Fielding Chapter 13: Maintenance Fluid Therapy in Horses
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Maintenance Fluid Therapy
The provision of fluid and electrolytes necessary to maintain homeostasis of body water and electrolyte content on a daily basis
Characteristics of Maintenance Fluid Therapy
Maintenance fluids generally considered to be hypotonic, unless free water needs are met through drinking
Often contain a higher concentration of potassium than replacement fluids intended for the ECF as potassium is the primary intracellular cation
Provision of free water through hypotonic fluids allows for hydration of the intracellular space as well as the ECF in horses not allowed access to oral water
Because maintenance fluids distribute into all body fluid compartments, including the intracellular fluid space, they should not be administered as a bolus; rapid administration could predispose to development of tissue edema, with concerns over cerebral or pulmonary edema
Maintenance fluids may also contain dextrose which may be isotonic in vitro but effectively hypotonic as soon as dextrose is metabolized in vivo
Metabolism in Adults vs Foals
Metabolic rate is relatively high in the neonatal foal and decreases to become much lower in adult horses
Adult horses generate less heat and waste solutes from metabolism per unit body weight than fluids
Decreases the fluid and electrolyte requirements per unit of body weight as both heat dissipation and elimination of waste products require water
What % of adult body mass does water comprise?
61-71% (0.61-0.71 L/kg)
What does ECF volume consist of?
Plasma, interstitial, lymph, and transcellular fluids
What % of body mass is ECF?
21-31% (0.21-0.31 L/kg)
What % of total body water is extracellular water?
33-40%
What % of body weight is plasma?
5-6%
What % of body weight are interstitial and lymphatic fluids?
8-10%
What % of body weight is transcellular fluid?
6-8%
What does transcellular fluid consist of?
Primarily GI fluid (feces comprise 71-81% water) but also body cavity, CSF, joint, and aqueous fluids
What % of body weight is intracellular fluid?
40-46%
What fraction of total body water is intracellular fluid?
2/3
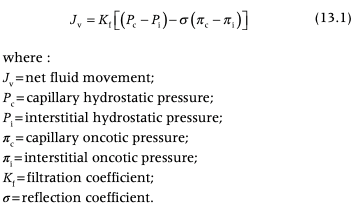
What governs movement of water between the subcompartments of the ECF?
Starling’s Forces
Starling Equation
What governs movement of water between the ECF and the ICF?
Osmotic forces
Water/Fluid Requirements in Normal Horses
2-3 ml/kg/h
Urine output in Normal Horses
0.4-2 ml/kg/h
Fecal Water Losses in Normal Horses
0.5-1.7 ml/kg/h
Insensible Losses in Horses
0.7-1.4 ml/kg/h
Metabolic Water Losses in Horses
0.26-0.28 ml/kg/h
What % of daily water loss do fecal losses account for?
30-55%
Fluid Requirements for Horses Off Feed
Fecal losses account for 30-55% of daily water loss so horses off feed and defecating minimally require less fluid intake than those that are eating and defecating regularly, 0.75-1/0 ml/kg/h have been suggested as being adequate
What causes urine production to vary?
Ambient temperature, feed intake, types of feeds fed, and access to salt
What can cause increases in insensible losses?
Hyperhidrosis or increased minute ventilation due to high ambient temperature or illness
What is metabolic water?
Water arising from metabolism by the organism
Maintenance Requirements of Electrolytes
Electrolyte requirements of horses are met through intake of feed under natural circumstances
Urinary and fecal excretion of sodium is low, respiratory losses of sodium are negligible because water is lost as water vapor, insensible evaporative loss from the skin is similar, sweat is high in sodium, chloride, and other electrolytes
Urinary and fecal elimination of potassium is substantially greater than sodium
In general, GI and transudative losses are sodium rich, whereas radiant losses are sodium free
Candidates for Maintenance Fluid Therapy
Horses that are unable to maintain adequate hydration through oral means
Horses with gastric or gastroduodenal reflux
Horses with severe dysphagia if long-term nasogastric intubation is not feasible
Horses with losses greater than their ability or willingness for water and electrolyte intake, especially if NGT is not possible or poorly tolerated due to ileus
Horse should meet two additional requirements to decide if they are ready for maintenance fluid therapy
Should not be suffering from shock, which would necessitate replacement fluid therapy
Should not be dehydrated
Assessment of Fluid Needs for Maintenance Fluids
Suggest using a rate of 2.5 ml/kg/h as a starting point
With ongoing losses, the component of the fluid rate required to account for diarrhea or reflux should be provided with replacement fluids rather than hypotonic fluids as the additional fluid losses occurring with diarrhea or reflux are from the ECF and are generally electrolyte rich, requiring isotonic fluid for replacement
Physical Examination for Monitoring During Maintenance Fluid Therapy
Physical examination signs of dehydration are fairly insensitive and may not manifest until late
Packed Cell Volume, Total Protein, and Electrolytes for Monitoring During Maintenance Fluid Therapy
PCV may not be a very sensitive indicator of hydration status
Total protein concentration is a reliable indicator of plasma volume decrease, provided pathologic protein loss or gain is not present
Hypernatremia or hyperosmolarity, when present, should signal free water loss
For maintenance fluid therapy purposes, a downward plateau of PCV and TP concentration is desired, without rapid or significant changes in magnitude
Osmolarity for Monitoring During Maintenance Fluid Therapy
Osmolarity, particularly when measured serially, is a good indicator of dehydration associated with water restriction
A serial drop in osmolarity after drinking water is consistent with rehydration, with plateau indicating that water repletion may be complete
Body Weight for Monitoring During Maintenance Fluid Therapy
Serial body weight measurement are useful for monitoring maintenance fluid therapy over time
Once the patient is rehydrated, body weight should not fluctuate in response to IV fluid therapy
How much urine should a horse receiving maintenance fluid therapy be producing?
