Urinary System | Chapter 24 | BIOL117
1/205
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
206 Terms
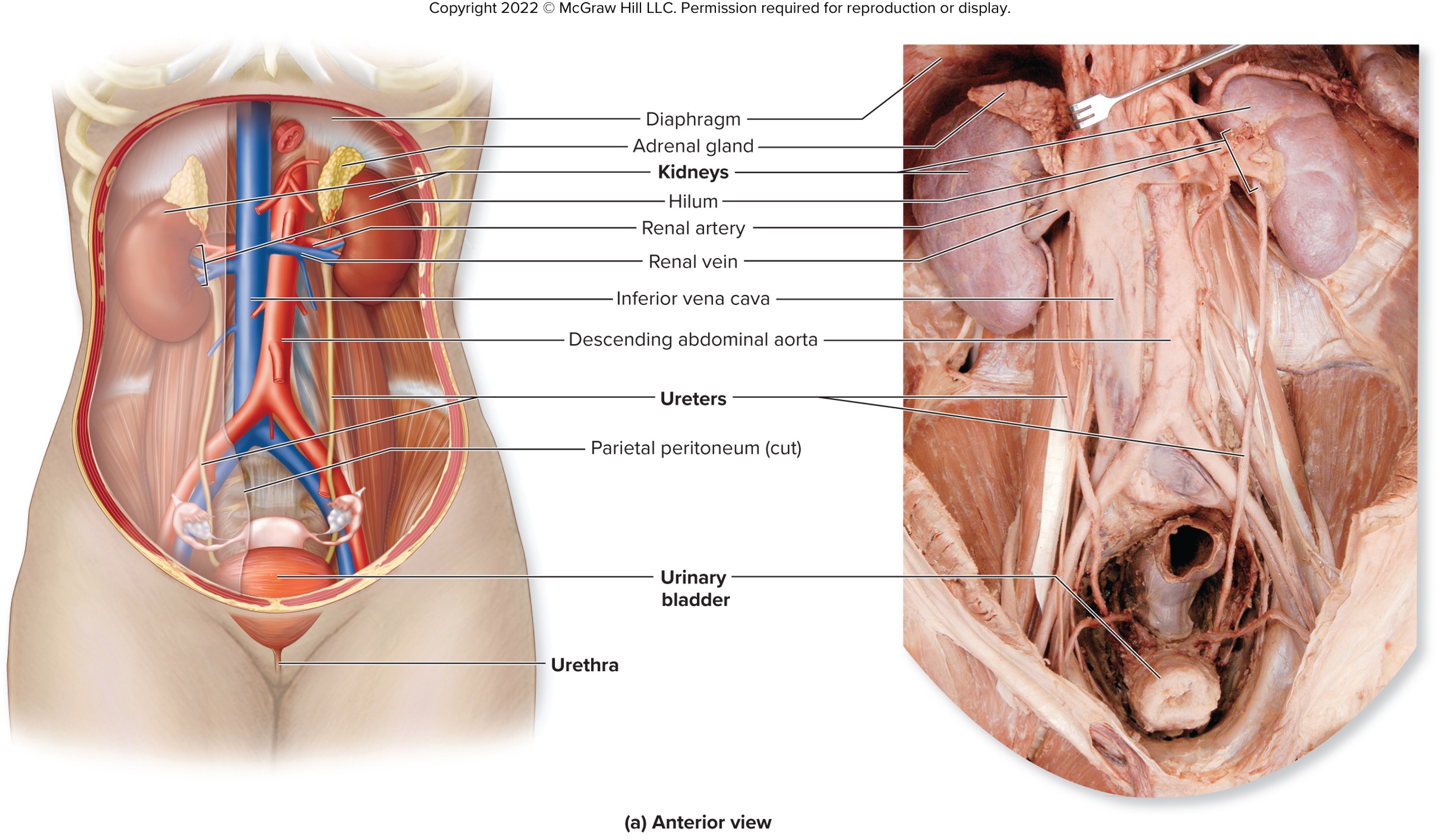
what are the different organs that make up of the urinary system and their PRIMARy functions?
kidneys - filter blood
ureters - transport urine
bladder - holds urine
urethra - eliminates urine
what are the functions of the urinary system?
elimination of metabolic wastes
regulation of ions level (e.g., Na+, K+ and Ca2+)
regulation of acd-base balance (e.g., H+ and HCO3-)
regulation of blood pressure
regulation of water levels
elimination of biologically active molecules (e.g., hormones, drugs)
formation of calcitriol (vitamin D metabolism)
production and release of erythropoietin
potential engagement in gluconeogenesis
____________ are two symmetrical bean-shaped organs with a concave medial border, ileum, and a lateral convex border
kidneys
__________ rests on the superior aspect of the kidney
adrenal glands
where is the kidneys located?
the left and right upper quadrant
on posterior abdominal wall
lateral to the vertebral column
why is the right kidney lower than the left kidney?
to accommodate the position of the liver
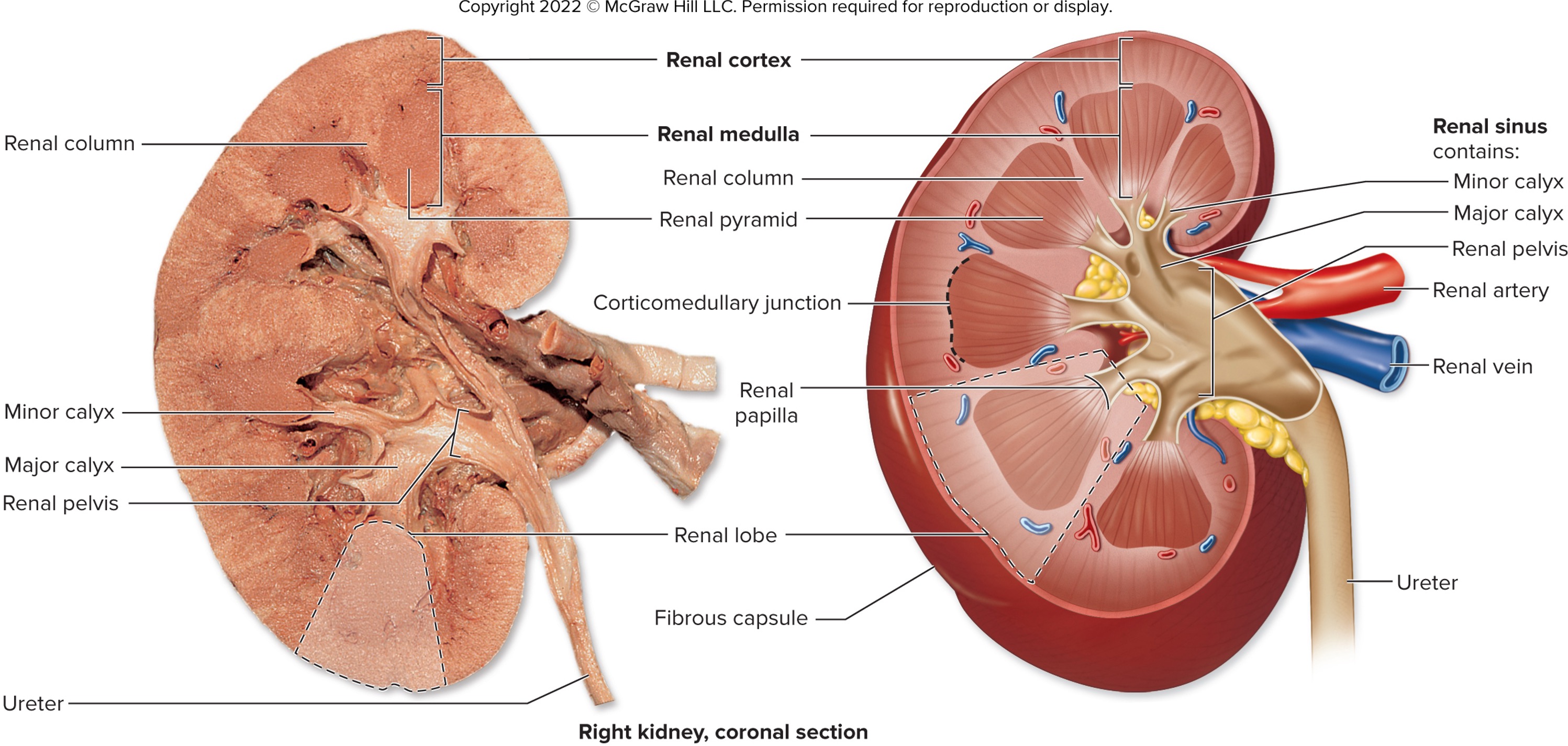
what are the different layers of the kidneys? (inner most to outermost)
fibrous capsule (dense irregular CT that helps maintains kidney’s shape
perinephric fat (dense irregular connective CT to help anchor the kidney to surrounding structure)
→ help cushion and support the kidneys)
renal fascia - external to perinephric fat made up of dense irregular CT to anchor the kidney to surrounding structures
paranephric fat (adipose CT that help cushion and support the kidneys)
what are the two region of functional tisue in the kidneys?
renal cortex
renal medulla
renal columns
extension of the cortex projecting into the medulla
renal pyramids
portion of the medulla divided by renal columns with wide base ar the external edge of the medulla and the medial aspect ar the renal papilla
corticomedullary junction
located at the medial apex where the renal papilla is
renal sinus
medially located urine drainage area
organized into minor calyces, major calyces, and the renal pelvis
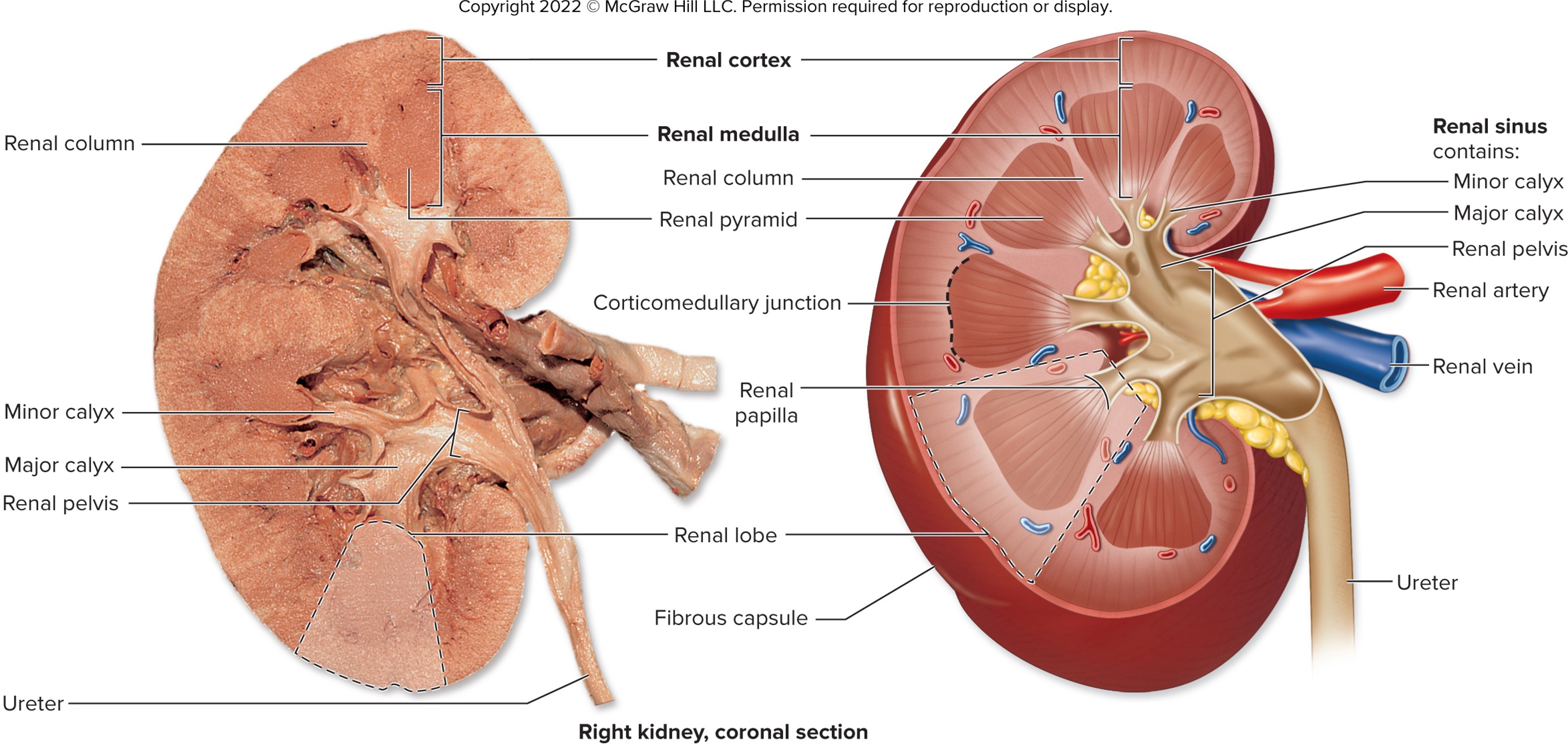
minor calyces
unflle-shaped structures of renal pyramids
merge to form major calyz
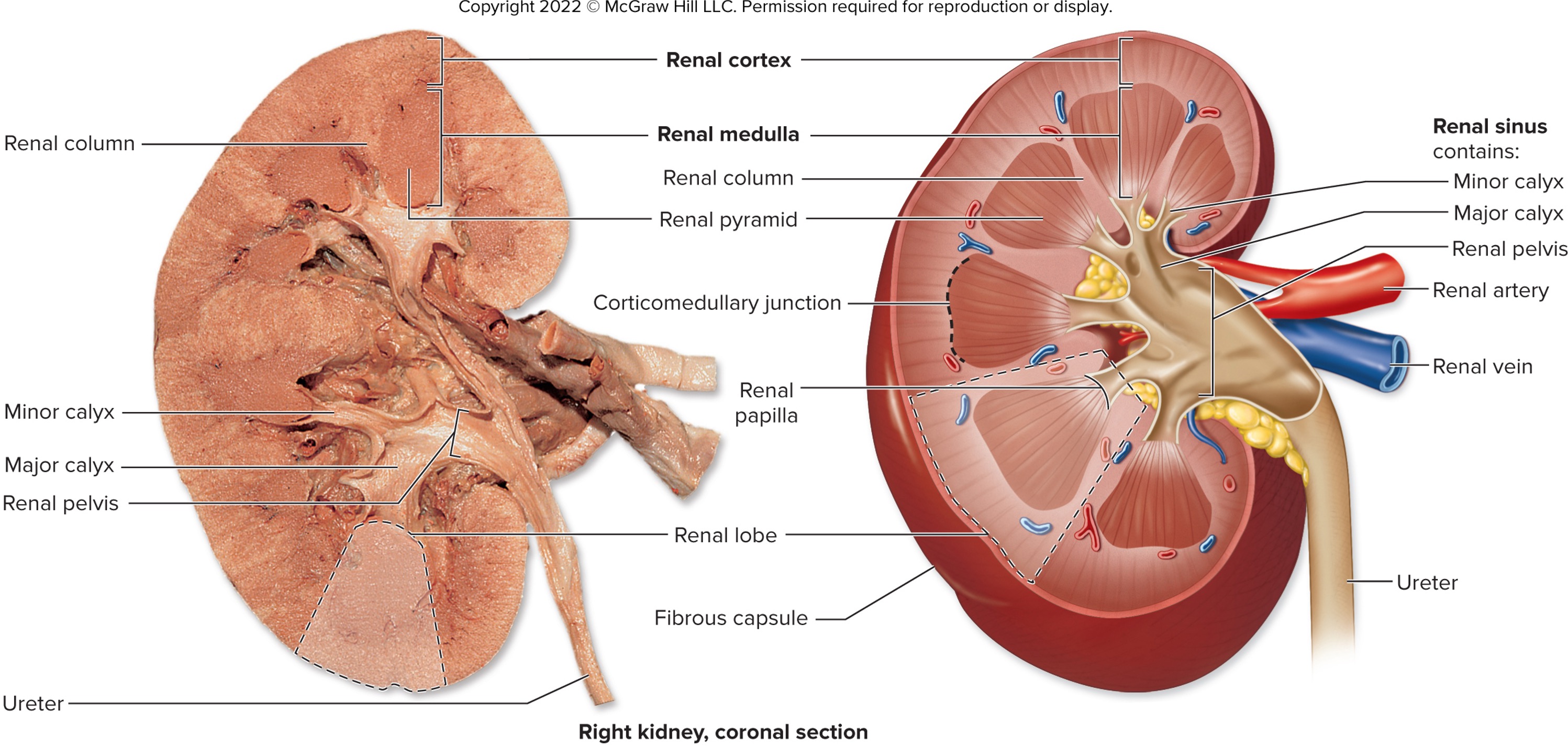
renal pelvis
formed from merged major calyces
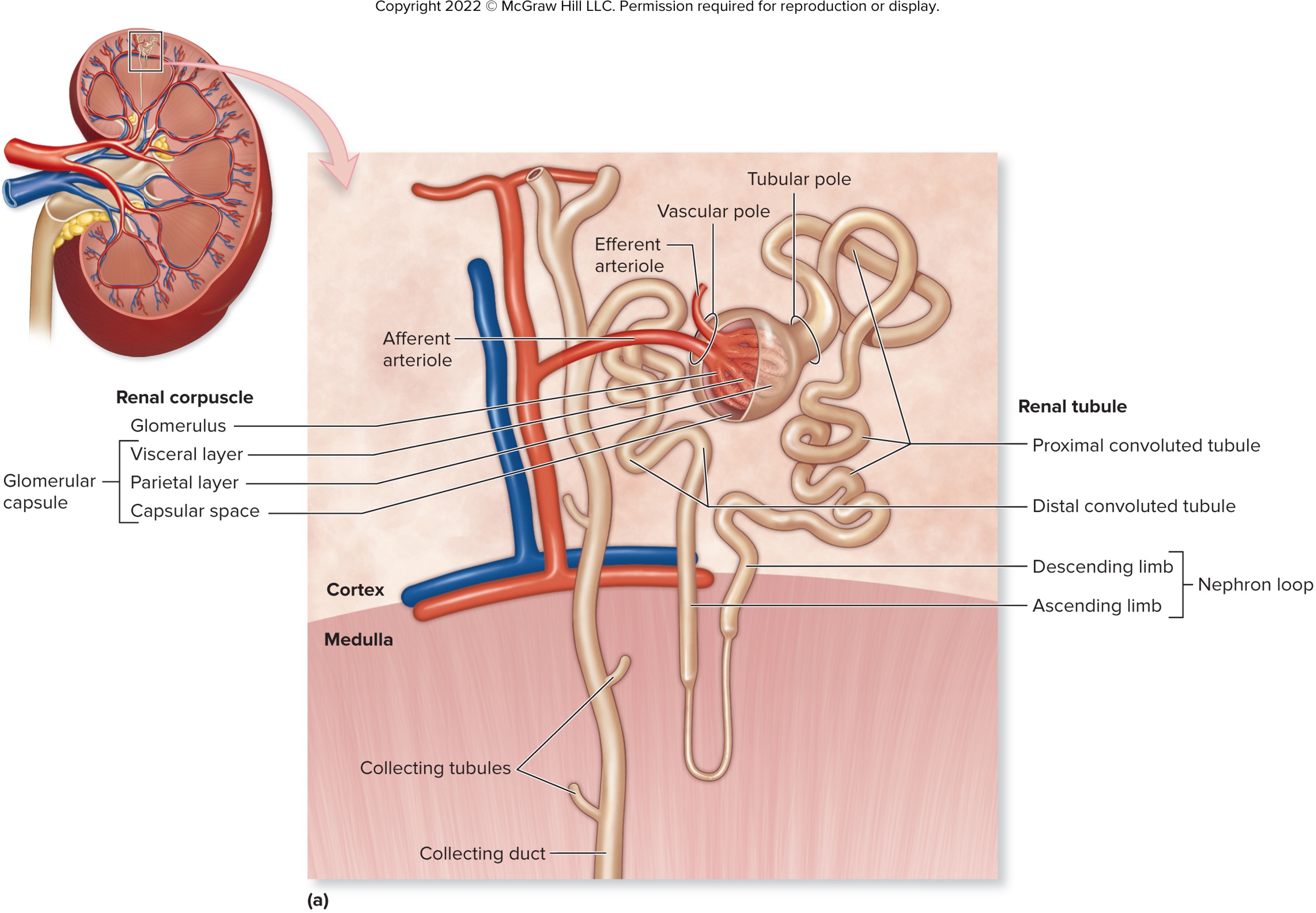
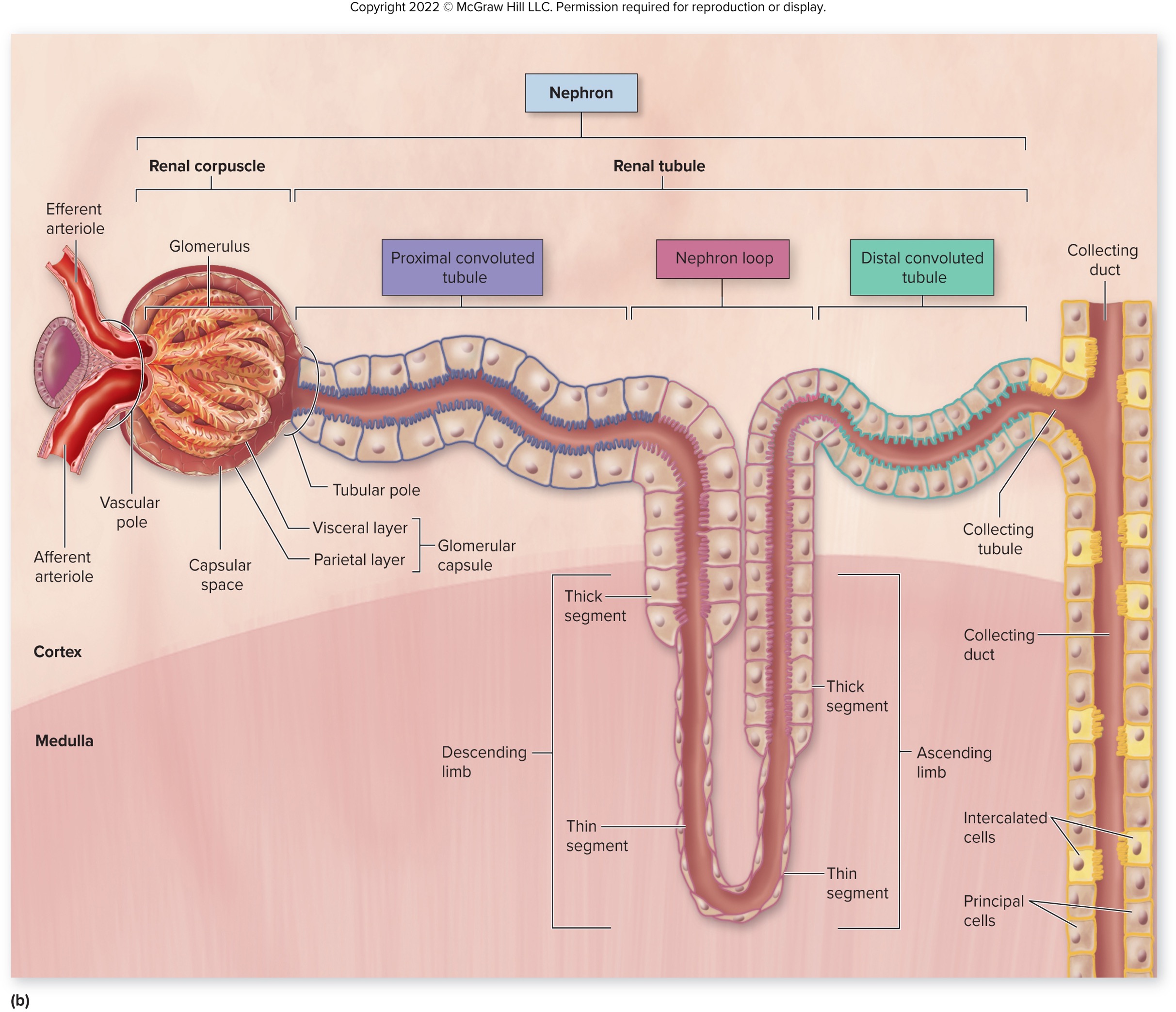
nephron
microscopic functional filtration unit of the kidney that consist of the renal corpuscle and renal tubules
renal corpuscle
enlarged bulbous region of nephron within the renal cortex that composed of two structures of glomerulus and Bowman’s (glomerular) capsule
glomerulus
tangle of capillary loops (glomerular capillaries) that allow blood to enter via the afferent arteriole and leaves via the efferent arteriole
in the bowman’s capsule, blood enters via the _________ arteriole and exits via the _________ arteriole
afferent; efferent
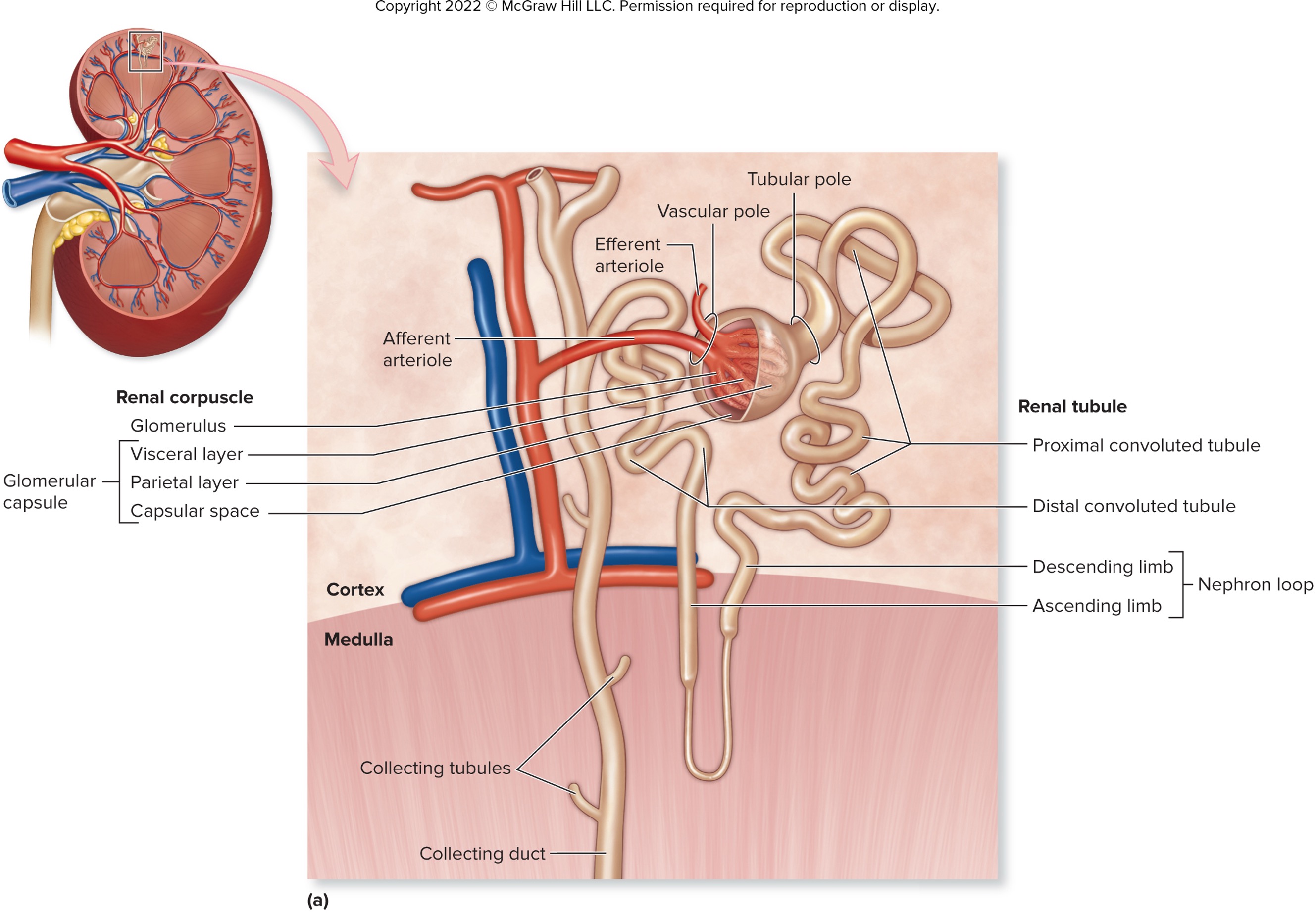
what are the three layers of the Bowman’s capsule?
