HO35_Ocular Allergies_Ocular vs Systemic Steroids
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
There are multiple medication classes used for ocular allergies/DED:
Ocular Steroids vs Systemic Steroids
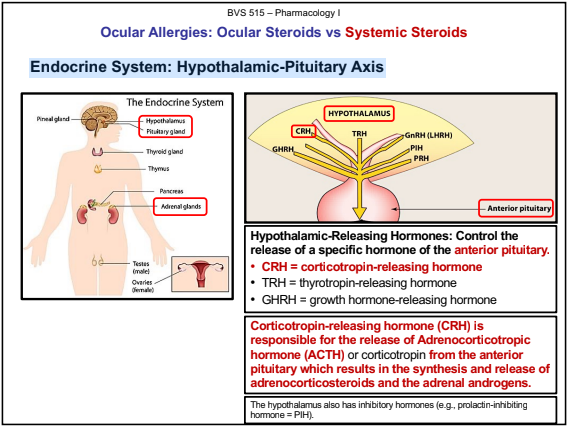
Endocrine System: Hypothalamic-Pituitary Axis
The Hypothalamic-Pituitary-Adrenal Axis (HPA) the main stress response system involving the hypothalamus, pituitary gland, and adrenal gland.
The primary function of the HPA is to release glucocorticoids (cortisol) in response to stress.
Hypothalamus: sending signals to the pituitary gland to release hormones.
Pituitary:produces hormones, adrenal glands,
Endocrine System: Hypothalamic-Pituitary Axis
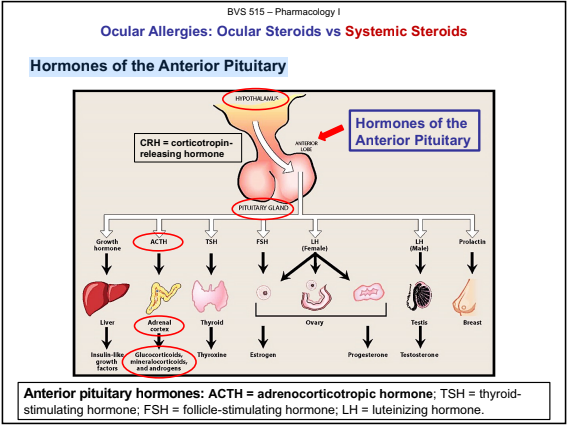
Hormones of the Anterior Pituitary
The anterior lobe of the pituitary produces and releases (secretes)
Adrenocorticotropic hormone (ACTH/Corticotropin): Stimulates the adrenal glands to produce cortisol (adrenal hormones).
Growth Hormone (GH): muscle formation
Thyroid-stimulating hormone (TSH): thyroid hormones.
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) (the gonadotropins):
Prolactin:
Hormones of the Anterior Pituitary
The Adrenal Gland: Consists of the Cortex and the Medulla
The adrenal cortex or cortex secretes:
Adrenal androgens: testosterone
Two types of corticosteroids:
Glucocorticoids: Involved with metabolism and response to stress (e.g., cortisol)
Mineralocorticoids: Regulate salt and water metabolism (e.g., aldosterone).
The adrenal medulla or medulla secretes:.
Catecholamines (epinephrine and norepinephrine).
The Adrenal Gland: Glucocorticoids (Steroids)
Cortisol is the principal human glucocorticoid.
Cortisol production is diurnal,
Stress and level of circulating steroid influence secretion.
Exogenous steroid replacement resulting in a reduction of endogenous steroid production,
This is the rationale behind “tapered steroid dosing” which is when large doses of steroids are tapered downward
Exogenous: originating from outside the body; Endogenous: originating from within the body.
