PATHO - Exam 2 Review
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
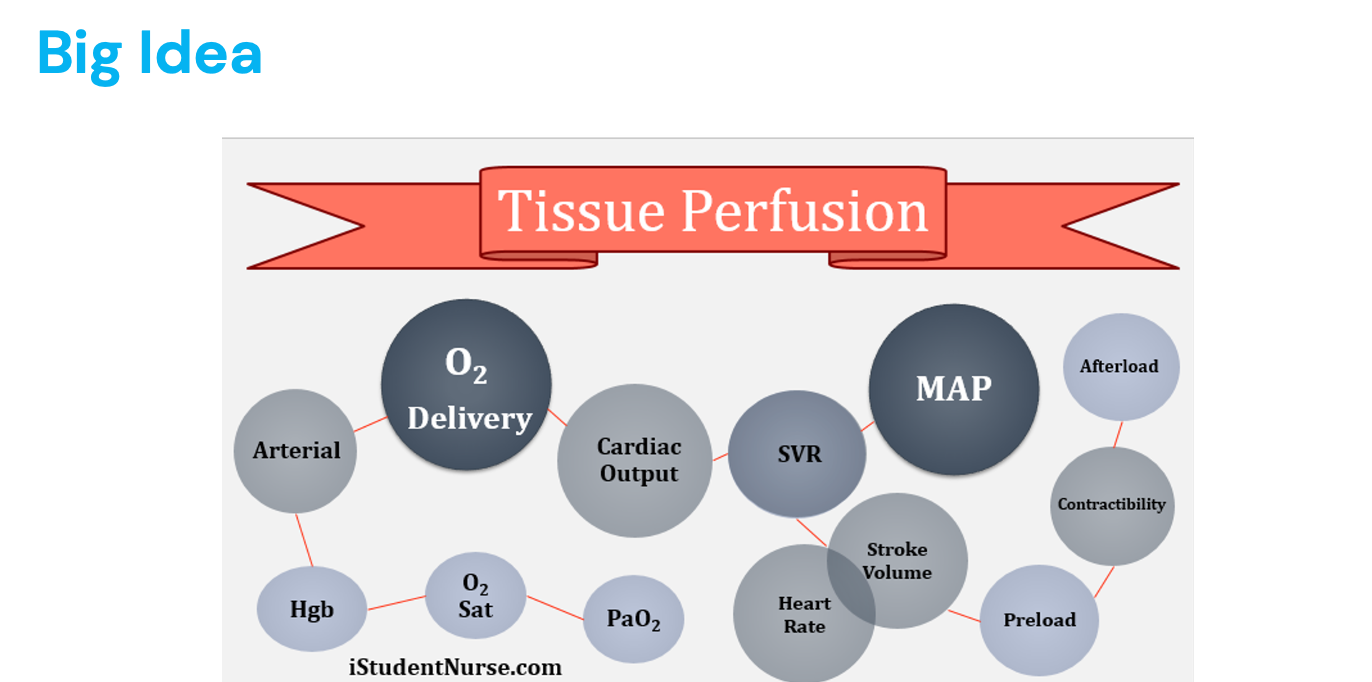
Tissue Perfusion
PaO2
O2 Sat
Hgb (hemoglobin) - oxygen carrying compacity of the blood
Arterial
O2 delivery
Cardiac output - how effective your heart is with pumping blood where it needs to go
SVR
MAP (average pressure in arteries)
Stroke volume/heart rate
SV - how much blood is pumped out per heart beat
Can be adjusted by increased contractability (by SNS)
HR - how fast/slow your heart is beating
Preload - amount of blood in heart before contraction
Contractability
Afterload - how much force the heart has pump against to get the blood out to the body
Problem with arteries: downstream
Problem with veins: upstream
Cardiac issues can affect the whole body
SVR
Systemic vascular resistance (also called peripheral vascular resistance)
Increase resistance down the pipeline:
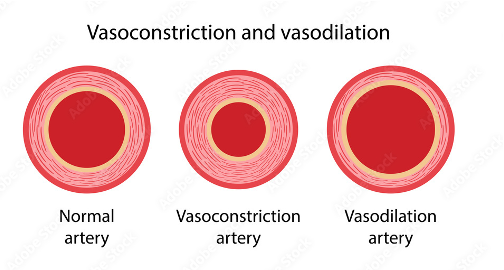
Diameter of the blood vessels (vasoconstriction and vasodilation)
“Clogged tube" in atherosclerosis
MAP
Difference between systolic and diastolic blood pressure
Tells us how much oxygen is getting to organs (perfusion)
Needs to be about 70, over 60 to perfuse adequately
Contractility
Forcefulness of heart’s contraction
Blood Pressure
Hydrostatic pressure + blood pressure (pressure of blood exerts on walls)
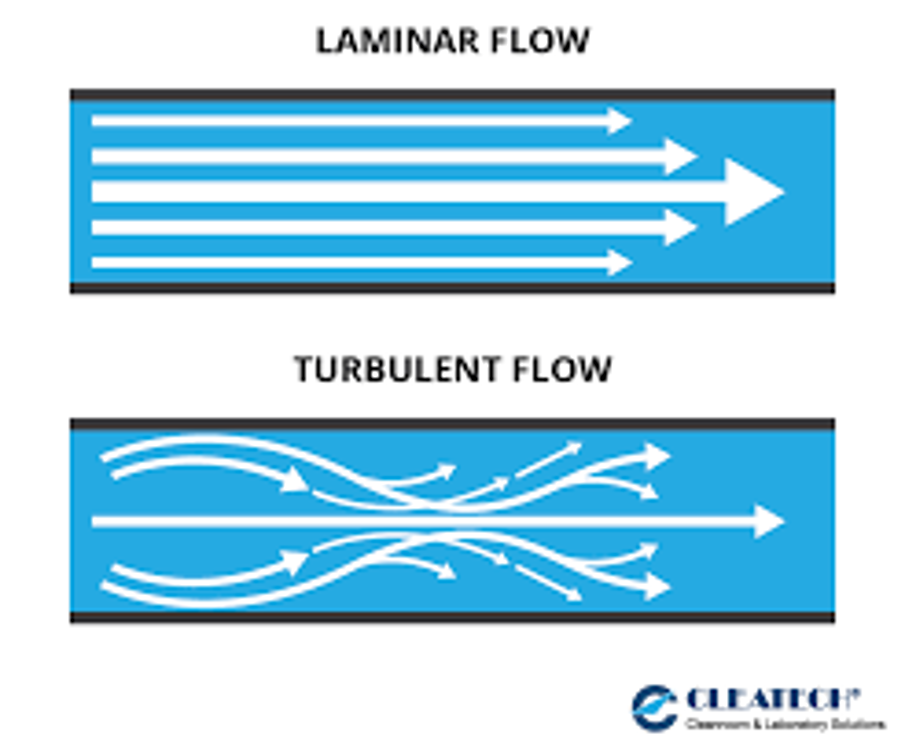
Laminar flow
Plasma on outside, cells on the inside
Stimulates prostaglandins and nitric oxide (dilates blood vessels)
Turbulent flow
More pressure required to move blood forward
Damage epithelium
Heart has to pump harder to move blood
EX: increased velocity, decreased vessel diameter, low blood viscosity
*Arteries = take blood to extremities (high pressure)
*Veins = bring blood back to the heart (low pressure)
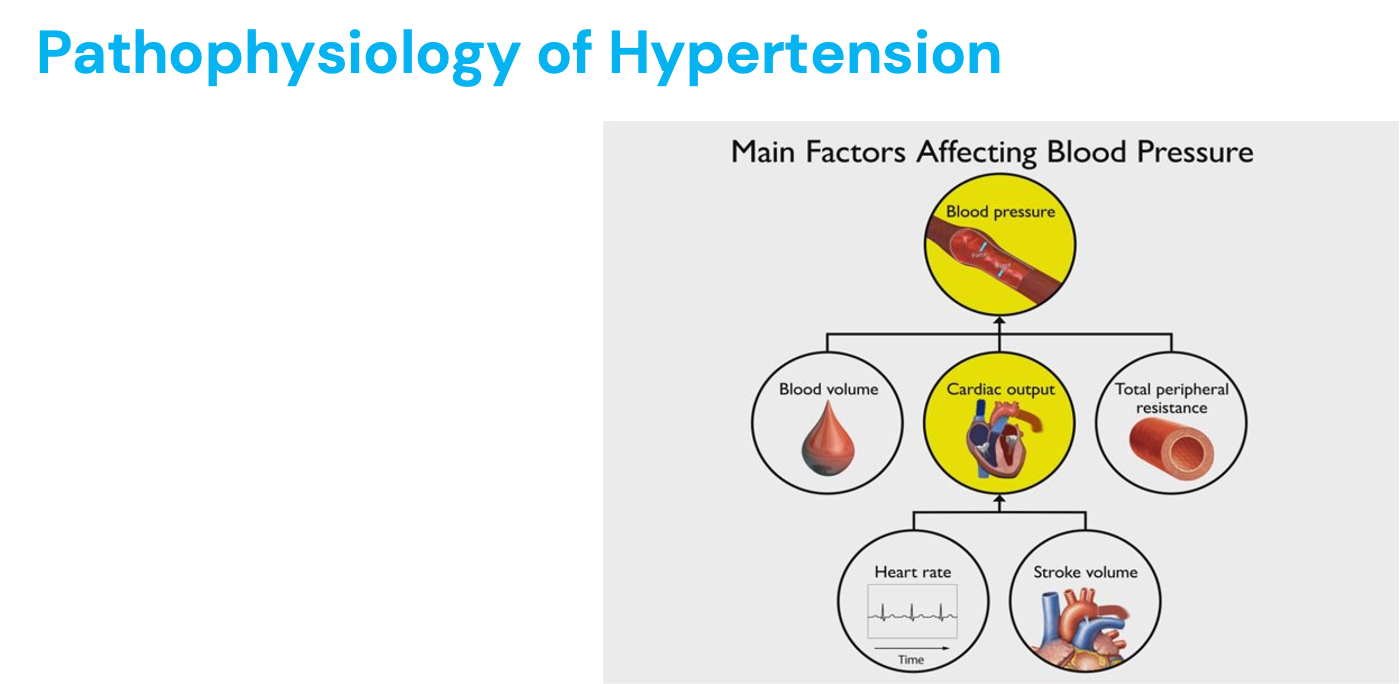
Components of Blood Pressure
Cardiac “pump”
Heart failure = pump failure
Vascular system “pipes”
Vascular tone
Vascular resistance
Blood volume “fluid”
Too little = shock
Cardiogenic shock
Vasodilation = Blood volume leaks out of capillaries (distributive)
Hypovolemic shock = decrease in blood volume
Too much fluid/vasoconstriction = hypertension
Blood Pressure + Resistance
Pressure differences drive blood flow: high to low (RA)
What generates driving pressure on arterial side of circulation?
Pump - muscle becomes pump
Veins can stretch and have valves
Lowest circulatory pressure in body = right atrium (2-7 mmHg) - where blood comes back to heart
Pressure in veins lower than arteries
Pressure = cardiac output (HR x SV) x resistance
SV = amount of blood ejected during contraction
Cardiac output in one minute
Resistance = opposition blood encounters in blood vessels
Ohm’s law: flow (CO) = pressure/resistance
Resistance increases, pressure constant = flow decreases
Pressure increases, resistance constant = flow increases
Factors affecting resistance:
Blood viscosity = overproduction of RBCs (thicker blood)
Vessel length = hypertension (more blood vessels heart needs to pump to, more pressure to pump against)
Vessel diameter = vasoconstriction and vasodilation
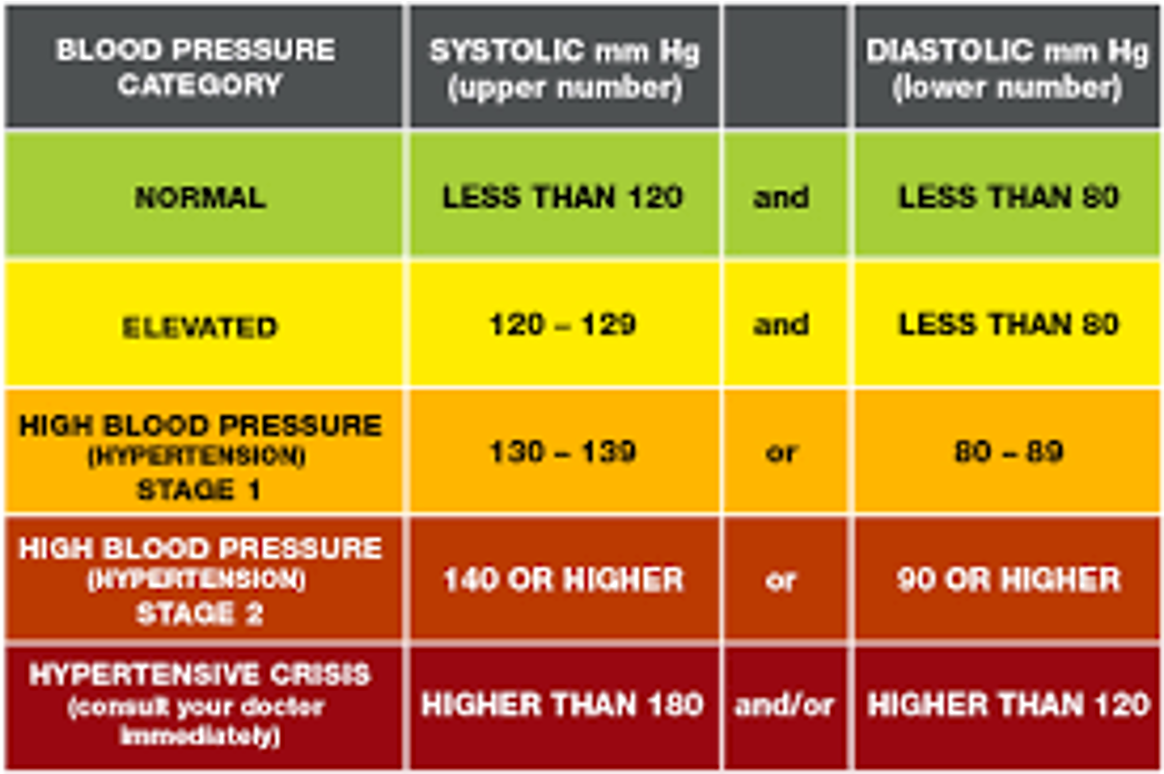
Hypertension
Sustained elevation of arterial blood pressure (causes endothelial and silent target organ damage)
Silent killer
Primary risk factor for cardiovascular disease
If pressure = CO x resistance, then:
What could raise blood pressure?
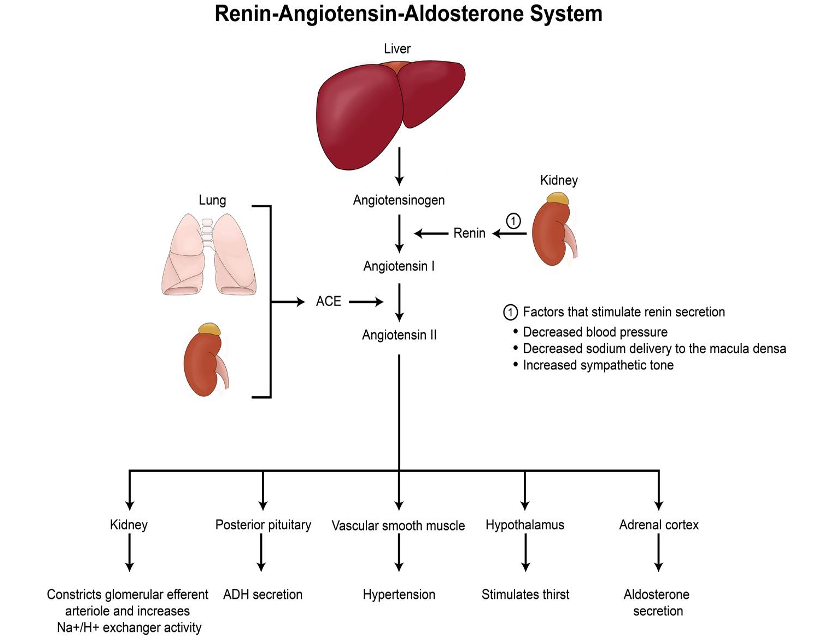
RAAS system
Vasoconstriction
High heart rate
Hypervolemia: indicate something is wrong with pump (high BP)
Thick blood
SAD diet: high processed food
Too much salt = hold on to more water = hypervolemic = high BP
Systole = arterial pressure during contraction
Diastole = arterial pressure during relaxation (filling)
Healthy = <120/80
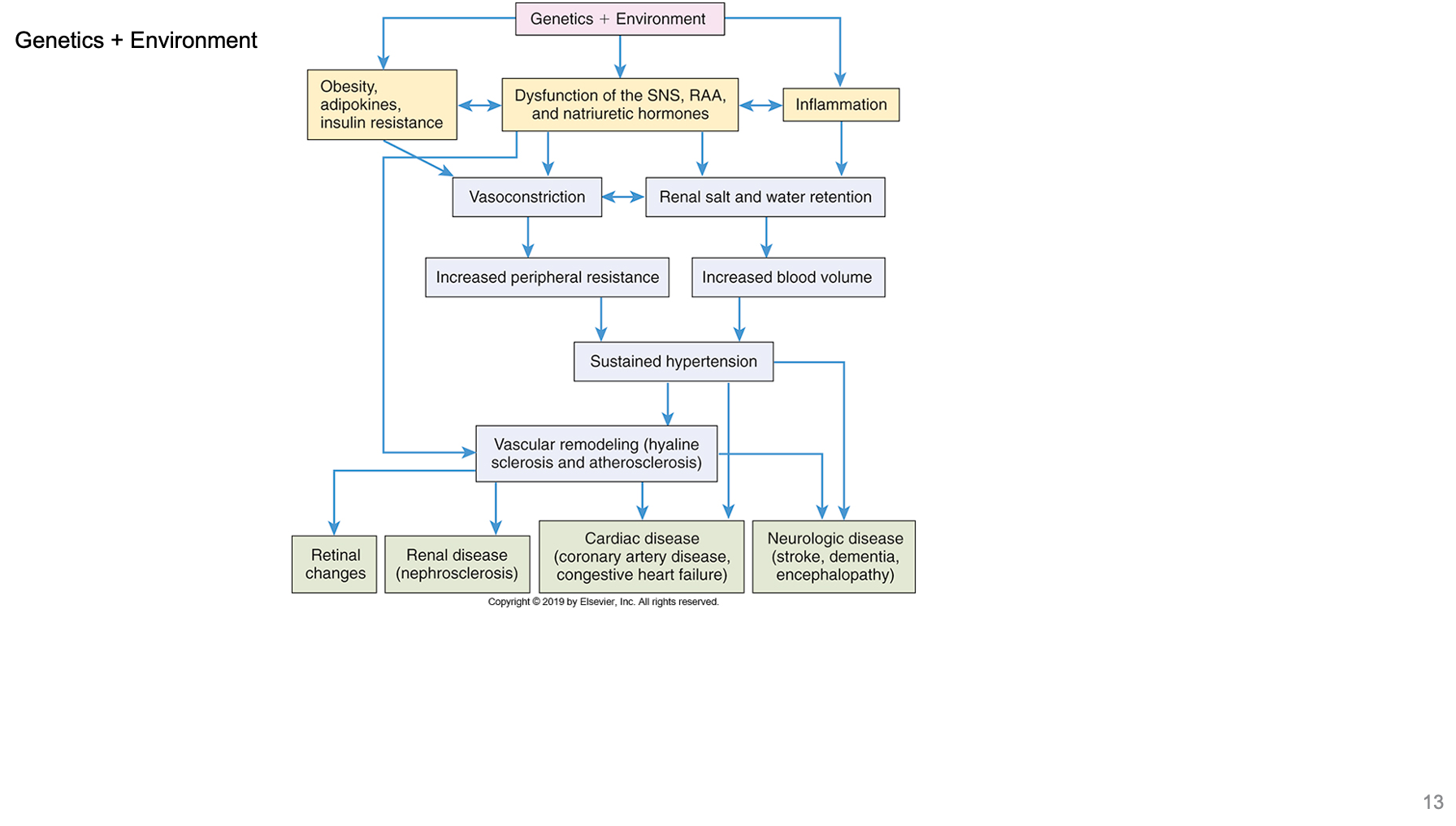
Primary Hypertension
Increased BP (heart has to pump even harder each heart beat - get extra muscle - can be pathologic in nature) due to 1+ of these factors:
Increased HR
To much thyroid hormone in blood = tachycardia
Increased myocardial contractility
Increased vasoconstriction
Too much renin
Increased blood volume
Increased blood volume due to high sodium diet
SNS, Baroreceptors, RAAS, plasma volume (controlled by kidneys) all determine blood pressure
Dysregulation from:
Ineffective communication/collaboration between organs responsible for regulating blood volume, vascular tone, and cardiac performance
Renal artery stenosis - kidneys not perfused well with blood, RAAS, blood pressure goes up
Risk Factors of Hypertension
Nonmodifiable
Age
BP gets higher with age (blood vessels loose elasticity, forcing heart to pump harder)
Kidneys can’t secrete sodium, blood volume higher
Older adults have low grade inflammatory response
Older biological males
Females catch up after menopause and they lose the protection of estrogen
Assigned sex at birth
Male = higher rate of hypertension earlier (based on hormones)
Women after menopause (loose estrogen) = heart attack becomes equal with men
Family history/genetics
Ethnicity = AA have more symptomatic problems with hypertension
Family history contributes 50% increase in susceptibility
Race
More bad outcomes in black populations then white
Modifiable
Diet
SAD diet = processed foods (sodium, sugar, trans fats, low in plants)
