12. Latent Viral Infections: Herpes Viruses - Audia
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
Herpes Virus
Characteristics (9)
Large dsDNA genome
Common structure (enveloped virus)
Infections are often asymptomatic
Establish latency - persist for life
Can reactivate from latency
Most reactivations are asymptomatic
Re-infections can occur
Most herpesviruses cause more than 1 disease
Interfere with immune response
Human Herpes Viruses
Genome Characteristics (3)
DNA Viruses
Double-stranded
Enveloped
What are the 3 Classes of Herpesviruses?
examples of each (3, 3, 2)
Alpha:
Herpes Simplex I (HSV-1)
Herpes Simplex II (HSV-2)
Varicella-zoster virus (VZV)
Beta:
Cytomegalovirus (CMV)
Herpesvirus 6
Herpesvirus 7
Gamma:
Epstein-Barr (EBV)
Herpesvirus 8
Summary of Diseases
List diseases caused by the following Herpesviruses:
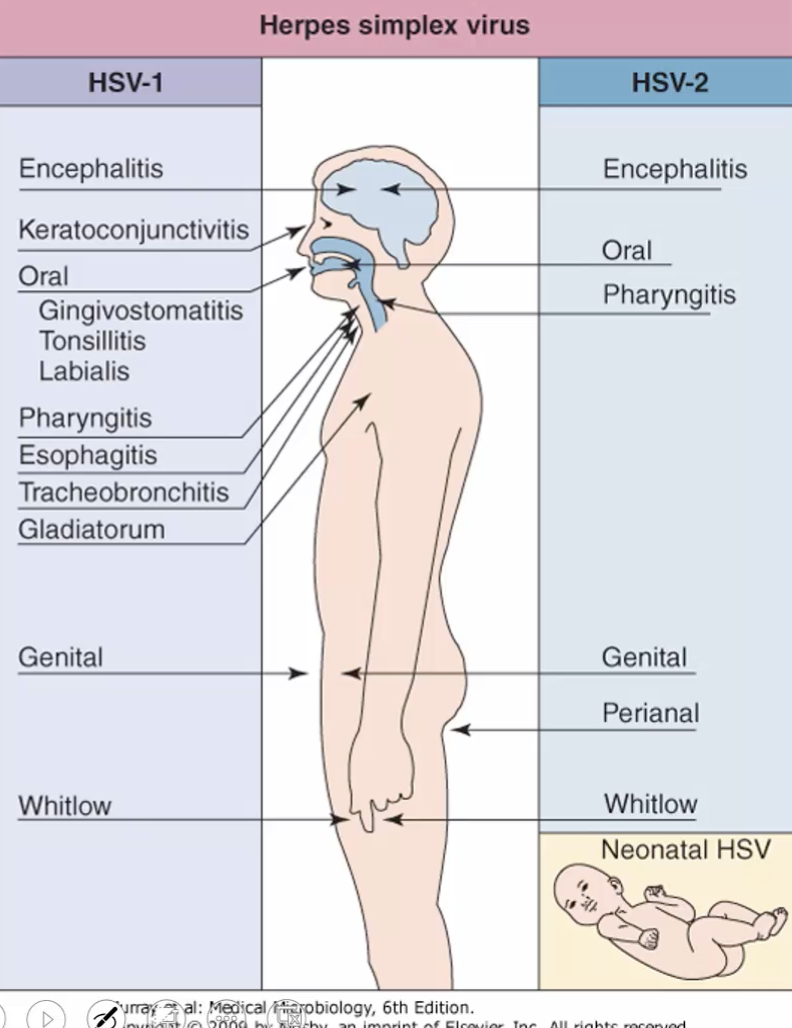
HSV-1 (3)
HSV-2 (3)
VZV (2)
HSV-1:
Keratoconjuctivitis
Gingivostomatitis
Encephalitis
HSV-2:
Genital Herpes
Neonatal herpes
Meningoencephalitis
VZV:
Chickenpox
Shingles
Summary of Diseases
List diseases caused by the following Herpesviruses:
EBV (3)
CMV (4)
EBV:
Infectious mononucleosis
Burkitt’s lymphoma
Nasopharyngeal cancer
CMV:
Cytomegalic inclusion disease
CMV mononucleosis
Pneumonia
Retinitis
Summary of Diseases
List diseases caused by the following Herpesviruses:
HHV-6
HHV-7
HHV-8
HHV-6:
Roseola
HHV-7:
Roseola
HHV-8:
Kaposi’s lymphoma
Overview of HSV Replication (8)
Replication occurs where?
Binding (attachment)
Direct Fusion (entry)
mRNA synthesis
Protein Synthesis
DNA Replication
Glycoprotein Synthesis
Assembly
Release
Replication occurs in NUCLEUS
Important HSV Enzymes (3)
what can be targeted*
DNA-dependent DNA polymerase
Thymidine kinase
Ribonucleotide reductase
Draw out Replication of Herpes Simplex Virus
Stage I
what is released? (2)
Alpha proteins (transcription regulation)
Beta proteins (DNA polymerase)
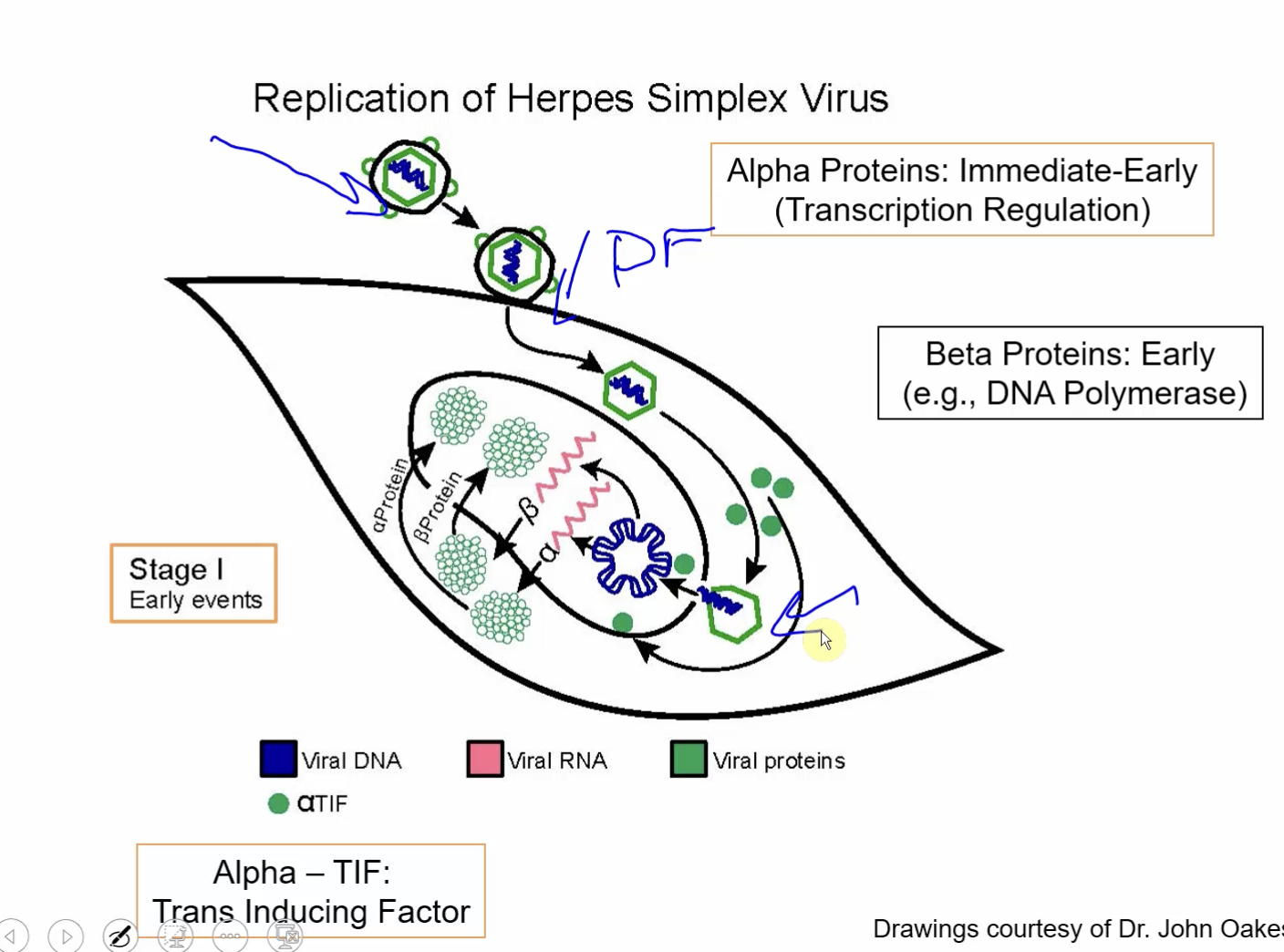
What genes/transcripts are turned on? (2)
in what order?
