PLTW BIOMED 2020-2021: Lesson 3.1
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
What is the role of an epidemiologist?
study trends in health issues and outbreaks in populations and deploy public protocols to maintain the health of a nation
outbreak/epidemic
a sudden increase in the occurrence of a disease in a localized area
pandemic
an outbreak that has spread across several countries or continents and affects a lot of people
endemic
a disease constantly present in a community within a specific geographic area.
name all 6 agents of disease
virus, bacteria, protist, prion, fungi, helminth
are viruses living or non-living? what's an example of a common virus?
non-living. Influenza- The Flu
are prions living or non-living?
non-living proteins
(little thingies that make brain fold abnormally and result in dementia)
answer the following questions about bacterium:
a.) living or non-living?
b.) prokaryote or eukaryote?
c.) unicellular or multicellular?
bacteria:
a.) living; microscopic
b.) prokaryotic
c.) unicellular
answer the following questions about protists:
a.) living or non-living?
b.) prokaryote or eukaryote?
c.) unicellular or multicellular?
protist:
a.) living; microscopic
b.) eukaryotic; animal-like organisms
c.) unicellular
answer the following questions about fungi:
a.) living or non-living?
b.) prokaryote or eukaryote?
c.) unicellular or multicellular?
fungi:
a.) living; both microscopic and macroscopic types exist
b.) eukaryotic
c.) multicellular
answer the following questions about helminths:
a.) living or non-living?
b.) prokaryote or eukaryote?
c.) unicellular or multicellular?
helminths:
a.) living; both microscopic and macroscopic types exist
b.) eukaryotic
c.) multicellular
(wormies)
how are prions spread and treated?
exposure occurs through contaminated medical equipment, receiving organs of infected individuals, and/or prion tainted meat. There is no cure for prions but medications can slow down the disease
how are viruses spread and treated?
can spread through touch, saliva, blood, or sexual contact. Viruses do not replicate on their own, they need a host. Antivirals may help in some cases; over-the-counter medication help relieve symptoms
how are bacteria spread and treated?
through an orifice (eyes/nose/mouth), through a wound, contaminated food, inhalation, or sexual contact. Antibiotics can be used to treat bacterial infections
how are protists spread and treated?
takes place when food/water contaminated with feces of an infected individual is ingested by another. some infections can be treated through antiprotozoal.
how are helminths spread and treated?
consumption of contaminated foods or water or getting bit by the infected insect. can be treated with deworming medications (they're the little wormie things)
how are fungi spread and treated?
when the spores (reproductive cells) of the fungi land or are inhaled by the host. treated using antifungals.
define reservoir and what role it plays in chain of infection
any person, animal, or environment in which an infectious agent normally lives and multiplies. it is where an infectious agent is originally resided before it leaves to be transmitted.
define transmission and what role it plays in chain of infection.
transmission is the action of an infectious agent entering its host. the two modes of transmission are direct or indirect.
define host and what role it plays in chain of infection.
the host is the actual organism that is vulnerable to the infection. the host provides a "home" for the infectious agent.
what are the 6 components of the chain of infection and examples of each?
1. agent of disease (ex. prion, virus, bacteria)
2. reservoir (ex. people, animals, environment)
3. susceptible host (ex. anybody, especially people with weakened immunity)
4. portal of entry (ex. skin, respiratory/gastrointestinal tracts, urogenital, conjunctiva)
5. mode of transmission (indirect or direct)
6. portal of exit (same examples as portal of entry)
what is the difference between direct and indirect contact? provide examples for each
direct- when a susceptible host touches an infected individual or is exposed to their body fluids.
indirect- when a susceptible host inhales infected particles, touches an infected object, or is bitten by an infected insect.
presymptomatic spread
spread of disease by infected individuals BEFORE they develop symptoms.
asymptomatic spread
spread of disease by infected individuals who NEVER develop symptoms.
symptomatic spread
spread of disease by infected individuals who HAVE AND SHOW symptoms.
define clinical and subclinical cases and explain the difference between them.
subclinical cases- when the infected individual does not seek care from their doctor and rests at home instead. ("invisible" cases)
clinical cases- when infected individuals seek care from their medical providers ("visible" cases)
what's a viral test? what does it tell you?
a test that tells you whether you currently have the infection or not
what's an antibody test? what does it tell you?
a test that tells you whether you had a past infection or not
what's innate immunity?
innate- immune defense mechanisms that we are born with. keep anything outside of us from coming in (tears, phagocytes, stomach acid)
what's acquired immunity?
specific immune defense mechanisms that are acquired over a lifetime and use antibodies to respond to antigens (vaccines, and your body's own antibodies)
what are the two types of acquired immunity?
