Lecture #8 Pulmonary system: response to exercise
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Why do we breath?
primarily to get rid of CO2
also aerobic metabolism → break down food, get energy
What 2 things does out pulmonary system do?
ventilation
Respiration
Ventilation allows respiration to occur
What is ventilation?
Breathing
The process of inspiration and expiration
Mechanical movement of gases into and out of the lungs
Inspiration
active process
increased volume inside thoracic cavity
decreased pressure
air comes in
Expiration
usually a passive process
relaxation of inspiratory muscles
elastic recoil of lungs & surrounding tissues
decreased volume inside thoracic cavity
increased pressure
air goes out
Process of inspiration and expiration
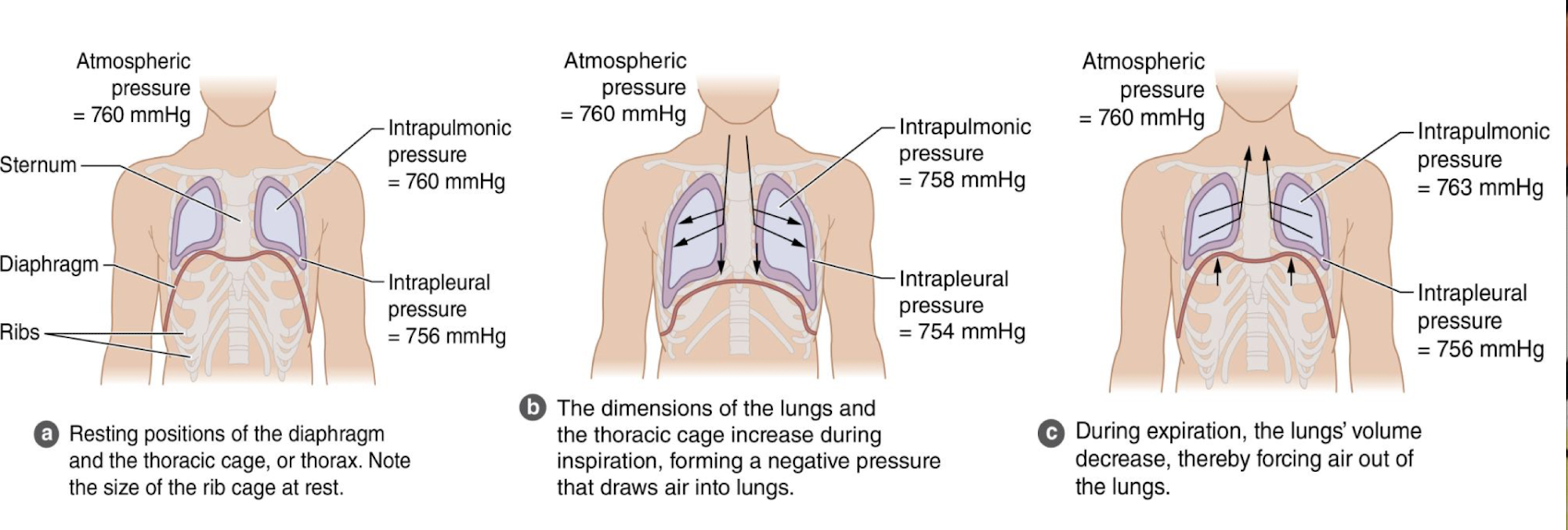
Boyle’s Law Equation
Muscles of Ventilation: Inspiration
Primary Muscles:
diaphragm
external intercostals
Accessory Muscles:
SCM
Scalenes
Upper trap
pec major & minor
serratus anterior & rhomboids
lats
serratus posterior superior
thoracic erector spinae
Muscles of Ventilation: expiration
Primary Muscles: there are none!
passive process in which there is relaxation of inspiratory muscles and elastic recoil of the lungs
Muscles of forced expiration:
abdominals
internal intercostals

Why do people do this?
Stabilizes the lats at the insertion so the origin can help with breathing
What moves first when you breath?
your abdomen
Usual Breath Sequence
1st: subtle rise of the upper abdomen
2nd: lateral costal expansion of the lower chest
3rd: subtle rise of the upper chest, mainly superior and anterior
Energy Cost of Breathing
healthy people: 11-15% of energy towards muscles of ventilation
COPD: 40% of energy used
What are the implications of COPD on functional mobility?