function of each
Alpha proteins: immediate-early
Transcription regulation
Beta proteins: early
DNA polymerase
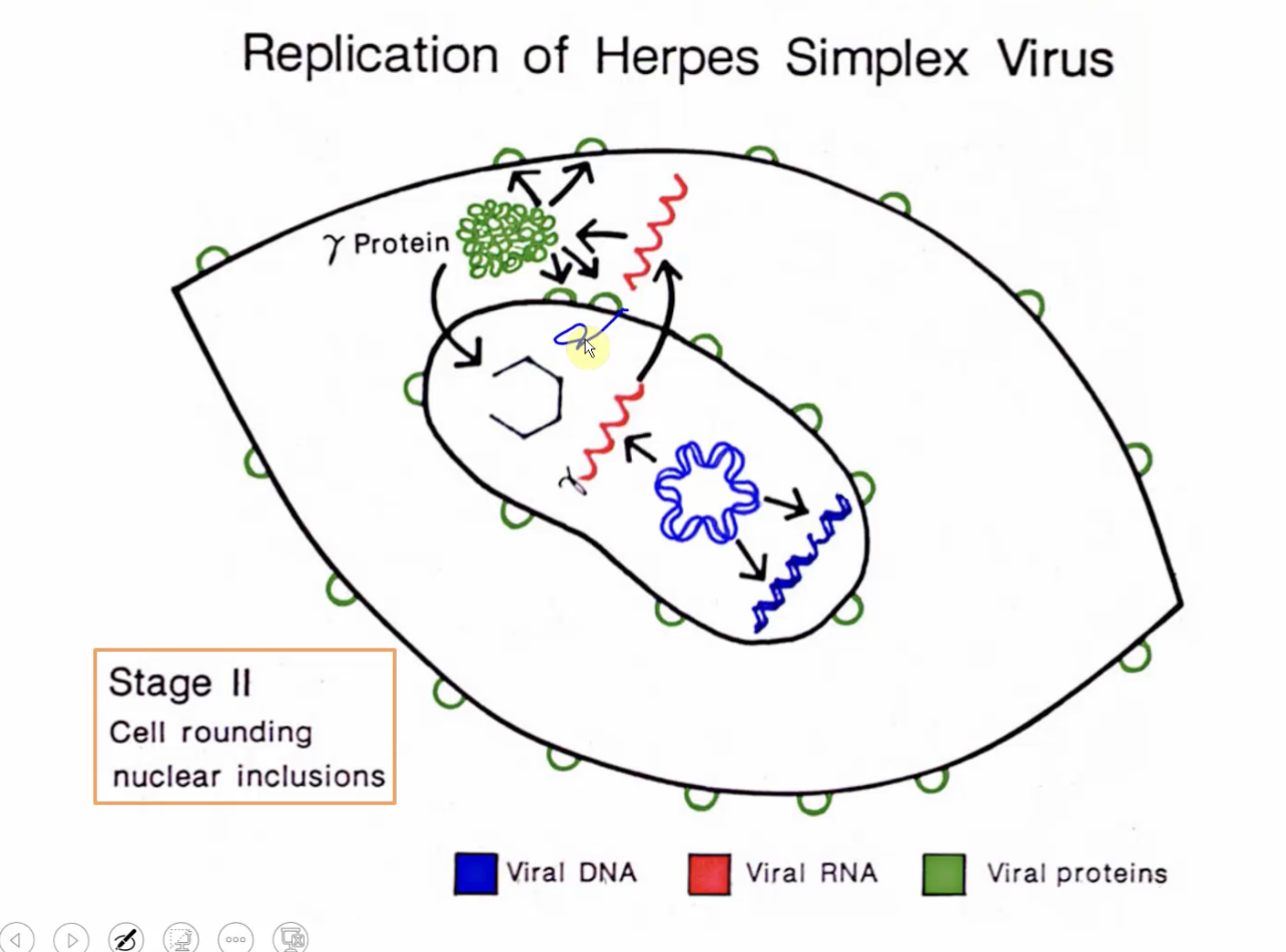
Draw out Replication of Herpes Simplex Virus
Stage II
Draw out Replication of Herpes Simplex Virus
Stage III
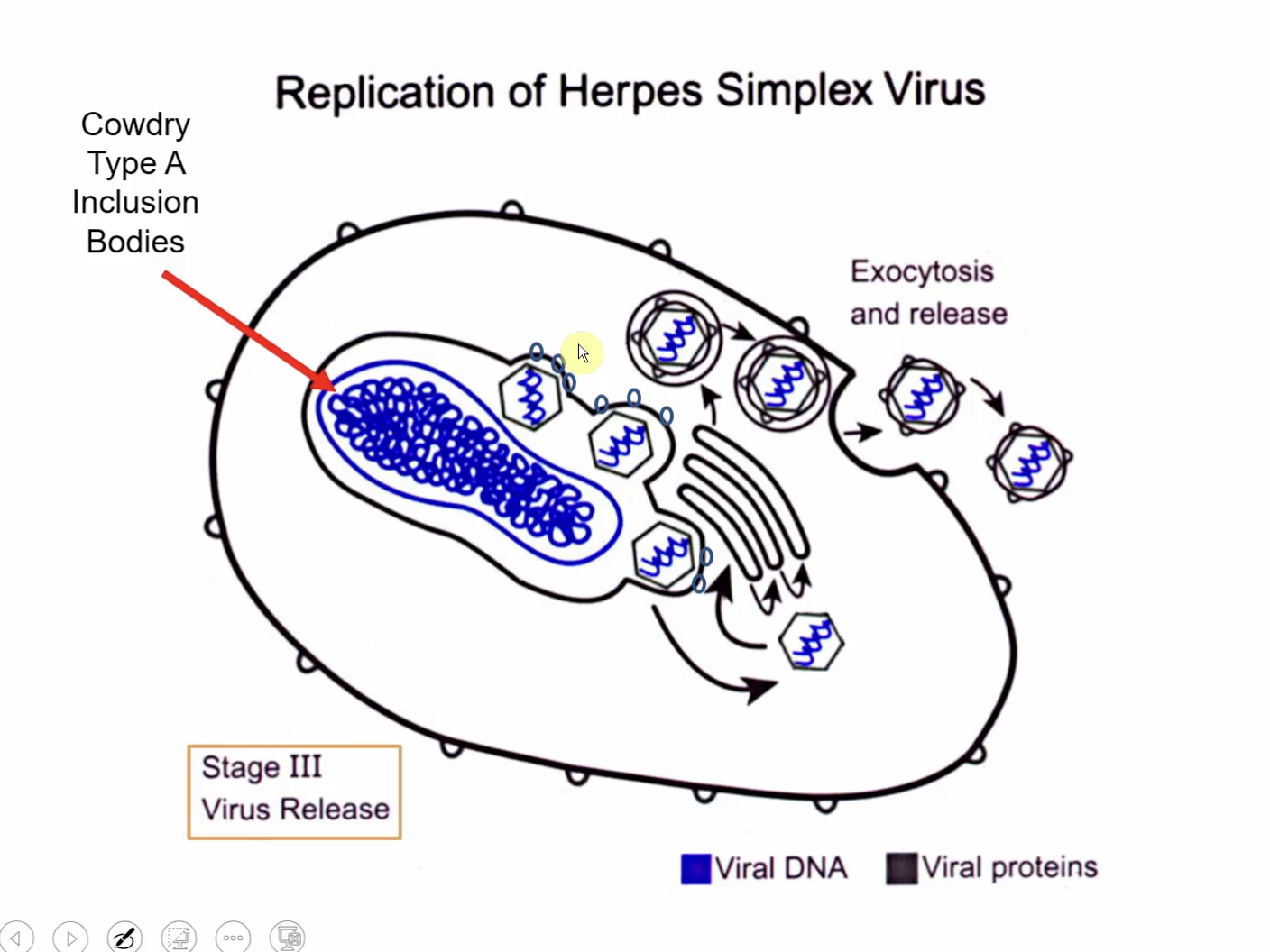
Assembly occurs where?
Nucleus! (buds from the nuclear membrane)
What are produced in Sensory Neurons?