visceral
→ directly overlies glomerular capillaries
parietal
→ simple squamous epithelium
capsular space
→ receive filtrate and modified to form urine
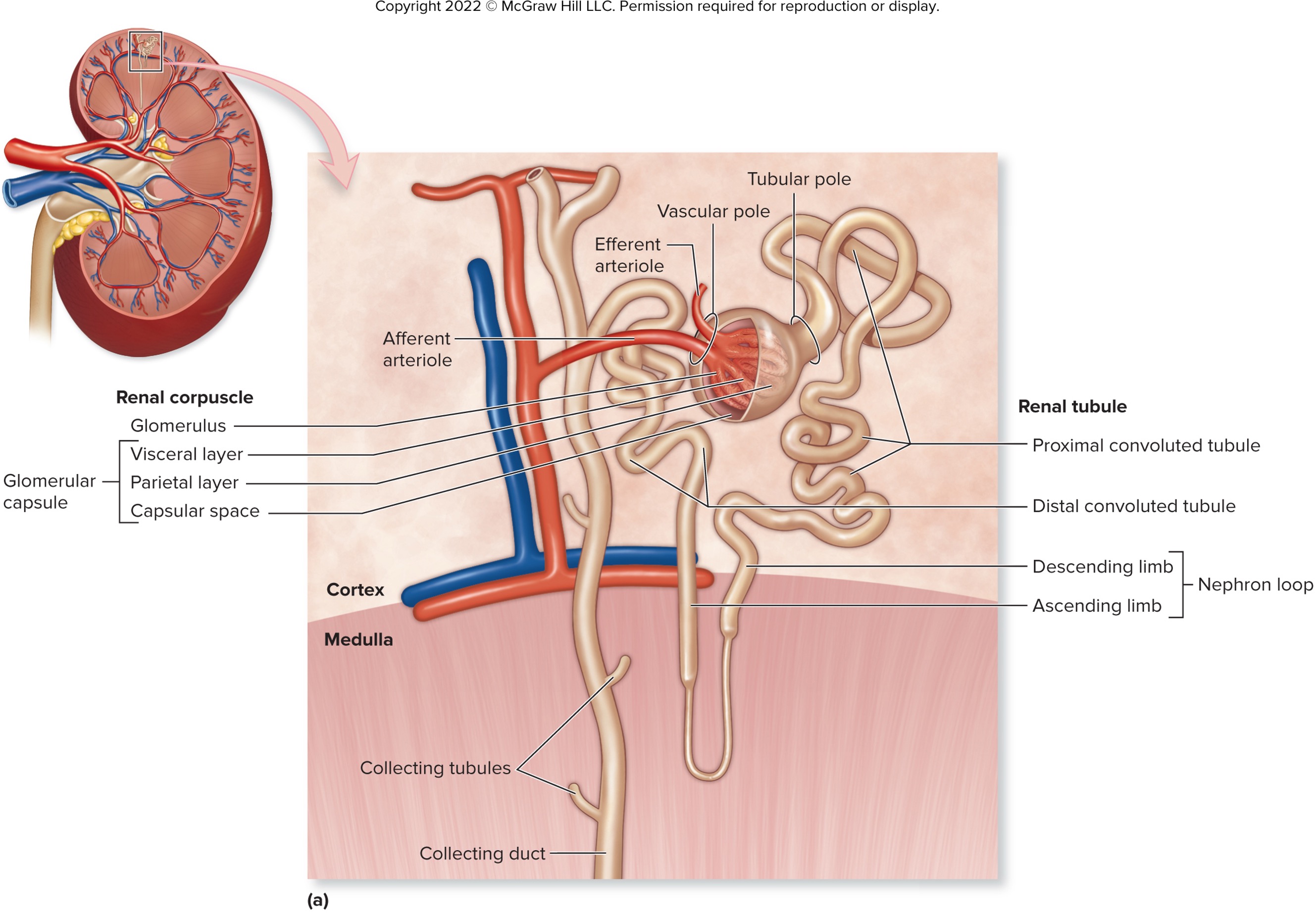
vascular pole
afferent and efferent arterioles attach to glomerulus
tubular pole
origin of renal tubule
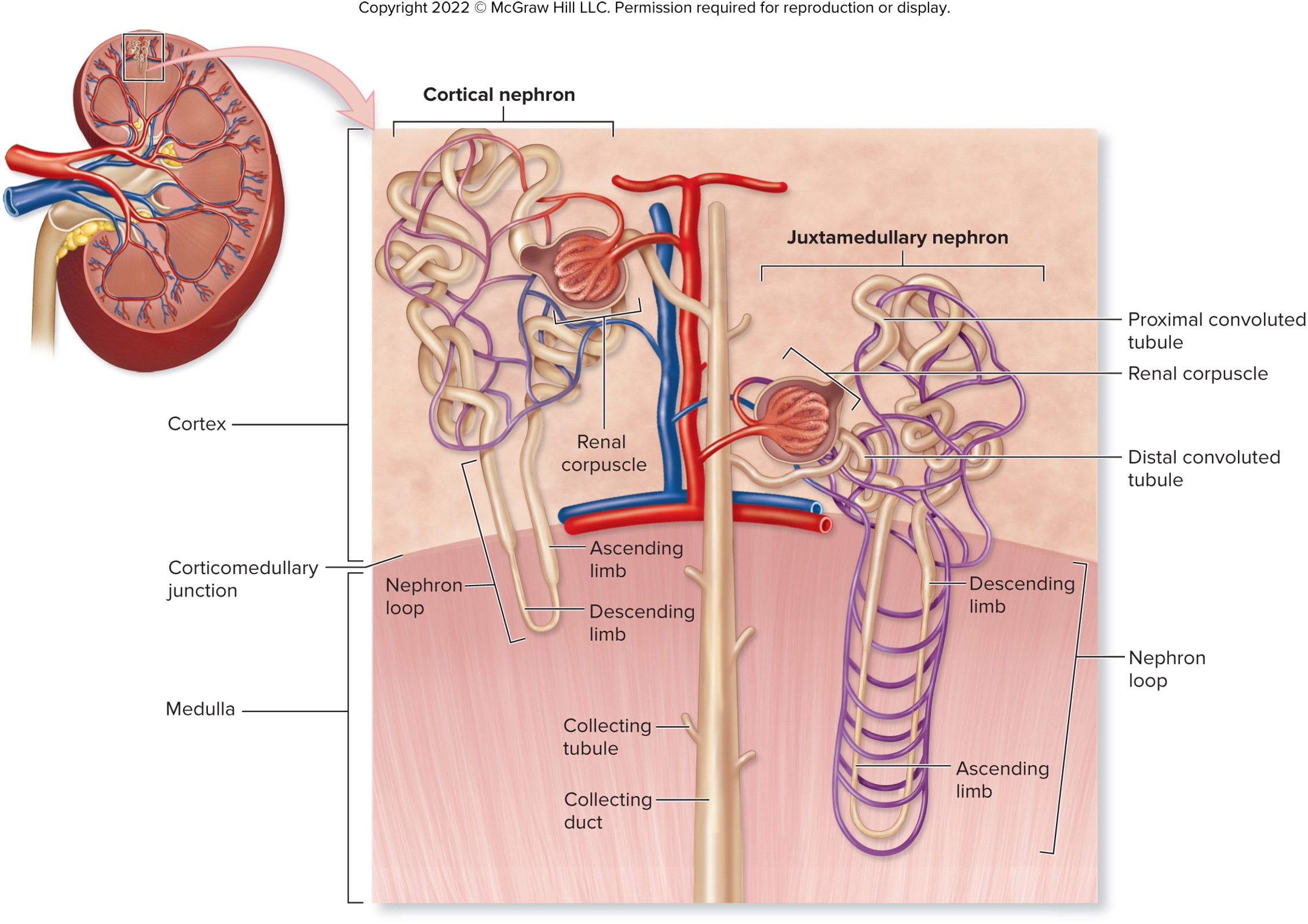
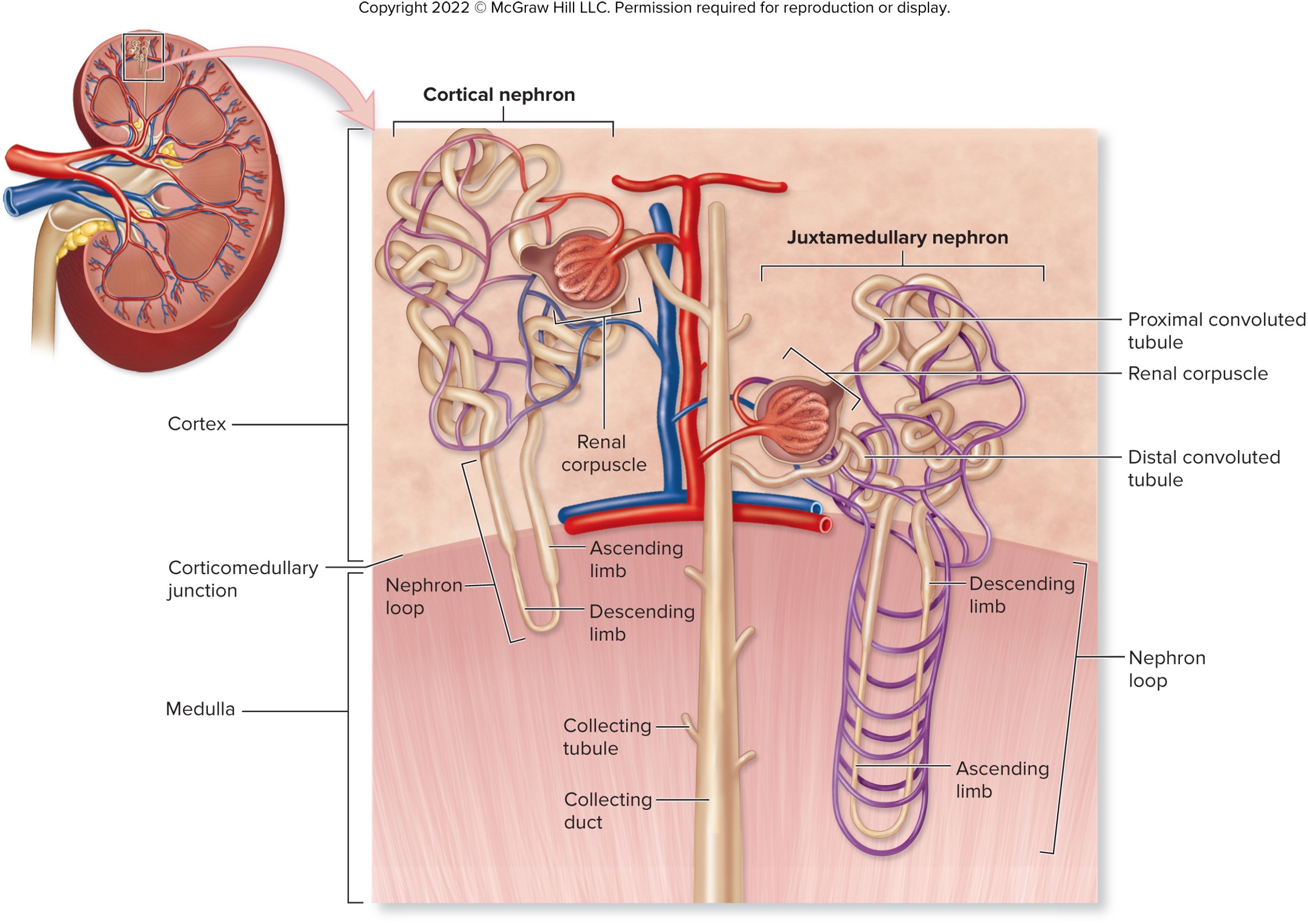
what are the three sections of the renal tubules? (in order)
proximal convoluted tubules (PCT)
nephron loop
distal convoluted tubule (DCT)
proximal convoluted tubule (PCT)
first region of the renal tubule
originates at tubular pole of renal corpuscle
made up of cuboidal epithelium
lined with microvilli to increase surface area for more efficient reabsorption capacity
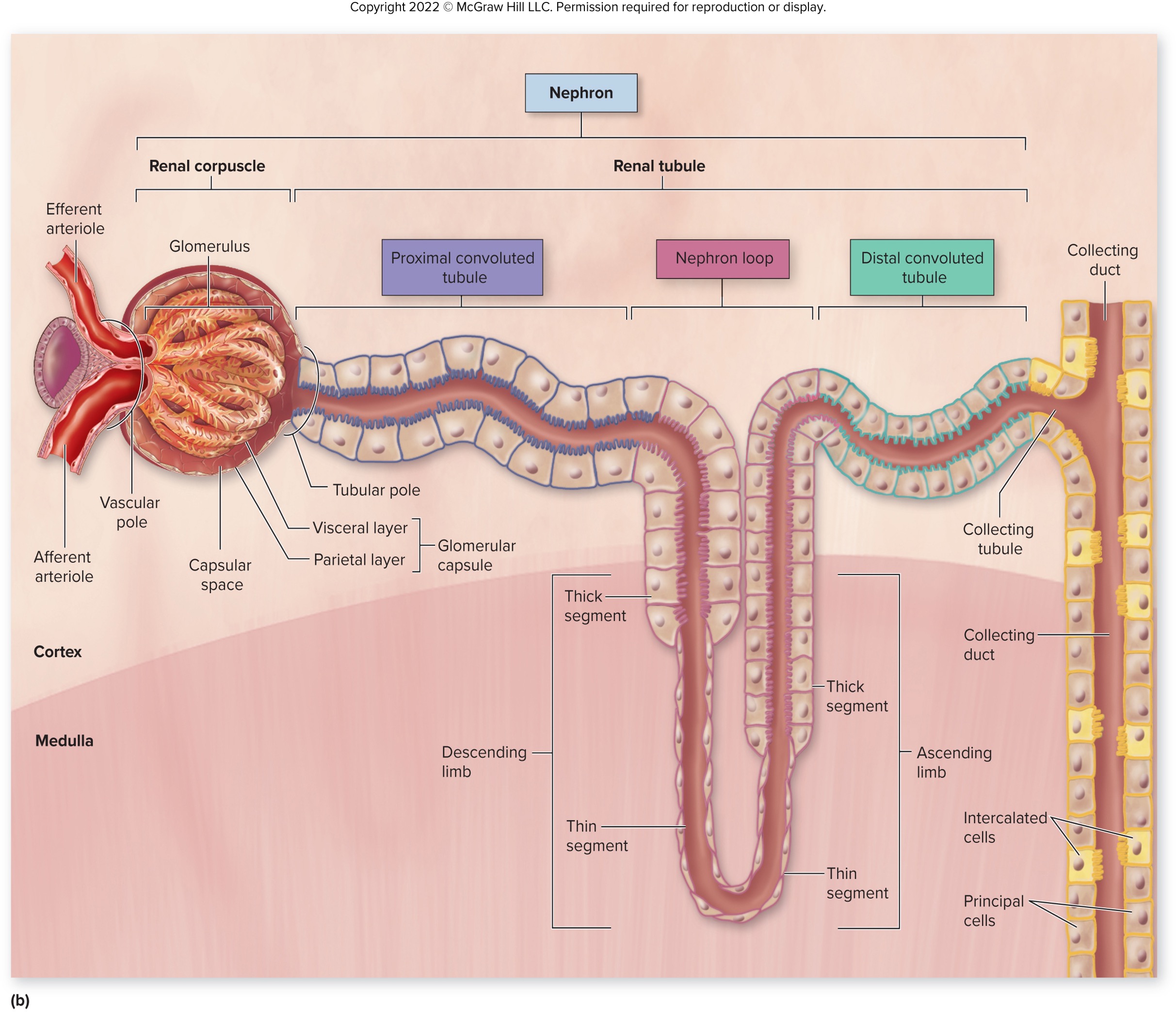
nephron loop (AKA hairpin turn)
originates at sharp bend in PCT
made up of te descending limb and the ascending limp
→ descending - extends medially from the PCT
→ ascending - return to the renal cortex and ends at DCT
thin segment lined with simple squamous epithelium
thick segment lined with simple cuboidal epithelium
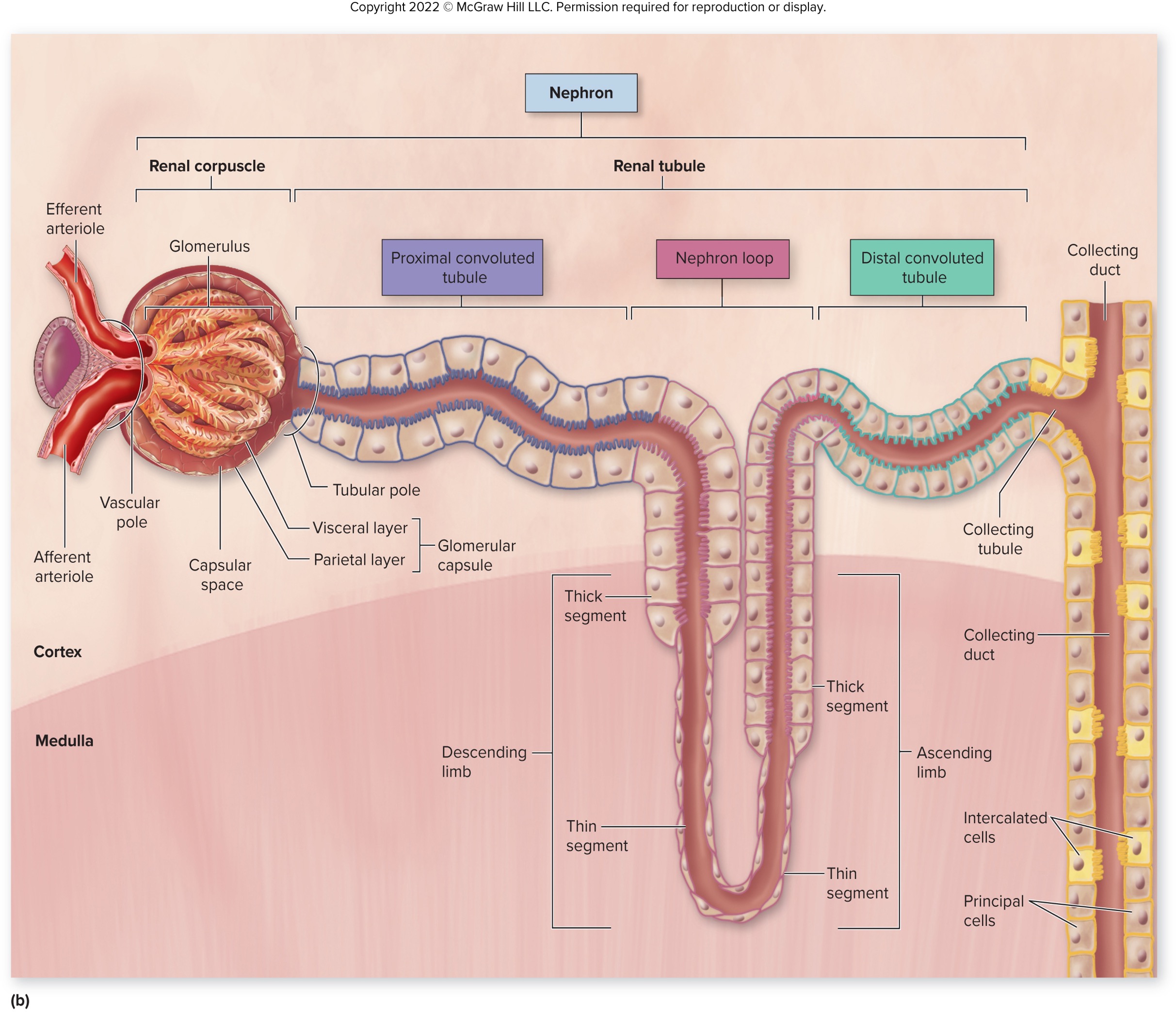
Distal Convoluted Tubule (DCT)
originates in the renal cortex at the end of the ascending limb
extends to collecting tubule
lined by simple cuboidal epithelium without microvilli
appears clear when viewed under a microscope
what are the two types of nephron?
