Balance and Postural Control
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
Postural balance
the ability to control the body’s position in space with respect to gravity, support surfaces, visual surround, and internal references for the dual purposes of stability and orientation
Stability
the ability to control the body’s center of mass (COM) in relation to the base of support (BOS) under quasi-static (minimal accelerations are occurring) and dynamic conditions
Orientation
relationship between the body’s segments, and between the body and the environment
Center of gravity
imaginary point in space, calculated biomechanically from measured forces and moments, where the sum total of all forces = zero; COM via force plate calculation
Base of support (BOS)
the body surface that receives pressure as the result of body weight and gravity
Limits of stability (LOS)
farthest distance a body can lean in any direction without (falling) altering the original BOS (perceived vs actual)
What sensory information is important for balance/postural control?
Somatosensory, visual system, vestibular system
Somatosensory system
Provides CNS with position and motion info about the body’s position in space in reference to the support surface
Visual systen
provides info regarding the position & motion of the head with respect to surrounding objects in the environment
Vestibular system
-provides info regarding position and movement of the head with respect to gravity & inertial forces
-contributes to control of CoM (VSR) and gaze stability (VOR)
What types of motor control are required for balance
steady state postural control, anticipatory posture control, reactive postural control
Steady state postural control (SSPC)
-ability to control the location of the body’s COM within the area defined by the BOS under predictable, quasi-static conditions
-This includes the ability to adapt motor behavior to meet the demands of different tasks and environmental conditions
Anticipatory postural control
-ability to generate postural adjustments prior to the onset of and during voluntary movement for the purpose of either countering an upcoming postural disturbance due to voluntary movement or realigning the body’s center of mass to change the base of support
-This includes the ability to adapt motor behavior to meet the demands of different tasks and environmental conditions
Reactive postural control
-Ability to respond to sensory input that signals a need for a response to ensure successful maintenance of postural control. The need for a response in unanticipated but may be generated externally (perturbation originating external to the body) or secondary to an internally generated movement
-This includes the ability to adopt motor behavior to meet the demands of different tasks and environmental conditions
Reactive movement strategies
-predictable, automatic responses following external surface perturbation in AP directions (ankle, hip, stepping)
Ankle strategy
-Controls COG by rotating the body primarily about the ankle joints with in-phase movement of the hips and head
-Muscle activation begins distally → proximally
-Utilized in response to small perturbations on firm surfaces (
Forward sway ankle strategy muscle activation
gastroc→hamstring→paraspinals
Backward sway ankle strategy muscle activation
tib anterior→ quad→ abdominals
Hip strategy
-controls COG with large & rapid motion at the hip and antiphase movement of the head
-muscle activation begins proximally
-utilized in response to larger, faster pertubations or when the support surface is compliant/unstable or narrow
Forward sway hip strategy muscle activation
abdominals→ quad
Backward sway hip strategy muscle activation
paraspinals→ hamstrings
Stepping strategy
-changes the BOS
-utilized when the perturbation is strong enough to displace the COG outside the BOS
