VS 6110 Final (pupils and clinical pupil testing)
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
Does an afferent pupillary defect present with anisocoria?
never
What causes an afferent pupillary defect?
damage to the optic nerve
Does an efferent pupillary defect present with anisocoria?
yes! -- muscles innervation is impacted
What are efferent pupillary defects?
1. Horner's syndrome
2. parasympathetic damage
What are the types of Horner's syndrome?
1. central -- Wallenberg syndrome
2. preganglionic
3. postganglionic
What are the types of efferent parasympathetic damage?
1. central
2. preganglionic
3. postganglionic
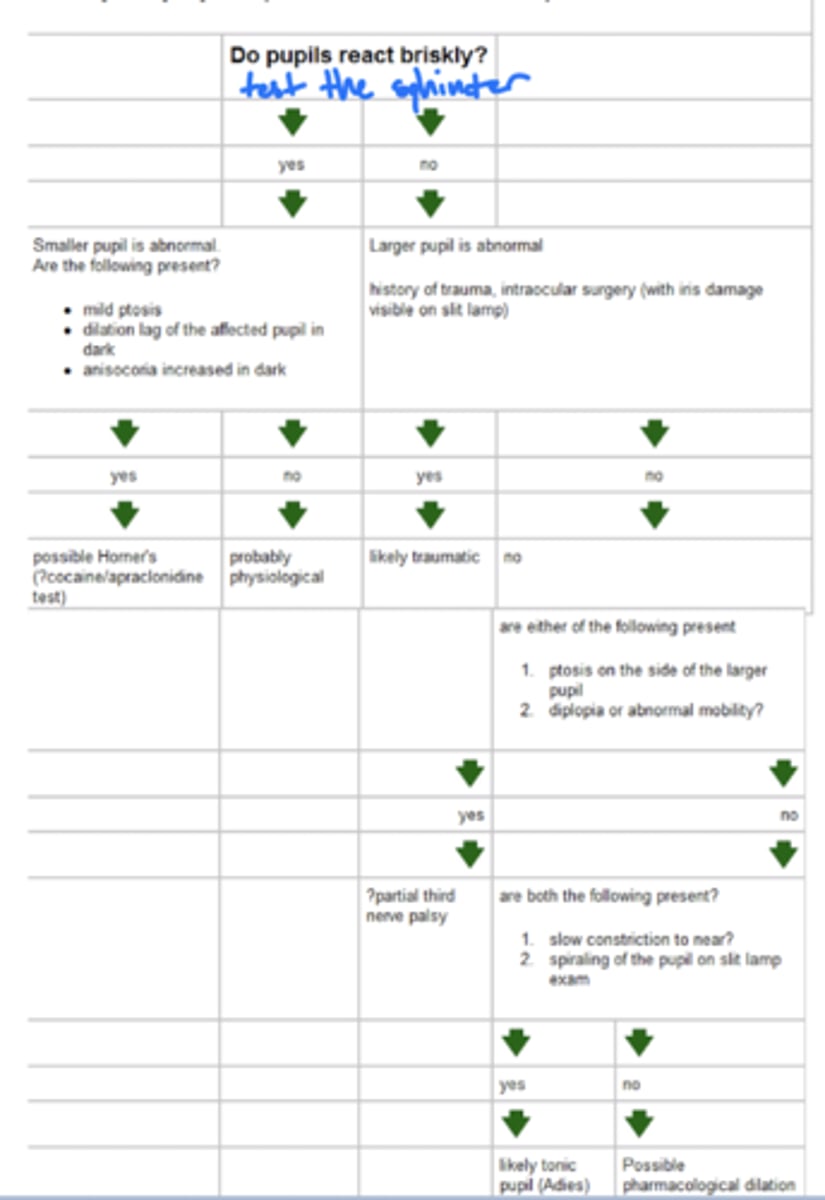
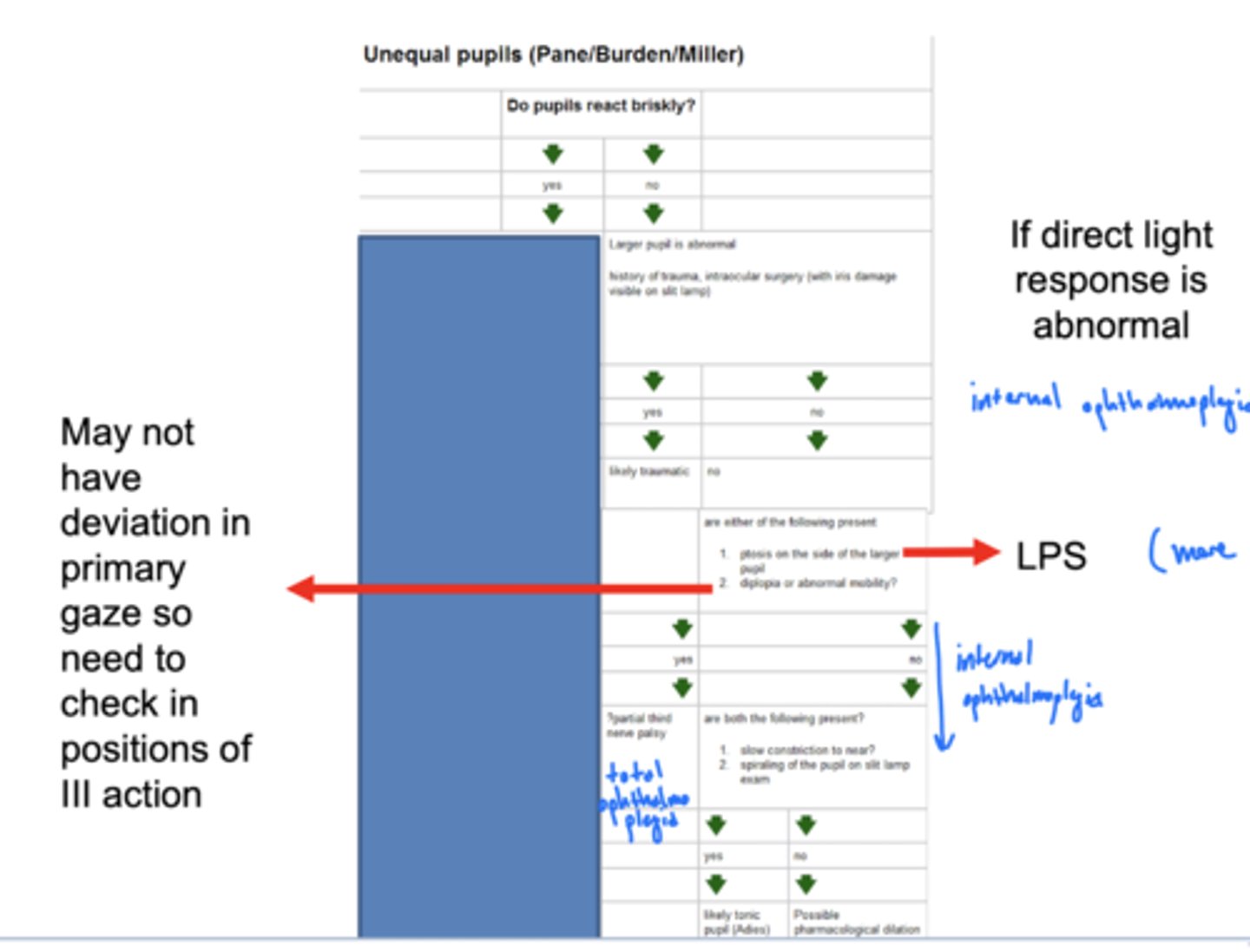
What should the first test be if someone presents with anisocoria?
Do the pupils react briskly?
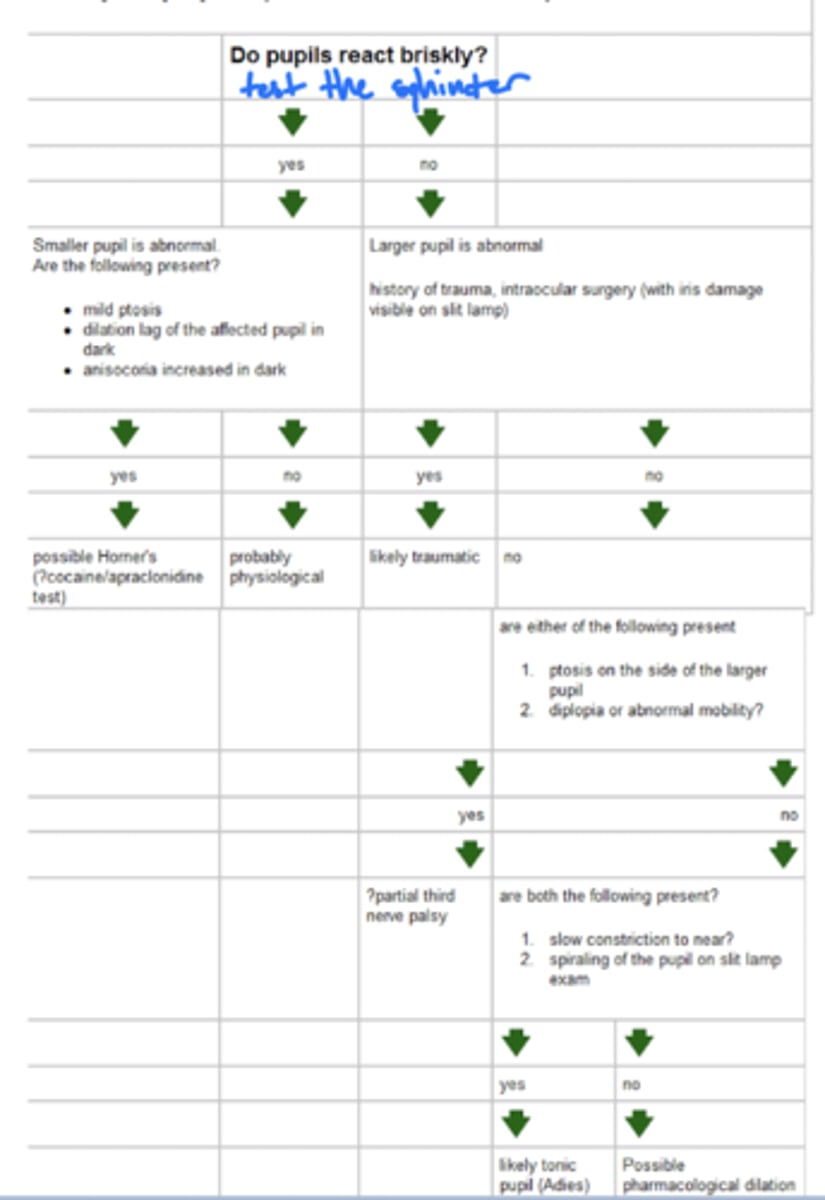
What does the direct light response test tell you (first thing)?
test the sphincter muscle (do the pupils respond briskly?)
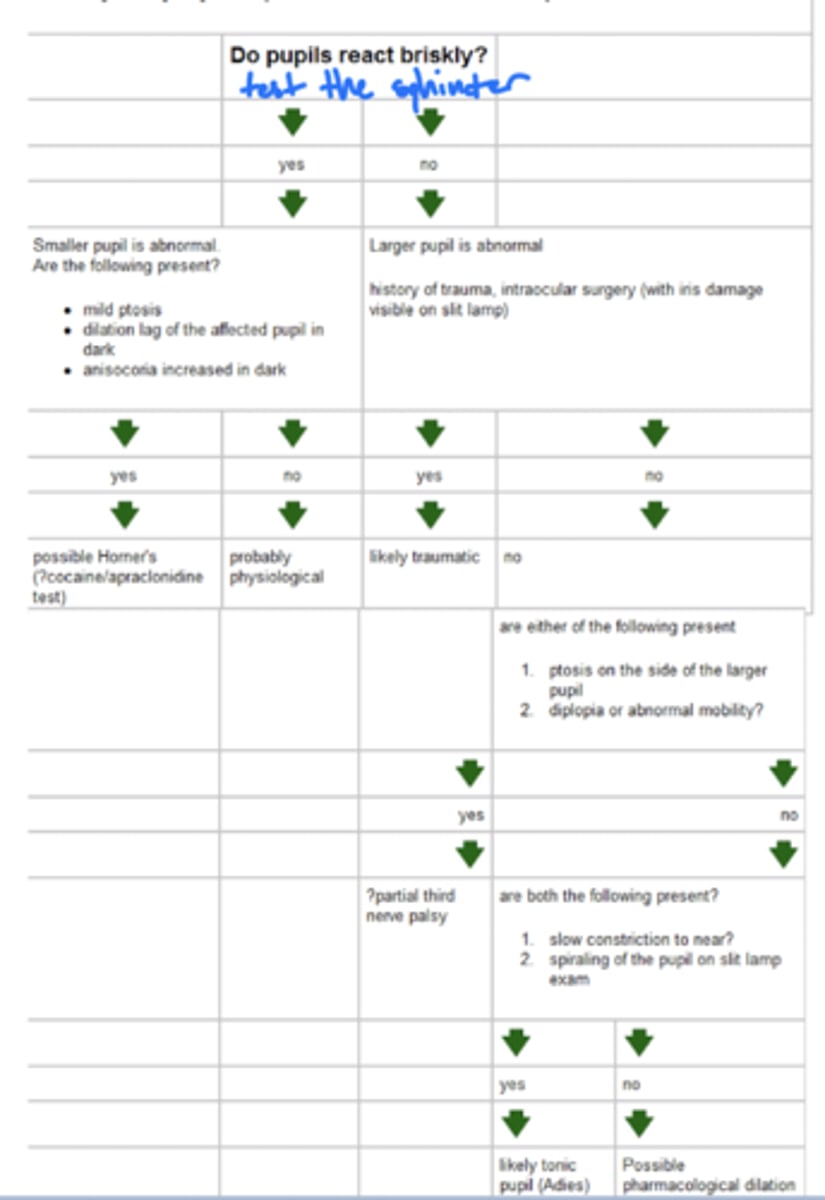
What if the pupils do respond briskly, but there is still anisocoria (what should you think)?
