The Cardiovascular System
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
Describe the location of the heart using anatomical terms.
2/3 of the heart is on the left side of the body between the lungs in the thorax, anterior to the vertebral column and posterior to the sternum.
What is the apex of the heart?
The pointed tip that points downwards and left.
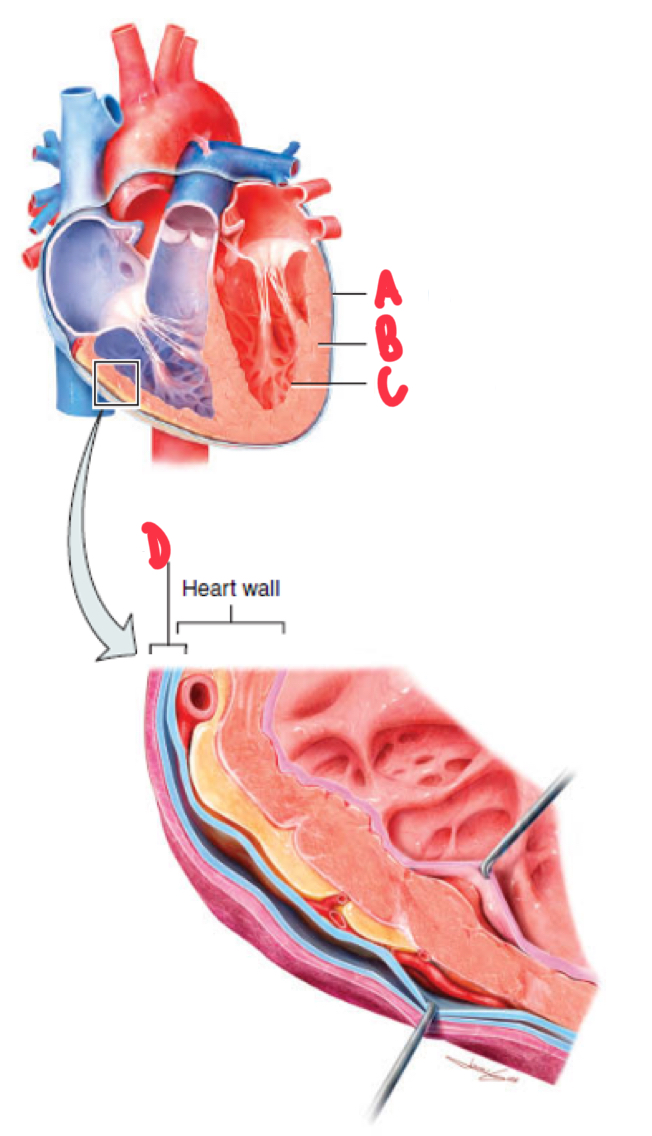
Name and describe the layers of the heart.
A - epicardium, external layer of the wall of the heart
B - myocardium, middle layer, primarily cardiac muscle that makes up majority of the wall of the heart
C - endocardium, innermost layer of the wall of the heart (thin layer of squamous epithelium and connective tissue)
D - pericardium, double-walled sac that surrounds the wall of the heart and contains pericardial fluid.
Describe the path of the blood circulation.
Systemic circulation, inferior and superior vena cavae, right atrium, tricuspid valve, right ventricle, pulmonary valve, pulmonary arteries, lungs, pulmonary veins, left atrium, bicuspid/mitral valve, left ventricle, aortic valve, aorta and systemic circulation.
How is blood supplied to the heart itself?
Through the coronary circulation which is seperate to the systemic and pulmonary circulations.
Describe the differences between the thickness of the walls of the chambers of the heart.
Atria have much thinner walls than the ventricles as they only need enough force to push blood into the ventricles
The left ventricle wall is much thicker than the right ventricle wall as it supplies the systemic circulation that covers greater distance than the pulmonary circulation
What are the 2 sets of valves in the heart?
Atrioventricular - tricuspid and bicuspid/mitral valves which are between atria and ventricles
Semilunar valves - pulmonary and aortic valves which are between the ventricles and greater arteries.
Describe the structure of atrioventricular valves.
Made up of flexible cups that are connected to connective tissue, chordae tendonae and then papillary muscles within the ventricular walls. Tricuspid had 3 cups and bicuspid/mitral has 2 cups.
Describe what occurs to atrioventricular valves when the ventricles are relaxed and when they contract.
when the ventricles are relaxed, the cups hang downwards into the ventricles and the valves are open, allowing for blood flow
When the ventricles contract, intraventricular pressure pushes the cups upwards and the valves are closed, preventing back flow of blood back into the atria.
Describe what occurs to semilunar valves when the ventricles are relaxed and when they contract.
When ventricles contract, intraventricular pressure pushes blood up against the semilunar valves, forcing them to open and allowing for blood flow into the arteries
When ventricles relax, blood in the arteries flows back, forcing semilunar valves to close to prevent backflow into the ventricles.
Describe the cardiac cycle.
The complete sequence of relaxation and contraction in a singular heartbeat.
