HIV and AIDs/Antiviral Agents (7/`9))
1/48
Earn XP
Description and Tags
Zhou Lecture 6 (Lecture 24)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
49 Terms
What is Zika Virus? what are the signs? what diseases are associated?
enveloped, icosahedral, nonsegmented, ss + sense RNA virus of Flaviviridae
related to Yellow, dengue, and west nnile
Disease:
microcephaly, severe brain malformations
may cause gullain-barre syndrome
Signs: fever, rash, joint pain, conjunctivitis, muscle pain, headaches within 2 weeks of travel from an area with Zika
How do retroviruses with oncogenes replicate?
helper virus/cell transformation
how is Zika virus spread?
transmitted by daytime active Aedes mosquitoes (A aegypti, Albopictus)
mosquito bites
pregnant woman to fetus
sex with infected person
lab exposure
blood transfusion
NOT breastfeeding
how does zika affect people?
generally asymptomatic/mild symptoms
symptoms last several days-week
not sick enough to go to hospital
low fatality rate
how does Zika virus cause Gullain Barre syndrome (GBS)?
GBS: NS state where immune system damages the nerve cells(myelin sheaths), causing muscle weakness, sometimes paralysis
Strongly associated with Zika, but only small portion with ZIka get GBS
How is Zika treated?
no specific medicine or vaccine
treating symptoms:
rest, drink enough fluids, do not take aspirin or NSAIDs
Prevention:
destory mosquito habitats
wear protective clothing
avoid unsafe sex with potentially infected partners
review treatment and prevention of arboviral diseases
difficult to diagnose from symptoms and travel history
treatment: control fever, convulsions, dehydration, shock, edema
Vaccination
control: pesticide/insect repellents, protective clothing, stay indoors at night
what are the general properties of retroviruses? 3 subfamilies?
induce neoplastic diseases and AIDs in the host
many species
subfamilies:
oncoviruses: acute, nonacute oncogenic virus
lentiviruses: slow virus
neurologic, pneumonias, AIDs
Spumaviruses: no pathological effects
Structure of retroviruses? A, B, C, D types?
spherical, 65-150nm diameter
viral genome: 2 identical RNA
Types:
A: no nucleocapsid
B: eccentrically located nucleocapsid
C: centrally located nucleocapsid
D: eccentric core, less gp
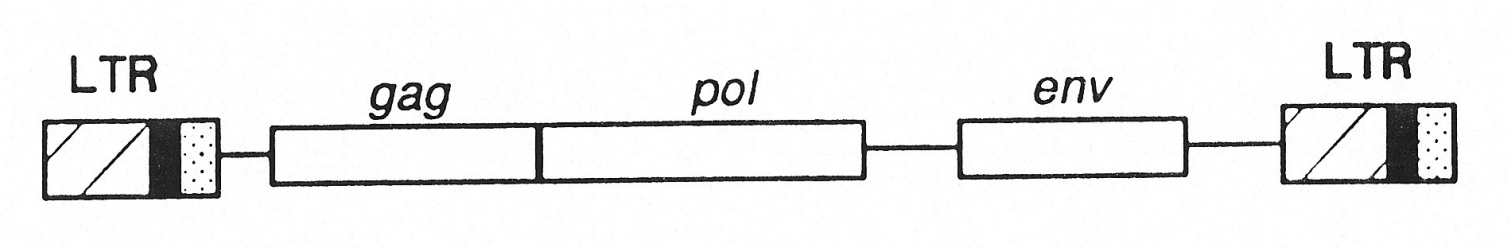
describe the structure of the retroviral genome
Gag: precursor polyprotein for capsidproteins
Protease for processing the polyprotein
Pol: reverse transcriptase
Env: envelope protein
LTR: long terminal repeat
What is the difference between oncoviruses and oncogenes?