Blue zone diet:
100% whole grains: farro, quinoa, brown rice, oatmeal, bulgur, cornmeal
Nuts and seeds: a handful a day
Beans, legumes, pulses: a cup of cooked beans/pulses per day
Fruits and vegetables: 5-10 servings per day
Blood lipid levels
Increased LDL levels, low HDL levels = fatty plaques in arteries
Tobacco/alcohol consumption
Toxins enter bloodstream from tobacco and damages endothelium
More than one drink a day = LDL cholesterol builds up
Activity/fitness level
Lowers stress
Lowers resting heart rate
Weight
1 pound of weight loss = 1 mmHg lost
Blood glucose levels
Damages endothelial lining of blood vessels if high for a long time
Glucose has osmotic pull, increases blood volume
Allostatic load
Chronic stress not able to be resolved
Minority populations
Poverty
Physiologic Systems Contributing to Hypertension (HTN)
RAAS
Kidneys not perfused = increased renin = vasoconstriction = increased blood pressure = aldosterone = sodium retention by kidney = increased blood volume and pressure = HTN
Thirst center (hypothalamus and ADH - retains water = increased BP)
SNS
Baroreceptors
Cardiac output increased = heart rate increased
Resistance increased = SNS (vasoconstriction)
Endothelial dysfunction
Reduced nitric oxide (NO) production - endothelium produces this, helps blood vessels relax
in HTN = the production of NO is reduced = vasodilation = vasoconstriction = can’t regulate inflammation
Oxidative stress - high BP increases oxidative stress, which damages endothelial cells and further reduces NO availability
Inflammation - chronic inflammation in HTN = endothelial cells become dysfunctional = pro-inflammatory and pro-thrombotic state
Creation of Hypertension
Obesity = adipocytokines = constant inflammatory state = hypertension
Blood Pressure and Vascular Damage
Blood pressure exerts shearing force (parallel movement) on blood vessels
Inner lining: endothelium (important for cardiovascular health - platelet formation, blood clotting, controlling resistance and blood flow, stops things from sitting to blood vessel wall, vasodilation)
NO promotes vasodilation
HTN = endothelium damaged due to turbulent flow = cholesterol particles are pulled under endothelium by immune system to be stored
Over time, hypertension damages blood vessels leading to chronic inflammatory process
Arteriosclerosis (hardening of vessels)
Atherosclerosis (fatty plaques in blood vessels)
Arteries with greatest shear force most effected (aorta, coronary arteries, branched arteries)
Bigger the artery = the stronger the force
Branching = strong shear force
What most heart disease is caused by
Atherosclerosis
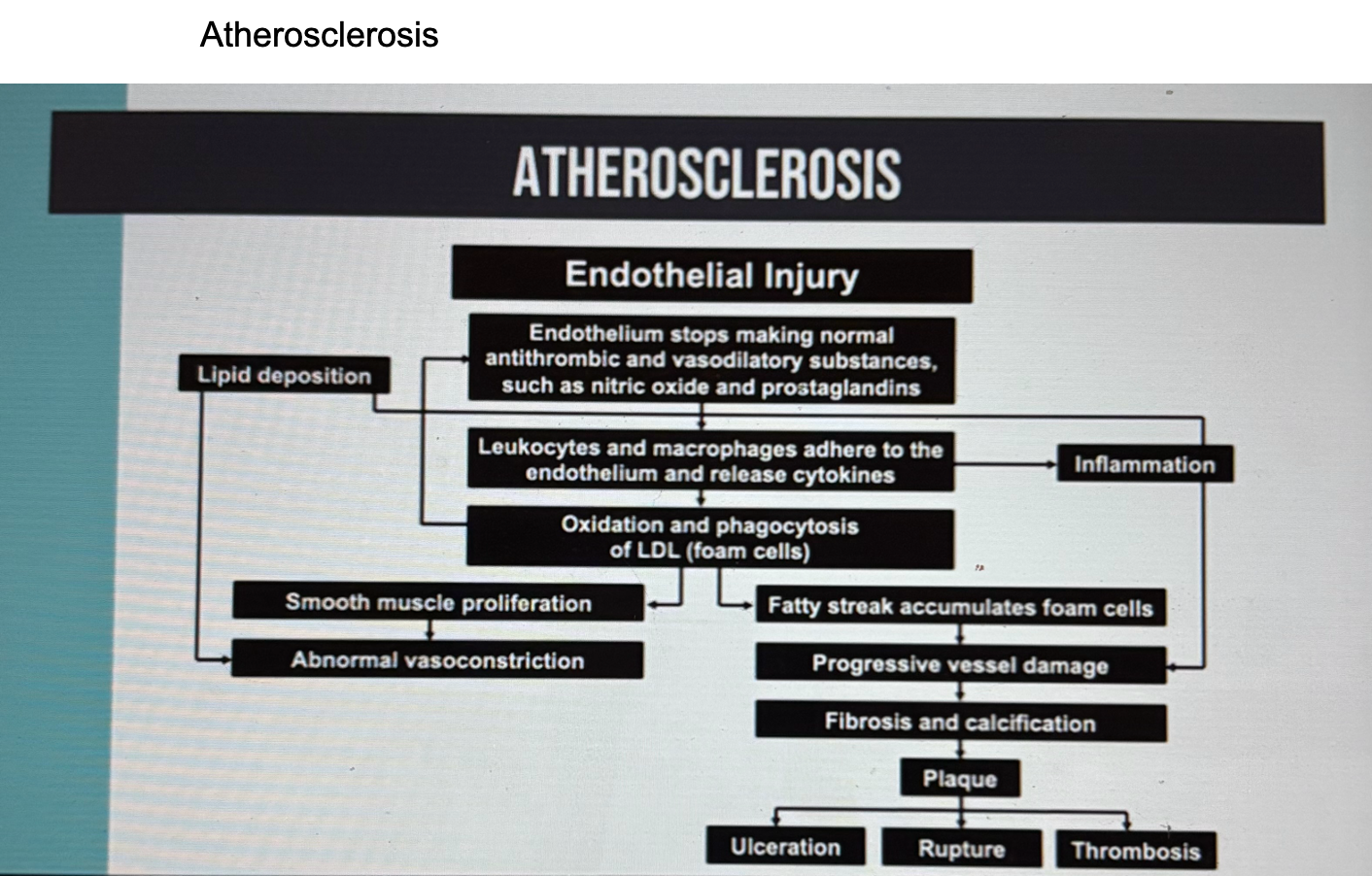
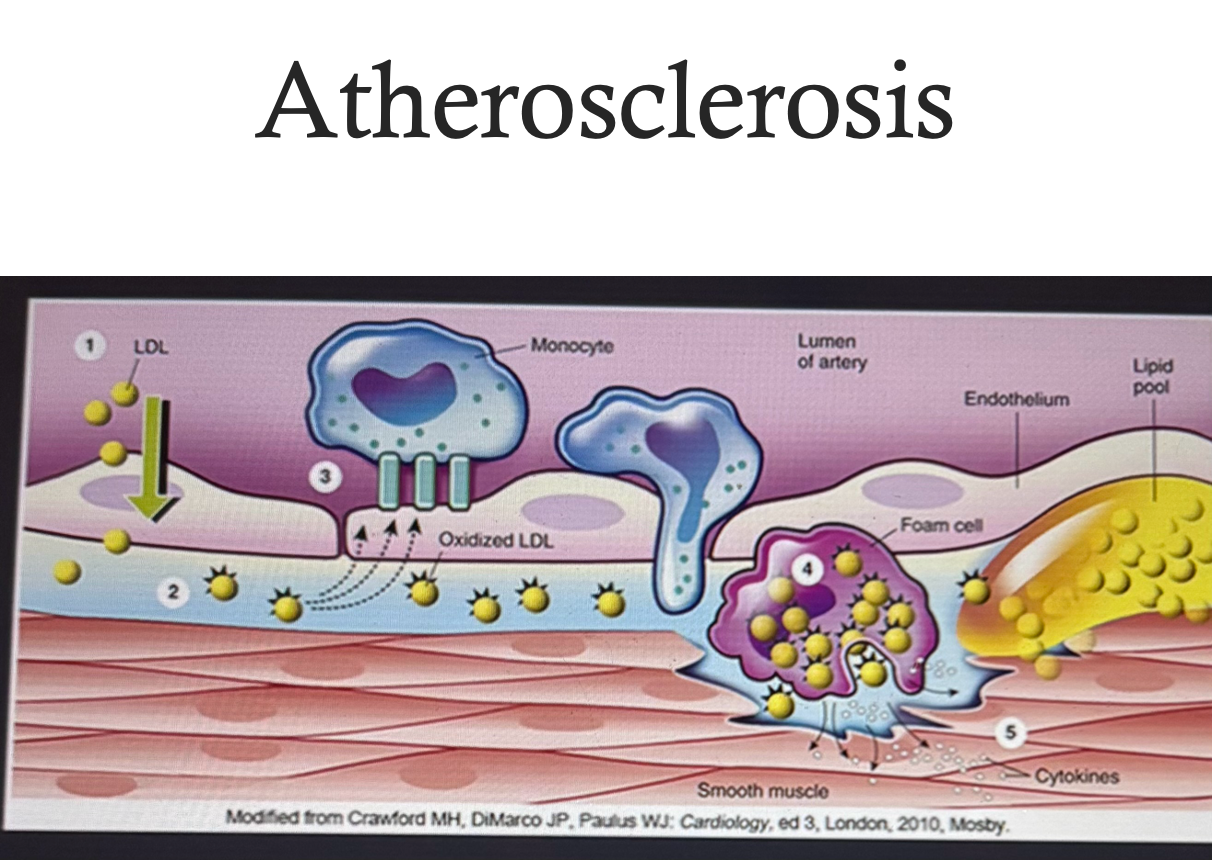
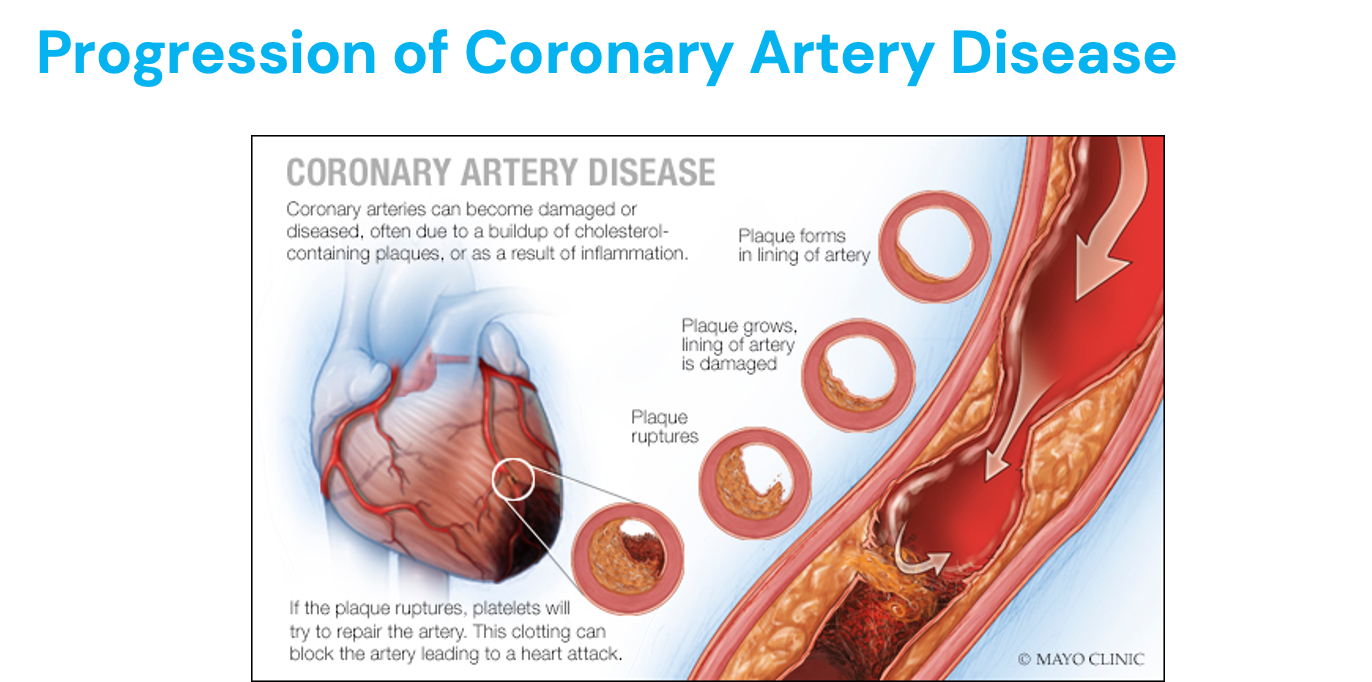
Creation of Atherosclerosis
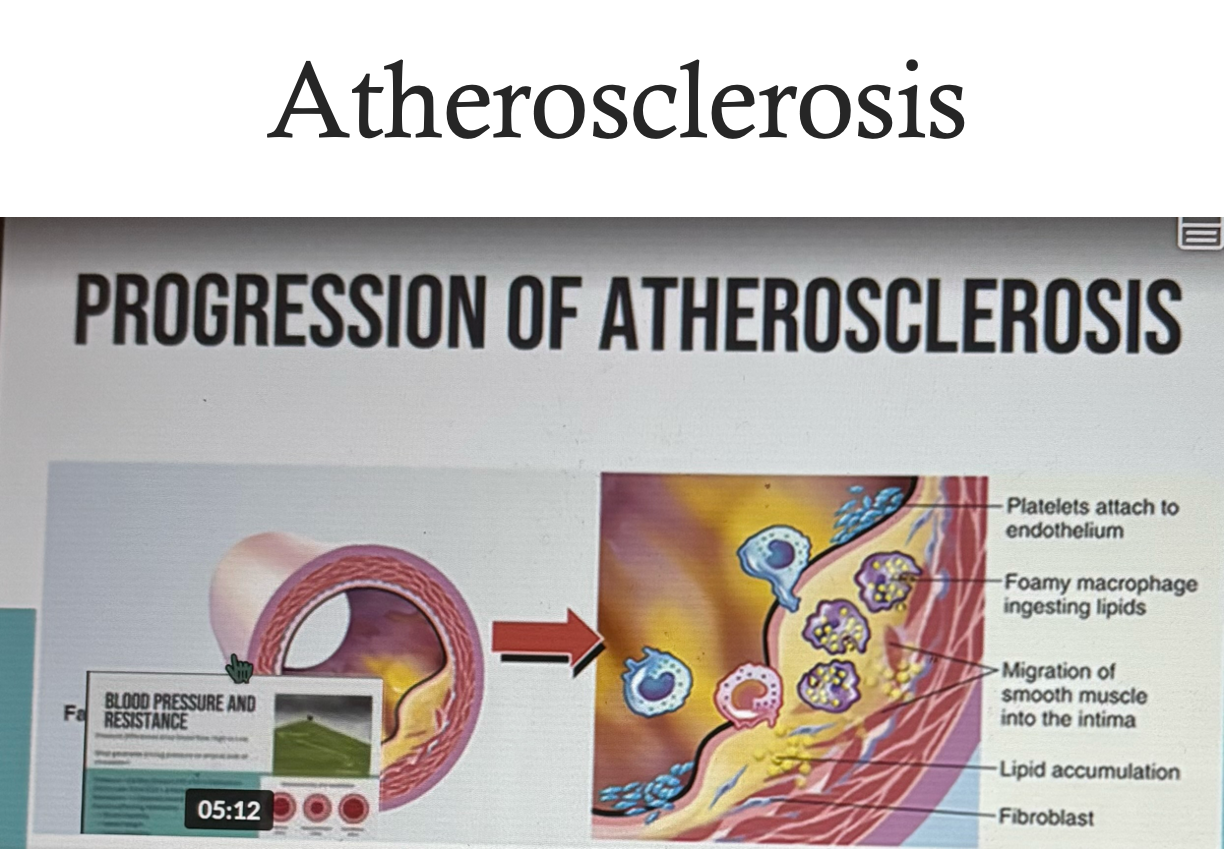
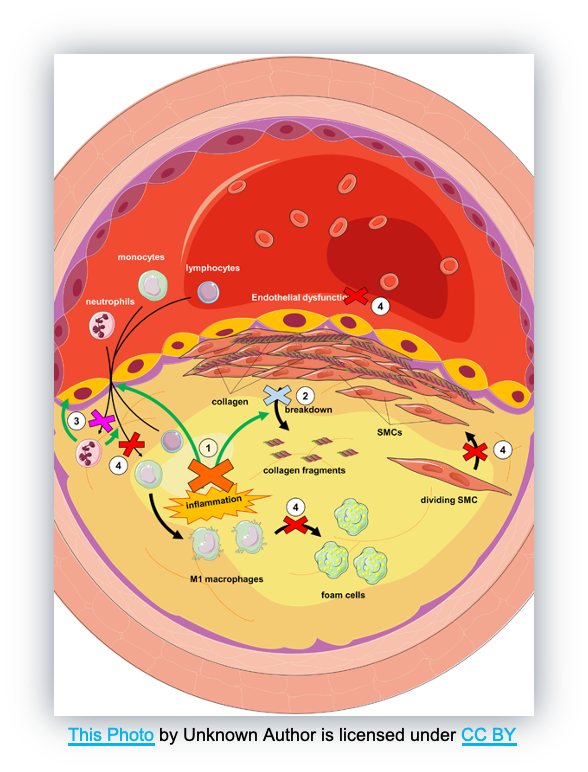
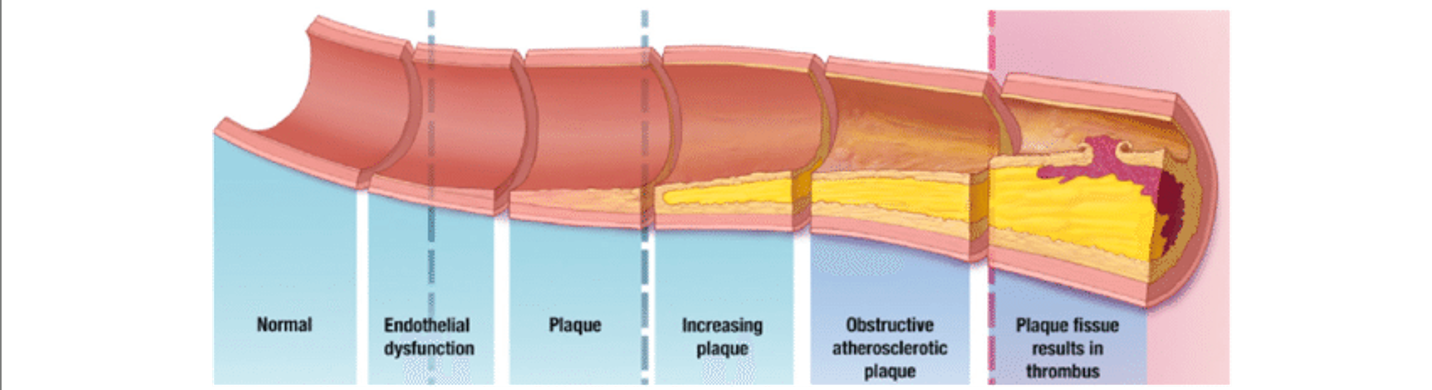
1) Things stick to damaged endothelium = release growth factors = becomes permeable = LDL go through and accumulate = macrophages eat LDL and become foam cells = foam cells release cytokines = more macrophages come to site
Lots of inflammation
2) Fatty streak process begins
Macrophages filled with LDL = foam cells = accumulation of foam cells (macrophages and T cells and T lymphocytes = release growth factors = collagen and smooth muscle cells form cap over fatty cap = artery becomes closed off
Patients becomes symptoms when 60-70% of blood vessel is closed off (ischemia - lack of blood flow to organs)
Angina (chest pain due to ischemia)
Fibrous cap can become eroded due to shear force = platelet form clot = blood flow shut off
Carotid artery = storke
Cornary arteries = heart attack
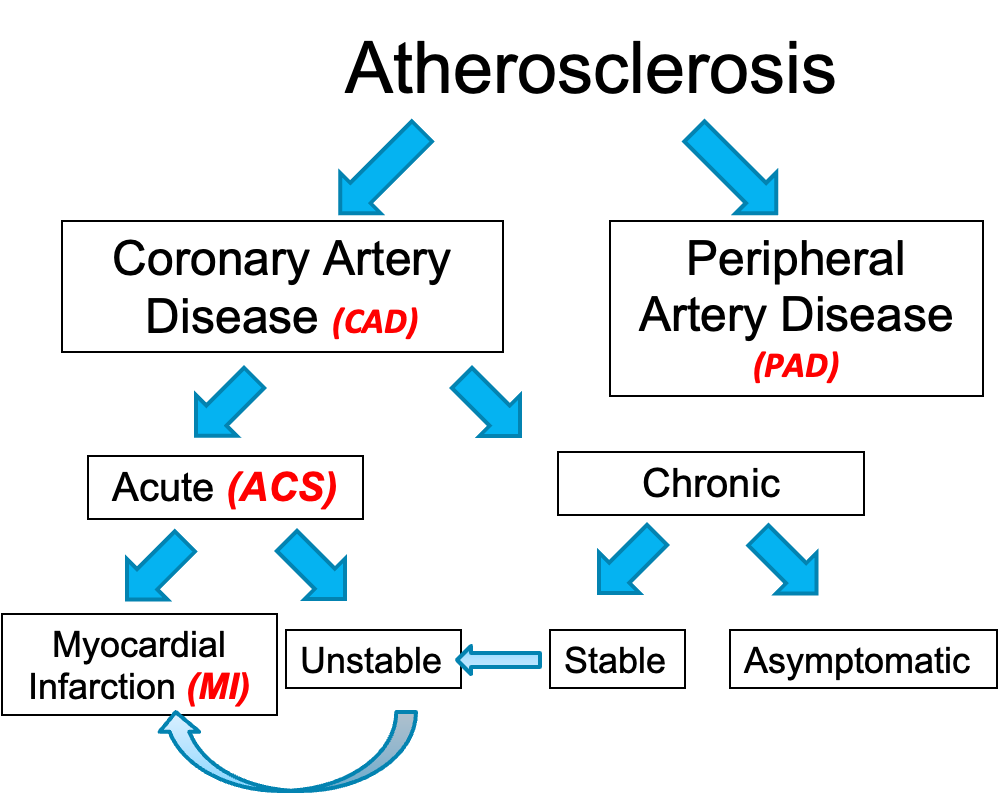
Atherosclerosis + Angina
Coronary artery disease (CAD) - atherosclerosis in coronary arteries
Acute (ACS)
Myocardial infarction (MI) - blood flow is completely blocked (tissue with undergo necrosis and die) servere
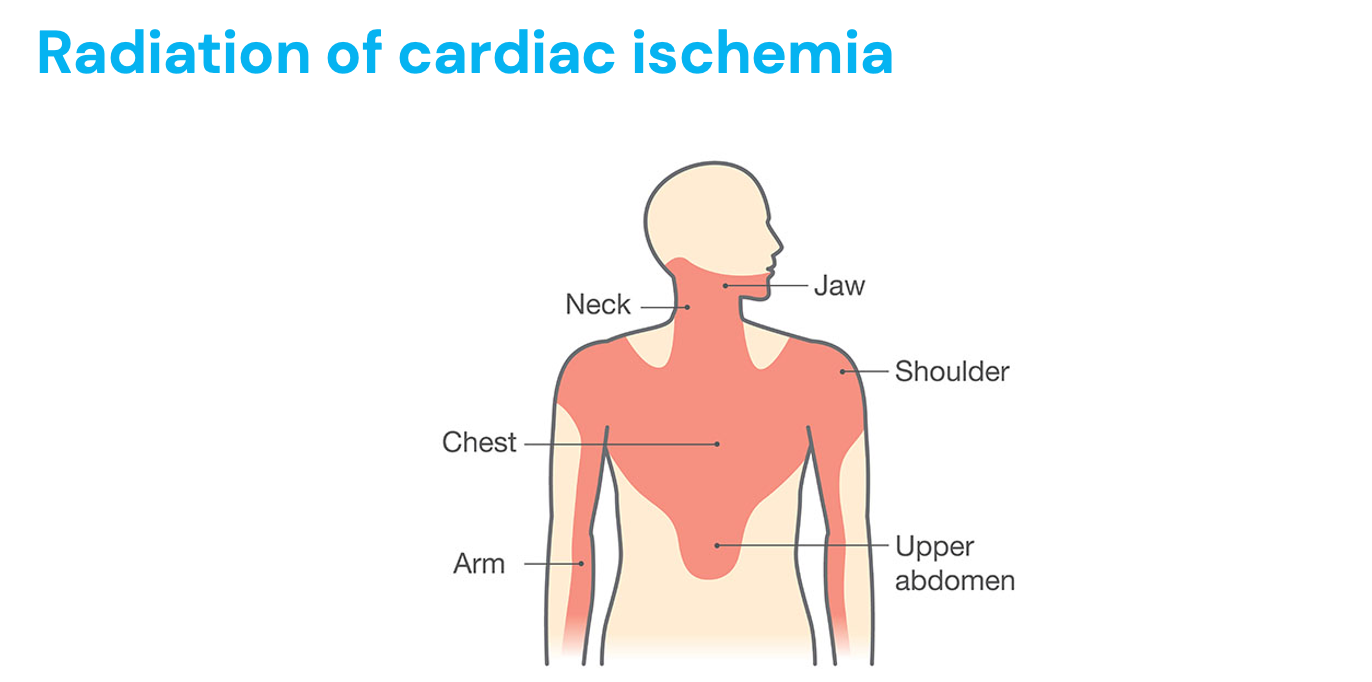
Chest pain, SOB, sweating (SNS), decreased BP, nausea/vomiting (ANS), pale, LOC, pain in back/stomach, left arm pain, jaw pain
Unstable - angina (chest pain due to decreased oxygen to heart) randomly appears (plaque in heart in so much that angina is unpredictable such as during rest)
Emergency
Chronic
Stable (can lead to unstable) - know when angina (chest pain) will occur such as with exercise (blood vessels vasoconstriction and plaque restricts blood flow to portion of the heart = chest pain)
Asymptomatic - no sides of symptoms but disease is still present
Peripheral artery disease (PAD) - atherosclerosis in legs (clotication - causes inadequate blood flow in peripheral due to plaque in arteries (which can cause increased pressure on arteries))
*CAD or PAD ultimately leads to tissue death of the heart muscle
Effects of Cigarette Smoke on Cardiovascular System
Increased sympathetic response
Increased systolic and diastolic pressure
Increased HR, CO, and coronary flow
Blood vessels vasoconstriction
More likely for aortic aneurysm - weakens vessels walls
Effects favoring thrombosis increases:
Platelet aggression
Platelet adhesiveness (more sticky, form blood clots (MI, stroke))
Plasma fibrinogen (protein involved in clot formation = thrombosis)
