Week 6: Intravenous Initiation and Phlebotomy
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
81 Terms
What is the most commonly used invasive device?
Peripheral Intravenous (PIV) Catheters
Are the risks associated with PIVs generally overestimated or underestimated?
Underestimated
1 multiple choice option
What percent of PIV's fail?
35-50%
List the types of PIV's used
-"Short" peripheral catheter (main ones used)
-Midline peripheral catheter
Outline Phillips' 16 Steps To Peripheral Short-Infusion Therapy
1. Authorized prescriber’s order
2. Hand hygiene
3. Equipment collection and preparation
4. Patient identification and psychological preparation
5. Site selection, vein dilation, and visualization technology
6. Attention to pain management
7. Catheter selection
8. Gloving
9. Site preparation
10. Vein entry
11. Catheter stabilization and dressing management
12. Labeling
13. Equipment disposal
14. Patient education
15. Rate calculations
16. Documentation
What are the general considerations when selecting a vein?
-Vein Condition
-Age
-Allergies
-Patient Preference
-Patient Activity
-Medications - Anticoagulants
-Medical Conditions
What are the general considerations for: Vein Condition
-Gently palpate the vein with your fingers and observe how it refills
-Note that patients with hypotension and hypovolemia their veins will be more difficult see and the veins tend to collapse
What are the ideal vein characteristics?
A vein that is relatively smooth and pliable
What are the general considerations for: Age
-Due to increased body fat infants don't have the same selection sites
- In elderly patients avoid the metacarpal veins, as they are very thin and fragile (Low SQ fat)
-Irritating solutions put elderly patients at risk for infiltration
What veins should we use on infants under 18 months old?
Scalp veins
What can we use instead of a tourniquet for vein dilation in elderly patients over 65?
Consider using a BP cuff dilated to about 30mmHg
What are the general considerations for: Allergies
Know your patients allergies, some patients could be allergic to chlorhexidine, tape, and other securement devices