What are the 2 parts that make up a single heartbeat.
Systole - contraction
Diastole - relaxation
Name and describe 2 features of cardiac myocytes.
Intercalated discs - the points where the plasma membranes of adjacent cardiac myocytes join, containing desmosomes and gap junctions
Mitochondria - dense as they rely on aerobic energy
Name and describe the 2 types of cardiac myocytes.
Contractile Myocytes - 99% of myocytes that generate force and are responsible for contraction
Autorhythmic/Pacemaker Cells - 1% of mycoytes which are non-contractile and have an unstable RMP, resulting in their spontaneous firing of action potentials.
Describe the process of pacemaker cells generating action potentials.
Pacemaker potential in which the unstable RMP potential and slow entry of sodium ions results in spontaneous depolarisation
Once membrane potential reaches threshold (-40mV), calcium ion channels open and calcium ions rush into the cell causing rapid depolarisation
Calcium ion channels close and potassium ion channels open in which potassium ions rush out of the cell causing rapid repolarisation
Describe the cardiac conduction cycle.
The process of specialised cells generating and spreading electrical activity throughout the heart.
Explain the process of the cardiac conduction cycle.
Spontaneous depolarisation of pacemaker cells within the sinoatrial (SA) node in the right atrium
Depolarisation spreads to the atrioventricular node with a delay to allow the atria to contract before the ventricles
Depolarisation then spreads to the septum via the AV bundles and bundle branches, left to left ventricle and right to right ventricle
Depolarisation spreads to ventricles via Purkinje fibres and gap junctions
Explain the different waves of an ECG
P Wave - atrial depolarisation from the SA nose that results in atrial contractions
QRS Complex - ventricular depolarisation
Q wave is a small negative deflection
R wave is a large positive deflection
S wave is a large negative deflection
T Wave - ventricular repolarisation
Why does an ECG not show atrial repolarisation?
Because atria are smaller and produce smaller amount of electrical activity than the ventricles in which atrial repolarisation is masked by the QRS complex.
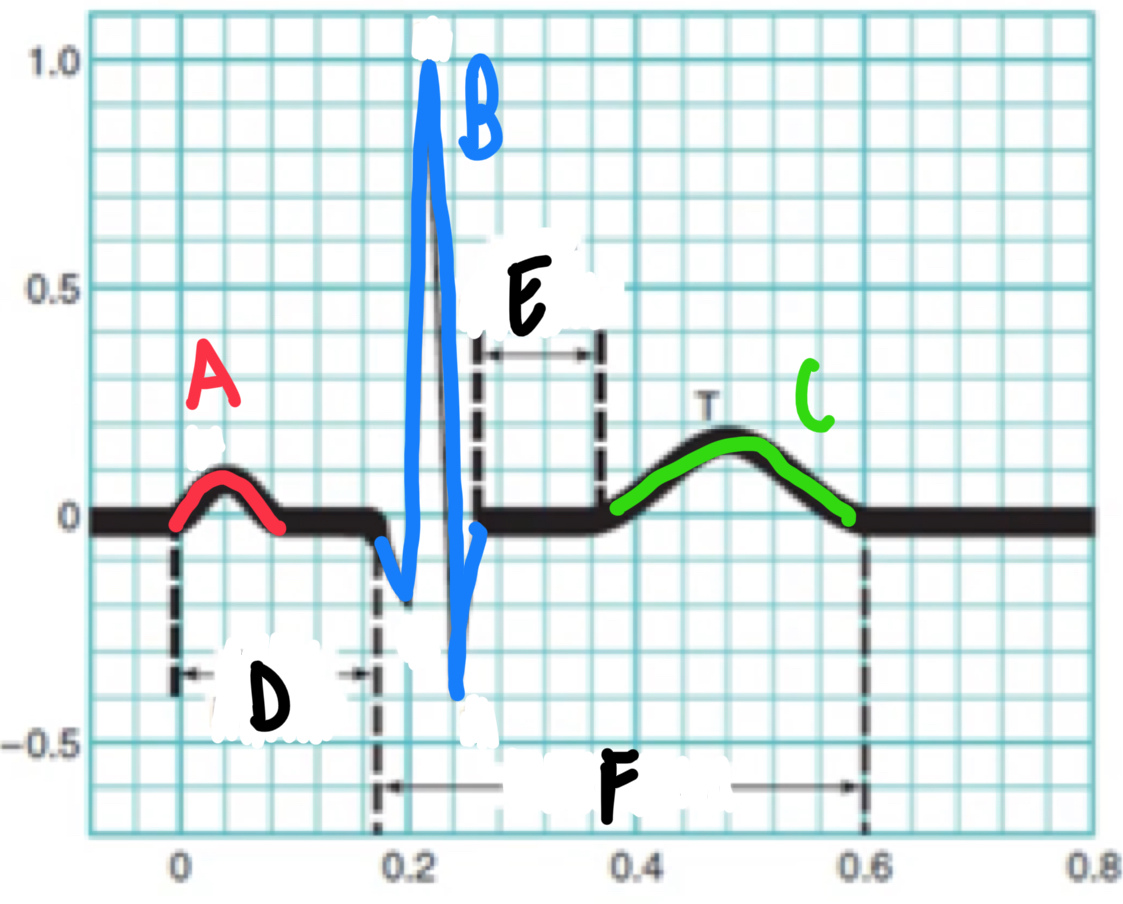
Identify the different parts of an ECG in this diagram.