When energy is going to ventilatory muscles, it is NOT going to the limbs so…
fatigued
short of breath
don’t want to do much physical activity
get tired quicker
If the body has to chose between breathing or completing an action or activity, what will it chose?
breathing
What 3 important lung properties facilitate ventilation?
compliance: stiffness of lung tissue
Elastic recoil: ability to return to its initial size after being distended
surface tension: create a force that helps the lungs recoil during exhalation
What is pulmonary fibrous (fibrotic lungs)?
people have low compliance or low distensibility of lung tissue (can’t inflate)
work of breathing increases because of inability to increase lung volume
What is emphysema?
over time, alveoli become overstretching and lose their elastic recoil
air becomes trapped in lungs and people with emphysema have a hard time blowing air out
Babies and Infant Respiratory Distress Syndrome
premature babies who lack surfactant are at increased risk for infant IRDS
surfactant aides in decreasing surface tension in the alveoli
without surfactant, alveoli collapse
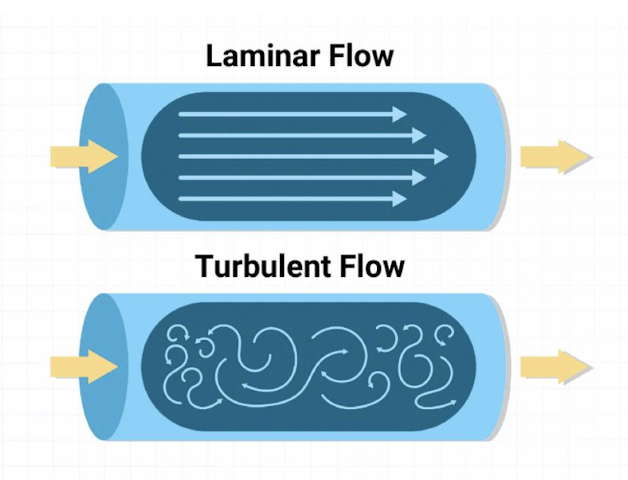
Airway Turbulence
collision of air molecules
upper airway is responsible for most of the airway resistance
Additional causes:
pathologies- asthma/bronchitis
bronchial constriction
mucus & edema
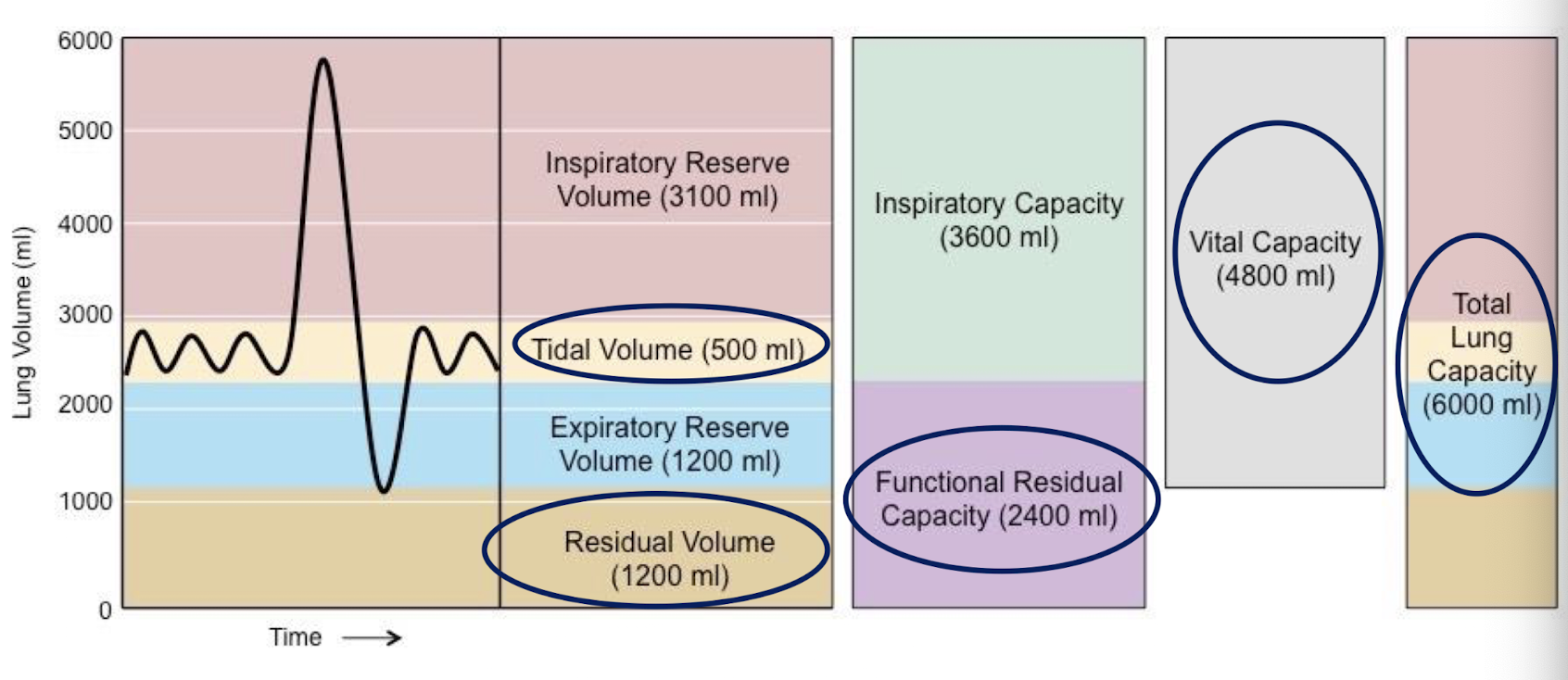
Tidal Volume (TV)
volume of air inspired and expired each normal breath
average: 0.4-1.0L per breath
Inspiratory Reserve Volume (IRV)
maximum inspiration at the end of a tidal inspiration
Avg: 2.5-3.5L
Expiratory Reserve Volume (ERV)
maximum expiration at the end of a tidal expiration
Avg: 2.5-3.5L
Vital Capacity
VC = TV+IRV+ERV
greatest amount of air that can be expired after a maximal inspiration
avg: male 4-5L, female 0.8-1.2L
Residual Lung Volume (RLV)
volume in lungs after max expiration
avg: male 0.9-1.4L, female 3-4L
Total Lung Capacity
TLC= VC+RLV
volume in lungs after maximal inspiration
Inspiratory Capacity (IC)
IC= TV+IRV
maximum volume inspired starting from a resting inspiratory position
