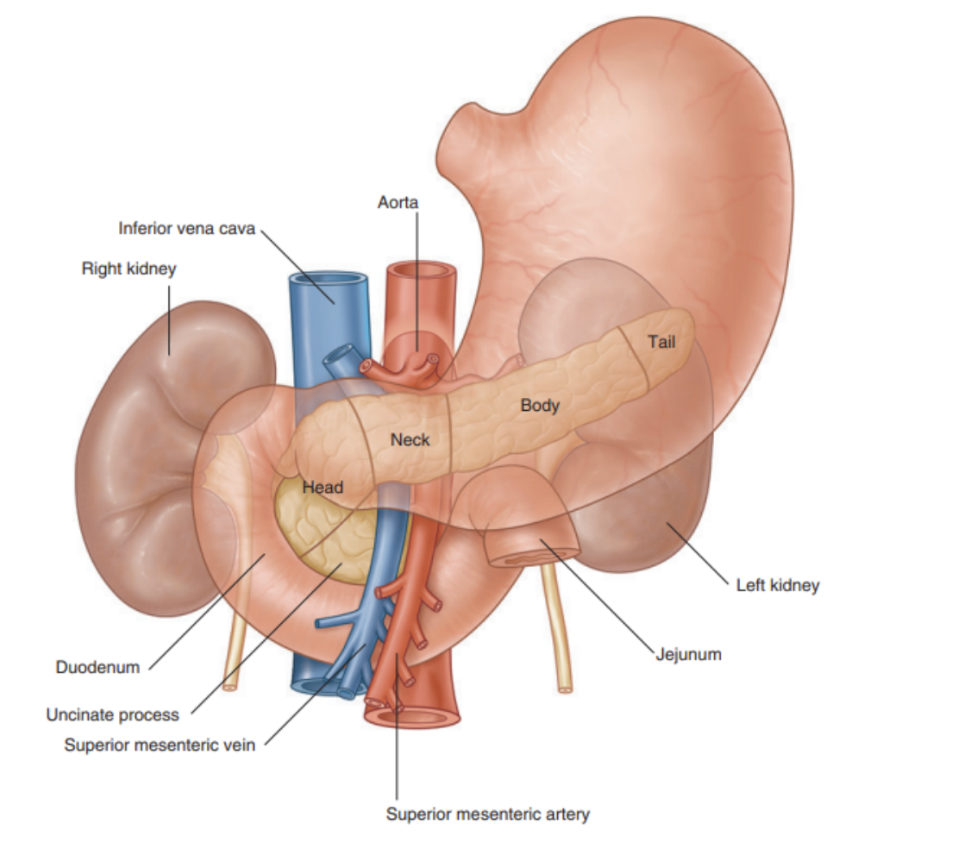
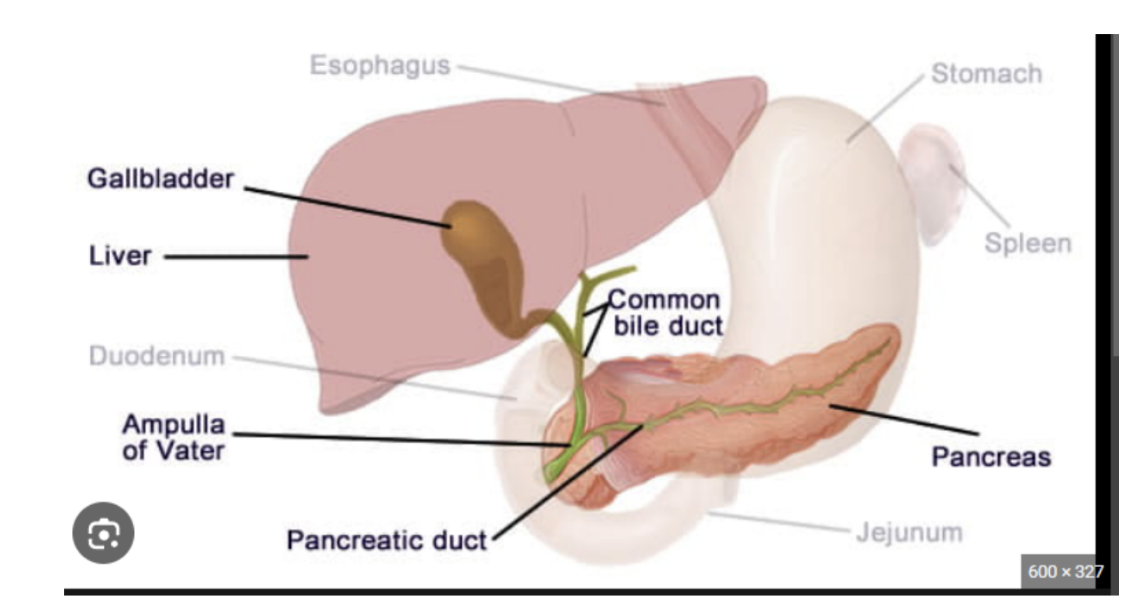
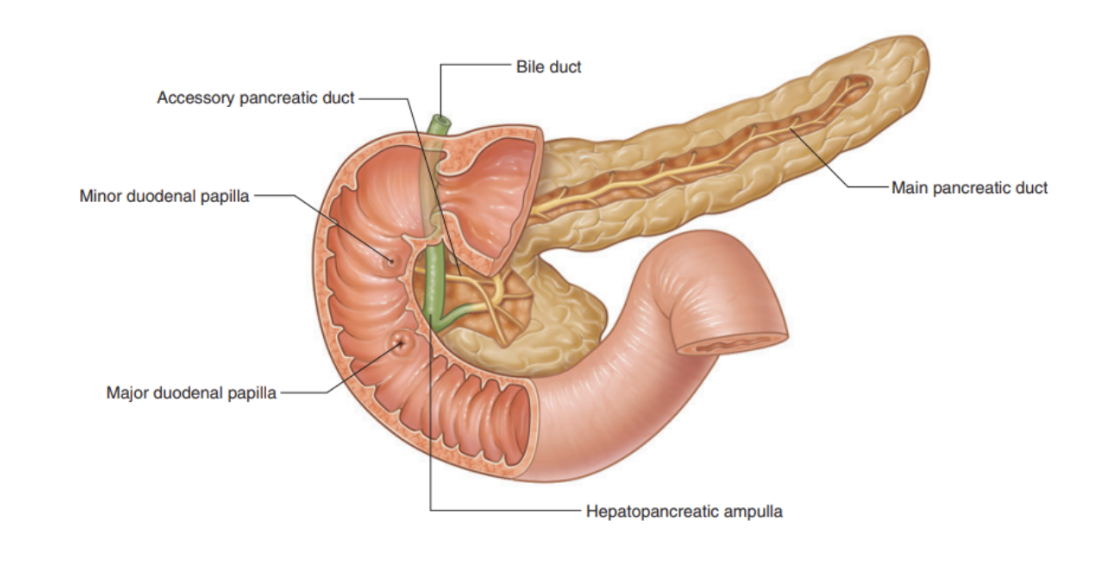
Pancreatic duct
Begins in tail of pancreas — passes right through body, & after entering head, turns inferiorly, where in the lower head it joins the bile duct
These 2 structures joining forms the hepatopancreatic ampulla (ampulla of Vater), entering the descending (second) part of the duodenum at the major duodenum papilla
Surrounding ampulla is sphincter of ampulla (sphincter of Oddi) — a collection of smooth muscles
Accessory pancreatic duct empties into duodenum just above major duodenal papilla at the minor duodenal papilla
Main & accessory ducts usually communicate with each other — presence of them reflects embryological origin of pancreas from dorsal & ventral buds of foregut
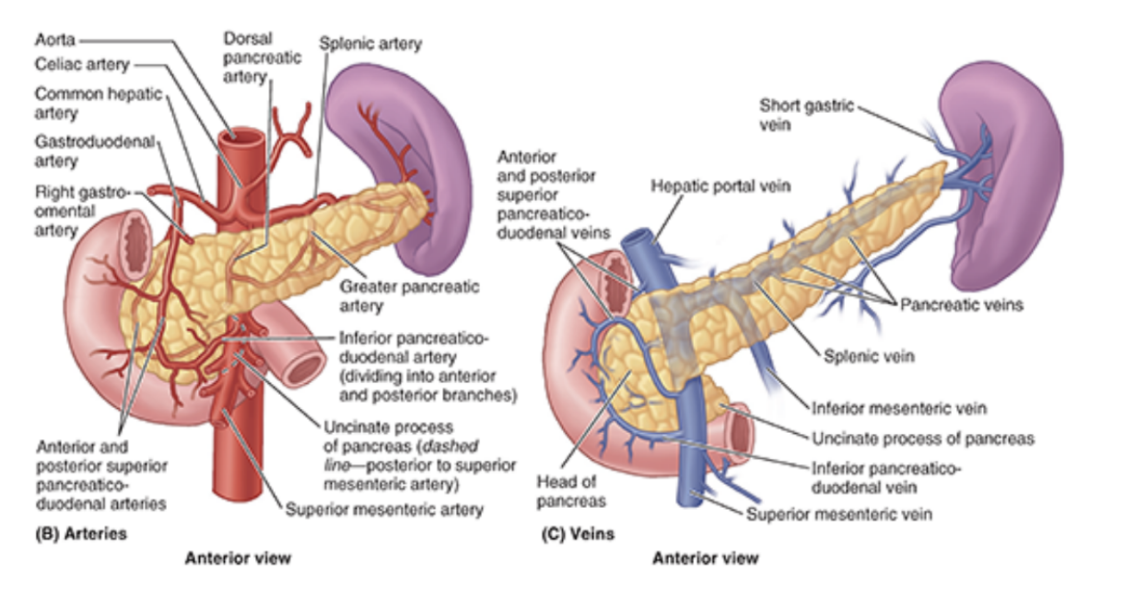
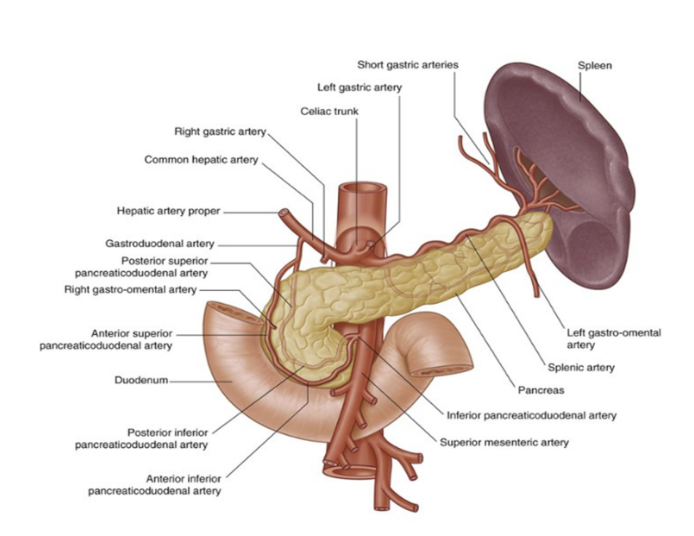
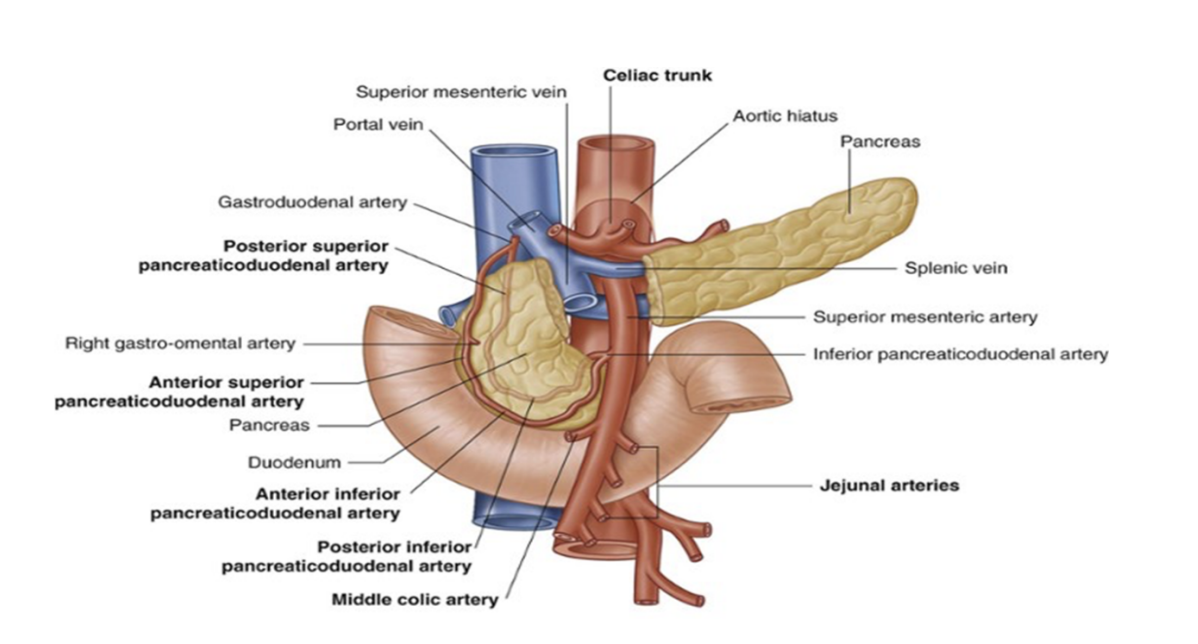
Vascularization of pancreatic duct/pancreas
Arterial supply —
Derived mainly from branches of markedly tortuous splenic artery — multiple pancreatic arteries form several arcades with pancreatic branches of gastroduodenal & superior mesenteric arteries
As many as 10 branches may pass from splenic artery to body & tail of pancreas
The anterior & posterior superior pancreaticoduodenal arteries, branches of gastroduodenal artery, and anterior & posterior inferior pancreaticoduodenal arteries — branches of SMA — form anteriorly & posteriorly placed arcades that supply the pancreatic head
(basically sup. post & ant pancreaditocuodenal from gastroduodenal & inf version from SMA, then 10 branches from splenic
Venous drainage —
Via corresponding pancreatic veins, going to splenic & superior mesenteric parts of the hepatic portal vein
Most empty into splenic vein
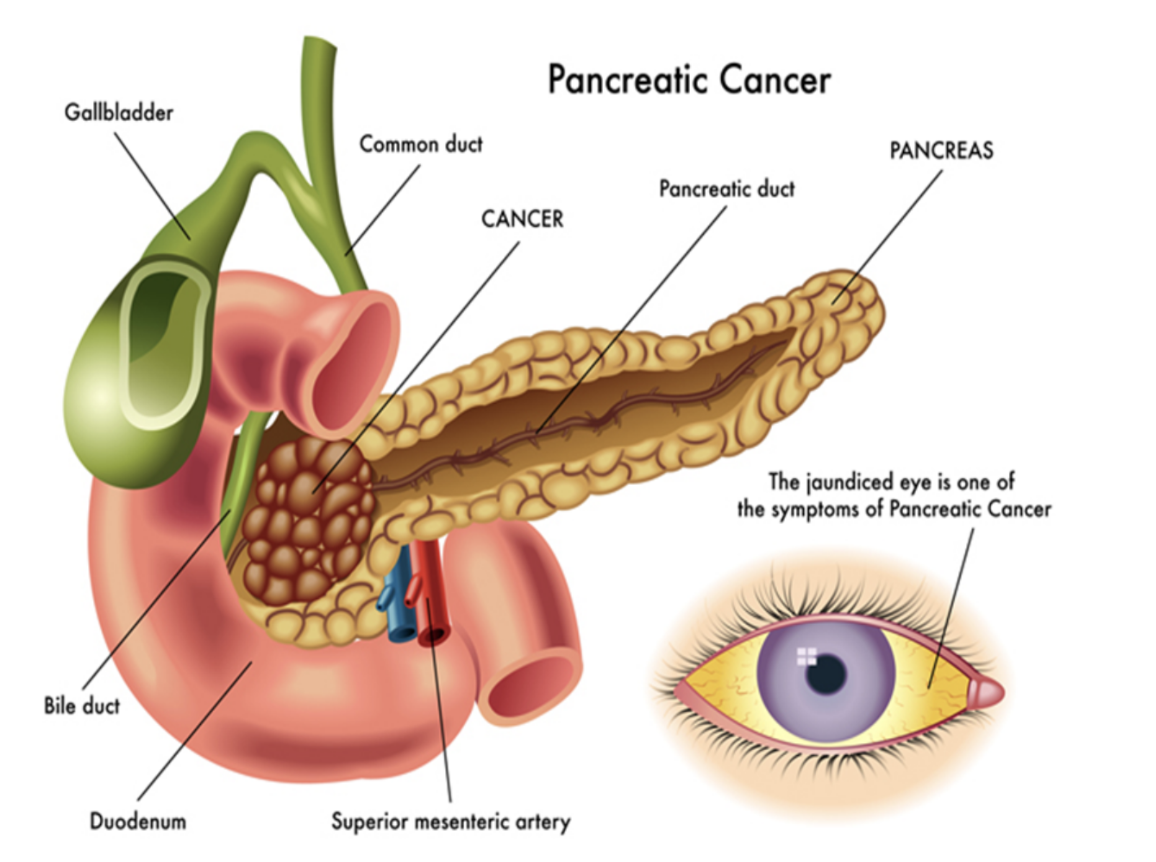
Clinical drop — pancreatic cancer
Malignant tumors of the pancreas may occur anywhere in the pancreas — but most frequent in head & neck
Number of nonspecific findings in patients with pancreatic cancer —
Upper abdominal pain, loss of appetite, & weight loss
Depending on site of cancer, obstruction of bile duct can occur, leading to obstructive jaundice
Most cancers spread locally — invading portal vein & superior mesenteric vessels, even extending into porta hepatis
Lymph node spread is also common, with these factors precluding curative surgery
Given position of pancreas, a surgical resection is a complex procedure involving resection of the region of the pancreatic tumor usually with part of the duodenum, necessitating a complex bypass procedure
Passage of bile
Bile duct system extends from liver, connects with gallbladder, & empties into descending part of duodenum