Blood viscosity (endothelial wall damage = no vasodilation, more blood cells = more likely to clot)
Decreased clotting time
*Daily aspirin helps
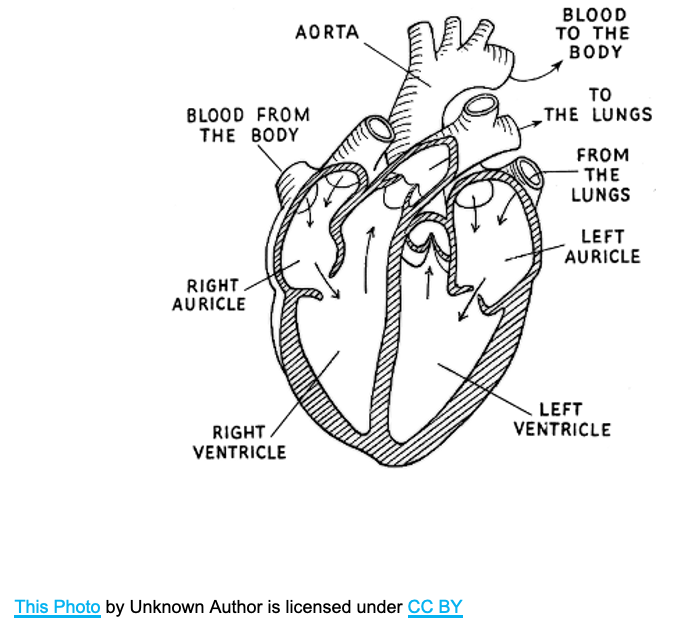
Heart Anatomy
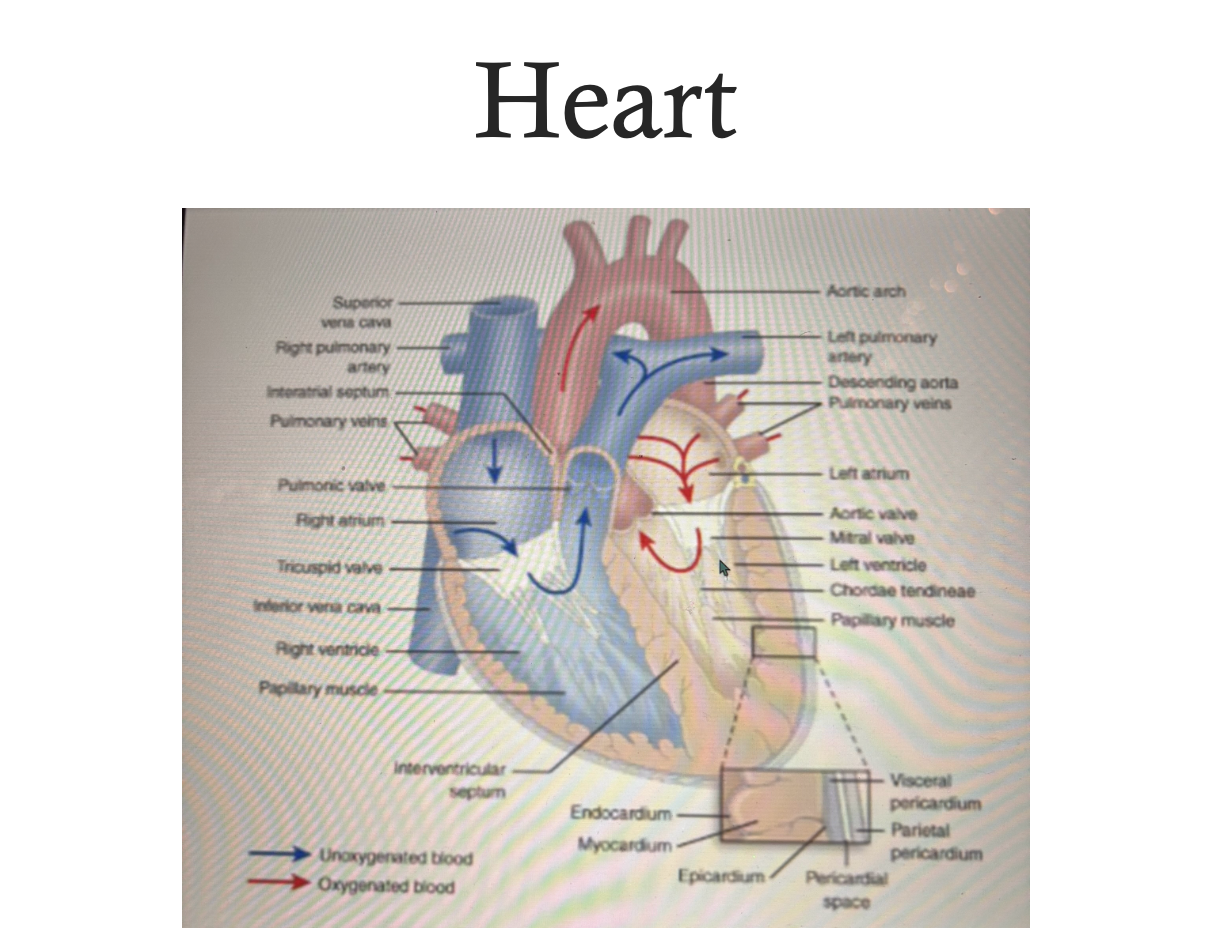
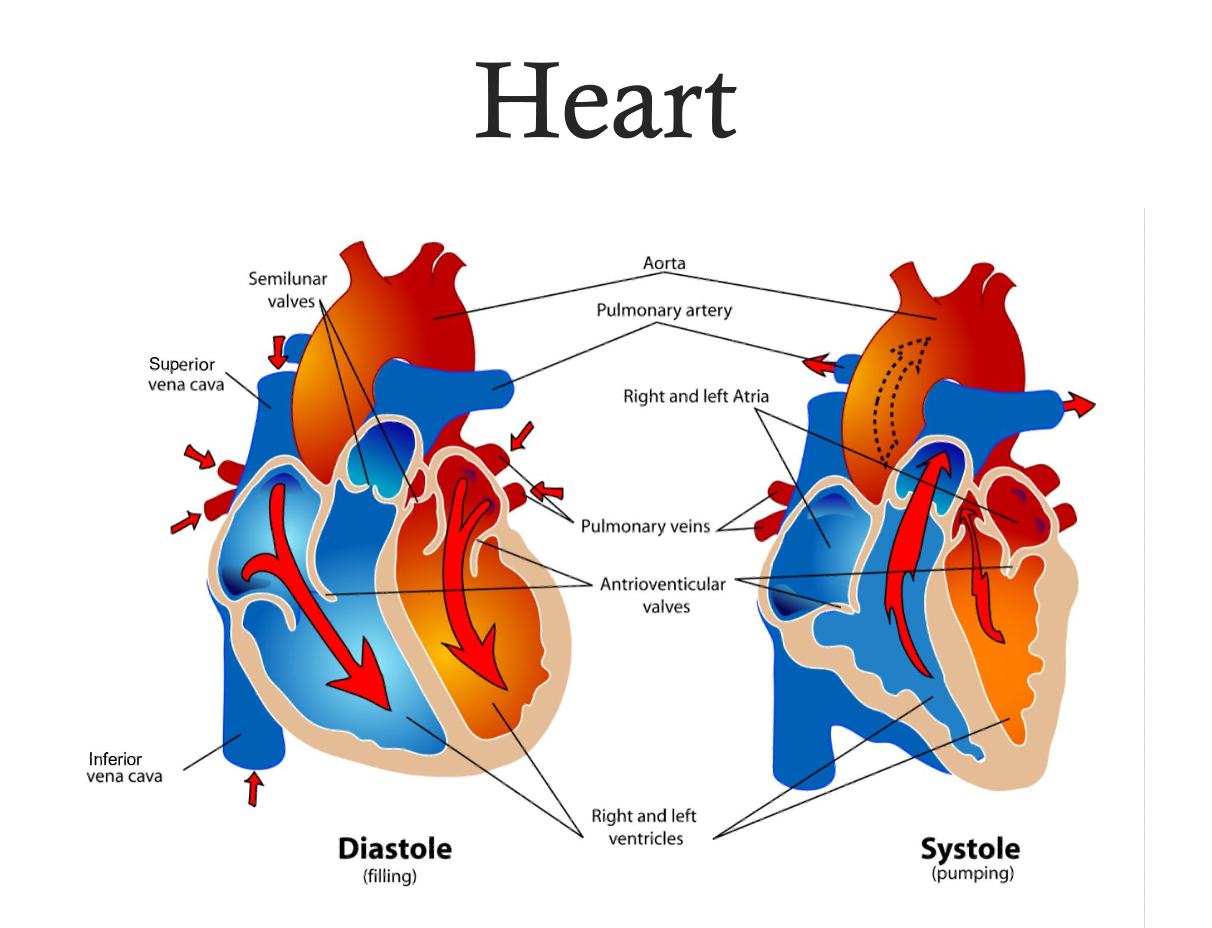
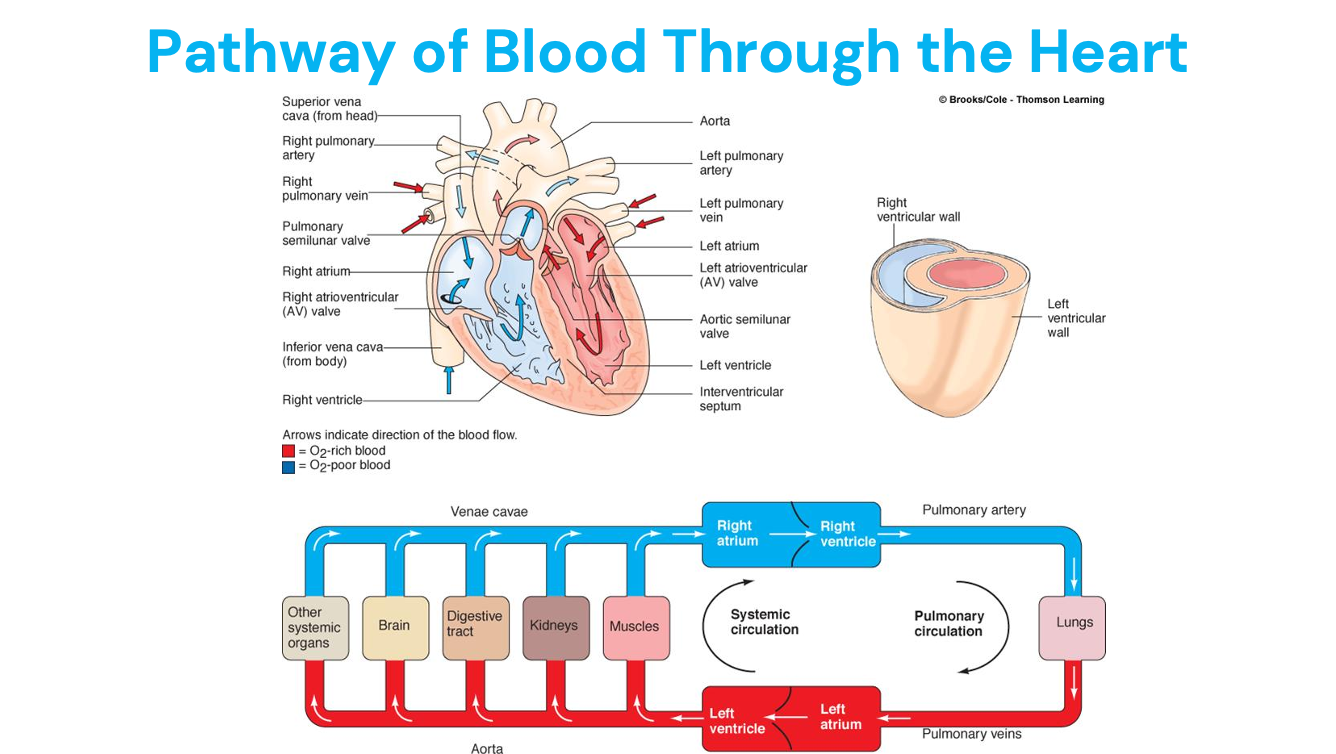
Pathway of Red Blood Cell Through the Heart
Deoxygenated vena cava = RA = tricuspid = LV = pulmonic = pulmonic arteries = lungs = oxygenated pulmonary veins = LA = mitral = LV = aortic valve = body
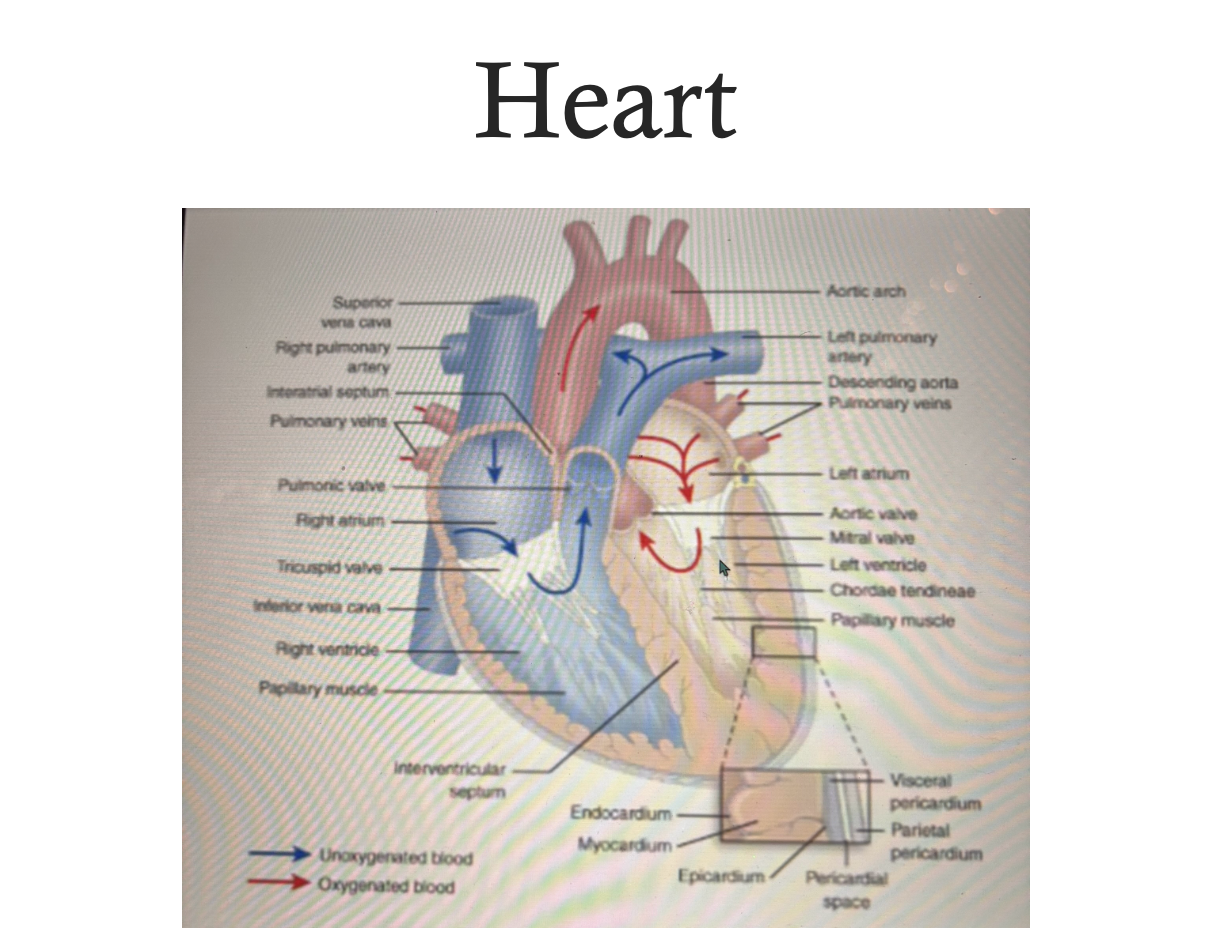
Heart as a Two-Sided Pump
Left side = to the body as systemic circulation
LV wall is thicker against RV (pumps against bodies systemic pressure)
Right side = to the lungs
Less muscle since only pumping to lungs
Pathway of blood:
Muscles
Kidneys
Digestive tract
Liver is gatekeeper for everything we digest (first pass effect - liver detoxifies, takes out of systemic circulation)
Brain
Other systemic organs
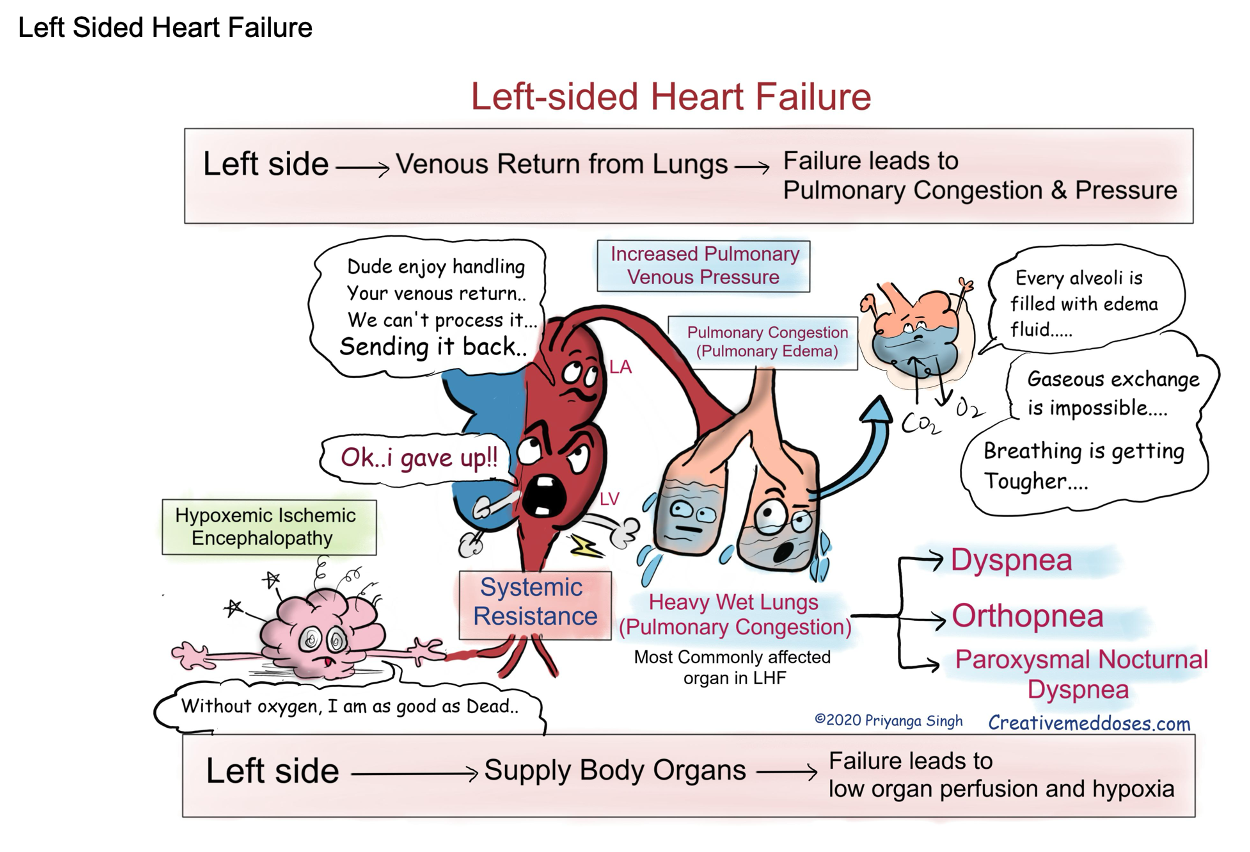
Congestive heart failure
LV can’t pump to body, backs up into LA into lungs
Increases hydrostatic pressure, lungs fill with fluid = pulmonary edema (difficulty breathing, fatigue, frothy sputum)
RV fails = blood backs up in RA and into vena cava and then systemic circulation = jugular venous distention = increases hydrostatic pressure = edema (peripheral edema - seen in legs due to gravity)
Back up into liver = hepatomegaly (enlarged liver)
Liver failure
Back up in slpeen = splenomegaly
Function vs. Dysfunction of Heart
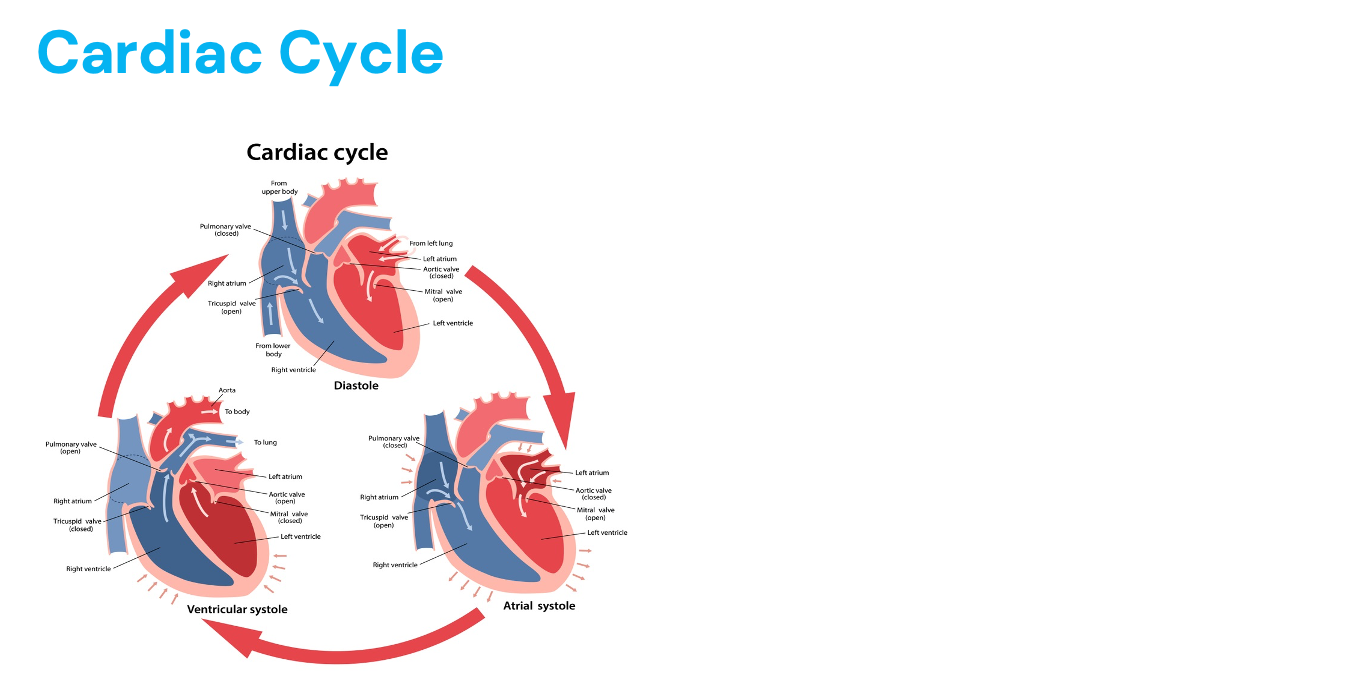
Diastole: ventricles relax
Dysfunction: ineffective filling
EX: cardiac tamponade (abnormal amount of fluid in pericardial sac around the heart - third spacing - compresses ventricle, decrease in CO, can’t fill = complication in heart surgery)
Systole: ventricle contract
Determines stroke volume (how much blood is being ejected from ventricle with each contraction)
Dysfunction: ineffective pumping
EX: aortic stenosis (aortic vavle doesn’t fully open = blood in ventricle can’t be pumped out fully)
Which valves are open
During systole: Pulmonic and aortic
During diastole: Tricuspid and mitral
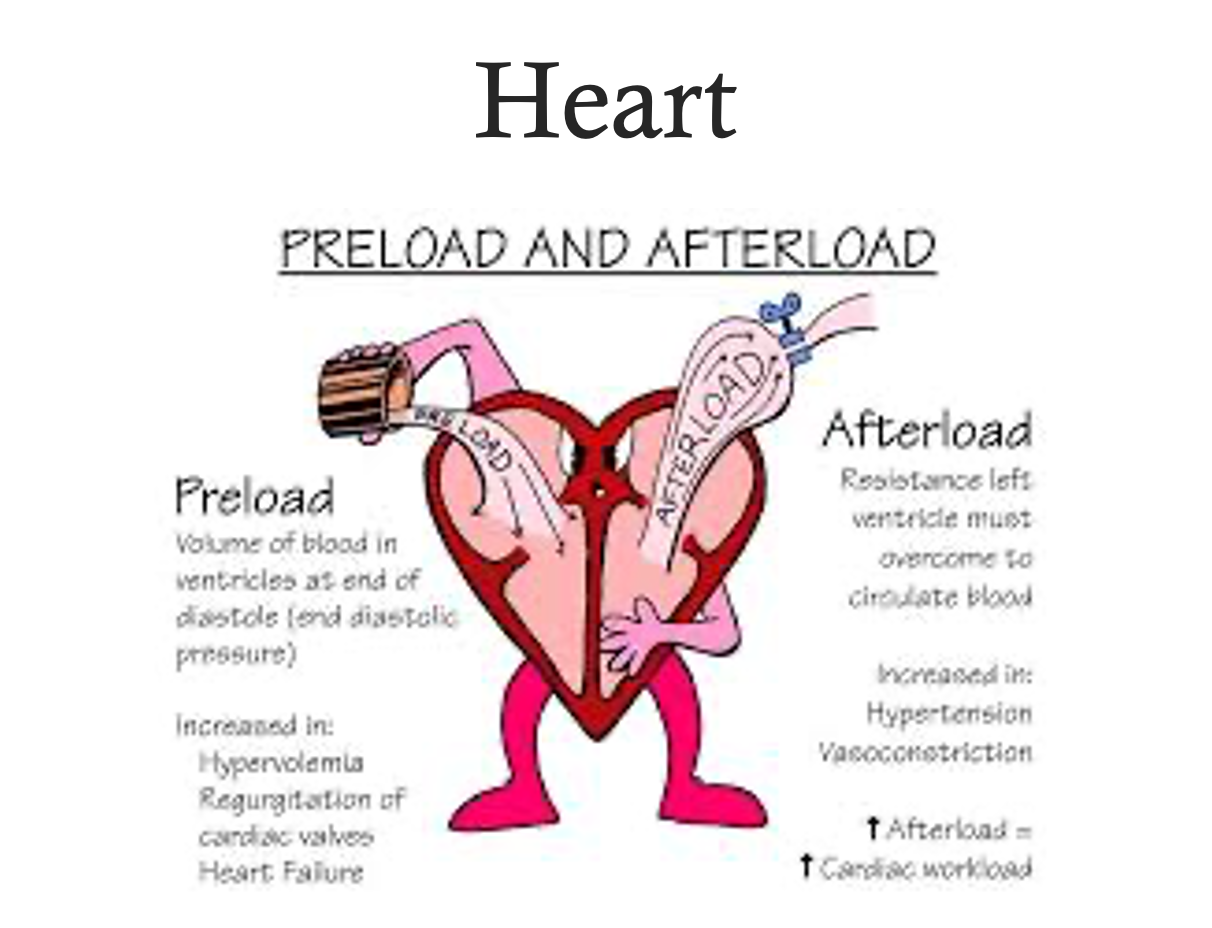
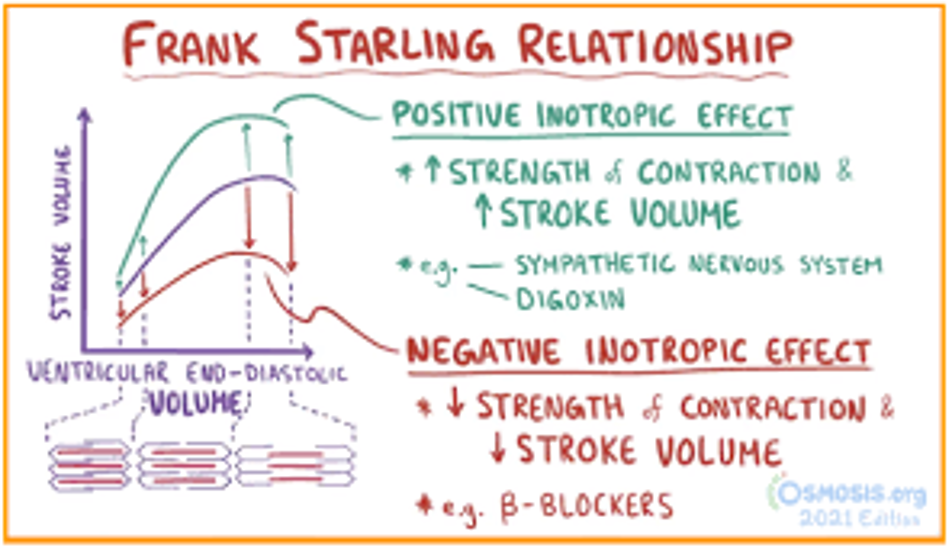
Preload vs. Afterload (NOT OPPOSITES)
Preload
End-diastolic pressure: the amount of stretch on the ventricle wall at the end of diastole (ventricle filling) BEFORE VENTRICLE CONTRACT
Frank Starling Mechanism = the greater the stretch on myocardium, the stronger the contraction (like a rubber band)
Increased by having more fluid
Increase fluid volume (IV)
Increase venous return through vasoconstriction (blood coming back to heart) - SNS and RAAS system
Decrease…
Vasodilation (not as much blood back to heart)
Bad = too much fluid in interstitial space, less blood in blood vessels
Diuretics that eliminate excess fluid volume
Hypervolemia would increase
Frank-Starling Mechanism - the greater the stretch, the stronger the recoil
Afterload
Work (or force) required of LV to move (eject) blood into the aorta
Higher pressure in aorta the heart has to overcome= higher the afterload
Blowing up a ballon (think resistance)
Increased = vasoconstriction, hypertension
Decreased = vasodilation
Increases ventricular wall tension, over time can eject blood (and impact ejection fraction)
Shock = drop in blood volume = less blood to heart (preload decreases) = blood pressure drops (afterload decreases)
Volume overload (hypervolemic) = preload increases (more blood volume to heart) = afterload increases = increases blood pressure
Decreasing work of heart (MI) = nitroglycerin = dilates blood vessels = decreases BP = decreases afterload and preload
Heart failure = ventricles hold more blood = preload increases = heart works harder to move more fluid
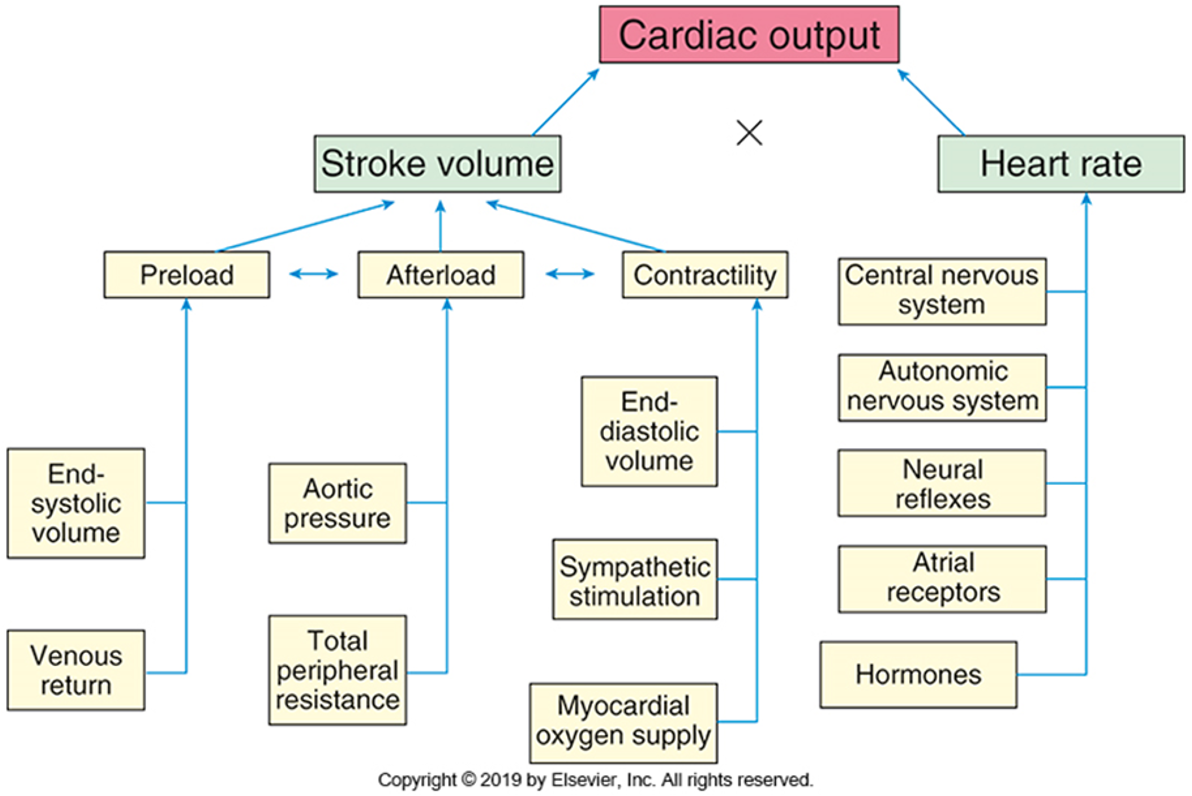
Cardiac Output
CO = the heart’s pumping output (L/min) normal = 5-6 L/min
CO = SV x HR
Stroke volume = how much the heart beats out in each beat (mL/beat)
Preload - initial stretch, fullness before contraction
End-systolic volume = whats left after systole
Venous return = amount of blood back to body
How much in ventricle
Increased preload = increases stroke volume
Vasodilation = decreases preload
Hypervolemia increases
Afterload - resistance (hypertension, vasoconstriction) heart overcome to eject blood to body
Total peripheral resistance
Aortic pressure
Aortic stenosis can increases
Increases cardiac workload
Increases ventricular wall tension (impact ejection fraction)
Contractility = how strong the heart beats
End-diastolic volume = whats left after diastole
Sympathetic stimulation (more forceful)
Myocardial oxygen supply (more O2 = more force)
Heart rate - beats per minute
CNS - pons and medulla regulate the rate and rhyth,
ANS = SNS (raises HR) and PNS (lowers HR)
Neural reflexes = startle reflex (jump in heart rate)
Barorecptors = increased stretch = PNS = decreases heart rate = vasodilation
Atrial receptors = stretch receptors = speed up heart rate to prevent pooling
Hormones
Epipinephrine
Thyroid = too much = tachycardic
You are taking care of a patient who has been diagnosed with atrial fibrillation. You are doing your morning assessment and notice their heart rate has increased to 200 bpm. Blood pressure has decreased from 110/78 to 88/60.