cortical
juxtamedullary
classified based on two factors: relative position of renal corpuscles in the cortex and the length of the nephron loop
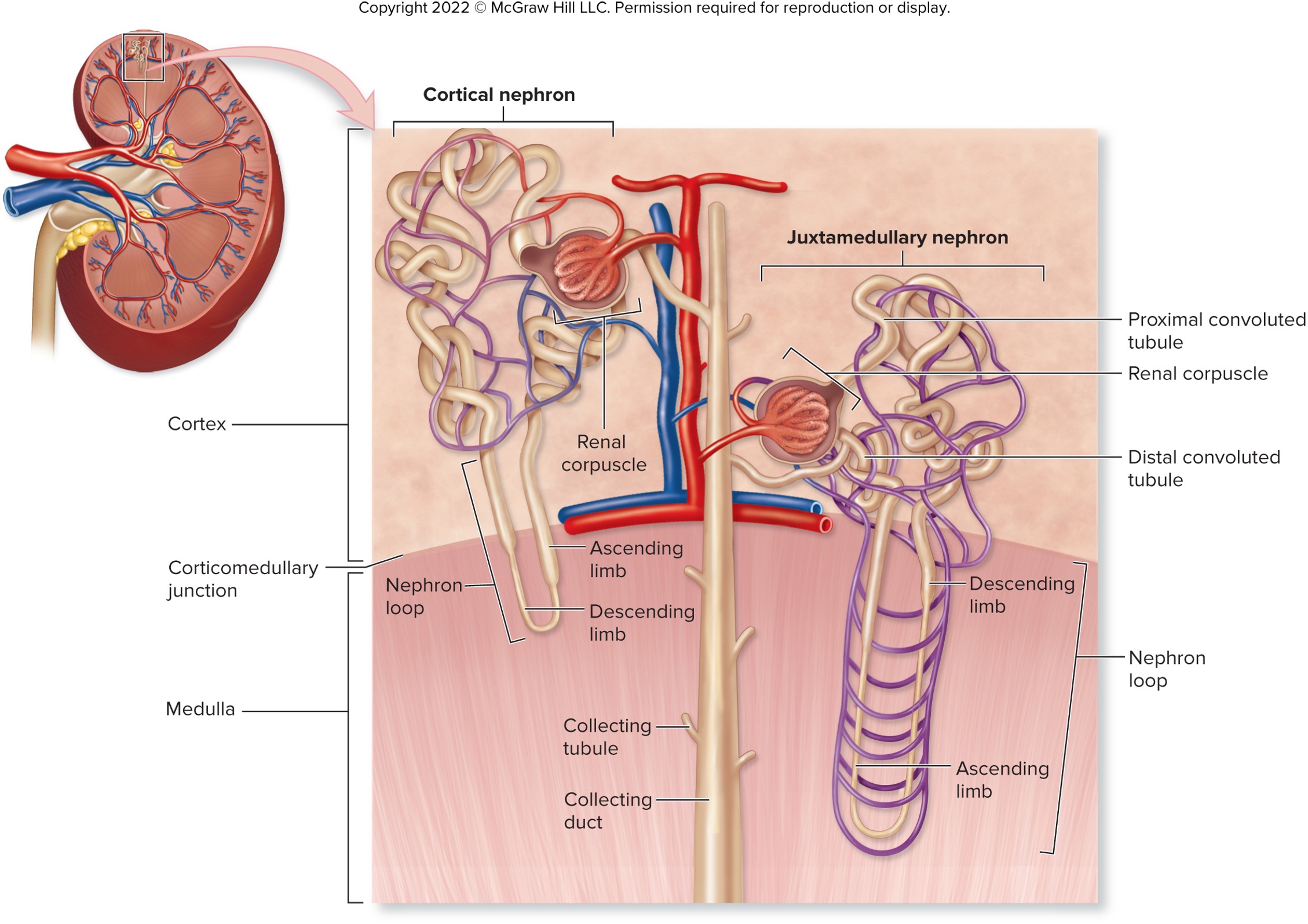
cortical nephrons
oriented with renal corpuscles near peripheral cortex
short nephron loop barely penetrate the medulla
made up of 85% of nephrons
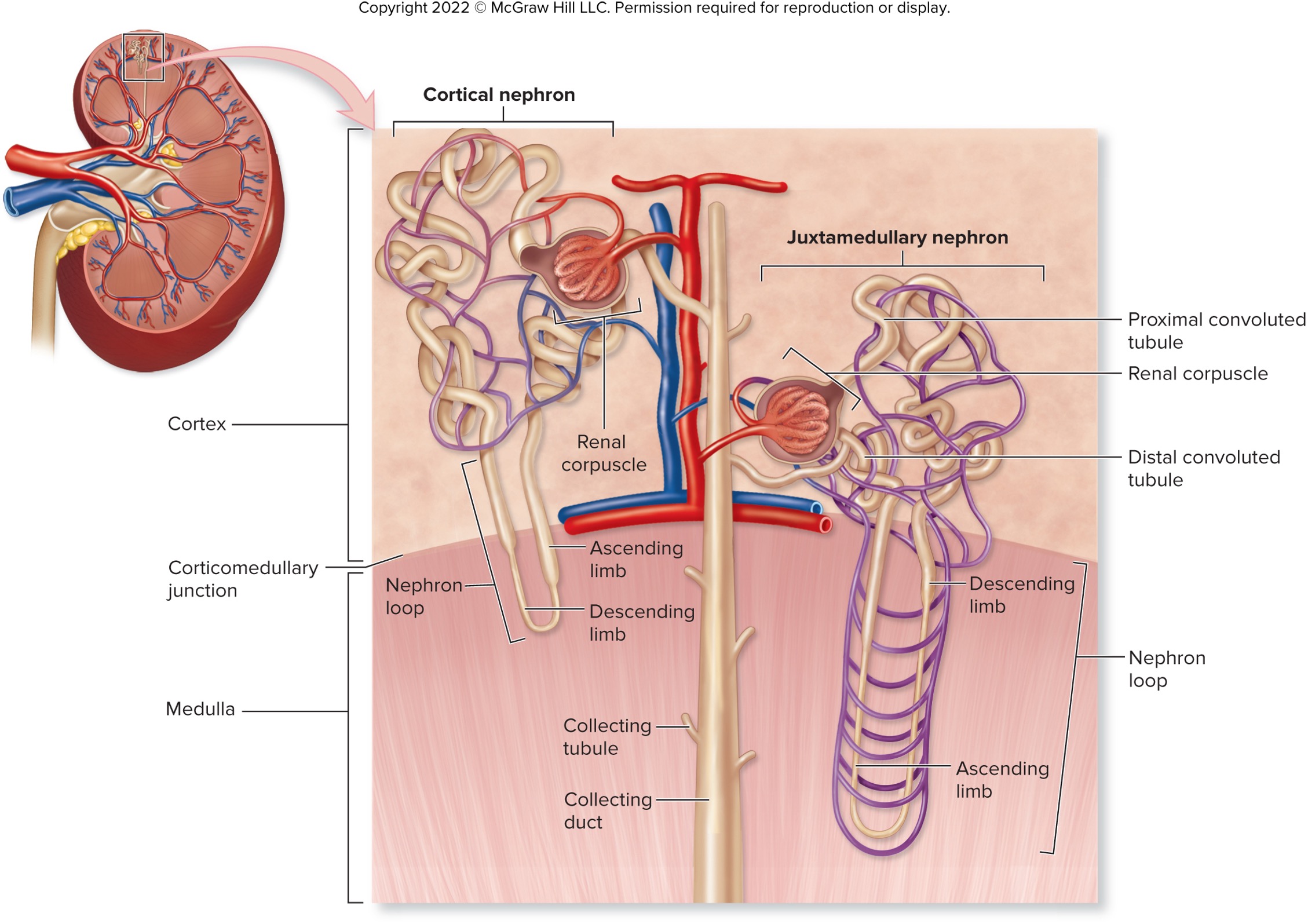
juxtamedullary nephrons
oriented at the renal corpuscles adjacent to the corticomedullary junctions
long nephron loops extend deep into the medulla
help establish salt concentration gradent in the interstitial space and allow foe regulation of urine concentration by ADH
made up of about 25% of nephrons
__________ nephrons help establish salt concentration gradient in interstitial space by allow for regulation of urine concentration by ADH
juxtamedullary
what are the specialized cells making up the collecting tubules and the collecting ducts and their PRIMARY functions?
principal cells - responsive to hormones aldosterone and antidiuretic hormone (ADH)
intercalated cells (A & B)
→ help regulate urine pH and blood pH
multiple collecting tubules empty into larger ______________
collecting ducts
numerous collecting ducts empty into ____________ located within the renal papilla
papillary duct
juxtaglomerular (JG) apparatus
regions made up of the granular cells, macula dense, and extraglomerular mesangial cells at the glomerular hilum
helps regulate filtrate formation and systemic blood pressure
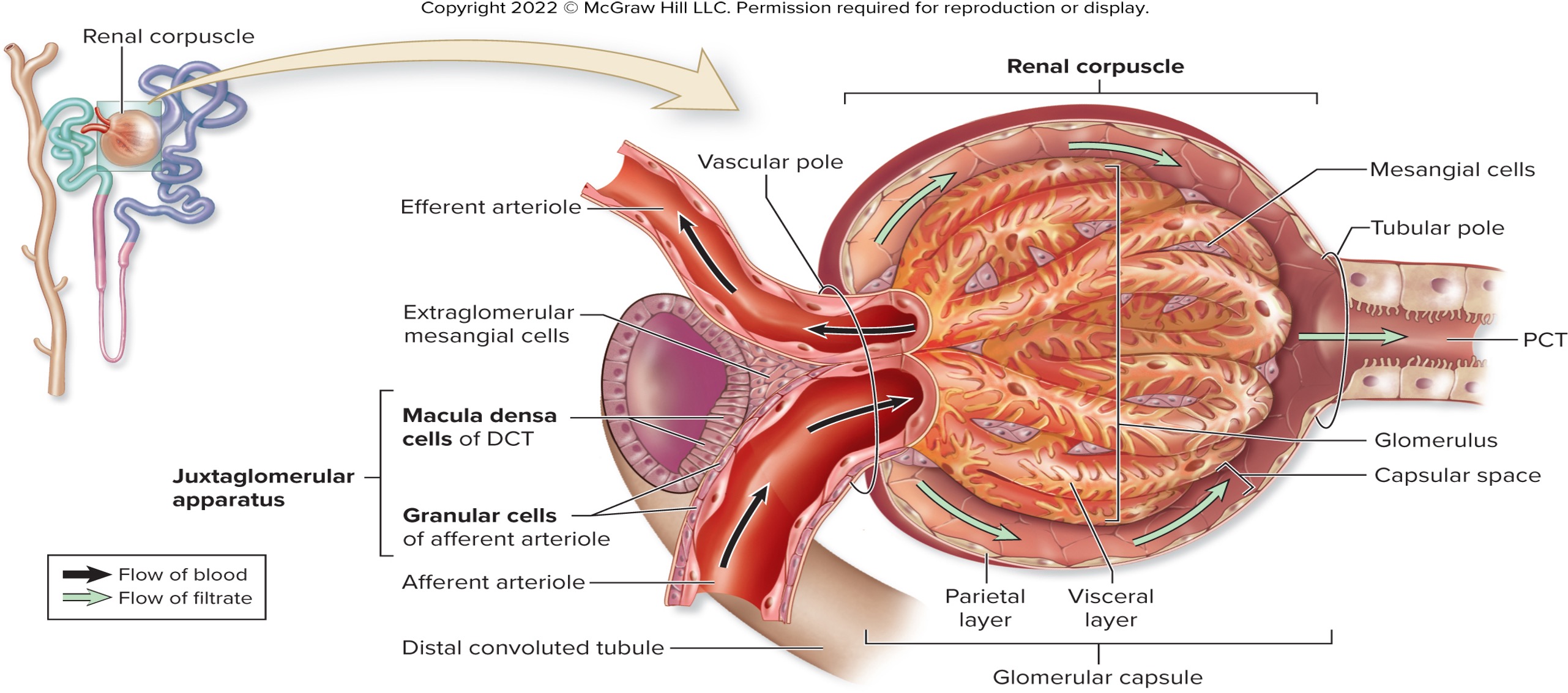
granular cells (compositions, location, and functions)