A - P wave
B - QRS complex
C - T wave
D - P-Q interval
E - S-T segment
F - Q-T interval
Name and describe the phases of the cardiac cycle
Atrioventricular Diastole - atria and ventricles are relaxed, AV valves are open ventricles fill with blood
Atrial Systole - SA node depolarisation to atria which contract and push all blood into the ventricles
Isovolumetric Contraction - depolarisation spreads down into ventricles which contract, AV valves close however pressure is not great enough to open semilunar valves
Ventricular Ejection - ventricles continue to contract, pressure increases and semilunar valves open, ejecting blood into the great arteries.
Isovulumic Ventricular Relaxation - ventricles repolarise and pressure drops, closing semilunar valves and opening AV valves.
What is auscultation and how does it work?
Auscultation involves using a stethoscope to listen to the heart in which the sounds are associated with the tuberlance of the blood when the valves close.
What are the 2 phases of auscultation?
S1 - AV valves close, louder and longer sound (lubb)
S2 - SL valves close, quieter and shorter sound (dup)
Describe cardiac output.
The volume of blood ejected out of the left ventricle per minute, measured in L/min.
What is the average cardiac output in adults?
5L/min and typical blood volume is 5L, therefore entire blood volume passes through circulation each minute.
Name and describe the determinants of cardiac output.
Stroke volume - the volume of blood pumped out of the left ventricle per beat in mL
Heartrate - the number of heart contractions per minute, measured in BPM.
Name and describe 2 conditions of abnormal heartrate.
Tachycardia - abnormally fast resting HR
Brachycardia - abnormally low resting HR
Describe how sympathetic NS dominance increases cardiac output through heartrate.
Noradrenaline is released from sympathetic neurons as well as adrenaline from adrenal glands
This activates adrenergic receptors in the SA node
This causes Na+ and Ca2+ channels to open and ions rush into the cell
This increases rate of depolarisation, therefore heartrate and therefore cardiac output.
Describe how parasympathetic NS dominance decreases cardiac output through heartrate.
Acetylcholine is released from parasympathetic neurons
This activated cholinergic receptors in SA node
This causes K+ channels to open and ions leave the cell
This decreases the rate of depolarisation and therefore heartrate and cardiac output.
How is stroke volume measured?
The difference between end diastolic volume (volume of blood in ventricles before contraction) and end systolic volume (volume of blood in ventricle after contraction).
Explain Frank Starling Law of the Heart
States that an increase in venous return increases EDV and therefore SV as the length-force relationship of cardiac muscle allows for a greater force of contraction when there is a greater stretch on the cardiac muscle.
Explain 2 ways that stroke volume can be increased through venous pressure.
Skeletal and respiratory muscle pump compress adjacent veins, increasing venous pressure, therefore venous return, EDV and stroke volume.
SNS activation causes vasoconstriction that increases venous pressure, therefore venous return, EDV and stroke volume.
Explain how stroke volume can be increased through increased diastole time.
Increasing diastole time increases the amount of time for blood to fill the ventricles, increasing EDV and therefore stroke volume.
Describe contractility of the heart.
The amount of force generated by the heart at a given muscle length.
Explain how SNS activation increases stroke volume.
SNS releases positive inotropes such as adrenaline and noradrenaline which increases heart contractility, decreasing ESV and therefore increasing SV.
Name and describe the 5 types of blood vessels.
Arteries - large vessels that carry blood away from the heart
Arterioles - small vessels that branch of arteries and carry blood to tissues
Capillaries - smallest vessels that branch off arterioles and allow for the exchange of substances between blood and tissues
Venues - small vessels that merge and receive blood from capillaries, carrying blood away from tissues
Veins - large vessels that return blood to the heart.
Name and describe the 3 layers of blood vessels
Tunica Interna/Intima - innermost layer in direct contact with the blood that is made of simple squamous endothelium and connective tissue
Tunica Media - middle layer that contains elastic fibres and smooth muscle
Tunica External/Adventitia - outermost layer that contains elastic fibres and connective tissue
Describe lumen
The space within a blood vessel in which blood travels through
Compare the blood vessels of arteries and veins.
Arteries have a much thicker layer of smooth muscle (tunica media) than veins.
Veins have thinner walls that are highly distensible (stretchy) and larger lumen that allows large amount of blood flow with little resistance, acting as volume reservoirs.
Name and describe the 2 types of arteries.
Elastic - large, thick-walled arteries that are located close to the heart and contain large amounts of elastin, allowing them to act like pressure reservoirs.
Muscular - located distal to elastic arteries and distribute blood to tissues and organs.