1. active- following infection recovery or from a vaccine. your body makes your own antibodies as well.
2. passive- acquired from mother's placenta or breastfeeding.
what is an antigen?
a toxin or other foreign substance that induces an immune response in the body.
explain the function of T-cells
when an antigen gains entry to the body, the body responds by sending T-cells to the site of infection. they work to kill the pathogen by secreting toxins or by ingesting and digesting the toxins.
explain the function of B-cells
a type of white blood cells that are produced in the bone marrow. B-cells produce antibodies
explain the function of antibodies
block pathogens from entering cells, prevent bacteria from ingesting nutrients, bind toxins released by pathogens to prevent them from harming us
Naturally acquired immunity
immunity gained when a person has been exposed to a pathogen and their immune system helped them recover. this is due to the memory of T-cells
artificially acquired immunity
immunity that results from a vaccination
what does the term R-naught (R0) refer to?
a measurement for how rapidly an infection is spread (the expected number of new infections that are spread by an already infected person)
what does an R0 value of greater than 1 mean? (R0 > 1)
it means that every person that has that infection will spread it to more than one person. considered very infectious
what does an R0 value of less than 1 mean? (R0 < 1)
it means that every person that has the infection will spread it to less than one person. considered not very infectious
what does an R0 value of equal to 1 mean? (R0 = 1)
it means that every person that has the infection will spread it to 1 person. considered somewhat infectious
how do you calculate an R-naught value?
R0 = number of new cases / number of existing cases.
when does someone need to be isolated, and how is that different from quarantine?
isolation- when a patient who has tested positive for the disease is kept away from others.
quarantine- separating people who may have been exposed to the virus in case they become sick. (individuals may self quarantine even when not exposed)
primary prevention
strategies to stop injury, illness, or disease from even occurring
secondary prevention
strategies for early detection, diagnosis, and prompt treatment to prevent the development of more severe issues
tertiary prevention
strategies to support and rehabilitate individuals with serious illness.
what are NPI's? examples?
non-pharmaceutical interventions; social distancing, face masks, hand-washing, quarantine, frequent sanitization, PPE
what are PI's? examples?
pharmaceutical interventions; laboratory testings, vaccines
what is medical surge?
when the number of new patients challenges or exceeds a hospital's ability to serve all of them.
how can preventive measures reduce the potential for medical surges?
when preventive measures are followed accordingly, fewer people are infected, therefore fewer patients need to be placed in a hospital. this way there's a lower chance of reaching the maximum capacity of patients.
what is surge capacity?
A measure of how many patients a medical facility can triage, treat, and manage IN ADDITION TO its normal average number of patients.
what is the process of creating a new drug or vaccine?
review the flowchart on "Activity 5_ Developing A Vaccine" in biomed canvas module of 2/24/21
what are the 5 main types of vaccines?
1 . Viral vector vaccines.
2. DNA vaccines
3. RNA vaccines
4. Live attenuated vaccines
5. Inactivated, protein-based vaccines
how do viral vector and DNA vaccines provide immunity?
they deliver a SARS-CoV-2 gene (made of DNA) into our cells so that the DNA can be transcribed and then translated into SARS-CoV-2 surface proteins. when these are released out of the cell, the immune system targets them. when the same surface proteins enter the body during an actual COVID-19 infection, the immune system will know how to destroy it immediately (just get a general idea, do not need to know word for word)
how do RNA vaccines provide immunity?
once the mRNA is injected into our cells, it is translated into SARS-CoV-2 surface proteins. these proteins are released from the cells and the immune system targets them. this "immune system memory" will then know how to destroy these proteins promptly if an actual COVID infection occurs. (the same process as DNA vaccines, just skip the transcription step)
how do live attenuated vaccines provide immunity?