1. not sphincter (i.e. dilator muscle)
2. which pupil is abnormal?
3a. smaller = Horner's
3b. neither benign
why smaller = Horner's? -- decreased sympathetic innervation to the dilator muscle
What does it mean if anisocoria worsens in bright light?
parasympathetic is affected
What does it mean if anisocoria worsens in dim light?
sympathetic is affected
What is the sympathetic pathway to the eye (to dilator muscle)?
1. internal carotid
2. ophthalmic
3. nasociliary
4. long ciliary nerve
5. iris dilator
6. mydriasis
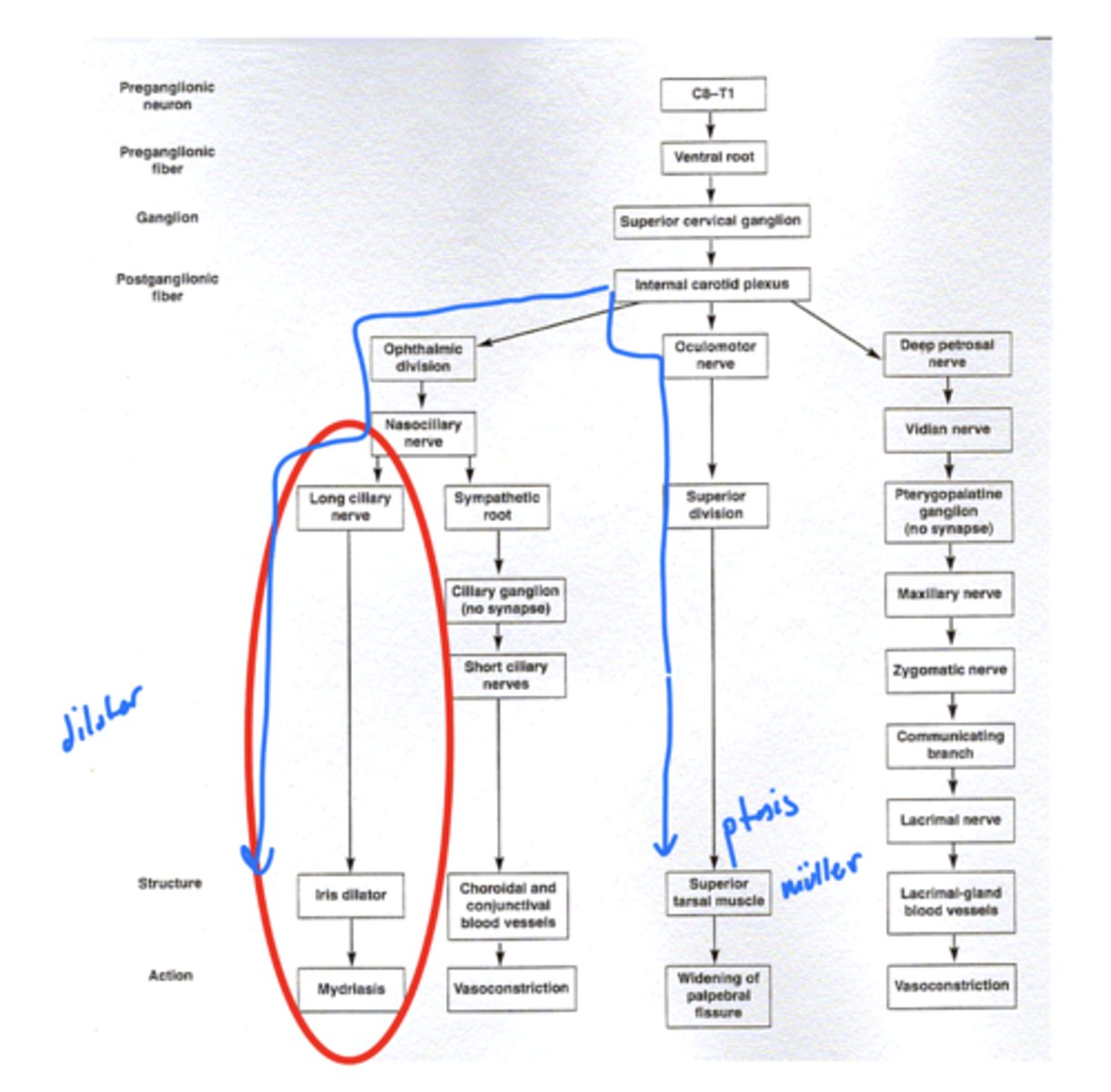
What are the margin reflex distance?
two of them
MRD 1 (red) -- measurement from pupillary reflex to center of upper lid
MRD 2 (orange) -- measurement from pupillary reflex to center of lower lid

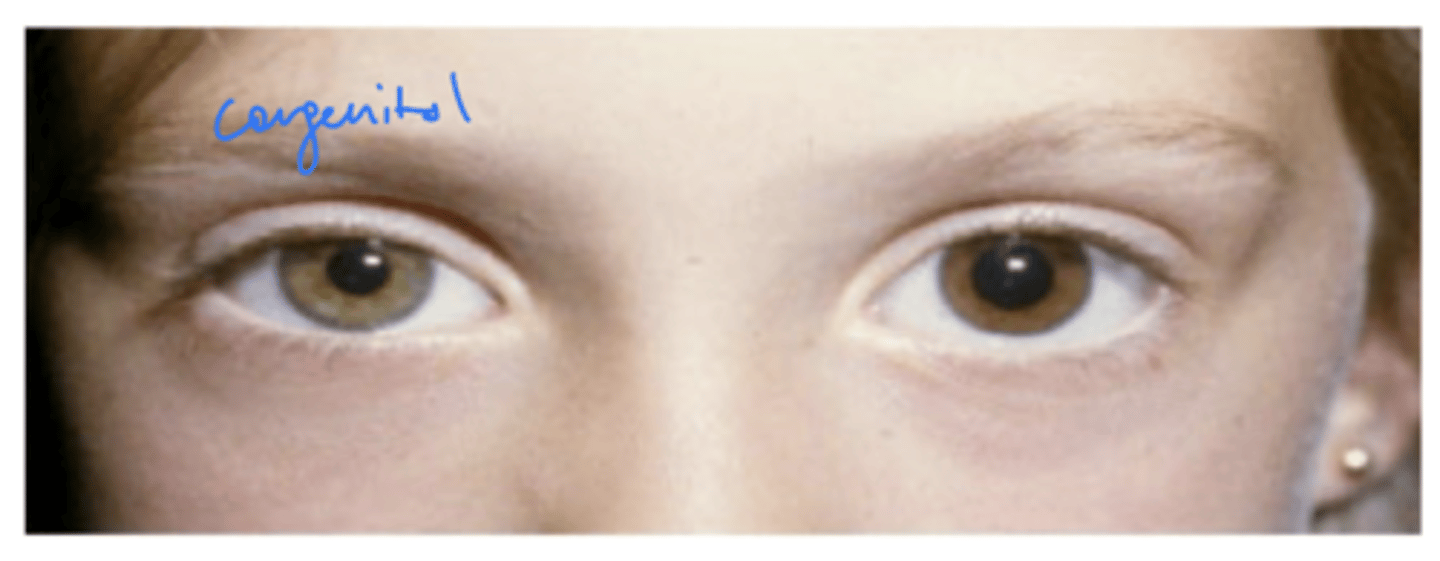
How can you tell if there's congenital Horner's syndrome?
congenital -- color change of the iris
cannot tell if it is blue eyes
What does it mean if the pupils don't respond briskly and the larger pupil is abnormal?
1. parasympathetic problem
2. likely from trauma (benign) -- can be from surgery
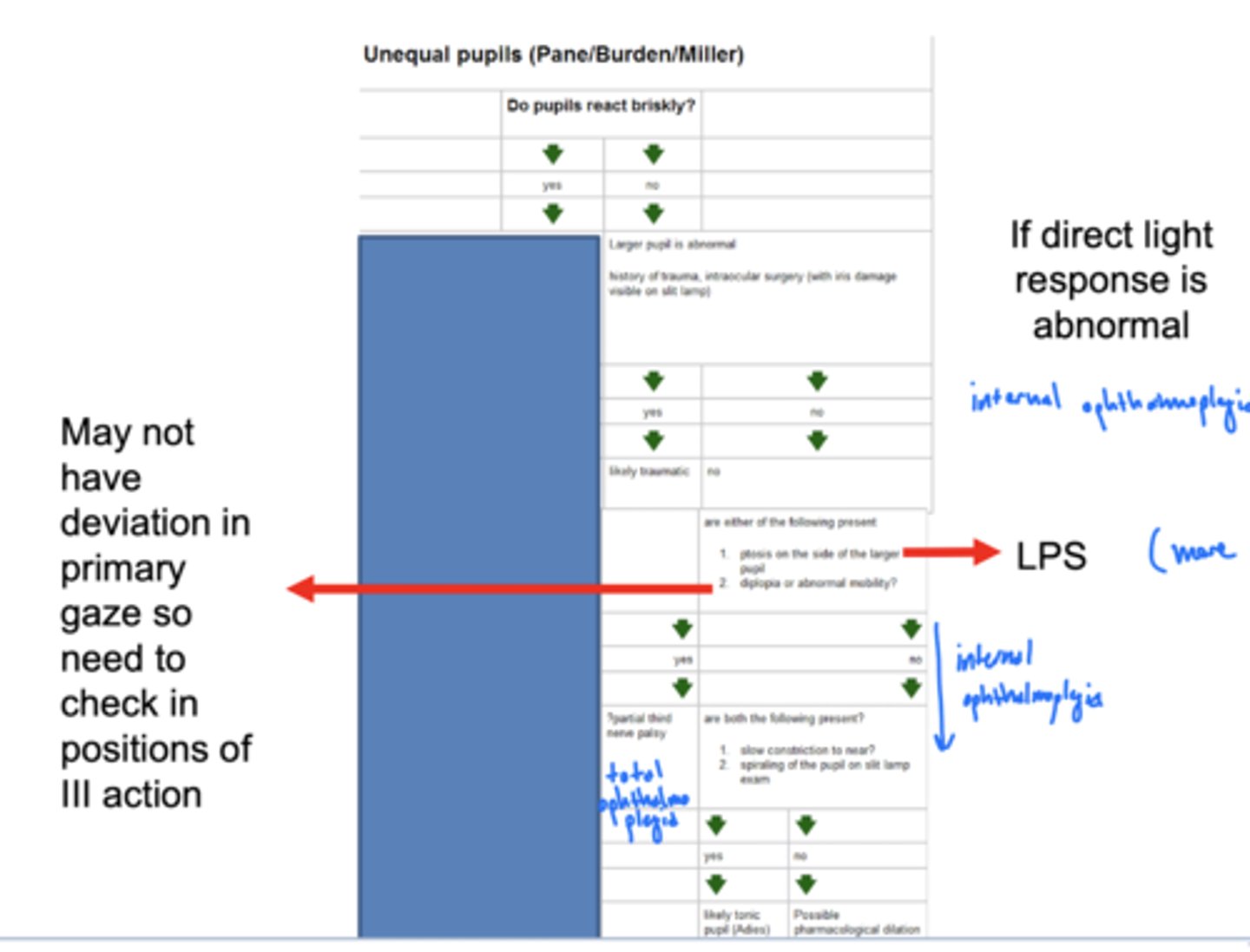
What does it mean if the pupils don't respond briskly and the larger pupil is not abnormal (both are abnormal)?
parasympathetic problem, but some type of ophthalmoplegia (total or internal)
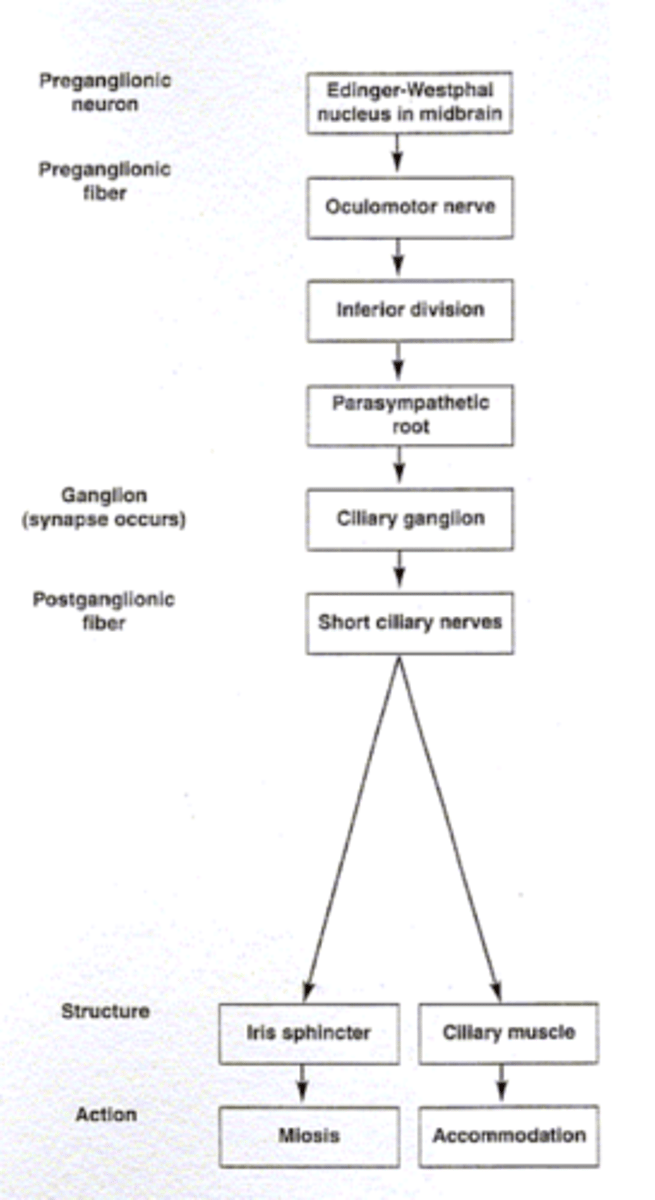
What is the parasympathetic route to the sphincter muscle?