Why do elastic arteries have thick walls and lots of elastin?
The thick walls and elastin allow them to withstand high pressures and expand during ventricular contractions to store pressure in walls and then recoil during ventricular relaxation to maintain pressure and constant blood flow.
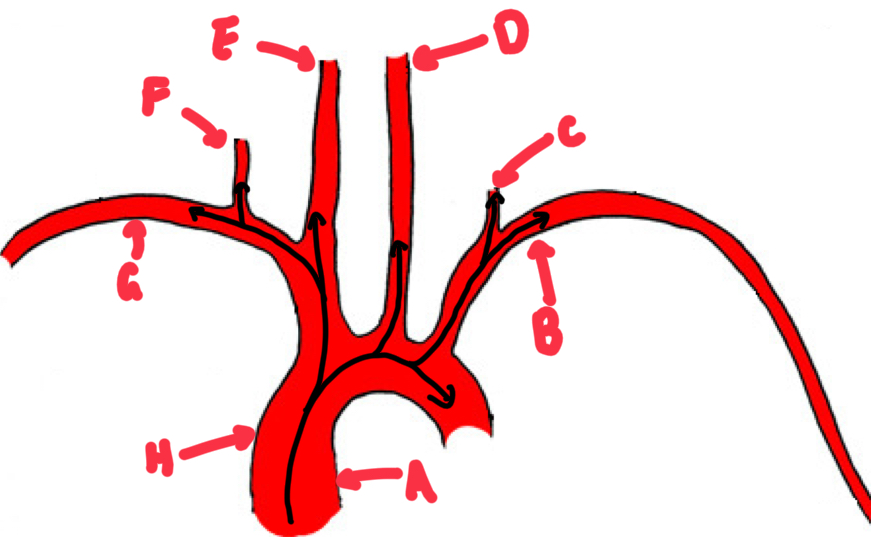
Name these major arteries from the heart.
A - aorta
B - left subclavian artery
C - left vertebral artery
D - left common carotid artery
E - right common carotid artery
F - right vertebral artery
G - right subclavian artery
H - brachiocephalic trunk
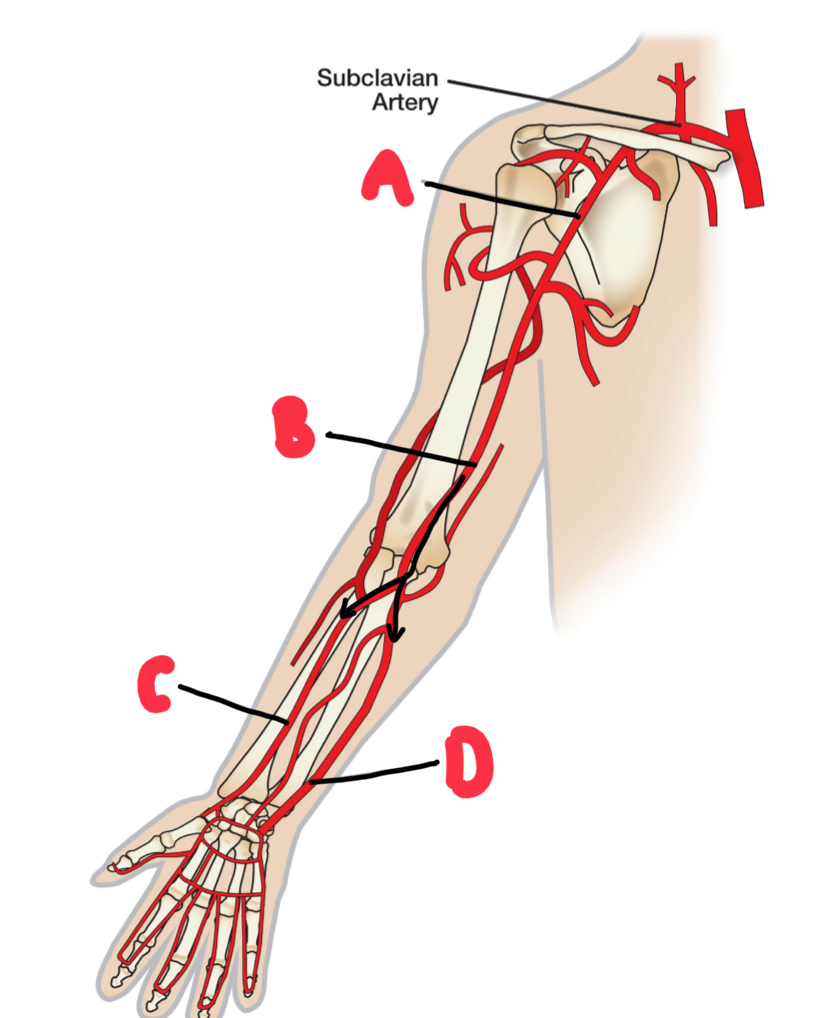
Name these major arteries of the arm.