Functional Residual Capacity (FRC)
FRC= RLV+ ERV
volume in lungs after tidal expiration
Lung Volume Chart
What is responsible for keeping your lungs from collapsing?
residual volume
Obstructive Lung Disease
difficulty exhaling all air from the lungs
poor elastic recoil of alveoli (emphysema)
chronic inflammation of airways (bronchitis)
narrowing of airways (asthma)
Restrictive Lung Disease
difficulty filling lungs with air due to inability to expand lungs
low distensibility or stiff lung tissue (pulmonary fibrosis)
postural restrictions limiting ability to expand (severe scoliosis or morbid obesity)
Forced Vital Capacity (FVC)
amount of air that can be forcefully exhaled as quickly as possible
Forced Expiratory Volume (FEV1)
Volume of air forcefully expired in the 1st second of FVC
Normal: FEV1 > 2.0 liters
Severe obstruction: FEV1 <1.0 liters
FEV1/FVC
80% or greater is considered normal
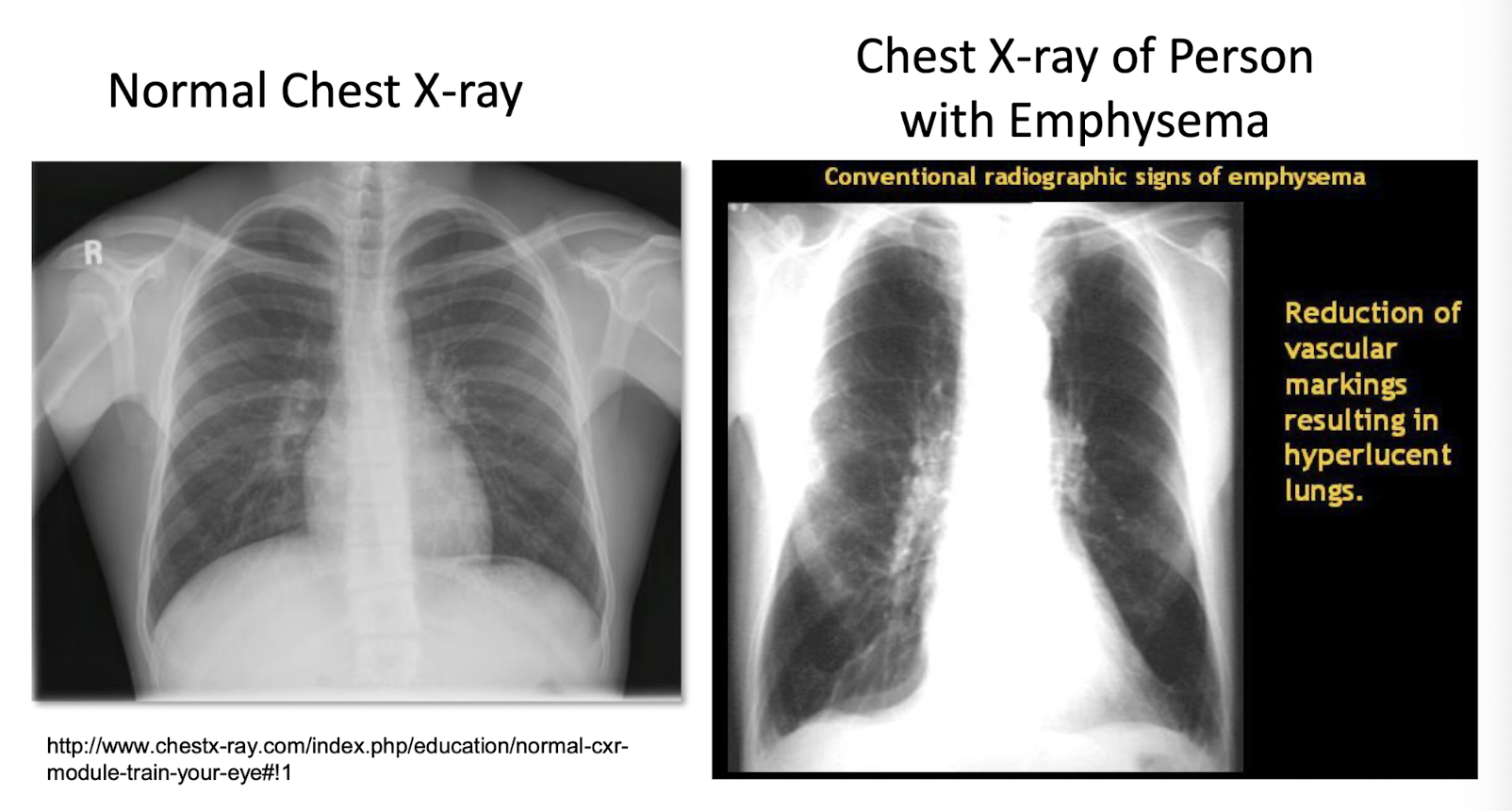
What would breathing be like?
hard
diaphragm is very low
lungs are narrow → not filling well