Using the CO = SV x HR, what should the HR in the case do to cardiac output
Why is BP low?
Ventricles aren’t filling due to high HR, have less time to fill (diastole shortened, systole doesn’t change) = smaller SV (less volume in ventricles)
Atrial fibrillation = atria quivering, not pump
HR increases = diastolic filling time drops = CO decreased = low BP
Needs cardioversion to jolt heart into normal rhythm
End Diastolic Volume (EDV)
Amount of blood in heart chamber at end of diastole
Determine preload
120 mL
Weak heart = EDV increases
Small aortic opening = increased EDV
Preload increases EDV, increases SV
End Systolic Volume (ESV)
Amount of blood remaining in ventricle after systole
Heart does not empty completely with each beat
Weak heart = increased ESV
Small aortic opening = increased ESV
Stroke Volume (SV)
Amount of blood ejected from chamber with each beat
EDV - ESV
Weak heart = decreased SV
Small aortic opening = decreased SV
If stroke volume goes up + heart rate goes up = cardiac output goes up
Influenced by the amount of blood that returns to right atrium from venous circulation (RIGHT SIDE) and left atrium (LEFT SIDE) from pulmonary veins
Higher SV increases workload of the heart…typically due to too much VOLUME
Tachycardia INCREASES cardiac oxygen demands, workload, and DECREASES stroke volume because there is less time for the ventricles to fill
Goal of medication therapy with any cardiac patient is to DECREASE cardiac workload through manipulating SV, HR, preload, afterload, and contractility
Ejection Fraction (EF)
Percentage of EDV ejected from heart with each beat
55-75%
Left side of heart
Weak heart = EF decreased
Small aortic opening = decreased EF
Increased TPR = decreases SV - hard to pump blood out of heart
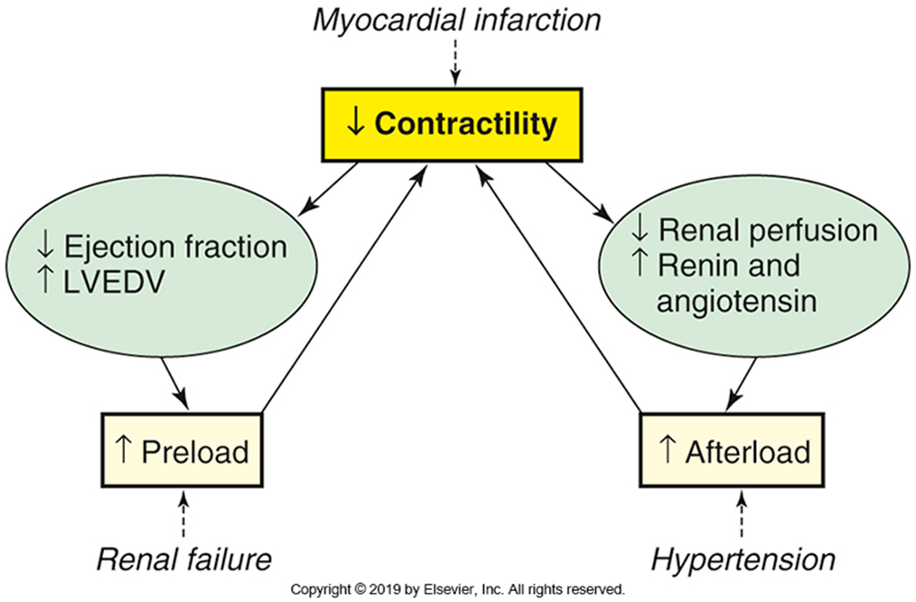
Heart failure: An MI kills heart muscle and affects its ability to pump effectively (decreases contractility)
Heart failure decreases ejection fraction and increases our left ventricular end diastolic volume, which increases our preload - which will lead to renal failure
OR we decrease our renal perfusion, which triggers our RAAS system and increases our blood pressure (increasing afterload and causes HTN)
Low EF = systolic HF
Low EDV = diastolic HF
Increase in preload = increase in blood return to heart
EX: 100 ml of blood in the LV at end of diastole (EDV), and 60 mL of blood pumped with each beat during systole (SV), EF = 60%
EDV around 120 mL
ESV around 50 mL
SV would be 70 mL
EF = 59%
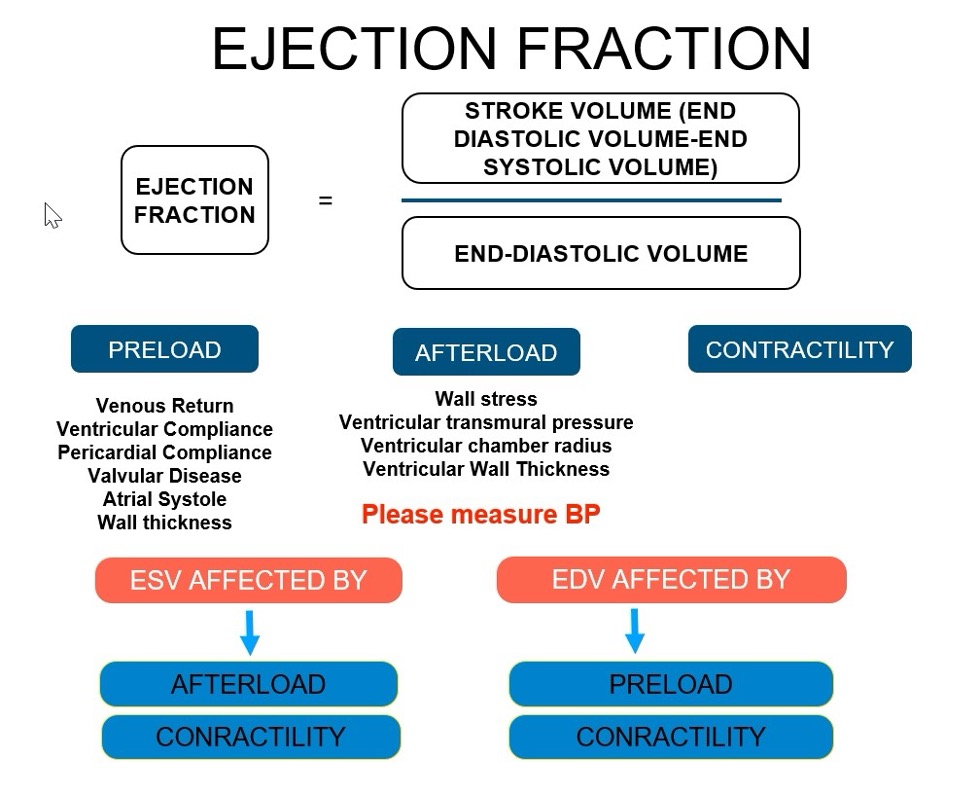
EF (%) = ?
(SV/EDV) x 100
Heart
“Plumber”
"Electrician”
How many sub-specialties?
Coronary artery disease
Heart failure
Rhythm disorders
Valvular disease
Normal Heart vs. Heart Failure
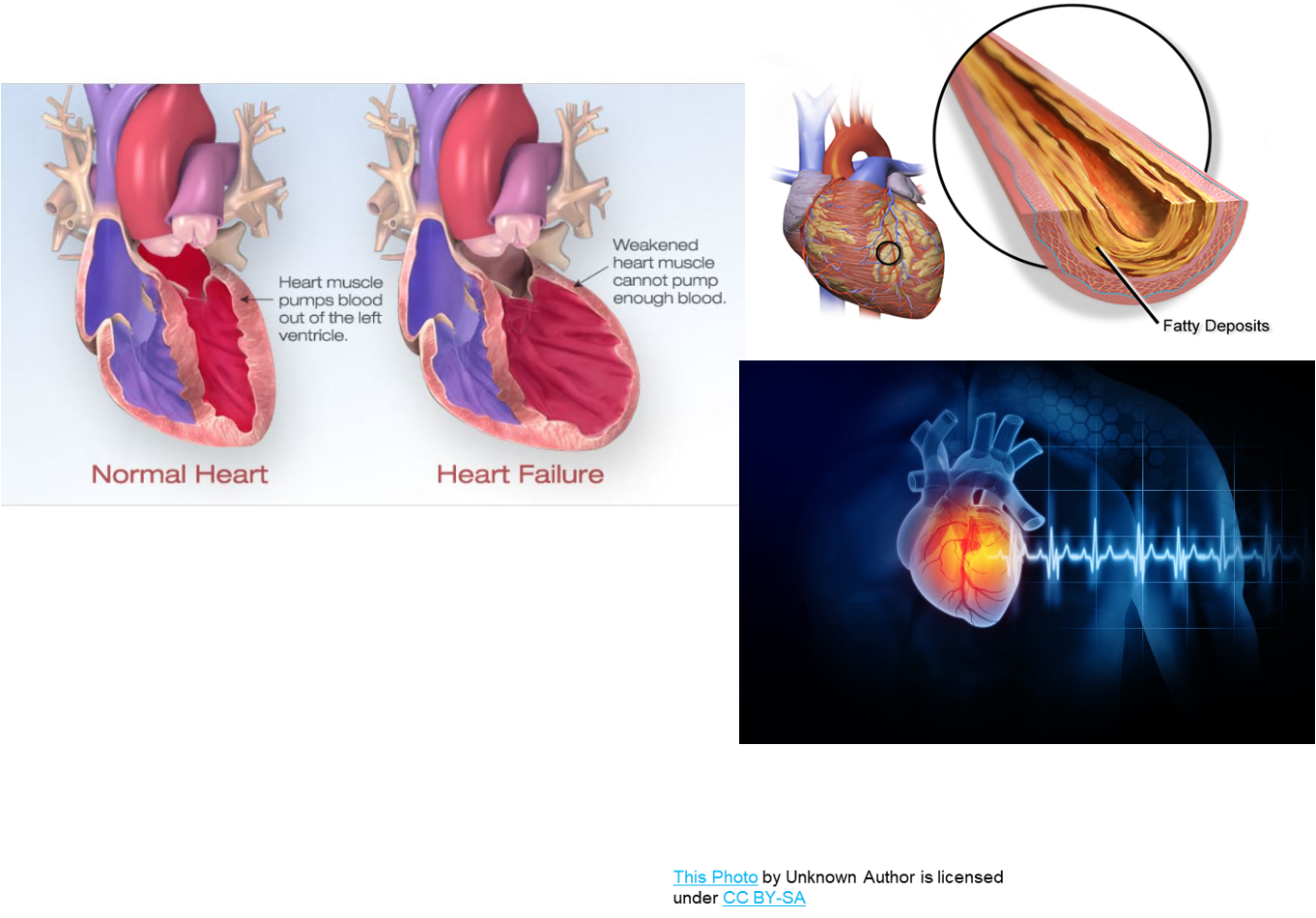
What are the functions of the cardiovascular system?
Delivery of oxygen and nutrients needed for metabolic processes to the periphery, and removal of wastes
Circulates hormones
Controls body temperature
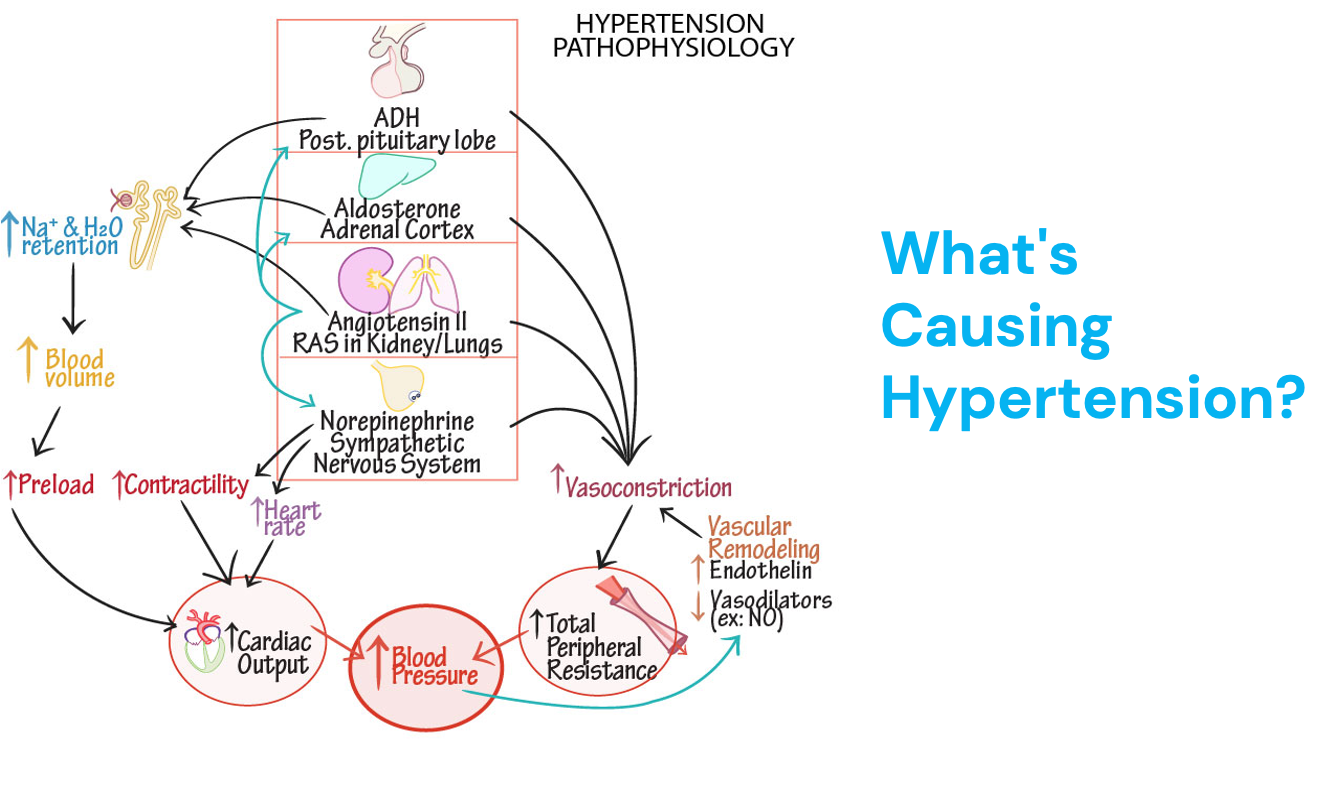
Pathophysiology of HTN
Diagnosed over a series of office visits and/or with continuous blood pressure monitoring
Increased risk for
Cardiovascular disorders
Ischemic heart disease and stroke
Peripheral arterial disease
Renal disease
Heart failure
Stiffening of arteries with age can cause, as well as sodium retention that occurs with age
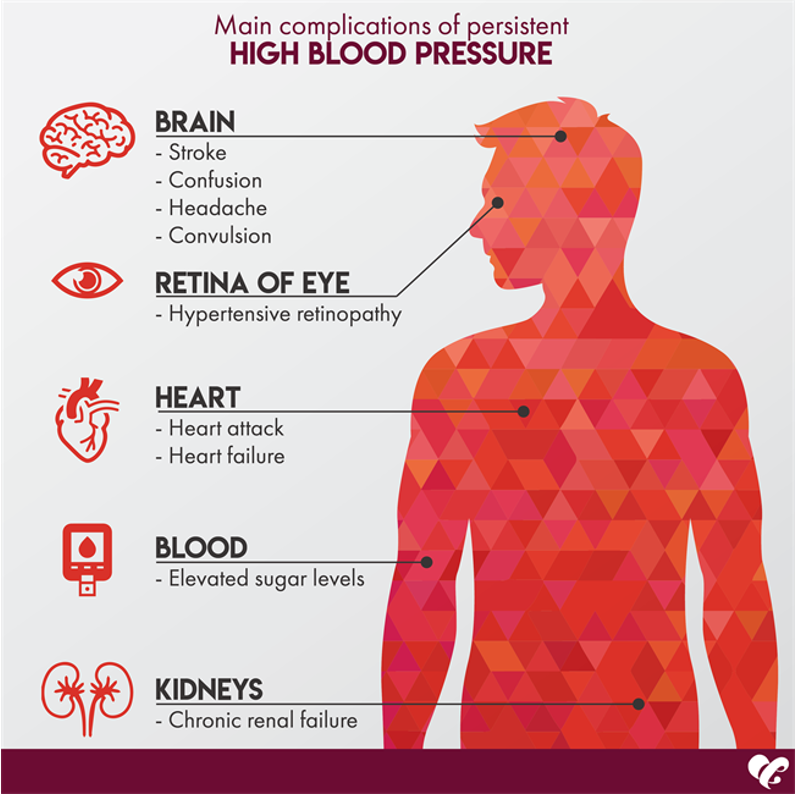
Complications of Persistent HTN
Risk Factors of Atherosclerosis
Hypercholesterolemia
Elevated LDL
Age
Family history
Biological males
Smoking
Vasoconstriction
Damages endothelial lining
Obesity
Hypertension
Diabetes
Atherosclerosis:
Cellular injury in smooth endothelial wall
Inflammatory cells are attracted to the area and gather
Causes gathering of lipids and smooth muscle tissue that begin to collect
Lipids/smooth muscle form a hard plaque in the vessel
Progression of Atherosclerosis
Thrombosis is the formation of the clot, the thrombus is the clot and the embolism is the clot on the move
Can be slowed or reversed
>75% = symptoms
Heart Anatomy
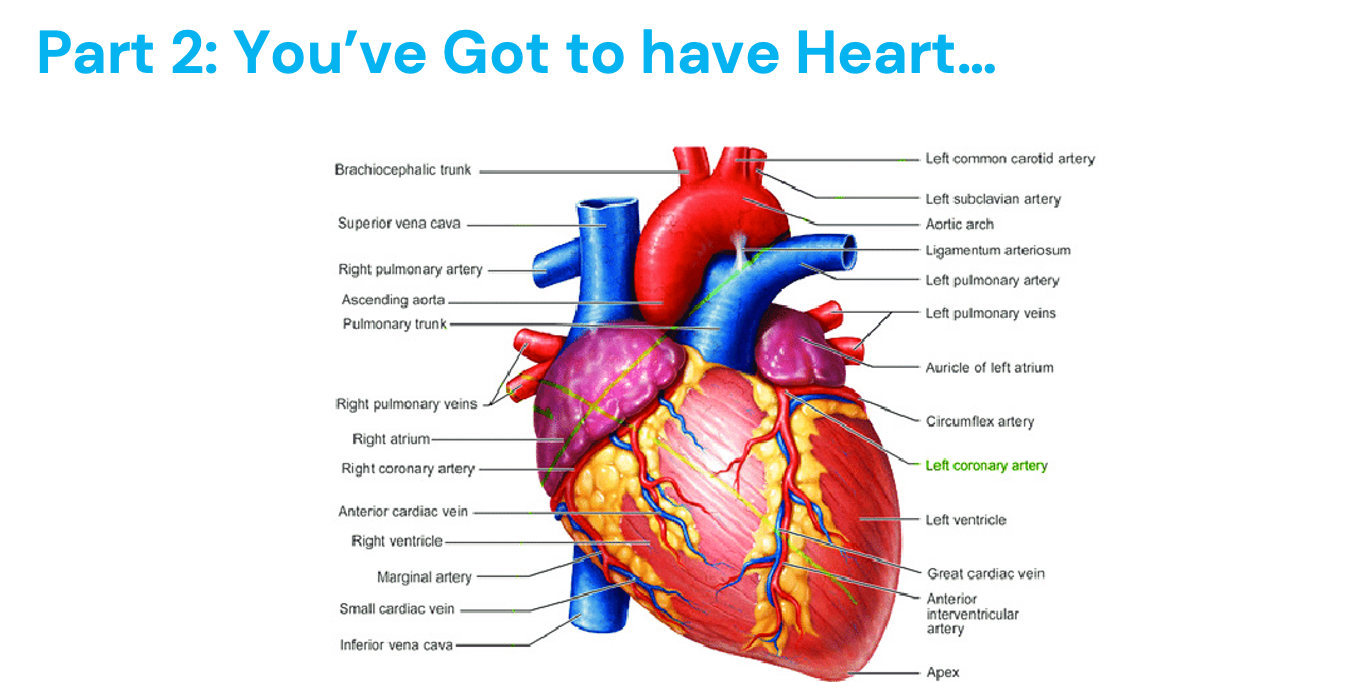
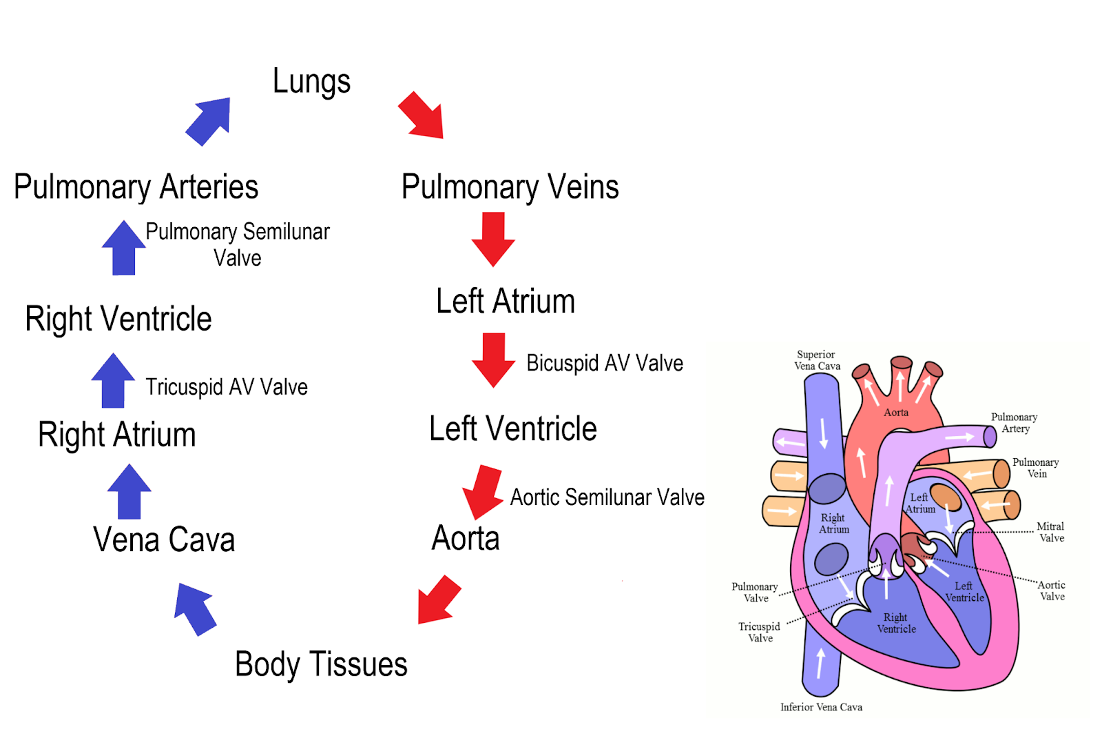
Pathway of Blood Through the Heart
AV and SL valves close and open at the same time
Left side of heart failures:
Blood backs up = wet lungs
Cardiac Cycle
Systole: ventricles contracting (pumping)
Top number for blood pressure
Atria and ventricles contract at same time
Atria stay open
Takes same amount of time
Diastole: ventricles are relaxed (filling with blood)
Bottom number for blood pressure
Lost due to to:
Stiff ventricles
Dysfunction of valves and veins
Heart rate
Over 180 = pass out
Time can change (atheltes have more time of filling)
Frank Starling Relationship
More preload = contraction is stronger
HF = overstretch = lose elasticity of heart muscle
Inotropic = strength of contraction
Cronotropic = how fast heart is beating
You are taking care of a patient who has been diagnosed with atrial fibrillation. You are doing your morning assessment and notice their heart rate has increased to 200 BPM. Blood pressure has decreased from 110/78 to 88/60.