A - right axillary artery
B - right brachial artery
C - right radial artery
D - right ulna artery
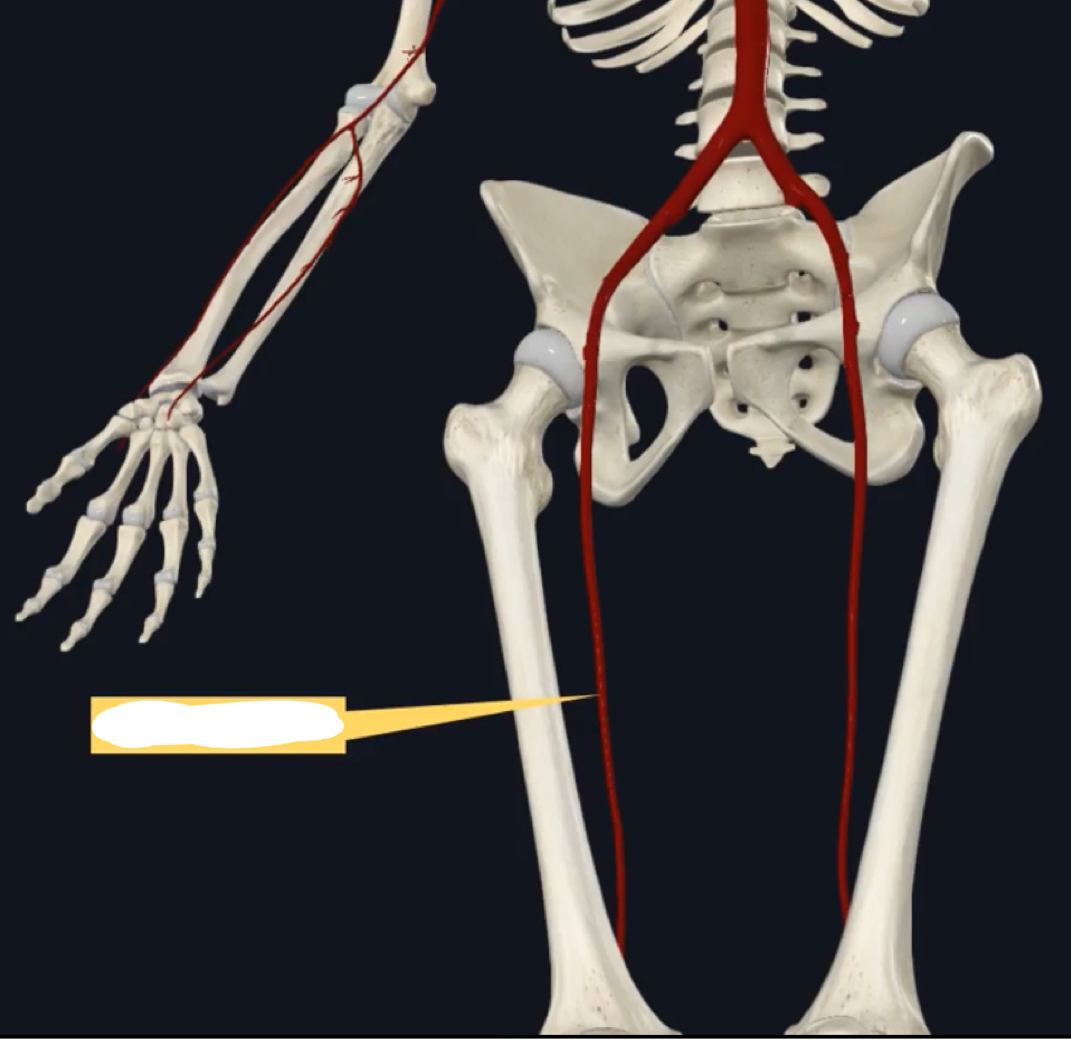
Name this artery of the lower body.
Right femoral artery
Describe blood flow.
The volume of blood that flows through a region each minute, measured in mL/min.
Describe local regulation of blood flow.
The process of arterioles regulating blood flow to tissues, ensuring they meet the needs of that tissue.
Explain how the SNS decreases blood flow.
Sympathetic neurons release noradrenaline that binds to adrenergic receptors in blood vessel walls, causing vasoconstriction that increases resistance and therefore decreases blood flow.
Describe basal tone in arterioles.
Basal tone is the partial contraction in arterioles, in between full contraction and full relaxation that allows for vasoconstriction and vasodilation.
Describe active hyperemia.
Active hyperemia is increased blood flow to tissues undergoing high amounts of metabolic activity. This is due to the production of local mediators that cause the vasodilation of arterioles
Explain why capillary beds allow for efficient exchange of substances.
Capillary walls are a single layer of endothelium and basement membrane and contain gaps between endothelial cells. Additionally, capillary beds have a high cross-sectional area and therefore slow velocity of blood flow, allowing longer time for substance exchange.
Describe interstitial fluid.
The fluid between capillaries and tissues.
Describe bulk flow.
The movement of fluid and small molecules between capillary beds and interstitial fluid.