made up of the juxtaglomerular (JG) apparatus
modified smooth muscles cells of afferent arteriole
located near entrance to renal corpuscle
contract when simulated by stretch or sympathetic stimulation
synthesize, store, and release renin
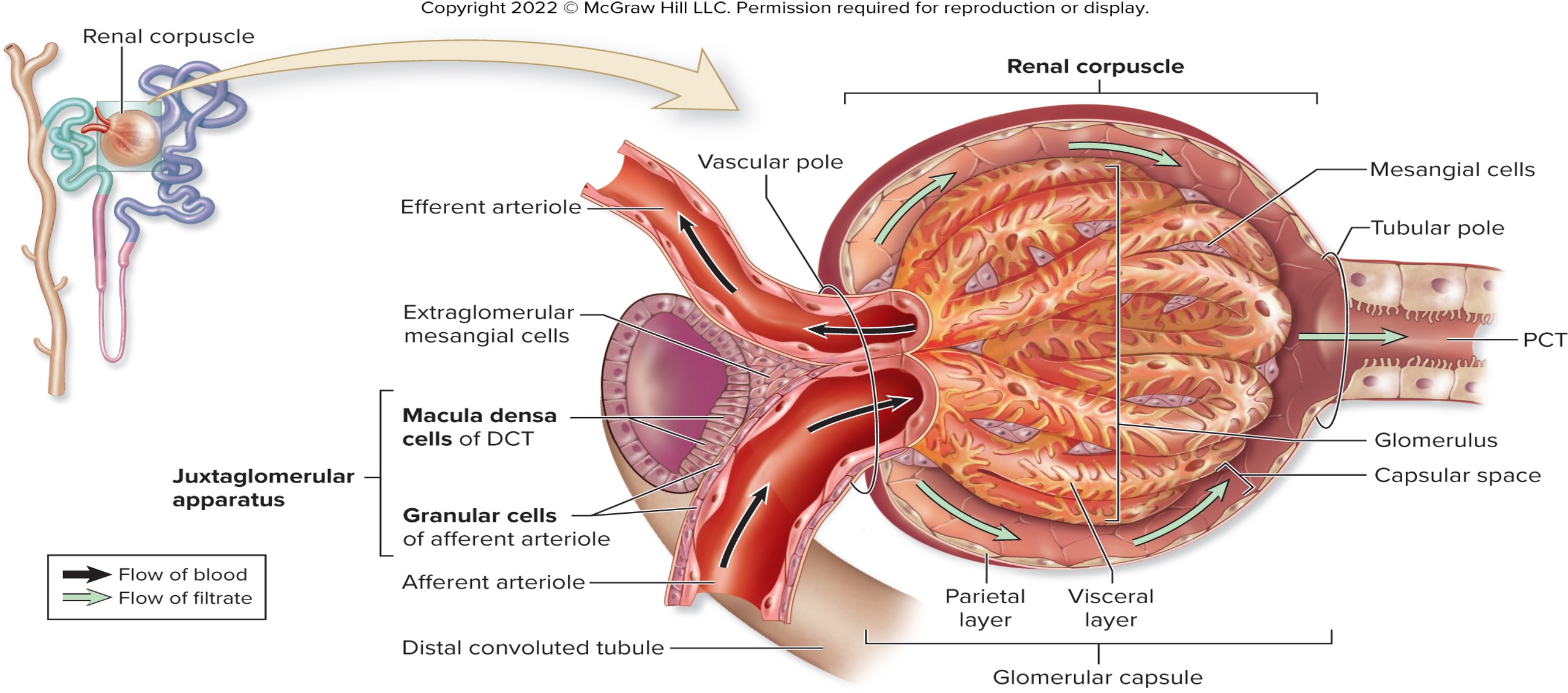
macula densa (compositions, location, and functions)
made up of the juxtaglomerular (JG) apparatus
modified epithelial cells in the wall of DCT
detect changes in NaCl concentration of fluid in the lumen of DCT
signal granular cells to release renin through paracrine simulation
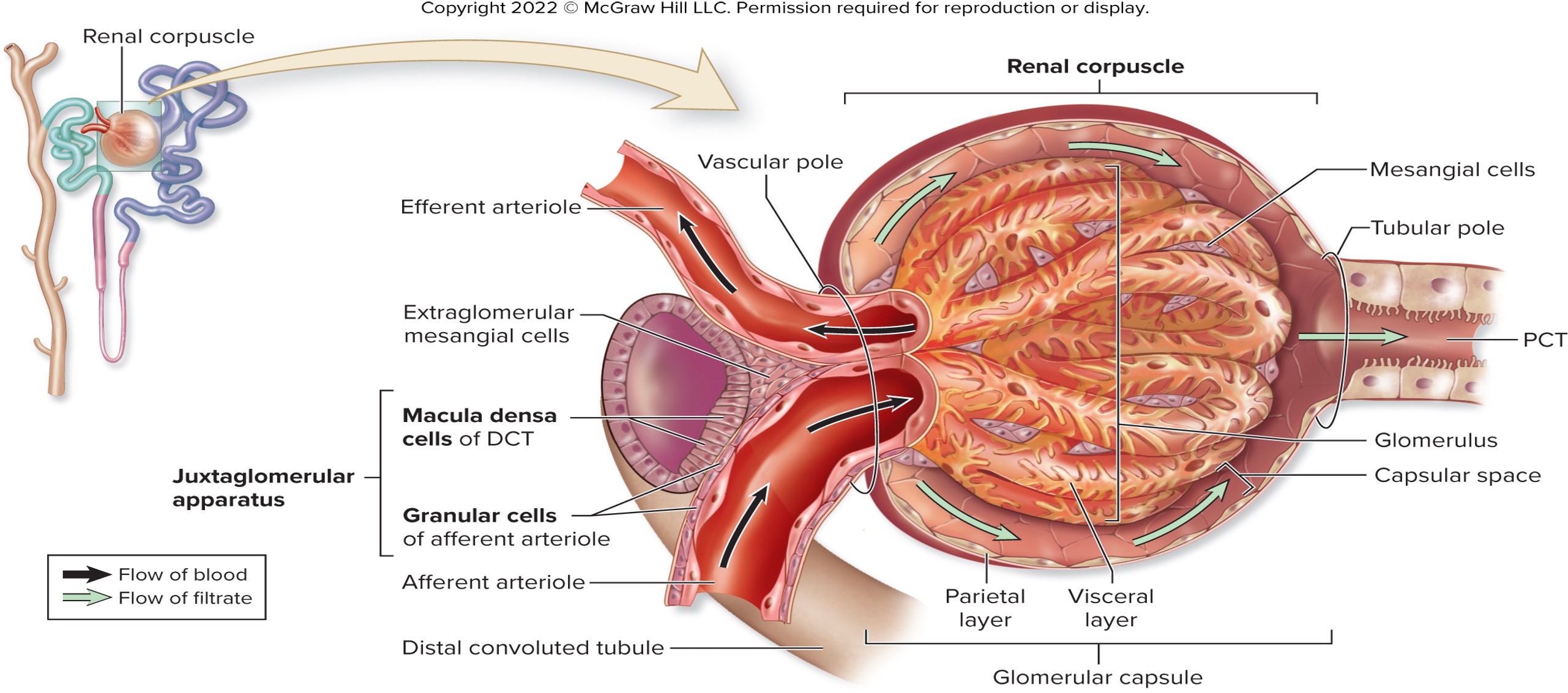
exraglomerular mesangial cells
smooth muscle cells between arterioles
helps with vasoconstriction to regulate flow
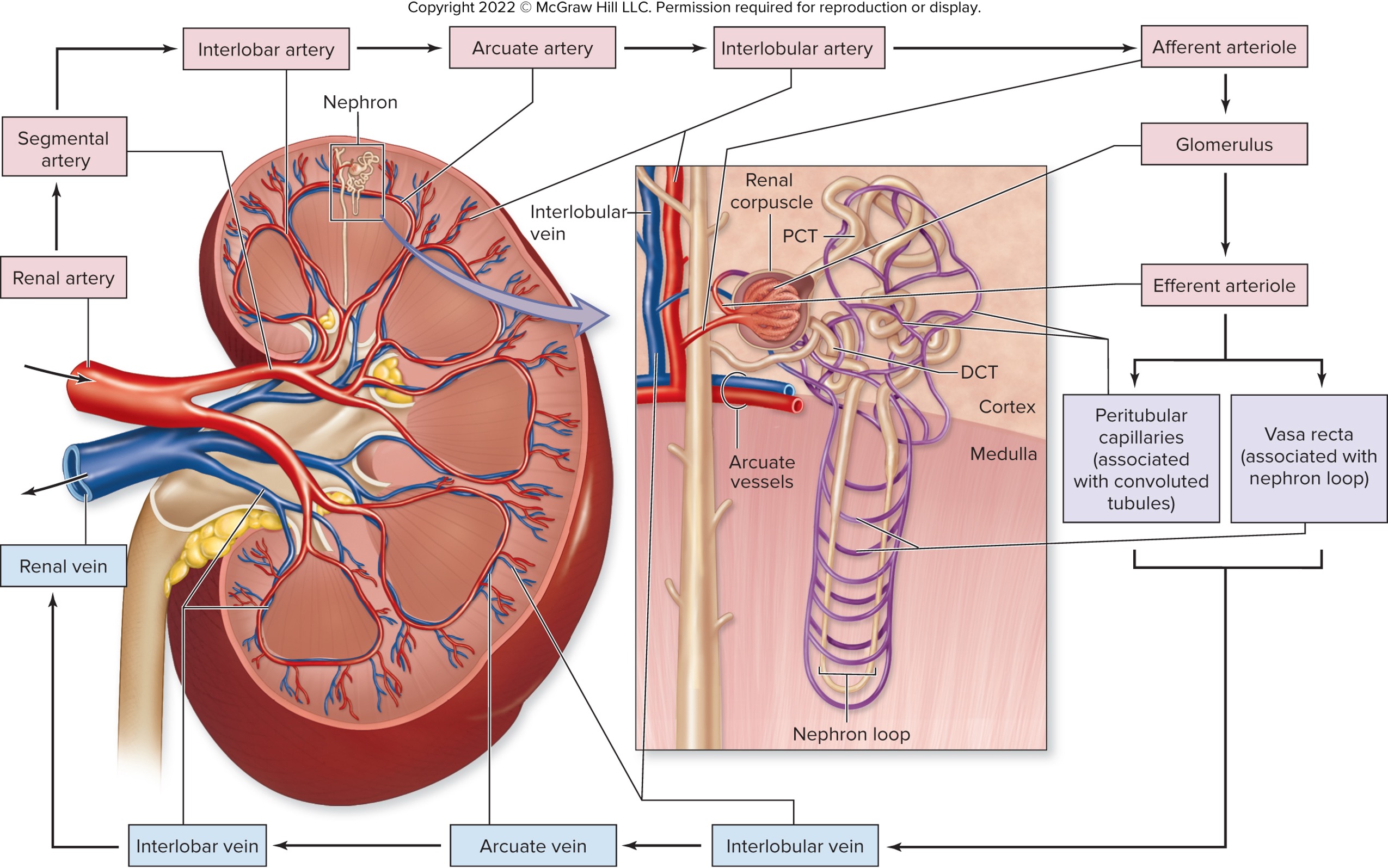
blood are delivered to each kidney by __________
renal arteries arisen from the abdominal aorta
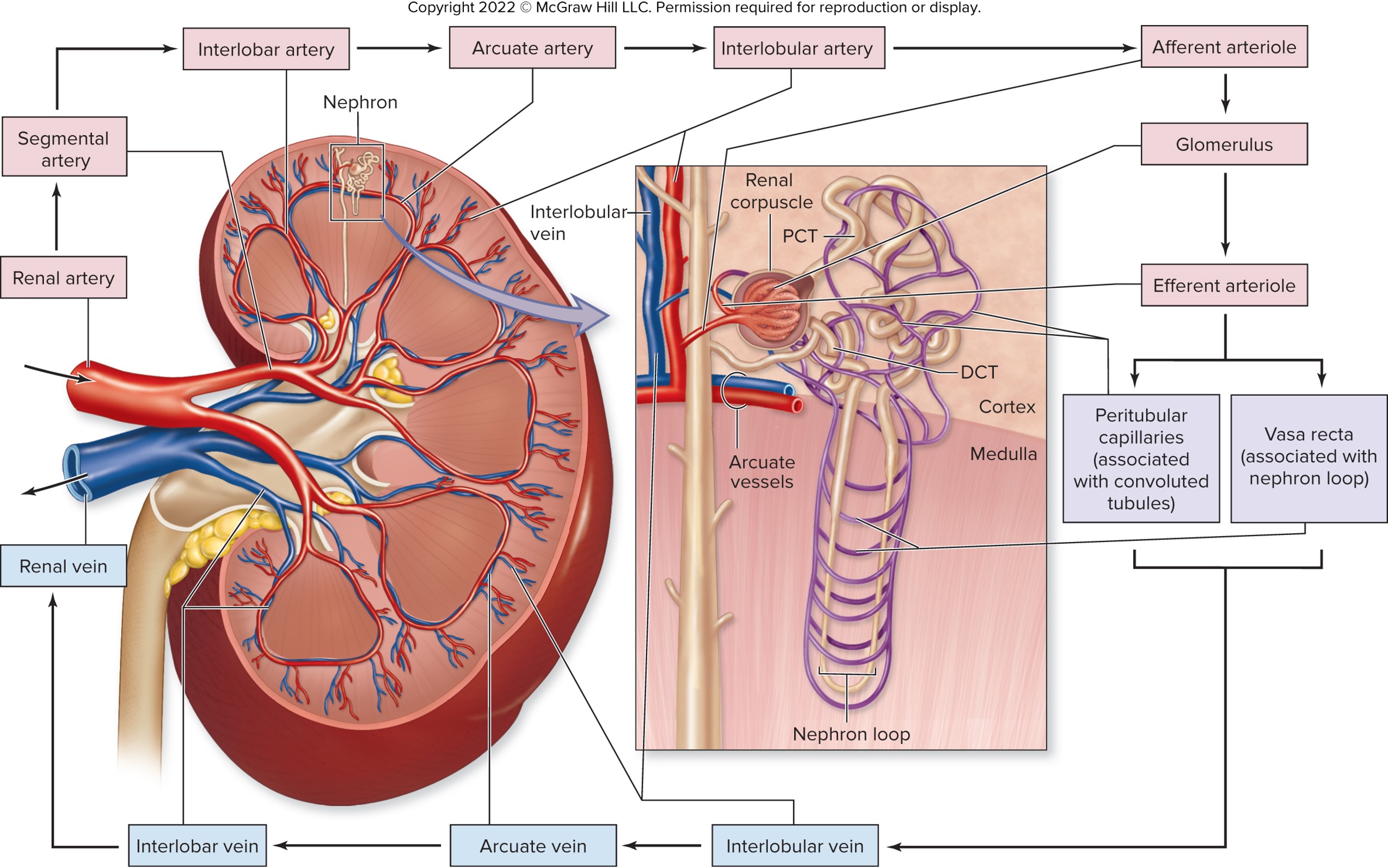
segmental arteries
branch from renal arteries within the renal sinus
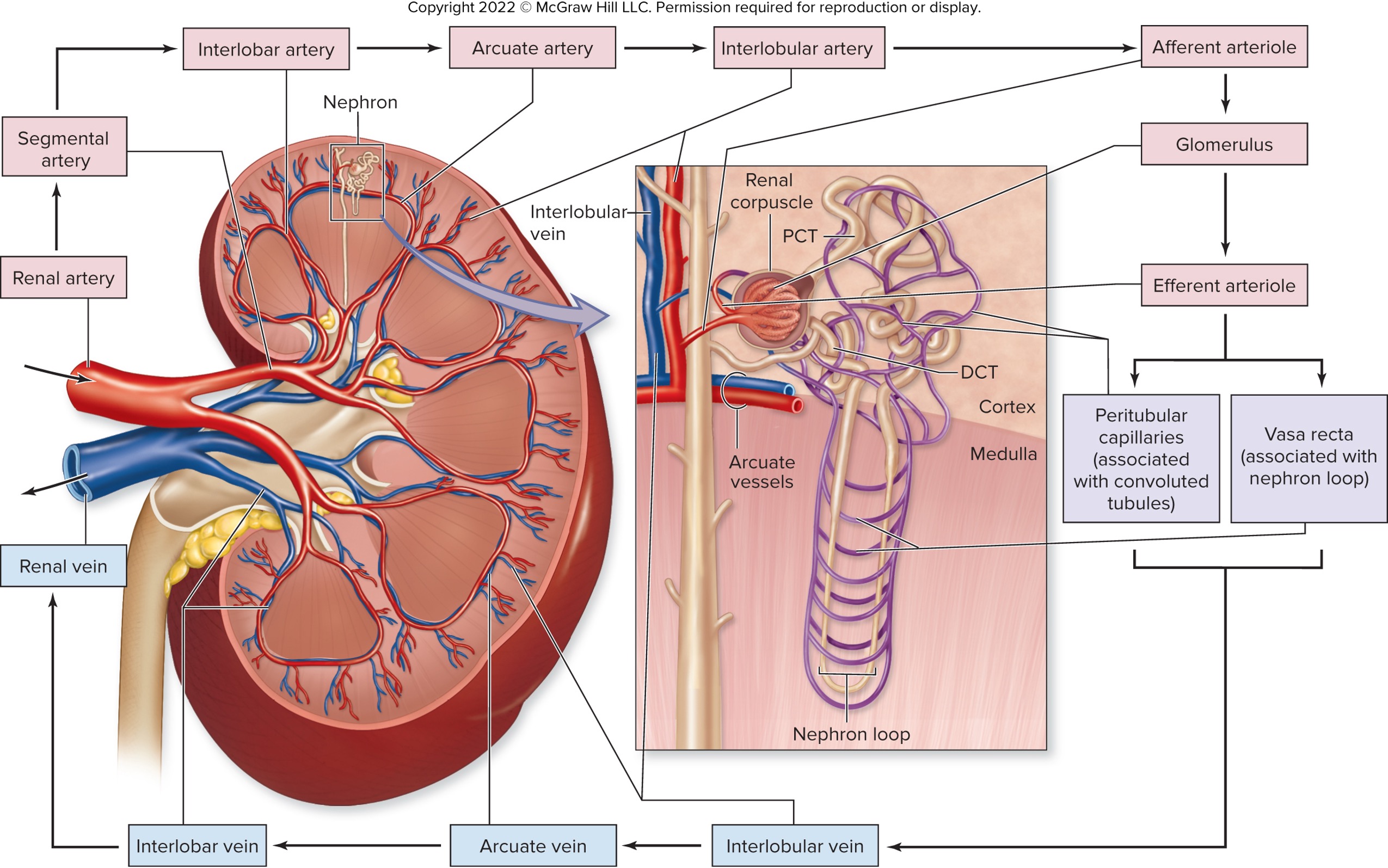
interlobar arteries
branch from segmental arteries
travel through renal columns toward corticomedullary junction
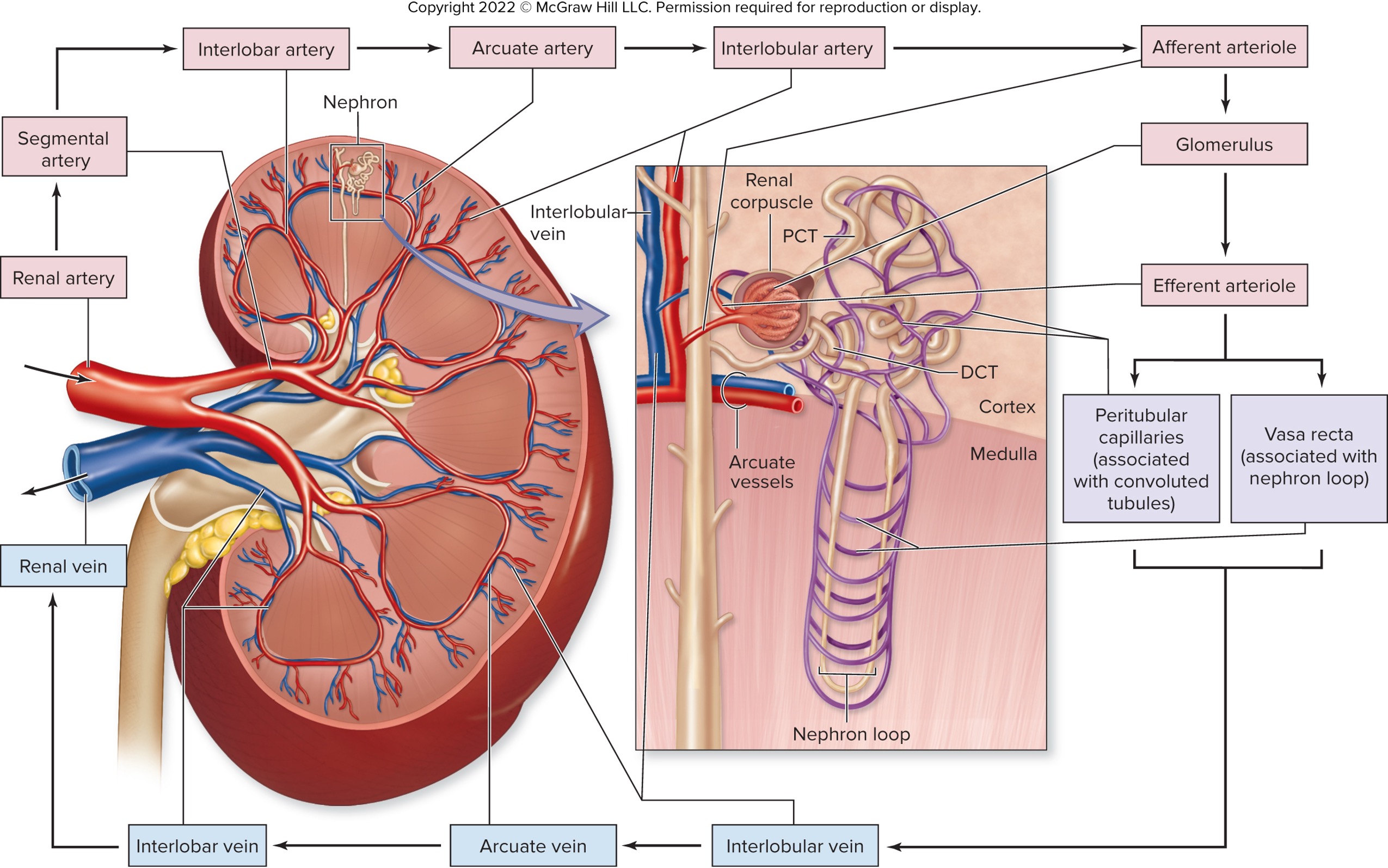
arcuate arteries
branch from interlobar arteries at corticomedullary junction
branch parallel to base of medullary pyramid
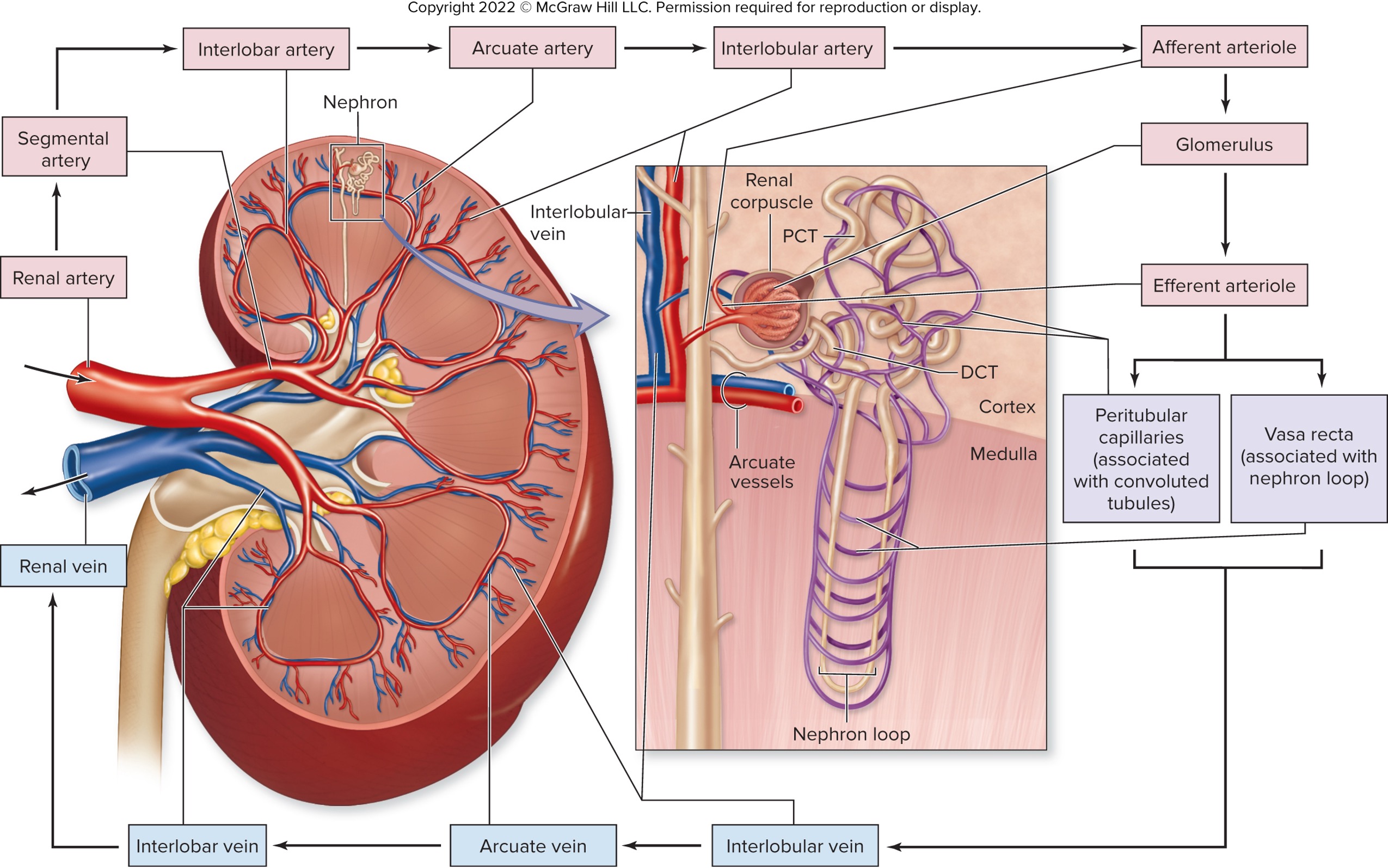
interlobar arteries
branch from arcute arteries
project peripherally into cortex
afferent arterioles branching off
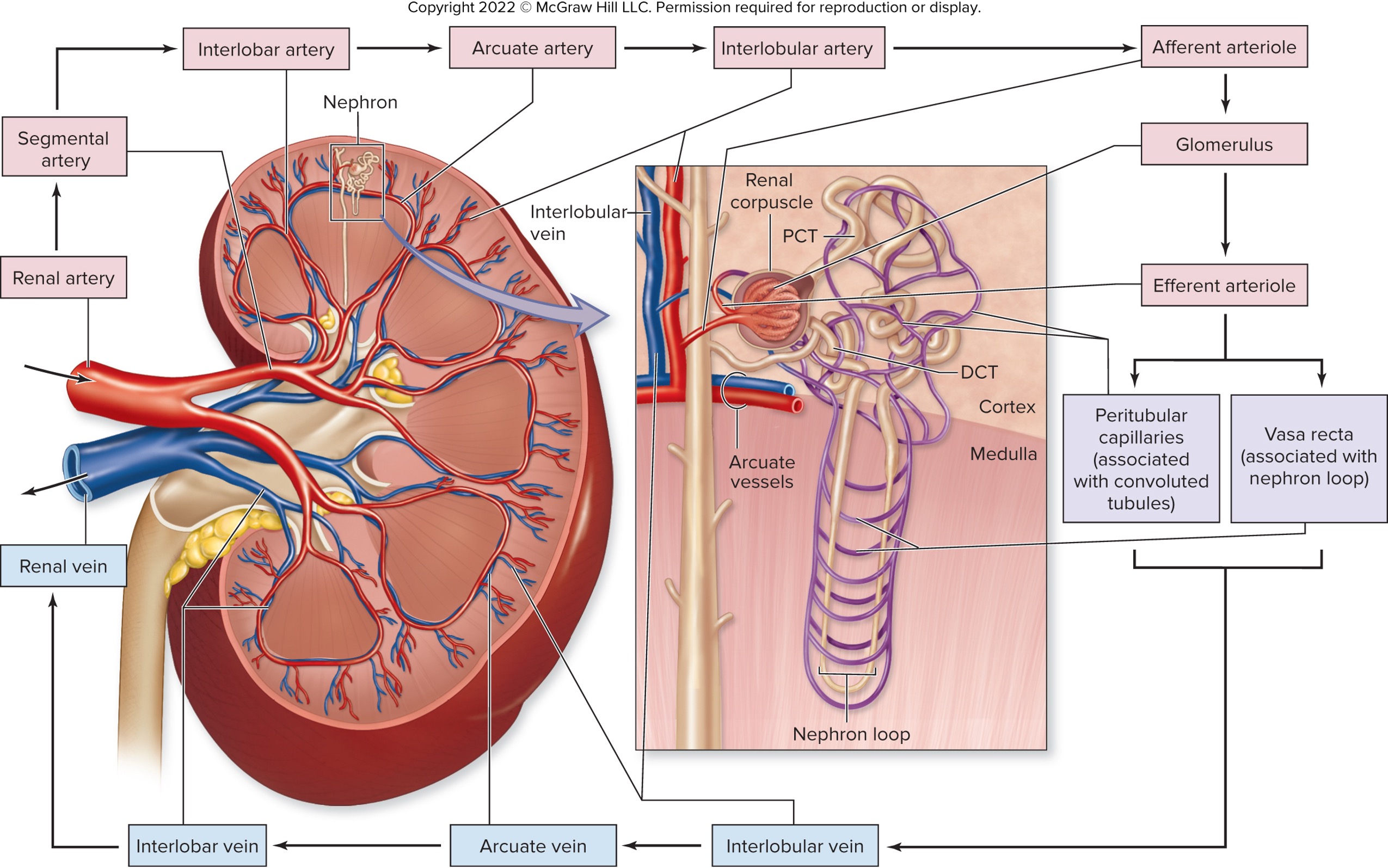
afferent artioles
ones that enters the renal corpuscle forming the glomerulus
some blood plasma filtered here
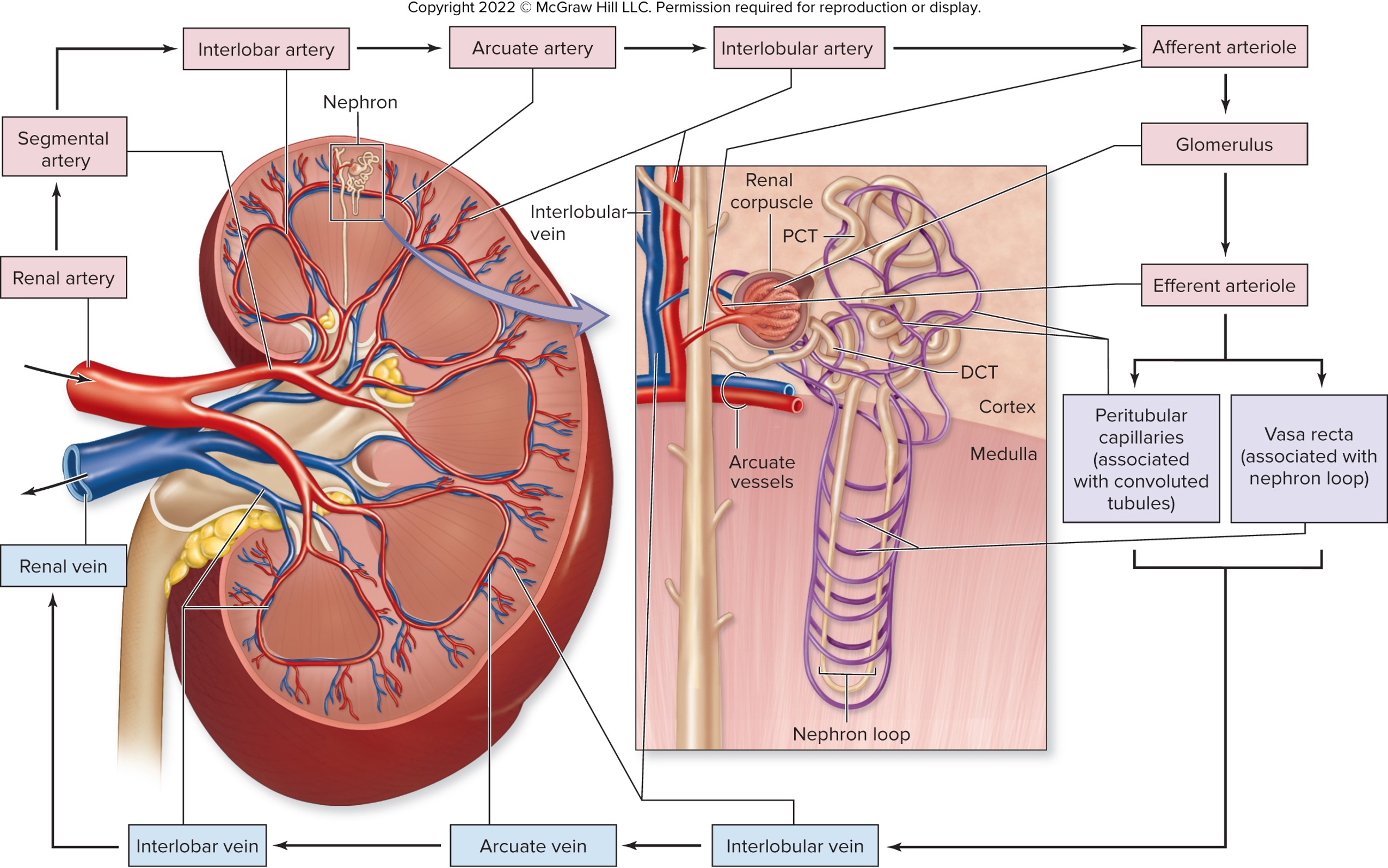