At least 0.7-1 ml/kg/h
How often should horses receiving adequate maintenance fluid therapy be urinating?
At least every 3-4 hours
What USG would suggest that the maintenance fluid rate is inadequate? What USG may indicate that the fluid rates can be decreased?
In adult horses, highly concentrated urine such as that with a specific gravity exceeding 1.030 suggests that the provided fluids may be inadequate
Urine from an adult horse with a USG less than 1.010 may indicate that fluid rates can be decreased, as long as renal dysfunction is not at the root of the isosthenuria
CVP for Monitoring During Maintenance Fluid Therapy
A normal CVP does not necessarily signify an adequate blood volume, but a high normal CVP should be regarded as a limit to further fluid volume expansion for safety reasons, namely to prevent edema
During the maintenance phase of fluid therapy, maintenance of a normal CVP should be a goal
Normal CVP in Adult Horses
7.5-12 cmH2O
Using Lactate to Monitor During Maintenance Fluid Therapy
Blood or plasma lactate concentration should ideally not change abruptly during maintenance fluid therapy
Complications of Maintenance Fluid Therapy
Fluid overload, catheter-related problems, electrolyte disturbances
Determining the Type of Fluid for Maintenance Fluid Therapy
Hypotonic fluids are indicated in horses that are not drinking or are held off water for a period of time
In the short term (2-3 days, depending on the underlying disease process and renal function), and when animals can drink water, isotonic fluids can be used for maintenance purposes
Isotonic replacement crystalloids commonly used for maintenance fluid therapy in veterinary practice because most horses are able to excrete electrolytes that are administered in excess of needs and this is convenient, reduces the risk of hyponatremia, and often many clinically ill horses experience ongoing abnormal electrolyte losses and no to poor feed intake so they benefit from replacement fluids
If hypotonic fluids are used, sodium should be monitored serially to ensure lack of free water excess and hyponatremia
Prolonged use of replacement fluids may lead to hypernatremia, hyperosmolarity, and subsequent contraction of the ICF especially in neonatal foals, which may be less tolerant of administration of large amounts of sodium over time
Adult horses that aren't allowed to drink water and those with renal disease are also at risk for developing hypernatremia over time
Plasma-Lyte 56 or Normosol-M
Hypo-osmolar relative to the ECF
Sodium concentration is lower and potassium concentration is higher than replacement fluids
Contain magnesium rather than calcium
Acetate is the only alkalinizing salt
Sodium to chloride ratio is 1:1
Slight disadvantage for acidotic patients with hyperchloremia
0.45% sodium chloride/2.5% dextrose
Isotonic in the bag but is a maintenance fluid and provides a source of free water once the dextrose is metabolized in vivo
Sodium:chloride ratio is 1:1
Lacks potassium or other electrolytes as well as alkalinizing agents
Advantage is that it is ready to use without having to add dextrose
Ideal for maintenance of hydration in patients with hyperkalemia and in those that require an energy source
Potassium should be added for normo- and hypokalemic patients
5% Dextrose in Water
Neither a replacement nor a maintenance fluid as it contains no electrolytes
Source of free water and dextrose
Solution is near isotonic as commercially prepared but due to metabolism of dextrose in vivo it becomes hypotonic in vivo
Can be used as a means of delivering free water to animals with free water deficits (hypernatremia) or losses
Serum sodium should not be decreased at a rate faster than 0.5 mEq/h in horses with significant hypernatremia in order to avoid CNS edema
Never bolus as a rapid infusion because it can cause acute reductions in osmolarity and risks causing cerebral edema
“Home-made Maintenance Fluids”: Making Hypotonic Maintenance Fluids from Replacement Fluids
Can be accomplished through the administration of half the desired fluid rate as 5% dextrose in water and half the desired rate as a replacement fluid such as LRS or Plasma-Lyte A
If glucose is not desired, sterile water can be used
Discontinuation of Maintenance Fluid Therapy
Maintenance fluids should be discontinued gradually, in order to avoid transient dehydration until horses develop an osmolar or volume drive to drink
Fluid rates should be decreased gradually over 24 hours or longer in order to minimize the transition period or transient lack of drinking after IV fluid therapy
Goal is to gradually provide a drive to drink (either through osmolarity or blood volume/pressure stimulus) without allowing significant dehydration
Potassium Supplementation in Maintenance Fluids
Important in horses with partial to complete anorexia
Potassium is primarily intracellular so determining total body status is not conducive to hourly or daily management of fluid status
Measurement of urinary fractional excretion (FE) of potassium can add to an understanding of potassium dynamics
Anorexia predisposes to hypokalemia as do fluid diuresis and renal tubular acidosis
Fractional Excretion Formula
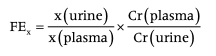
Reported Range of Fractional Excretion of Potassium
Reported range of FE of potassium is 15-80%
Highly diet dependent
Most horses are somewhere between 20 and 50%
Horses with renal dysfunction or magnesium deficiency may have altered or inaccurate FE of potassium
FE of potassium is lower in neonatal foals than adults with a range of 9-18%
What is the maximum safe rate of potassium administration?