Increase resistance to stress
Anti-Inflammatory Actions
Immunosuppressive Actions
Corticosteroids: Comparative Potency – Systemic Steroids
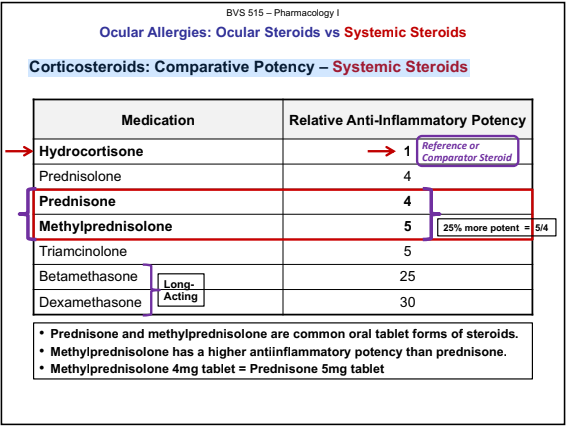
Ocular Allergies: Ocular Steroids vs Systemic Steroids
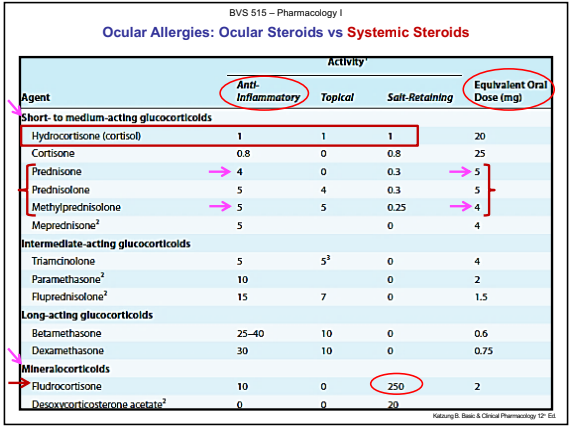
Corticosteroids (Steroids)
Adverse drug effects of steroids are dose and duration related (e.g., suppression of the hypothalamic-pituitary-adrenal axis).
Always evaluate the risk vs benefit
In general, systemic steroids disrupt the inflammatory cascade and suppress normal immune response by impacting every aspect of the immune system.
Corticosteroids
Mechanism of Action: Steroids suppress normal immune response by impacting every aspect of the immune system.
Inhibit phospholipase A2 synthesis
Inhibit both production and release of inflammatory mediators
Suppress of T-cell lymphocyte proliferation
Summary of Effects:
Corticosteroids: Warnings/Significant ADEs Endocrine Effects: Adrenal Suppression
Reversible HPA (hypothalamic-pituitary-adrenal) axis suppression with the possibility of glucocorticoid insufficiency.
HPA suppression may be minimized by gradual reduction of dosage (e.g., tapered dose schedule or tapering).
Tapered Dose Schedule or Steroid Tapering
Gradual daily dosage reduction to allow the HPA to recover from the HPA-suppressant effects of large steroid doses.
Medrol Dose-Pack (Methylprednisolone)
Steroid adverse effects are dose and duration related.
Corticosteroids: Warnings/Significant ADEs Cardiovascular Effects
Elevation of blood pressure due to salt and water retention,
Caution
Corticosteroids: Warnings/Significant ADEs
Gastrointestinal (GI)
Increased risk of GI perforation
Corticosteroids: Warnings/Significant ADEs General: Hyperglycemia,
Hyperglycemia,
Corticosteroids: Warnings/Significant ADEs
CNS and Psychiatric/Behavioral Effects
Euphoria, mood swings, insomnia, personality changes
(steroid psychosis)
Corticosteroids: Warnings/Significant ADEs
Decrease in Bone Density
Increased potential for osteoporosis and fractures decrease bone formation and increase bone resorption
May lead to growth retardation and inhibition of bone growth in
children and adolescents.
Corticosteroids: Warnings/Significant ADEs Ocular Effects
Increased intraocular pressure (IOP), glaucoma (open-angle)
Posterior subcapsular cataract.
Ocular Steroids
Ocular corticosteroids relative anti-inflammatory efficacy.
The effectiveness of ocular steroids in suppressing inflammation is also due to differences in penetrating the cornea,
The ideal steroid should be biphasic in its polarity,
Modification of a steroid base impacts the following:
– Formulation of the steroid product.
– Ocular penetration and metabolism.
– Anti-inflammatory potency/efficacy.
Ocular steroids are produced in three main formulations:
Alcohol and Acetate formulations (sparingly soluble in water, lipid soluble suspensions/ointment)
Phosphate formulations (water soluble solutions)
The more lipid-soluble derivatives (alcohol and acetates) are available as suspensions/ointments
The water-soluble salts (phosphates) generally are formulated as solutions.
Injectable Ocular Administration
Ocular Steroids: Impact of Formulation on Potency and Efficacy
Systemic steroids are categorized
Ocular steroids
Potency/Drug Concentration
Ocular penetration
Formulation/Vehicle
Alcohol and Acetate (lipid soluble suspensions/ointment)
Phosphate (water soluble solutions)
Alcohol and acetate formulations are sparingly soluble in water (e.g., more lipophilic) and are formulated as suspensions.
acetate 0.1%, ((Flarex®, gen.) is more potent than Fluorometholone alcohol 0.1% ophth. suspension (FML Liquifilm®).
Phosphate derivatives are very soluble in aqueous media (e.g., more hydrophilic) and are formulated as solutions.
acetate 1% ophthalmic suspension (Pred Forte®, gen.) is more potent than Prednisolone sodium phosphate 1% ophthalmic solution (generic).