efferent arteriole
ones that leave the corpuscle
branches into the peritubular capillaries or vasa recta
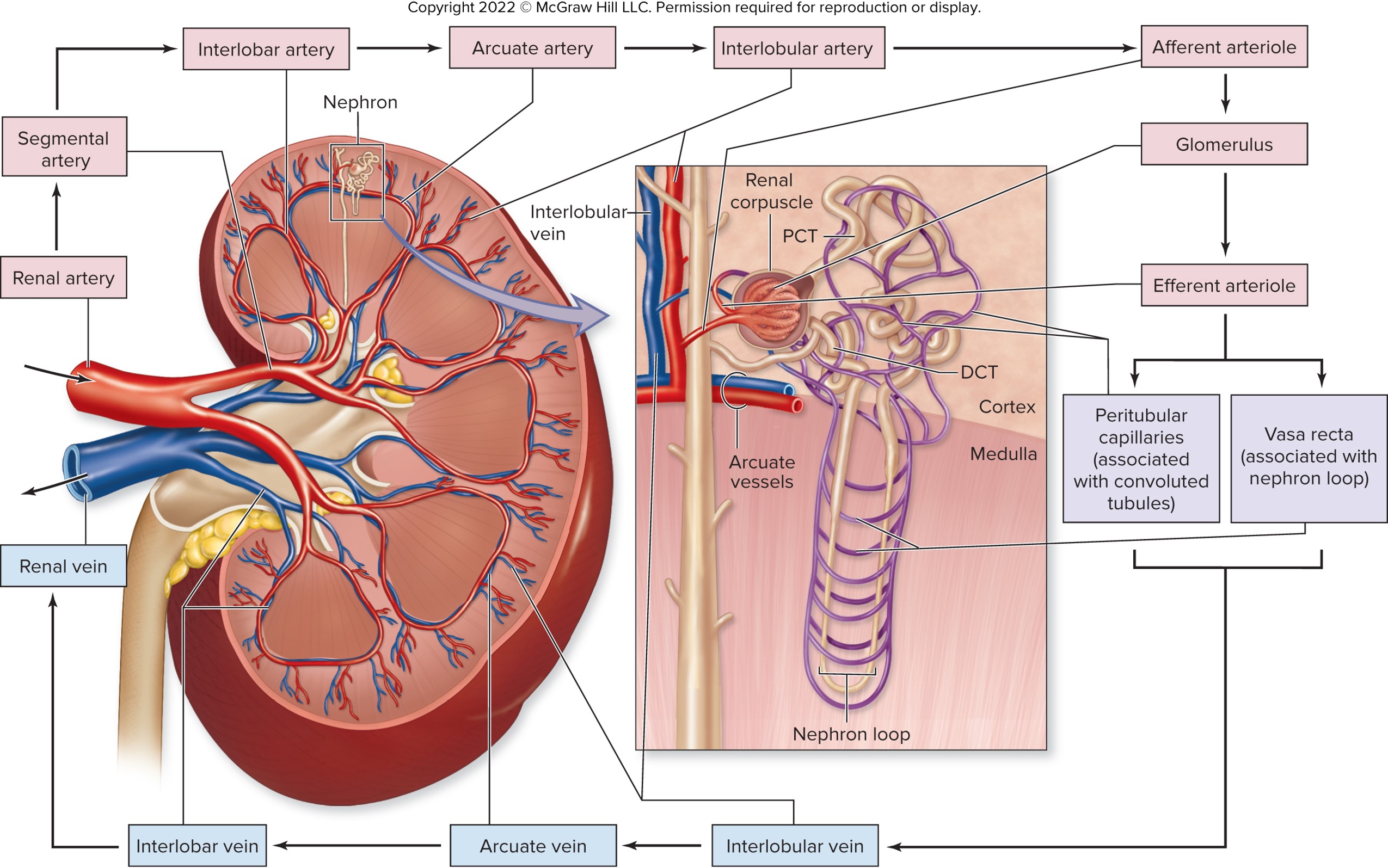
peritubular capillaries
intertwined around PCT and DCT
primarily reside in cortex of kidney
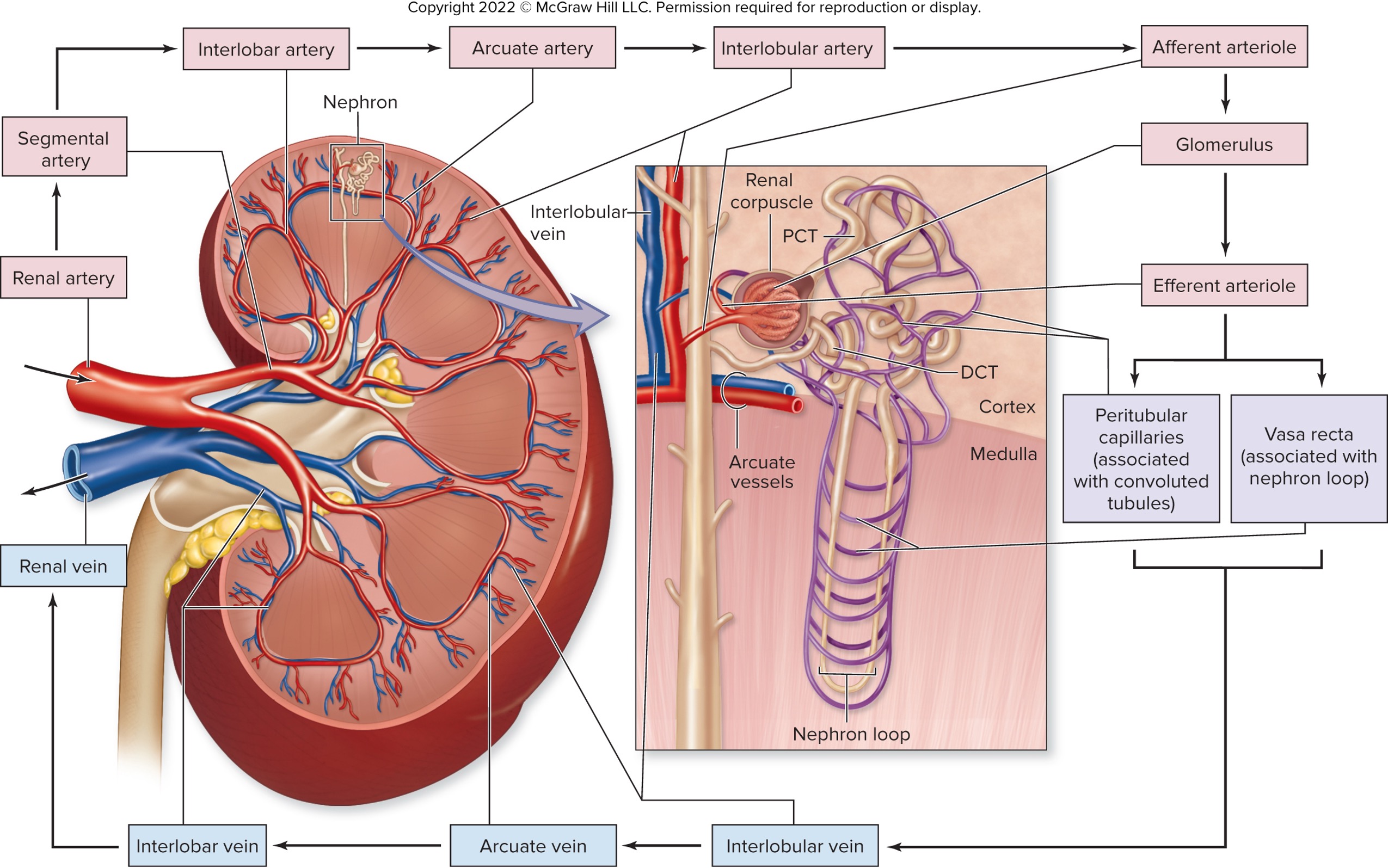
vasa recta
straight capillaries bed associated with the nephron loop
primarily reside in medulla of kidney
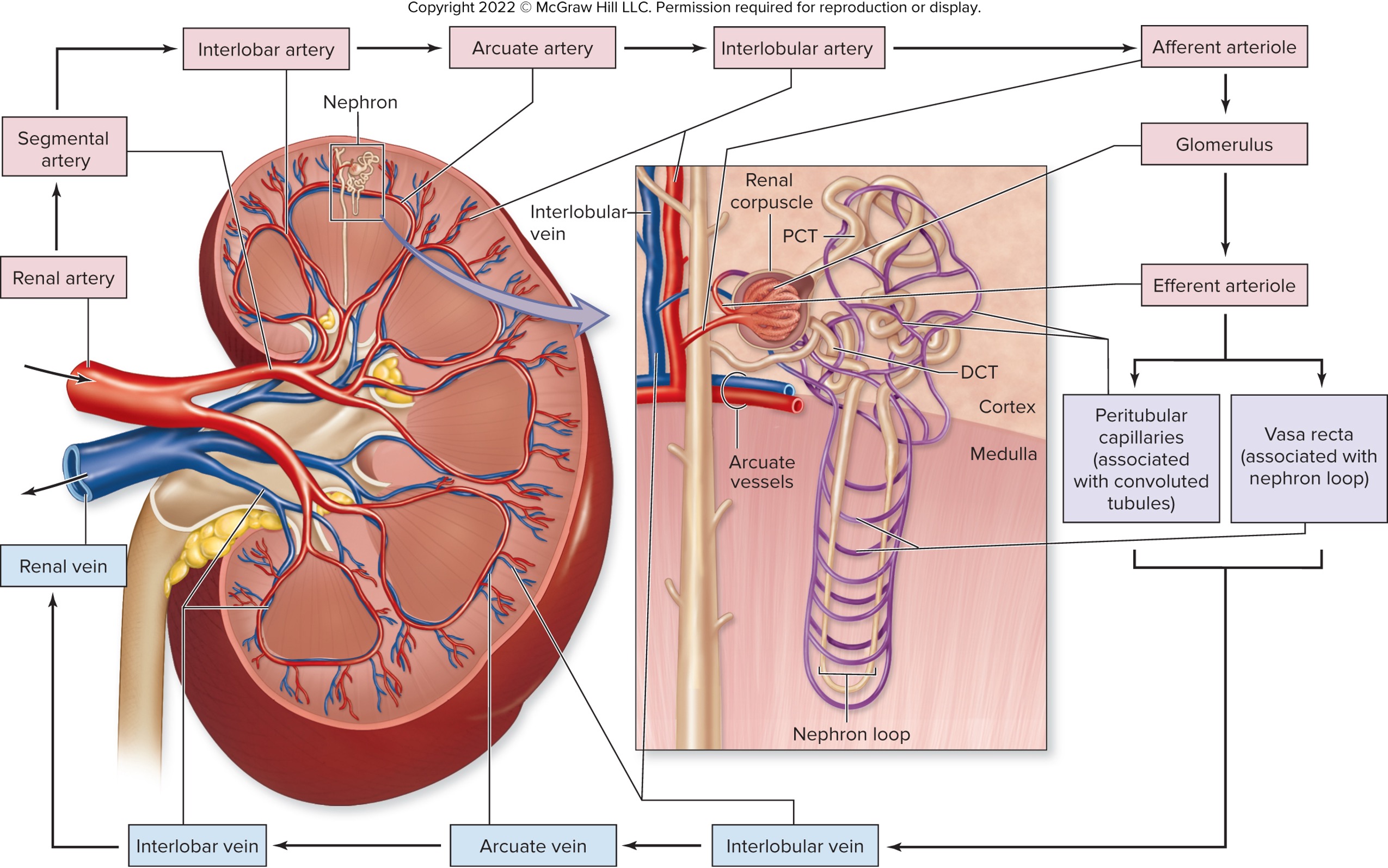
blood move through the ____________ capillaries to be filtered and then it passes through the ____________ capillaries or ____________ for gas exchange, nutrients, waste and then finally drain into network of veins
glomerular; peritubular; vasa recta
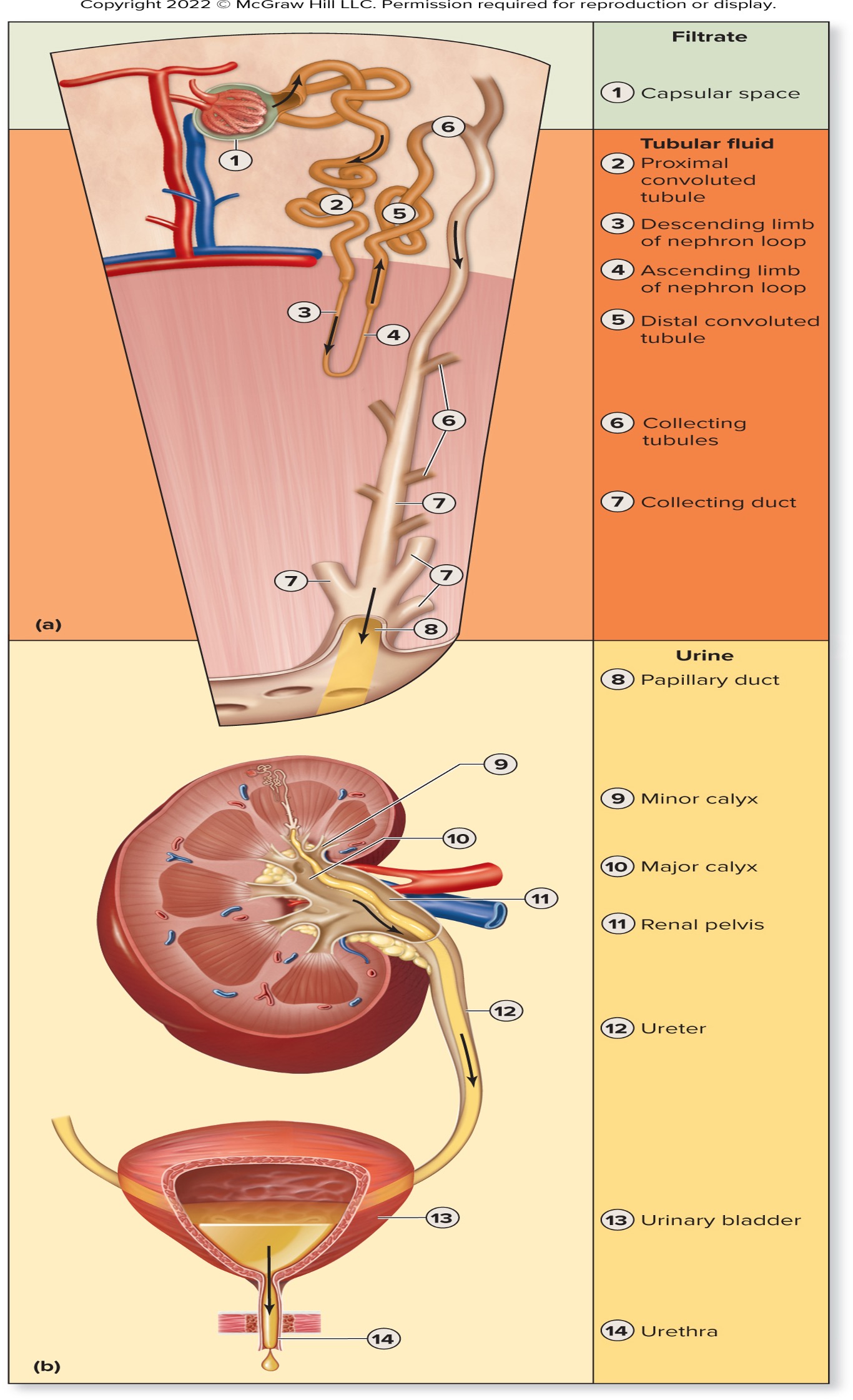
filtrate
water and solutes filtered from blood plasma at the glomerulus that is able to move across the wall of glomerular capillaries into the capsular space
trace the movement of filtrate → tubular fluid → urine starting from the capsular space…
capsular space
proximal convoluted tubule
descending limb of nephron loop
ascending limb of nephron loop
distal convoluted tubule
collecting tubules
collecting ducts
papillary duct
minor calyx
major calyx
renal pelvis
ureter
urinary bladder
urethra
glomerular filtration
the movement of subtances from the blood within the glomeruls into the capsular space
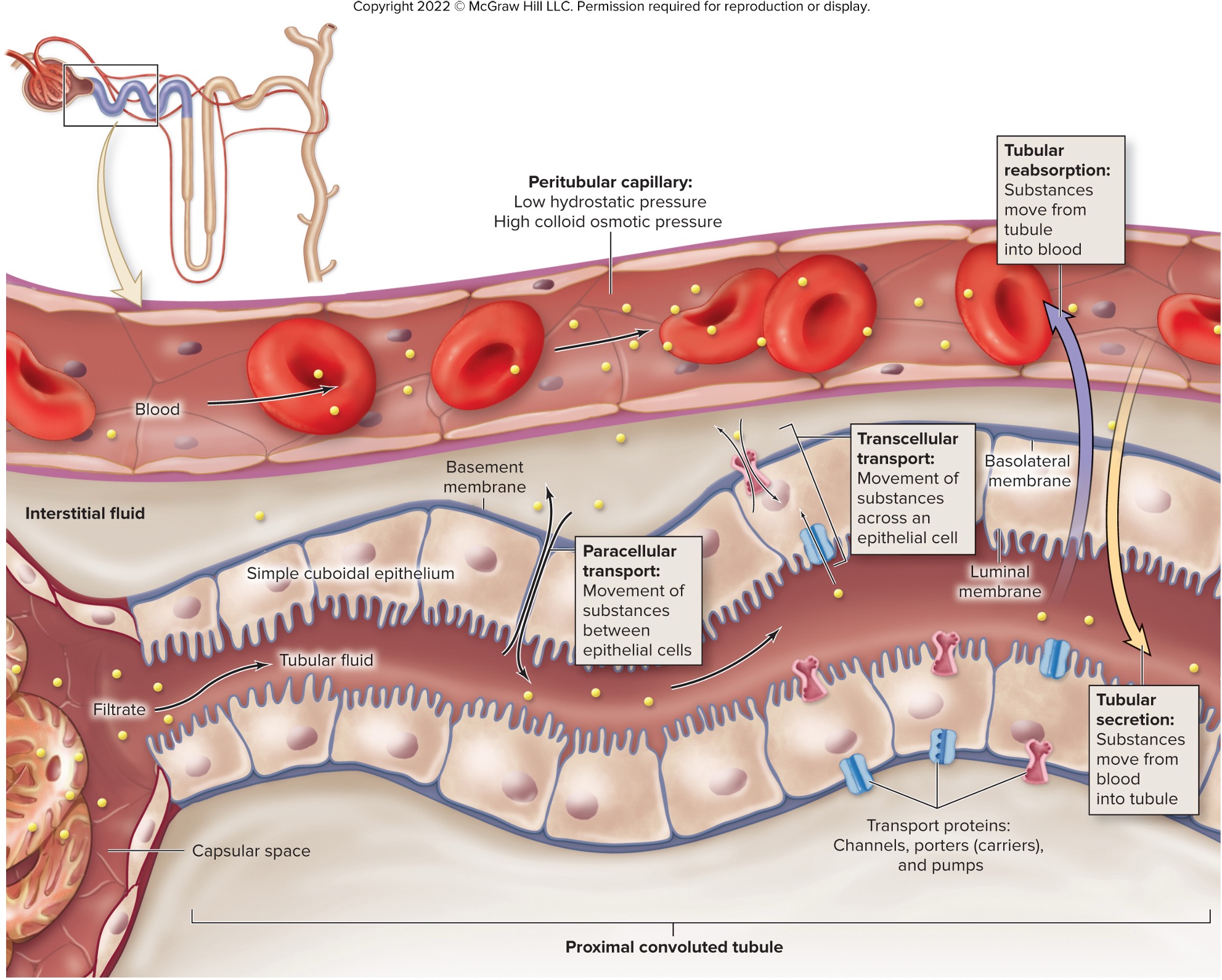
tubular reabsorption
the movement of sustbances from the tubular fluid back into the blood
tubular secretion
the movement of susbtances from the lood into the tubular fluid
what are the different steps of urine formaton?
