L16: Ataxia and paresis: principles of spinal and lumbosacral disease
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
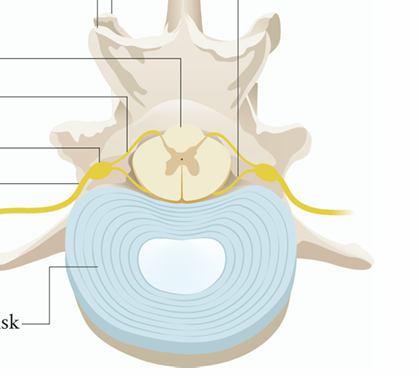
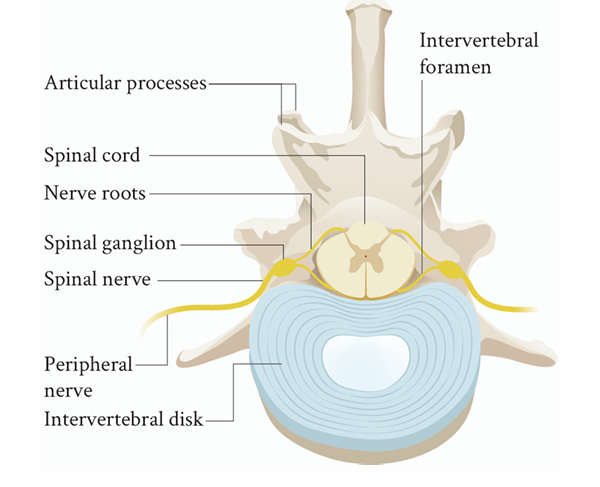
Label this
What are some anatomical considerations of the spine
Spinal cord and vertebral column do not have the same length
Vertebral column is longer than spinal cord
There is no spinal cord present at the lumbosacral junction
the lumbosacral vertebral canal is occupied by the caudal equina
When does the spinal cord end in dogs and cats
Dogs: ~L6
Cats: ~L7
How many segments are in the spinal cord
four functional segments based on whether it contains functional LMN
What are the 4 functional segments of the spinal cord
C1-C5
C6-T2
T3-L3
L3-S3
Does sensory and motor ascend, descend or both
Ascending is sensory
Descending is motor information
What tends to characterise spinal cord disorders
combination of sensory and motor dysfunction
What occurs in the dorsal and lateral funiculi and what happens if its damaged
sensory and proprioceptive tracts
ataxia
What occurs in the ventral and lateral funiculi and what happens if its damaged
Motor or UMN tracts
UMN paresis
what occurs in the LMN cell bodies
Ventral horn grey matter
LMN paresis
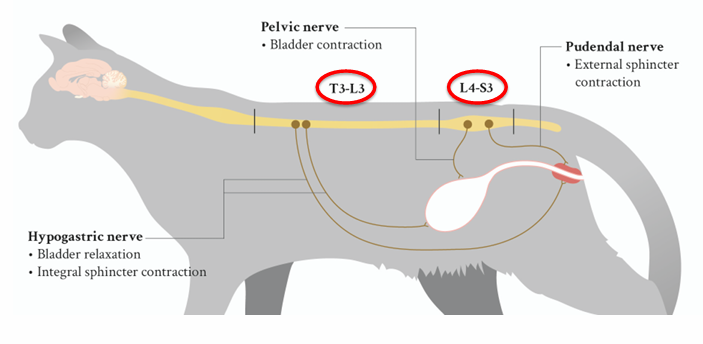
What dysfunction also occurs with spinal cord dysfunction
Bladder
Hypogastric nerve
Bladder relaxation
integral sphincter contraction
Pelvic nerve
Bladder contraction
Pudendal nerve
External sphincter contraction
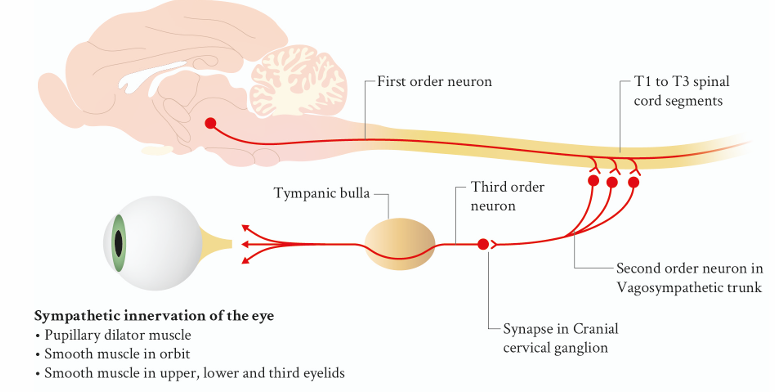
What type of innervation of the eye runs through how much of the spinal cord
Sympathetic innervation of the eye runs through entire cervical spinal cord
What are the typical clinical signs for spinal cord disease
Ataxia, paresis, plegia
Spinal hyperaesthesia
Bladder dysfunction
Gait abnormality typically characterized by COMBINATION of ataxia and paresis:
Proprioceptive or spinal ataxia
Define ataxia
A- (G) without
-taxis (G) order
Synonym = Incoordination
Sensory phenomenon
Spinal or proprioceptive ataxia in spinal disease
Define paresis
Decreased voluntary movement
Motor phenomenon
ambulatory and non-ambulatory paresis
can be UMN or LMN in nature
Define plegia
Absence (complete loss) of voluntary movement
mono, hemi, para, tetra
TRUE OR FALSE
the spinal cord has no pain receptors
True
What structures around the spinal cord have an abundance of pain receptors
Meninges
intervertebral disc
periosteum
TRUE OR FALSE
Intrinsic spinal disorders are really painful (degenerative myoelopathy)
will not be painful
What sign can help in finding the most likely differential diagnosis
Spinal hyperaesthesia
Define urinary/fecal continence
Ability to fill and empty bladder/intestines voluntarily d
define urinary/faecal incontinence