1. EW nucleus
2. oculomotor nerve (CN III)
3. ciliary ganglion
4. short ciliary nerve
5. iris sphincter
What differentiates a complete and internal ophthalmoplegia?
complete -- extreme ptosis (LPS), deviation (both motor and parasympathetic). internal: pupil only
Why is complete ophthalmoplegia a medical emergency?
tumor could be pushing on CN III
What is vermiform movement?
some areas come in more than other (non-uniformal) when pupil constricts
no vermiform movement -- 360º movement of pupil
Why is non-vermiform movement bad?
complete ophthalmoplegia -- medical emergency
assume compression of III by an aneurysm or tumor near interpeduncular fossa (compression of preganglionic)
What is Adie's pupil?
presents with vermiform movement -- idiopathic inflammation of ciliary ganglion therefore postganglionic loss
Is Adie's pupil pre or postganglionic lesion?
postganglionic
What drug confirms Adie's pupil (vermiform movement) and why?
dilute pilocarpine (0.125%)
why? -- postganglionic causes hypersensitivity of muscarinic receptors, dilute will not affect either healthy or preganglionic
What else does Adie's pupil present with?
poor tendon reflexes -- non-progressive defect of autonomic system
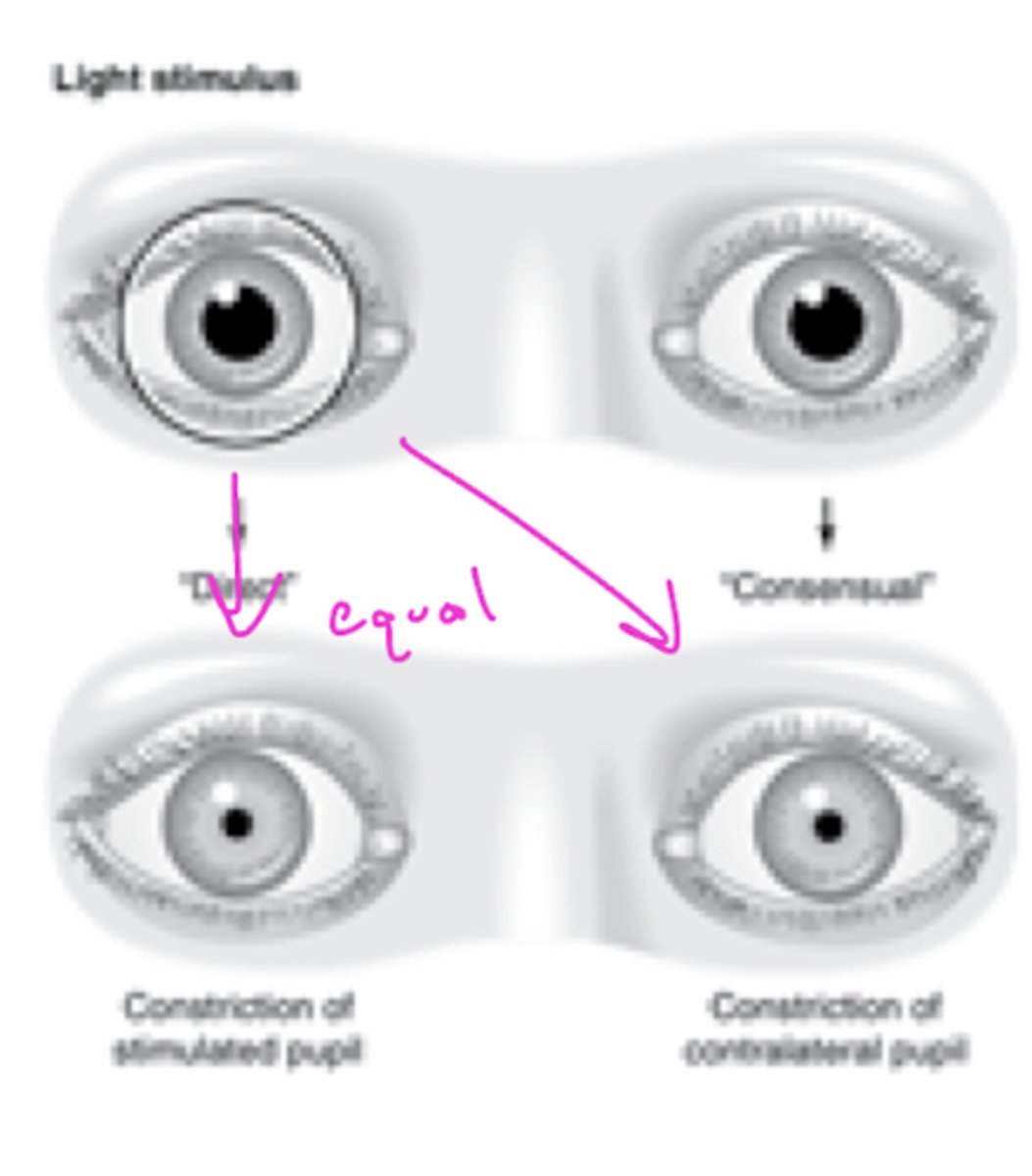
What is a direct pupil response?
eye with light constricts
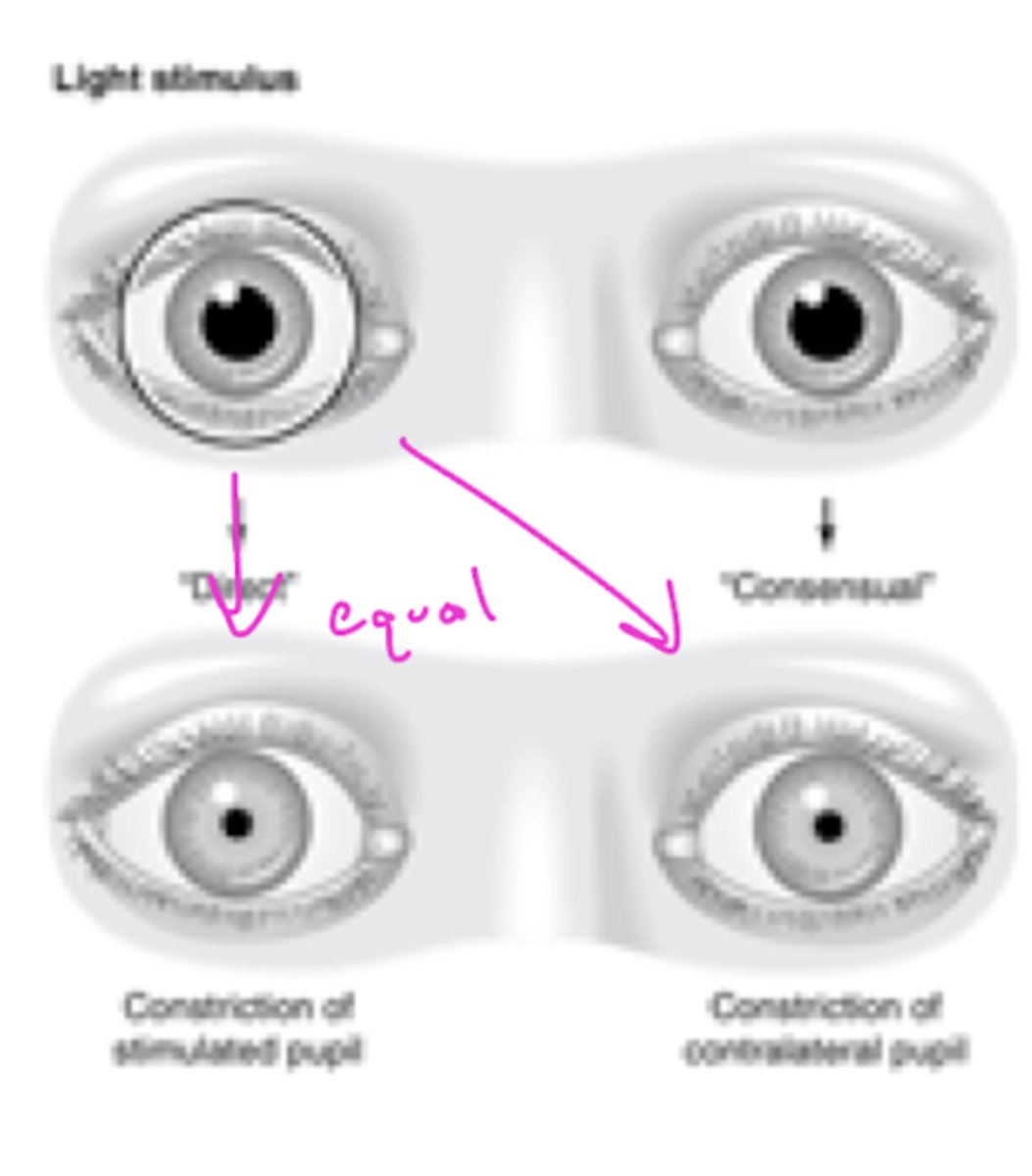
What is a consensual pupil response?
eye without light consensually constricts (magnitude should be the same)
Why do retinal ganglion fibers bypass the LGN?
reach the pretectal nucleus for the pupillary reflex
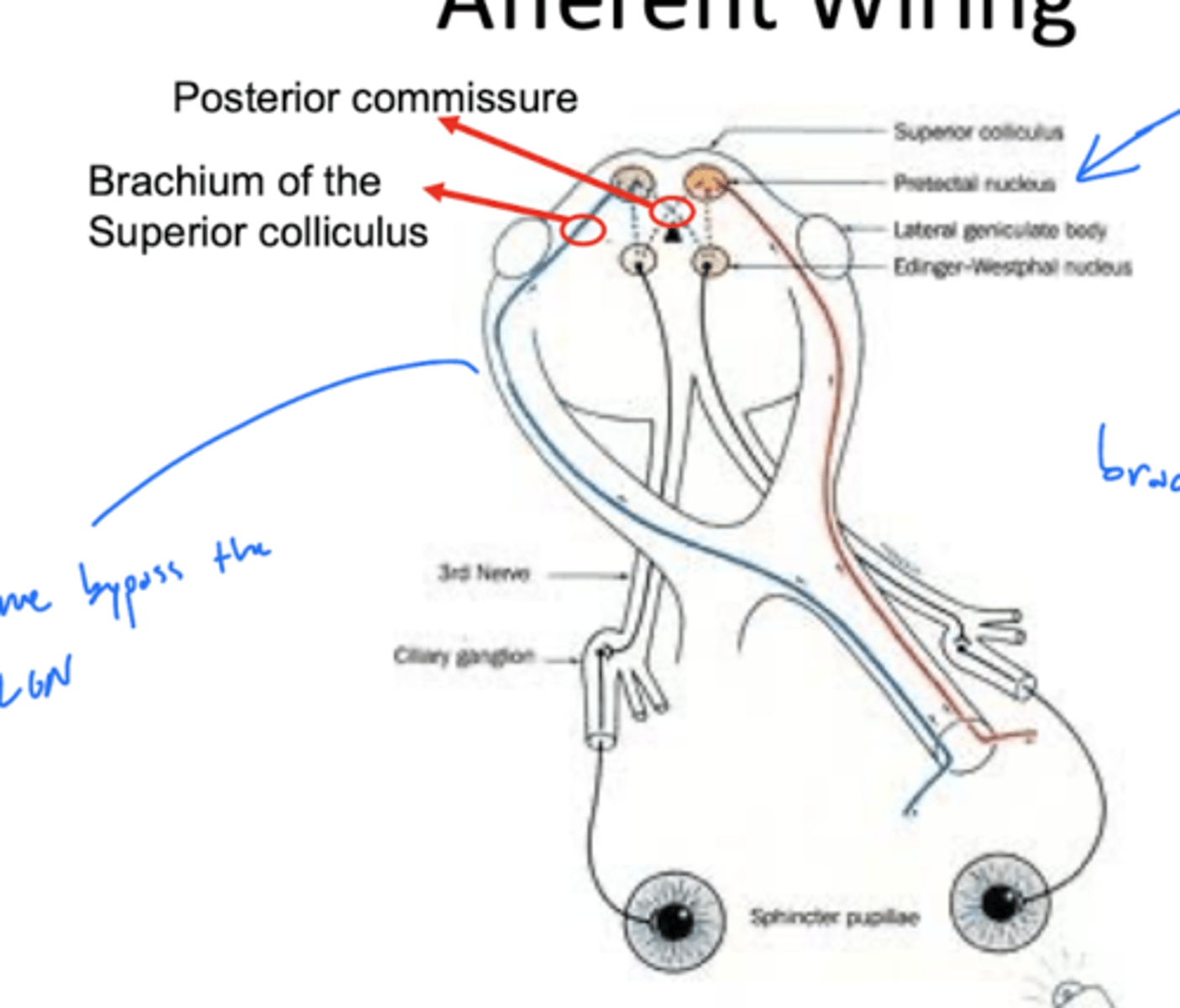
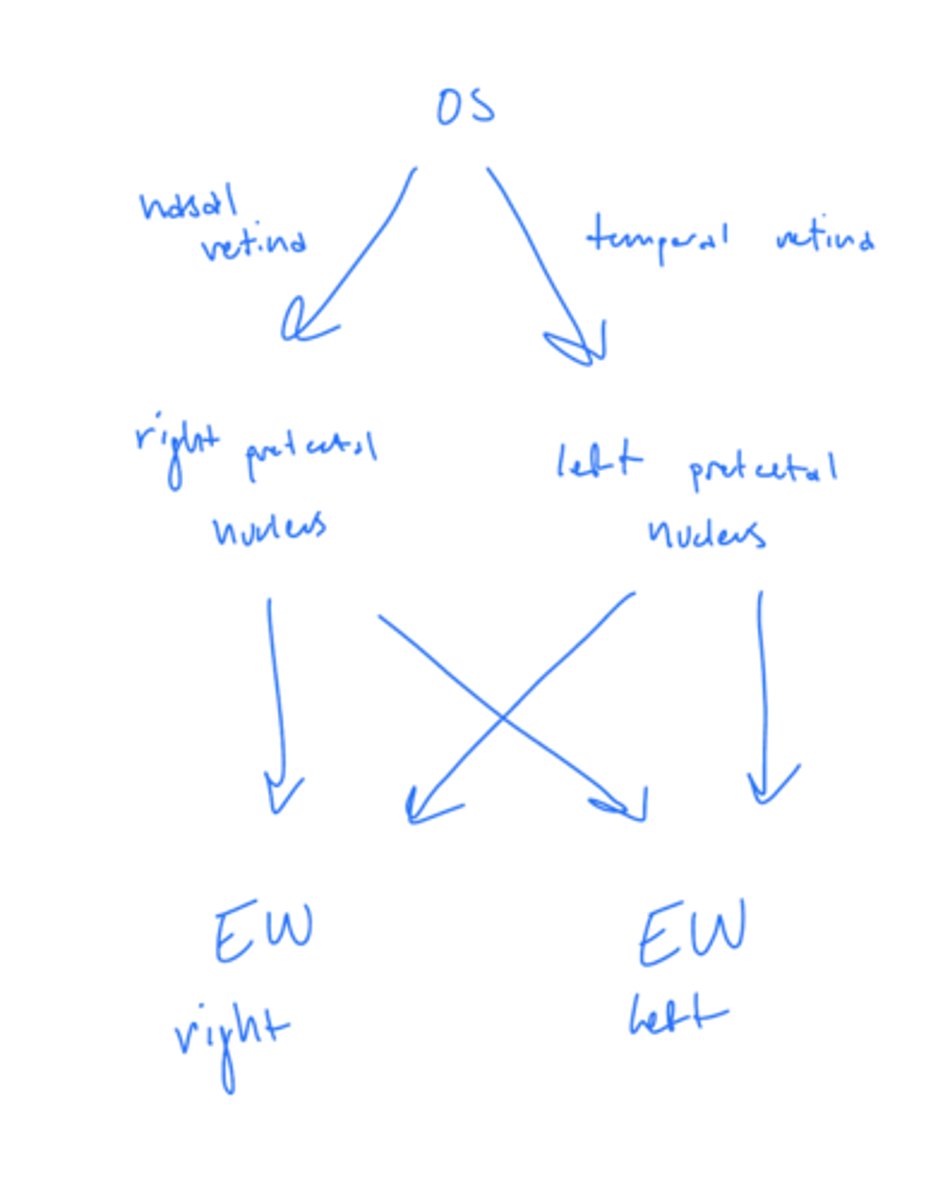
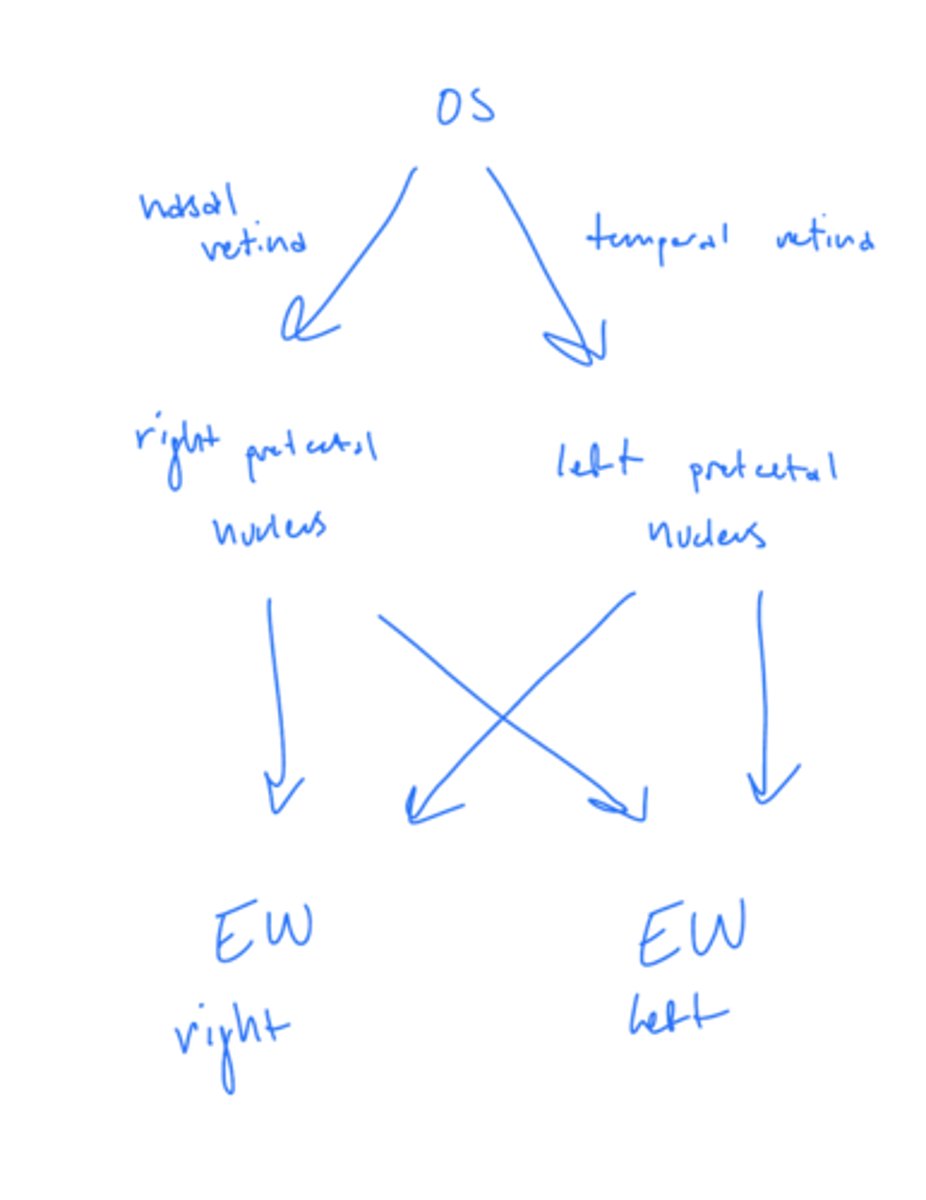
Where does the temporal retina project in the afferent pupillary light reflex?
ipsilateral pretectal nucleus (red)
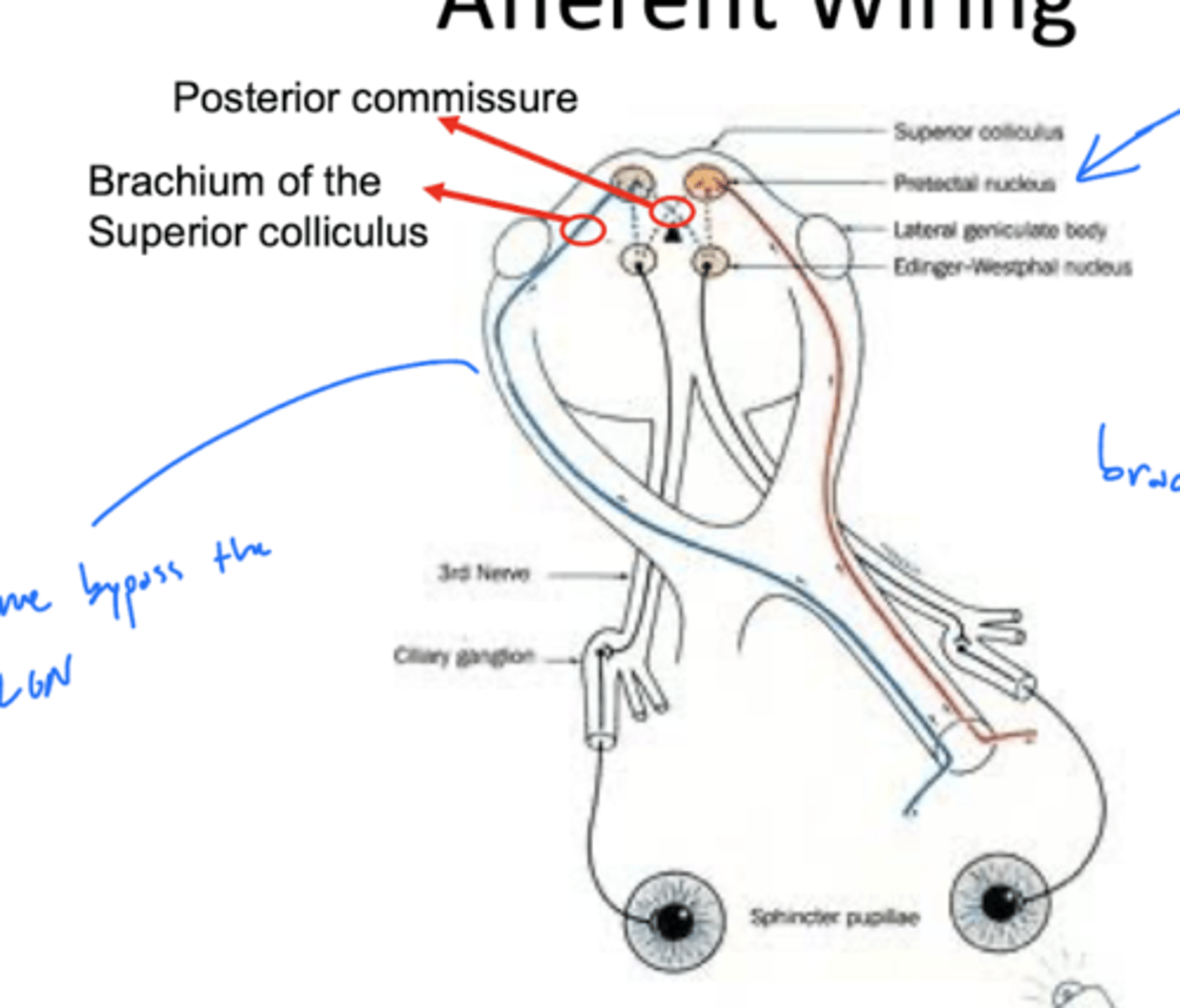
Where does the medial retina project in the afferent pupillary light reflex?
contralateral pretectal nucleus (blue)
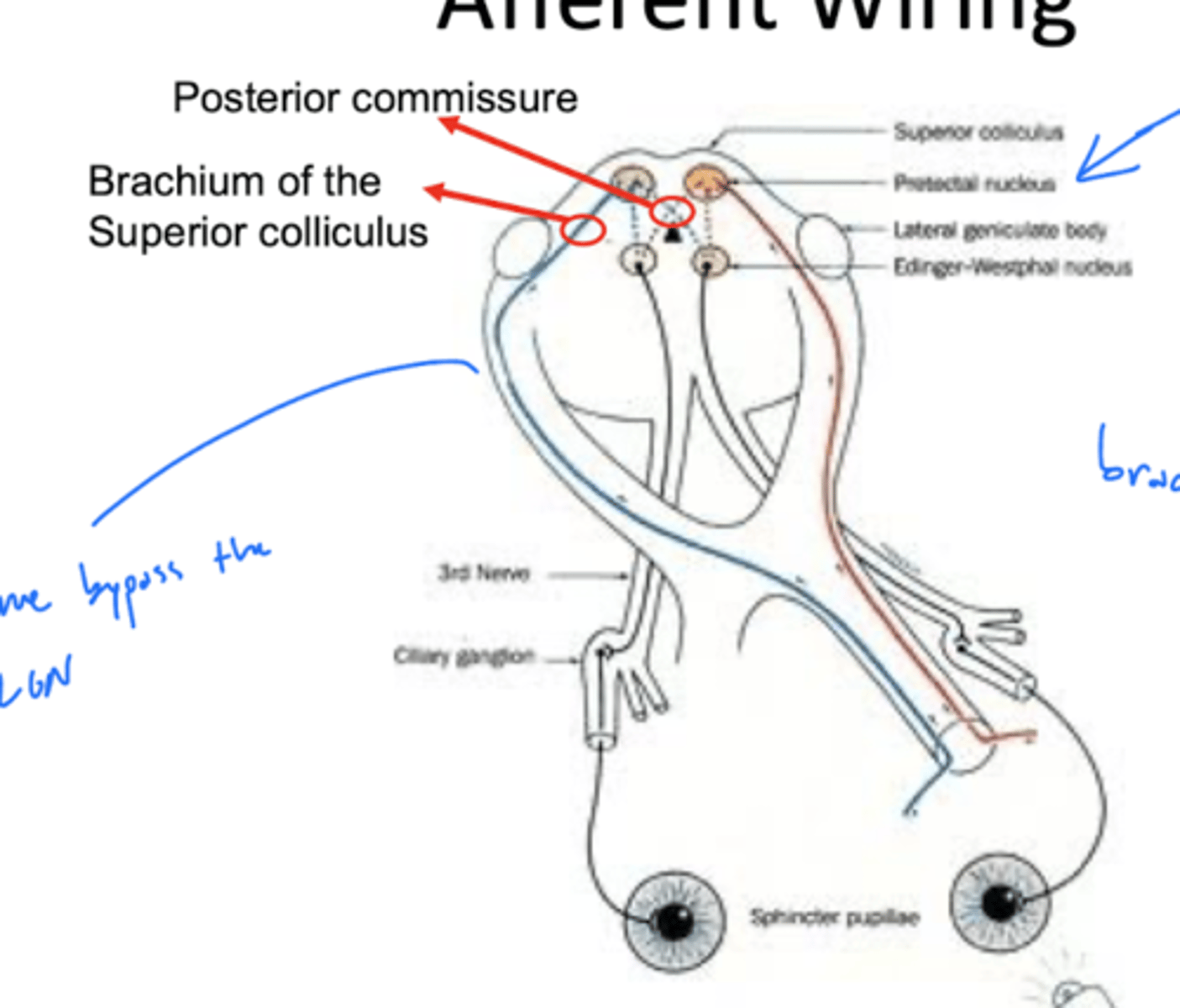
Where is the pretectal nucleus?