What are the general considerations for: Patient Preference
Find out if the patient is right or left hand, and use the non-dominant hand so they can perform activities without tubes getting in the way
True or False: For Patient Activity, you can more commonly put an IV wherever you'd like with bed ridden patients?
True
1 multiple choice option
What are the general considerations for: Medications – Anticoagulants
Be mindful of prolonged bleeding times (during insertion and removal) and bruising, being careful how much pressure you apply with the tournique
What are the general considerations for: Medical Conditions
-Avoid starting IV on the affected side of patients who’ve had a stroke, due to poor circulation and higher risk of having infiltration and phlebitis of the affected site
-Avoid starting IV’s on the affected side of patients whose had mastectomies with lymph node removal
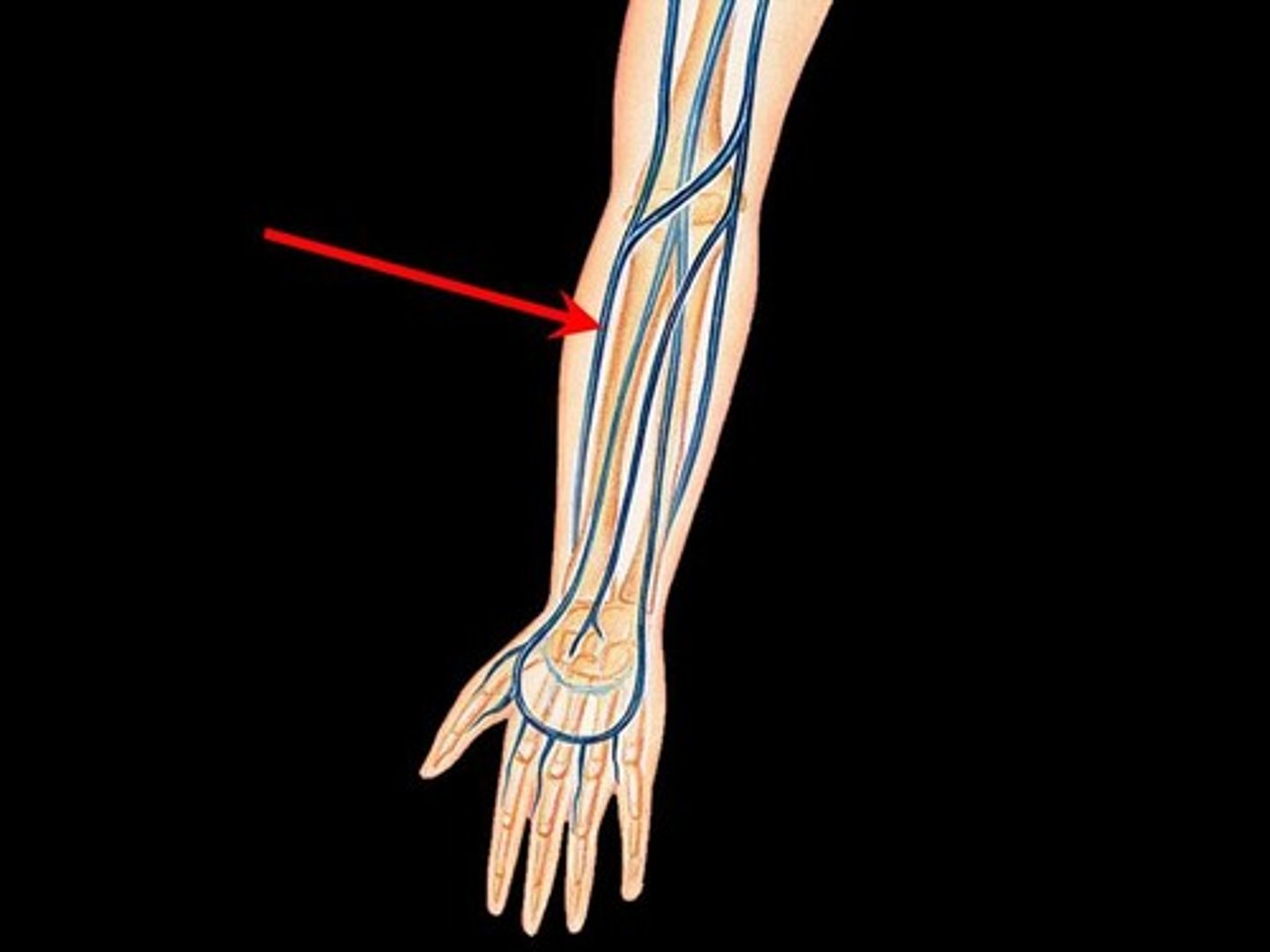
What IV sites are associated with greater risk of nerve injury
-Cephalic vein at wrist: Very close to the radial nerve
-Antecubital Fossa: Contains the tendons of the bicep, medium nerve, and brachial artery
-Palm side of wrist: Close proximity to the medium nerve
List the superficial veins of the dorsum (back) of the hand
-Dorsal venous arch
-Basilic vein
-Digital veins
-Metacarpal veins
-Cephalic vein
Why would we not ideally use the basilic vein?
It's a large vein, but harder start due to location and likes to roll
Why would we not ideally use the digital vein?
Avoided due to high risk of infiltration
Why would we not ideally use the metacarpal veins?
-Fragile in elderly patients
-Cannot infuse irritating or caustic medications (E.g. Antibiotics, KCL)
What vein would a nurse use to infuse an irritating solution?
Cephalic vein
What is the ideal (first choice) vein for PIV's and why?
Cephalic vein of the forearm
A large vein that is easily accessed (Go at least 8-10 cm above the thumb to avoid the radial nerve)
Which vein is suggested for students to try and find their first start?
Cephalic vein
How can you stabilize veins that like to roll?