loss of ability to fill and empty bladder/intensifies voluntarily
Can be UMN or LMN
What happens to urinary incontinence when the lesion is located in the thoracolumbar spinal cord segments
UMN bladder
increased tone detrusor muscle
increased tone urethral musculature
What happens to urinary incontinence when the lesion is located in the S1-S3 spinal cord segments
LMN bladder
decreased tone detrusor muscle
decreased tone urethral musculature
What does an upper motor neuron bladder feel like on palpation/presentation
Large an full bladder, feels firm and turgid
resistance to manual expression
inconsistent leakage from overly full bladder
overflow incontinence
risk of bladder wall damage
Persistent atonic bladder wall
caused by over stretching
What does an lower motor neuron bladder feel like on palpation/presentation
Decreased bladder tone, flaccid bladder
easily expressed
can leak urine spontaneously
skin irritation (urine scald)
Persistent UTI
What are the associated issues with urine retention
UMN and LMN bladder result in both urine retention
Increases UTI risk
Occur commonly in non- ambulatory spinal patients
what does emptying the bladder for non ambulatory spinal patients prevent
Development of UTI
damage bladder wall by overstretching
overstretching can result in persistent bladder atony
urine leaking resulting in urine scald
What are some methods for bladder emptying
Manual bladder expression
repeated aseptic catheterisation
indwelling foley catheter with closed collection system
What is cauda equina compression associated with
Associated with clinical signs than dogs with spinal disorders
different pathophysiology and principles of regeneration
What are the common signs of cauda equina syndrome
Often vague, unspecific clinical signs
Paresis WITHOUT ataxia
Pelvic limb lameness
Spinal hyperaesthesia can be present
Often pain on extension hips
Can be painful on dorsal extension tail
Decreased tail tone
Urinary/faecal incontinence
Often no neurological deficits
What posture is seen on neuro exam of spinal and lumbosacral exam
Crouched kyphosis
low head carriage
schiff-sherrington
What is the schiff sherrington posture
Acute T3-L3 spinal cord injuries
Borders cells (L1-L7 spinal cord segments)
Project to cervical intumescence
Provide inhibition to extensor muscles thoracic limbs. “Disinhibtion”
Paraplegia with increased extensor tone thoracic limbs
Differentiation from cervical lesion:
Thoracic limbs neurologically normal
Indication of localisation, NOT prognosis
What is gait like in a neuro exam of spinal and lumbosacral exam
Often combination of ataxia and paresis in animals with spinal cord disease
Paresis or lameness in animals with lumbosacral disease
What is proprioception like in a neuro exam of spinal and lumbosacral area
reliable indicator for presence of neurological disease