What do they do? (2)
microRNA precursors called Latency-associated transcripts (LATs)
bind early transcripts and prevent/SILENCE their expression (early genes - alpha proteins, needed for viral replication)
prevents viral replication
Reactivation of Herpes Simplex Virus
What can reactivate? (2, etc)
What happens after? (3)
Stimuli:
stress
UV light, etc
Reactivation:
Viral replication
Transport along periphery sensory nerves
Replication in the epithelium with the production of vesicles
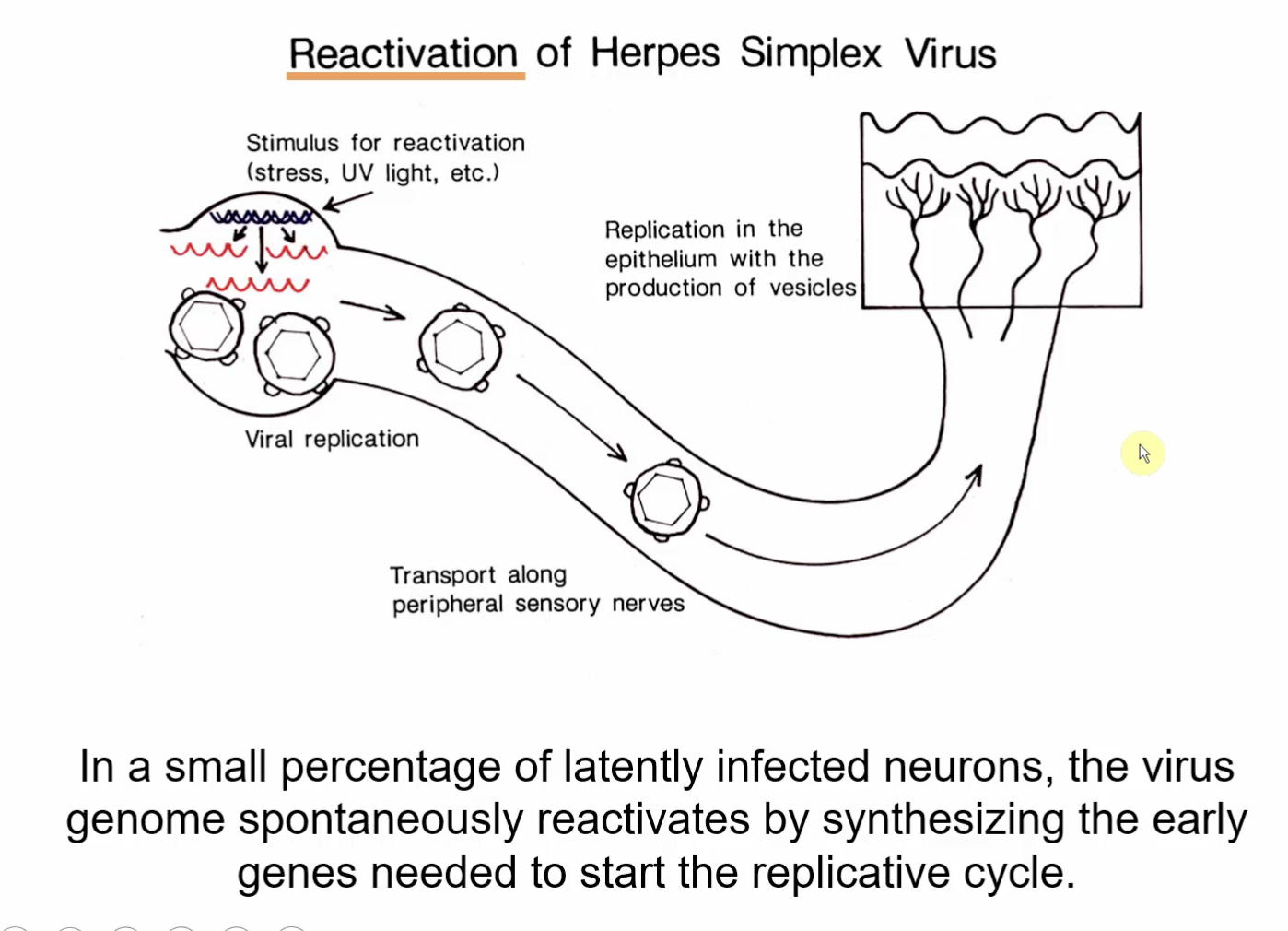
HSV uses what type of transport?
Retrograde transport
ex.) lips to the nucleus and anterograde transport back to the site of infection.
Pathogenesis of Herpes Simplex Virus
General (2)
HSV-1
HSV-2
Immunocompromised → Dissemination
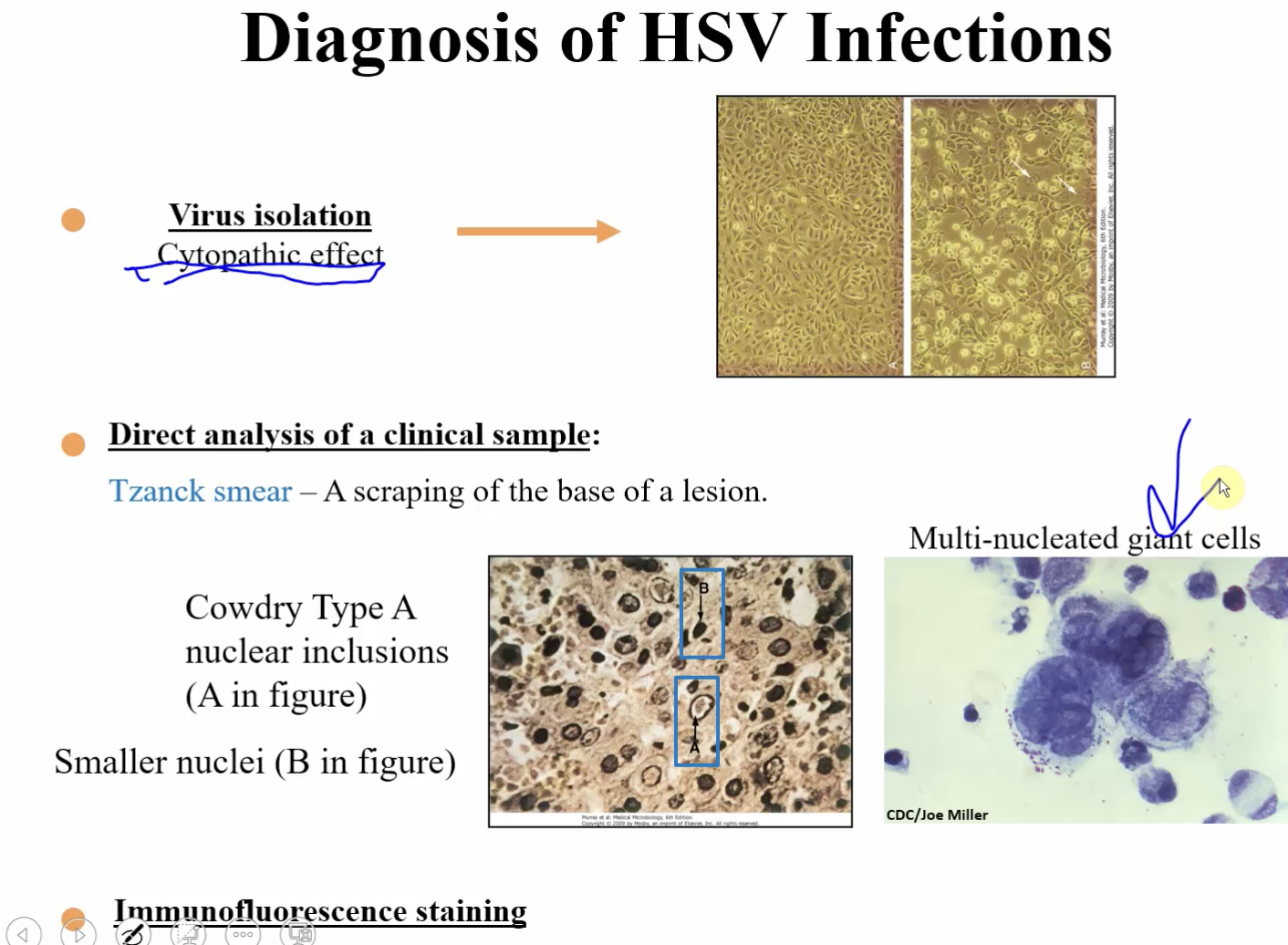
Diagnosis of HSV Infections (3)
Examples of each (1)
Virus Isolation:
Cytopathic Effect
Direct analysis of clinical sample:
Tznack Smear - a scraping of the base of a lesion
Cowdry Type A nuclear inclusions
Immunofluorescence Staining
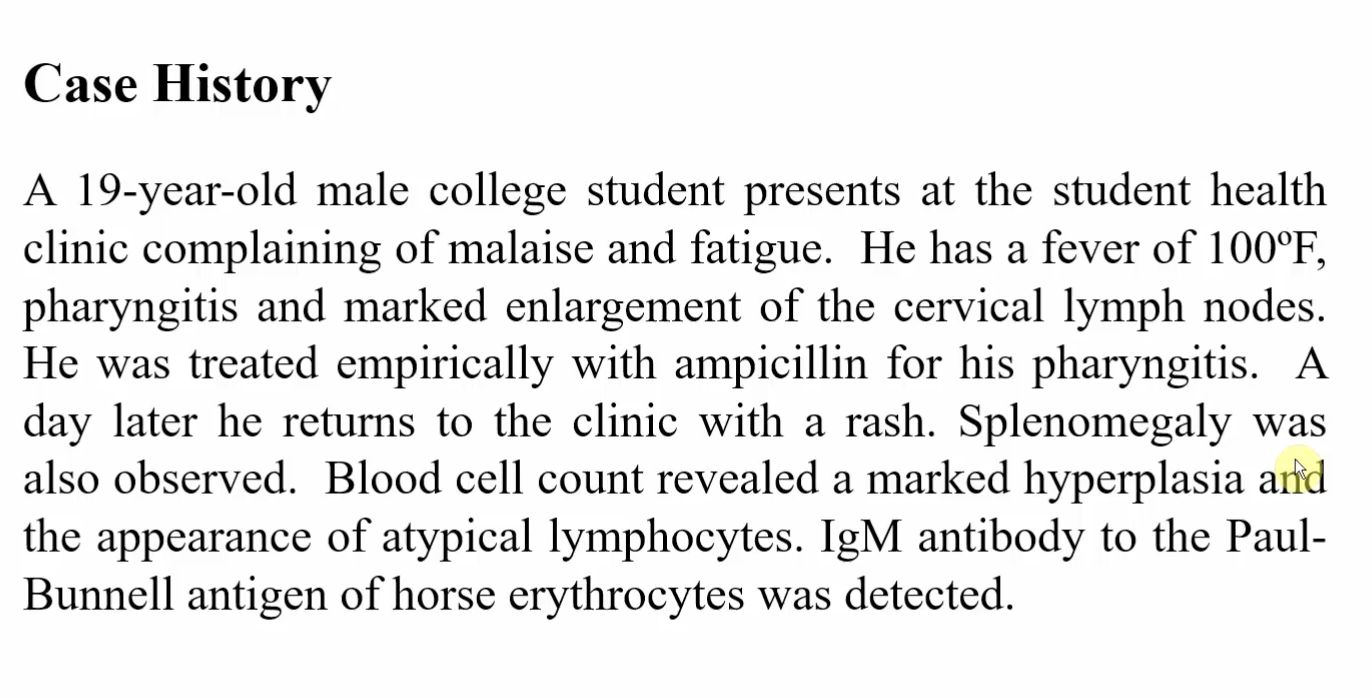
Epstein-Barr Virus
Epstein-Barr Virus
Causative agent of what?