Using the CO = SV x HR, what should the HR in this case do to cardiac output?
Why is BP low?
HR increase should increase CO
Not enough time for the ventricles to fill
How does hypertension affect afterload? What would be the consequences for the heart? Why might someone with long-standing hypertension develop heart failure?
Afterload is the resistance the heart must overcome to eject blood from a given chamber. Hypertension increases afterload in the ventricle because the heart must generate more force to overcome the elevated blood pressure and eject blood from the chamber. This could create afterload in the left ventricle (if it is systemic hypertension/elevated blood pressure in the aorta) or the right ventricle (if it is pulmonary hypertension/elevated blood pressure in the pulmonary artery leading to the lungs). Another example of a process that could increase afterload would be valve stenosis. For example, in aortic stenosis, the heart must generate more pressure to push blood through the narrowed heart valve.
If the heart has to continually work against high blood pressure, the cardiomyocytes (heart muscle cells) will hypertrophy to compensate, just like any other muscle that has to work against increased resistance. Unfortunately, the hypertrophy of cardiomyocytes is pathologic and leads to ventricular wall thickening and stiffness which decreases the chamber size. Both of these factors can contribute to diastolic dysfunction (the ventricle has a filling issue) and leads to heart failure.
A patient has been diagnosed with left sided heart failure and an ejection fraction of 33%. What is the significance of this EF? How would this patient's left ventricular end-systolic volume (ESV) compare to someone with a healthy heart? Would the ESV be increased or decreased? Explain your answer.
Ejection fraction tells us what percentage of the EDV is pumped out of the heart with each beat. Thus, ejection fraction is very much related to cardiac output. A normal EF is somewhere between 55%-70%. So a person with a normal EF who starts with an EDV of 100 mL will pump out between 55 and 70 mL of blood during systole. A person with an EF of 33% has systolic dysfunction. If they start with 100 mL of blood, then they only pump out 33 mL of blood during systole, which results in a subsequent drop in cardiac output.
ESV in the left ventricle would be increased because more blood would be remaining in the ventricle at the end of systole. When the heart relaxes during diastole, the heart will continue to fill as normal, and the blood entering from the atria during diastole is added to the excess blood already in the ventricle. This will lead to increased ventricular pressures, which cause excessive stretch of the ventricle. The increased stretch of the myocardium will lead the atria and ventricles to release ANP and BNP respectively, which increases sodium (and therefore water) excretion in the kidneys.
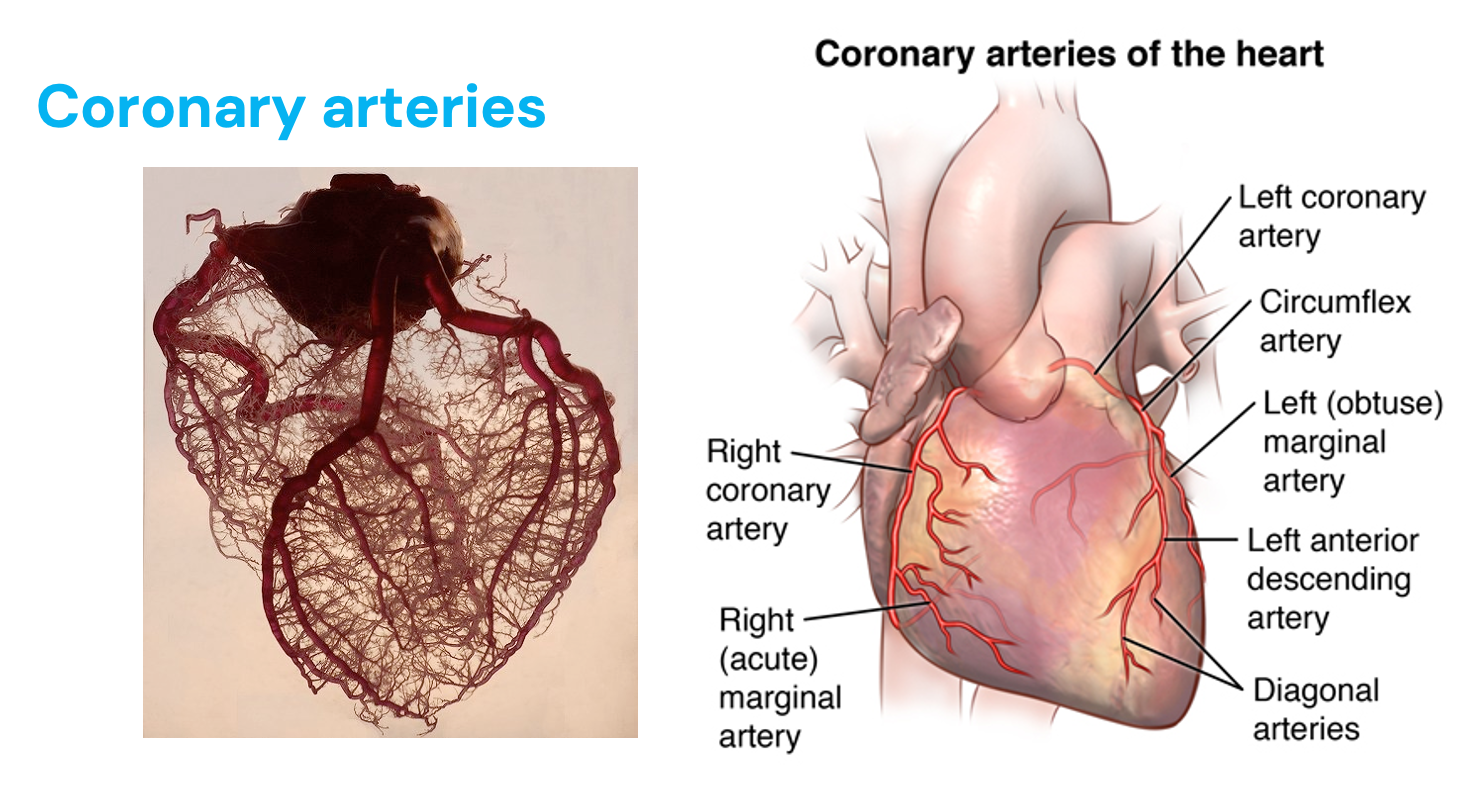
Coronary Arteries
RCA = SA node, AV node pacemakers of the heart
Myocardial infarction = clot on plaque
Cardiomyocytes starved of oxygen = angina
Originate in aorta (blood high to low - aorta has highest pressure)
Blockage affects things downstream (higher up the worst)
Left CA blockage = widowmaker (supplies smaller amount of oxygen to heart)
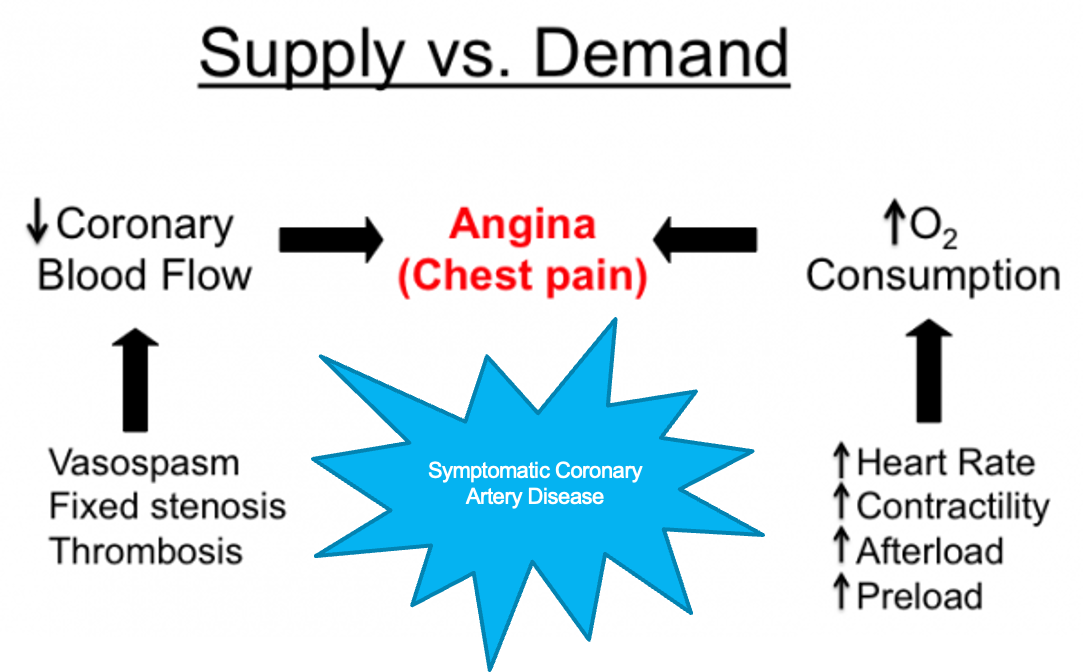
Supply vs. Demand
Lack of oxygen and then tissue death, you get chest pain even at rest
Angina = chest pain, substernal, radiate to left arm or jaw
MI = clot on plaque
Goals of Heart Related Symptoms
Decrease platelet aggregation - give aspirin
Decrease preload and afterload - give nitrates
Decrease oxygen demand - give oxygen
Decrease SNS involvement and pain - give morphine
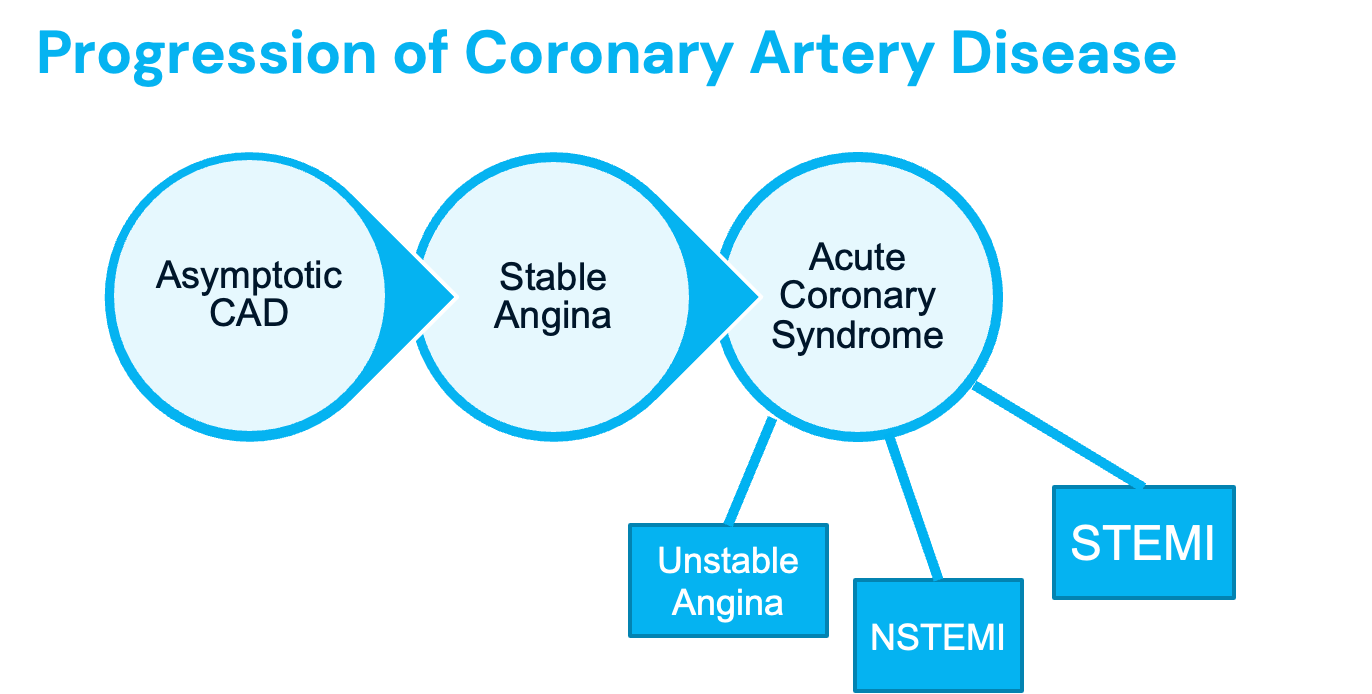
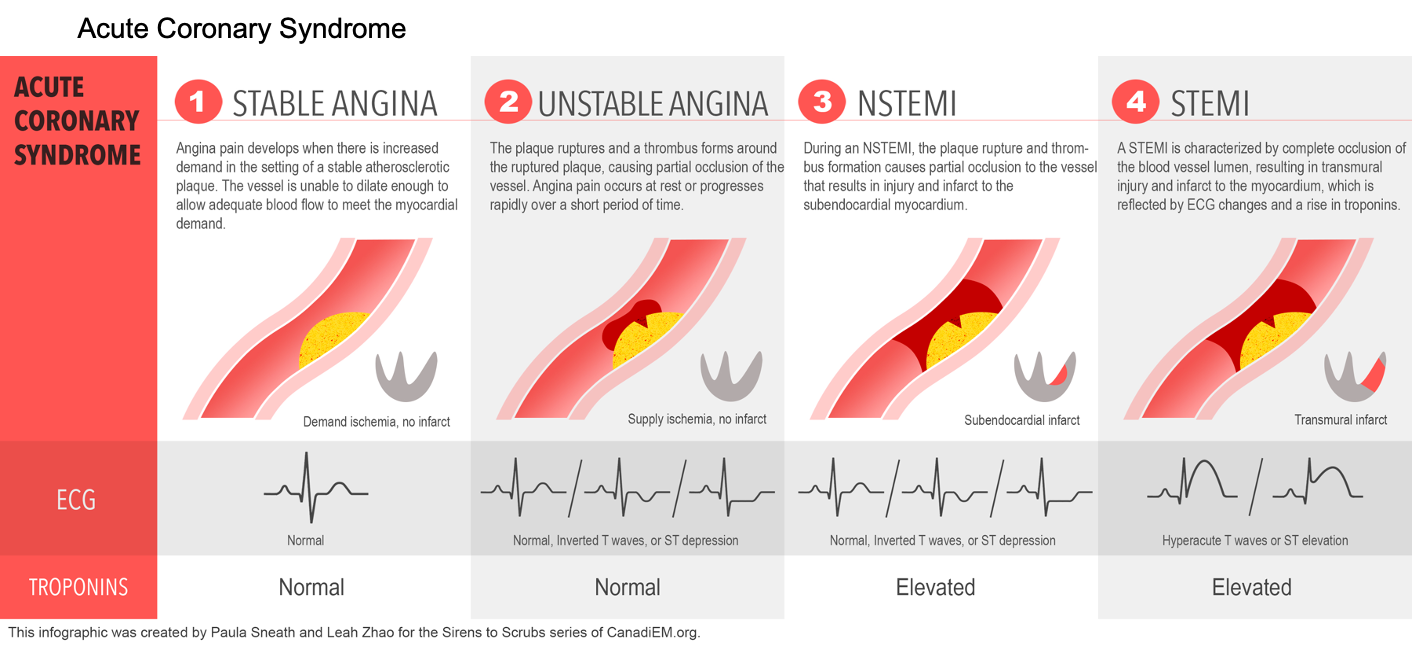
Progression of Coronary Artery Disease
May get complete obstruction of the vessel, cutting off the oxygen supply (STEMI)
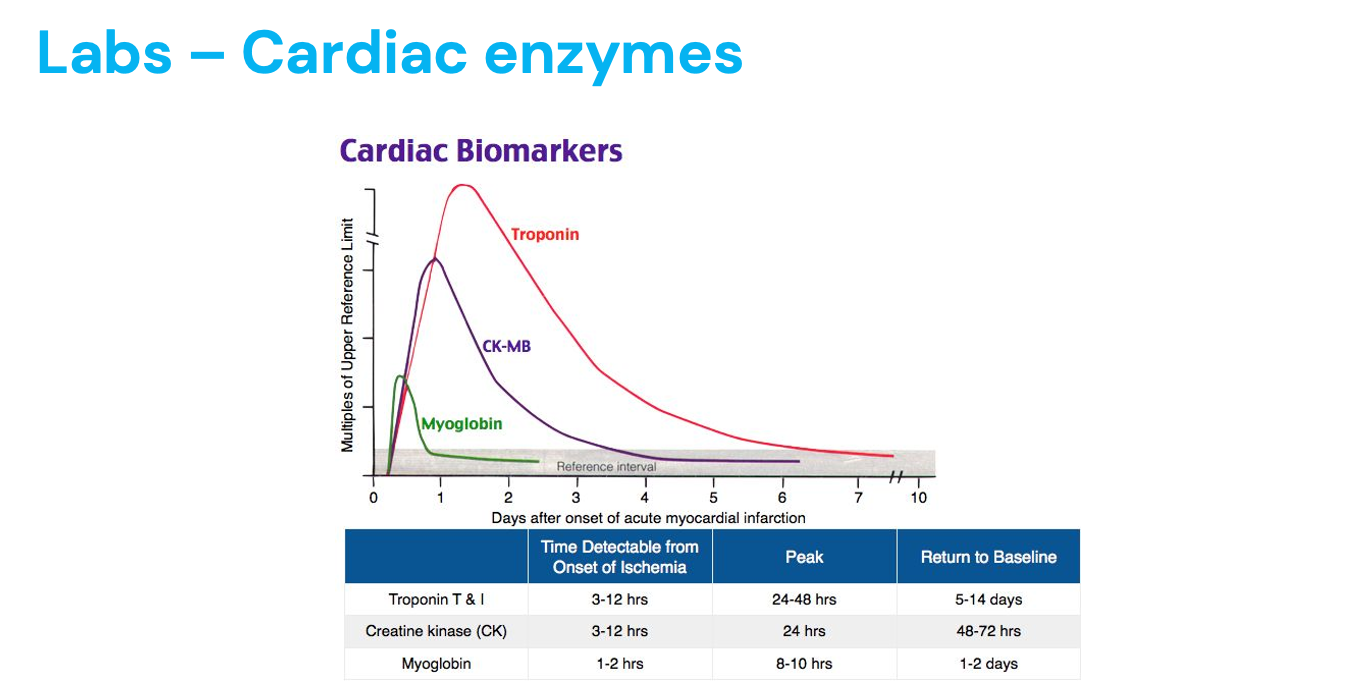
Troponin being released in bloodstream is key in diagnosing MI
Asymptomatic CAD = no symptoms, but have disease = coronary calcium score = tells us of the plaque in arteries since calcium stabilizes clots
Stable angina = chest pain with activity, goes away with rest = oxygen demand high, but supply low
With unstable angina, symptoms may occur at rest; become more frequent, severe, or prolonged than the usual pattern of angina; change from the usual pattern of angina; or not respond to rest or nitroglycerin (chest pain at rest shows myocardial ischemia) = no calcium
NSTEMI - partial blockage = troponins present
STEMi - complete blockage = ST elevation on EKG troponins present = worse
Acute Coronary Syndrome
Progression to complete blockage of blood flow to the heart muscle causing tissue death
Unstable angina = no positive troponin
NSTEMI - non ST elevated myocardial infarction (unstable angina, with elevated cardiac enzymes)
STEMI - ST segment elevation myocardial infarction (tombstone) = positive troponin, full thickness damage
Radiation of Cardiac Ischemia
Ischemia causes pain, typically radiating to these areas
“Crushing, vice like pain”
DM< females, older adults more likley to have different sex, fatigue
Symptoms of Myocardial Infarction
Myocardial infarction - tissue death of the cardiac muscle due to blockage of blood vessels of the heart
No oxygen = no contraction = no CO