mesencephalon at the level of the superior colliculus
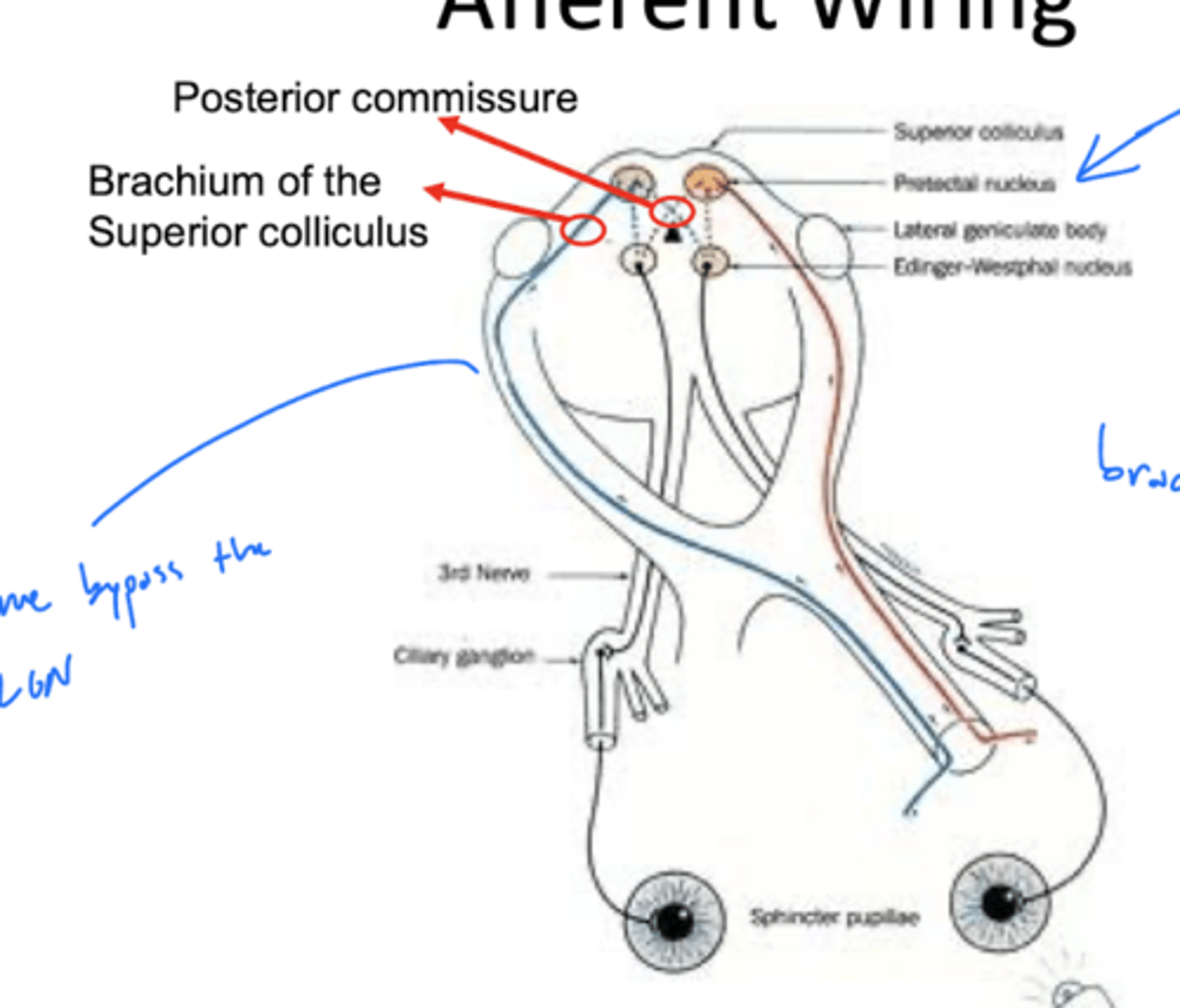
Where does the right pretectal nucleus project?
both left and right EW nuclei
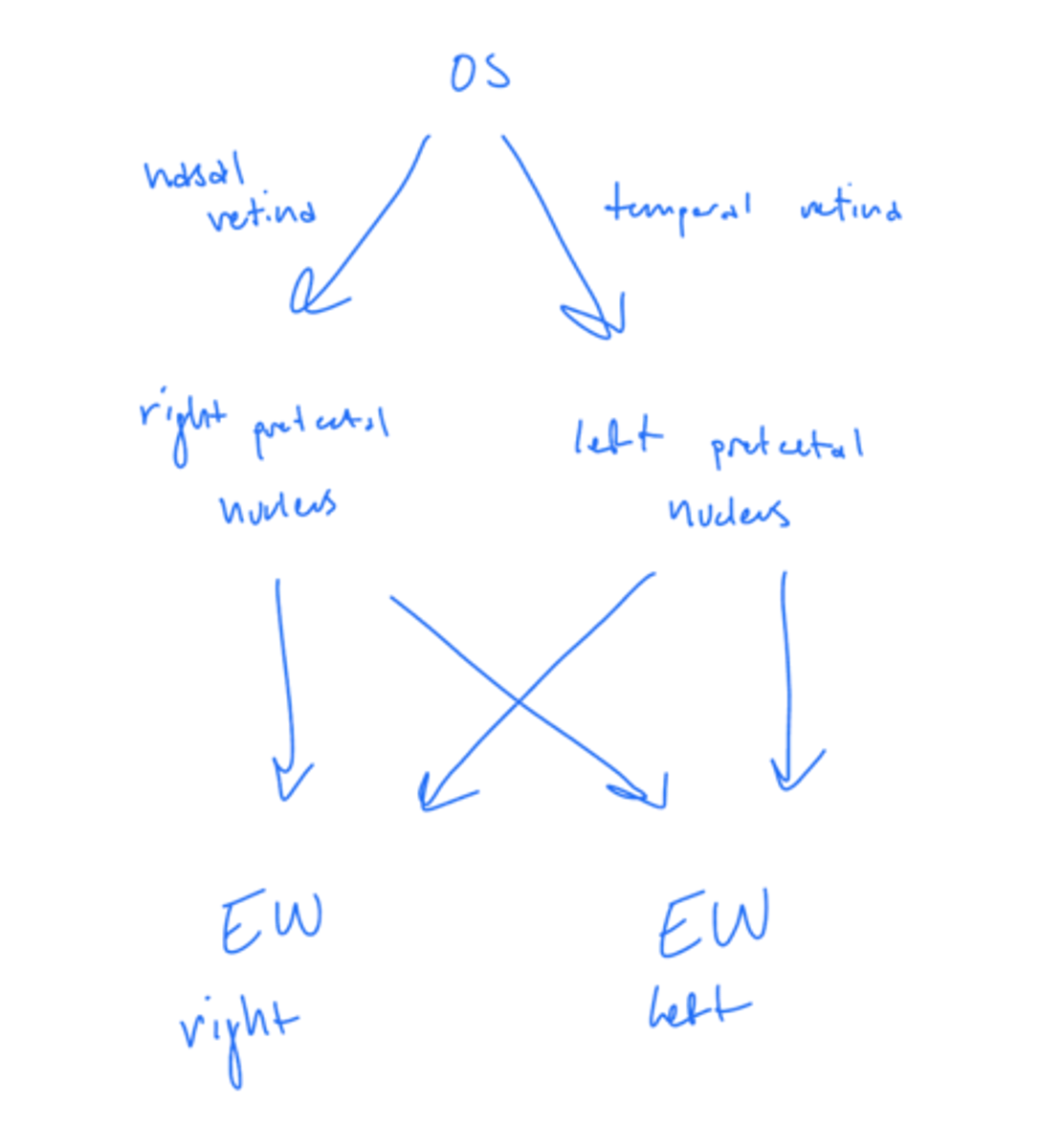
Where does the left pretectal nucleus project?
both left and light EW nuclei
Where do the fibers of the pretectal nucleus decussate?
posterior commissure
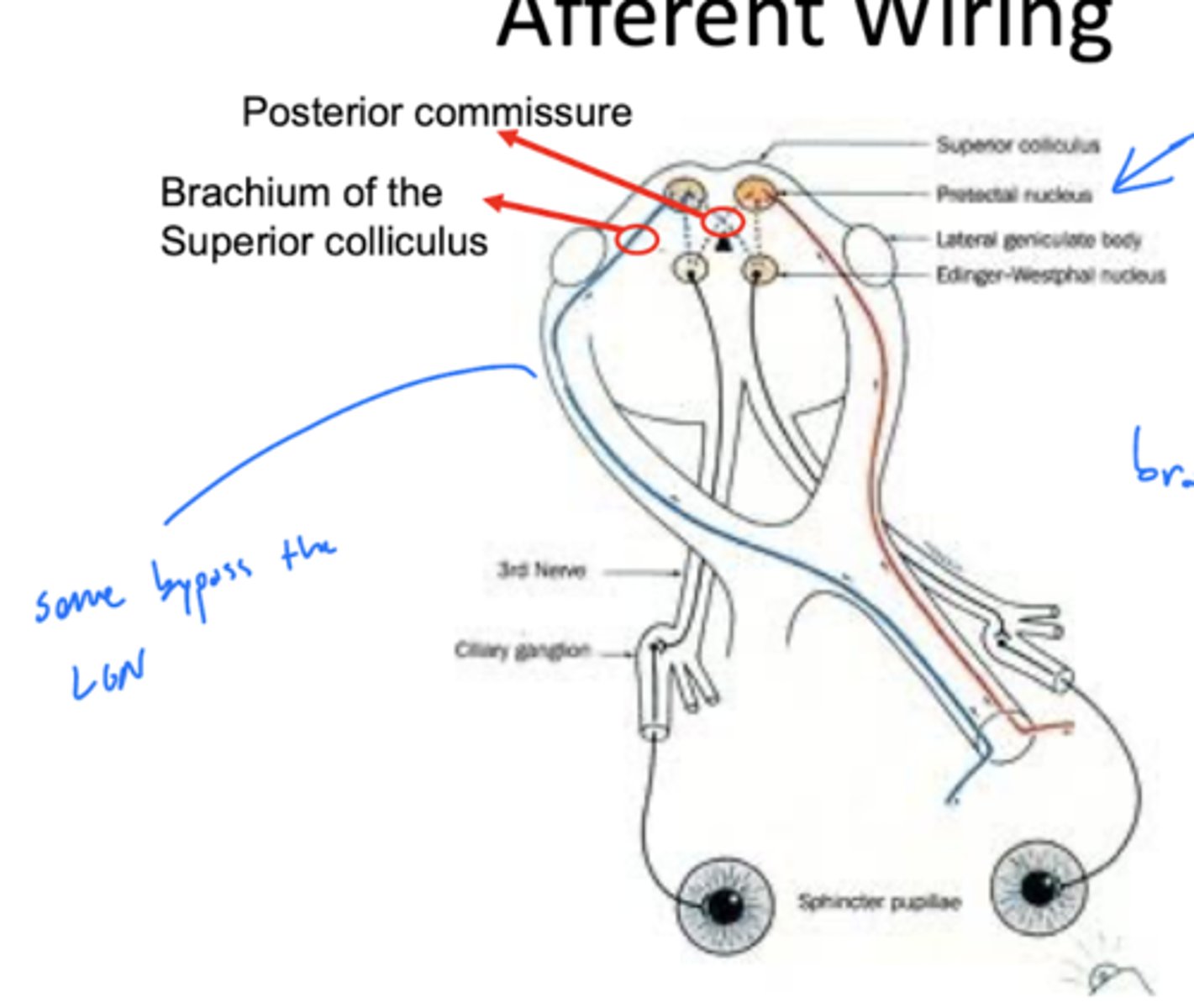
What is the consequence of the pretectal nuclei projecting to both EW nuclei?
consensual pupillary response -- both EW nuclei active which activates the sphincter pupillae in both eyes equally
What does the swinging flashlight test test?
consensual pupillary response
What is the swinging flashlight test?