Name and describe the 2 pressures that drive bulk flow.
Hydrostatic pressure - pressure generated by blood on the capillary walls that pushes fluid out of the capillaries and into the interstitial fluid. This decreases as blood moves through the capillary bed.
Osmotic pressure - pressure generated by plasma proteins in the blood that draw fluid back into the capillaries from the interstitial fluid to maintain fluid balance. This stays the same as blood moves through the capillary bed.
Explain bulk flow as blood moves through the capillary beds.
At the arteriole end, hydrostatic pressure > osmotic pressure, pushing fluid out of the capillaries and into the interstitial fluid.
At the venous end, osmotic pressure > hydrostatic pressure, drawing fluid back into the capillaries from the interstitial fluid.
However there us greater bet hydrostatic pressure and therefore more overall fluid being pushed out of the capillaries into the interstitial fluid.
Describe the role of the lymphatic system.
Lymphatic capillaries lie close to capillary beds and collect excess interstitial fluid from bulk flow. Now known as lymph, it is carried through lymphatic vessels that contain one-way valves to prevent back-flow, allowing lymph to reach lymphatic trunks that drain the fluid back into the venous circulation.
Describe oedema.
The build up of excess interstitial fluid due to lymphatic blockage.
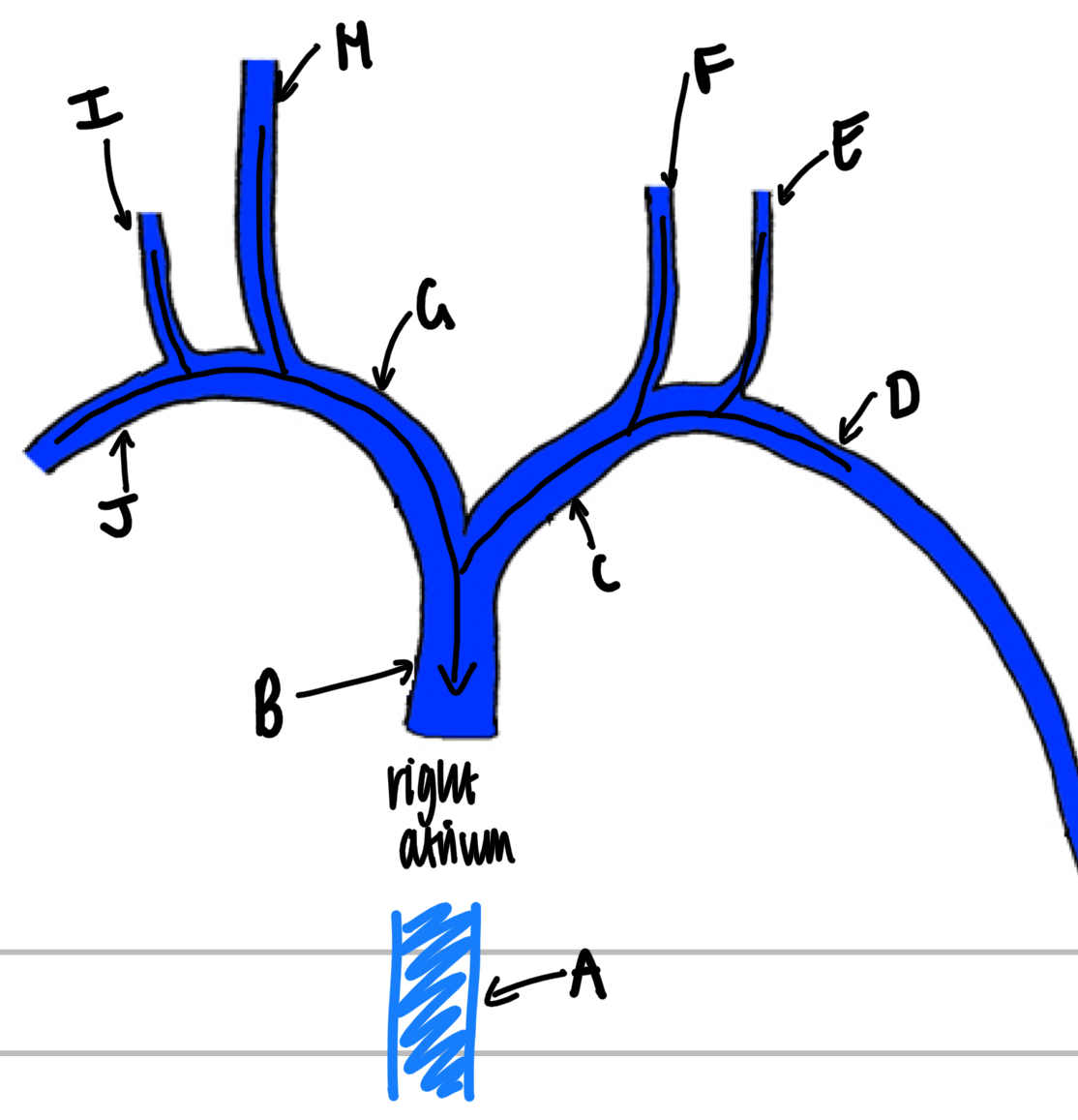
Name these veins from the heart.