Ocular Steroids: Steroid-Related IOP Elevation
prolonged ocular steroids can result in steroid-related IOP elevation
Changes in the trabecular meshwork and its extracellular matrix causes resistance to aqueous outflow which increases IOP.
Steroid responders can experience IOP increases within a few hours of therapy.
Ocular Steroids: Indications
Indications: Treatment of steroid-responsive inflammatory conditions
Allergic Conjunctivitis and Infective Conjunctivitis
Ocular Steroids: Mechanism of Action
Mechanism of Action: Steroids suppress normal immune response by impacting every aspect of the immune system.
Inhibit phospholipase A2 synthesis
Inhibit both production and release of inflammatory mediators
Suppress of T-cell lymphocyte proliferation.
Reduce/Reverse capillary permeability and cellular exudation.
Ocular Steroids: Relative Contraindications/ADEs/Cautions
Relative Contraindications: Infections in general
In general, ocular steroids with greater anti-inflammatory potency have potential for increased risks of elevated IOP, cataracts, etc.
General Ocular ADEs/Cautions: elevated IOP, glaucoma, cataracts, optic nerve damage, keratitis, secondary ocular infections (viral, fungal, bacterial), exacerbation of current infection, corneal thining erosion/ulceration/edema, globe perforation,
General Non-Ocular ADEs/Cautions:
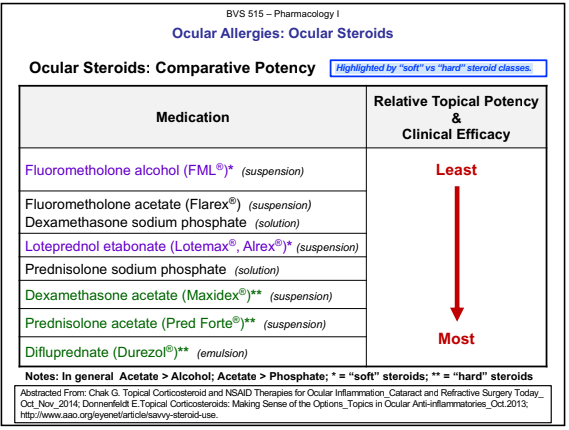
Ocular Steroids: Steroid Related IOP Elevation – “Soft” vs “Hard”
“Soft” corticosteroids have been strategically designed to reduce the risk of IOP elevation
Loteprednol etabonate 0.2% and 0.5%
Fluorometholone alcohol
“Hard” corticosteroids are more potent or stronger and have a greater risk of side effects.
Difluprednate 0.05% (Durezol® emulsion), Prednisolone acetate 1% suspension (Pred Forte®), and Dexamethasone Acetate 0.1% suspension (Maxidex®).
Ocular Steroids: Ketone vs Ester Classification
Ketone Steroids:
Ester Steroids: Loteprednol
Loteprednol is formulated with an ester instead of a ketone group at the C-20 position which makes loteprednol less cataractogenic
“soft” steroid
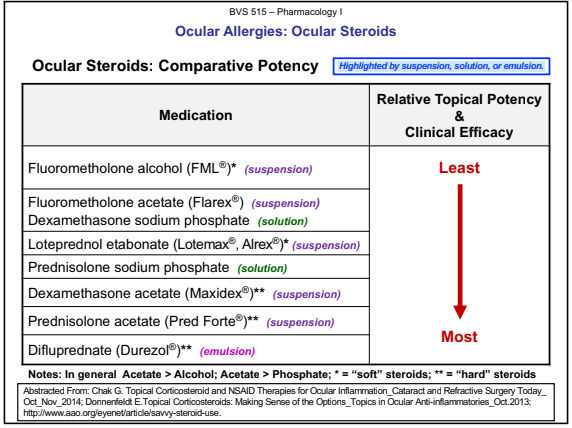
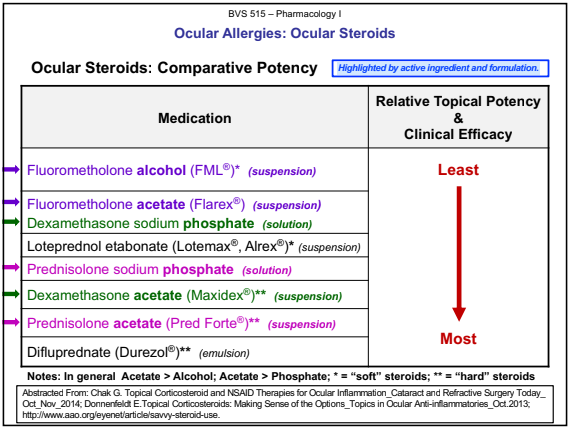
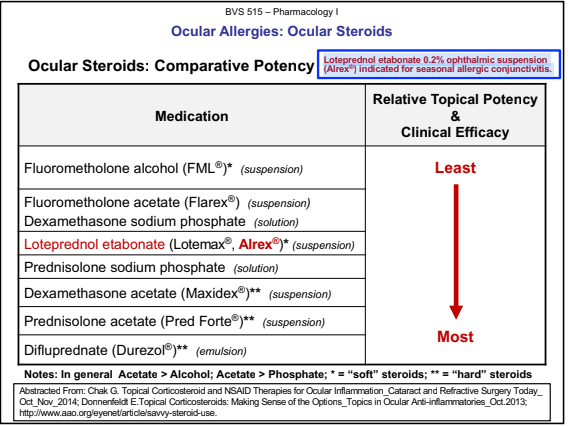
Ocular Allergies: Ocular Steroids
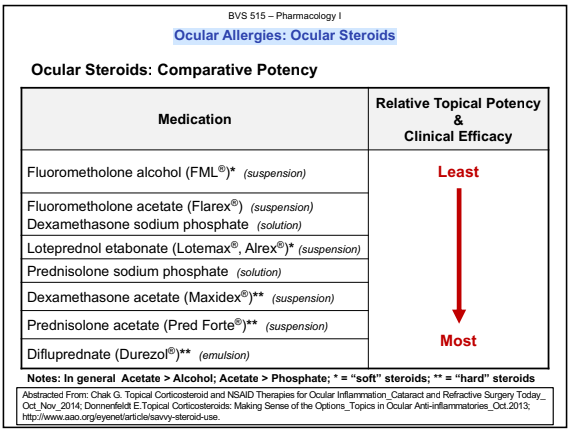