The coalescence of ducts begins in liver parenchyma & continues until right & left hepatic ducts are formed, which drain their respective lobes of the liver
These combine to form common hepatic duct, which runs near the liver along with hepatic artery proper & portal vein in the free margin of the lesser omentum
As it descends, it is joined by the cystic duct from the gallbladder, forming the bile duct
At this point lies right of hepatic artery proper & usually right & anteriorly to the portal vein in the free margin of the lesser omentum
Omental foramen is posterior to these structures at this point — bile duct continues to descend, passing posteriorly to superior part of duodenum before joining with pancreatic duct to enter descending part of duodenum at major duodenal papilla
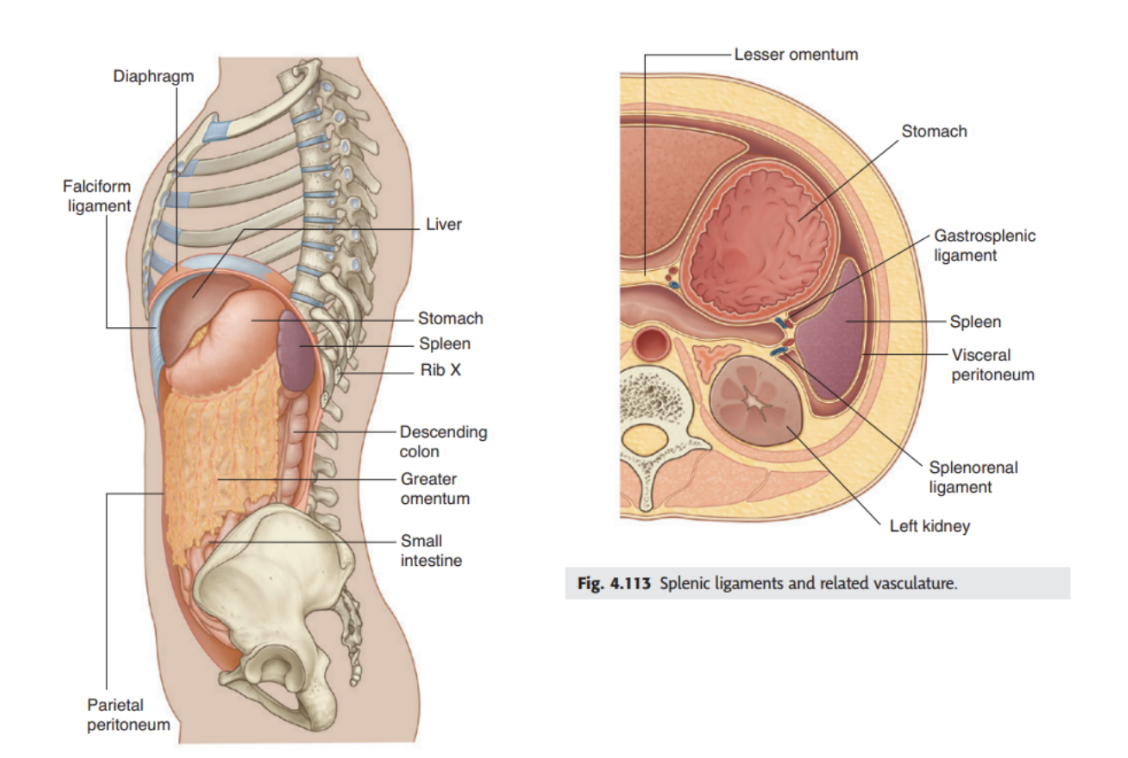
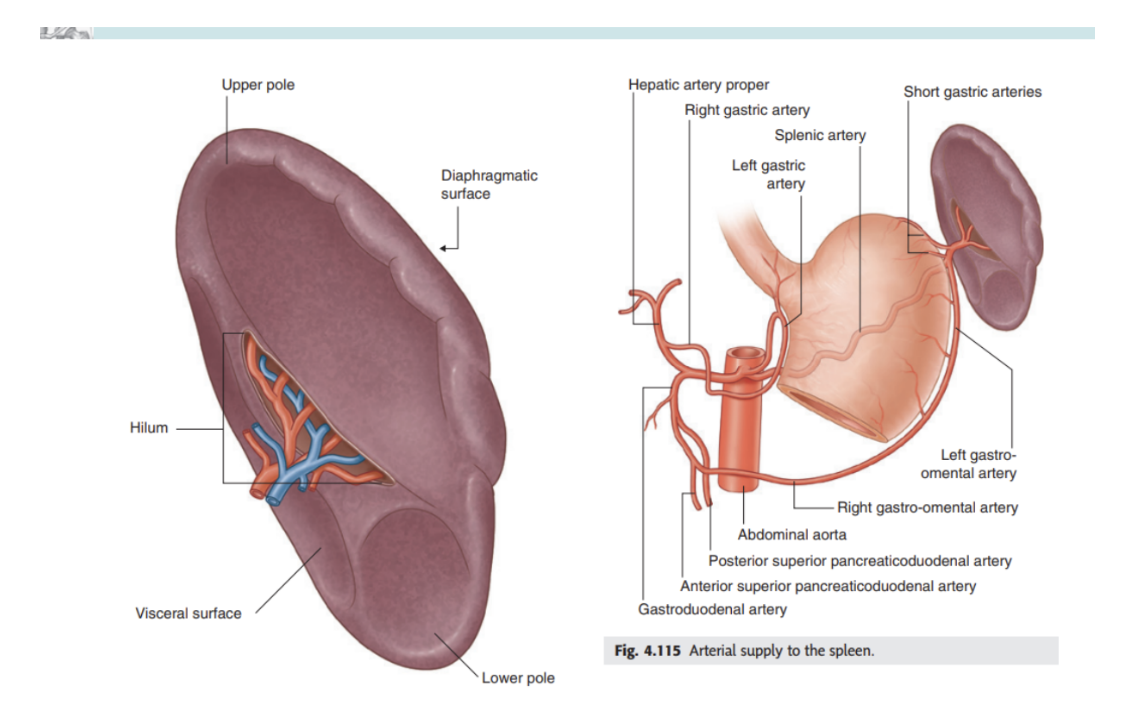
Spleen
intraperitoneal
Develops as part of vascular system in the part of the dorsal mesentery suspending the developing stomach from the body wall
In the adult, lies against the diaphragm in area of rib 9-10 — thus in upper left quadrant/left hypochondrium of the abdomen
Connected to —
Greater curvature of stomach by the gastrosplenic ligament, containing short gastric & gastromental vessels
Left kidney by splenorenal ligament, containing the splenic vessels
Both ligament are part of the greater omentum — spleen is surrounded by visceral peritoneum except around the hilum on its medial surface
Splenic hilum — entry point for splenic vessels, along with occasionally tail of pancreas in this area
Vascularization —
Arterial supply — the splenic artery from celiac trunk
Venous drainage — splenic vein, also receiving blood from inferior mesenteric vein
Clinical drop — splenic rupture & enlargement
Splenic rupture —
Tends to occur due to localized trauma to left upper quadrant — may be associated with left lower rib fractures
Due to extremely thin capsule, susceptible to injury even when there isn’t damage to surrounding structures
As it is highly vascular, when ruptured, bleeds profusely into peritoneal cavity
Splenic rupture should always be suspected with blunt abdominal injury
Current treatments preserve as much of spleen as possible, but some patients require splenorectomy
Splenic enlargement (splenomegaly)—
As an organ of the reticuloendothelial system, it is involved in hepatopoiesis & immunological surveillance
Diseases affecting this system *ex. leukemia or lymphoma), can produce generalized lymphadenopathy and enlargement of the spleen
Often enlarges when performing normal physiological functions — ex. clearing microorganisms & particulates from circulation, producing increased antibodies in course of sepsis, or removing deficient/destroyed erythrocytes (ex. due to thalassemia or spherocytosis)