0.5 mEq/kg/h
Potassium Additive Amounts
Most commonly, 20-40 mEq/L of potassium chloride (KCl) is added to crystalloid fluids during maintenance fluid therapy
Plasma potassium below 3.5 mEq/L warrants supplementation of fluids with a rate of 10-20 mEq/L
A potassium level below 3.2 mEq/L should be supplemented with 20 mEq/L
A potassium concentration below 3 mEq/L may indicate supplementation with 30-40 mEq/L
LRS contains 4 mEq/L of potassium and Plasmalyte A and Normosol-R have 5 mEq/L
Commercial maintenance fluids such as Plasma-Lyte 56 and Normosol M contain higher potassium concentration (13 mEq/L)
What may cause hypokalemia that is refractory to potassium supplementation?
Horses with hypokalemia that is refractory to potassium supplementation may have concurrent magnesium depletion
Magnesium is a cofactor for Na/K ATPases so hypomagnesemia leads to decreased intracellular potassium and increased intracellular sodium concentrations, leading to lowered resting membrane potential
Hypomagnesemia leads to loss of intracellular potassium stores and to reduced reabsorption of potassium in the kidney
Increased potential for spontaneous cardiac depolarization as well as increased Purkinje cell excitability and increased likelihood of dysrhythmia generation
Calcium Supplementation in Maintenance Fluids
Mild hypocalcium is common in horses that are partially to completely anorexic
Surgical colic or colitis, prolonged exercise with heavy sweating, endotoxemia, or small intestinal disease (especially of the duodenum where most calcium absorption occurs) often causes hypocalcemia in horses
Ionized calcium should be measured whenever possible because it is the active form in plasma
Calcium should be diluted in crystalloids and administered over 2-3 hours in order to avoid bradycardia or other cardiac dysrhythmias
Calcium Additive Amounts
Supplementation should certainly occur at values at or below 1.0 mmol/L (4.0 mg/dl) because of the associated potential for dysrhythmias when values below 0.9 are reached
Many clinicians supplement calcium when ionized calcium is below 1.2-1.3 mmol/L (4.8-5.2 mg/dL)
Adult horses would meet their resting calcium requirement with 0.94-1.26 ml/kg/day of 23% calcium gluconate
What can cause refractory hypocalcemia?
Horses with refractory hypocalcemia should have their plasma ionized magnesium concentrations evaluated
Magnesium is needed for parathyroid hormone (PTH) synthesis and secretion, as well as tissue responsiveness to PTH
Phosphorous Supplementation in Maintenance Fluids
Majority of phosphorous is intracellular
Generally phosphorous is not added to fluids unless significant hypophosphatemia is present
Can get hypophosphatemia with large colon resection because the sites of phosphorous absorption are in the large and small colon
Absorption efficiency of phosphorous in the equine gut appears to be approximately 40%
Phosphorous Additive Amounts
Daily phosphorous requirement is 27 mg/kg/day
Since absorption is approximately 40%, IV requirement is 0.35 mmol/kg/day
Maximum recommended rate is 0.24 mmol/kg/day unless marked hypophosphatemia is present as excessive phosphorous supplementation can cause hyperphosphatemia-associated ventricular dysrhythmias and precipitation with calcium
Magnesium Supplementation in Maintenance Fluids
May be low in horses with anorexia and GI diseases, especially those with strangulating lesions, endotoxemia, and ileus
Clinical signs of hypomagnesemia include ileus, ventricular dysrhythmias, muscle tremors, hyperhidrosis, seizures, and ataxia followed by collapse
Hypomagnesemia may increase intracellular calcium concentrations, potentially making the myocardium and other tissues more susceptible to cardiotoxicity from glycosides and other cardiotoxins as well as to consequences of ischemia
Most dietary magnesium is absorbed by the small intestine
Magnesium supplementation is indicated for refractory hypokalemia or hypocalcemia because magnesium is required for renal reabsorption of potassium and PTH release, respectively
Magnesium Additive Amounts
Daily dietary requirement is 13-15 mg/kg
With an estimated 40-50% absorption the IV dose would be 0.43-0.62 mEq/kg/day
Dextrose Supplementation to Maintenance Fluids
50% dextrose should not contact the endothelium and erythrocytes directly without dilution due to hyperosmolarity