A - inferior vena cava
B - superior vena cava
C - left brachiocephalic vein
D - left subclavian vein
E - left external jugular vein
F - left internal jugular vein
G - right brachiocephalic vein
H - right internal jugular vein
I - right external jugular vein
J - right subclavian vein
Describe blood pressure.
The amount of pressure that the blood exerts on vessel walls, measured in mmHg.
Describe arterial BP.
The amount of pressure that the blood exerts on vessel walls of systemic arteries located close to the heart.
Name and describe the 2 measurements of blood pressure.
Systolic BP - pressure exerted on vessel walls during systole (contraction)
Diastolic BP - pressure exerted on vessel walls during diastole (relaxation)
Describe BP formula.
Systolic BP/Diastolic BP
Describe pulse pressure.
The difference between systolic and diastolic BP.
Name 2 ways to measure BP.
Using an inflatable cuff, pressure gauge and stethoscope
Use an automated BP device
Describe the process of measuring BP with a stethoscope.
Place the cuff around the arm between the shoulder and elbow, measuring from the brachial artery.
Inflate the cuff above systolic BP (typically >120mmHg) to compress the artery so there is no blood flow or sound.
Once pressure drops between systolic and diastolic BP (typically between 80 and 120mmHg) use a stethoscope to hear the Korotkoff sounds of turbulent blood flow.
Once pressure drops below diastolic (typically 80mmHg), there is normal blood flow and no sound.
Describe mean arterial pressure and the formula.
The average BP in the systemic arteries, calculated by diastolic BP + pulse pressure/3.
Name the factors that affect MAP.
Cardiac output, therefore heartrate and stroke volume
Blood volume
Total peripheral resistance, therefore vessel length, blood viscosity and vessel diameter.
Describe how parasympathetic NS affects MAP.
Parasympathetic NS decreases heartrate through the release of acetylcholine to cholinergic receptors that increase K+ flow of the SA node, causing slower rate of depolarisation. Therefore decreased heartrate decreases cardiac output and therefore MAP.
Describe how sympathetic NS affects MAP through heartrate.
Sympathetic NS increases heartrate through release of noradrenaline to adrenergic receptors, increasing Na+ and Ca2+ flow into the SA node, increasing rate of depolarisation. Therefore increased heartrate increases cardiac output and therefore MAP.
Describe how sympathetic NS affects MAP through stroke volume.
Sympathetic NS increases heart contractility through adrenaline and noradrenaline (positive inotropes) release that decreases ESV, therefore increasing stroke volume, cardiac output and therefore MAP.
Describe the 2 ways that the sympathetic NS affects MAP through vasoconstriction.
Sympathetic NS activates vasoconstriction through release of noradrenaline to adrenergic receptors in blood vessel walls.
in veins this increases venous return, stroke volume, cardiac output and therefore MAP
In arterioles this increases total peripheral resistance and therefore MAP.
Describe the barocepter reflex.
The neural reflex pathway for the short term regulation of MAP through baroreceptors in the walls of the aorta and carotid arteries.
Describe the feedback loop of the baroceptor reflex.
Variable is stretch of the arterial walls.
Stimulus is the increase in stretch of the arterial walls due to increased MAP.
Receptors are the baroreceptors in the walls of the aorta and carotid arteries that fire action potentials to the control centre.
The control centre is the medulla that processes this input and determines if MAP is outside of its set point. If so, it fires outputs to effectors.
The effectors are the heart and blood vessels that receive output and carry out functions to decrease CO and TPR to return MAP to homeostasis.
Describe how baroreceptors detect increase in MAP.
Baroreceptors are tonically active when MAP is between systolic and diastolic BP. When MAP is above systolic BP, firing rate increases and when MAP is below diastolic BP, firing rate decreases.
Explain how long-term MAP is regulated by the kidneys.
increased salt and water excretion from the blood decreases blood volume and MAP
decreased salt and water excretion from the blood increases blood volume and MAP
Explain how hormone regulation maintains MAP homeostasis when there is a decrease.
Activation of the renin-angiotensin system that increases the production of angiotensin ll (Ang ll)
This triggers the release of aldosterone which increases salt retention (consequently increasing water retention)
This also triggers the release of anti-diuretic hormone (ADH) which increases water retention
This also triggers an increase in thirst which increases physical water uptake
Increase in water retention increases blood volume and therefore returns MAP to homeostasis
Name and describe the 3 overall functions of the heart.
Transportation
Oxygen from the lungs to the tissues
Carbon dioxide from the tissues to the lungs
Nutrients from the GI tract to the tissues
Metabolic waste from the tissues to the kidneys and liver
Hormones around the body from the endocrine system
Regulation
Body temperature
pH
Protection
Blood clot formation
Immune cells and proteins
Describe blood.