Live Attenuated = Alive but weak
inject a weaker version of the SARS-CoV-2 virus that the immune system responds to. it is not strong enough to make us sick but strong enough for antibodies to be produced, which provide protection against an actual COVID infection
how do inactivated vaccines provide immunity?
carry a SARS-CoV-2 surface protein combined with adjuvant to enhance immune response. immune system recognizes pathogen and targets it + creates antibodies. antibodies protect from future COVID infection.
what is a nosocomial disease?
HAI (hospital-acquired infection)
these infections are acquired during patients' visit at the hospital
what are two ways we can use to help identify a bacterial species? (How do they help us ID the species?)
1. morphology- the shape of their cells
2. their ability to metabolize certain compounds
what does it mean to culture a bacterial sample on an agar plate?
it means to GROW bacteria on the agar plate for observing it
briefly describe the process of aseptic technique, why it's important, and some examples
aseptic technique- performing a procedure under totally clean, sterile conditions.
important because it ensures that no contaminants or infectious agents are spread
ex. hair tied back, food/drinks away from lab, PPE worn, disinfect work surfaces, wash hands before and after
what is an isolation streak? why do we use the quadrant method to streak bacteria?
an isolation streak is a process by which bacteria are streaked onto an agar plate to separate the different species of bacteria.
we use the quadrant method for this to dilute bacteria on the agar so that they spread well enough apart that when they grow, the colonies will be isolated.
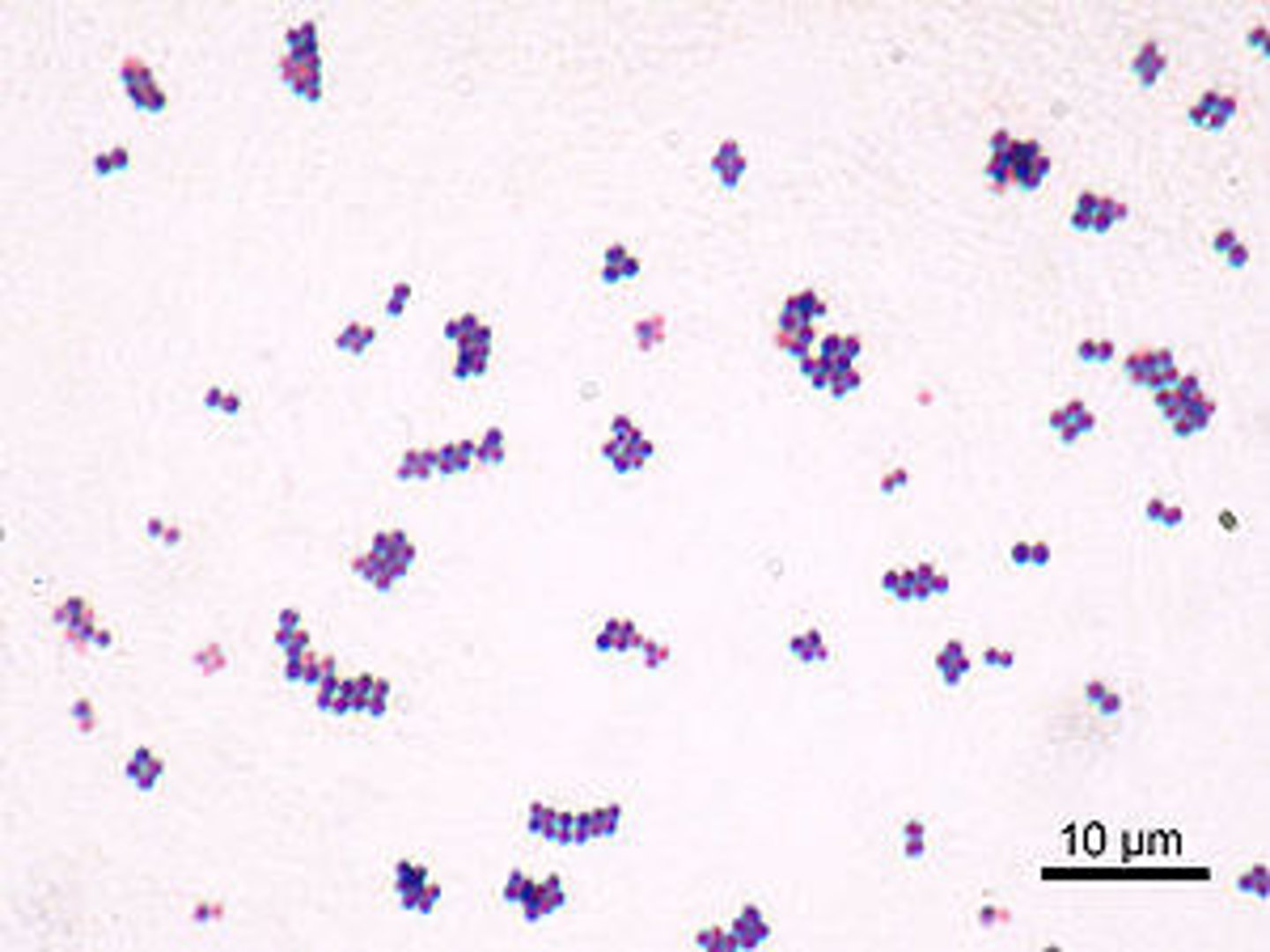
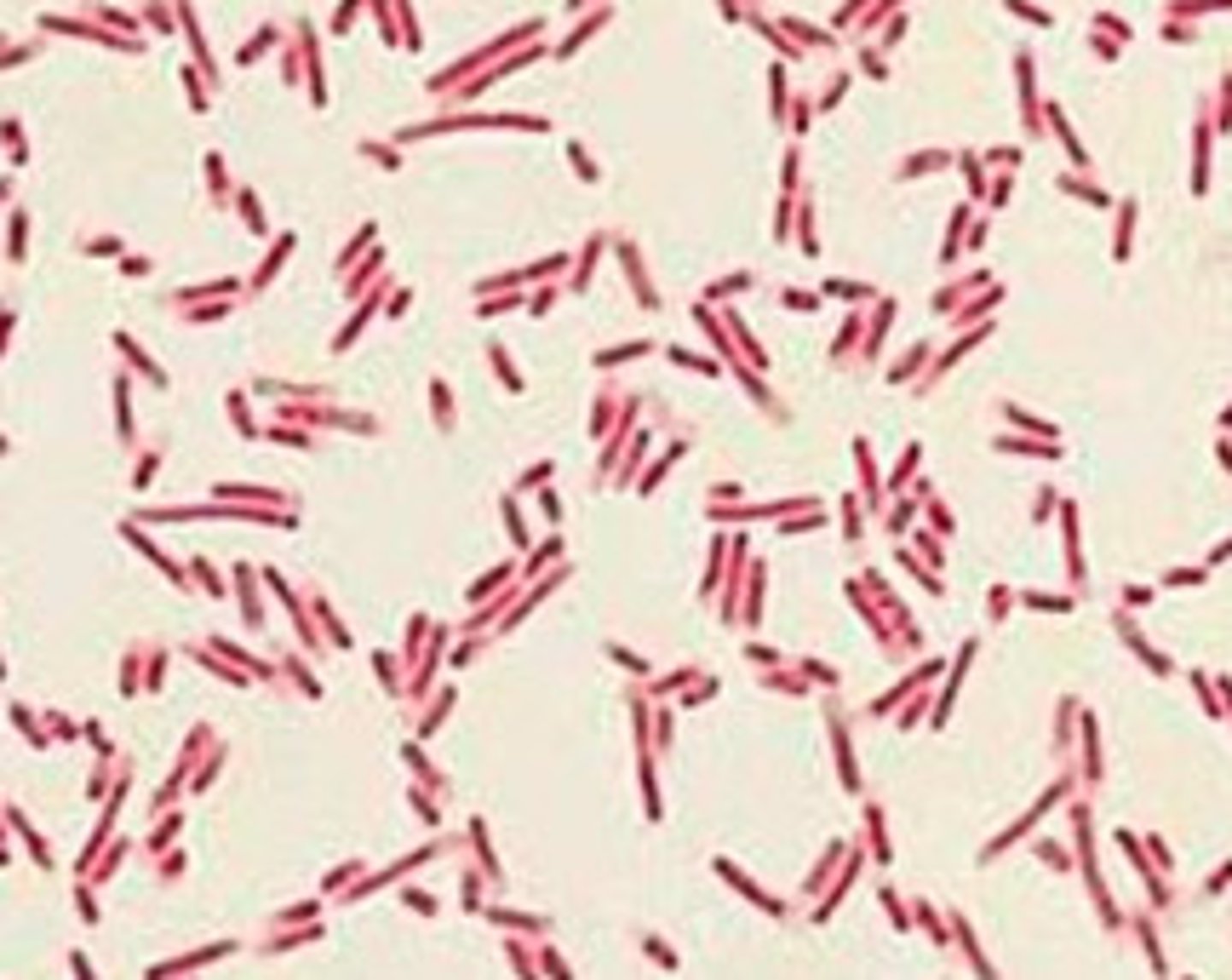
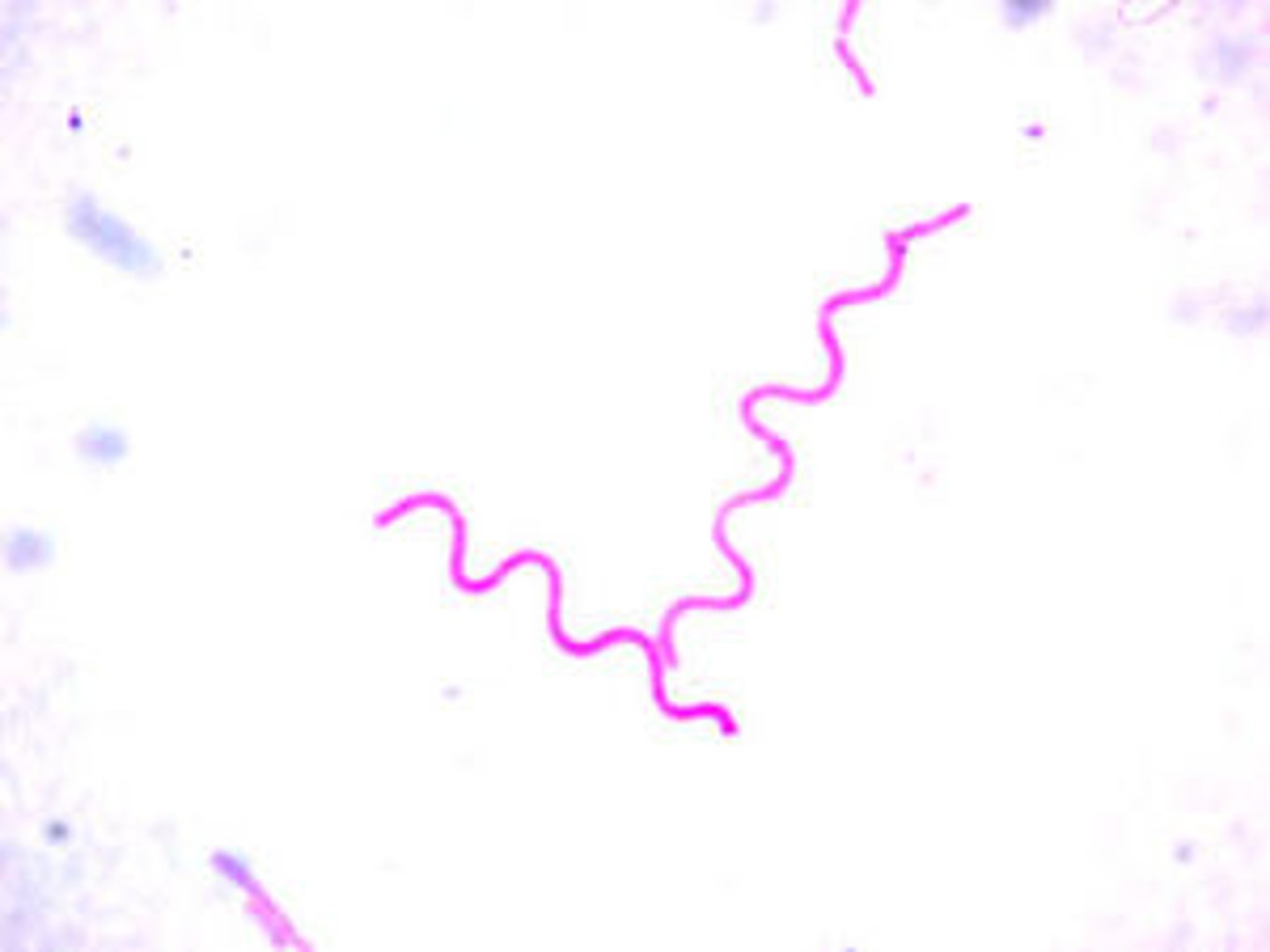
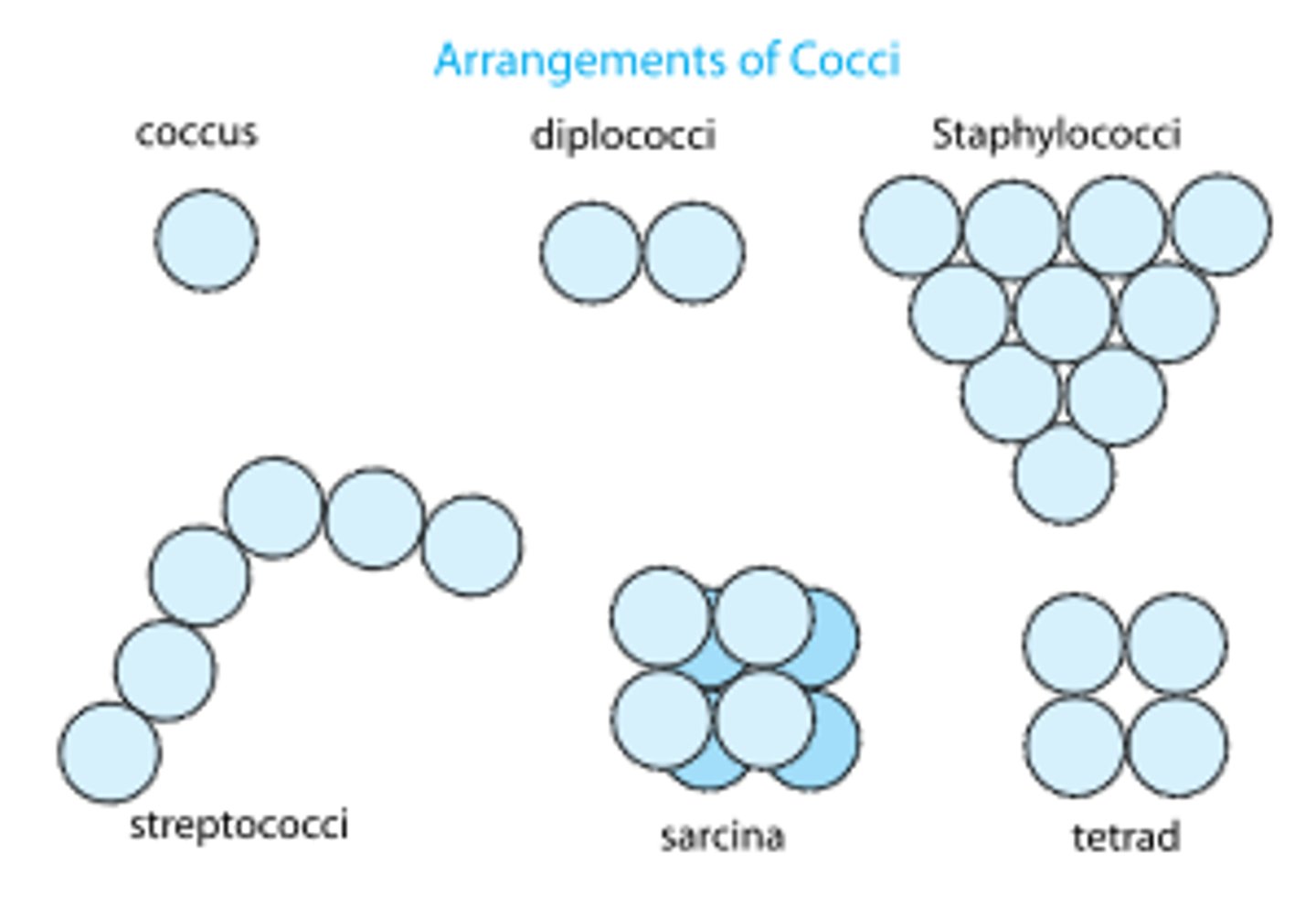
what are three cellular characteristics we can use to identify a bacterial species under a microscope?