respiration
gas exchange through the process of simple diffusion
replenishment of oxygen for energy production and removal of CO2
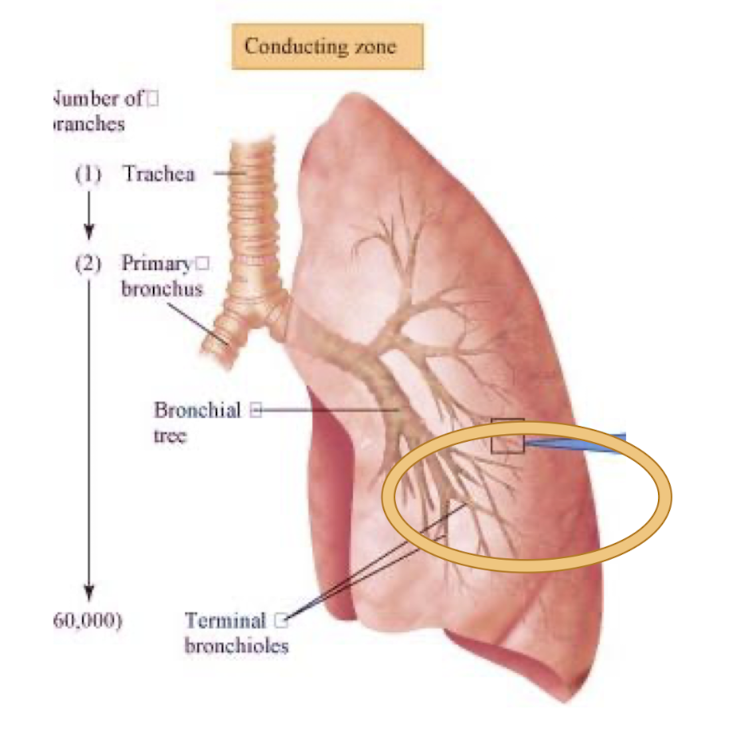
Conduction zone pulmonary anatomy
trachea
bronchiole tree
bronchioles
Respiratory Zone
bronchioles
alveolar ducts
alveolli
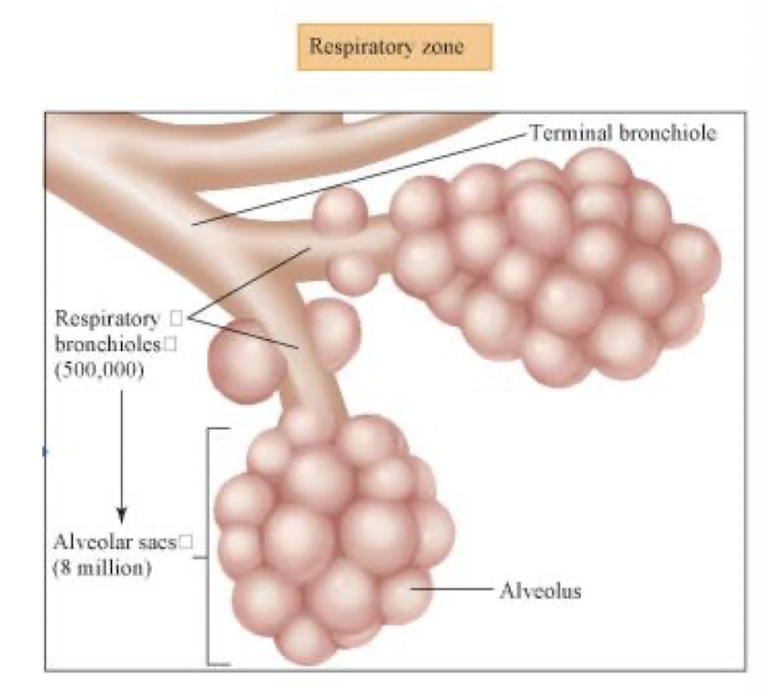
Pulmonary diffusion
The process by which gases are exchanged across the respiratory membrane in the alveoli
replenishes blood’s O2 supply that has been depleted for oxidative energy production
removes CO2 from returning venous blood
Pulmonary circulation picture
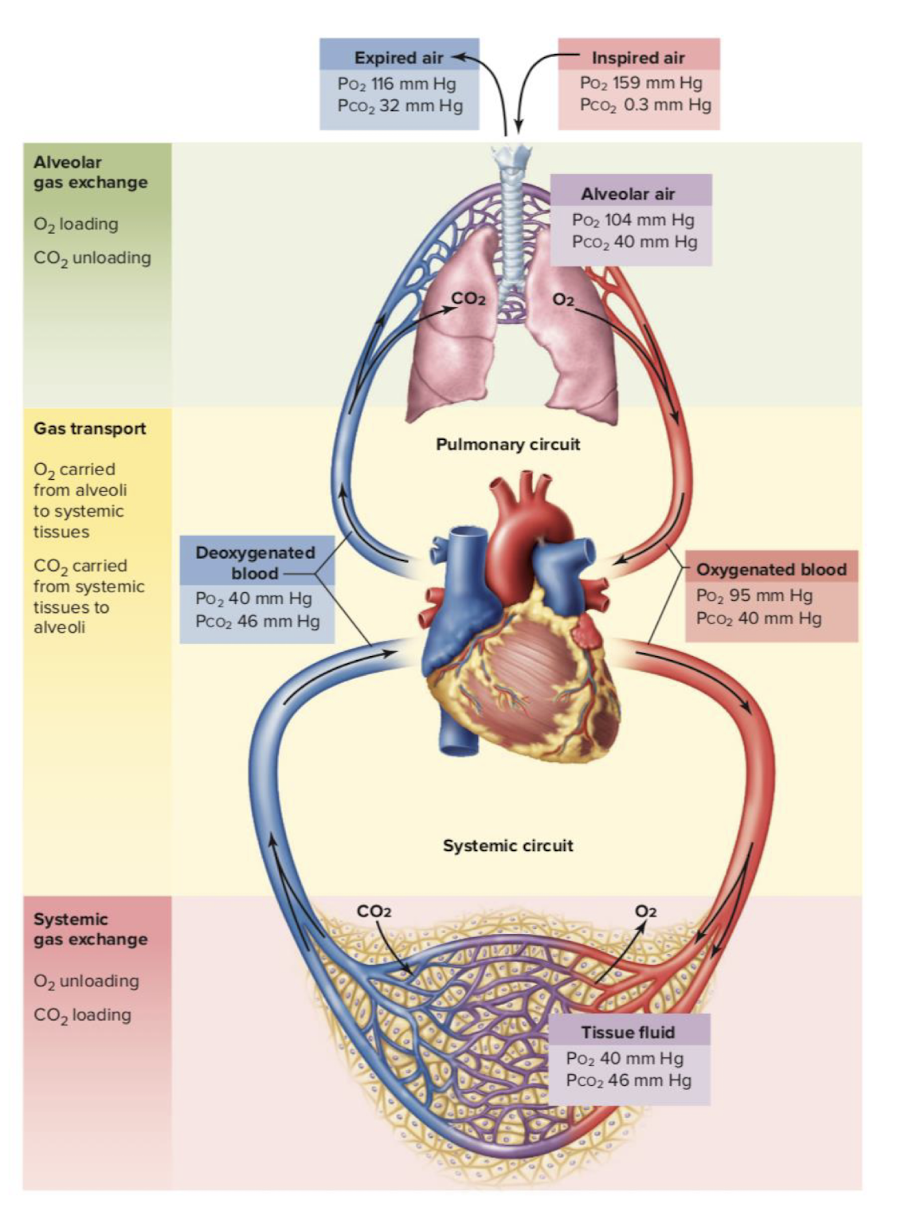
Pulmonary diffusion and exercise
oxygen diffuses from high pressure to low pressure
oxygen diffusion rate increases with exercise
when venous oxygen is depleted due to muscle uptake of oxygen, oxygen exchange at the alveoli is facilitated due to an increased pressure gradient
oxygen transport
bound to hemoglobin (>98%) or dissolved in plasma (<2%)
What determines the O2 carrying capacity of blood?