oncovirus:
acutely oncogenic, usually defective
slowly oncogenic,replication competent
human leukemia virus > leukemia
oncogenes:
acute transformation
not important for virla replicatoin
numerous
location variable
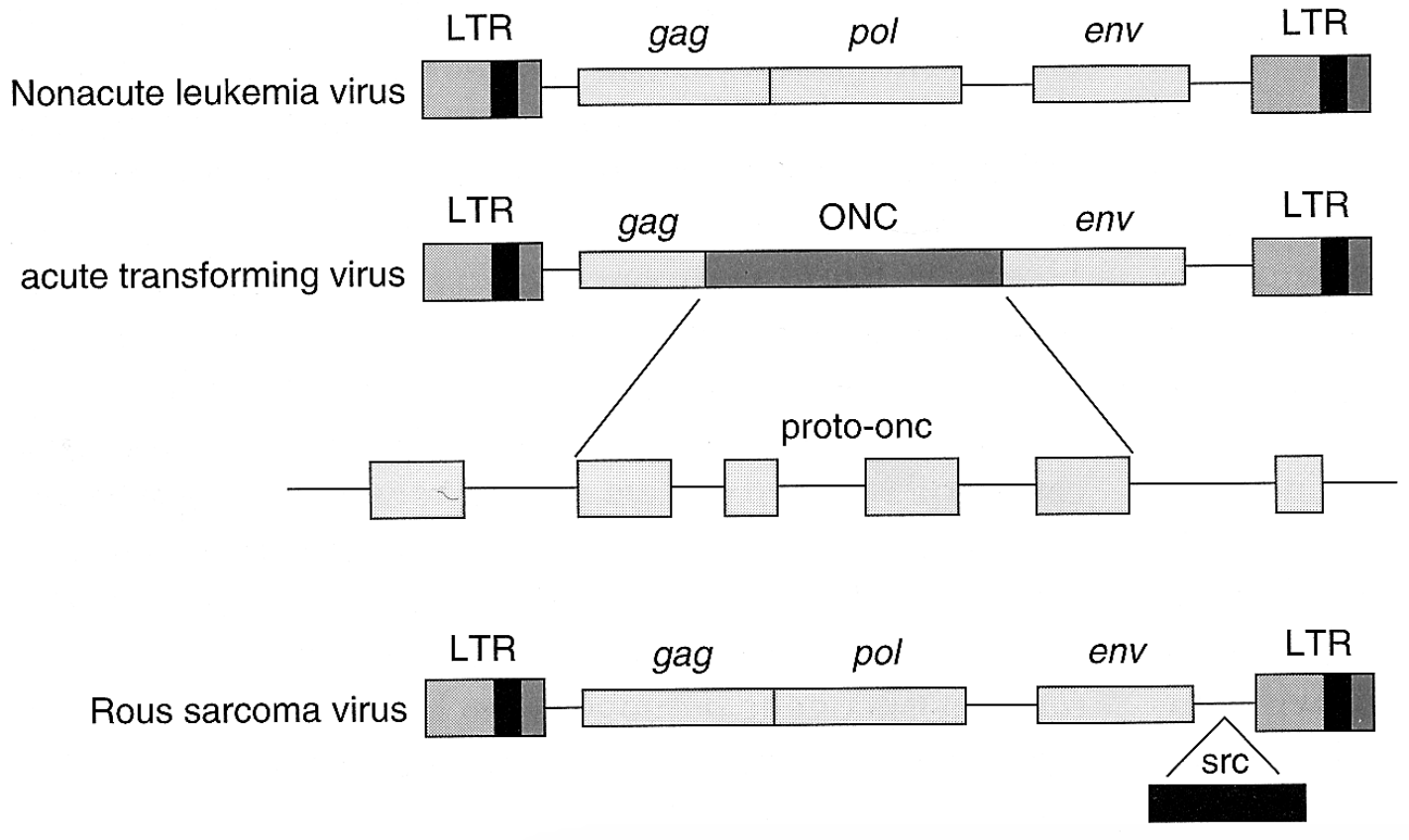
what is the difference between non-acute leukemia virus, acute transforming virus, and rous sarcoma virus structure?
nonacute leukemia virus: lacks an oncogene > slow cancer
acute transforming virus: contains an oncogene > rapid cancer
rous sarcoma virus structure: contains src (potent oncogene) > very rapid cancer
SEQ replication of a defective oncogenic virus
defective transforming virus defects cell
helper virus infects same cell
3 ways:
A) Cell gets both: transforming virus + helper virus
It becomes a transformed virus-producing cell, making lots of virus.
B) Cell gets only the transforming virus
It becomes a transformed cell (cancer-like),
but cannot produce virus, because it lacks the helper.
C) Cell gets only the helper virus
It becomes non-transformed, but produces helper virus only.
proto-oncogenes
normal cellular genes
highly conserved
share homology with viral oncogenes
differ in structure and activity from viral oncogenes: point mutations, truncations, constantly active
what are the 3 oncogene families?
cell surface receptors
cytoplasmic signaling intermediates
nuclear transcription factors
how are retroviruses and cancer associated?
retroviruses lead to tumor formation
oncogenes not necessary for replication
constantly lost
viral tumor mostly not infectious
retroviruses are tools for studying tumor formation
proto-oncogenes can be activated into oncogenes
What are AIDs? symptoms?