Proprioceptive deficits can be seen in animals with spinal, brainstem and forebrain diseases
what is the sequence of progressive neurological deficits with acute spinal disease
Proprioceptive deficits (occur before gait)
Paresis and ataxia
plegia
bladder dysfunction
tail dysfunction
pain sensation/nocioception
What is spinal reflexes like in a neuro exam of spinal and lumbosacral exam
Withdrawal reflex and patella reflexes
Cutaneus trunci reflex
Differentiation UMN and LMN signs
Spinal cord and neuromuscular (neuropathy)
Patella reflex can be “physiologically” absent in:
Older dogs (symmetrical)
After stifle surgery
Withdrawal reflex and nociception are not the same
What does an absent of decreased spinal reflex suggest
Lesion is localised in the reflex arc
does not give prognostic information
differentiation UMN and LMN signs
what is the cutaneous trunci reflex
‘Panniculus reflex’
Pinching the skin over the dorsum and observing a muscle twitch
Between T2 and L4-L5
(absent in neck and lumbosacral region)
Lesion is located approximately two
vertebrae proximal of ‘cut-off ‘:
Unreliable to predict specific localisation
Confirmation of thoracolumbar spinal injury
IF neurological deficits are observed in animals with lumbosacral disease, this is often characterised by what nerve dysfunction
Sciatic nerve
How does lumbosacral disease cause nerve dysfunction and where
Exits the L7-S1 intervertebral foramen as the sciatic nerve
Splits more distally into
Peroneal nerve, which innervates dorsal part distal limb
Tibial nerve, which innervates plantar side distal limb
Tibial nerve dysfunction most obvious in dogs with lumbosacral disease
What is seen in tibial nerve dysfunction
Dropped hock
Plantigrade stance in cats
Decreased tarsal innervation can result in ‘characteristic’ gait with overflexion of the tarsus
Decreased muscle tone distal from tarsus
Loss of hock flexion during withdrawal
What is palpation like in a neuro exam of spinal and lumbosacral exam
Keep this part for the end
Sometimes against intuition
start with gentle palpation
What is nocioception like in a neuro exam of spinal and lumbosacral exam
Provide painful stimulus
pinching nailbed with
Fingers: superficial pain perception
Artery forceps: deep pain perception
Look for conscious reaction
Vocalisation
trying to flee
trying to bite
only necessary to test in
plegic animals
differentiation stupor from coma
Suspicion of sensory neuropathy
extremely are
if necessary, don’t test it
What is the clinical presentation with clinical signs and abnormalities
Clinical signs
No gait abnormalities, but spina hyperaesthesia
Combination of ataxia and paresis
paresis → plegia
bladder dysfunction
urine retention or leakage
Abnormalities
Proprioceptive deficits
intact or abnormal spinal reflexes