1. shine light in OD and look at OD response (direct OD)
2. hold for 3 secs
3. "swing" light to OS, but continue to look at OD response (consensual OD)
4. hold for 3 secs
5. repeat above while looking at OS
Results of swinging flashlight test:
Light in OD
OD 5mm (direct) OS 5mm (consensual)
Light in OS
OD 3mm (consensual) OS 3mm (direct)
OD has an RAPD (rapid afferent pupillary defect)
Is anisocoria an afferent or efferent problem?
efferent
Why is there no anisocoria during an afferent issue?
unaffected eye is determining pupil size in BOTH eyes
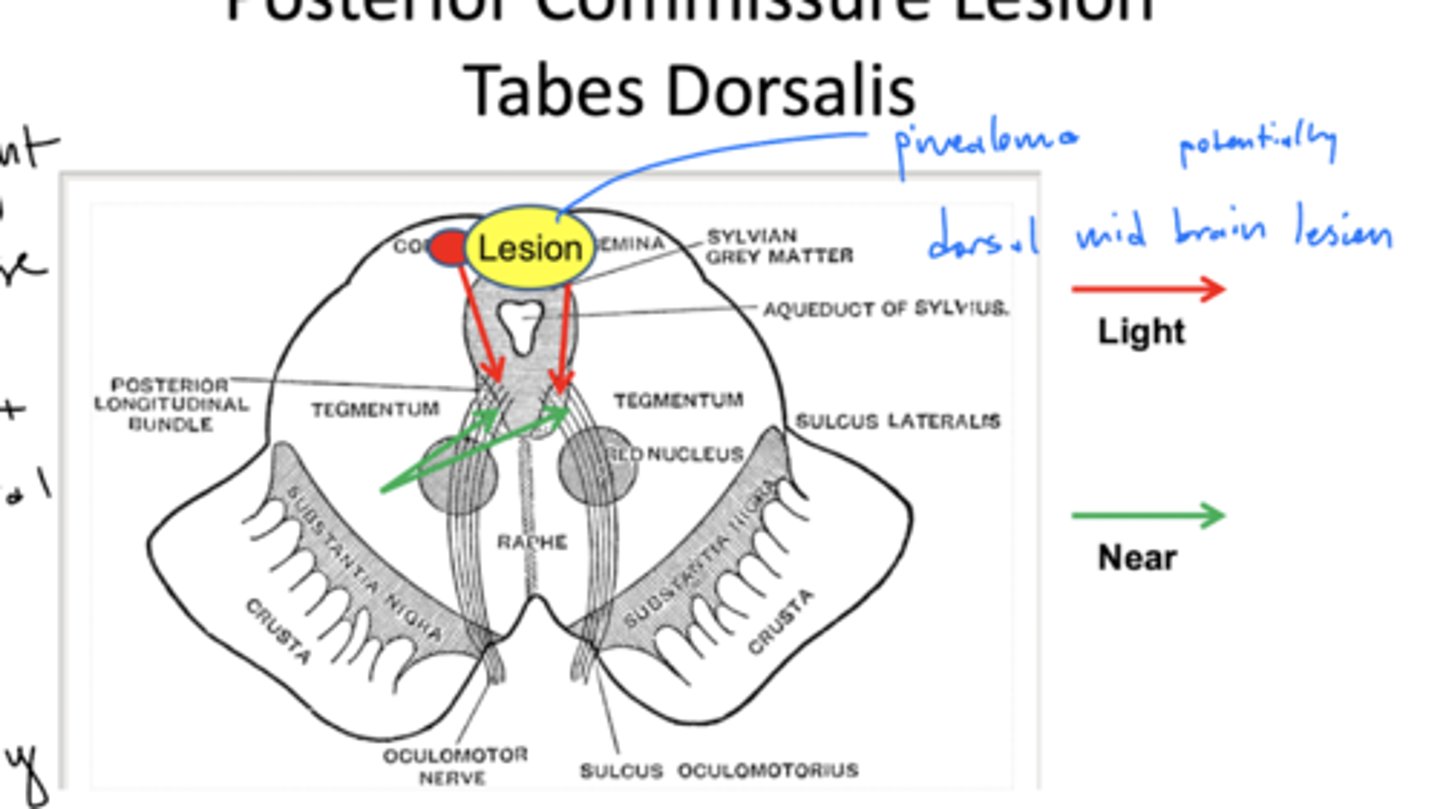
What is the difference in location of light vs. near response?
light -- posterior
near -- anterior
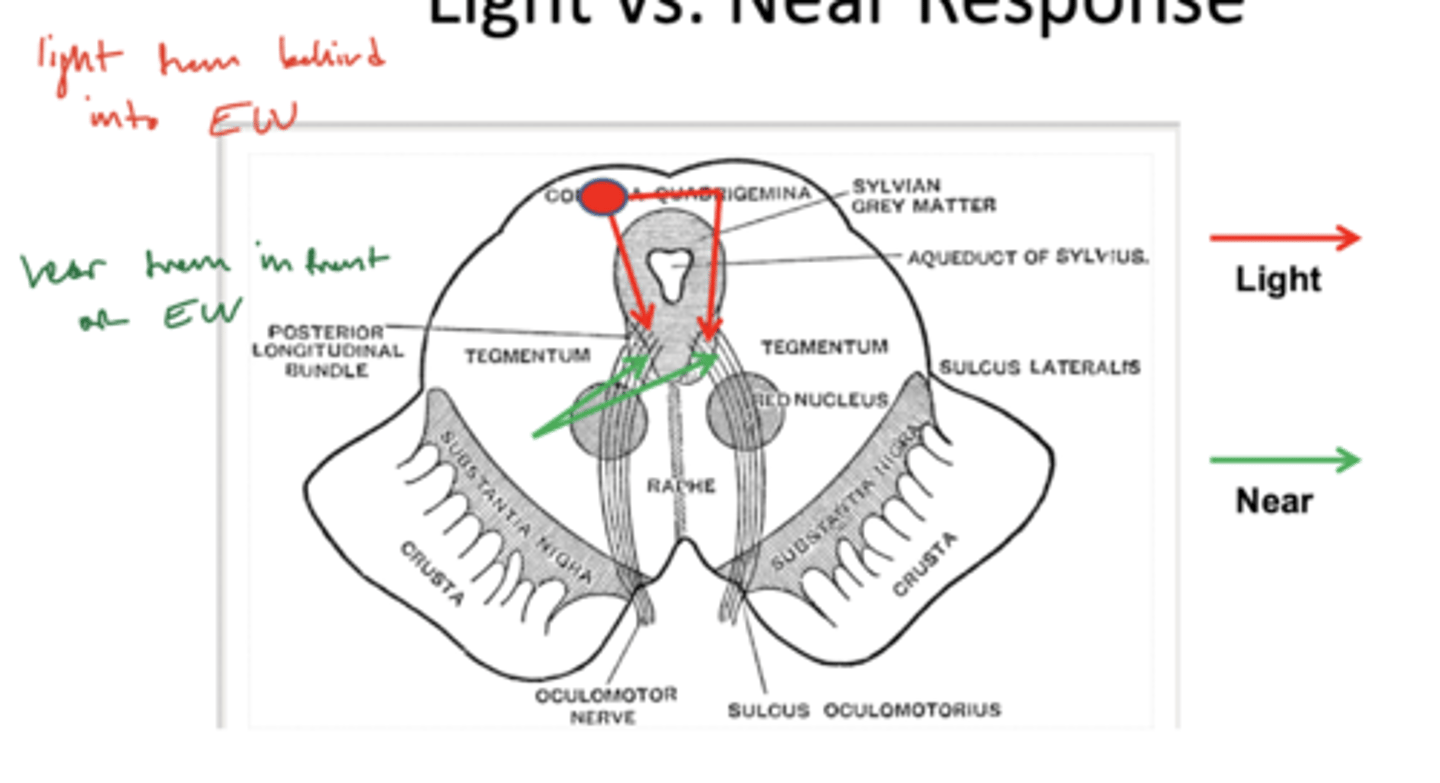
What does a posterior commissure lesion cause?
no light reflex
check near response!
What is a phoria?
position of the eyes in the absence of fusional vergence
What should the patient use to fix exophoria?
convergence
What should the patient use to fix esophoria?
divergence
What is an incomitant deviation?
beyond (con/di)vergence ability to fix -- deviation is worse when you force patient to use paretic muscle
Why is the deviation often the opposite direction of the muscle action?
non-paretic muscles act unopposed
example -- LR palsy would cause esotropia because MR has no resistance
What causes esotropia?
lateral rectus (CN VI) issues
What causes exotropia?
medial rectus (CN III) issues
What muscles pull the eye up?
1. superior rectus
2. inferior oblique
What muscles pull the eye down?
1. inferior rectus
2. superior oblique
What is hypertropia?
eye turns up
What is hypotropia?
eye turns down
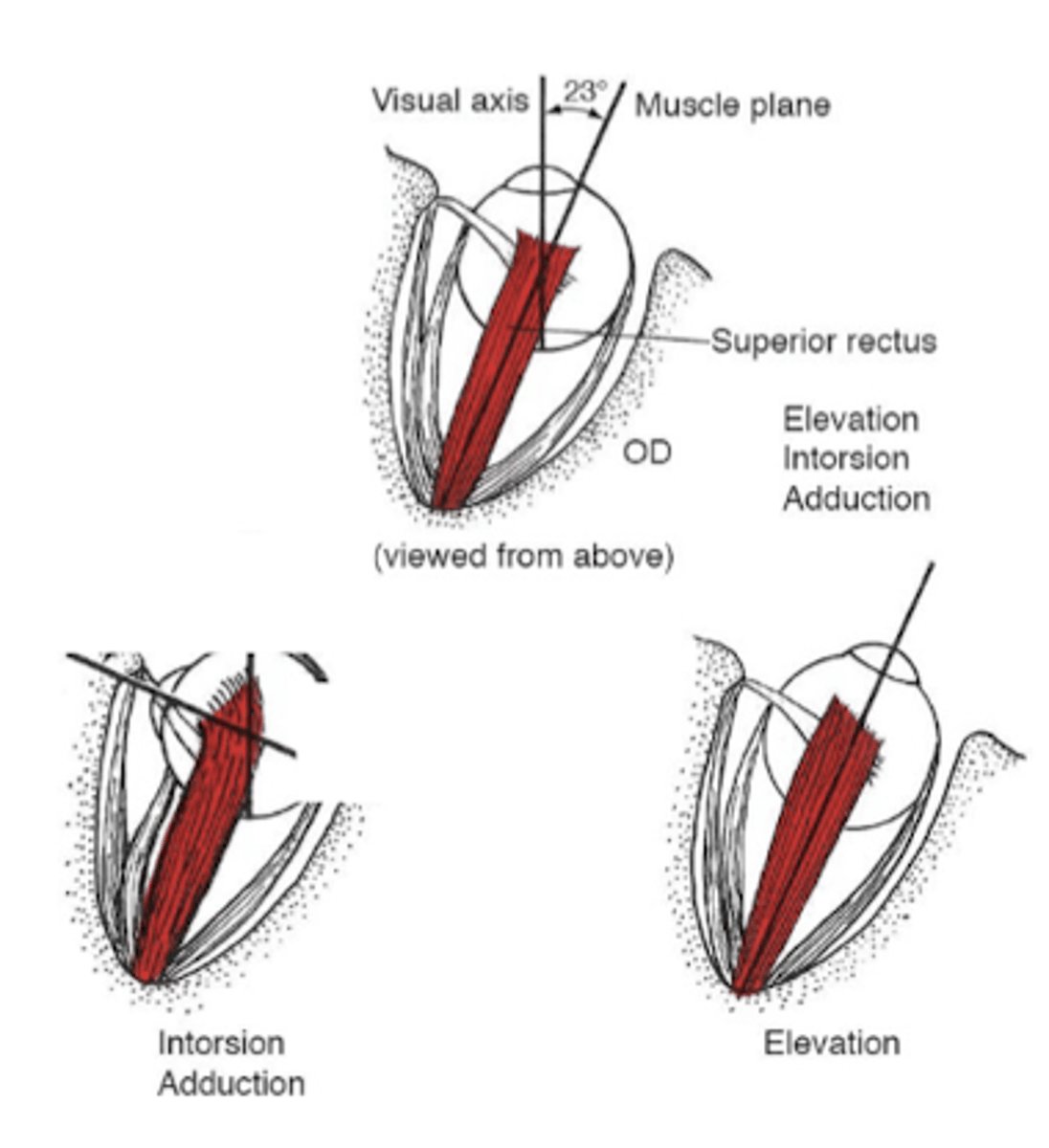
What is the orbital axis?
23º outwards
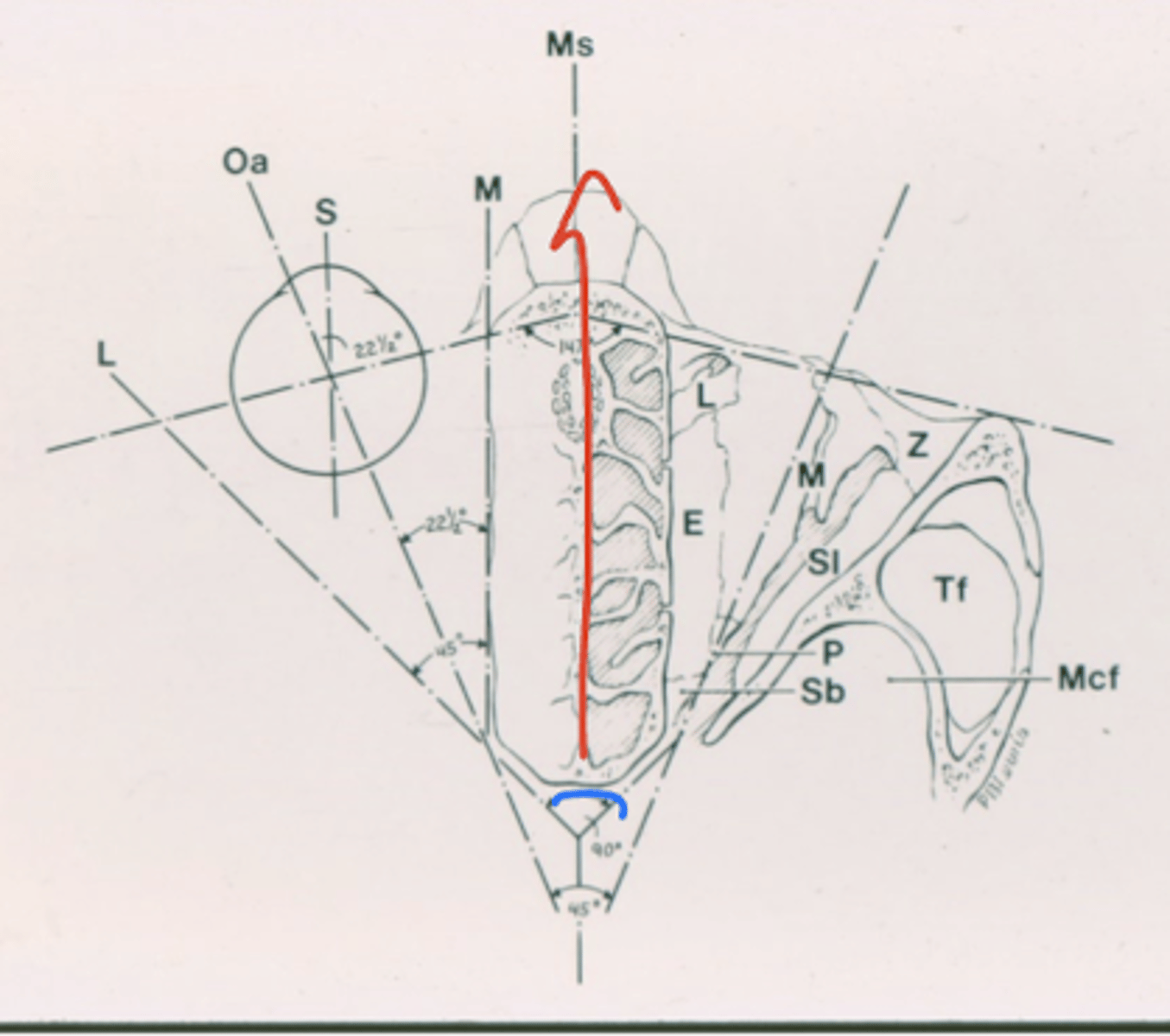
What is the axis of the superior/inferior rectus?