fatal immunodeficiency disease arising form infection of HIV and accompanied by some of the following symptoms
opportunistic infection
persistent fever
unusual cancer — karposi sarcoma
extensive wt loss
chronic diarrhea
neurological disorders
common symptoms: fever, loss of appetite, wt loss, extreme fatigue, englargement of lymph nodes
What are different types of AIDs?
malignancy: Kaposi’s sarcoma (skin and mucous membranes)
AID dementia complex: neurological abnormalities
pnemonia: pneumocystis carinii
encephalitis: toxoplasmia gondii
yeast infection
mononucleosis: cytomegalovirus
herpes simplex virus
What are some risk factors of HIV?
anal sex
HIV carriers in heterosexual sex
multiple sexual partners
blood transfusions and blood products
congenital and neonatal AIDs
medical and dental personnel
How does AIDs enter the body?
HIV enters through blood or sexual secretions via broken skin or mucous membranes, infects dendritic cells and macrophages under the skin, and then spreads to lymph nodes, bone marrow, and the bloodstream where it amplifies and disseminates.
What are some misconceptions of AIDs?
transmission by: inhalation, hand shaking, sharing public facilities, food, swimming
insect bites
no transmission among family members when blood transfer is not involved
HIV Life Cycle
Entry and integration
HIV binds and fuses with host cell membrane
viral ssRNA enters the cell
reverse transcriptase converst ssRNA > ssDNA > dsDNA
viral dsDNA moves into nucleus, viral DNA inserted into host chromosomes
Latent Period:
provirus sits silently inside host DNA months-yrs
immune system is triggered, provirus reactivated and produce viral mRNA
Assembly and Release
viral mRNA translated into capsid proteins, enzymes and envelope proteins
viral RNA and proteins assemble into new HIV particles
bud off > kill lyses the host cell
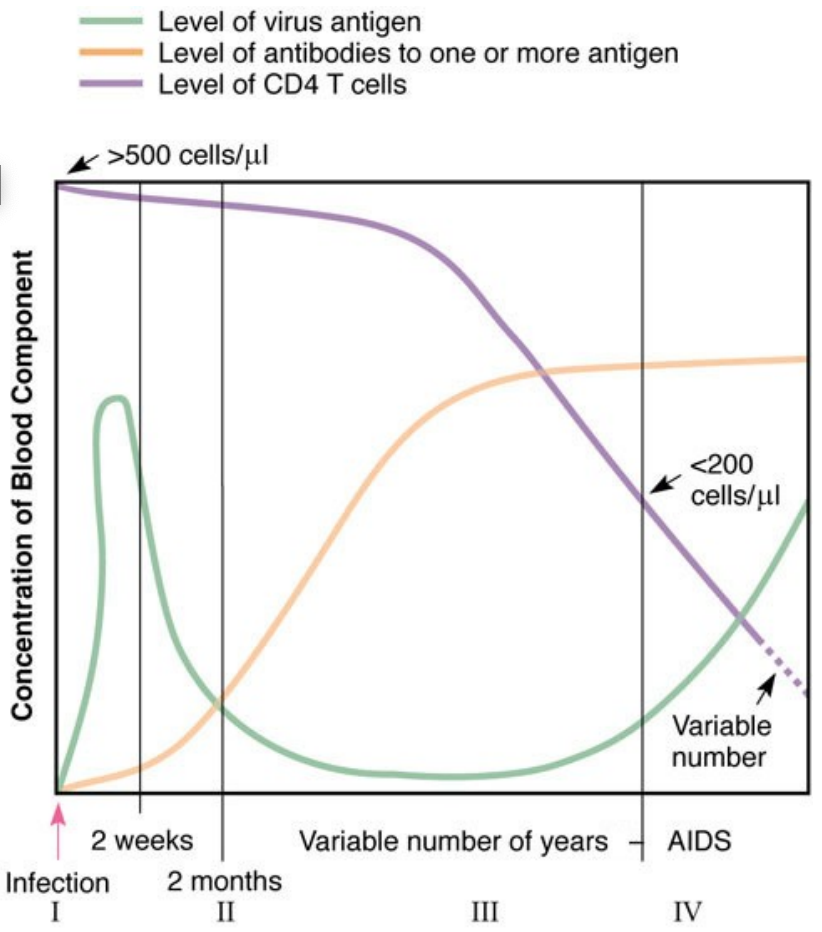
How do virus levels, antibody levels, and CD4 T-cell counts change over the course of HIV infection?
HIV levels spike early, then drop and stay low for years before rising again in AIDS
antibodies appear after a few weeks and stay high
CD4 T-cells stay near normal for years but gradually decline and fall below 200 cells/µL in AIDS.