Diaphoresis = sweating
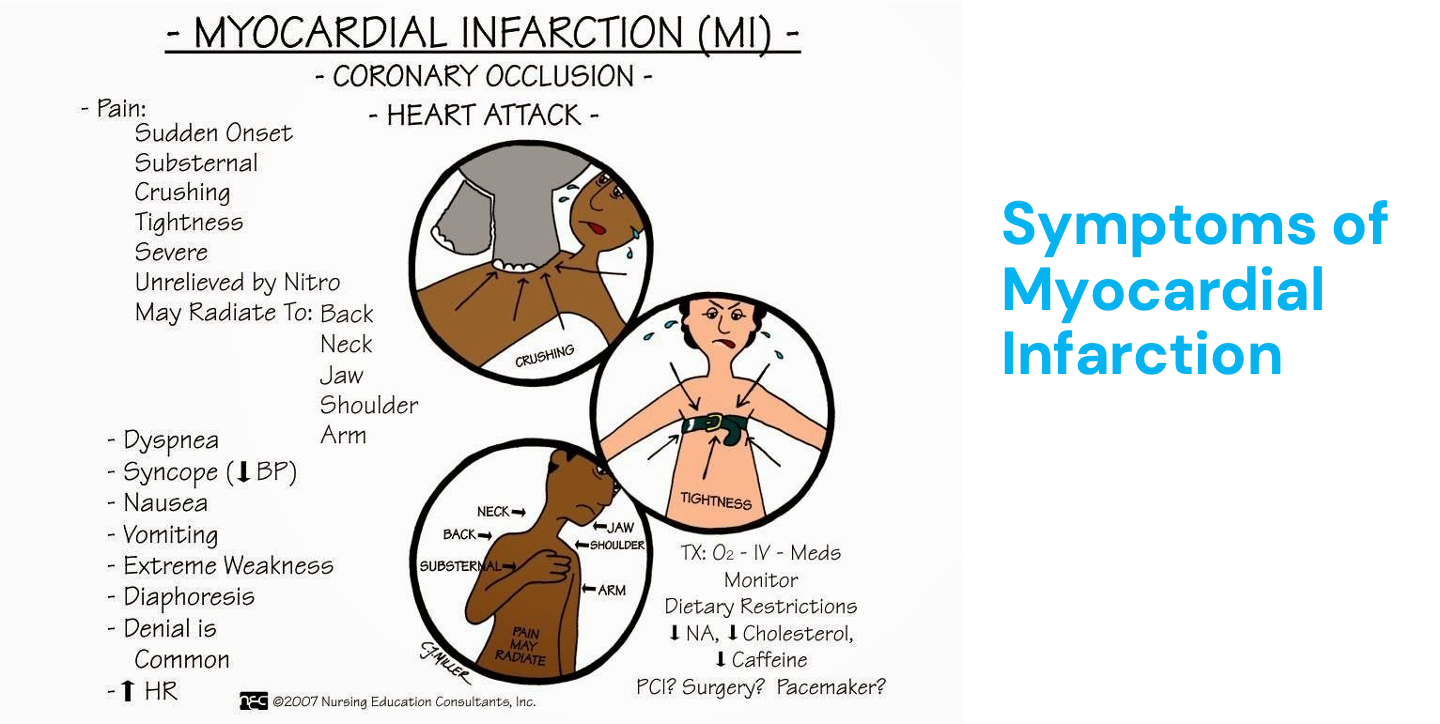
Acute MI
Diagnosis based on 3 findings:
Clinical presentation
Serial 12-lead ECG’s
Earliest findings in areas of ECG representing repolarization
Lab findings: cardiac enzymes
Heart attack is suspects - reperfution (best within 90 mins+)
Troponin = heart attack
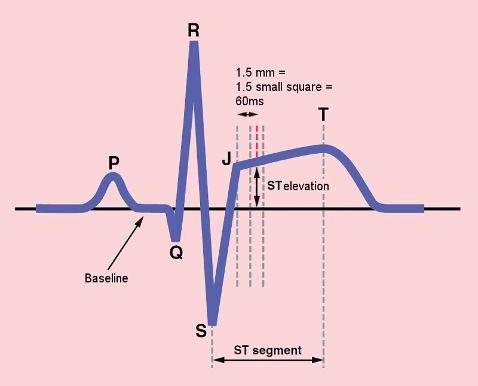
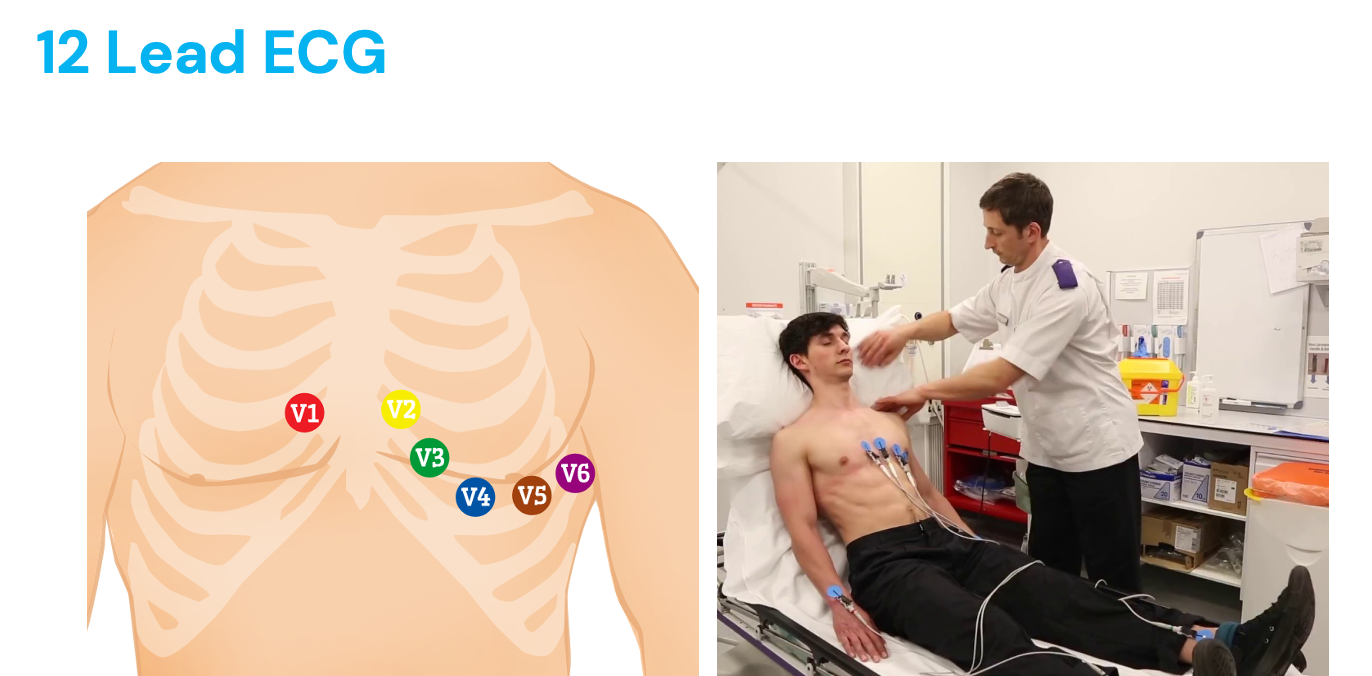
12 Lead ECG
Deploarization and repolarization of the atria and ventricles
“Organization of the squeeze” of the cardiac muscle
Atrial depolarization = p wave
Ventricle depolarization = big bump
Ventricle repolarization = last part
Labs of Cardiac Enzymes
Troponin is the main indicator
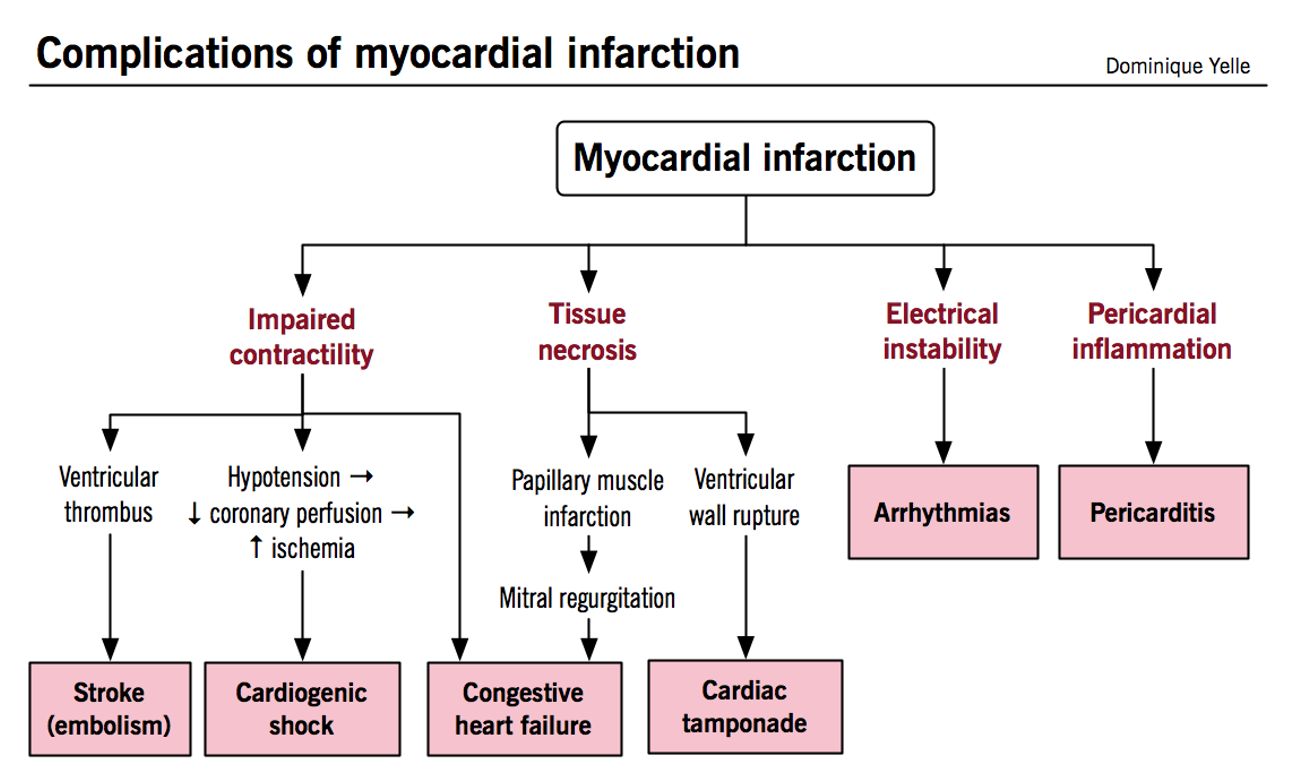
Complications of Myocardial Infarction
Tissue necrosis = death of heart tissue
Irreversible tissue damage
Acute MI = contractility decreases = blockage can form = stroke
Papillary muscle = controls mitral valve
What would happen to…
SV
CO
UOP
Valve Disorders
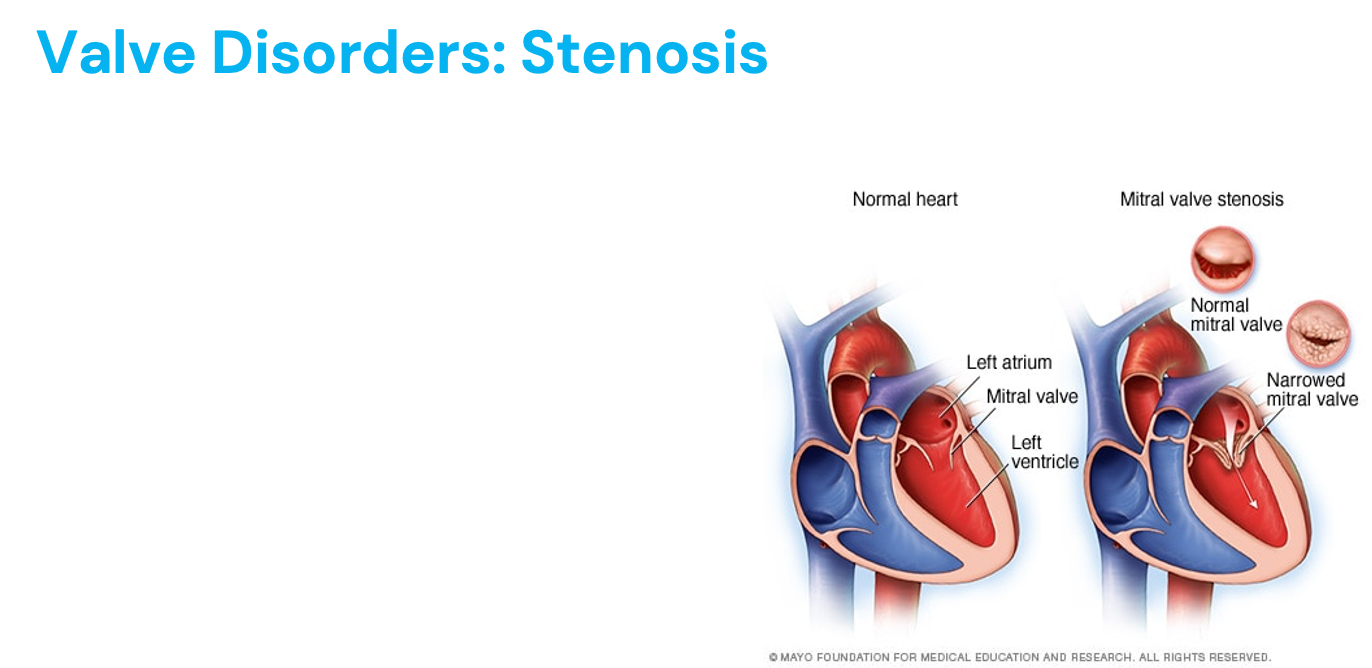
Stenosis - not enough blood passes through, hardened, narrowed artery (hypertrophy, afterload increases)
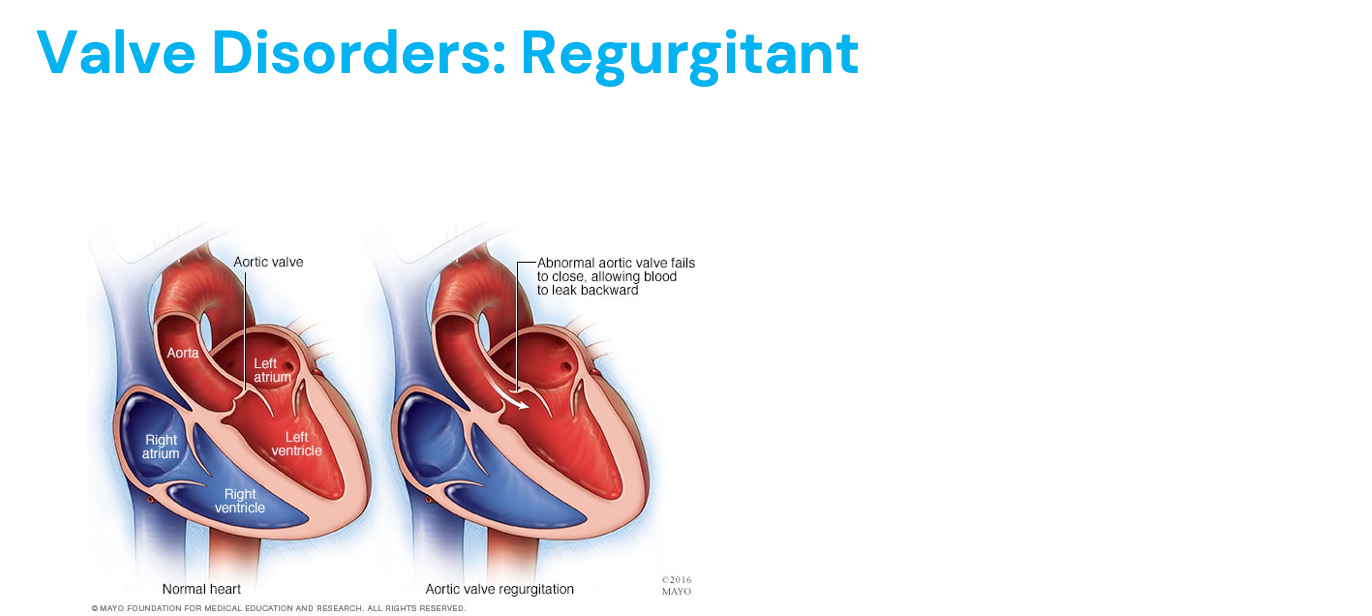
Regurgitation - blood leaks backwards (RV lowest pressure, high to low, preload high and EDV)
AV valves - mitral and tricuspid (“tri” to be right)
Tricuspid = prone to damage from IV drug use
Semilunar valves - aortic and pulmonary
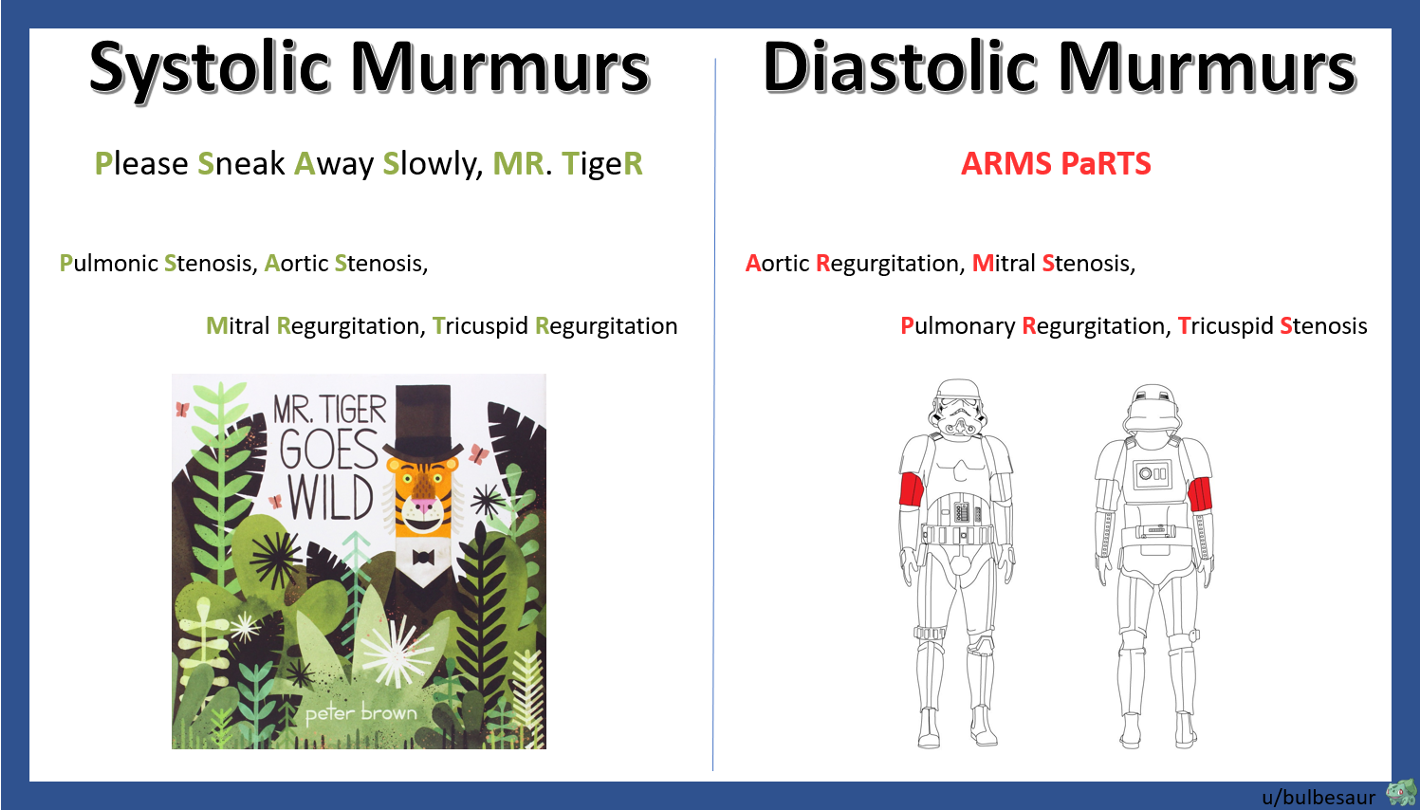
Murmur during systole (ventricular contraction) = aortic/pulmonic stenosis, mitral/tricuspid regurgitation
Murmur during diastole (ventricular relaxation) = aortic/pulmonic regurgitation, mitral/tricuspid stenosis
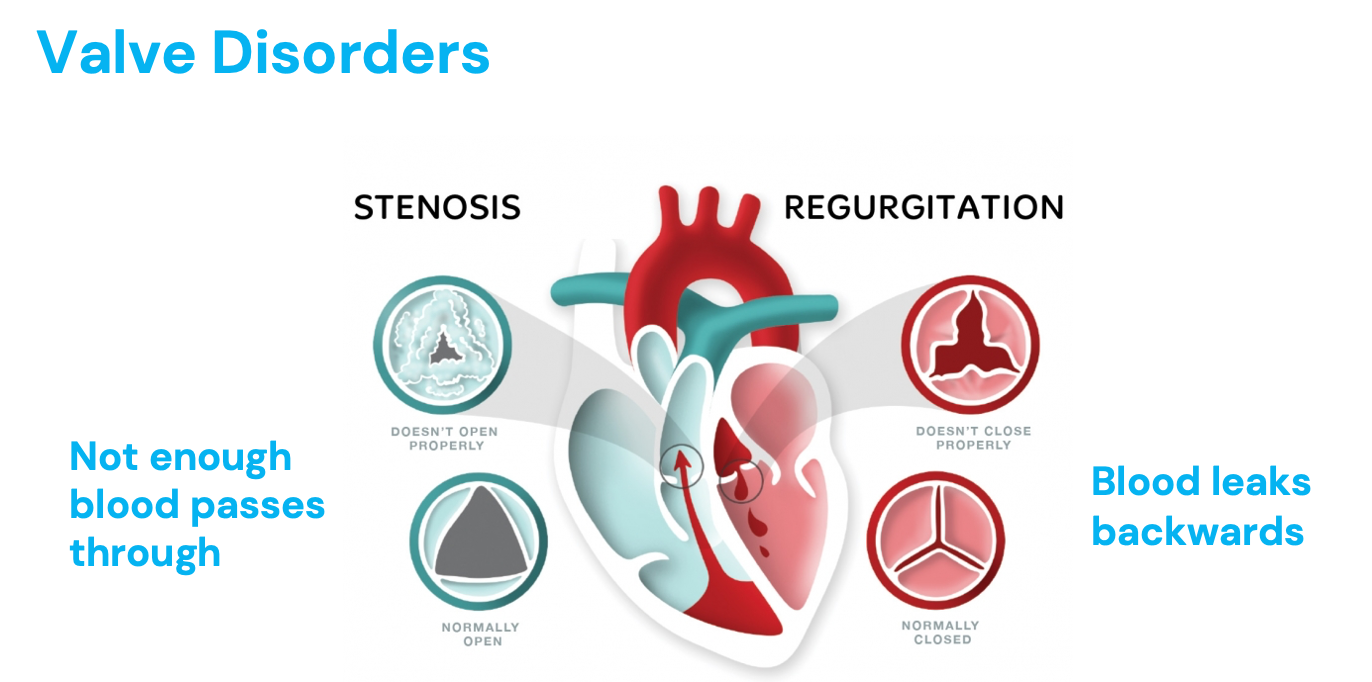
Valve Disorders - Stenosis
Aortic and mitral valve most common
On same side of heart (left) = muscular, more friction, force, wear and tear
Scar from rheumatic fever (from untreated strep throat) - can destroy valves
Wear and tear
Congenital anomalies - babies born with heart abnormalities
Valve doesn’t open completely
Tricuspid valve disorders - drug abuse (first that blood encouters, unproper use of needles)
Young women - mitral valve regurgitation
High pressure - treatment
Where does blood back up into? What would these patients present with?
Aortic stenosis = left ventricle, LV ESV increased (afterload increased), chest pain, fatigue, syncope, dyspnea (no pulmonary edema), can eventually cause LVH
Mitral stenosis = left atrium, EDV decreased (preload decreased), can cause pulmonary congestion
Pulomonic stenosis = right ventricle, EV EDV increased (RV afterload increased), can cause RVH
Would this increase or decrease blood flow to the lung?
What would happen to LV preload?
Tricuspid stenosis = right ventricle, RV ESV increased, abdominal distention, fluttering discomfort in the neck (why??)
Stenosis Signs + Symptoms
Mitral Valve
Pulmonary congestion (would you hear crackles on examination?)
Orthopnea
Nocturnal paroxysmal dyspnea
Palpitations
Fatigue
Aortic Valve
Angina
Syncope (LOC - valve replaced immediately)
Easily tired
Dyspnea
Peripheral cyanosis
Poor perfusion
Valve Disorders - Regurgitant
“Closing disorder”
Can be caused by:
Mitral valve prolapse
Damaged tissue cords
Rheumatic fever
Endocarditis
Heart attack
Abnormality of the heart muscle (cardiomyopathy)
Trauma
Congenital heart defects
Where does the blood back into? What would these patients present with?
AR = LV preload/EDV? LV ESV?
MR = retrograde flow from LV to LA during systole, LV preload? (increased(
Increased EDV!
Endocarditis = vegetations
Regurgitation Signs and Symptoms
Mitral Valve
Don’t develop symptoms for years
Pulmonary congestion
Dyspnea on exertion
Orthopnea
Aortic Valve
Exertional dyspnea
Orthopnea
Drop in diastolic pressure (blood is getting out, but diastolic is low)
Widening arterial pulse pressure
Systolic Murmurs
Problems occurs during ventricular squeeze:
Aortic stenosis (think as pair) - systolic (only when contracts, aortic valve doesn’t open)
Mitral regurgitation (doesn’t close)
Pulmonic stenosis (doesn’t open)
Tricuspid regurgitation (doesn’t close)
Heard after S1
*Know when valves are open and closed during systole
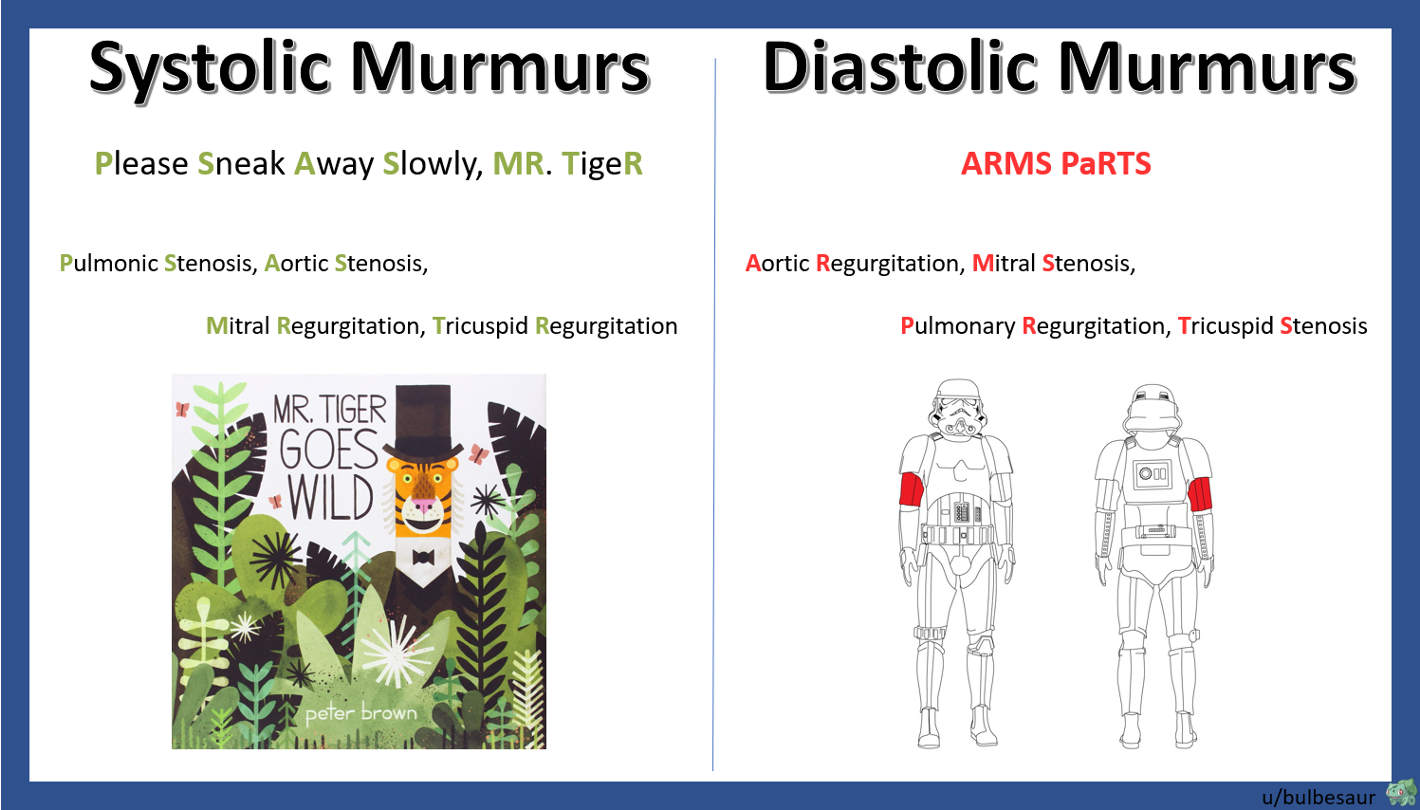
Diastolic Murmurs
Problem occurs during ventricular filling:
Aortic regurgitation (open)
Mitral stenosis (not opening)
Pulmonic regurgitation (open)
Tricuspid stenosis (not opening)
Hear murmur during diastolic (after lub dub)
*Know when valves are open and closed during systole
Heart Failure
Progressive and often fatal mortality resulting from decreased cardiac output and tissue perfusion and increased fluid retention (peripheral edema/SOB/exercise intolerance)
Caused by heart attack, high (chronic) BP
After load high = hypertrophy
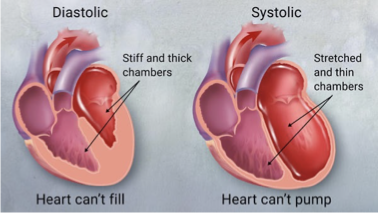
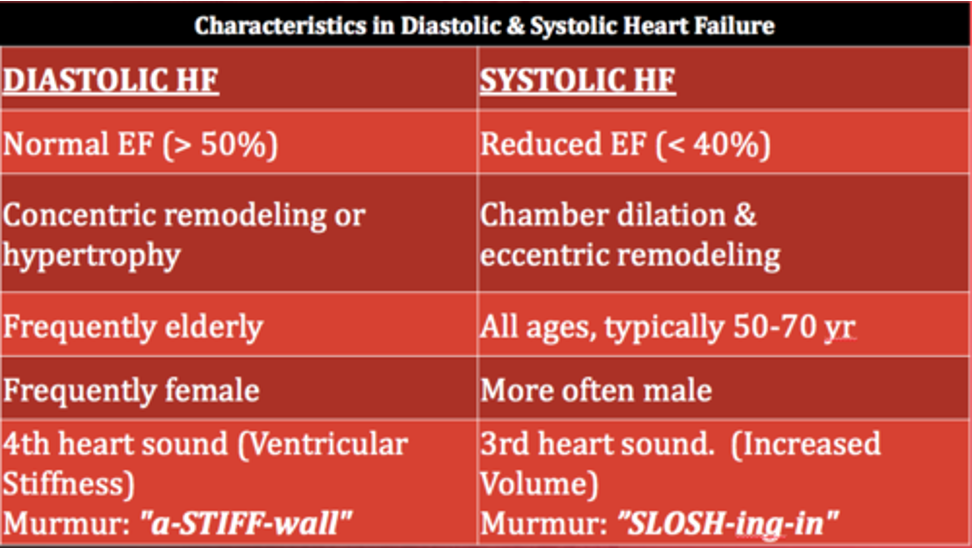
Diastolic (preserved EF) HFpEF (HF with perserved EF)
Stiff and thick chambers
Heart can’t fill, not a lot of blood goes out with contraction
Stronger LV - pump to whole body
Hypertrophy (can’t fill properly) = due to tachycardia, high BP, obesity (increased after load due to more peripheral vascular resistance)
Systolic (reduced EF) HFrEF (HF with reduced EF)
Stretched and thin chambers
Heart can’t pump (not strong enough)
Severe heart attack (damage to myocytes) = weak heart muscle
Have blood in ventricle, just can’t squeeze it out
Can be right sided, left sided, or both!