23º outwards -- same as orbital axis
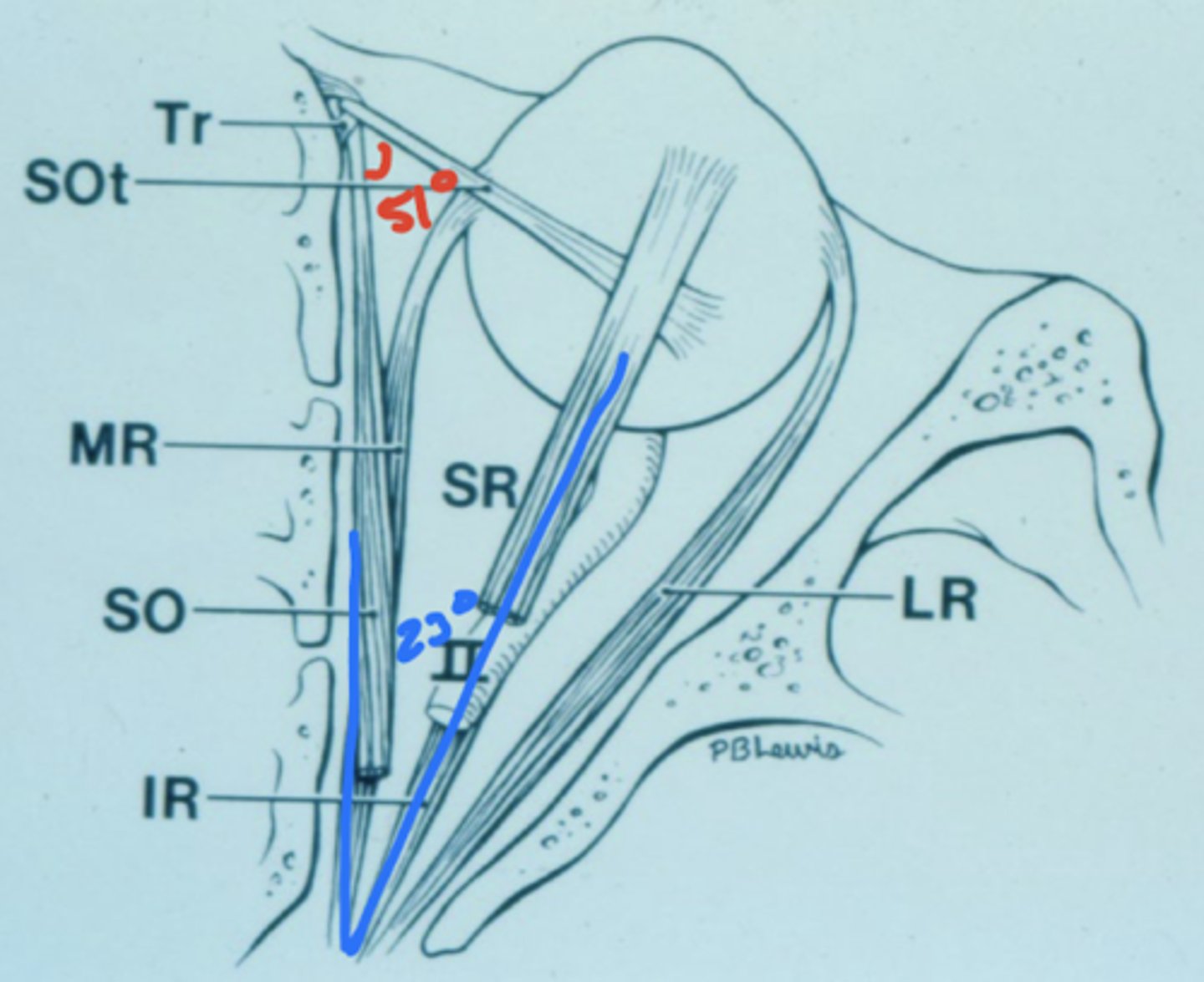
What is the axis of the superior/inferior oblique muscles?
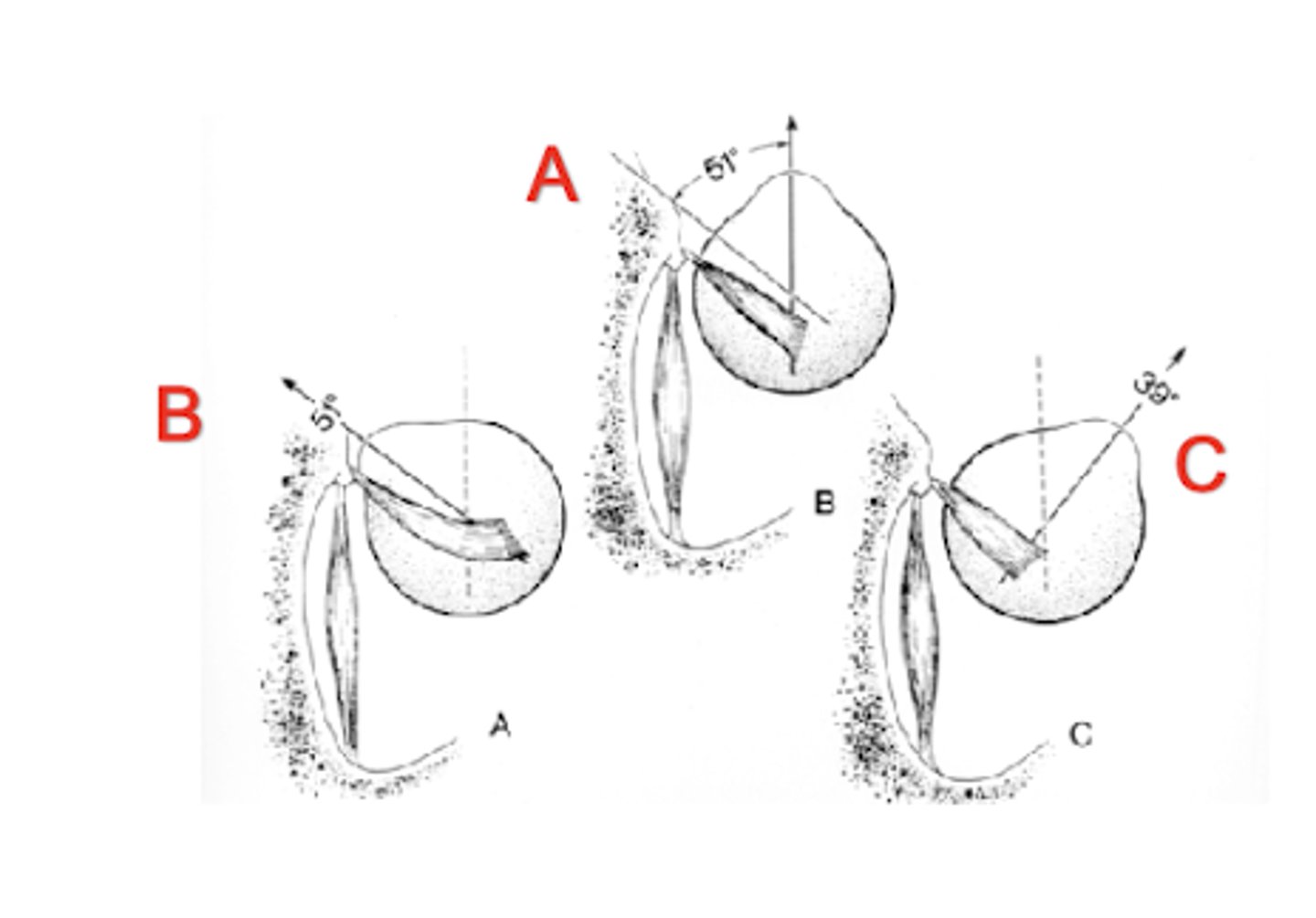
51º
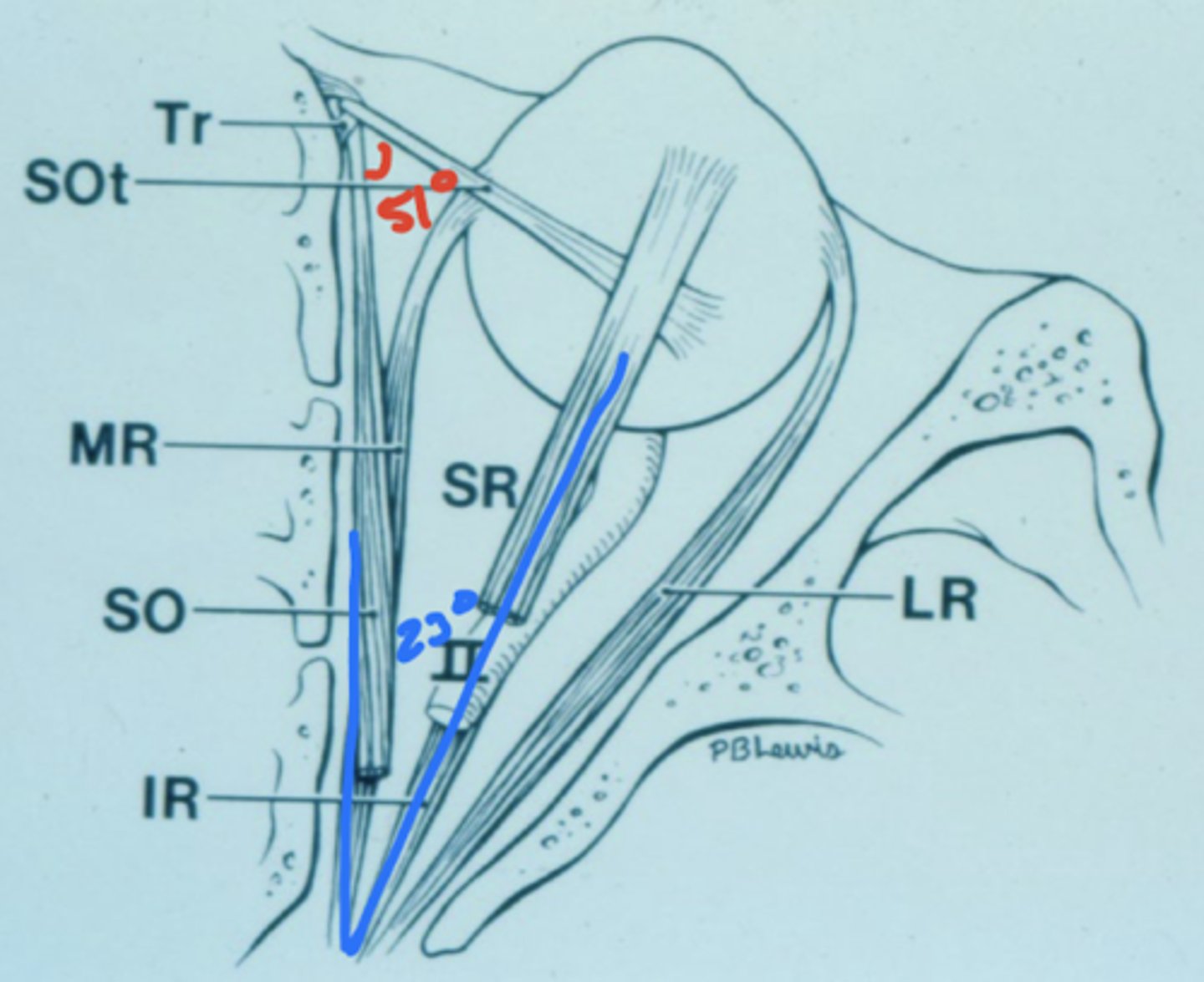
What are the actions of the superior rectus?