Causally associated with what? (3)
Causative agent of Infectious Mononucleosis
Causally associated with:
Burkitt's Lymphoma
Hodgkin's Lymphoma
Nasopharyngeal Carcinoma
Epstein-Barr Virus
Replicates in what cells? (2)
Causes latent infection in what cells?
What else does it cause in these cells? (2)
Replicates in B-cells or permissive epithelial cells
Causes latent infection of B-cells
Stimulates and Immortalizes B-cells
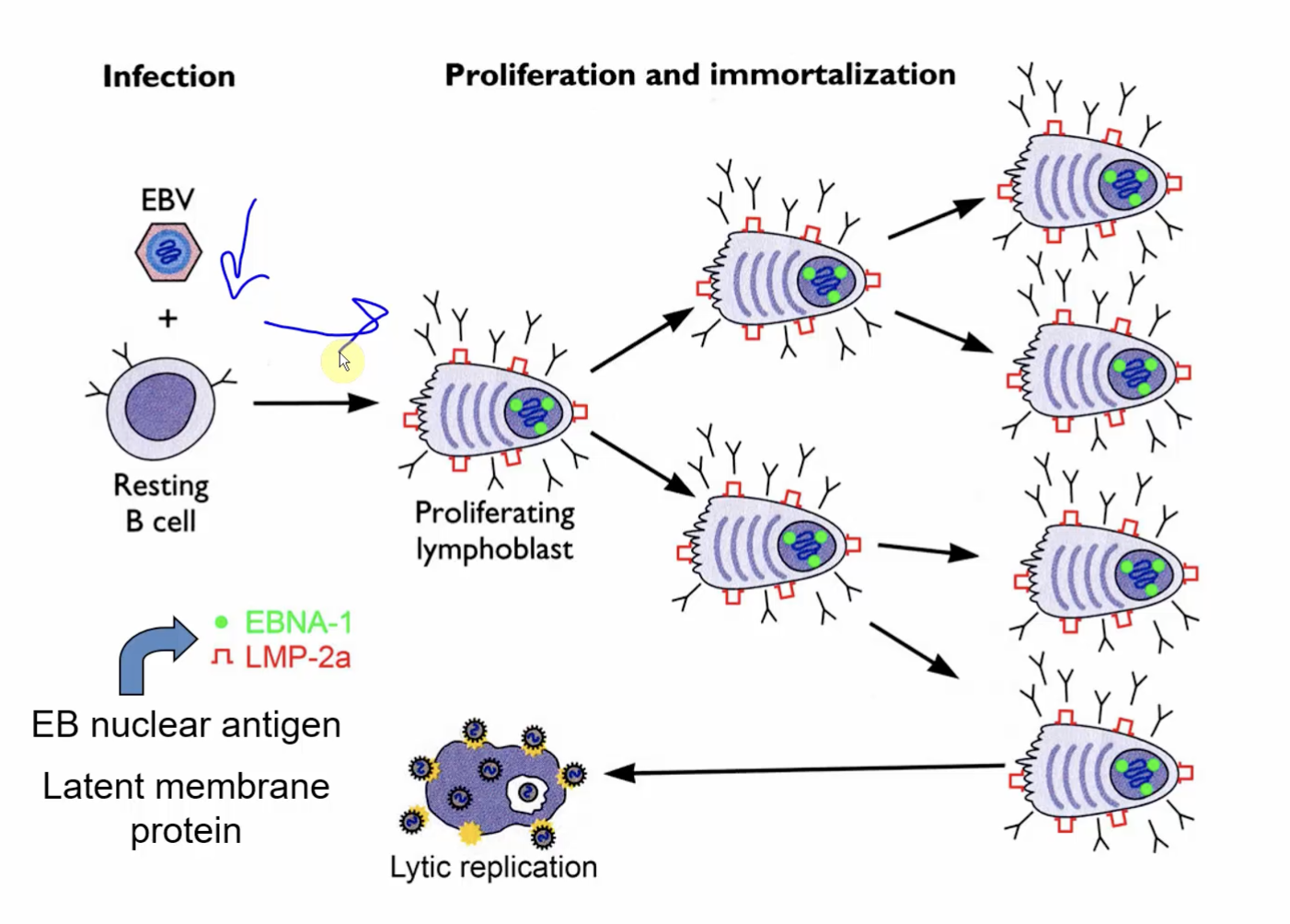
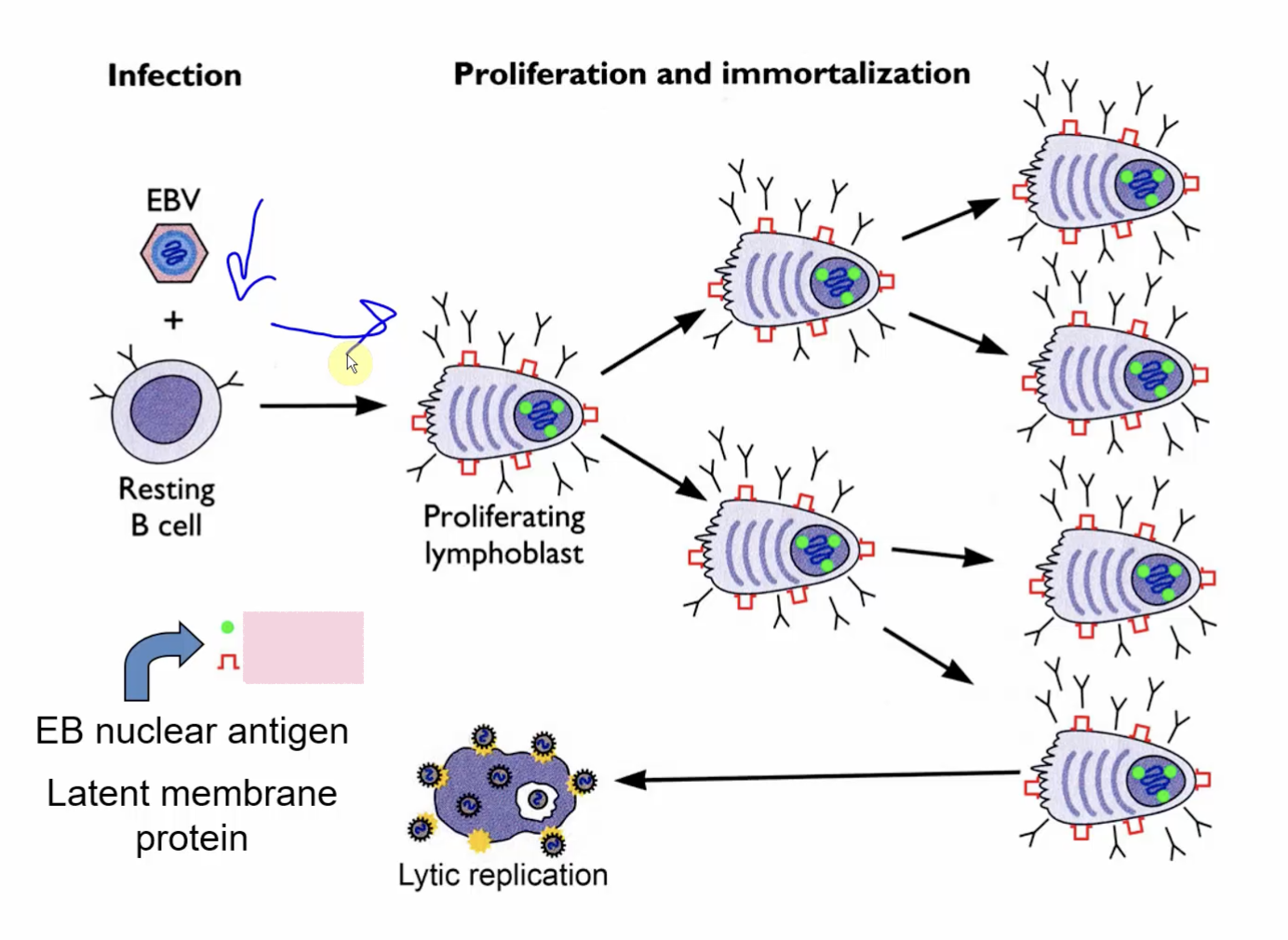
What are the 2 EB nuclear antigens involved?