Use traction during venipuncture
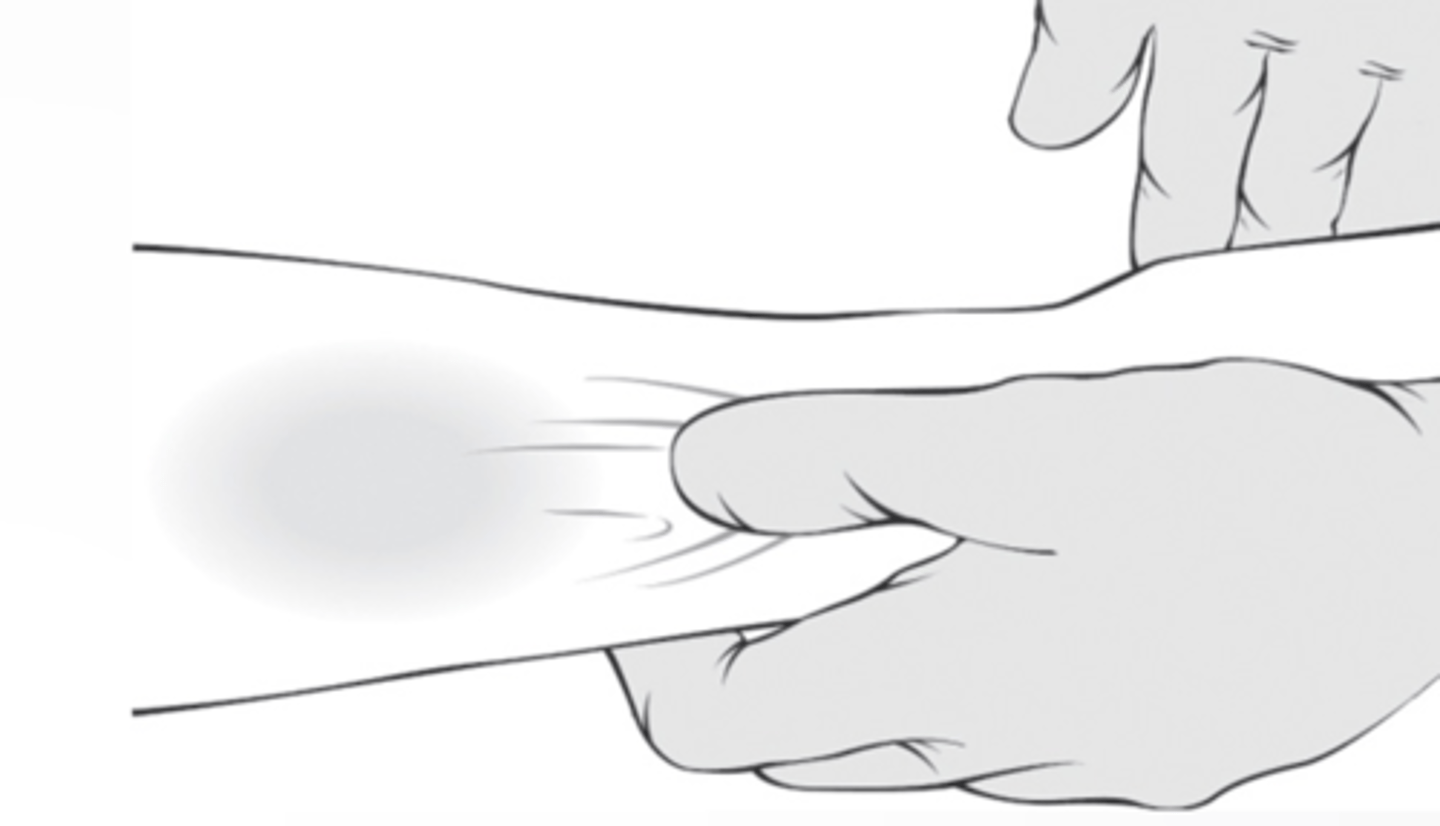
Explain the traction method of venipuncture
Use the thumb of your non-dominant hand to gently pull the skin and subcutaneous tissue taut (about 1–2 inches) below the venipuncture site to straighten and anchor the vein in place
List the superficial veins of the forearm
-Cephalic vein
-Accessory cephalic vein
-Basilic vein
-Median antebrachial vein
-Median cubital vein
Why would we not use the accessory cephalic vein?
Harder to locate in patients with large adipose tissue (can be short so the catheter may not fit)
Why would we not use the median antebrachial vein?
Avoided due to increased nerve in the area and blood work is done often done there
Why would we not use the AC fossa?
Only used in emergencies or when no other options are available
As the site will often occlude due to flexion at the site increasing the risk of phlebitis and infiltration
Which areas for PIV's should be avoided in adult patients?
Ventral surface (inner aspect) of the wrist
List the ways we can distend the vein
-Position the extremity lower than the heart for 1-2 minutes
-Have the patient clench or pump their fist
-Place a ball or rolled face cloth in their hand to help them squeeze
-Warm compress (warm blanket)
-BF cuff (30mmHg)
-Tourniquet
Between moist heat and dry heat, which is better for vein distention?
Dry heat
1 multiple choice option
How do you apply a tourniquet?
Apply 10 cm above the puncture site.
Ensure it impedes venous flow but NOT arterial flow, meaning you should still have a radial pulse

When should you release the tourniquet?
Once you see flashback (blood in the catheter hub)
What is the colour code for a 16 gauge catheter?