glomerular filtration (happens in the glomerular capillaries that separate some water and dissolved solutes from blood) —> water and solutes enter capsular space of renal corpuscle (filtrate)
tubular reabsorption (happens in the tubules where the water and solutes would move and get reabsorbed back into the BV to maintain balance of fluid electrolytes)
tubular secretion (happens in the, movement of solute by active transport out of the blood into tubular fluid to maintain fluid and electrolytes balance
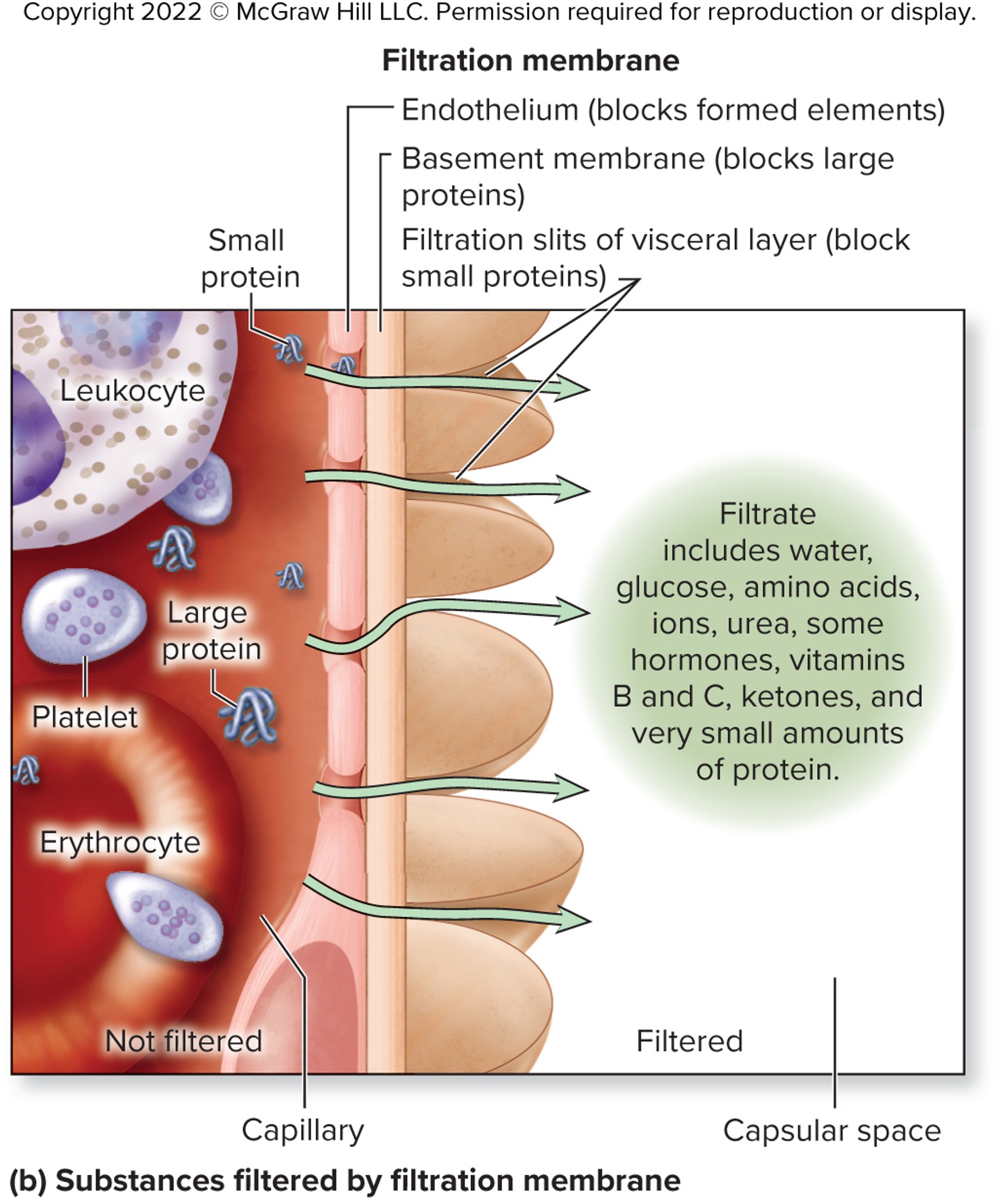
what are the characteristics of the filtration membrane of the glomerulus
porous, thin, negatively charged structure
formed by glomerulus and visceral layer of the glomerular capsule
made up of different layers
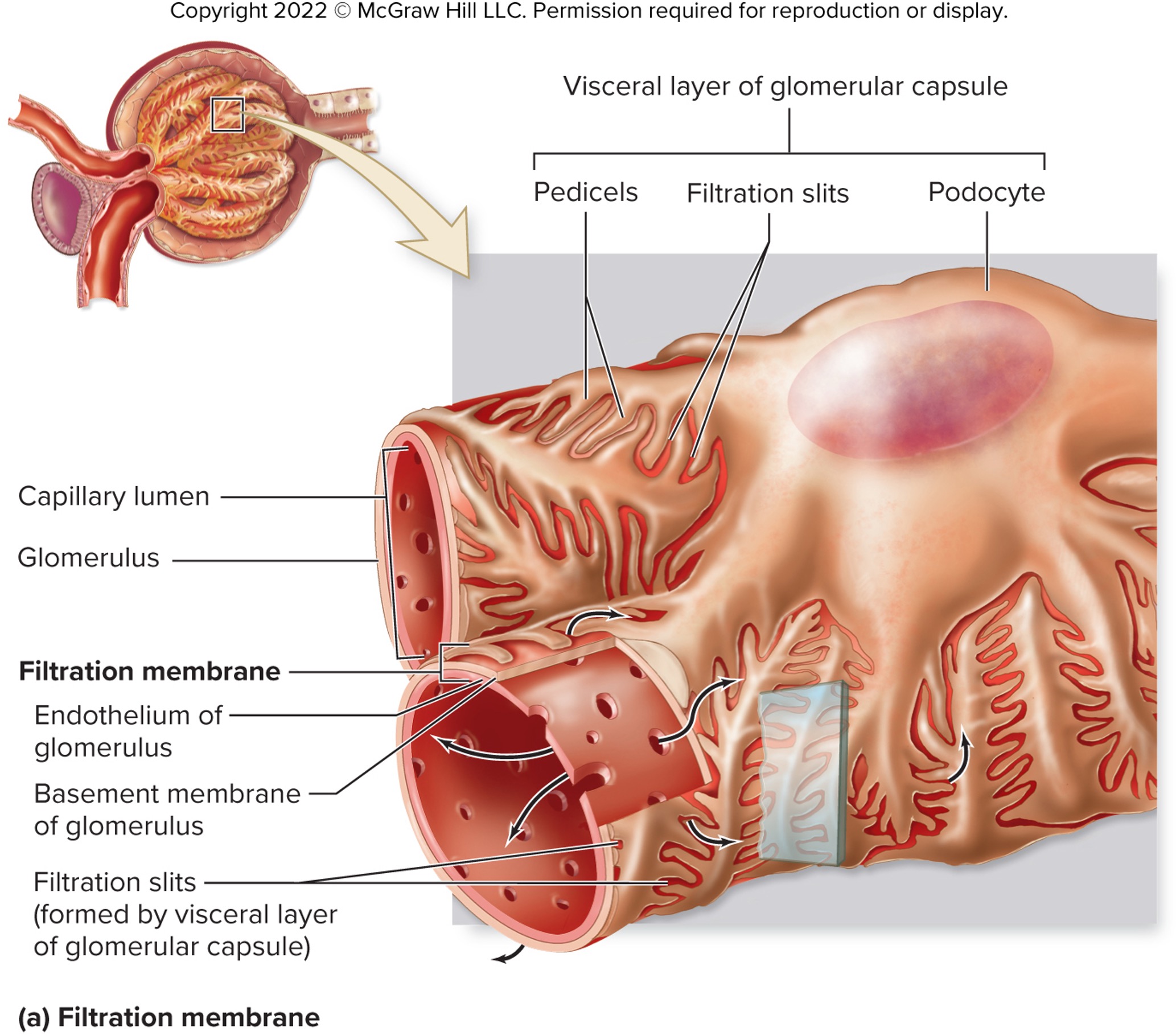
what are the different layer of the filtration membrane and their unique functions?
endothelium of glomerulus - fenestrated to allow plasma and dissolved substances to pass and restrict passage for larger substances
basement membrane of glomerulus - restrict passage of large plasma proteins (glycoproteins and proteoglycan)
visceral layer of glomerular capsule - composed of podocytes and have long processes called pedicels that support capillary wall and restrict passage of most small proteins
mesangial cells - positions between glomerular capillary loosp that have phagocytic, contractile, and signalling properoties
true or false: 180 L of urine is produced daily
true; filtered plasma with certain solutes and minimal amounts of proteins
some filtered material that are trapped within the basement membrane are phagocytized by ________cells
mesangial
what are the three categories of substances in the blood?
freely filtered (small substances that pass easily through filtration membrane)
not filtered (form elements an large proteins that cannot pass thru)
limited filtration (proteins of intermediate size tha usually blocked from filtration but occasionally go through)
glomerular hydrostatic (blood) pressure (HPg)
“pushes” water and solutes out of the glomerulus into the capsular space of renal corpuscle
→ allow filtration to occur
higher than blood pressure of other systemic capillaries
dependent on the diameter of the afferent and efferent arteriole
blood colloid ostomic pressure (OPg)
osmotic pressure exerted by dissolved solutes
opposes filtration
→ draws fluid back into glomerulus
capsular hydrostatic pressure (HPc)
pressure in the glomerular capsule due to filtrate
impede movement of additional fluid
net filtration pressure (NFP) (slide 46)
HPg - (OPg - HPc) = NFP
blood going out through the efferent is _________ because most of the water leaked out of it
viscous
which of the filtration pressure is directly related to blood pressure?
glomerular hydrostatic pressure (HPg)
glomerular filtration rate (GFR)
rate at which the volume of filtrate ie formed (volume per unit of time - usually per 1 min)
what does increased net filtration pressure cause?
increases GFR
increases solutes and water remaining in tubular fluid
increases substances in urine
decreases filtrate reabsorption
glomerular filtration rate (GFR) helps kidney _____________ based on physiologic condition
control urine production
what are the factors that influence glomerular filtration rate?
changing the luminal diameter of afferent arteriole
altering surface areas of filtration membrane
intrinsic controls of regulation of glomerular filtration rate
processes of regulation that happens within the kidney itself through myogenic response and tubuloglomerular feedback mechanism
extrinsic controls of regulation of glomerular filtration rate
proccesses of regulation that happens external to the kidney
myogenic response
contraction or relaxation of smooth muscle of afferent arteriole in response to stretch
causes smooth muscle cells to relax/contract and the vessel to dilate/constrict
allows more/less blood into the glomerulus
→ increased BP = more stretched
compensate for lower/greater system pressure
GFR remains normal
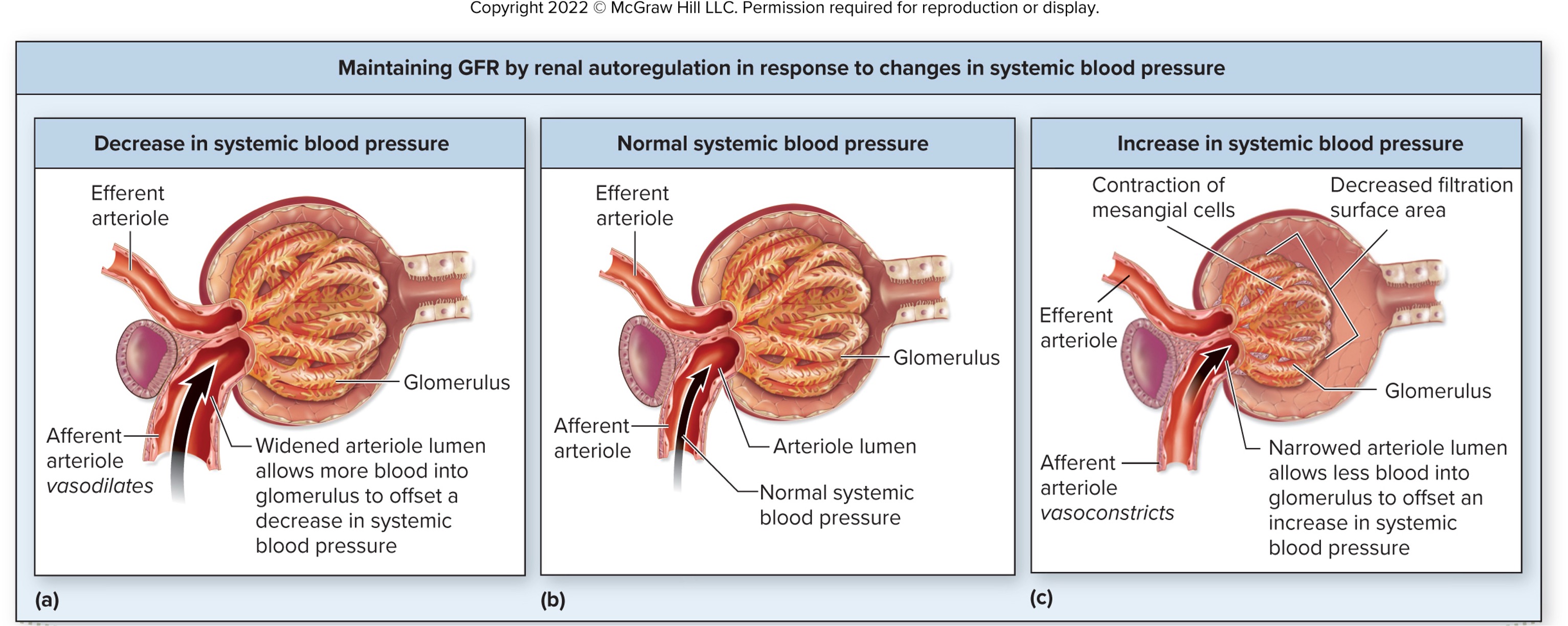
what would the myogenic response be if there is there decrease in systemic blood pressure?
afferent arteriole vasodilates to allow more blood into the glomerulus to offset a decrease in systemic blood pressure
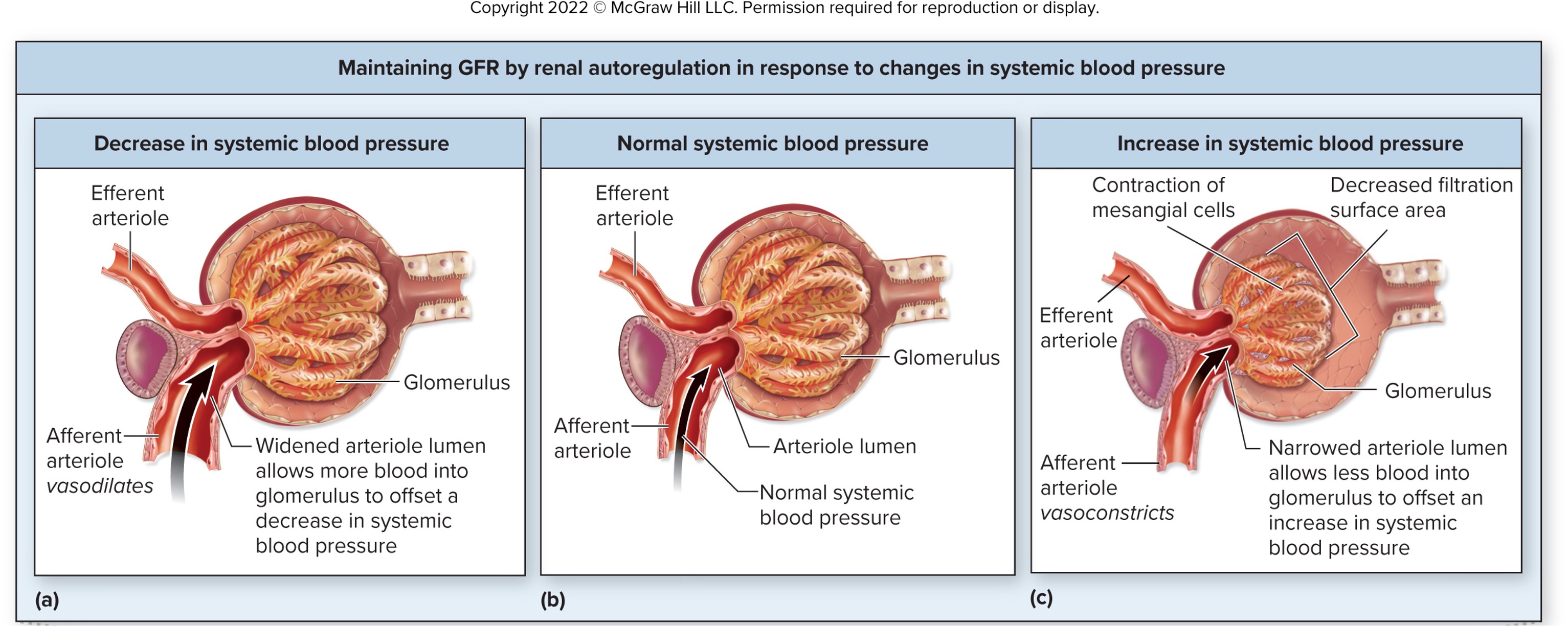
what would the myogenic response be if there is there increase in systemic blood pressure?
afferent arteriole constrict to allow less blood into the glomerulus to offset an inrease in systemic blood pressure
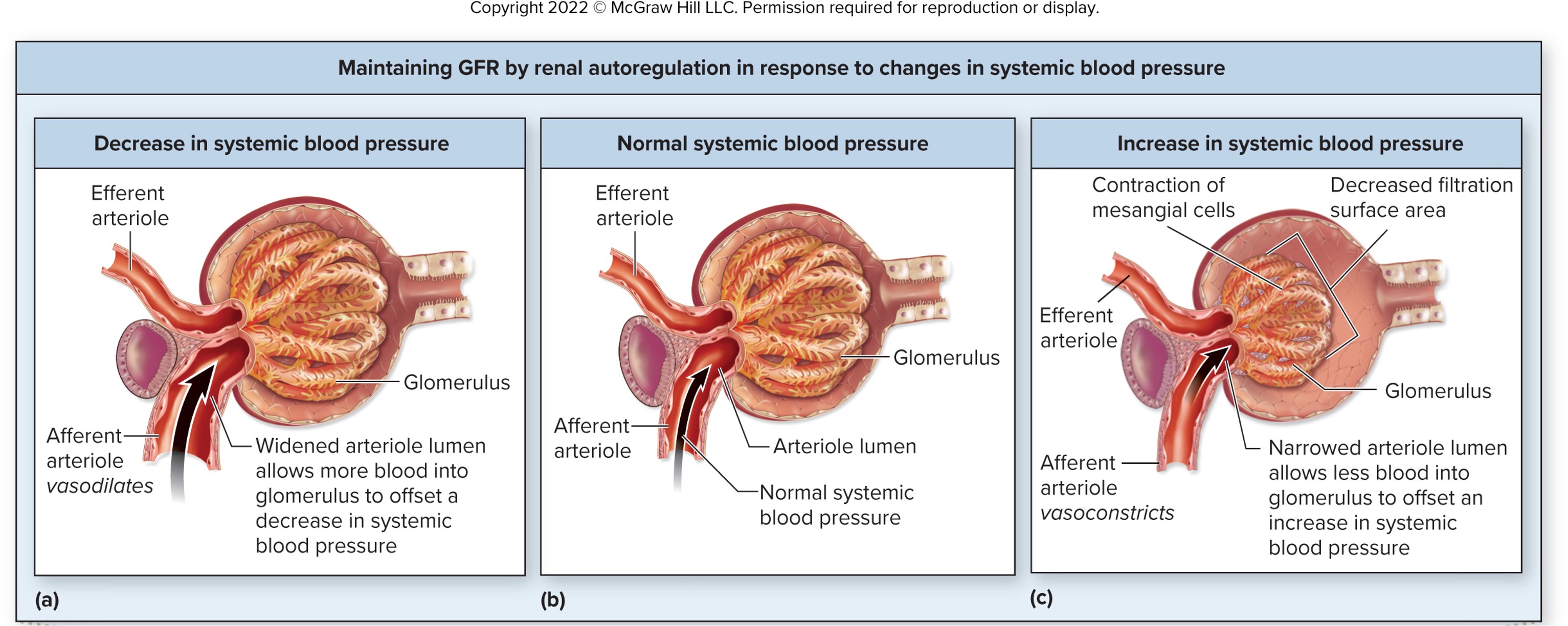
tubuloglomerular feedback mechanism of the regulation glomerular filtration rate
back up system second to the myogenic response to increased/decrease blood pressure - also control the contraction or relaxation of smooth muscle of afferent arteriole
detected by macula densa cells in juxtaglomerular apparatus
result in further vasoconstriction/vasodilation of afferent arteriole
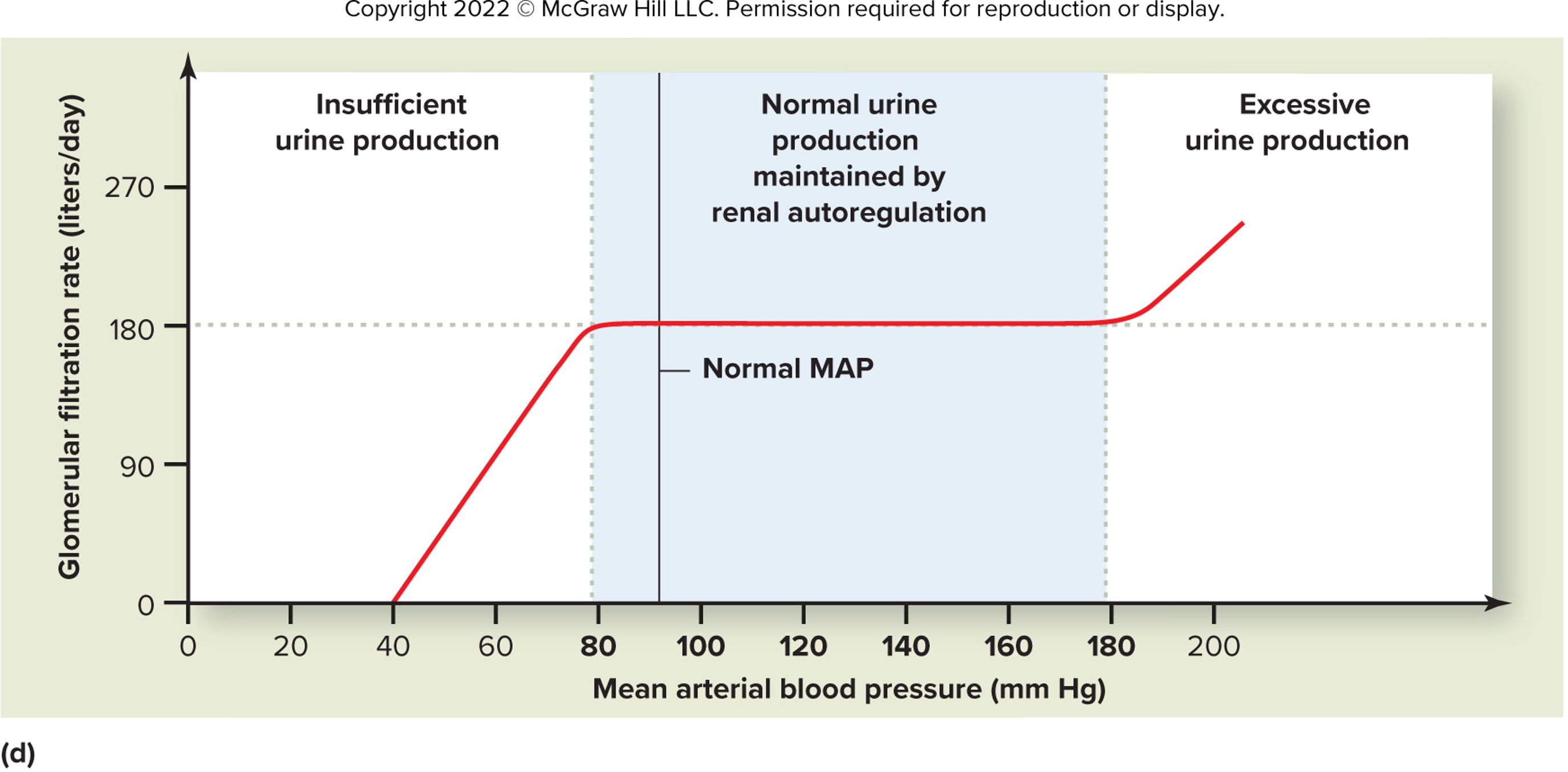
what is the purpose of renal autoregulation?