A type of fluid connective tissue in which the extracellular matrix is the plasma and the cellular component is the cells/formed elements within the plasma.
Describe plasma.
A pale, yellow fluid that is made up of 90% water as well as dissolved solutes, making up ~55% of the blood.
Describe the formed elements of the blood.
Make up 45% of the blood.
RBC/erythrocytes make up almost 100% of formed elements
White blood cells/leukocytes make up <1% of formed elements
Platelets make up <1% of formed elements and are not considered cells, instead cell fragments as they don’t contain a nucleus and cannot reproduce.
What do the layers of the blood look like when a sample is centrifuged?
dense layer of erythrocytes at the bottom (~45%)
Buffy coat/thin layer of leukocytes and platelets in between erythrocyte and plasma layers (<1%)
Less dense layer of plasma at the top (~55%)
Explain the structure of erythrocytes.
Small bioconcave disc-shaped cells that do not contain a nucleus or organelles to leave space for ~250 million haemoglobin molecules, giving them their red colour.
Describe haematopoiesis
The process of formed elements being developed from haematopoietic stem cells in red bone marrow.
Describe erythropoiesis
The formation of erythrocytes through a negative feedback loop controlled by erythropoietin (EPO).
Explain the process of erythropoiesis.
Hypoxia (decreased oxygen delivery) is detected.
Kidneys release erythropoietin
Erythropoietin stimulates stem cells within red bone marrow to divide into erythrocytes
Increased erythrocytes increases oxygen delivery
Describe haemostais.
Haemostasis is the process of stopping blood loss at a highly localised site of damage.
Name the 3 stages of haemostasis.
Vascular spasm
Platelet plug formation
Coagulation Cascade
Describe vascular spasm.
The initial response of vasoconstriction to reduce further blood loss.
Explain the process of platelet plug formation.
When endothelium is damaged, platelets activate as they are exposed to connective tissue and adhere to collagen fibers.
Activated platelets are enlarged and have a rough outer surface, aggregating together
Activated platelets release of chemical mediators that begin a positive feedback loop, activating nearby platelets to aggregate.
Undamaged endothelium on either side of the damage release different chemical mediators that inhibit aggregation to limit the platelet plug to the site of injury.
Describe clotting factors.
Soluble proteins present in plasma that are activated by the coagulation cascade.
Name and describe the phases of the coagulation cascade.
Initiation - formation of prothrombin activator
Extrinsic pathway is faster and activated by tissue factors which enters the damaged vessel from the outside
Intrinsic pathway is slower and activated by factors from within the blood
Thrombin formation - prothrombin activator converts prothrombin (inactive clotting factor) into thrombin (active enzyme)
Fibrin Formation - thrombin converts fibrinogen (inactive clotting factor) into fibrin (active insoluble protein), forming protein networks to stabilise the blood clot.
Describe fibrinolysis
The breakdown of fibrin for the removal of the blood clot once vessel wall has been repaired, preventing accumulation of blood clots and blockages of blood flow.
Explain the process of fibrinolysis.
Repaired endothelial cells release a plasminogen activator which converts plasminogen (inactive clotting factor within the blood clot) into plasmin (active enzyme).
Plasmin breaks down fibrin into fragments, destabilising and breaking down the clot.
How are blood types determined?
Blood types are determined by the presence or absence of antigens on the surface of erythrocytes.
Name the ABO blood groups and explain the antigens present on their erythrocytes and antibodies present in the plasma.
Type A - A antigens on erythrocytes and anti-B antibodies in plasma
Type B - B antigens on erythrocytes and anti-A antibodies in plasma
Type AB - Both A and B antigens on erythrocytes and no antibodies in plasma
Type O - no antigen on erythrocytes and both anti-A and anti-B antibodies in plasma
Name the Rh blood groups and explain the antigens present on their erythrocytes and antibodies present in the plasma.
Rh+ - RhD antigen present on erythrocytes and no antibodies present in plasma
Rh- - RhD antigen absent on erythrocytes and anti-RhD antibodies present in plasma
What occurs if an Rh- mother has an Rh+ baby?
If the mother is exposed to the Rh+ blood during delivery, her immune system will produce anti-RhD antibodies which could attack the erythrocytes of a second Rh+ developing foetus. Therefore Rh- mothers with an Rh+ baby are injected with Rho-GAM after delivery to prevent production of anti-RhD antibodies.
Describe blood typing
Determining the blood types of both donor and recipient for blood transfusions.
Explain ABO blood typing
Drops of blood samples are mixed with antisera solutions that contain either anti-A or anti-B antibodies.
Anti-A antisera will cause agglutination in erythrocytes with the A antigen present (in type A and AB)
Anti-B antisera will cause agglutination in erythrocytes with the B antigen present (in type B and AB)
Type O blood will show no agglutination with either antisera
Explain RhD blood typing.
Drops of blood samples are mixed with antisera solutions containing anti-RhD antibodies.
Erythrocytes with RhD antigen present will agglutinate (Rh+)
Erythrocytes with RhD antigen absent will not agglutinate (Rh-)