Splenomegaly can also be the result of increased venous pressure caused by congestive heart failure, splenic vein thrombosis, or portal hypertension
An enlarged spleen is prone to rupture
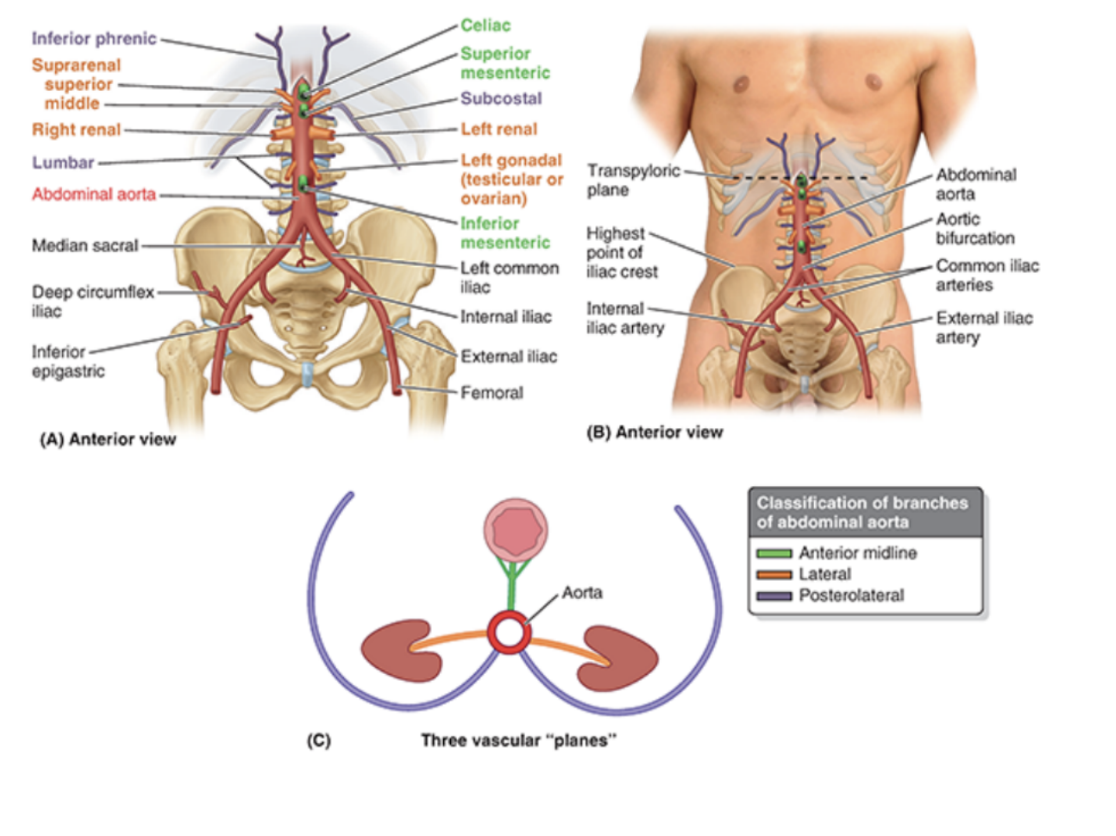
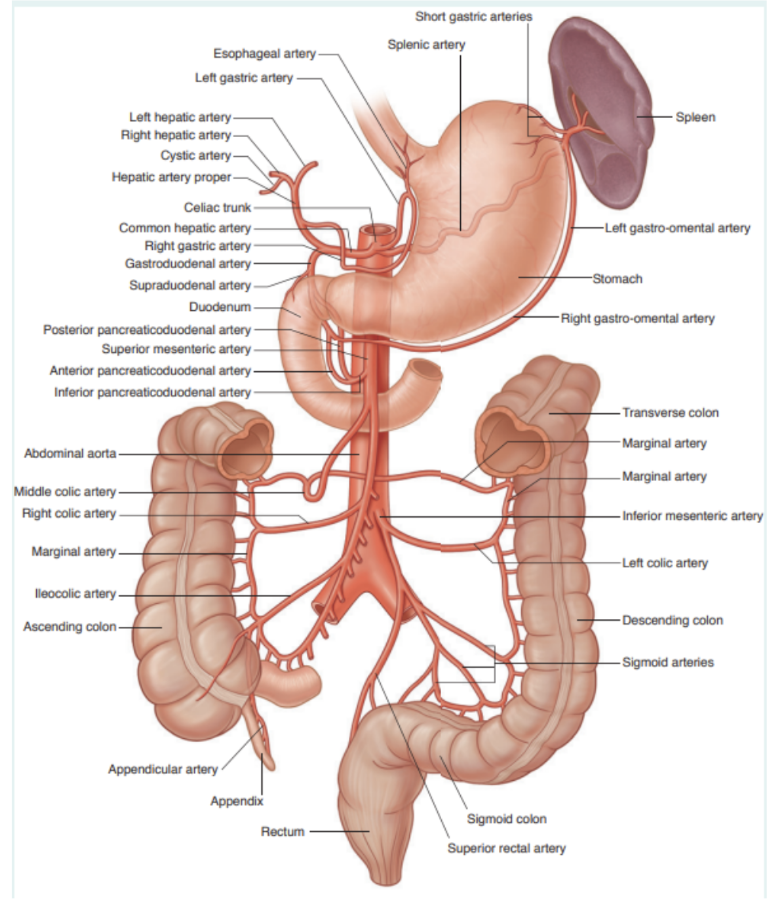
Abdominal aorta & arterial supply
Most arteries supplying posterior abdominal wall arise from abdominal aorta
Abdominal aorta is approximately 13 cm in length — beginning at aortic hiatus in diaphragm at level T12, ending at level L4 by dividing into right & left common iliac arteries
Can be represented on the anterior abdominal wall by a band (approximately 2 cm wide) extending from a median point, approximately 2.5 cm superior to the transpyloric plane to a point slightly (2–3 cm) inferior to and to the left of the umbilicus at the level of the supracristal plane (plane of the highest points of the iliac crests).
In children and lean adults, the lower abdominal aorta is
sufficiently close to the anterior abdominal wall that its pulsations may be detected or apparent when the wall is relaxed
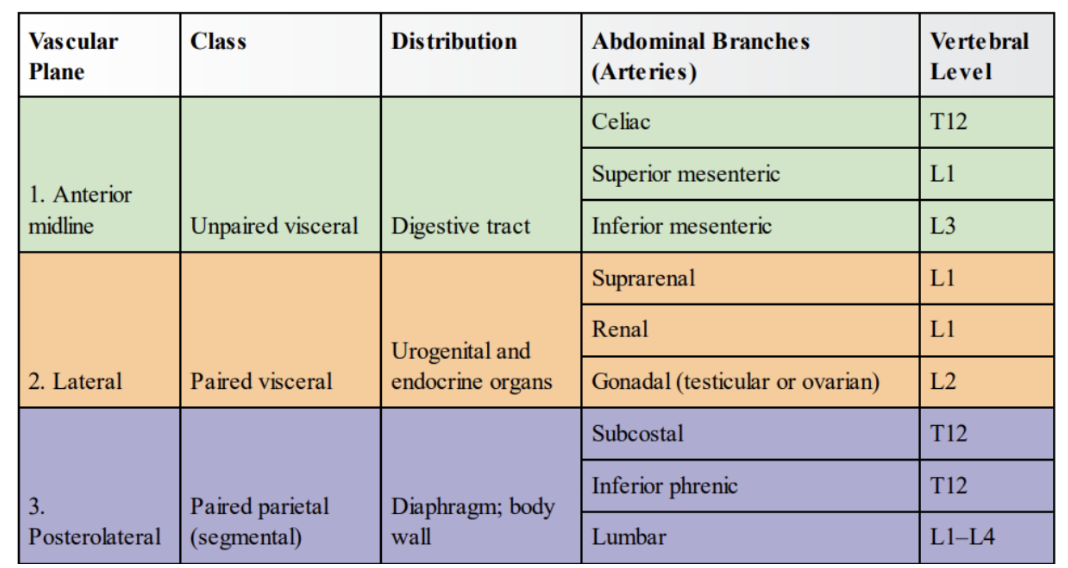
Note on embryological origin relating to aorta, as well as branches (mostly for diagram of all branches)
Foregut, midgut, hindgut, vascularized by celiac artery, SMA, IMA, respectively thing again — look at diagram
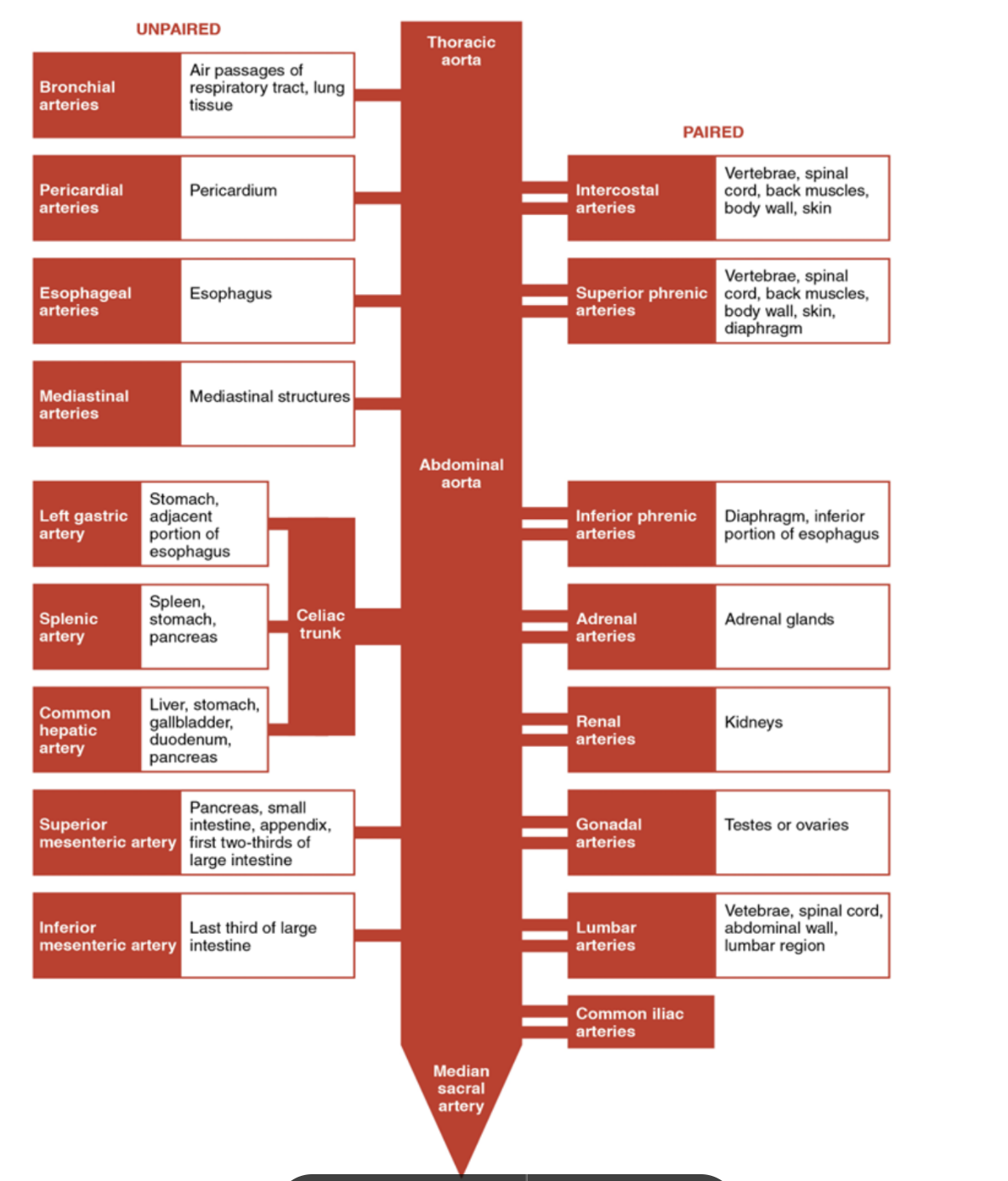
Celiac trunk
Major artery of the abdomen — arising from abdominal aorta, spplying many of the gastrointestinal viscera
Second branch of abdominal aorta
(First branches are paired inferior phrenic arteries)
Arises from anterior aspect of aorta, at aortic hiatus of diaphragm (T12)
After emerging from the aorta, it extends approximately 1cm before dividing into the left gastric, splenic, & common hepatic arteries
Of these branches, 2 go left & 1 goes right
Collectively, they are the major arterial supply to the stomach, spleen, liver, gallbladder, abdominal esophagus, pancreas, & duodenum
Left gastric artery —
Smallest of 3 celiac trunk branches — ascends across the diaphragm, giving rise to esophageal branches, before continuing anteriorly along lesser stomach curvature
At lesser curvature anastomoses with right gastric artery
Splenic artery
Arises from trunk just inferior to left gastric artery
Travels towards spleen, running posterior to the stomach & along the superior margin of the pancreas
During its course, it is contained by the splenorenal ligament
Then terminates into 5 branches that supply segments of the spleen
In addition to supplying the spleen, it also gives rise to several important vessels —
Left gastroepiploic —