maintains stable GFR despite BP fluctuations
effective range: 80–180 mmHg
uses myogenic mechanism (afferent arteriole) + tubuloglomerular feedback
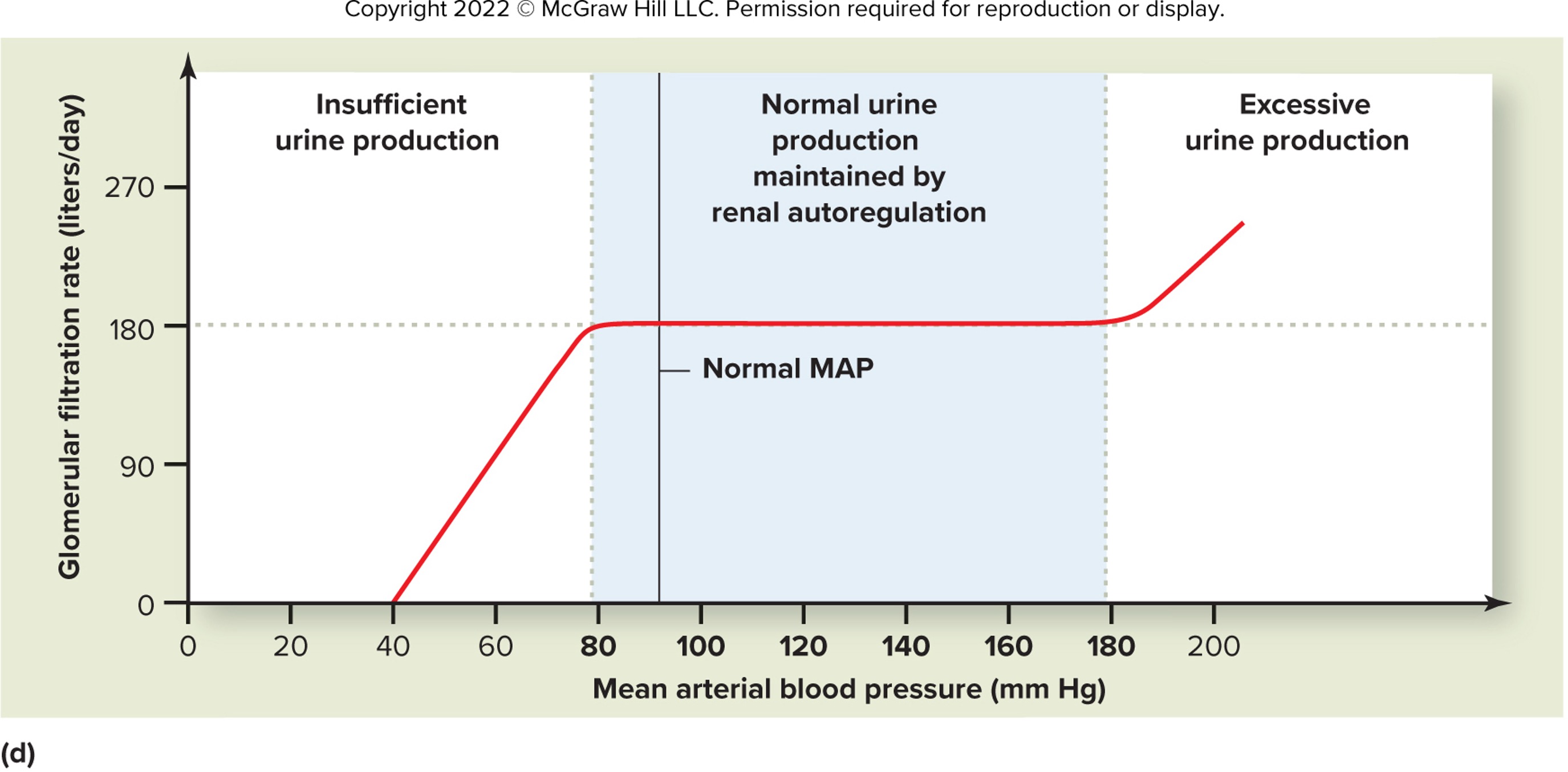
how does the kidney respond when BP drops below 80 mmHg?
Arterioles maximally dilated (can’t compensate further)
because ↓ Glomerular hydrostatic pressure → ↓ GFR
Critical consequence:
Waste accumulation (azotemia)
Oliguria/anuria if severe
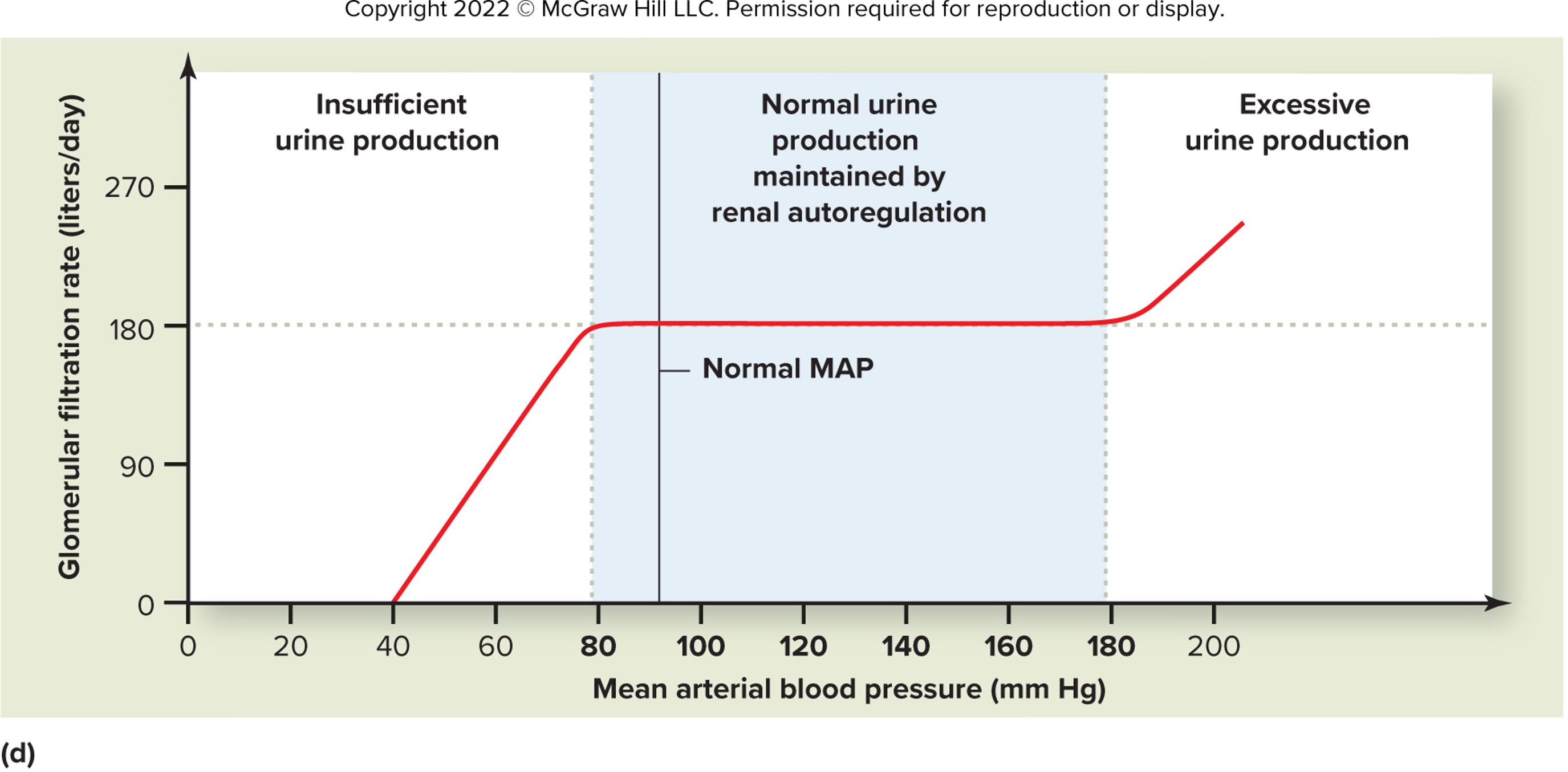
how does the kidney respond to BP >180 mmHg?
Arterioles maximally constricted (can’t compensate further)
↑ Glomerular pressure → ↑ GFR
Consequences:
Hyperfiltration injury (glomerular damage)
Proteinuria (loss of filtration barrier integrity)
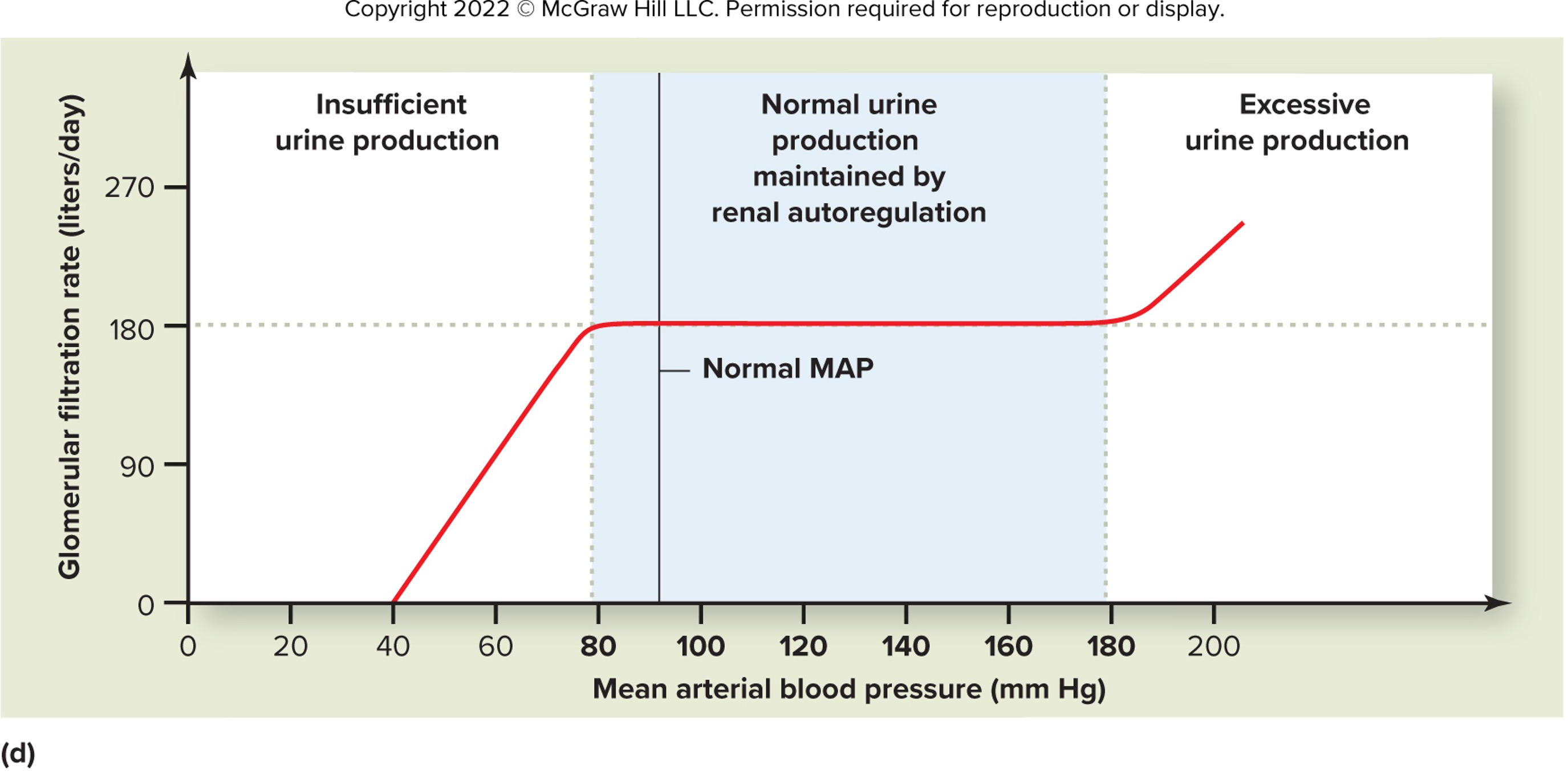
what happens when autoregulation of GFR and BP fails?
<80 mmHg: Acute kidney injury (prerenal azotemia)
>180 mmHg: Glomerulosclerosis (e.g., in hypertension)
Key sign: GFR becomes BP-dependent
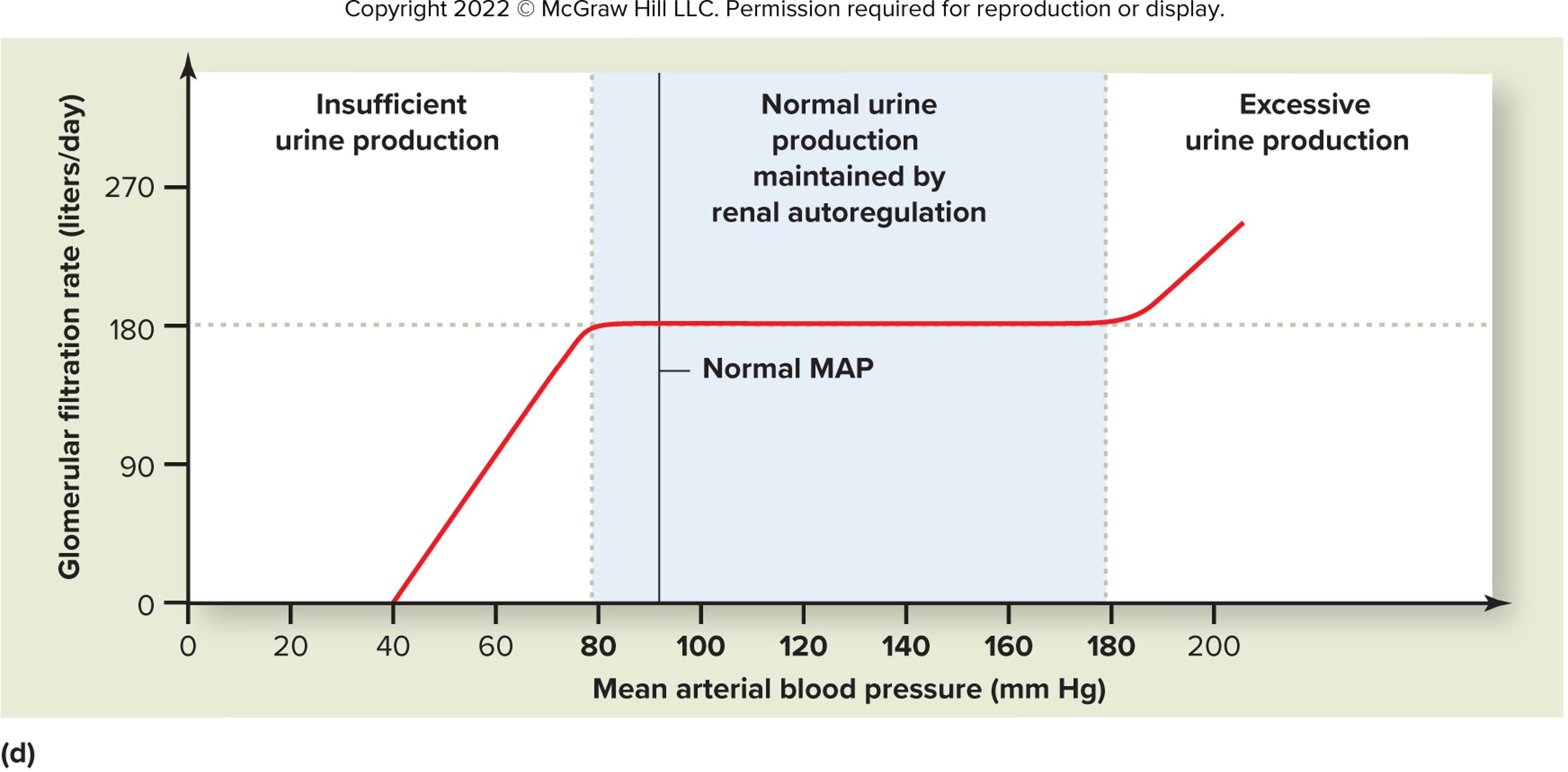
why is autoregulation limited to 80–180 mmHg?
lower limit: Arterioles physically can’t dilate further
upper limit: Smooth muscle can’t constrict enough to counteract higher pressure
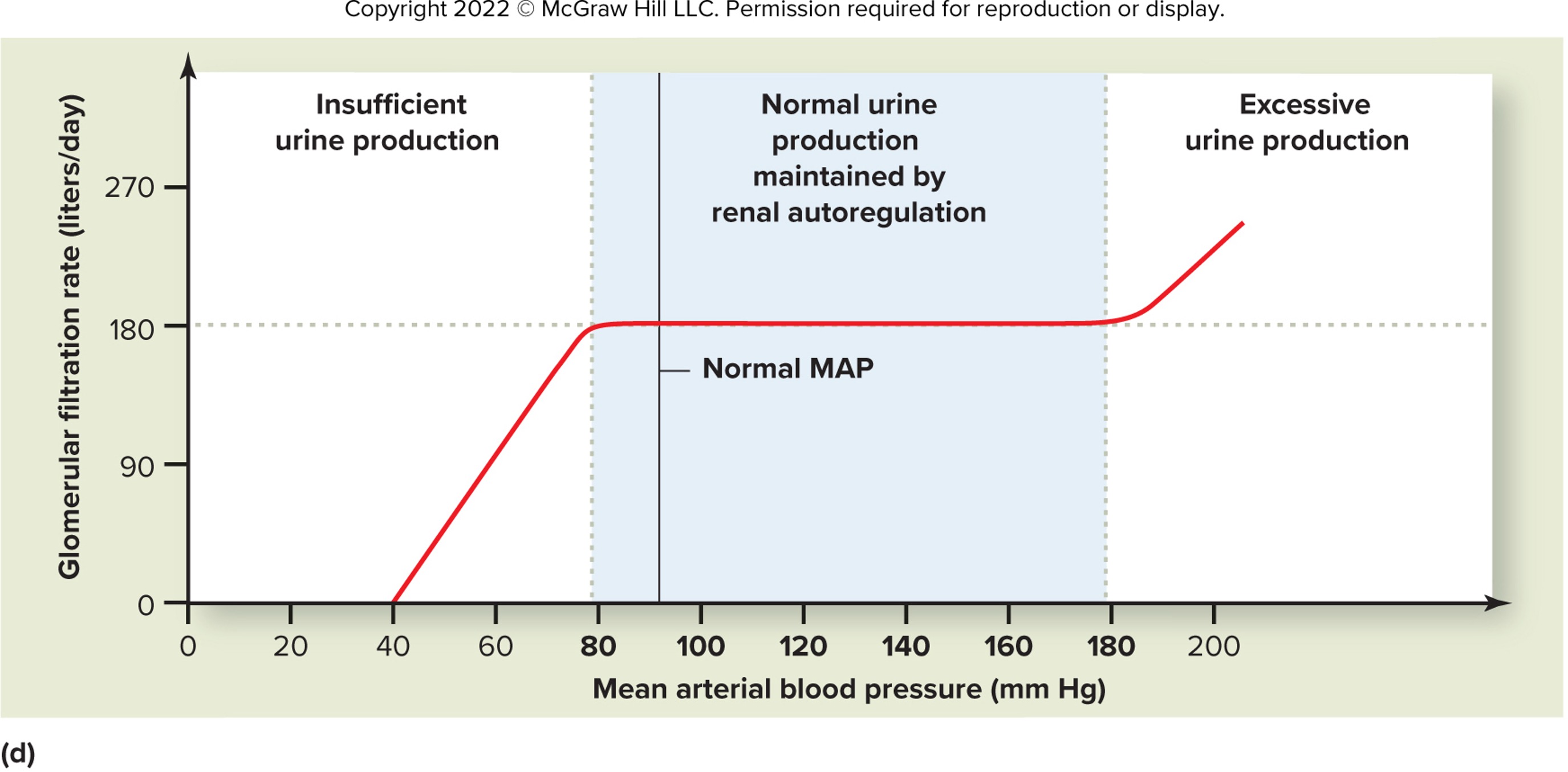
how does the kidney response to BP <50 mmHg?
GFR → near zero
Cessation of urine output
Life-threatening:
Electrolyte imbalances (hyperkalemia)
Metabolic acidosis
how do extrinsic controls differ from renal autoregulation?