1. morphology (shape of cells)
2. cell arrangement (how they group)
3. cell wall composition
what are the three types of cellular morphology
1. coccus
2. bacillus
3. spirillum
what does a coccus look like?
spherical
what does a bacillus look like?
rod shaped
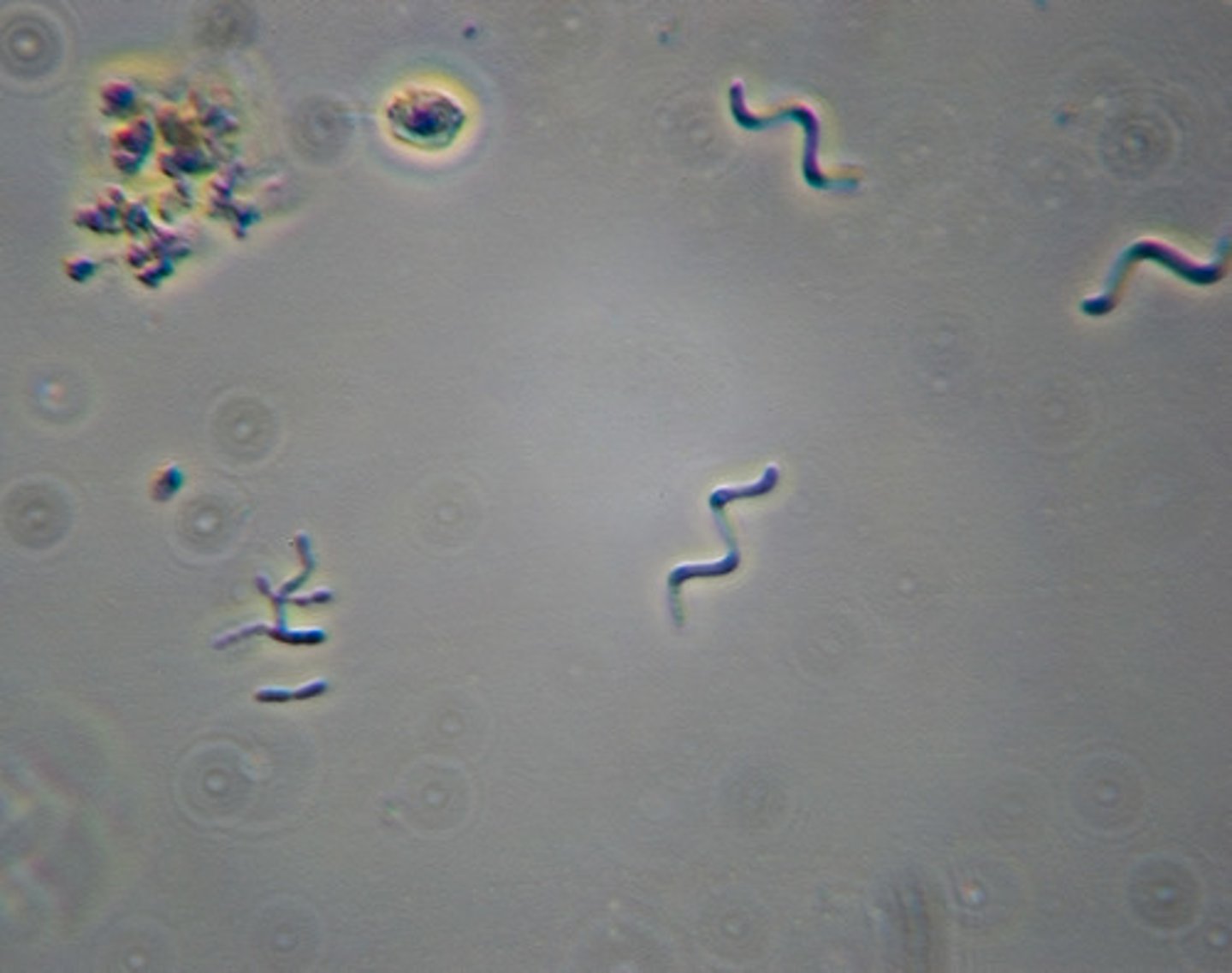
what does spirillum look like?