Supplies the greater curvature of the stomach
Anastomoses with the right gastroepiploic artery
Short gastrics —
5-7 small branches supplying fundus of the stomach
Pancreatic branches —
Supply the body & tail of the pancreas
The splenic artery has a tortuous appearence (tortuous meaning turning — similar to facial branch of external carotid) — thus easily identifiable from other nearly vessels
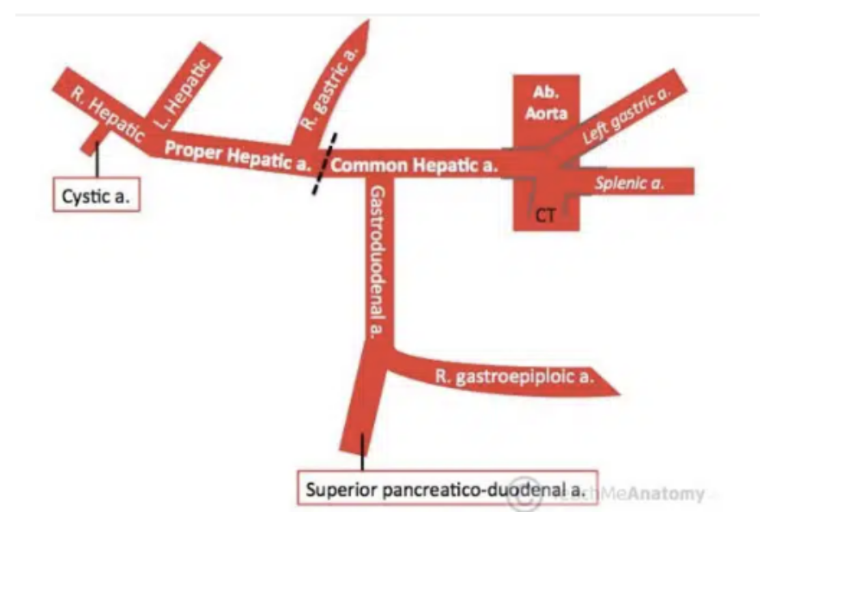
Common hepatic artery + branches (& branches of branches)
Sole arterial supply to liver & only branch of celiac artery to pass to the right
As it travels past superior part of duodenum, it divides into its 2 terminal branches, each with their own branches (arrangement of those branches is variable —
Proper hepatic artery
Ascends through lesser omentum towards liver, giving rise to —
Right gastric —
Supplies stomach pylorus & lesser curvature
Right & left hepatic —
Divides inferior to porta hepatis to supply their respective lobes of the liver
Cystic —
Branch of right hepatic artery — supplies gallbladder
Gastroduodenal artery
Descends posterior to superior portion of duodenum, giving off —
Right gastroepiploic —
Supplies greater stomach curvature, found between layers of greater omentum, which it also supplies
Superior pancreaticoduodenal —
Divides into an anterior & posterior branch supplying head of pancreas
Superior mesenteric artery
Anterior branch of abdominal aorta supplying the midgut — arises from aorta immediately below celiac artery, around level L1
Crossed anteriorly by splenic vein & neck of pancreas
Posteriorly can find left renal vein, uncinate process of pancreas, & inferior part of duodenum
After giving off its first branch (inferior pancreaticoduodenal), it gives off jejunal & ileal arteries on its left
Will turn into vasa recta (longer for jejunum)
Branching from the right side of its main trunk —
Middle coli artery
Right colic artery
Ileocolic artery
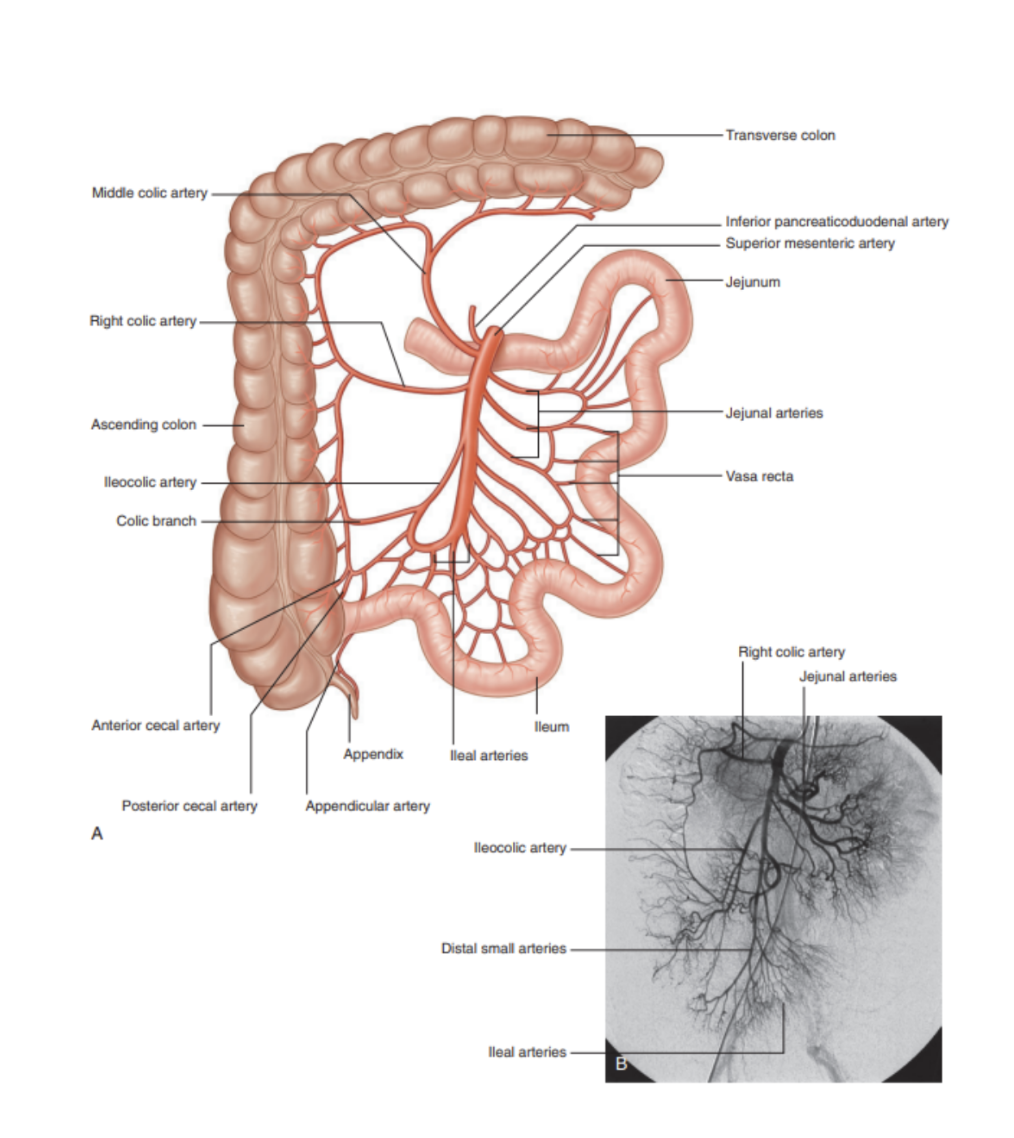
Branches of Superior Mesenteric Artery
Inferior pancreaticoduodenal artery —
First branch of SMA — forms anterior & posterior vessels that anastomose with branches of superior pancreaticoduodenal artery (from celiac trunk)
Supplies inferior region of head of pancreas, uncinate process, & duodenum
Jejunal & ileal arteries —
Pass between layers of mesentery to form anastomotic arcades, from which vasa recta (smaller, straight arteries) will arise to supply the organs
Jejunal blood supply has a smaller number of arterial arcades with longer vasa recta, while ileal blood supply has more arterial arcades with shorter vasa recta
Middle colic artery —
Arises from right side of SMA to supply transverse colon
Right colic artery —