Diastolic-systolic HF (whole heart)
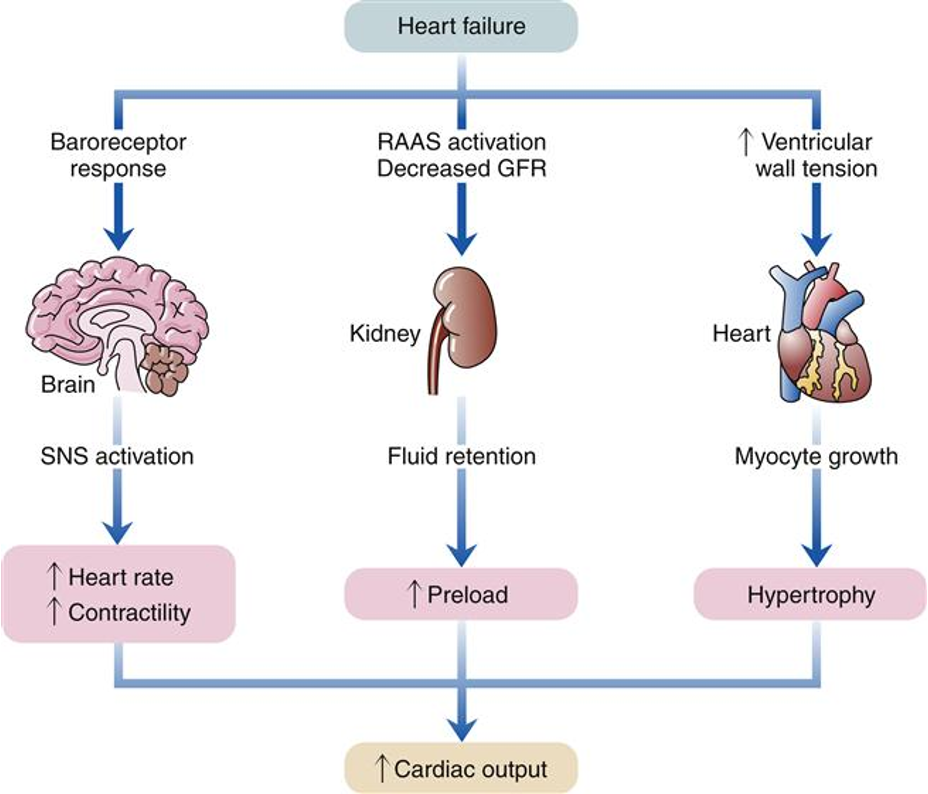
How does the body compensate for the decrease in cardiac output that occurs during heart failure?
Cardiac remodeling: dilating ventricles (systolic) and increasing wall thickness (diastolic)
Increased fluid and Na+ retention: (increasing BP)
RAAS
Causes more afterload with increased BP (process of HF is ongoing)
Activating the SNS: +inotropic (contractility, or force of heartbeat) and +chronotropic (heart rate)
Often begins asymptomatically
*Body is great at short term surivivial (long term harmful)
*A slow process
Main Consequences of Heart Failure Compensation - Hypertrophy
Diastolic HF (can’t fill/rest = hypertrophy = increase in oxygen demand = supply of oxygen can’t meet demands)
More muscle = more oxygen/calories
Increase in muscle mass and cardiac wall thickness in response to chronic dilation, resulting in…
Impaired filling
Higher O2 needs
Poor coronary artery circulation
Risk for ventricular dysrhythmias
Chronic HTN + increase systemic afterload = LVH
Main Consequences of Heart Failure Compensation - Dilation
Enlargement of the chamber of the heart that occurs when pressure in the left ventricle is elevated (systolic)
Initially an adaptive mechanism
Frank-Sterling Law
More stretch, stronger contraction
If preload is increased, a greater quantity of blood is ejected during systole due to increased stretch of the myocardium and larger amount of circulating blood volume present
Only up to a maximal point, greatest force of contraction is when the muscle fibers are stretched 2.5 times their normal length
Overstretch of cardiac muscle is like an overstretched rubber band; it will decrease cardiac contractility and efficient over time
Why an enlarged heart is not good!
Eventually this mechanism becomes inadequate, and CO decreases
*EF decreases (SV/EDV) = filling a lot, SV small, EDV big
*Diastolic EF = don’t need, look clinically
Heart Failure + Cardiac Output
Heart Failure
4-5 meds to combat these mechanisms
Baroreceptor response
Detect decrease in volume + pressure
RAAS activation, decreased GFR
Decreased CO = increases fluid retention = increases BP = increases preload (more fluid back to heart)
Increased ventricular wall tension
Helps at first
Hypertrophy = abnormal/ineffective
*ALL mechanisms are short term, harmful long term (HF)
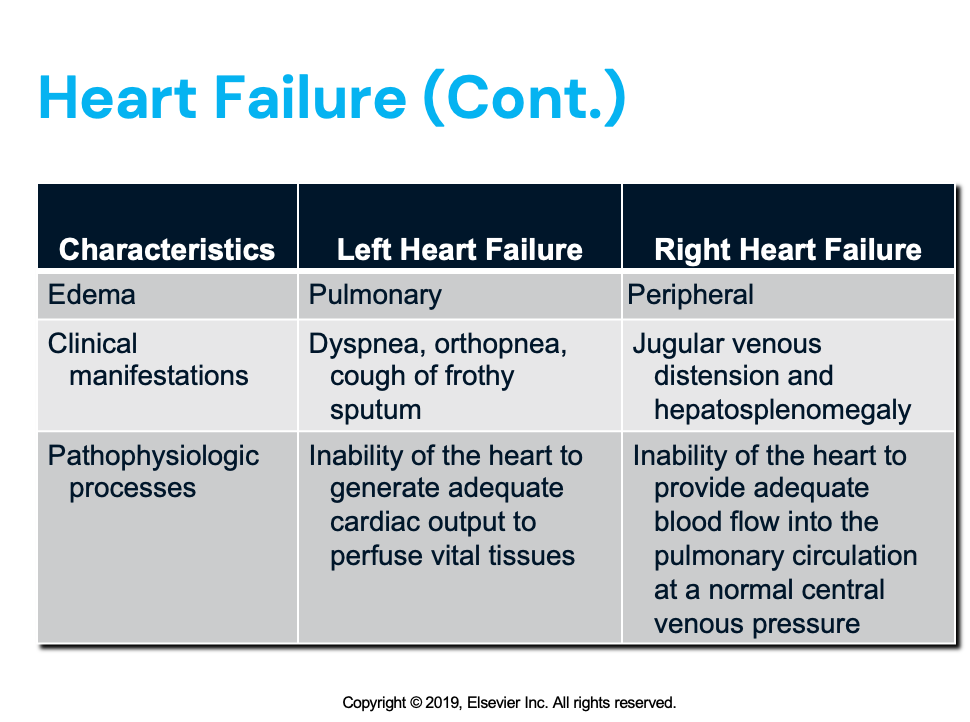
What are two ways of viewing heart failure?
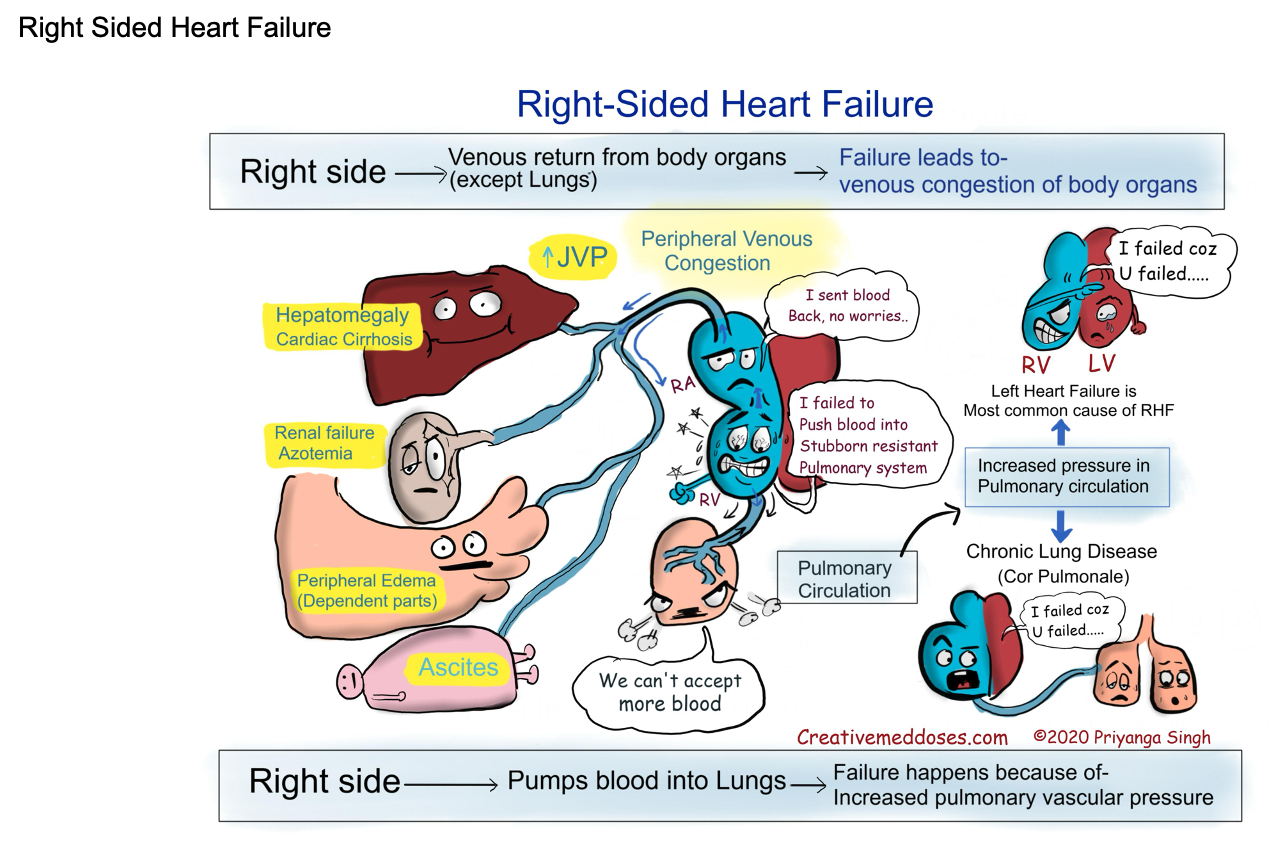
Right vs. Left Sided Heart Failure
Heart is two pumps
Either pump or both could fail
Useful for understanding clinical presentation, and isolated left or right failure does happen
Right: JVD, sacrum + scrotum + lower extremity edema, liver + spleen enlargement (where blood back up), abdominal distentsion
Back up to the body
Pump to lung
Left: SOB, coughing, crackles/wheezing, PND (Paroxysmal nocturnal dyspnea - SOB at night since fluid backs up into lungs), increased work of breathing, orthopnea (can breath laying down, have to prop themselves up)
Back up to lung
Pumo to body
Most patients present with failure of both sides
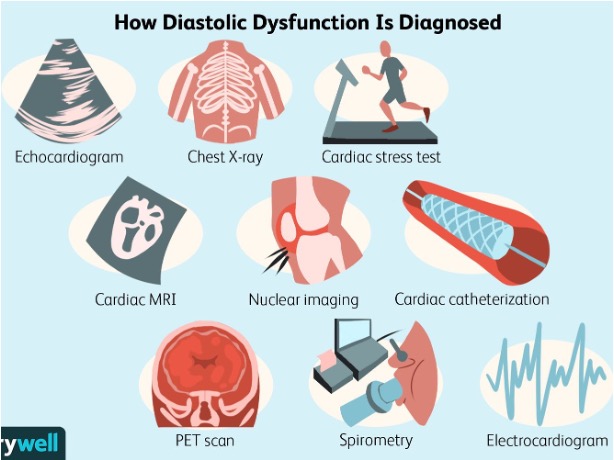
Systolic (decreased EF, weak) vs. Diastolic (normal EF, stiff) Dysfunction
More recent way of viewing heart failure
Compromised pumping (systolic failure)
Compromised filling leading to underfilling (diastolic failure)
Reduced ejection fraction vs. preserved ejection fraction
Systolic = can’t pump
Diastolic = can’t relax/fill
*SL and SV valves work together at the same time
Characteristics of Heart Failure
Right or left?
Enlarged liver (R)
JVD (R)
SOB (L)
Venous congestion/edema (R)
Crackles on exam (L)
Orthopnea (L)
Cough (L)
Pulmonary edema (L)
Cool, clammy extremities (R)
Hypoxia - not enough oxygen to tissues (BOTH)
Left Sided Heart Failure
Systolic: coronary artery disease, MI, dilated cardiomyopathy, myocarditis, acidosis, hyperkalemia, aortic valve stenosis and regurgitation, hypervolemia
Diastolic: restrict cardiomyopathy, LVH, pericarditis, tamponade, mitral stenosis (all increase ESV and pressure, back up blood flow into pulmonary circulation)
#1 cause of LHF = CAD/MI
Common cause of RHF (blood backs up to heart) = symptoms of everything
Left side failed, back up into lungs, eventually into right side
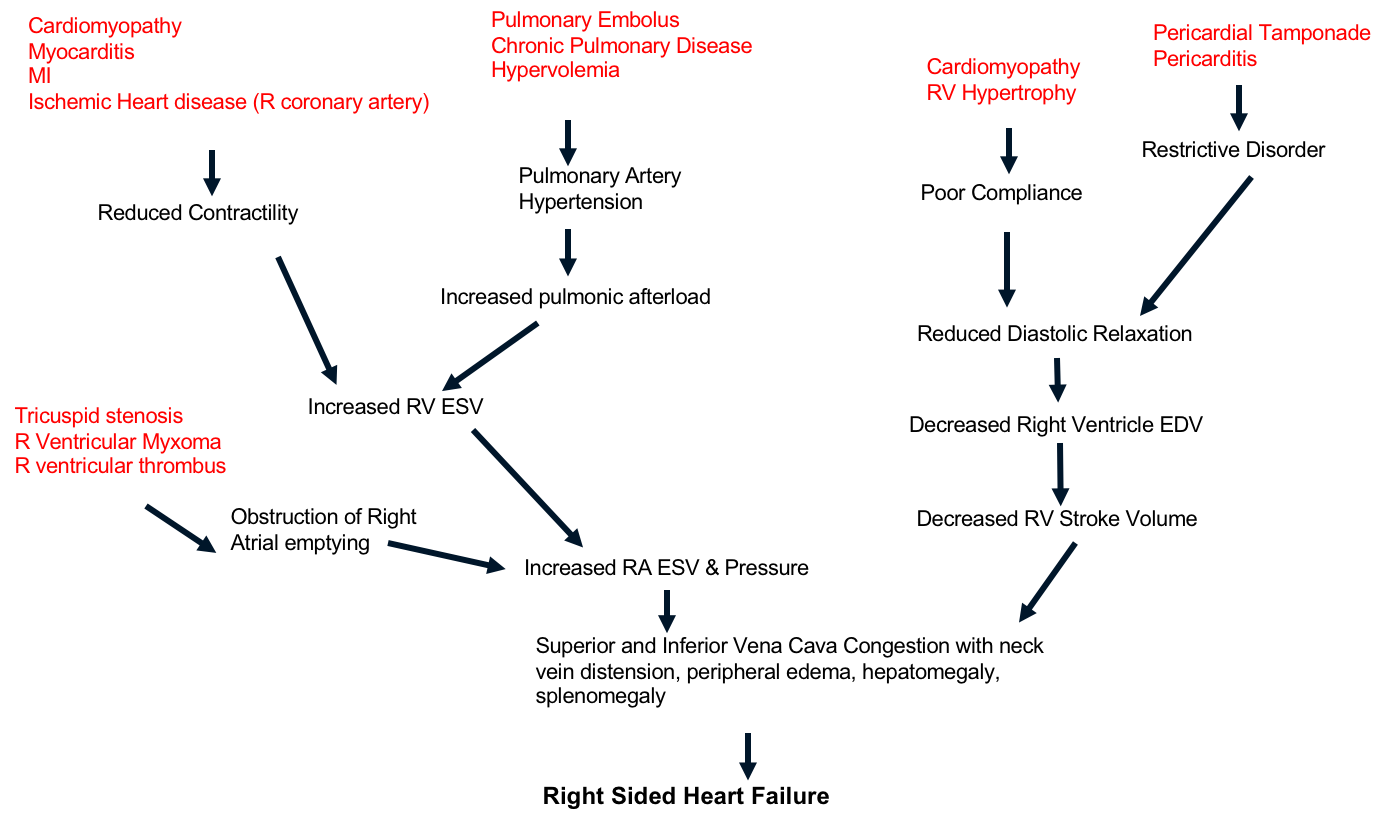
Right Sided Heart Failure
Fluid backed up into peripheral circulation
Is it leaving body? Why not?
Systolic dysfunction: cardiomyopathy, myocardits, weak heart muscle due to MI, ischemia, heart disease, pulmonary embolism, chronic pulmonary disease, hypervolemia, tricuspid stenosis (all increase RA ESV and pressure)
Diastolic dysfunction: cardiomyopathy with right ventricular hypertrophy, cardiac tamponade or pericarditis
In this case blood backs up into the peripheral circulation (organ distention - hempatomegaly, splenomegaly, peripheral edema, JVD)
#1 cause of RHF = LHF and pulmonary HTN
Cor pulmonale = chronic pulmonary HTN (due to lung disease - left side if fine, caused by lungs) that causes RHF/enlargment “pulmonary heart”
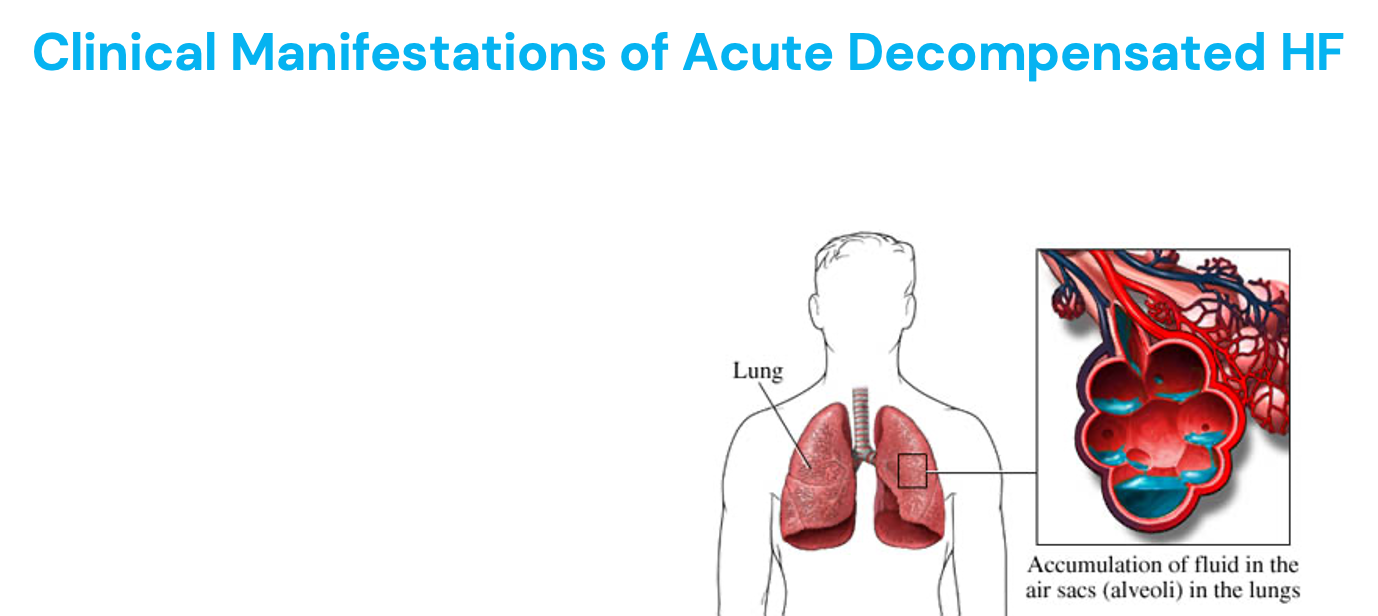
Clinical Manifestations of Acute Decompensated HF
When HF becomes severe enough to cause symptoms requiring immediate treatment
Manifests as pulmonary edema and poor organ perfusion
Lungs alveoli become filled with fluid
Signs and symptoms of pulmonary edema:
Symptoms of low CO (body not perfused) = pale, weak, LOC, low blood pressure, low oxygen staturation, syncope
Anxious
Pale, possibly cyanotic
Skin is clammy and cold
Severe dyspnea
Wheezing, coughing, frothy/blood-tinged sputum
Crackles, wheezes, rhonchi
HR rapid, BP variable
Causes: off meds, too much salt/water intake, alcohol use, pregnancy, infection/illness, arrythmia, ACS/MI
Tests ordered = echo (might shown low EF)
<25% severe
<40% abnormal
Treatment
Diurectic = decrease preload
If BP elevated = decreade afterload + inotropic meds
*Worse! EMERGENCY!
Signs and Symptoms of Decompensated HF
Like an elephant sitting on their chest - fluid, stress, sodium
Cyanosis - bluish discoloration - too much desaturated hemoglobin (poorly oxygenated blood) - need oxygen!
Best monitored in lips/mucus membranes
Why the pallor/pale skin color?