Hemoglobin
This is lower in people with anemia
Factors affecting oxygen uptake and delivery
oxygen content of blood
amount of blood flow
local conditions within the muscle
increased H+ acidity and temperature of a muscle favors oxygen unloading in the muscle
Central and peripheral regulators of ventilation
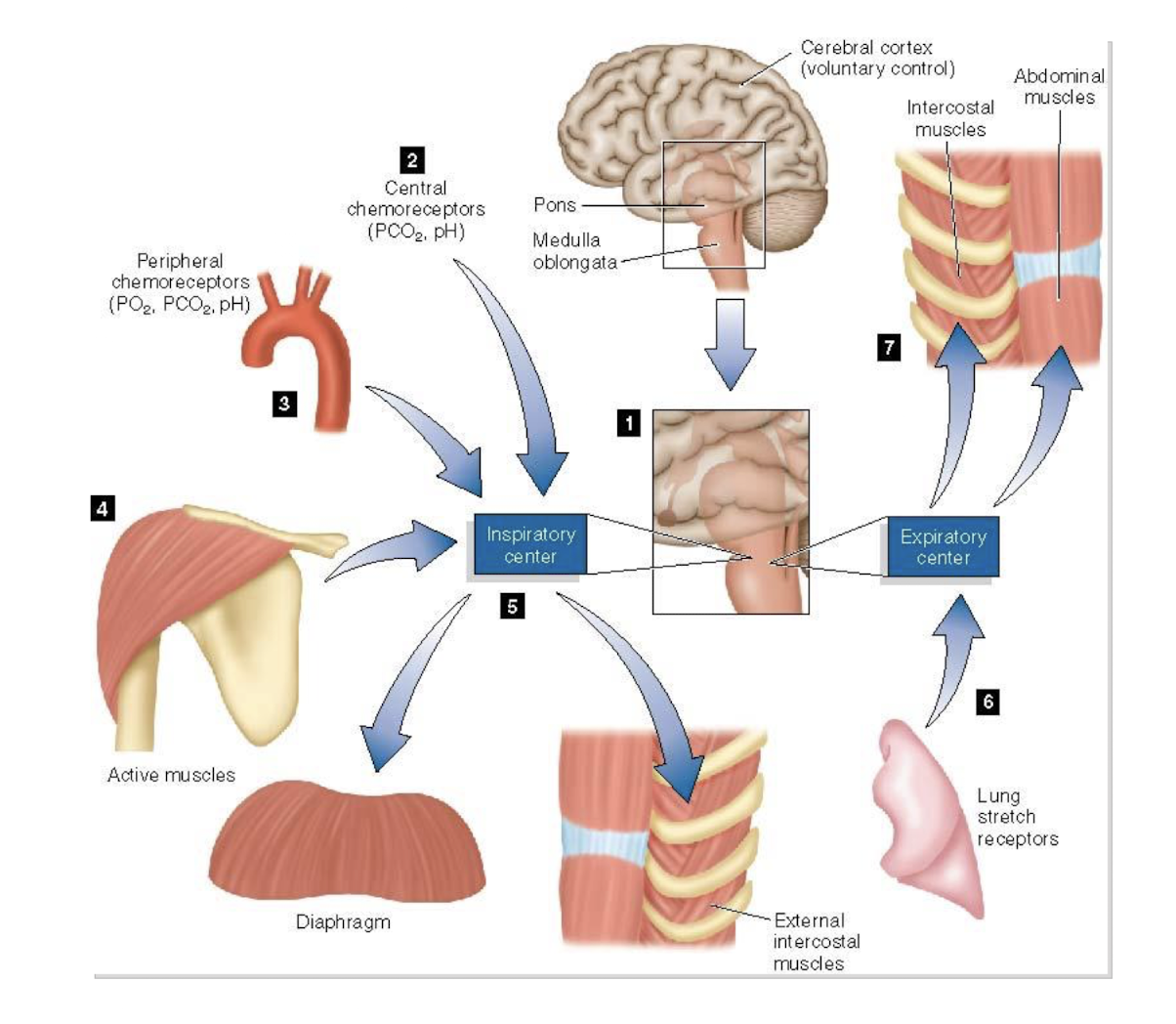
Chemoreceptors
senses changes in blood pH, CO2, O2
Hypothalamus and Limbic system function
pain and emotions
What is normal ventilation driven by?