Arises from right side of SMA to supply ascending colon
Ileocolic artery —
Final major branch of SMA — passes inferiorly & to right, giving rise to branches to the ascending colon, appendix, cecum, & ileum
In cases of appendectomy, the appendicular artery is ligated
Inferior mesenteric artery
Anterior branch of abdominal aorta — supplying hndgut
Smallest of 3 anterior branches of abdominal aorta, arising anteriorly to L3
Initially descends anteriorly to aorta then passes left as it continues inferiorly
Branches into —
Left colic artery
Several sigmoid arteries
Superior rectal artery
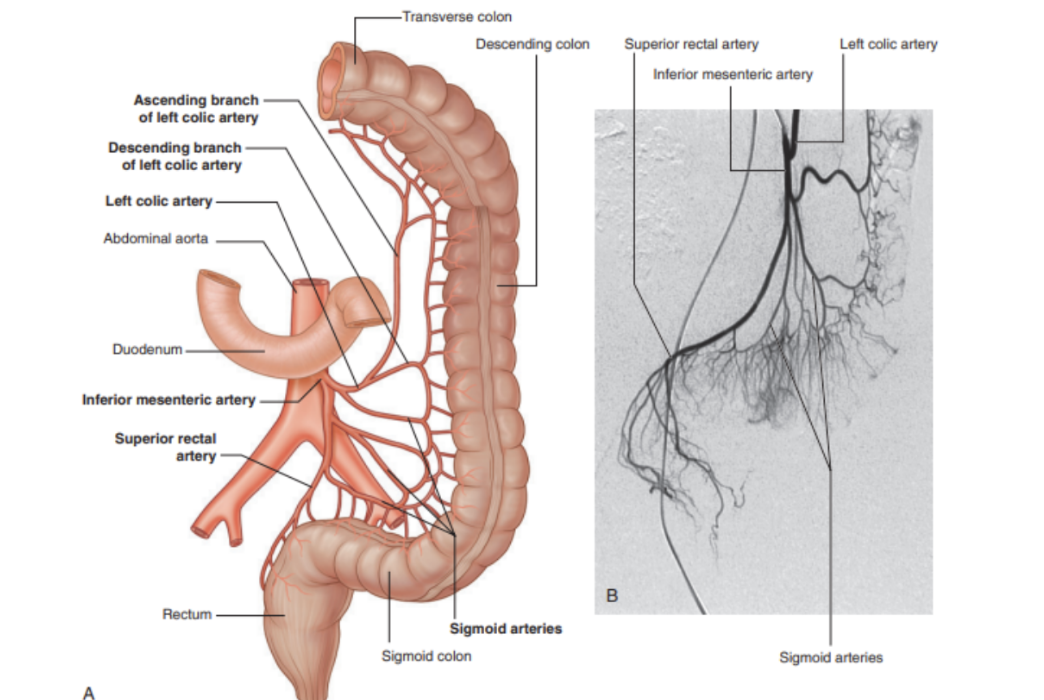
Branches of inferior mesenteric artery
Left colic artery
First branch of IMA, ascending retroperitoneally & dividing into ascending and descending branches —
Ascending branch —
Passes anteriorly to left kidney, then entering transverse mesocolon to pass superiorly to supply the upper part of the descending colon & distal part of transverse colon
Anastomoses with branches of middle colic artery
Descending branch —
Passes inferiorly, supplying lower part of descending colon, anastomosing with first sigmoid artery
Sigmoid arteries —
2-4 branches descending to the left in the sigmoid mesocolon to supply lowest part of descending colon & sigmoid colon
These branches anastomose superiorly with branches from left colic artery & inferiorly with branches from superior rectal artery
Superior rectal artery —
Terminal branch of IMA — descends into pelvic cavity in the sigmoid mesocolon, crossing left common iliac vessels
At level S3 divides into 2 terminal branches, that then descend on either side of the rectum to divide into smaller branches once in the rectal wall
These smaller branches continue inferiorly to the internal anal sphincter, anastomosing along the way with branches from middle rectal arteries (from internal iliac artery), and the inferior rectal arteries (from internal pudendal artery)
Image of summary of arterial supply of abdominal viscera
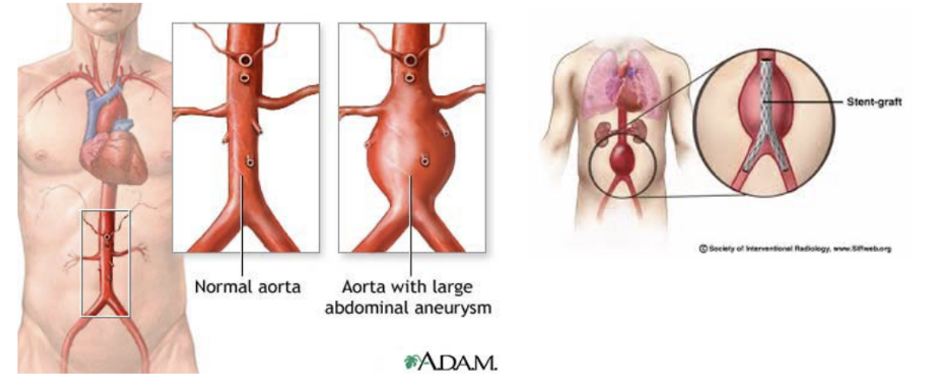
Clinical drop — abdominal aortic aneurysm & stent graft
A dilation of the aorta — generally tends to occur in infrarenal region (at or below renal arteries)
As aorta expands, the risk of rupture increases — generally accepted that when an aneurysm reaches 5.5 cm+ an operation will be significantly beneficial
New techniques (other than solder surgical methods) have been developed — ex. endovascular graft —
Surgically dissecting the femoral artery below inguinal ligament, with a small incision made in the femoral artery & preloaded compressed graft with metal support struts passed on a large catheter through femoral artery into abdominal aorta. X-ray is used for guidance to open the graft, lining the inside of the aorta