Ocular Steroids: Comparative Potency Highlighted by suspension, solution, or emulsion.
Ocular Steroids: Comparative Potency Highlighted by active ingredient and formulation.
Ocular Steroids: Comparative Potency Highlighted by “soft” vs “hard” steroid classes.
Fluorometholone
Products
Fluorometholone alcohol 0.1% ophth. suspension (FML Liquifilm®)
Fluorometholone acetate 0.1% ophth. suspension (Flarex®, gen.)
Fluorometholone alcohol 0.25% ophth. suspension (FML Forte®)
Note: The 0.1% acetate formulation (Flarex®) is more potent than the 0.1% alcohol formulation (FML®).
In general Acetate > Alcohol.
FML® = Alcohol; Flarex® = Acetate
Dexamethasone
Dosage
Solution
Suspension
Pharmacology:hard or strong corticosteroid, 3rd
most potent steroid
ADEs:
Products
Dexamethasone sodium phosphate 0.1% ophthalmic solution generic)
Dexamethasone 0.1% ophthalmic suspension = acetate (Maxidex®)
Acetate is more potent than phosphate.
Generic solution = Phosphate; Maxidex® suspension = Acetate
Ocular Steroids: Comparative Potency
Loteprednol etabonate 0.2% ophthalmic suspension (Alrex®) indicated for seasonal allergic conjunctivitis.
Loteprednol
Pharmacology
Considered a soft corticosteroid
“soft” steroid
formulated with an ester instead of a ketone
ADEs:
Products
Loteprednol etabonate 0.2% ophthalmic suspension (Alrex®)
Loteprednol etabonate 0.5% ophthalmic suspension, ointment and gel (Lotemax®)
Indicated for SAC Lowest % suspension.
4 times daily.
Prednisolone
Pharmacology: The acetate suspension (Pred Forte®) is considered a hard or strong corticosteroid, 2nd in potency after difluprednate
Indications: Ophthalmic inflammatory conditions/corneal injury.
ADEs:
Products
Prednisolone acetate 0.12% ophthalmic suspension (Pred Mild®)
Prednisolone acetate 1% ophthalmic suspension (Various generic, Omnipred®, Pred Forte®)
Prednisolone sodium phosphate 1% ophthalmic solution (generic)
Note:acetate more potent than the
phosphate
Acetate is more potent than phosphate.
Generic solution = Phosphate; Pred Mild® and Pred Forte® = Acetate
Difluprednate(Durezol® – emulsion)
History
A difluorinated derivative of prednisolone
Pharmacology: The most potent ophthalmic steroid.
ADEs:
Dosage
Endogenous anterior uveitis:
Inflammation/pain associated with ocular surgery: