Evidence-Informed Practice in Nursing: Key Concepts and Steps
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
Evidence
Information acquired through research and scientific practices (CNA, 2010).
Evidence-based medicine
Integrating individual clinical expertise + the best available external clinical evidence from systematic research.
Evidence-based practice (EBP)
A problem-solving approach to clinical practice that involves integrating high-quality research, clinical expertise, and patient/family values.
Best evidence for practice
Includes empirical evidence from systematic reviews, randomized controlled trials, and other scientific methods such as descriptive and qualitative research.
Critics of EBP
Argue that it will turn clinicians into technicians who follow a recipe and that there is a tendency to forget the client's or patient's values.
Research utilization
The process of using research findings to improve patient care, often based on a single study (Melnyk & Fineout-Overholt, 2019).
Evidence-informed practice
A broader term that encompasses not only research utilization but also the use of case reports and expert opinion in deciding the practices to be used in health care.
High-quality research in nursing practice
Will improve patient outcomes when combined with individual patient values and clinical expertise from nurses.
Barriers to implementing evidence into practice
Include the perception that it takes too much time, lack of evidence-informed practice knowledge and skills among clinicians, and lack of support in organizations.
Dissemination
The communication of research findings; dissemination activities take many forms, including publications, conferences, consultations, and training programs.
Lack of evidence-informed practice mentors
A barrier to implementing evidence into practice.
Resistance from colleagues
A barrier to implementing evidence-informed practice changes.
Focus in health professional education
Often on the research process rather than evidence-informed practice.
Patient factors in EBM or EBP
Indicate that EBM or EBP requires the integration of the best research evidence with our clinical expertise and our patient's unique values and circumstances.
Evidence-informed safety practices
Now an expected standard in many institutions.
Time perception barrier
The perception that it takes too much time to implement evidence into practice.
Knowledge and skills barrier
A lack of evidence-informed practice knowledge and skills among clinicians.
Support in organizations
Lack of support is a barrier to implementing evidence-informed practice.
Appropriate resources barrier
Lack of appropriate resources is a barrier to implementing evidence-informed practice.
Conceptual forms of using research evidence
Influence the thinking of the health care provider but not necessarily the action.
Decision-driven forms of using research evidence
Using evidence in practice encompasses application of scientific knowledge as part of a new practice, policy, procedure, or intervention.
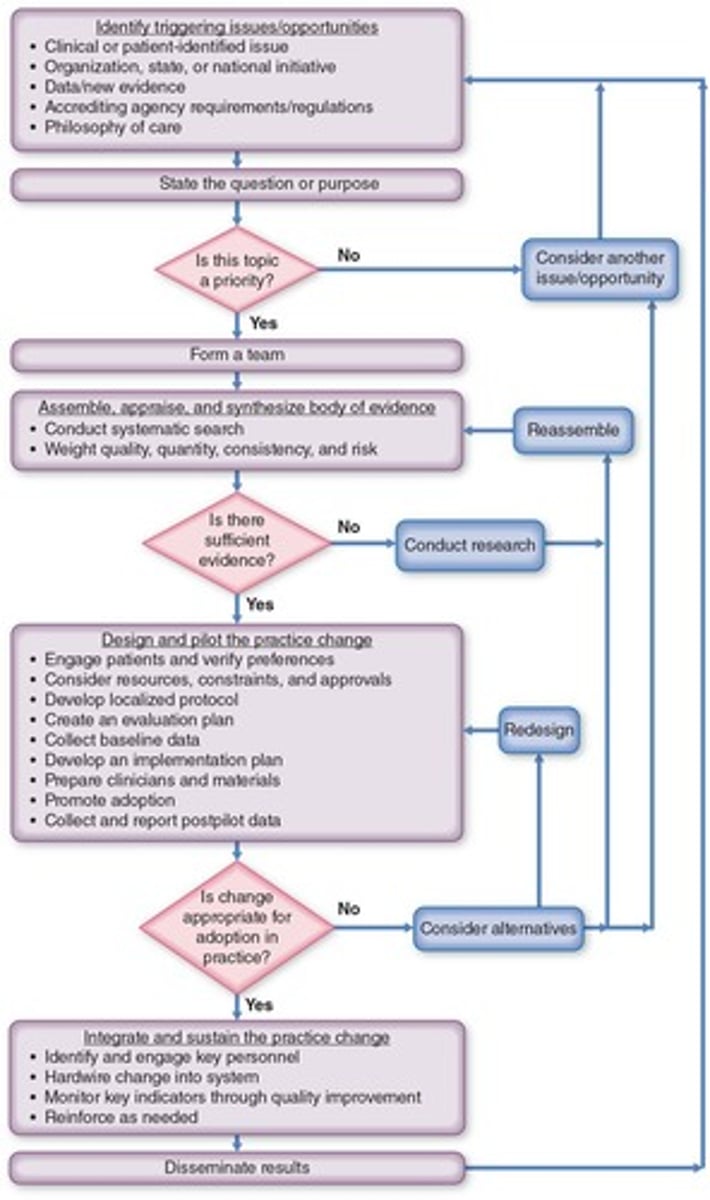
Evidence-Based Practice to Promote Excellence in Health Care
Iowa Model Collaborative, 2017.
The Ottawa Model of Research Use
OMRU; Logan & Graham, 1998.
The Promoting Action on Research Implementation in Health Services model
i-PARIHS model; Kitson & Harvey, 2016.
Conduct and Utilization of Research in Nursing model
CURN model; Haller, Reynolds, & Horseley, 1979; Horsley, Crane, Crabtree, et al., 1983.
Identification of a clinical problem or question of practice
The first step common to most models of evidence-informed practice.
Search for best evidence
The second step common to most models of evidence-informed practice.
Critical appraisal of evidence
Involves assessing the strength, quality, quantity, and consistency of evidence.
Recommendation for action
Based on the appraisal of evidence, this can be no change, change, or further study.
Implementation of recommendation
The process of putting the recommended action into practice.
Evaluation of recommendation
Assessing the recommendation in relation to desired outcomes.
Selection of a Topic
The first step in the evidence-based process.
Forming a Team
The second step in the evidence-based process.
Evidence Retrieval
The fourth step in the evidence-based process.
Implementing the Practice Change
The fifth step in the evidence-based process.
Development of Evidence-Informed Practice
The third step in the evidence-based process.
Decision to Change Practice
The third step in the evidence-based process.
Critique of Evidence
An essential part of evaluating the quality of published articles.
Setting Forth Evidence-Informed Practice Recommendations
The second step in the evidence-based process.
Synthesis of the Research
The first step in the evidence-based process.
Selection Criteria for an Evidence-Informed Practice Project
Criteria include priority of the topic, magnitude of the problem, and applicability to clinical areas.
Strength of Evidence
High: Further research is very unlikely to change our confidence in the estimate of effect.
Quality of Evidence
Moderate: Further research is likely to have an important impact on our confidence in the estimate of effect.
Low Quality of Evidence
Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Low
Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very Low
Any estimate of effect is very uncertain.
Strength of Evidence
Level of evidence + quality of evidence = strength of evidence and confidence to act and change practice.
American Association of Critical-Care Nurses
Professional organization that published evidence informed practice guidelines.
American Pain Society
Professional organization that published evidence informed practice guidelines.
Canadian Heart and Stroke Foundation
Professional organization that published evidence informed practice guidelines.
National Institute for Health and Care Excellence
Professional organization that published evidence informed practice guidelines.
Registered Nurses' Association of Ontario (RNAO)
Professional organization that published evidence informed practice guidelines.
American College of Physicians
Source for best evidence from studies of clinical problems.
Centre for Health Evidence
Source for best evidence from studies of clinical problems.
Cochrane Library
Source for best evidence from studies of clinical problems.
Joanna Briggs Institute
Source for best evidence from studies of clinical problems.
Steps of Evidence-Informed Practice
Selecting a topic, forming a team, retrieving the evidence, grading the evidence, developing an evidence-informed practice standard, implementing the evidence-informed practice, and evaluating the effect on staff, patient, and fiscal outcomes.
Evaluation
Includes both process and outcome measures.
Culture of Evidence-Informed Practice
Creating this culture requires an interactive process.
Research Utilization
The terms research utilization and evidence-informed practice are sometimes used interchangeably.
Forms of Evidence Use
There are two forms of evidence use: conceptual and decision driven.
Models of Evidence-Informed Practice
A key feature of all models is the judicious review and synthesis of research and other types of evidence to develop an evidence-informed practice standard.
Evidence-Informed Practice in Nursing
The integration of the best available research evidence with clinical expertise and patient preferences.
Important Step in Developing Evidence-Informed Practice
Evaluating the strength of the evidence from research studies.
Role of the Nurse in Evidence-Informed Practice
Incorporating clinical expertise, patient preferences, and the best available evidence.
First Step in Implementing Evidence-Informed Practice
Formulate a clinical question based on patient care needs.