Gray
What is the colour code for a 18 gauge catheter?
Green
What is the colour code for a 20 gauge catheter?
Pink
What is the colour code for a 22 gauge catheter?
Blue
What is the colour code for a 24 gauge catheter?
Yellow
What is the colour code for a 26 gauge catheter?
Violet
The smaller the gauge number the _____ the catheter
Bigger
3 multiple choice options
Is it recommended to use the smallest or biggest gauge catheter appropriate for the prescribed therapy?
Smallest
1 multiple choice option
Do larger catheters require larger or smaller veins for insertion?
Larger
1 multiple choice option
What gauge size is selected for most patients and things?
22-24 gauge
What gauge size is selected for blood transfusions?
18-20: Adults
22-24: Elderly, neonates/infants, fragile veins
How should you site prep if the site is visibly dirty
Cleanse the site with soap and water
How should you site prep if the site has excessive hair?
Clip the excess hair with scissors or surgical clippers with a disposable head.
DO NOT shave, as shaving can cause micro-abrasions that can lead to infection.
What should you prep the site with?
Chlorhexidine based solution using a back and forth scrubbing motion for 30 seconds, and let the site air dry to allow antiseptic properties to work (DO NOT blow, fan, or wipe the site)
What can happen if you insert the IV before the site is dry?
The IV will tract antiseptic into the patient's vein
True or False: Once the site is prepped you cannot re-palpate the vein?
True, but if you must re-palpate don sterile gloves
1 multiple choice option
What are the two methods of venipuncture?