Reflex vasoconstriction - shunting blood flow to increase the peripheral vascular resistance
Can be due to MI
Symptoms of both sides of HF
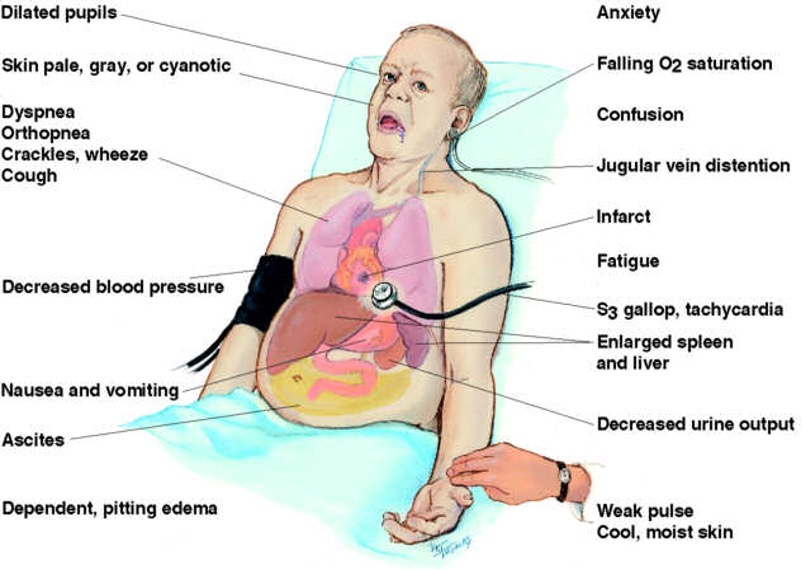
Right Sided Heart Failure
Left Sided Heart Failure
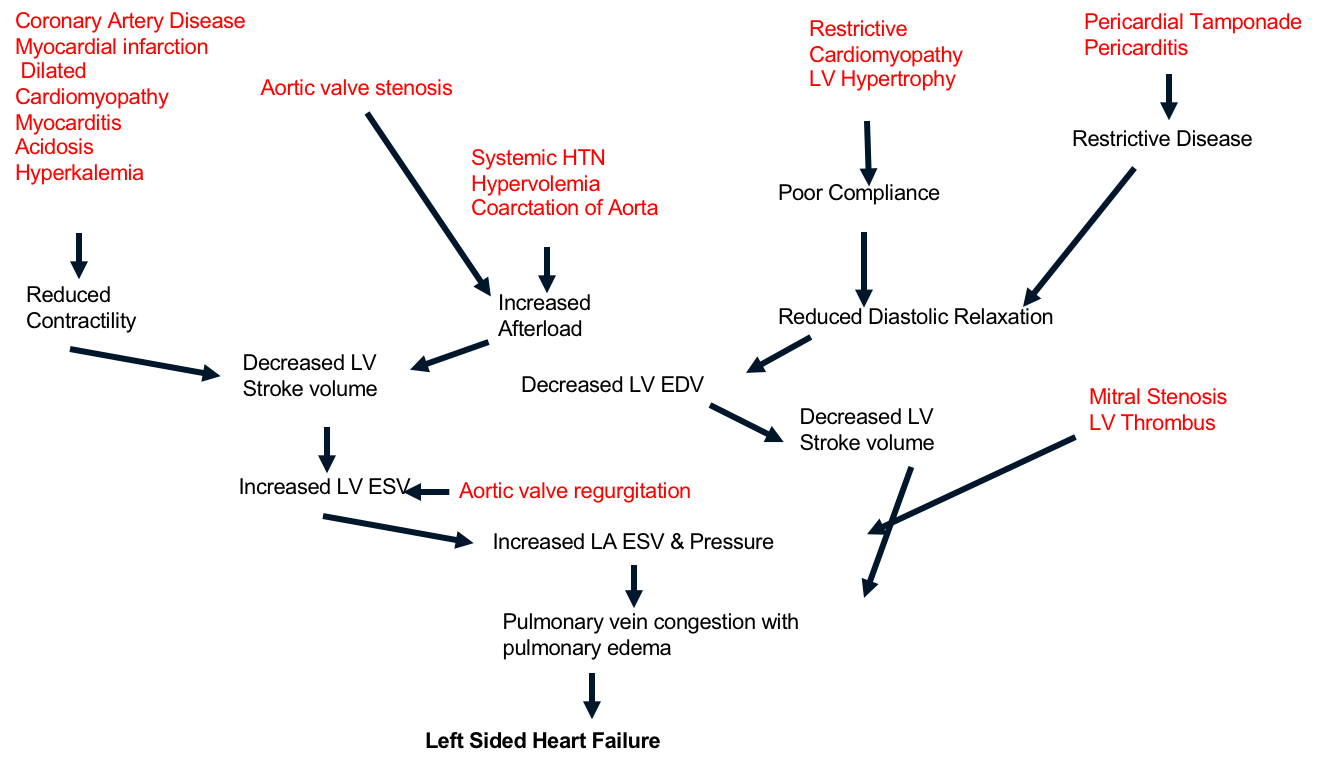
Patho of Ventricular HF - Systolic
Decreased ability to pump due to increased afterload, impaired contractile function, cardiomyopathy, or mechanical abnormalities
Heart muscle is damaged and nor contracting as it should to move blood flow forward
LV loses its ability to generate enough pressure to eject blood forward through the aorta
Hallmark = decrease in ventricular ejection fraction (EF)
Leads to low-output failure, because the heart isn’t pumping as it should - cardiomyopathy or damage from MI
Reduced EF
Systemic vasoconstriction, cold, pale, cyanosis in extremities
EF = <30% (very severe)
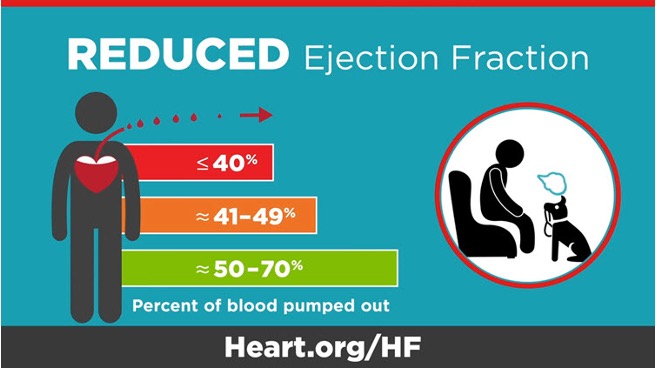
Patho of Ventricular HF - Diastolic
Inability of the ventricles to relax and fill during diastole
Normal EF
Leads to decreased SV + CO
Leads to venous engorgement in pulmonary and systemic vascular systems
Diagnosis: pulmonary congestion, pulmonary HTN, ventricular hypertrophy, normal EF
Fluid backs up into lungs
Heart Sounds in HF - S3
Early diastolic sound
Blood is not moving forward enough
Thin and weak
Low pitched
Suggest poor systolic function and/or volume overload
After systole, there is too much blood in the ventricle
Occurs when mitral valve opens and blood enters overfilled ventricle
Blood coming from the atria hit the overfilling and causes turbulence - S3
Happens when AV valves first open at the beginning of diastole (fluid overload)
*Systolic = 3 syllables
*Abnormal = occur in HF
Lub - ventricles contract (AV valves close)
Dub - ventricles relax (SL valves close)
Heart Sounds in HF - S4
Late diastolic sound (before S1)
Stiff as a board
Caused by atrial kick
Low pitched
Suggest poor diastolic function
Occurs from atrial kick squeezing blood into stiff ventricle
When atrial squeeze and push blood forward, that still and small ventricle can’t accept the blood
When atrial squeeze to force it in is squeezes it in and makes that sound
Poor diastolic dysfunction
*Diastolic = 4 syllables
*Abnormal = occur in HF
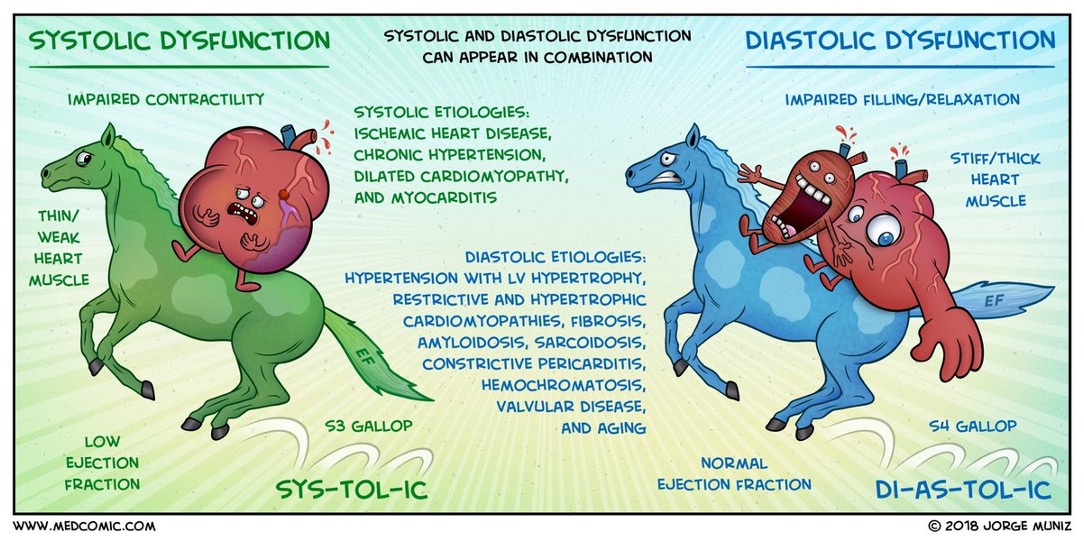
Systolic vs Diastolic Dysfunction Summary
Systolic is a pump problem (clot on plaque)
What impacts pump: pump impacts EF and drops it
Diastolic is a filling problem (glass too small)
From chronic issues like HTN, obesity
What impacts filling: heart swollen and too big, pressure within the pericardial sac (like tamponade)
Natriuretic Peptides
Blood tests for HF
Natural substances released by the heart (for increased stretch - fluid overload)
ANP (atrial natriuretic peptide) - secreted from atria
BNP (B-natriuretic peptide) - secreted from ventricles, elevated in decompensated HF
More common
Increased stretch of heart ventricle = BNP released
Inhibits compensatory mechanisms
Higher levels may indicate a heart is stretched too much and releasing high levels of these substances (HF)
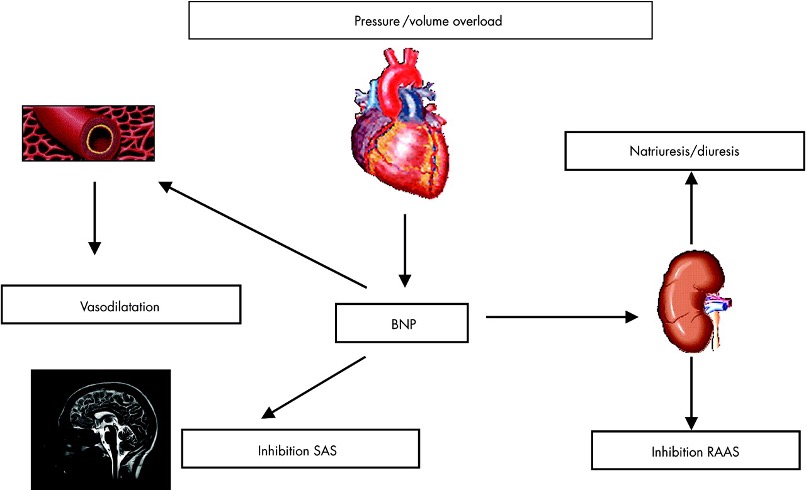
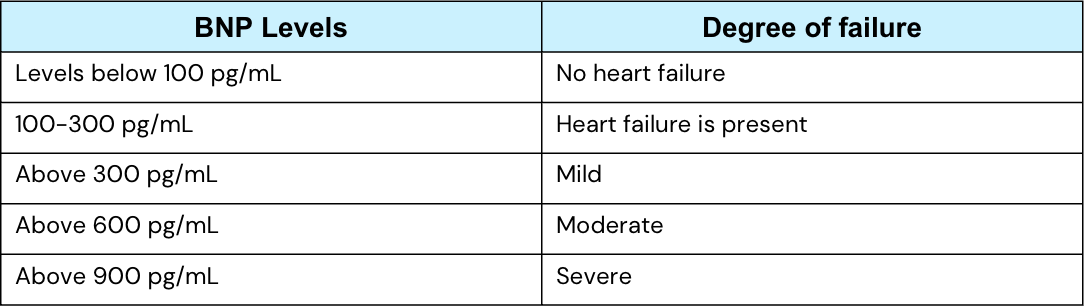
Natriuretic Peptide Labs
Monitoring the circulating BNP levels is an important indicator of cardiac health
High BNP = poor cardiac health (lower chance of survival, fluid overload)
Low BNP = better cardiac health/survival rate
Increased preload (ventricle stretch) = increased BNP
Vicious Cycle of HF
HF = tachycardia (SNS stimulated)
Decreased BP = decreased afterload (direct relationship)
Vasodilation = decreased afterload = decreased BP
Vasoconstriction = increased afterload = increased BP
Patho of Heart Failure
• Lifetime risk of HF ≈ 20% for patients >40 yrs.
• Most common causes: long-standing hypertension, multiple myocardial infarctions, diabetes mellitus.
• Categories:
- By side: Left Ventricular Failure (LVF) vs Right Ventricular Failure (RVF).
- By function: Systolic dysfunction (HFrEF = reduced EF) vs Diastolic dysfunction (HFpEF = preserved EF).
Left Ventricular Failure (LVF)
Main problem: Backup into lungs → pulmonary symptoms.
Symptoms/Signs:
- Dyspnea on exertion
- Cough, orthopnea, paroxysmal nocturnal dyspnea (PND)
- Cyanosis
- Crackles on auscultation
- Pulmonary edema → pink frothy sputum + coarse crackles
Compensatory mechanisms:
- RAAS activation → ↑ blood volume, ↑ BP, ↑ resistance (afterload).
- Sympathetic stimulation → ↑ HR, ↑ strain on heart.
Diagnostics:
- BNP to distinguish cardiac vs pulmonary cause of dyspnea.
- LVEF <40% = Heart failure.
Right Ventricular Failure (LVF)
Main problem: Backup into systemic venous circulation.
Symptoms/Signs:
- Jugular venous distension (JVD)
- Ascites
- Hepatomegaly & splenomegaly
- Peripheral edema (ankle, sacral)
Key Clinical Findings of HF
• S3 gallop rhythm common in HF.
• Preload = blood returning to right atrium.
• Afterload = resistance against ventricle (aortic pressure).
Management of HF
Lifestyle modifications: diet, exercise, fluid/salt restriction.
Pharmacologic therapy:
- ACE inhibitors / ARBs
- Beta blockers
- Diuretics
- Nitrates, vasodilators
- Ivabradine
- Neprilysin inhibitors
- Digitalis (digoxin)
- Spironolactone (aldosterone antagonist)
Devices/Procedures:
- ICD: prevents sudden cardiac death.
- LVAD: bridge to transplant or destination therapy.
- Intra-aortic balloon pump: temporary support in end-stage HF.
- Transplantation in severe/end-stage cases.
Left vs. Right HF
Category | Left Ventricular Failure (LVF) | Right Ventricular Failure (RVF) |
|
|
|
Main cause | Often HTN, MI, DM | Often secondary to LVF or lung disease |
Primary backup | Lungs | Systemic veins |
Symptoms | Dyspnea, orthopnea, PND, pulmonary edema, crackles, pink frothy sputum | JVD, ascites, hepatomegaly, splenomegaly, peripheral edema |
Diagnostics | ↓ LVEF, BNP elevated | Clinical exam findings |
Heart Failure - Study Tips
• Remember: LVF = Lungs; RVF = Rest of body.
• HFrEF = reduced EF (<40%), HFpEF = preserved EF but stiff ventricle.
• BNP helps distinguish HF-related dyspnea from pulmonary disease.
• S3 heart sound = classic for HF.
How could myocardial infarction lead to low blood pressure and shock? What signs and symptoms might you see and why would they be present?
Myocardial infarction is death of a portion of the myocardium (those myocardiocytes) due to blockage of a coronary artery. When part of the myocardium dies, this can lead to acute systolic dysfunction of the heart (an acute pumping problem), as the heart can no longer pump effectively. The heart's reduced pumping ability leads to a drop in stroke volume, and can lead to inadequate cardiac output. Remember, cardiac output = stroke volume x heart rate. If the cardiac output drops too much, then blood pressure will drop due to a decrease in the overall circulating blood volume. (Remember, blood pressure has 3 main components; the blood, the blood vessels, and the cardiac pump). To compensate, the heart can increase the heart rate, so we may see tachycardia. The sympathetic nervous system causes vasoconstriction and attempts to shunt blood from the extremities back to the core organs (the heart and the brain). Thus we may see pale or ashen skin and the skin would likely feel cool to the touch. This is because we have a drop in the blood flow to the skin, much like we saw with hypovolemic shock. The kidneys would begin retaining more sodium and water from the urine in an effort to increase blood volume even though the heart can not effectively pump blood forward. So patients will have reduced urinary output as well.
How could a pulmonary embolism lead to right-sided heart failure?
The right ventricle pumps deoxygenated blood through the pulmonary semilunar valve into the pulmonary artery and into the lungs. A pulmonary embolism is a blockage in one of the pulmonary arteries of the lungs. That blockage can thus cause blood to back up into the right ventricle. The right ventricle then has to pump harder to overcome the increased afterload in pulmonary circulation. However, if the PE is large enough, the pressure may become too great for the RV to overcome, and it can lead to sudden, acute right ventricular failure. It can be a rapidly developing situation that requires emergency care to prevent cardiac arrest and respiratory failure.
What is the difference between valve stenosis and valve regurgitation (incompetence)? How could these valve disorders lead to heart failure?
Valve stenosis is a thickened, stiff, scarred, or malformed valve that does not open fully. Regurgitation is an "incompetent" valve that does not close fully (it can't make an effective seal when it is closed). Both of these disrupt the normal one-way route of blood flow through the heart, leading to congestion in the chambers and structures before the valve.
The last sentence is very important! For example, mitral stenosis or regurgitation will lead to congestion in the left atria. This causes left atrial hypertrophy and an increase in the left atrial ESV. The left ventricle, however, will have a decreased ESV. Why does the left ventricle have a reduced ESV? Here is why:
1. With mitral stenosis, less blood makes it into the left ventricle during filling, which decreases end diastolic volume. If you start with less blood at the beginning of systole, you will have less at the end of systole as well.
2. Mitral regurgitation reduces left ventricular afterload. How? Because you essentially now have two "doors" out of which blood can escape during systole (both the aortic valve and the mitral valve are now allowing blood out during systole). Since blood is escaping out of both valves, more blood is pumped out during systole, leading to a lower left ventricular ESV.
Heart failure will eventually happen in valve stenosis/regurgitation because of blood back up. For example:
Aortic stenosis --> blood backs up in to left ventricle--> ventricle dilates and hypertrophies to compensate --> compensatory mechanisms eventually are inadequate (remodeling of heart becomes pathologic) --> blood backs up into left atria --> blood backs up into lungs, potentially leading to pulmonary edema and to signs of inadequate organ perfusion (dizziness, possible fainting, chest pain, low urine output, diminished pulses, etc.)
Like the preceding example, you could chart a backward course of blood congestion and heart failure for each of the valves!
Which of these conditions would likely lead to diastolic heart failure? Select All That Apply
a. Left ventricular aneurysm
b. Cardiac hypertrophy from long-standing hypertension
c. Cardiac tamponade
d. Aortic regurgitation
e. Restrictive cardiomyopathy
f. Dilated cardiomyopathy
g. Long-standing anorexia nervosa
a. Left ventricular aneurysm. This would be a systolic function. Ventricular aneurysm is a large outpouching in the ventricle. Filling isn't compromised, but pumping is. Thus, this is a systolic issue.
b. Cardiac hypertrophy from long-standing hypertension - CORRECT. The ventricle becomes bulky, stiff, and non-compliant. This compromises filling (a diastolic problem)
c. Cardiac tamponade- CORRECT. When fluid accumulates in the pericardial sac it will impede ventricular filling (It is "squeezing the heart). This is a diastolic issue.
d. Aortic regurgitation- Blood moves backward during diastole, which overfills the ventricle. This results in a loss of SV and a reduction in ejection fraction (the blood initially moves out during systole, but then some of it travels backward back to the ventricle). This overfills the ventricle and causes an overall reduction in the ejection fraction. This would be a systolic issue.
e. Restrictive cardiomyopathy- CORRECT. A restrictive cardiomyopathy is when the heart becomes stiff from infiltrative connective tissue. This impedes the heart's ability to relax and fill, which is a diastolic issue.
f. Dilated cardiomyopathy- In dilated cardiomyopathy the ventricular chamber is large (dilated) and the muscle is reduced in size. This leads to problems pumping, which is a systolic issue.
g. Long-standing anorexia nervosa- Long standing anorexia can cause heart muscle fibers to degenerate because of lack of nutrients to maintain healthy cardiac muscle. This leads to a weak cardiac pump, which is a systolic issue.
Mr. Alwyn is a 53-year-old man who began experiencing chest pain while playing tennis with his friend. He described the pain as crushing and vice-like. The pain radiated up into his left jaw and down his left arm. He noticed that his heart was racing as well. He sat down in the shade and the pain subsided after 10 minutes. He went home and had no further problems. He decided that it was probably due to the large breakfast he had before the game and so did not seek medical treatment.
What information in the scenario suggests that this is cardiac-related pain?
Why did the pain go away after he sat down?
Could the large breakfast that Mr. Alwyn ate play a role in his chest pain?
What information in the scenario suggests that this is cardiac-related pain?
Chest pain (angina) that radiates, tachycardia
Why did the pain go away after he sat down?
Stable angina - pain only occurs with exertion (less demand of oxygen with rest = adequate supply of oxygen to heart)
Could the large breakfast that Mr. Alwyn ate play a role in his chest pain?
Yes - body will shunt blood away from other organs to ones that are doing more work (digestive organs)
Not enough blood/oxygen to the heart
MI mostly happen between 4 am - 10 am (breakfast time)
Mr. Alwyn has the following medical history:
HTN, diagnosed 12 years ago
Type 2 DM, diagnosed 5 years ago
Hypercholesterolemia
BPH (biegnin prostatic hypertrophy) , diagnosed 2 years ago
Mr. Alwyn has the following family/social history
Father had history of DM, died of an MI at age 55
Mother died from breast cancer at age 79
Brother has hypertension
Occasional alcohol use, reports drinking 2-3 beers a week
Grandparents “may have had heart disease”
What are Mr. Alwyn’s most significant risk factors for coronary artery disease?
How do each of these risk factors contribute to the pathogenesis of CAD?
Which risk factors would you want to target as a nurse?
Mr. Alwyn is prescribed sublingual nitroglycerin PRN for his chest pain.
Nitroglycerin is a potent vasodilator. How could this help alleviate chest pain in patients with angina?
What are Mr. Alwyn’s most significant risk factors for coronary artery disease? How do each of these risk factors contribute to the pathogenesis of CAD?
HTN - turbulent blood flow that damages walls of blood vessels, inflammatory response, increased after load (pressure for heart to pump against), plaque formation and rupturing increased, risk for heart attack
DM - inflammatory to blood vessels (increased cytokine release), increased risk for plaque rupture
Hypercholesterolemia - LDL forms plaques
Which risk factors would you want to target as a nurse?
HTN - treated to decrease workload of heart
Hypercholesterolemia - want to decrease cholesterol to decrease plaques
Controlling blood glucose levels to decrease inflammation in the body
Mr. Alwyn is prescribed sublingual nitroglycerin PRN for his chest pain. Nitroglycerin is a potent vasodilator. How could this help alleviate chest pain in patients with angina?
Decreases preload (amount of blood coming back to heart)
Dilates arteries - decreased blood pressure and after load
Mr. Alwyn wakes up at 3:00 in the morning with crushing, substernal chest pain. He takes three doses of his nitroglycerin, but the chest pain is unremitting. He is nauseous, diaphoretic, and extremely anxious. He tells his wife “I think I’m dying”. His wife notices that he is cold and clammy. She calls 911 and he is brought to the emergency department. The paramedics transmit a 12-lead ECG to the ED physician along the way. They also give Mr. Alwyn an aspirin, which they tell him to chew. At the ED, Mr. Alwyn presents as follows:
Vital Signs | |
BP 156/88 mmHG, right arm sitting | Temp 98.3 F |
HR 105 | HT 70” |
RR 26 | WT 83.5 kg |
Skin | Cool, diaphoretic, pale without cyanosis |
Chest | Slight bibasilar inspiratory crackles with auscultation. No wheezes or friction rubs |
Cardiac | Tachycardia with occasional premature beats. Normal S1 and S2. No S3, soft S4 |
Abdomen | Soft, nontender, hypoactive bowel sounds present in all quadrants. |
MSK | Normal range of motion throughout, Pulses 2+, distinct bruit over the femoral artery, no pedal edema |
Neuro | Cognition, sensation, gait, DTR in normal limits. Anxious and restless |
Describe the physiologic mechanisms behind Mr. Alwyn’s abnormal vital signs.
Describe the physiologic mechanisms behind Mr. Alwyn’s clinical presentation.
Describe the physiologic mechanisms behind Mr. Alwyn’s abnormal vital signs.
High blood pressure (systolic noted)
High heart rate
High respiratory rate - pain, panic
Temperature - normal
Height + weight not significant at the moment
Describe the physiologic mechanisms behind Mr. Alwyn’s clinical presentation.
Blood being shunted away from body - core blood to vital organs by SNS
Sweaty - SNS
Crackles - fluid backing up into lungs
S4 - always pathologic (diastolic issue - filling problem)
Not as much function in bowel sounds - blood in vital organs
Bruit - turbulent blood flow
Anxious - SNS
*SNS - body uses too much oxygen (give morphine which decreases oxygen intake)
Ms. Duquette is admitted to the ICU with a right-sided MI due to occlusion of the right coronary artery. Heart rate is 45 BPM, blood pressure is 86/40 mmHg.
Why might this patient have a low HR and a low BP?
The physician has prescribed the following medications that are often given to patients in the acute phase on MI:
Nitorglycerin (vasodilator)
Beta blocker (negative inotropy and negative chronotropy).
Considering Ms. Duquette presentation, you might want to:
A. Administer the nitroglycerin and hold the beta blocker
B. Administer the beta blocker and hold the nitroglycerin
C. Administer both medications
D. Hold both medications
Why might this patient have a low HR and a low BP?
Right-sided MI
RCA - perfuses SA and AV nodes (pacemakers of the heart)
SA node is killed, AV node takes over - around 40 bpm (bradycardia)
Low HR = low BP (drop in CO)
Dizziness and syncope (LOC)
Brain not perfused - fall risk
The physician has prescribed the following medications that are often given to patients in the acute phase on MI:
Nitroglycerin (vasodilator)
Beta blocker (negative inotropy and negative chronotropy)
Slow contractility, HR
Considering Ms. Duquette presentation, you might want to:
A. Administer the nitroglycerin and hold the beta blocker
B. Administer the beta blocker and hold the nitroglycerin
C. Administer both medications
D. Hold both medications - vasodilator will drop her BP
Thanks to an amazing health care team and the support of his wife and children, Mr. Alwyn survives his MI and returns from the cath lab after two stents are placed in his LAD artery. On day two, the nurse notices that Mr. Alwyn is becoming more short of breath. Course, bilateral crackles are auscultated in the mid and lower lobes. The nurse also notices that there is both and S3 and and S4 heart sound present. His heart rate is elevated again (102 BPM) and his blood pressure is at 100/64 mmHg.
Explain Mr. Alwyn’s respiratory symptoms
Why would Mr. Alwyn be hypotensive?
You would expect Mr. Alwyn’s ESV to be:
Increased
Decreased
Within normal limits
You would expect Mr. Alwyn’s LVEDV to be:
Increased
Decreased
Within normal limits
You would expect Mr. Alwyn’s pulmonary pressures to be:
Increased
Decreased
Explain Mr. Alwyn’s respiratory symptoms
Crackles - fluid in lungs (pulmonary edema)
HF a complication of MI = heart not pumped blood forward, backing up into lungs (left side of heart not pumping effectively)
Why would Mr. Alwyn be hypotensive?
Reduced CO
Blood is backed up into lungs
Blood not leaving heart = low BP
You would expect Mr. Alwyn’s ESV to be:
Increased - more blood left in V after systolic
Decreased
Within normal limits
You would expect Mr. Alwyn’s LV EDV to be:
Increased - more blood staying in ventricle
Decreased
Within normal limits
You would expect Mr. Alwyn’s pulmonary pressures to be:
Increased - pulmonary congestion, right side has a lot of pressure to push against
Decreased
Mr. Norrell has experienced increasing fatigue and shortness of breath over the past few months. He developed a dry cough and his legs swell by the end of the day. He reports that he has to prop his head up on four pillows at night and that he goes to the bathroom to urinate 4-5 times during the night (orthopnea - fluid in lungs when laying fluid, nocturia - laying flat = edema comes back into vessels = goes to kidneys). His past medical history includes diabetes (type II), hyperlipidemia, and peripheral arterial disease. An echocardiogram reveals an ejection fraction of 33% (systolic HF) and a BNP (brain-type natriuretic peptide) level is 750 pg/mL (normal range: < 100 pg/mL). His vital signs upon presentation are: HR 94 bpm, BP: 160/94, RR: 22/minute, Temp: 97.4 oral, O2 saturation: 94% on room air. Mr. Norrell is diagnosed with heart failure.
Based on the preceding information, Mr. Norrell likely has:
Systolic dysfunction
Diastolic dysfunction
BNP would most likely indicate:
Increased EDV
Decreased ESV
Decreased ventricular filling pressures
A and B
A, B, and C
Based on the scenario, Mr. Norrell is likely experiencing:
Left ventricular dysfunction
Right ventricular dysfunction
Biventricular dysfunction
True or False: Left ventricular afterload appears to be severely decreased.
True or False: From a clinical standpoint, we probably need to focus on interventions that will increase Mr. Norrell’s preload so that we can increase cardiac output.
Based on the preceding information, Mr. Norrell likely has:
Systolic dysfunction - heart is pumping blood out (pumping problem) = EF < 40%
Diastolic dysfunction
Filling problem
BNP would most likely indicate:
Increased EDV - too much stretch
Decreased ESV
Decreased ventricular filling pressures
A and B
A, B, and C
Based on the scenario, Mr. Norrell is likely experiencing:
Left ventricular dysfunction
Right ventricular dysfunction
Biventricular dysfunction - edema (right sided issue, blood backs up in RA, body, JVD), orthopnea, cough, pulmonary symptoms - all left side
True or False: Left ventricular afterload appears to be severely decreased.
BP is elevated
True or False: From a clinical standpoint, we probably need to focus on interventions that will increase Mr. Norrell’s preload so that we can increase cardiac output.
Don’t want to increase if there is a pumping problem
High BNP - already too much preload (want to decrease)
Ms. Terry has been diagnosed with mitral stenosis r/t rheumatic fever. Based on this diagnosis, answer the following questions:
True or False: You would expect Ms. Terry to present with a systolic heart murmur.
What type of hypersensitivity reaction led to her condition?
Type I
Type II
Type III
Type IV
What type of antibodies are primarily responsible for this type of hypersensitivity?
Which chamber in the heart will most likely undergo pathologic remodeling first?
Left ventricle
Left atria
Right ventricle
Right atria
Based on her condition, you would expect left ventricular end-diastolic volume to be:
Increased
Decreased
True or false: The ESV of her left ventricle will likely be increased
True or false: Ms. Terry’s condition would likely contribute to increased fluid formation in the pulmonary interstitial space.
True or false: Over time, the right ventricle is likely to hypertrophy.
True or False: You would expect Ms. Terry to present with a systolic heart murmur.
Stenosis - problem with opening
Mitral opens during diastolic
What type of hypersensitivity reaction led to her condition?
Type I
Type II - IgM + IgG
Type III
Type IV
What type of antibodies are primarily responsible for this type of hypersensitivity?
IgG and IgM (type II hypersensitivity)
Which chamber in the heart will most likely undergo pathologic remodeling first?
Left ventricle
Left atria
Right ventricle
Right atria
Based on her condition, you would expect left ventricular end-diastolic volume to be:
Increased
Decreased - not enough blood in ventricle due to stenosis mitral valve
True or false: The ESV of her left ventricle will likely be increased
Not filling enough (not enough EDV) = less ESV
True or false: Ms. Terry’s condition would likely contribute to increased fluid formation in the pulmonary interstitial space.
Blood back flows into the lungs = pulmonary edema
True or false: Over time, the right ventricle is likely to hypertrophy.
Pulmonary edema = increases right side pressure to push against