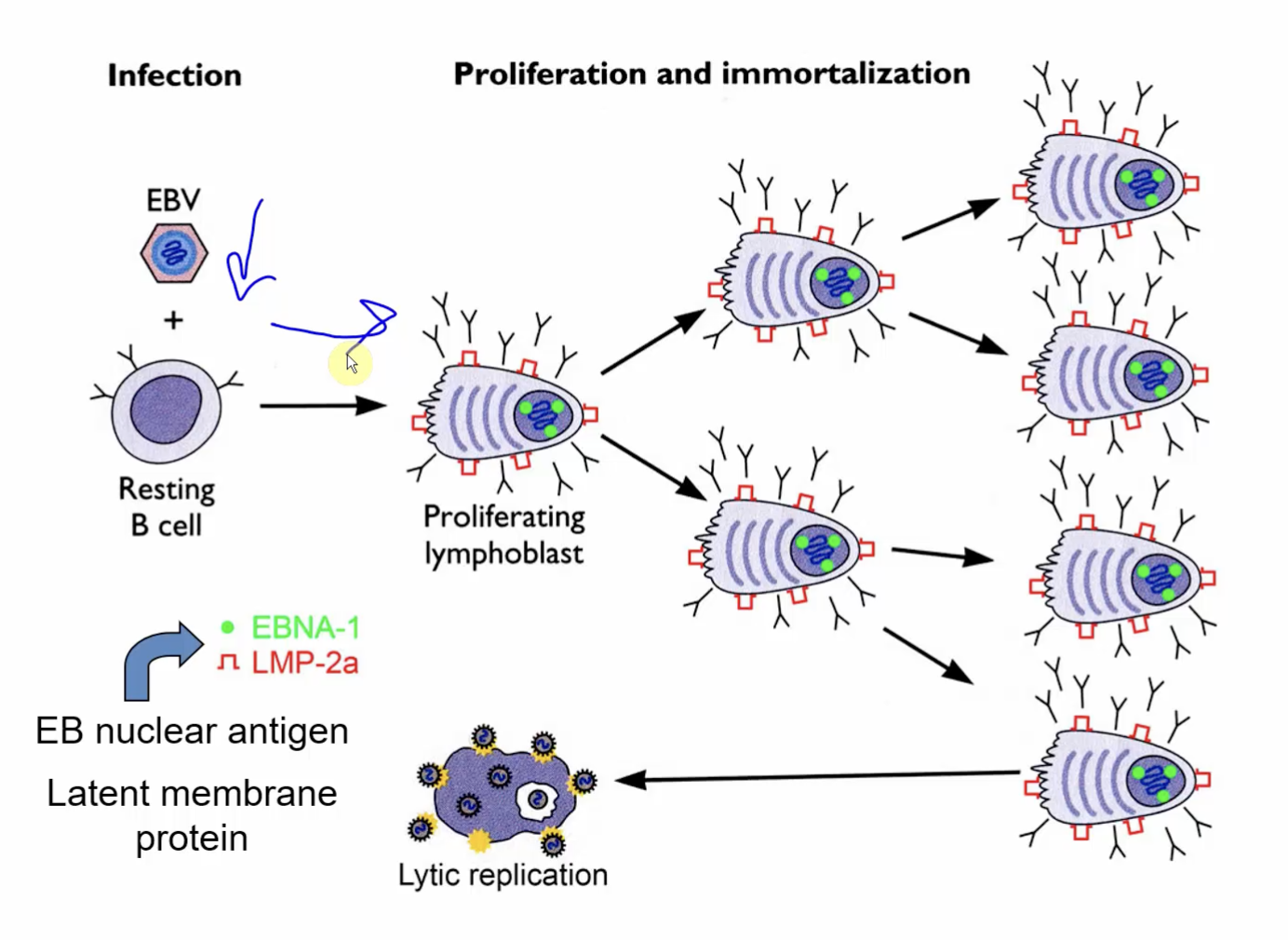
When does EBV become activated?
When infected B-cells undergo Lytic Replication
What allows EBV to enter Latency and evade host immune system?
Establishes Latency in what types of cells?
EB nuclear antigens:
EBNA-1
LMP-2a
Establishes in Memory B-cells
Overview of Epstein-Barr Virus (6)
Virus in saliva infects oral epithelial and B cells in lymphatic tissue where it initiates productive infection
Virus immortalizes B cells (proliferation)
T-cells kill and limit B cell outgrowth
Virus establishes Latency in memory B cells
T-cell response (lymphocytosis) contributes to symptoms of mononucleosis
Can be responsible for lymphoma in immunosuppressed persons and African children in malarial regions (African Burkitt’s lymphoma) and with nasopharyngeal carcinoma in China
EBV Antigens on the following:
Burkitt’s Lymphoma (1)
Hodgkin Lymphomas (2)
Nasopharyngeal Cancer (2)
Burkitt’s Lymphoma:
a B-cell tumor of face and jaw expressing EBNA-1
Hodgkin Lymphomas:
many of these tumors express EBNA-1 and LMP-1
Nasopharyngeal Cancer:
a tumor of epithelial cell origin expressing EBNA-1 and LMP-1
Epstein-Barr Virus
Pathogenesis (Picture)