1. supraduction (elevation)
2. intorsion
3. adduction
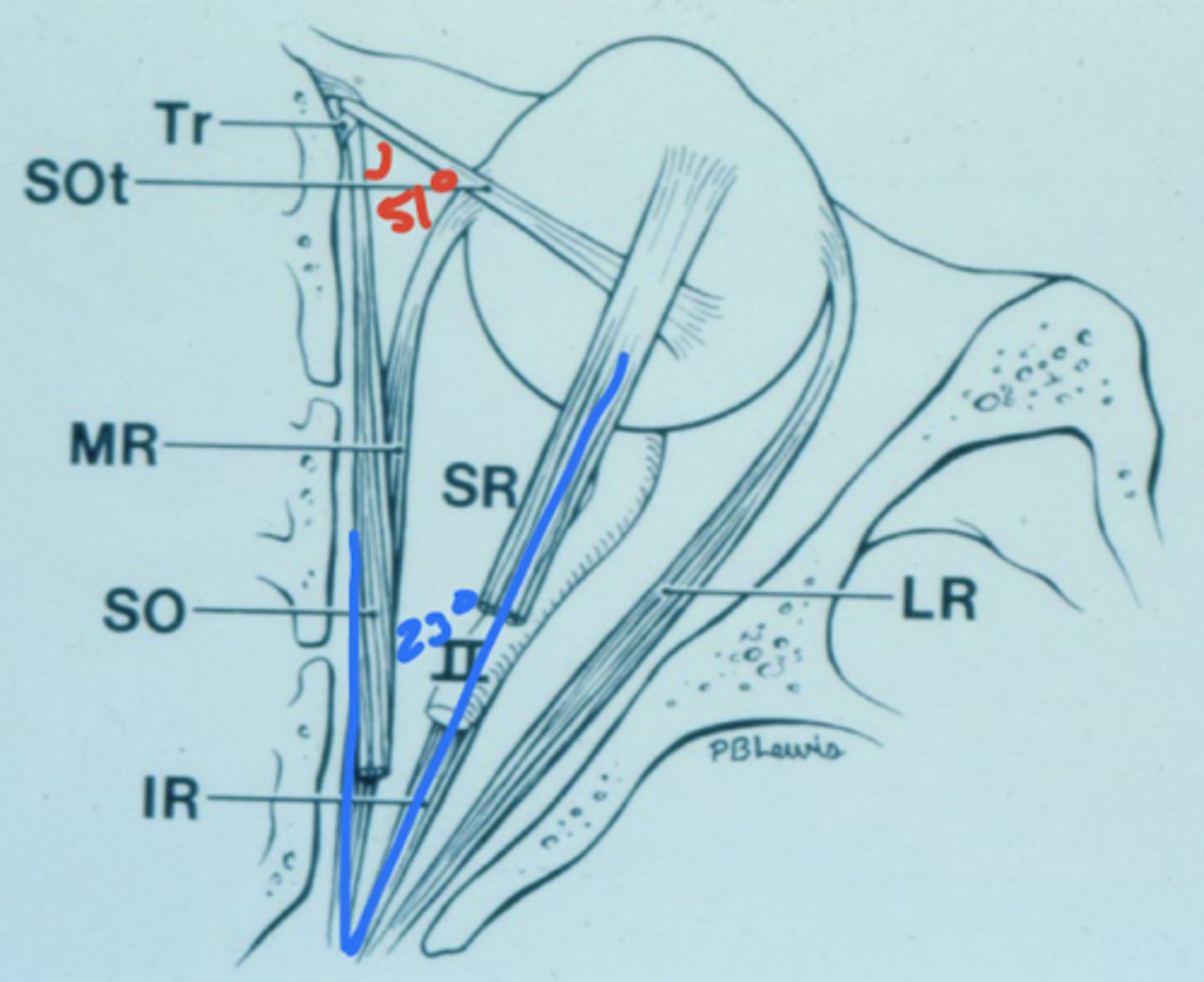
What are the actions of the inferior rectus?
1. infraduction (depression)
2. exotorsion
3. adduction
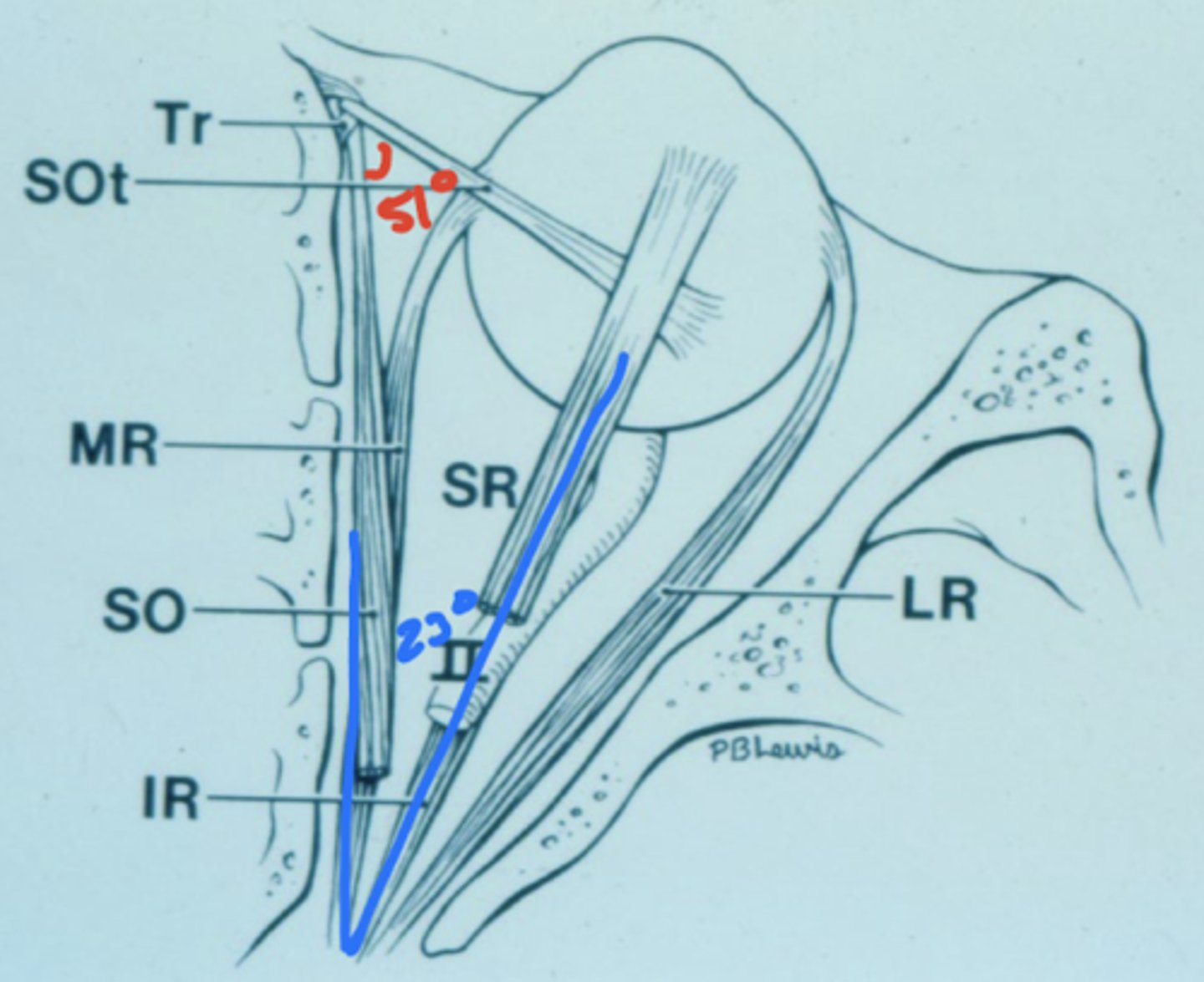
What are the actions of the superior oblique?
1. intorsion
2. infraduction
3. abduction
What are the actions of inferior oblique?
1. extorsion
2. supraduction
3. abduction
How can you isolate supraduction/infraduction of the superior/inferior rectus muscles?
23º abduct
How can you isolate intorsion/extorsion of the superior/inferior oblique muscles?
abduct the eye 39º (C)
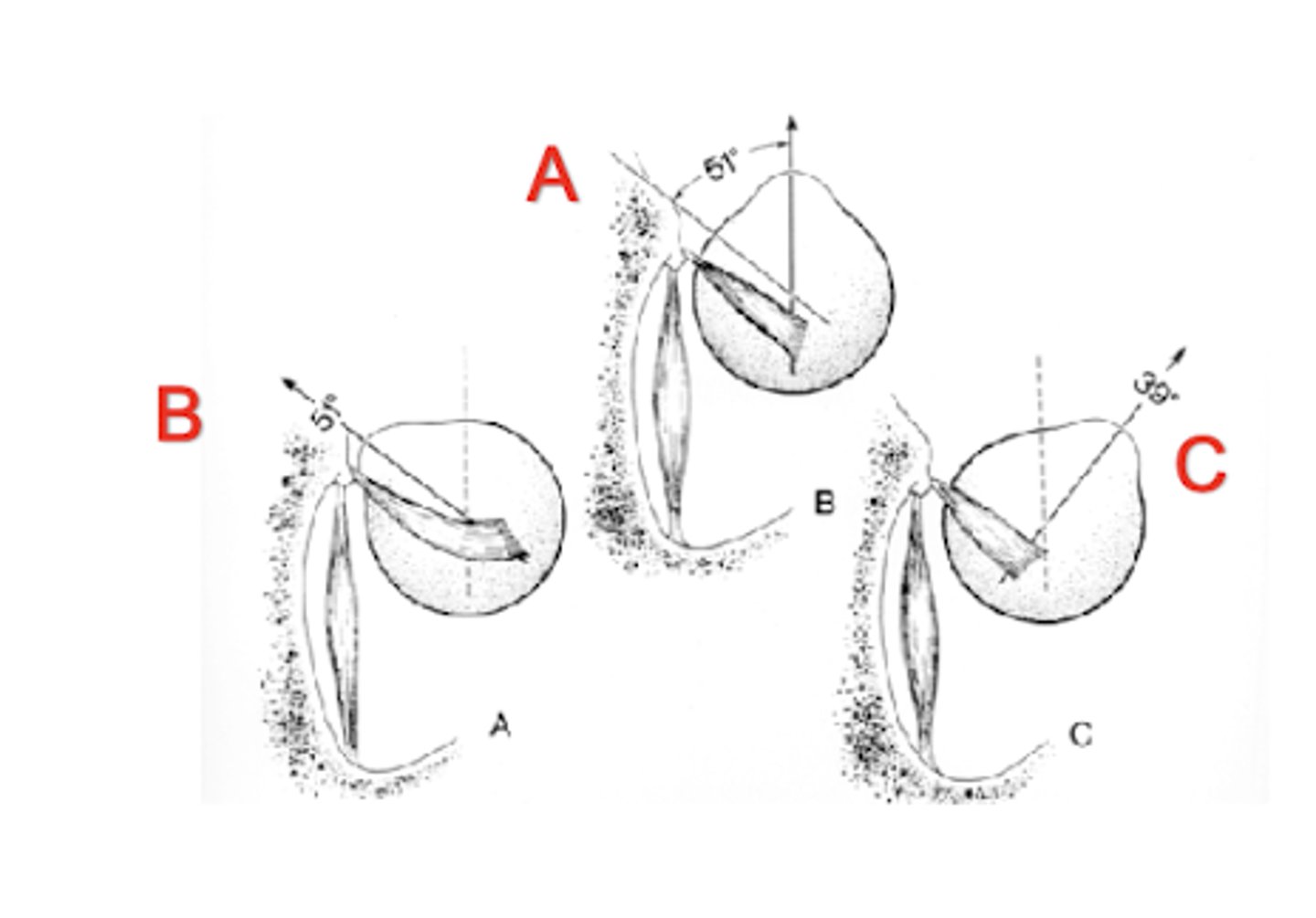
How can you isolate supraduction/infraduction of the superior/inferior oblique muscles?
adduct 51º (B)
What muscles vertical action work better/worse when you abduct?
1. recti better
2. obliques worse
What muscle vertical action work better/worse when you adduct?
1. oblique better
2. recti worse
If OD hypertropia and deviation got worse when tilting right, which eye muscle is responsible?
RSO
deviation got worse then the paretic muscle must be the intorter i.e. the RSO
Why would a patient "decide" to fixate with the paretic eye?
increased acuity or dominant eye
How does body use a paretic EOM?
sends EXTRA innervation to the RSO to pull the right eye down
How would using a paretic EOM affect the opposite eye?
sends the same amount of innervation to the opposite eye (EXTRA innervation)
for example... RSO palsy sends extra innervation to OD to use the paretic muscle, same amount of innervation to the LSO, both eyes would go down (present as a left hypo)
What is the primary vs. secondary angle of paretic EOMs?
primary -- if fixate with non-paretic eye then paretic deviation angle
secondary -- if fixate with paretic eye then paretic deviation angle + whatever extra innervation they're using
secondary > primary
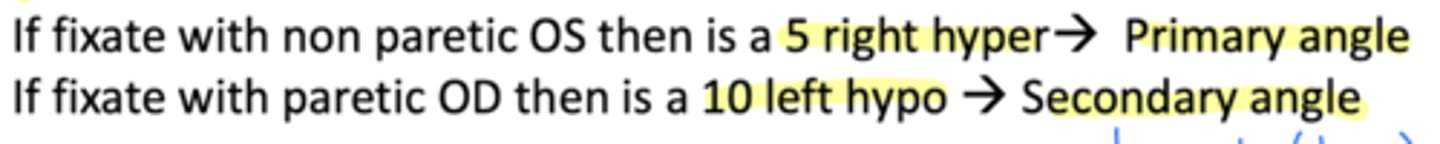
Why is the secondary always greater than the primary angle?
always have to work harder to fixate with the paretic eye
How would someone innervate the opposite eye if they wanted to fixate with their right hypertropia eye?
left hypotropia
why? (example)
1. innervate their OD with extra (10) strength (RSO or RIR)
2. innervate the same amount on the opposite side muscles (LSO or LIR)
3. extra innervation of OS causes depression
appears as either a right hypertropia or left hypotropia
What are the possible EOMs that are paralyzed during a right hypertropia?
right hyper -- RSO or RIR
left hypo -- LSR or LIO (if fixating with paretic muscles)
What are the possible EOMs that are paralyzed during a left hypertropia?
left hyper -- LSO or LIR
right hypo -- RSR or RIO (if fixating with paretic muscles)
What are the possible EOMs that are paralyzed during a right hypotropia?
right hypo -- RSR or RIO
left hyper -- LSO or LIR (if fixating with paretic muscles)
What are the possible EOMs that are paralyzed during a left hypotropia?
left hypo -- LSR or LIO
right hyper -- RSO or RIR (if fixating with paretic muscles)
Right hypertropia worsens when looks right, which muscles are suspected?
OD hypertropia -- RSO or RIR
isolate RIR by abducting
OS hypotropia (if fixating with paretic eye) -- LSR or LIO
isolate LIO by adducting
Left hypotropia worsens when looks right, which muscles are suspected?
OS hypotropia -- LSR or LIO
adducting isolates LIO
OD hypertropia (if fixating with paretic eye) -- RSO or RIR
abducting isolates RIR
If you've narrowed it down to two muscles (in different eyes), what would you tell the patient to do next?
tilt head to isolate the action of the oblique muscles
What are Park's three steps?
1. Is there a vertical? (narrows down to 4 muscles)
2. Is the vertical worse in right or left gaze? (narrows down to two muscles, whichever is isolated)
3. Is the vertical worse with right or left head tilt?