Limb attachments are made to the graft that extend into the common iliac vessels, with this bifurcated tube device effectively excluding the abdominal aortic aneurysm
Not suitable for all patients — those with the device don’t need to go to intensive care unit, with many patients leaving hospital in 24-48 hours. Importantly — this device can be used for patients deemed unfit for open surgical repair
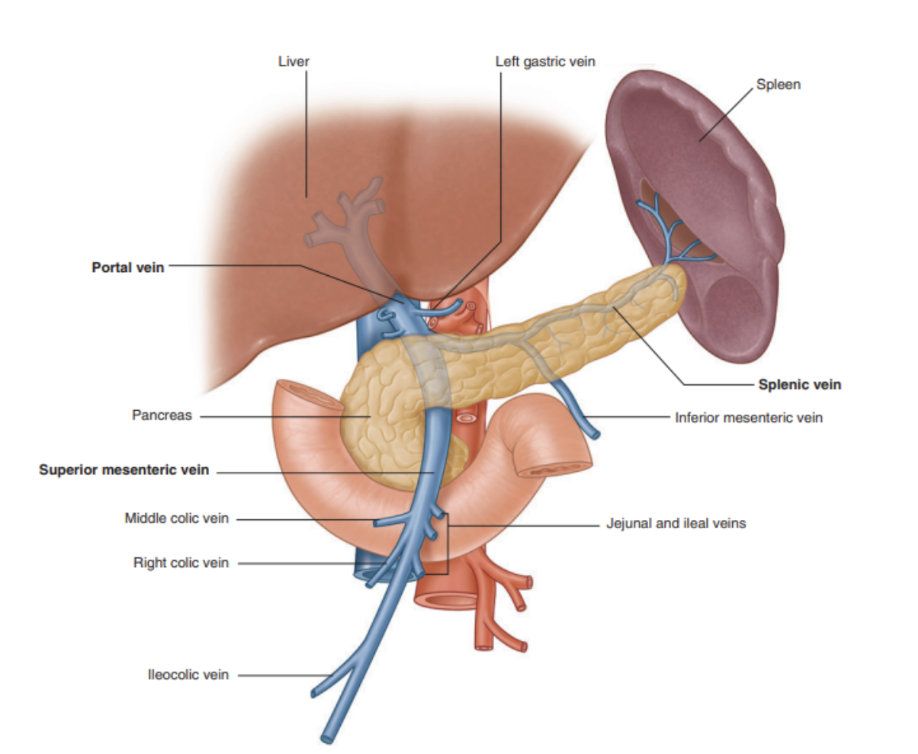
Portal vein (+ tributaries)
Final common pathway for venous blood transport from the spleen, pancreas, gallbladder, & abdominal part of GI tract
Formed by union of splenic & superior mesenteric vein, posterior to the neck of the pancreas at level L2
Ascending towards the liver, it passes posterior to superior part of duodenum to enter right margin of lesser omentum
As it passes through this part of lesser mentum, it is anterior to the omental foramen, & posterior to the bile duct (slightly on the right) and the hepatic artery proper (slightly on its left)
On approaching the liver, it divides into right & left branches that enter the liver parenchyma
Tributaries —
Right & left gastric veins
Draining lesser stomach curvature & abdominal esophagus
Cystic veins (from gallbladder)
Para-umbilical veins
Associated with obliterated umbilical vein & connect to veins on anterior abdominal wall
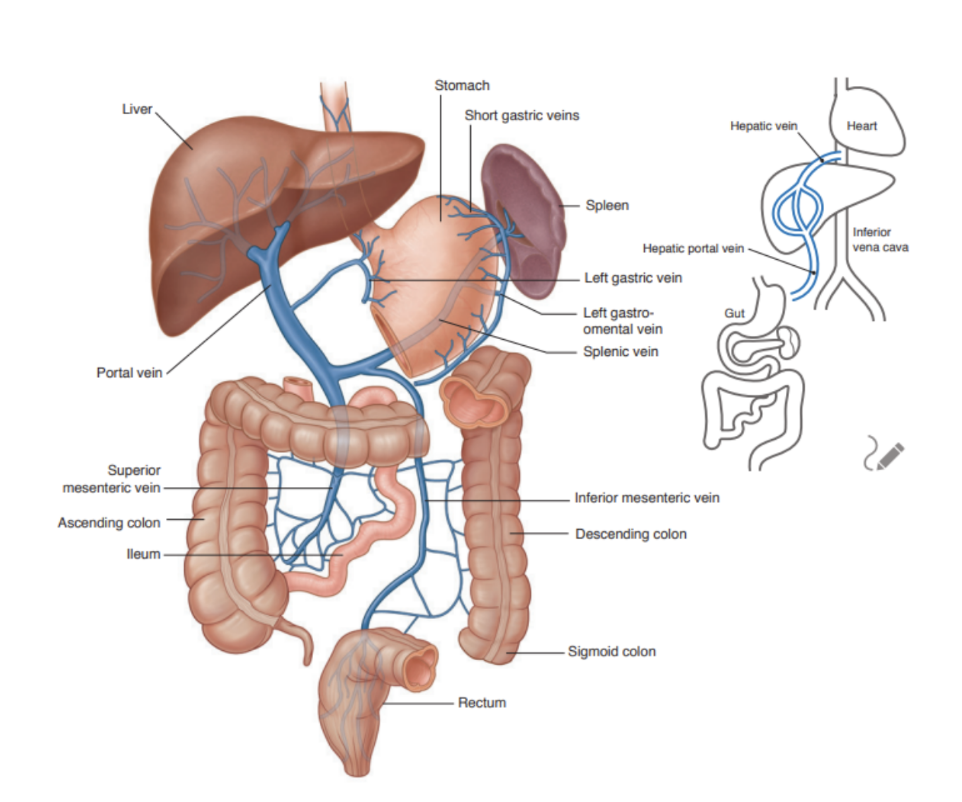
Splenic vein (+tributaries)
Forms from numerous smaller vessels leaving splenic hilum
Passes to the right, through the splenorenal ligament along with splenic artery & tail of pancreas
Continuing right, large straight splenic vein contacts pancreatic body as it crosses posterior abdominal wall
Posterior to neck of pancreas, it joins superior mesenteric vein to form portal vein
Tributaries —
Short gastric veins —
From fundus & left part of greater stomach curvature
Left gastro-omental vein —
From greater stomach curvature
Pancreatic veins —
Draining body & tail of pancreas
Inferior mesenteric vein (usually) —
Superior mesenteric vein —
Drains blood from small intestine, cecum, ascending colon & transverse colon
Begins in right iliac fossa, where veins draining terminal ilecum, cecum, & appendix join, and ascends in mesentery to right of superior mesenteric artery
Posterior to neck of pancreas, joins splenic vein to form portal vein
A corresponding vein accompanies each branch of superior mesenteric artery — thus tributaries —
Jejunal, ileal, ileocolic, right colic, & middle colic veins
Additional tributaries —
Right gastro-omental vein
Drains right part of greater stomach curvature
Anterior & posterior inferior pancreaticoduodenal veins —
Pass alongside arteries of same name