small spirals/cords
what are common arrangements for bacilli?
individual or chains
what are common arrangements for cocci?
individual, groups of two (DIPLOCOCCI), four (TETRAD), or will form chains/large groups.
what are common arrangements for spirillum?
spirilla present as individual cells.
what is the purpose of a gram stain test?
to differentiate between bacteria into one of the two groups based on their cell wall composition
what is peptidoglycan? which cells have more/less of it?
peptidoglycan is a sugar and amino acid-rich substance
gram-negative has less peptidoglycan
gram-positive have more peptidoglycan
which colors (pink/purple) are indicative of what kind of bacteria (positive/negative)
positive- purple
negative- pink
what are the 5 stages of a gram stain?
1) fixation --> 2) crystal violet --> 3) iodine treatment --> 4) decolorization --> 5) counter stain safranin
explain the purpose of all stages of a gram stain
1st step fixation- cells on a slide are passed through a flame so that they don't rinse off or move around during the process
2nd step crystal violet- a stain that penetrates the peptidoglycan layer and stains the cells purple
3rd step iodine treatment- iodine is applied to the cells and it binds with the crystal violet to form a CVI complex
4th step decolorization- ethyl alcohol is applied to the cells
--> in gram-positive, alcohol causes the water to leave the cell, blocking the CVI from leaving
--> in gram-negative, alcohol dissolves the outer membrane and CVI leaves the cell
5th step counterstain- safranin is applied to the cells
--> in gram-positive, safranin penetrates the cell but it is not seen b/c it's lighter than CVI
--> in gram-negative, safranin penetrates the cell and stains it a reddish-pink color
which stain (safranin/crystal violet) dyes which type of cell (gram positive/negative)?
crystal violet: gram-positive (PURPLE)
safranin: gram-negative (REDDISH-PINK)
which type of bacteria cell is more harmful? (positive or negative)
gram negative are usually more dangerous because of their additional lipopolysaccharide layer.
what type of infectious agent is COVID-19?
virus
what body system does COVID-19 usually affect?
respiratory
what are the signs and symptoms of COVID-19
mild- fever, dry cough, fatigue, coughing up phlegm, headache, joint pain, sore throat, chills, nausea, nasal congestion, diarrhea
severe- pneumonia, ARDS (makes lungs fill up with fluid), shortness of breath, faster breathing
critical- respiratory failure, septic shock, organ dysfunction/failure, or death
what types of things can impact the severity of a host's symptoms/case?
pre-existing conditions, weaker immune system, smoking/drinking, older/younger people
What are the most common ways that COVID-19 is transmitted from one host to another?
direct- touch
indirect- airborne droplets through sneezes/coughs
How does your immune system fight a COVID-19 infection?
T-cells stimulate B-cells to produce antibodies against the S protein of the virus. These antibodies coat the S-protein and block the virus from attaching to and infecting lung cells.
what type of PI's and NPI's have we used to slow the spread of COVID-19 during this pandemic?
PI's: the recent vaccines, laboratory testing and diagnosing, lock-downs
NPI's: face coverings, washing hands more often, frequent sanitization
How does SARS-CoV-2 attack a cell in order to reproduce within a host?
the E-protein helps assemble the virus within host cells and supports the release of the virus from host cells. the S-protein enables the virus to bind to lung cells in a host, infecting them.
how does a vaccine disrupt SARS-CoV-2 from invading a cell?
a vaccine for COVID-19 will familiarize your immune system to the surface proteins so that if an actual COVID-19 infection does happen, it will be destroyed before actually harming your body.