-Direct
-Indirect
Explain the direct venipuncture method
Approach directly over the vein at a 15-30 degree angle
Appropriate for small gauge needles, fragile and/or rolling veins
Explain the indirect venipuncture method
Enter the skin slightly adjacent to the vein, and direct the device into the side of the vein wall at a 15-30 degree angle
True or False: You can use the indirect venipuncture method for all vein sites?
True
1 multiple choice option
How many venipuncture attempts does a healthcare facility allow the nurse to attempt before they must notify another professional?
Two total
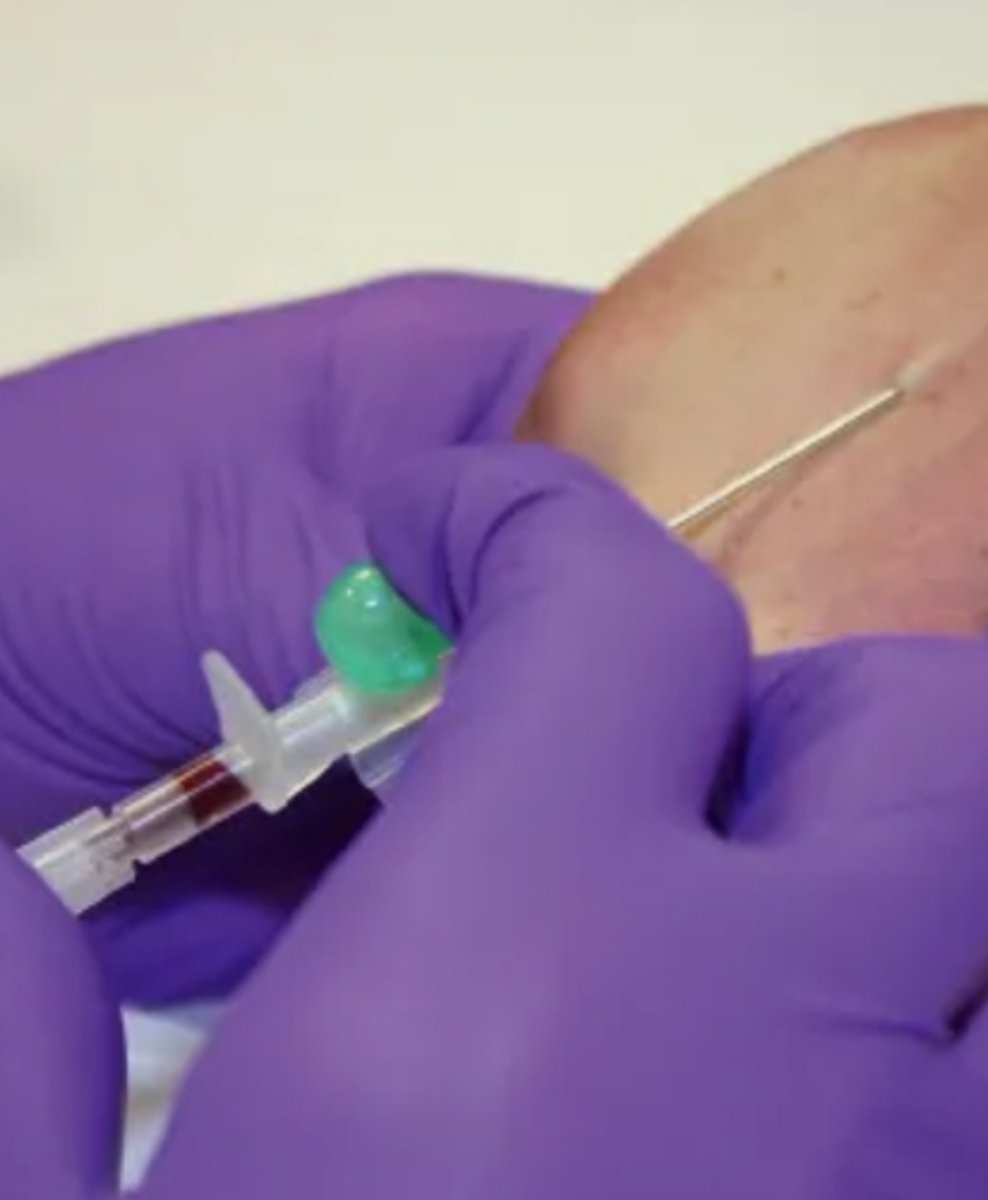
What is an indication that the catheter is in the vein?
Blood flashback
What is the appropriate dressing type of PIV's?
Transparent Dressing:
-Tegaderm
-Tegaderm Advanced IV (Built in stabilization device)
How should you dress the catheter?
Centre the dressing over top the IV site, ensuring the top margin of the cannula hub is covered
What should you include in the documentation of the PIV?
-Date and time of insertion
-Site preparation used
-Gauge and length of device
-Vein used
-Dressing type
-Patient response (tolerance)
-What you did with the IV (E.g. IVSL, infuse fluids, etc)
-Ongoing assessment
How often should you assess the site post insertion?
-Every 4 hours (Q4H): Alert and oriented adult patients
-Every 1 to 2 hours (Q1-2H): Critically ill patients and adults with cognitive/sensory deficits
-Every hour (Q1H): Pediatric and neonatal patients
List the common troubleshooting/missteps with PIV's
-Not releasing the tourniquet
-Using a stop/start technique
-Inadequate vein stabilization