Autoregulation: Maintains constant GFR (BP 80-180 mmHg)
Extrinsic controls: Adjust GFR for body needs (e.g., stress, hydration)
Primary mechanisms:
Sympathetic NS
RAAS (renin-angiotensin-aldosterone system)
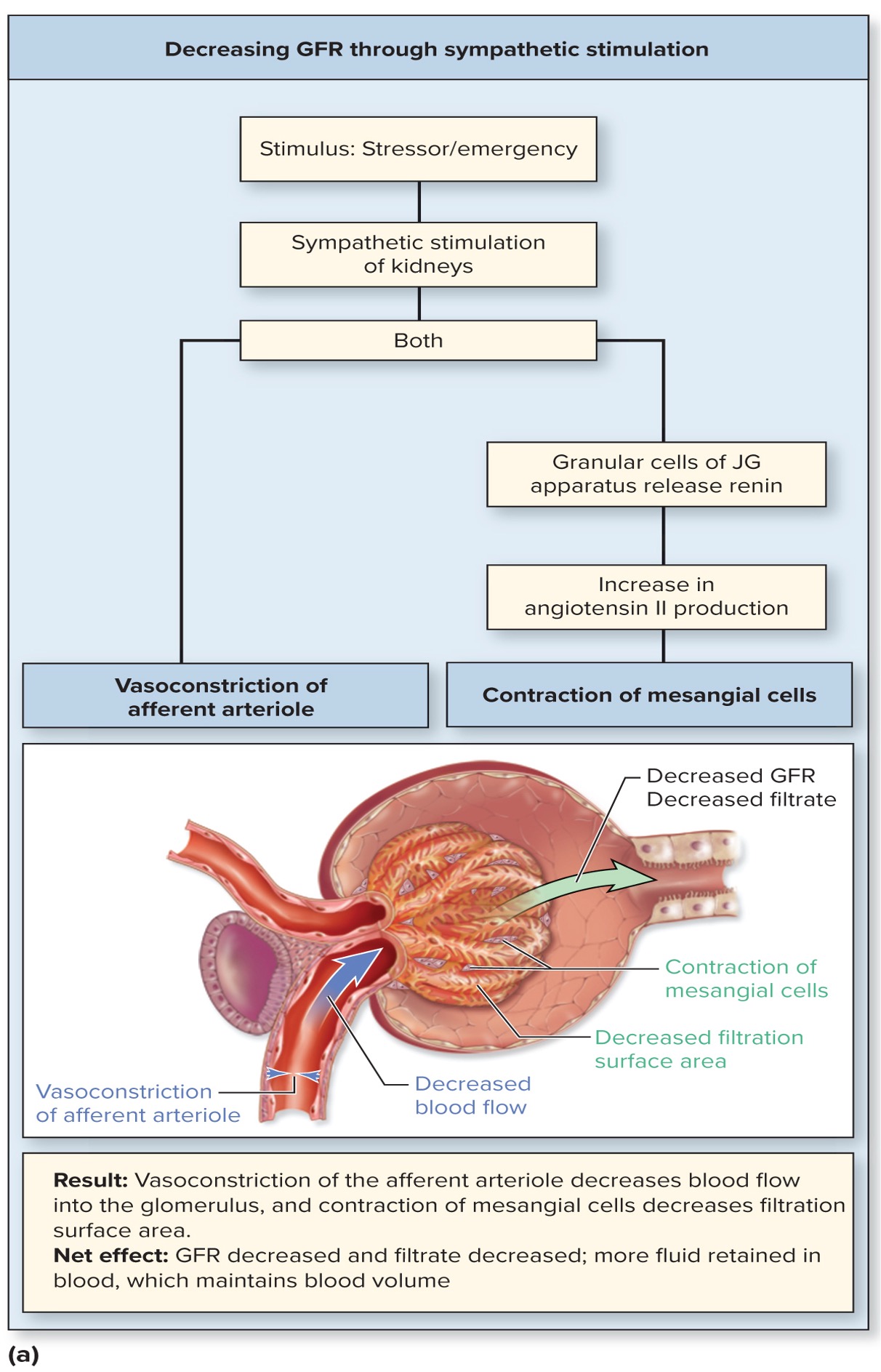
how does sympathetic activation reduce GFR?
Vasoconstriction of afferent > efferent arterioles (via α₁-adrenergic receptors)
↓ Blood flow → ↓ glomerular pressure → ↓ GFR
JG cells release renin → activates RAAS
Angiotensin II further constricts arterioles
Mesangial cell contraction ↓ filtration surface area
what stimulates JG cells to release renin?
↓ BP (renal baroreceptor response)
Sympathetic stimulation (β₁-adrenergic)
↓ NaCl at macula densa (tubuloglomerular feedback)
how does angiotensin II decrease GFR?
Constricts afferent & efferent arterioles (efferent > afferent)
Contracts mesangial cells → ↓ glomerular SA
Net effect: ↓ GFR, ↑ filtration fraction (conserves water)
Why does the body reduce GFR during stress?
Prioritizes blood flow to heart/brain (shunts from kidneys)
Conserves water/salt for BP maintenance
Trade-off: Temporary ↓ waste excretion
how can chronic sympathetic activation harm the kidneys?
prolonged vasoconstriction can lead to ischemic injury
RAAS overactivation → hypertension and glomerular damage
e.g., seen in heart failure, chronic stress, hemorrhagic shock
what is ANP and what triggers its release?
atrial natriuretic peptide (ANP)
released by cardiac atrial myocytes in response to atrial stretch, hypervolemia
opposes RAAS
ANP’s actions in one phrase?
"Dump the Volume!"
Dilates arterioles
Urine output ↑
Mesangial relaxation
Pressures drop
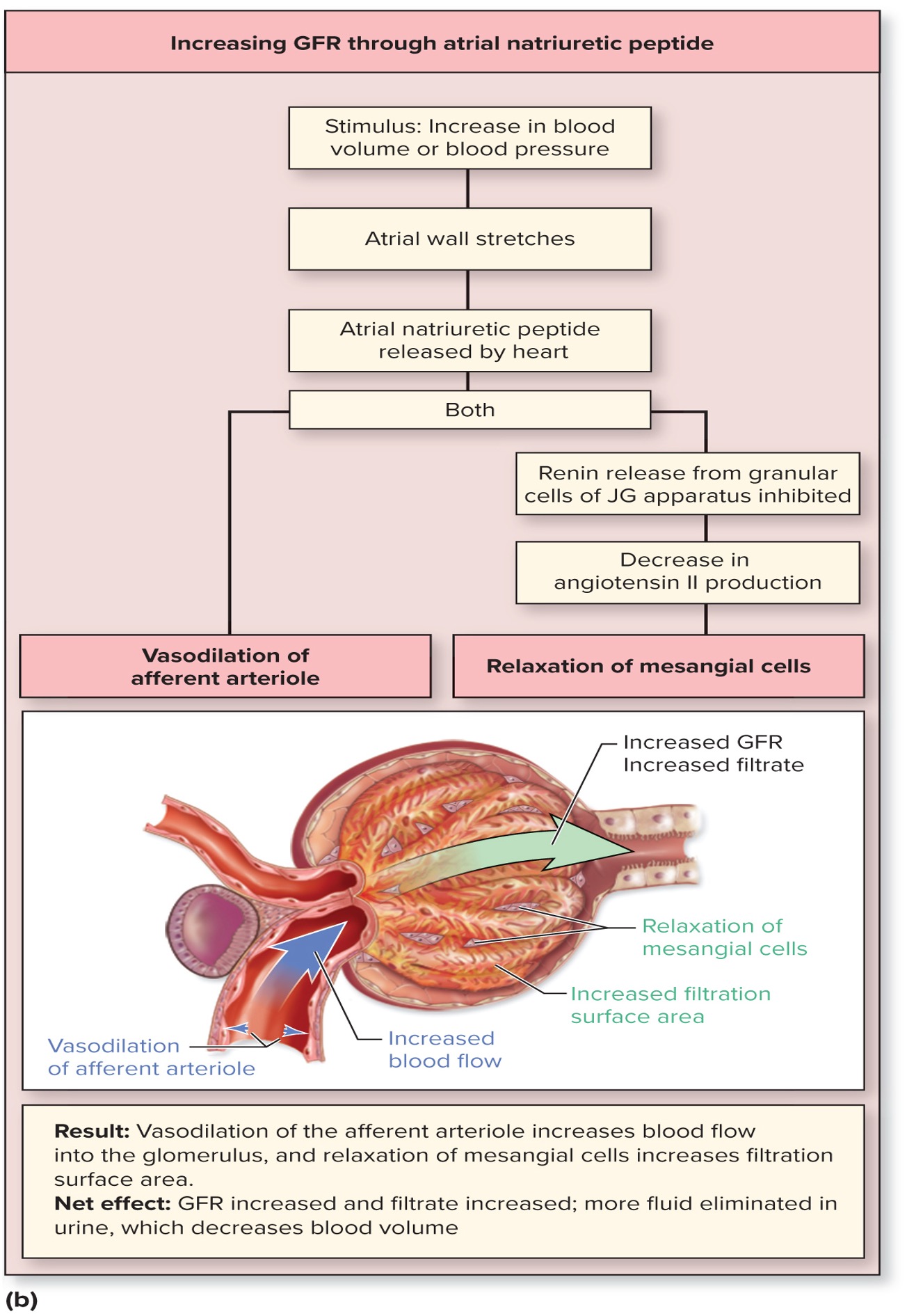
how does ANP (atrial natriuretic peptide) increases GFR?
Dilates afferent arteriole → ↑ glomerular pressure
Inhibits renin release → ↓ angiotensin II → relaxes mesangial cells → ↑ filtration surface area
Net effect: ↑ GFR, ↑ urine output (diuresis)
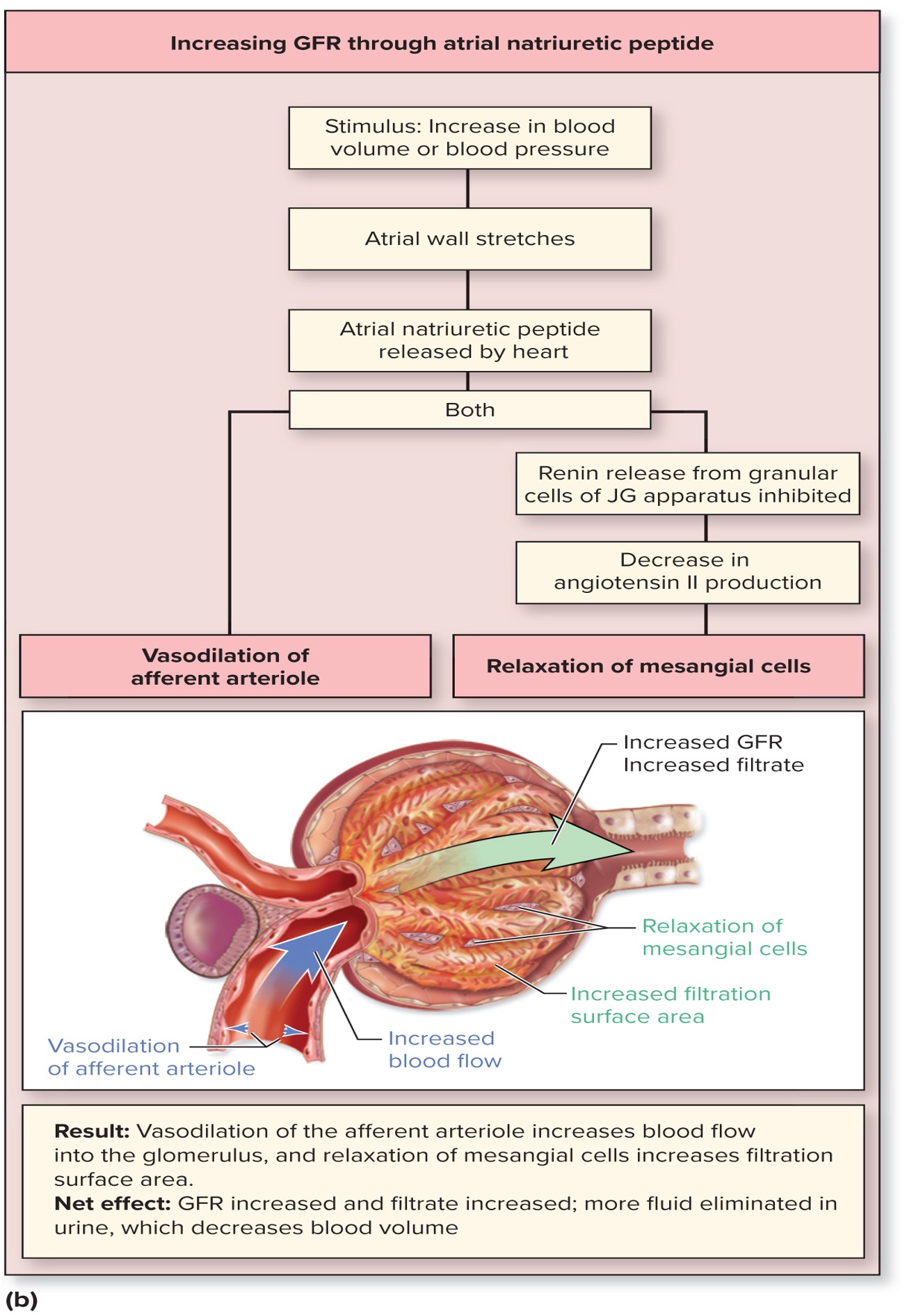
what are ANP’s overall effects on blood volume and pressure?
↓ Blood volume: ↑ Na⁺/water excretion (natriuresis)
↓ Blood pressure:
Vasodilation (systemic)
↓ Aldosterone (reduces Na⁺ reabsorption)
contrast ANP and sympathetic effects on GFR.
ANP: ↑ GFR (afferent dilation, ↓ RAAS) → lowers BP
Sympathetic: ↓ GFR (afferent constriction, ↑ RAAS) → raises BP
Balanced during homeostasis
When is ANP most active?
Volume overload (e.g., heart failure)
High-salt diet
Therapeutic target: Synthetic ANP (nesiritide) for acute HF
what is the functional unit for reabsorption/secretion in nephrons?
Simple epithelium of tubule wall
Forms transport barrier with:
Luminal membrane (faces filtrate)
Basolateral membrane (faces blood)
paracellular transport
movement of susbtances between epithelial cells
Driven by:
Concentration gradients
Solvent drag (water flow)
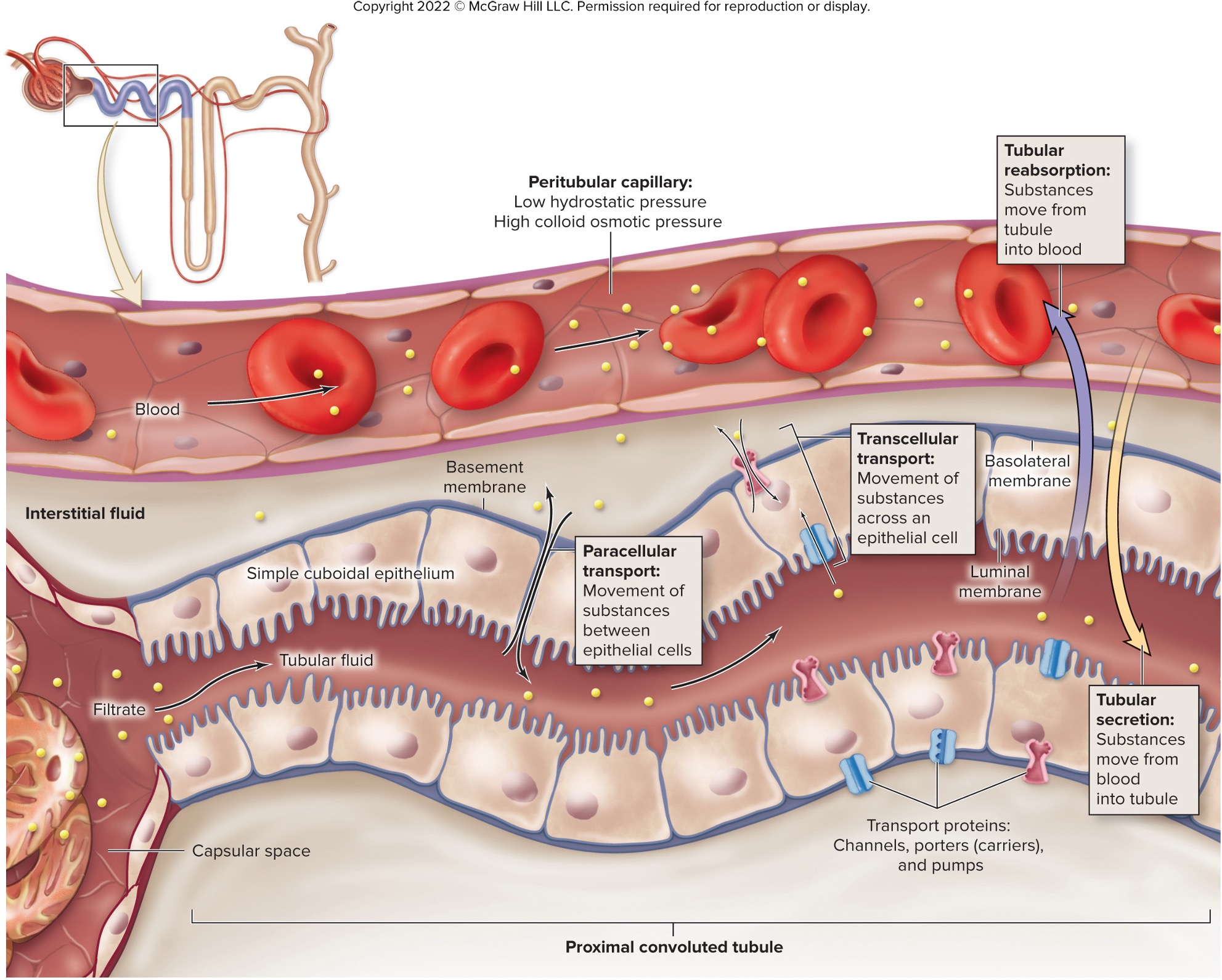
describe transcellular transport steps.
Luminal membrane: Substance enters cell
Cytoplasm: May be modified (e.g., metabolized)
Basolateral membrane: Exits to interstitial fluid
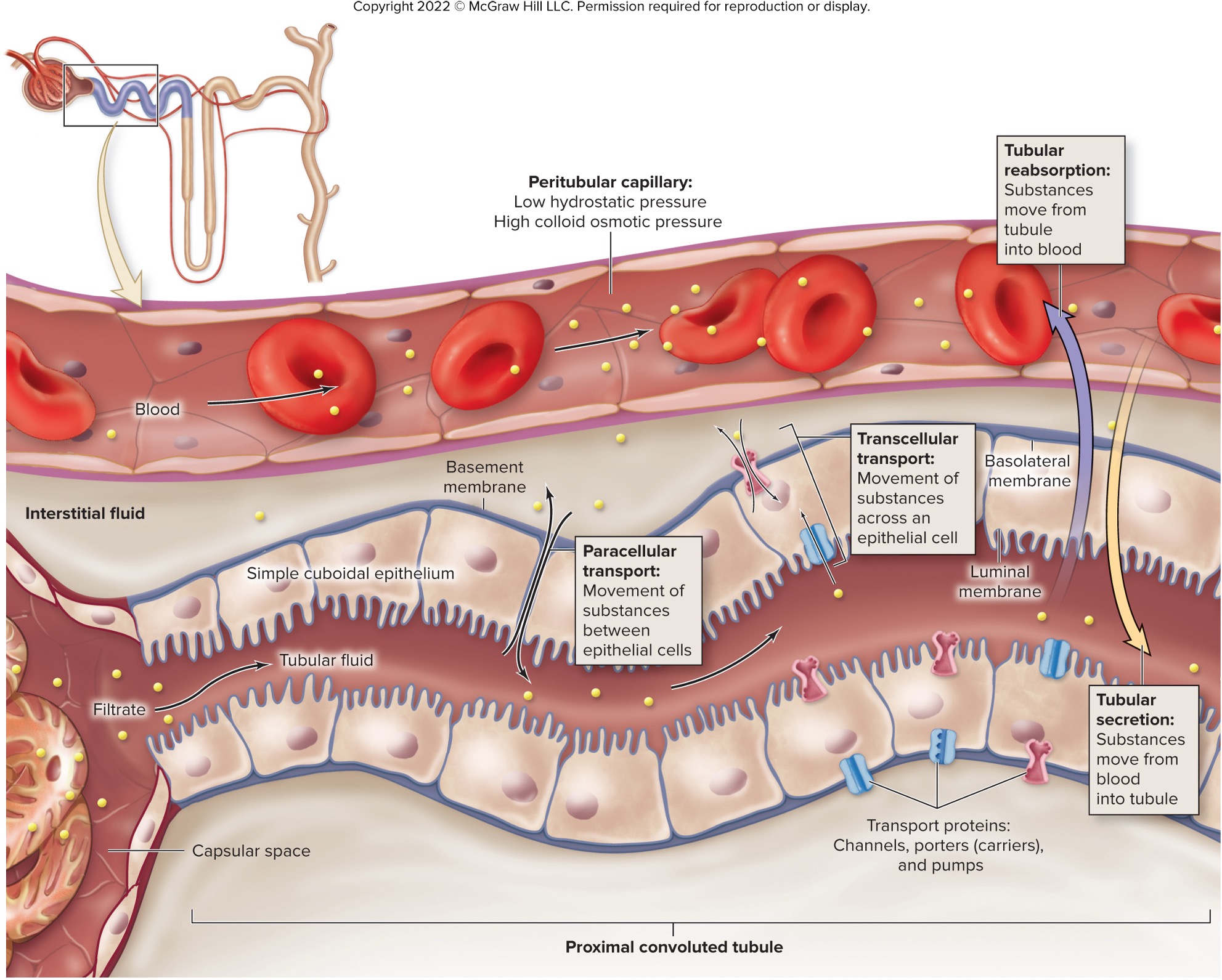
how does transport differ for reabsorption vs. secretion?
Reabsorption:
Luminal → Basolateral (filtrate → blood)
Example: Glucose, Na⁺ in PCTSecretion:
Basolateral → Luminal (blood → filtrate)
Example: K⁺, H⁺ in DCT
transport maximum (Tm) (what it is and what factors control it)
maximum rate of substances that can be reabsorbed (or secreted) across tubule epithelium per a certain time
depend on the number of transport proteins in the membrane
→ if no more than 375 mg/min, glucose in tubule all reabsorbed
→ if greater than 375 mg/min, excess glucose excreted in urine
renal threshold
max plasma concentration of a substance that can be transported in the blood without appearing in the urine
if Tm is exceeded, substance excreted in urine
how are nutrients typically handled by the kidney?
100% reabsorbed in healthy individuals (PCT)
Each nutrient has specific transport proteins
Occurs primarily via secondary active transport
how is glucose transported into tubule cells?
Via Na+/glucose symporter proteins
Energy from Na+ moving down its gradient
Moves glucose up its gradient into tubule
Secondary active transport
how does glucose exit tubule cells?
moved by uniporters across basolateral membrane
returned to blood in peritubular capillaries