Anterior superior pancreaticoduodenal vein usually empties into right gastro-omental vein, while posterior superior pancreaticoduodenal vein usually empties directly into portal vein
Inferior mesenteric vein
Drains blood from rectum, sigmoid colon, descending colon, & splenic flexure
Begins as superior rectal vein & ascends, receiving tributaries from sigmoid veins & left colic vein
All of these veins accompany arteries of same name
Continuing to ascend, it passes posterior to pancreatic body to (usually) join splenic vein
Occasionally ends at junction of splenic & superior mesenteric veins, or joins superior mesenteric vein
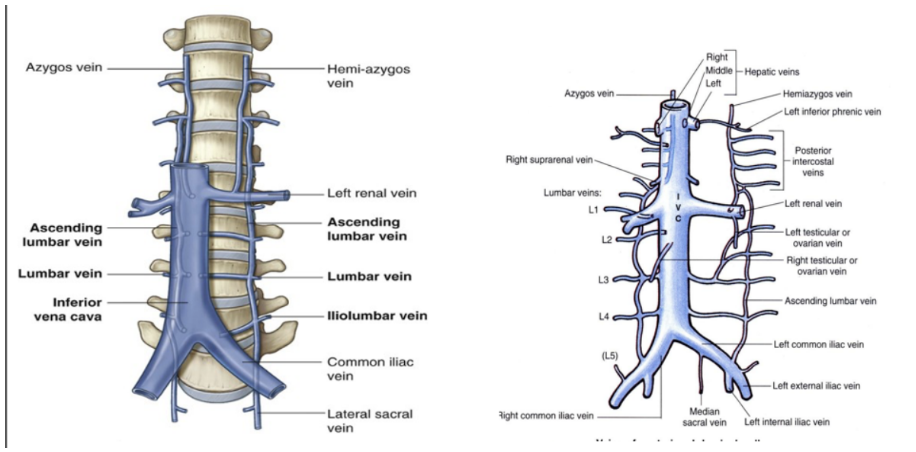
Inferior vena cava (+ tributaries)
Common convergence of venous drainage from all structures below the diaphragm, located on posterior abdominal wall anterior to vertebral column & to the right of the abdominal aorta
Formed by union of common iliac veins at level L5. Then ascends superiorly, leaves abdomen by piercing central tendon of diaphgram at T8 (caval hiatus). In the thorax, it drains into right atrium of heart
During its long course, it shares an anatomical relationship with numerous abdominal structures, including —
Right common iliac artery, root of mesentery, head of pancreas, bile duct, portal vein, & liver
Tributaries —
Common iliac veins
Formed by external & internal iliac veins, draining lower limbs & gluteal region
Lumbar veins
Drain posterior abdominal wall *** (look at next flashcard)
Renal veins
Drain kidneys, left adrenal gland, & left testis/ovary
Right testicular/ovarian vein
Drains right testes/ovary (the left gonads drain into left renal vein)
Inferior phrenic veins
Drain the diaphragm
Hepatic veins
Drain the liver
No tributaries from spleen, pancreas, gallbladder, or abdominal part of GI tract — these structures are first drained into portal venous system
However blood from them eventually ends up in inferior vena cava after being processed by liver via hepatic veins
Lumbar veins
Special tributary of inferior vena cava — don’t all drain directly into inferior vena cava
5th lumbar vein — generally drains into iliolumbar vein (into common iliac vein)
3rd & 4th lumbar veins — usually drain into inferior vena cava
1st & 2nd lumbar veins — may empty into ascending lumbar veins
Ascending lumbar veins — long anastomosing venous channels connecting common iliac, iliolumbar, & lumbar veins with azygos & hemiazygos veins
**** — if inferior vena cava is blocked, ascending lumbar veins become important collateral channels between lower & upper parts of body
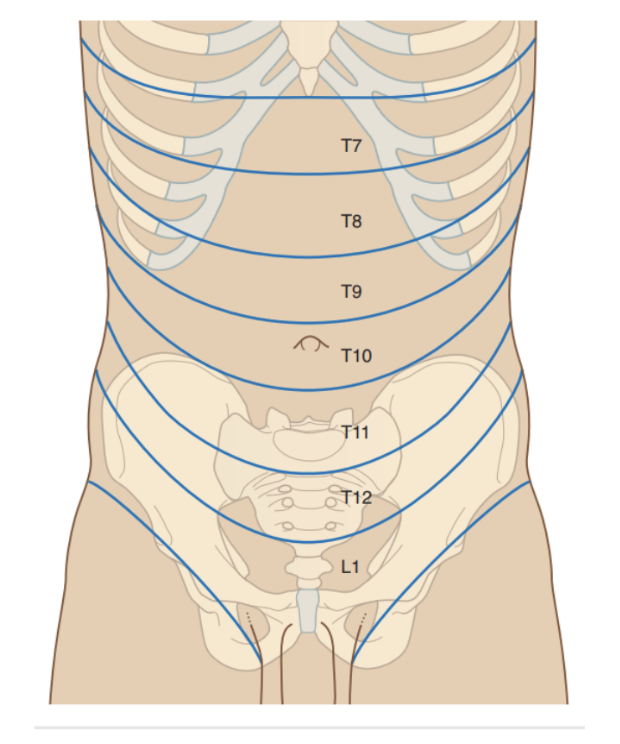
Innervation of the abdominal wall
Skin, muscles, & parietal peritoneum of the anterolateral abdominal wall are supplied by T7 to T12 & L1 spinal nerves