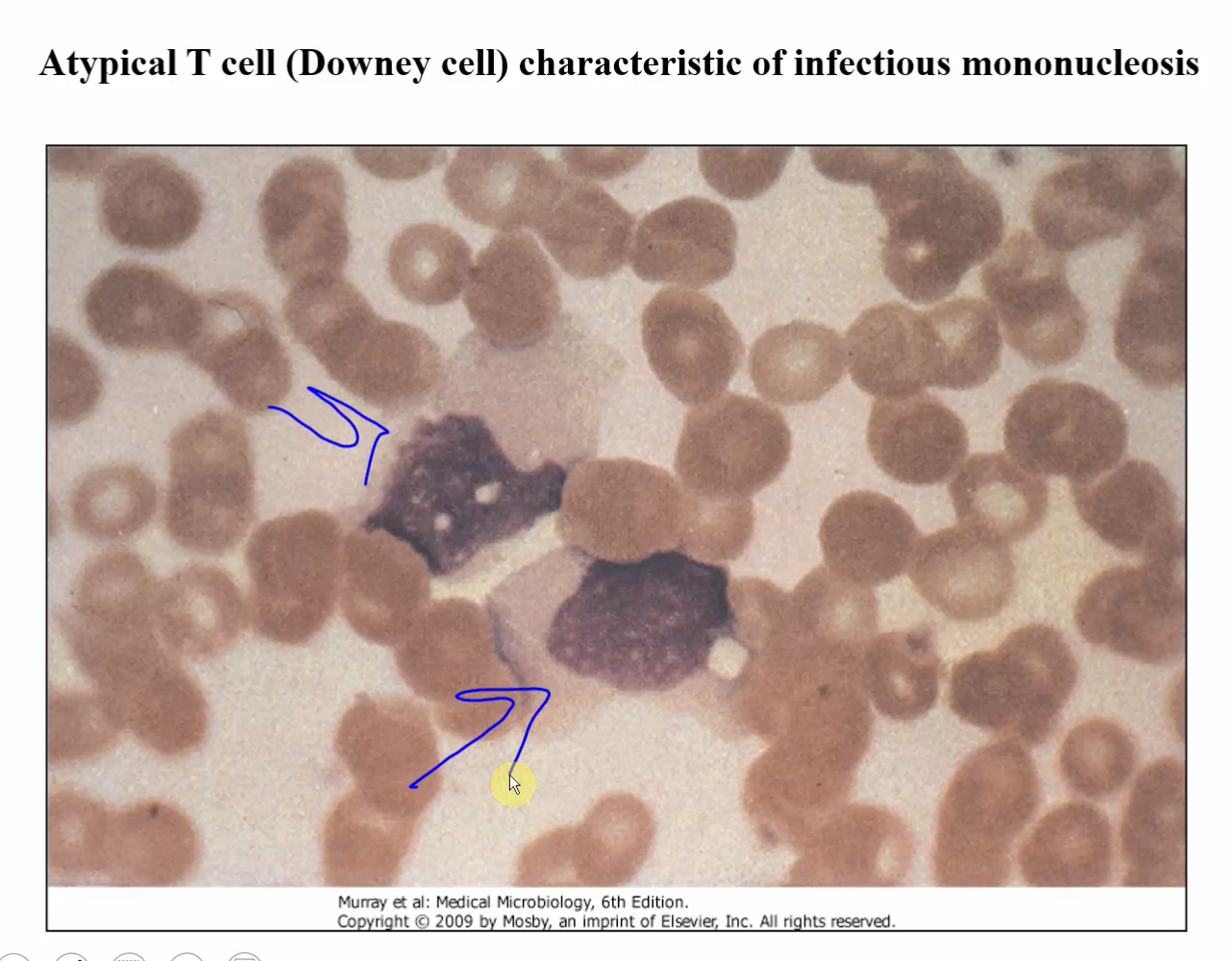
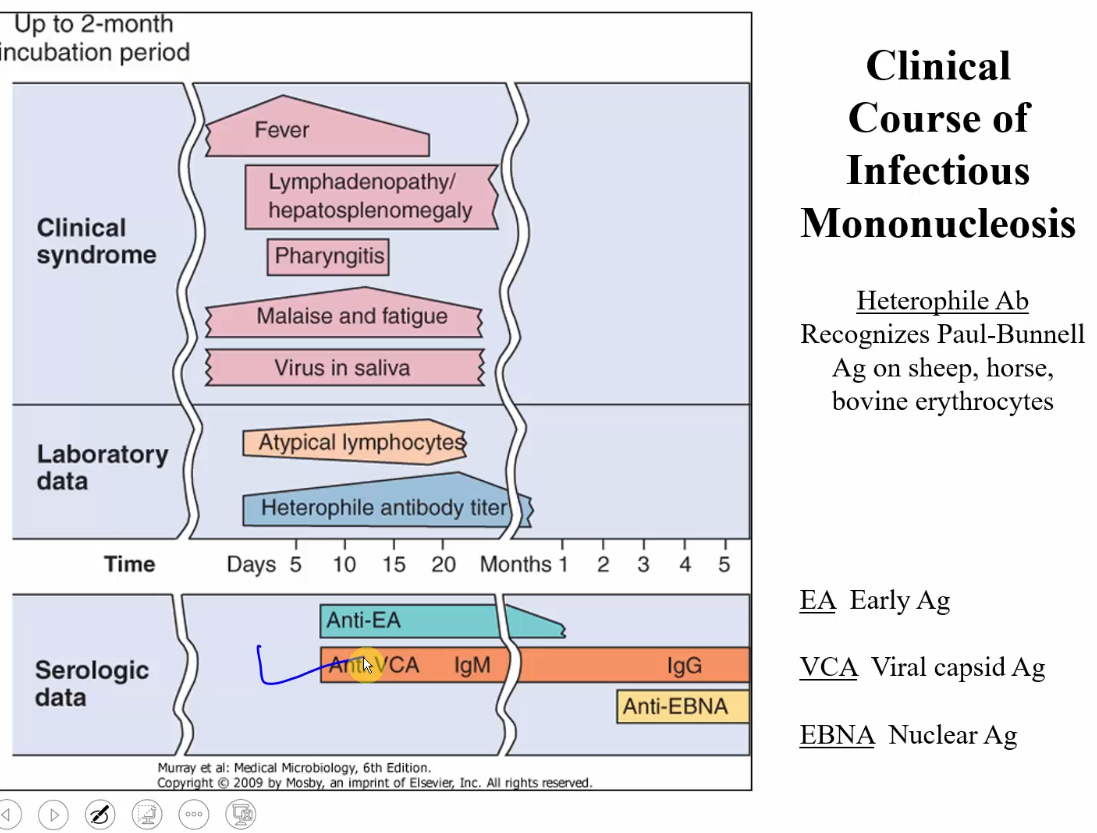
⭐What should point you to EPV or Cytomegalovirus? (4)
Pharyngitis
Swelling of lymph nodes
Atypical lymphocytes (downey cells)
Heterophile antibody (+ in EBV, - in CMV)
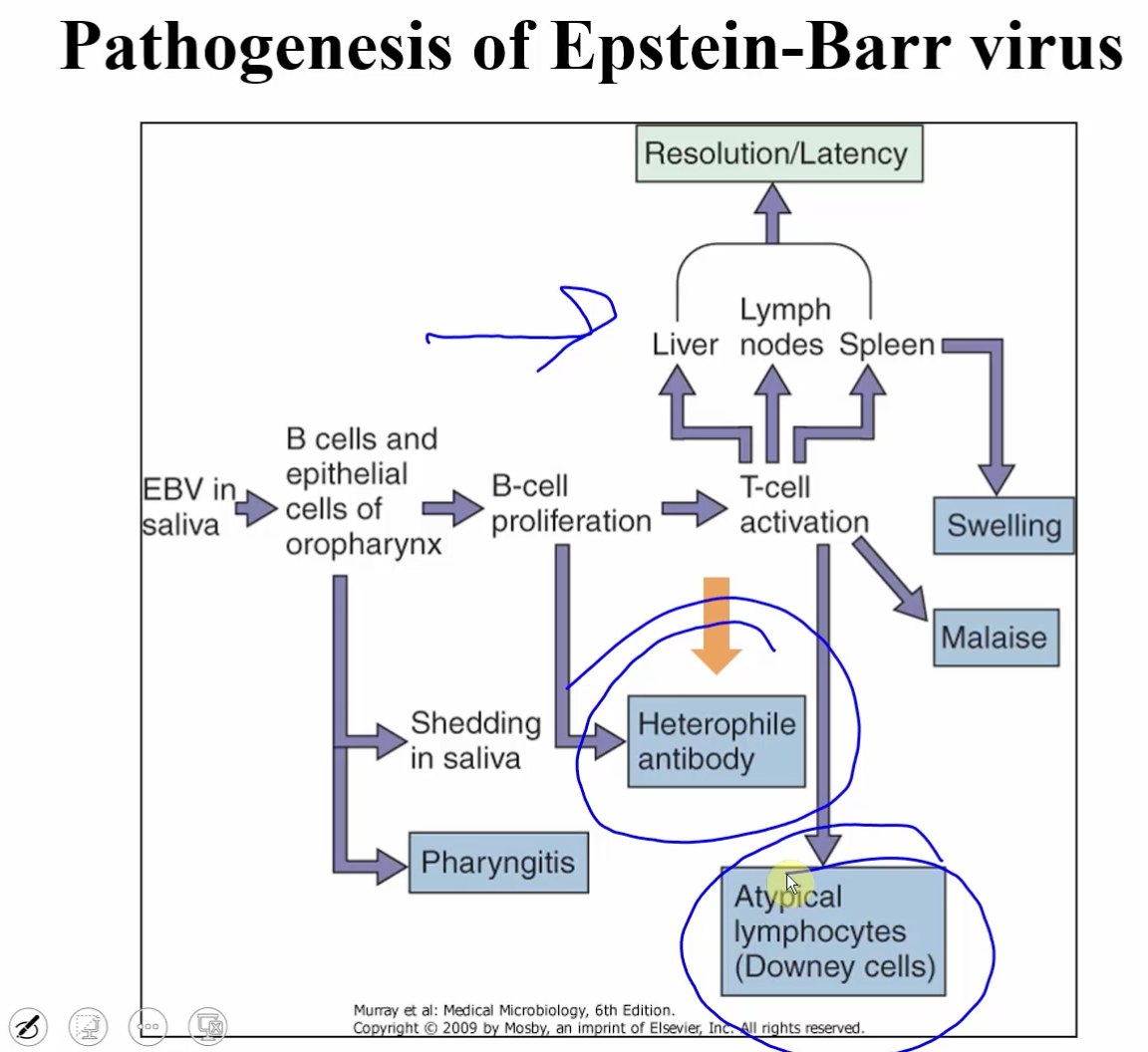
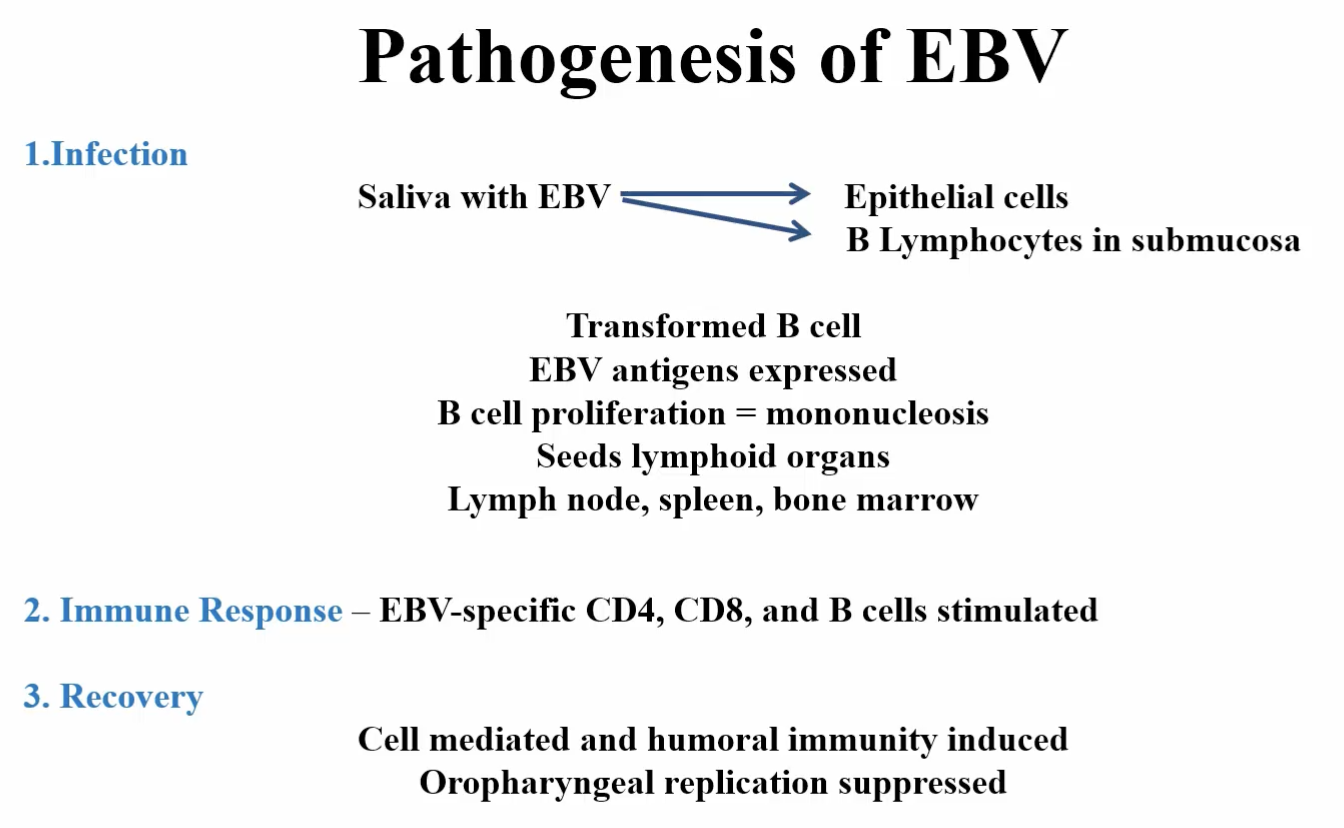
Pathogenesis of EBV
Steps (3)
6, 1, 2
Infection:
Saliva with EBV → Epithelial cells or B Lymphocytes in submucosa
Transformed B cell
EBV antigens expressed
B-cell proliferation = mononucleosis
Seeds lymphoid organs
Lymph node, spleen, bone marrow
Immune Response:
EBV-specific CD4, CD8, and B cells stimulated
Recovery:
Cell-mediated and humoral immunity induced
Oropharyngeal and replication suppressed
Epstein Barr Diagnosis (4)
Symptoms (6)
Complete Blood Cell Count (2)
Symptoms:
mild headache, fatigue, fever
Triad:
Lymphodenopathy
Splenomegaly
Exudative Pharyngitis
Other:
hepatitis
ampicillin-induced rash
Complete Blood Cell Count:
hyperplasia
atypical lympocytes (downey cells)
Heterophile Antibody (transient)
EBV-antigen specific antibody
Epstein-Barr Virus
Effective Treatment/Vaccine
NO effective treatment or vaccine!