-Puncturing through the back of the vein
-Stopping too soon
-Going too deep
-Wrong angle selection
List the possible methods of blood collection
-Venipuncture
-Capillary puncture (E.g. Side of the heel of a neonate)
-Vascular access device (E.g. Central Line and PICC for blood sample)
What are the purposes of Phlebotomy?
-Diagnostic testing
-Blood donation
-Therapeutic reasons
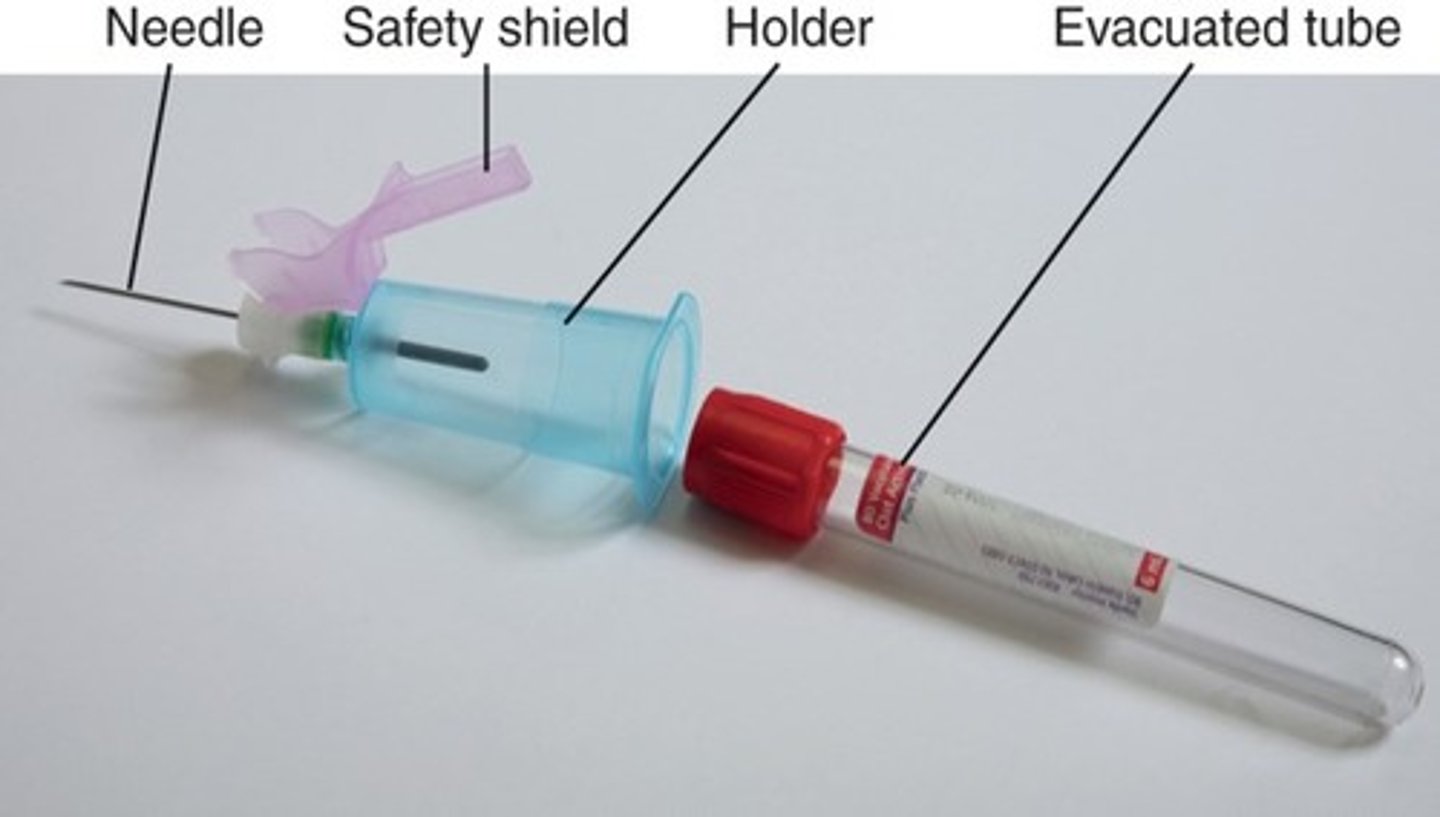
Outline the characteristics of the traditional components of an evacuated tube system (ETS)
-Self assembly
-The top part of the multi-sample needle has a rubber sleeve over the needle, and will have to screw it into the bottom of the tube holder to make a complete system
What is the syringe system?
Attaching a syringe and gently pulling back on the plunger to obtain a blood sample
What is the Butterfly/Winged infusion set?
A butterfly needle attached to a vacutainer (syringe or IV line) (same method in the assembly of the ETS system)

What are the indications for the use of a butterfly/winged infusion set?
Commonly used in patients with:
-Small or difficult veins
-Pediatrics
-Older adults
-Patients with severe arthritis
-Patients who might be restrictive positions (traction)
-Patients with numerous needle sticks that have scarring and require a smaller needle
What are evacuated tubes?
Color coded tubes made of unbreakable plastic with pre-measured amounts of vacuum used to collect samples
What additives do evacuated tubes contain?
-Anticoagulants
-Oxalates
-Citrates
-Ethylenediaminetetraacetic acid (EDTA)
-Heparin
What procedures are involved in the collection of blood?