What are the primary effects of HIV infection?
destruction of T4 lymphocygtes
infection of brain tissues leads to inflammation
What are the Secondary Effects of HIV Infection
opportunistic infections:
fungus infections: pneumocystis carinii pneumonia (PCP), widespread, usually harmless
Protozoan infections: toxoplasmosis
herpes infection, bacteria infections — tuberculosis
Cancers: kaposi sarcoma, herpesvirus-8 (KSHV)
Other: neurological problems, fatigue, wt loss
AIDs Test
detecting anti-HIV antibodies
ELISA — false positive
Western blot
false engative retest
ID HIV: research phase
AIDs Therapy
no cure
control opportunistic and HIV infections
PCP: pentamidine, sulfamethoxazole-trimethoprim
CMV: ganciclovia, foscarnet
Fungal infection: fluconazole
kaposi sarcoma: alpha inferferon and chorionic gonadotropin
HIV: combination
supportive care
Anti-HIV Drugs
most effective drugs target HIV reverse transcriptase: AZT, ddI, 3TC, d4T
protease inhibitors, block maturation of HIV
combination therapy:
drug resistance for single drug therapy
HAARRT
Other drugs: integrase inhibitors, viral fusion inhibitors, interferons
What is HAART?
highly active anti-retroviral therapy
Use two RT inhibitors and one protease inhibitors
significant reduction of death rate
HIV+ but healthy possible
high cost and toxic fx
HIV Drug Classes
non-nucleoside reverse transcriptase inhibitors (NNRTIs)
nucleoside reverse transcriptase inhibitors
Protease inhibitors (PIs)
fusion inhibitors
CCR5 antagonists (CCR5s — entry inhibitors)
integrase stand transfer inhibitors (INSTIs)
AIDS Prevention
sexual history of life style
monogamous, safe sex, no anal sex, no drugs, clean needles, nor needle sharing
AID testing: critical for control
What is the target of Remdesivir?
Remdesivir targets the viral RNA-dependent RNA polymerase (RdRP), which is essential for viral RNA replication.
What kind of nucleic acid do retroviruses contain?
Retroviruses contain RNA genomes, specifically two identical RNA molecules.
How many RNAs does each retrovirus have?
Each retrovirus carries 2 identical RNA strands in its virion.
What are the three basic genes the retroviral genome encodes?
Retroviruses encode gag (capsid proteins), pol (reverse transcriptase), and env (envelope proteins).
What is provirus?
A provirus is double-stranded viral DNA integrated into the host chromosome, remaining latent until activated.
retroviral DNA integrated from their RNA genome
What enzyme makes retroviral DNA from their RNA genome?
Retroviruses use reverse transcriptase to convert their RNA genome into DNA.
What is the unique aspect of retroviral replication compared with other viruses?
Retroviral replication is unique because the virus converts RNA into DNA and integrates into the host genome before producing new virus.
retroviruses make DNA from their RNA genome and integrate the viral DNA into host DNA
What is a retroviral LTR?
LTRs (long terminal repeats) are regulatory sequences at both ends of the retroviral genome used for integration and transcription.
transcription promoter that is crucial for viral replication
Are retroviral oncogenes required for viral replication?
No—retroviral oncogenes are not required for viral replication and are often lost because they do not contribute to viral fitness.
Where do viral oncogenes come from?
Viral oncogenes originate from host proto-oncogenes that retroviruses capture and modify during infection
host DNA
do non-acutely oncogenic viruses have oncogenes?
no, they do not cause cell transformation and tumor in a short period of time. They can cause tumor after a long latent period
What does aids stand for? What is the key problem in AIDs?
Acquired Immuno Deficiency Syndrome
immune deficiency, T4 lymphocyte depletion
What causes AIDs? Why are they non-progressors
Acquired Immuno Deficiency Syndrome
lack of the cytokine receptor and infection by a weakened mutant
Stages of HIV infection and disease
initial infeciton: vague, mononucelosis like symptoms
first antibodies detected 2 months after infection
asymptomatic incubation period: 2-15 yrs
disease: fever, swollen lymph glands, fatigue, diarrhea, wt loss, neurological syndromes, opportunistic infection and cancer
Is HIV an RNA or DNA virus?
RNA
What is AZT?
A nucleoside reverse transcriptase inhibitor (NRTI)
Inhibits HIV reverse transcriptase activity
What is HAART?
Highly Active Antiretroviral Therapy
Uses two reverse transcriptase inhibitors
Plus one protease inhibitor
How can AIDS transmission be prevented?
Blood screening
Clean needles
Safe sex practices