best to be infected early in life — more benign
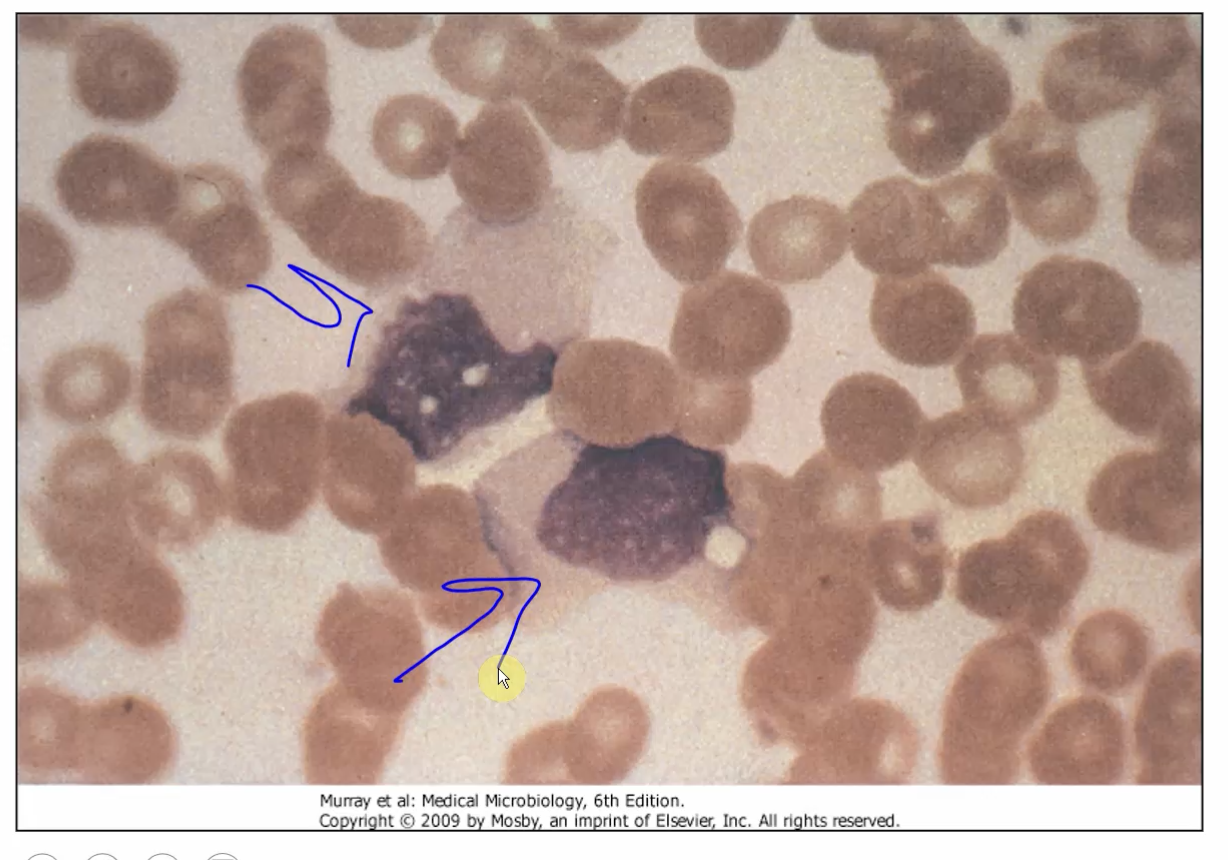
What are these? What virus?
Atypical T-cells (Downey Cells)
Epstein Barr Virus
Epstein-Barr Virus
When do antibodies (IgG) begin to appear?
months after clinical syndromes
IgM antibodies appear 10 days after clinical syndromes
Cytomegalovirus (CMV)
The most common viral cause of what?
Important as a ____ pathogen in immunocompromised patients
Many cell types are ____
examples (3)
Virus can establish latency in what? (2)
Most common viral cause of congenital defects
Important as a opportunistic pathogen in immunocompromised patients
Many cell types are permissive
fibroblasts
epithelial cells
macrophages and others cells
The virus can establish latency in:
mononuclear lymphocytes
stromal cells of the bone marrow and others cells
Cytomegalovirus (CMV)
What class of Herpesvirus?
Beta class
Epstein-Barr Virus (EBV)
What class of Herpesvirus?
Gamma class
Cytomegalovirus (CMV)
Transmission through what? (8)
Significant fact about transmission
Oropharyngeal Secretions
Cervical and Vaginal Secretions
Spermatic Fluids
Urine
Breast Milk
Tears
Blood
Feces
Can be transmitted through PLACENTA to baby!