spinal hyperaesthesia present or absent
pain sensation can be decreased in plegic animals
What syndrome can be seen in animals with cervical spinal disease
Horner’s
What are the clinical signs of hooch
Ipsilateral miosis
enipthalmos
third eyelid protrusion
ptosis upper eyelid
normal vision
What is the concept of UMN and LMN lesions
UMN= situated CNS and controls LMN
LMN- final pathway between CNS and target organ
What clinical signs do you see on a LMN lesions
Loss of stimulation or excitation
decreased muscle tone
Flaccid paralysis
Decreased spinal reflexes
What clinical signs do you see on a UMN lesion
Loss of inhibition= disinhibition
Excessive stimulation or excitation
increased muscle tone- spastic paresis
increased spinal reflexes
what is the theory behind how LMN and UMN lesions differ
Spinal cord lesion causes LMN signs at site of injury and UMN signs caudal from site of injury
in clinical practice: LMN signs only visible if lesion localised at the cervicothoracic or lumbosacral intumescence
basis for localising spinal cord lesions to specific spinal cord segments
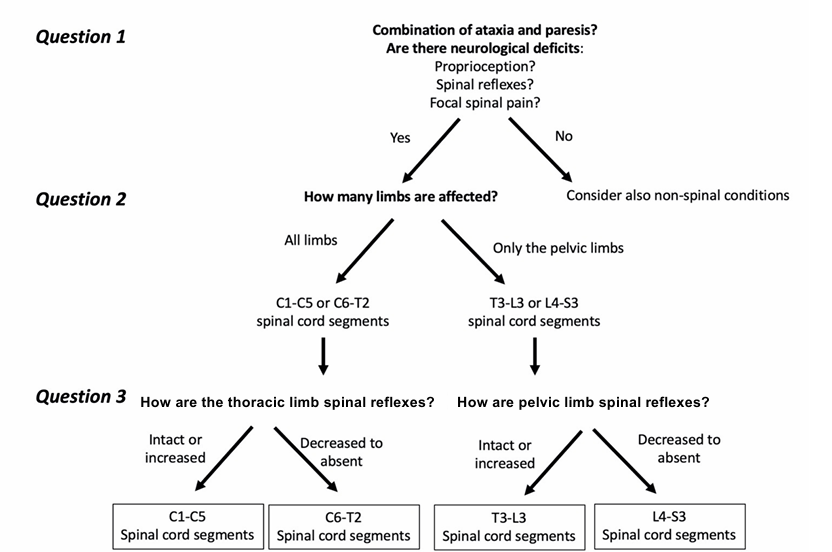
What questions do you ask to localise a lesion
What are the ways in diagnosing/ getting differentials
DAMNIT V
5 finger rule
How does the 5 finger rule work
Start with localisation:
Onset:
Difference between acute and per-acute!!
Chronic
Progression:
Not many disorders improve spontaneously
Don’t get fouled by first 12-24 hours
Symmetry:
Not many disorders are truly asymmetrical
Pain:
Presence of pain excludes several conditions
Not all painful conditions are necessarily associated with pain
Signalment:
Species → cats vs dogs
Breed: not every Dachshund has IVDD though
Age
What are the common differentials for dogs
Type I intervertebral disc disease – 29.8% § Intervertebral disc extrusion (IVDE)
Type II intervertebral disc disease – 19% § Intervertebral disc protrusion (IVDP)
Ischaemic myelopathy – 9.6% • Neoplasia - 8.8%
Syringomyelia – 5.8%
Immune mediated myelitis – 5.8%
Acute non-compressive nucleus pulposus extrusion § high-velocity low-volume disc extrusion – 4.8%
Degenerative lumbosacral stenosis – 2.8% § Most common cause of lumbosacral disease
Cervical spondylomyelopathy – 2.0%
Steroid responsive meningitis arteritis – 1.8%
Spinal arachnoid diverticulum – 1.8%
What are the common differentials for cats
Neoplasia other than lymphoma - 19.9%
Intervertebral disc disease – 19% § Type I and Type II
Vertebral fracture and luxation – 15.4%
Ischaemic myelopathy – 10%
Feline infectious peritonitis virus - 8.1% § Young cats!
Spinal lymphoma – 7.2% § Young cats!
Thoracic vertebral canal stenosis – 5.0% § (no information in textbooks)
Acute non-compressive nucleus pulposus extrusion – 5.0%
Traumatic spinal cord contusion – 3.6%
Spinal arachnoid diverticulum - 3.2%