-Review test requisition
-Collect supplies
-Assess and approach the patient
-Select a puncture site
-Select and prepare puncture site
-Choose venipuncture method
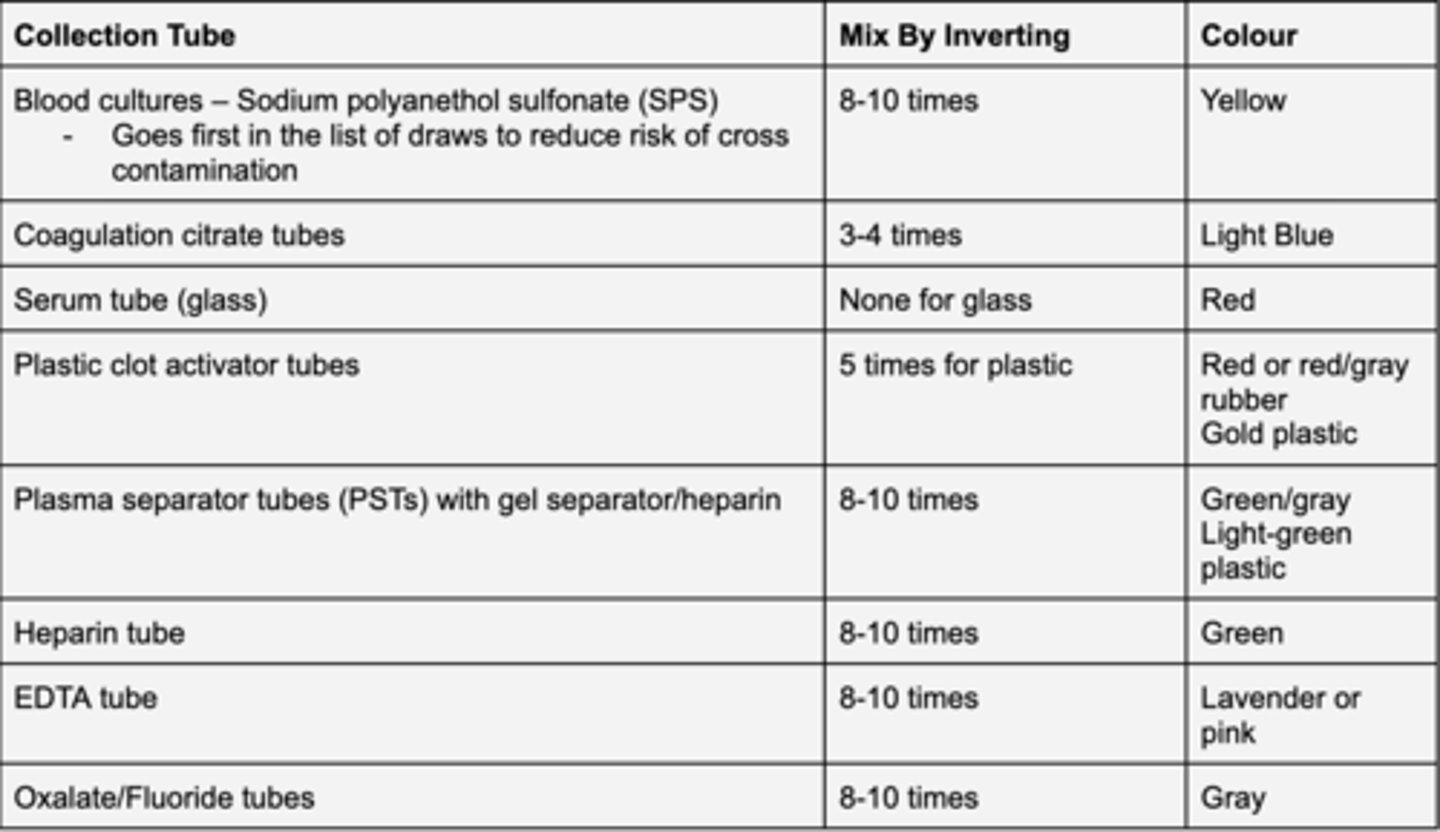
Order for draw for multiple tube collections
What is the first tube collected during a blood draw?
Blood cultures (yellow cap), to reduce the risk of contamination
What should you do when drawing for coagulation studies (PTPT)?
Will often use another tube without an additive before to have a pure sample without contamination from the tissues
Which veins are considered during IV site selection?
-Antecubital
-Median cubital
-Cephalic
-Basilic
What is the proper patient positioning for venipuncture?
Hold the patient's arm by putting your hand behind their elbow to help stabilize it. Then line up and insert the needle
How should the needle bevel be positioned during insertion?
Bevel up
3 multiple choice options
What should you label each tube with?
Label individually with the patients ID
List the possible phlebotomy complications
-Hematoma
-Iatrogenic Anemia
-Infection (Follow asepsis)
-Nerve Injury
-Vein Damage (Improper technique or frequent technique)
What is the proper treatment for a hematoma complication?
Stop and apply pressure for two minutes and use a cold compress.
Then apply pressure for 15 minutes afterwards to prevent.
What is Iatrogenic Anemia
Anemia caused by excessive and frequent blood draws (Lowered hematocrit and hemoglobin count)