BODILY FLUIDS
Cytomegalovirus (CMV)
Possible Pathways (3)
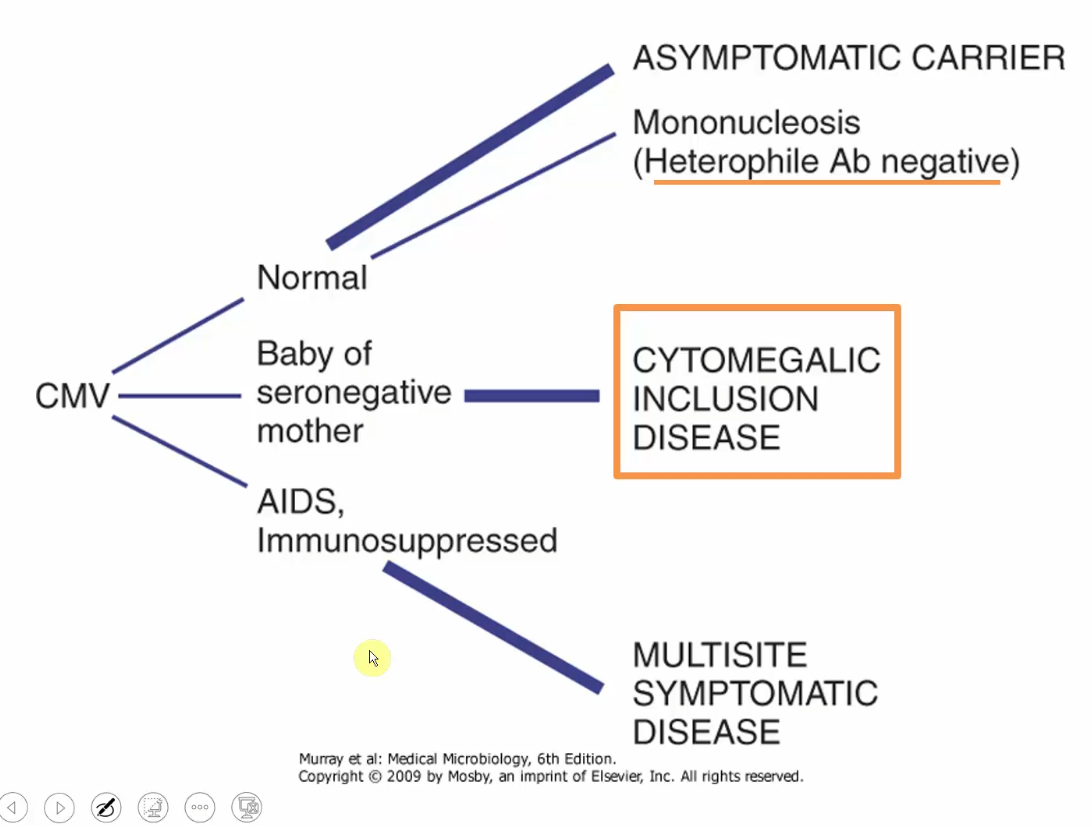
⭐Which Herpesvirus is Heterophile Ab negative? Which is not?
Heterophile Ab (+) → Epstein-Barr Virus
Heterophile Ab (-) → Cytomegalovirus
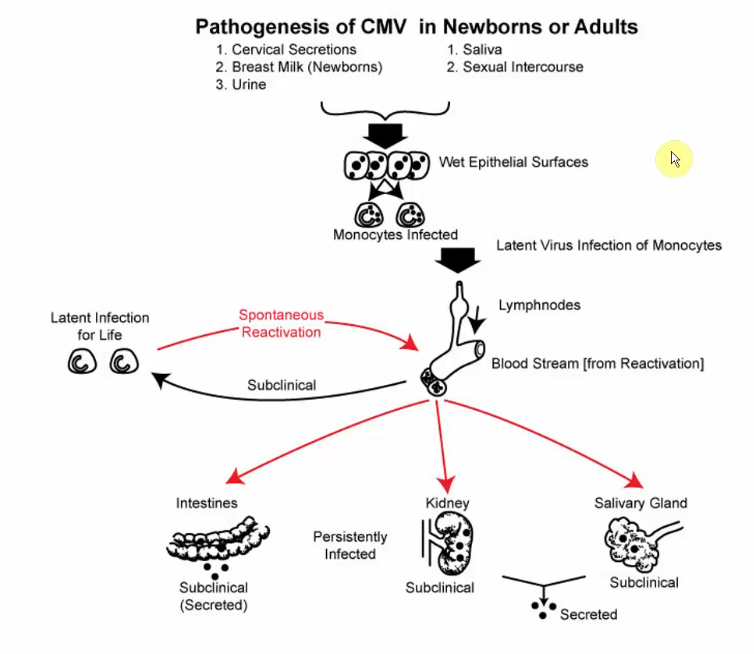
Cytomegalovirus (CMV)
Pathogenesis (draw out)
Cytomegalovirus (CMV)
Immunity is mediated by what cells?
What helps in clearing active infection and maintaining the virus in its latent state? (2)
What can cause reactivation?
Immunity is mediated by T-cells
NK cells and antibody participate in clearing active infection and in maintaining virus in latent state
Impairment of immunity can result in reactivation
Cytomegalovirus (CMV)
Histological hallmark?
Diagnosis how? (3)
Histological Hallmark:
cytomegalic cell - enlarged cell that contains a dense, central “owls eye” intranuclear inclusion body
Diagnostics:
Antigen detection using immunofluorescence
ELISA
PCR
Treatment of Herpes Virus Infections
Treatments (4, 3+2+1+1)
What do they all have in common?
Which drugs are readily absorbed from the gut?
What does this do?
Acyclovir: analog of Guanosine
phosphorylated by viral thymidine kinase, then further by cellular enzymes to be ACTIVATED
activated only in infected cells
Terminates synthesis because Acyclovir lacks 3’—hydroxyl group (Chain terminator)
Penciclovir: analog of Acyclovir
phosphorylated more efficiently
intracellular half-life is 10-fold longer but 100x less potent in its inhibition of viral DNA polymerase
Valaciclovir: Acyclovir analog
Famciclovir: Penciclovir analog
All use NUCLEOSIDE ANALOGS to mess up viral replication
Valaciclovir/Famciclovir are more readily absorbed from the gut → increases plasma levels over the parent compound
Herpes Virus Infections
What can treat latent infections?
Treatments for HSV-1 and HSV-2 (2)
Characteristics of each (4, 1)
NOTHING
Ara-A (Adenine Arabinoside) (Vidarabine):
Analog of Adenosine
Phosphorylated by cellular kinases to triphosphate
Competitive inhibitor of HSV DNA polymerase
Disadvantages:
high toxicity
low solubility
Trifluorothymidine (TFT):
incorporates causing errors
Clinical Uses
Oral Acyclovir, Valacyclovir, and Famciclovir are effective treatments for what? (3)
IV Acyclovir can be used to treat what?
For genital HSV infections, when is treatment beneficial?
Oral Acyclovir, Valacyclovir, and Famciclovir are effective treatments for:
oral mucosal lesions
genital lesions
keratitis
IV Acyclovir can be used to treat HSV-1 encephalitis
For genital HSV infections, treatment is beneficial in first outbreak if given early
treat themselves at first “tingle” of a new outbreak
Clinical Uses
Oral Valacyclovir can be given to people when? Why?
What OTC cream can be used?
What is it?
What does it inhibit?
Oral Valacyclovir can be given to people when they have frequent genetical occurrences for 1 year or longer
Docosanol (Abreva)
OTC cream
active ingredient is a 22 carbon alcohol
inhibits viral attachment
reduces symptoms when applied early (prodrome)
Cyclomegalovirus
Treatment
structure?
lacks what?
characteristics (3)
Significant FACT
Ganciclovir:
chemically slightly different from Acyclovir (additional hydroxymethyl group)
lacks the thymidine kinase of other herpes viruses
Characteristics:
CMV encodes a different kinase to phosphorylate Ganciclovir
Cellular enzymes convert Ganciclovir monophosphate to triphosphate
Triphosphate form of Ganciclovir inhibits CMV DNA polymerase more efficiently than it inhibits host cell DNA polymerase
ACYCLOVIR and analogues are NOT effective b/c CMV lacks TK gene!
Resistance to 2nd generation antivirals can occur by what 2 mechanisms?
Which is the most common resistance mechanism?
Thymidine kinase (or CMV viral kinase) undergoes mutation so that it no longer phosphorylates the drug
this is the most common resistance mechanism
DNA polymerase gene undergoes mutation so that they polymerase no longer recognizes the phosphorylated analogs
What drugs are useful in treating:
Acyclovir-resistant HSV (2)
Ganciclovir-resistant CMV (1 + 3)
Acyclovir-resistant HSV:
Adenine arabinoside (Ara-A)
Foscarnet
binds directly to HSV DNA polymerase and inhibits its action
Ganciclovir-resistant CMV: Cidoforver
drug not dependent on CMV kinase for its activity
posses initial phosphate: cytidine analog
inhibits CMV DNA polymerase directly
What can be taken when patient experiences tingling sensation?
What does this sensation indicate?
Acyclovir
tingling sensation is a prodromal symptom that indicates the onset of a herpes virus outbreak
Taking Acyclovir at this stage can help reduce the severity and duration of the outbreak