Co2 levels in the arteries as detected by peripheral chemoreceptors
Hypercapnia
chronically high CO2 levels in the blood
people with severe COPD
O2 receptors become the primary means of regulating ventilation
What happens if you give someone with COPD O2?
Normal ventilation is normally driven by CO2 levels in the arteries as detected by peripheral chemoreceptors
People with severe COPD may have chronically high CO2 levels in the blood – hypercapnia
In people with hypercapnia, O2 receptors become the primary means of regulating ventilation
increased O2 → decreased hypoxic drive → decreased drive to breath (ventilation) = increased risk of respiratory failure
what are the 3 Lung Receptors?
irritant
stretch
J receptor
Irritant receptor
initiates cough reflex, bronchial constriction, and increased respirator rate
Stretch receptor
protects the lung from excessive inflation during exercise
J receptor
senses pulmonary capillary pressures and congestion
this initiates rapid, shallow breathing, and produces the cough reflex with fluid accumulation during pulmonary edema and pleural effusion
Joint and muscle receptors
change in movement at the joints of the extremities → increased ventilation
during exercise, there is an initial abrupt increase in ventilation due to signals from the joint and muscle receptors
What are 4 things that happen for pulmonary ventilation during dynamic exercise?
neurally-mediated increase in ventilation
increased metabolism generates CO2 and H+
stimulate chemoreceptors
Stimulated receptors increase in ventilation
Pulmonary ventilation returns to normal at a slower rate when exercise ceases
Ventilatory response graph
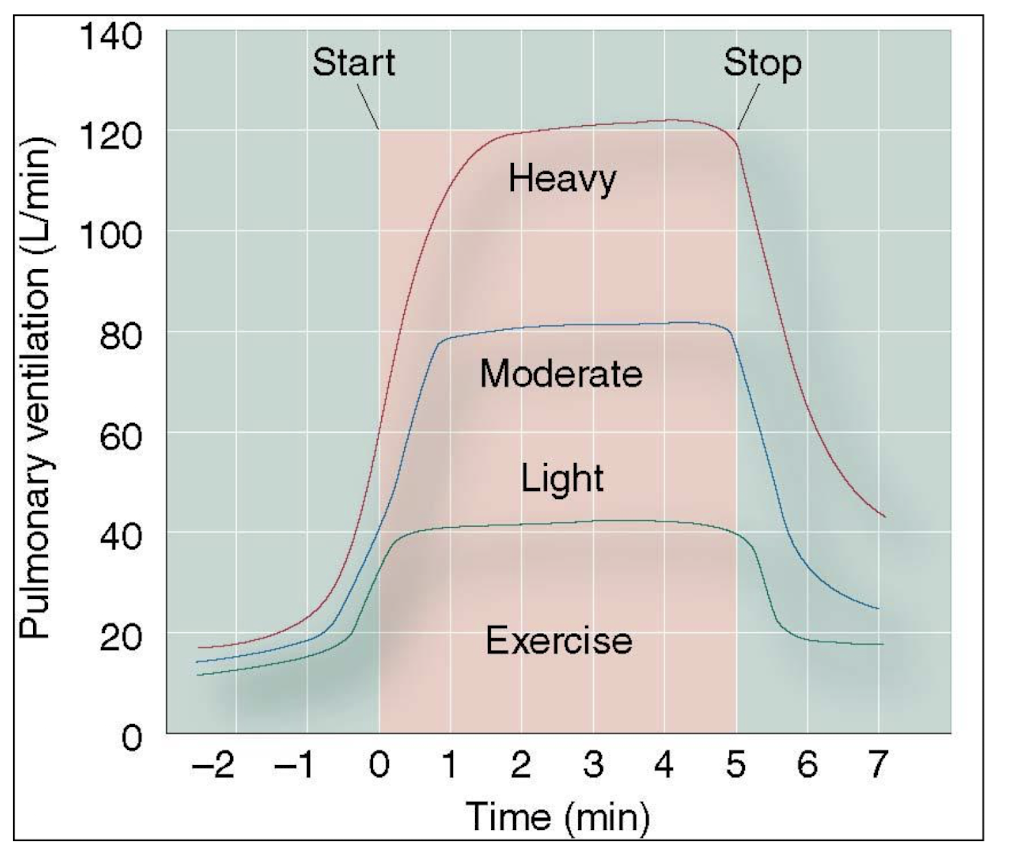
Ventilatory threshold
point when ventilation increases disproportionately to oxygen consumption
occurs at approximately the same point lactate begins to accumulate in the blood
lactic acid is buffered by sodium bicarbonate
ventilation increases due to increased CO2 stimulation the chemoreceptor
What are 3 breathing irregularities during exercise?