The anterior rami of these spinal nerves pass around the body (from posterior to anterior) in an inferomedial direction
As they proceed, they give off a lateral cutaneous branch and end as an anterior cutaneous branch
Path of T7-T11 nerves
Leave their intercostal space, passing deep to costal cartilages, & continue onto anterolateral abdominal wall (beteen internal oblique & transversus abdominis muscles)
Once reaching lateral aspect of rectus sheath, they enter it & pass posterior to lateral aspect of rectus abdominis
Approaching midline, an anterior curaneous branch passes through the rectus abdominis muscle & anterior wall of rectus sheath to supply the skin
Path of T12 & L1 nerves
follows similar path as intercostal nerves, however branches of L1 (iliohypograstric & ilioinguinal nerve), which originate from the lumbar plexus, deviate from this pattern once near their final destination
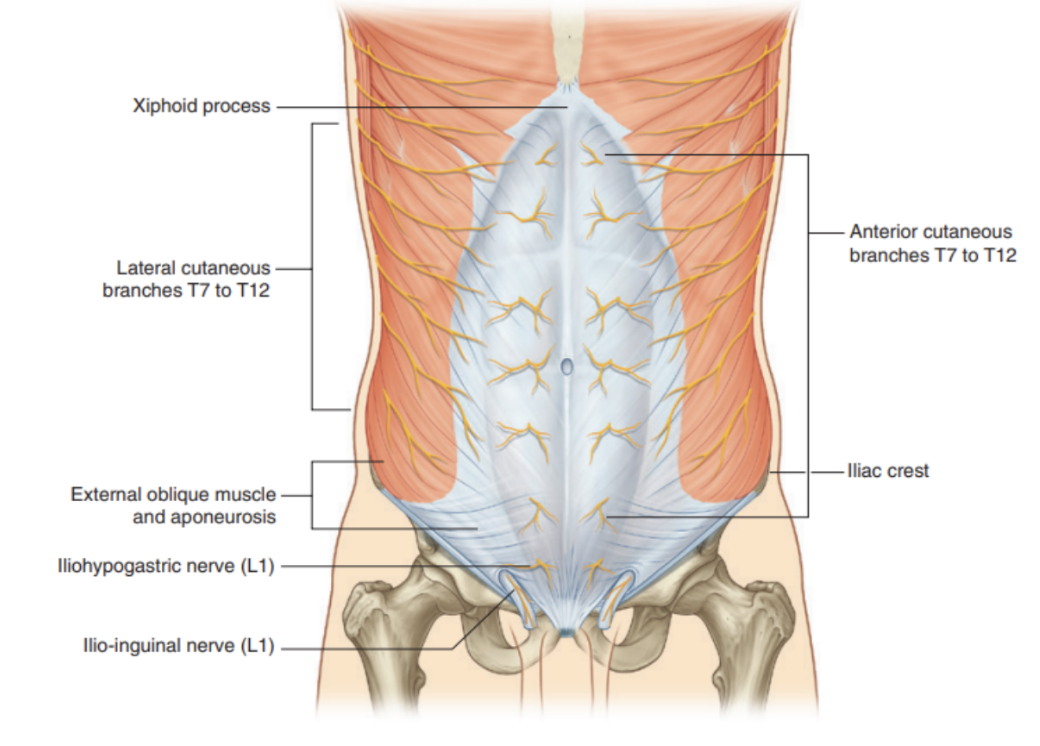
Dermatomal innervation
Innervation of abdominal wall terminates at innervation of skin — these nerves correspond to a different zone that their innervate —
Nerves T7-T9 supply the skin from xiphoid process to just above the umbilicus
T10 supplies skin around umbilicus
T11, T12, & L1 supply the skin from just below the umbilicus to (& including) the pubic region
Ilio-inguinal nerve (L1 branch) supplies anterior surface of scrotum or labia majora, & sends a small cutaneous branch to the thigh
During their course through the anterolateral abdominal wall, the thoracoabdominal, subcostal, & iliohypogastric nerves communicate with each other
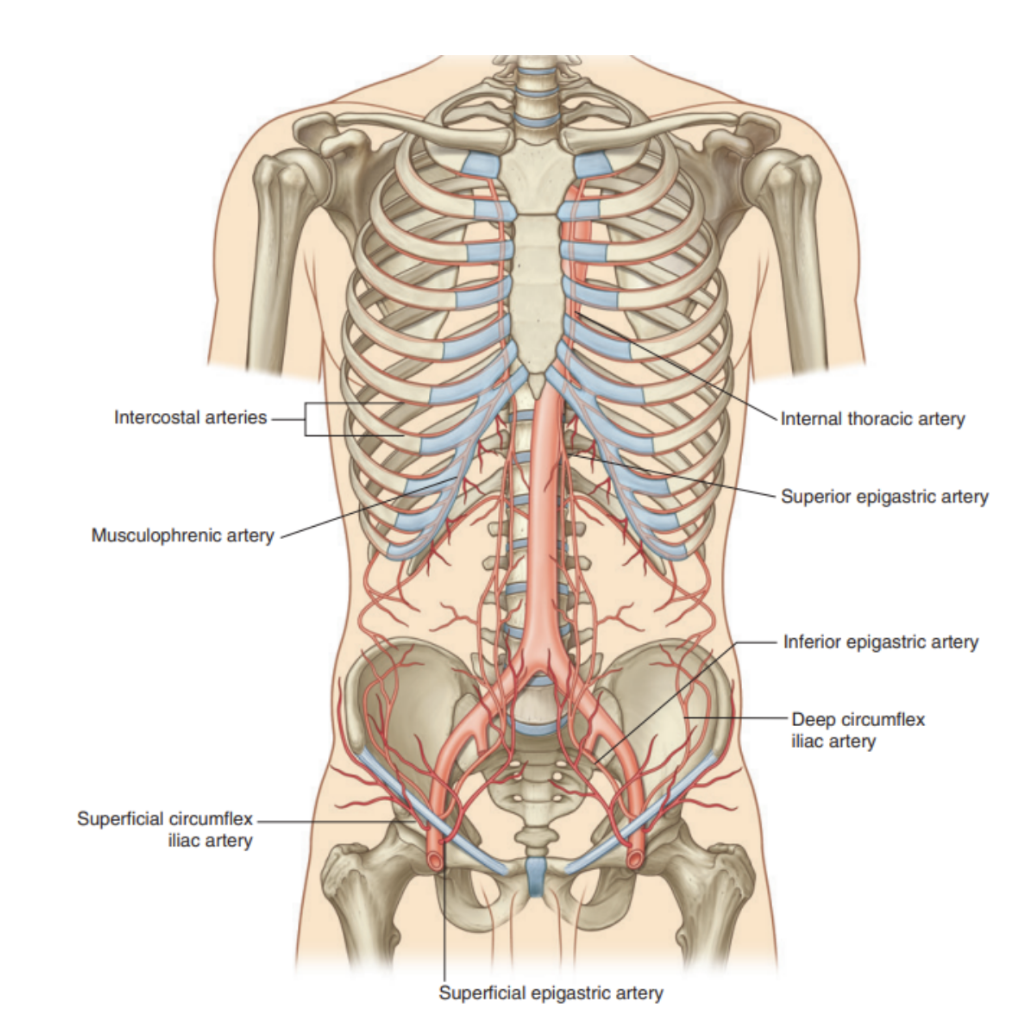
Arterial supply & drainage of anterolateral abdominal wall
Superficial branches
Musculophrenic artery —
Branch of internal thoracic artery, supplies superior part of superficial anterolateral abdominal wall
Superficial epigastric artery & Superficial circumflex iliac artery
Lateral to one another — branches of the femoral artery that supply the inferior part of the wall
Deep branches —
Superior epigastric artery
Terminal branch of internal thoracic artery
Runs in rectus sheath behind rectus muscle & supplies superior part of wall
Inferior epigastric artery & Deep circumflex iliac artery —
Both branches of external iliac artery & supply inferior part of the wall
Inferior epigastric artery enters rectus sheath after piercing the fascia transversalis & ands by anastomosing with the superior epigastric artery
Both superior & inferior epigastric arteries enter the rectus sheath, posterior to rectus abdominis in their course, & anastomose with each other
10th & 11th intercostal arteries & subcostal artery
Supply the lateral part of the abdominal wall