dyspnea
hyperventilation
valsalva maneuver
Dyspnea (DOE)
exertional breathlessness caused by inability to readjust the blood PCO2 and H+
Hyperventilation
an increase in ventilation that exceeds the metabolic need for oxygen
Valsalva maneuver
a breathing technique where air is trapped in the lungs against a closed glottis, and intra-abdominal and intrathoracic pressure are increased
Respiratory Regulation of Acid-Base Balance
Excess H+ (decreased pH) impairs muscle contractility and ATP generation
increased H+ concentrations stimulate respiratory centers to remove CO2
whenever H+ levels begin to rise, bicarbonate ions can buffer the H+ to prevent acidosis
this increased CO2 to be removed through ventilation
Arterial blood gases
Normal:
pH: 7.35-7.45
must buffer hydrogen ions to maintain this
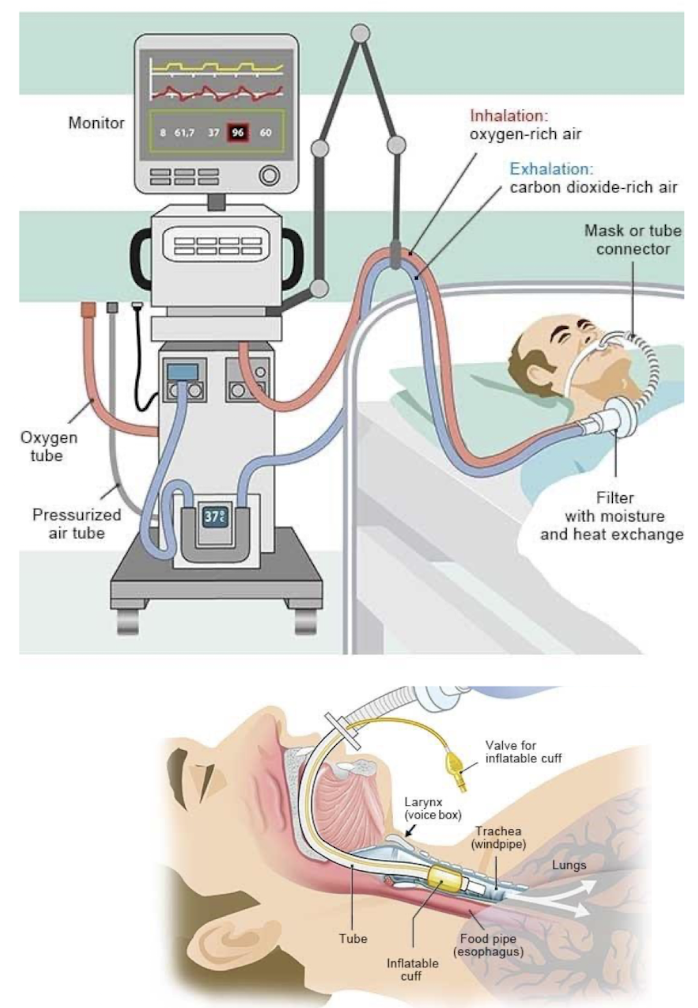
What happens when a person fails to maintain acid-base balance?
they go on ventilatory system to get CO2 out or keep airways open
What are the benefits of mechanical ventilation?
decreased work of breathing (muscles rest), helps get oxygen into the body and CO2 out
What are the risks of mechanical ventilation?
Barotrauma, infection, difficulty weaning
Non-invasive positive- pressure ventilation CPAP and BiPAP

Invasive mechanical ventilation