-BOS moves to “catch up” with the displaced COG
What underlying systems are important determinants of balance
-MSK
-Neuromuscular
-Cognitive/mental function
-Behavioral factors
MSK system
-ROM
-Flexibility (muscle length, joint mobility)
-Muscle performance (strength, power, endurance)
-Alignment (posture)
Neuromuscular system
-postural movement strategies
-coordination
-sensory integrity
-sensory processing (integration)
-perceptual function (verticality)
Cognitive/mental function
-executive function
-multi-tasking capacity
-arousal and alertness
behavioral factors
-balance confidence (Degree of certainty that an individual has in their ability to maintain balance and remain stable while performing tasks)
-falls self-efficacy (Degree of certainty that an individual has in their ability to maintain balance and remain stable while performing tasks)
-fear of falling (A lasting concern or worry about falling regardless of history of fall)
-activity avoidance (The limiting of an activity that an individual is capable of performing that can result in an increased risk of falling and deterioration in physical and mental health and quality of life)
What functional tasks (activity level) are important to examine in the context of balance
-sitting
-sit to stand
-standing
-walk and turn
-step up/down
-reach, grasp, and manipulate
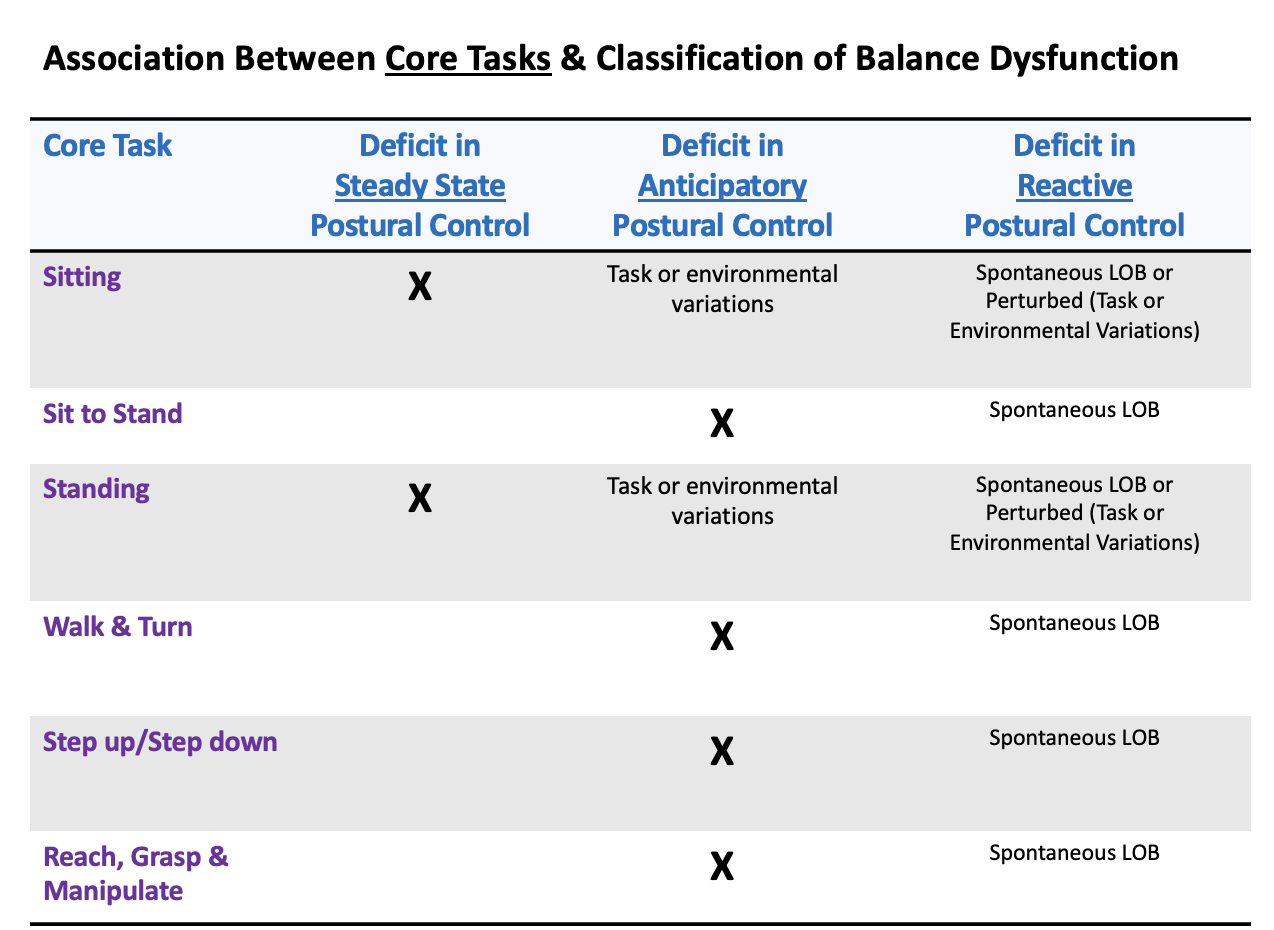
Association between core tasks and classification of balance dysfunction
Summary of normal postural control
1) Postural control depends on the integration of information from 3 senses and the application of appropriate motor strategies
2) Stability, orientation, and adaptation to changing demands on flexibility in the selection of the appropriate control strategy
3) Balance performance depends on multiple underlying systems, as well as the goal of the task and other aspects of the environment in which it is performed (task specificity)
During exam of balance what should you avoid doing
-”poor, fair, good” as descriptors for balance, which are subjective, vague, and meaningless
-Instead, strive for objective measures that encompass a battery of tests to address the complex nature of balance
Types of balance tests
-Quiet standing
-Active standing
-Task performance
-Self-report
-Specialized vestibular testing
Quiet standing
-Steady state (Rhomberg, sharpened/tandem rhomberg, SLS/one leg stance time (OLST), postural sway)
-Perturbed (nudge/push or environmental variations (foam), motor control test (MCT)- computerized))
-Sensory integration (sensory organization test (SOT)-computerized, clinical test of sensory interaction on balance (CTSIB) - (“foam and dome”)
Active standing OMs
-functional reach (FR)
-multidirection reach test (MDRT)
-Limits of stability (LOS)
Task performance
-Observation (ANPT 6 core tasks)
-BBS*
-TUG
-Tinetti performance oriented mobility assessment (POMA)
-Community balance and mobility scale (SB&M)
-Short physical performance battery (SPPB)
-Fullerton advanced balance scale (FAB)
-Postural assesment scale (PASS)
-Trunk impairment scale (TIS)- sitting
-Gait tasks (complex gait: DGI, FGA*; for environmental variations, use Emory Functional Amulation Profile E-FAP)
-Dual Tasks (stop walking when talking (SWWT), multiple tasks test (MTT), TUGman or TUGcog)
Self-report
-Falls efficacy scale (FES)
-Activities-specific balance confidence scale (ABC)*
-Dizziness handicap inventory DHI
-Fall logs/diaries
Specialized vestibular testing
-Dix hallpike maneuver (r/o BPPV)
-Vertiginois positions
-Occulomotor tests
-VOR Tests (visual-vestibular interaction)
-Dynamic visual acuity
-Fukuda stepping test
-Complex gait tasks (DGI, FGA)
Other examination issues
-testing with or without the use of devices or equipment
-technology-assisted assessments vs clinical assessments
-environmental issues (distractions affordances, constraints)
-safety & guarding
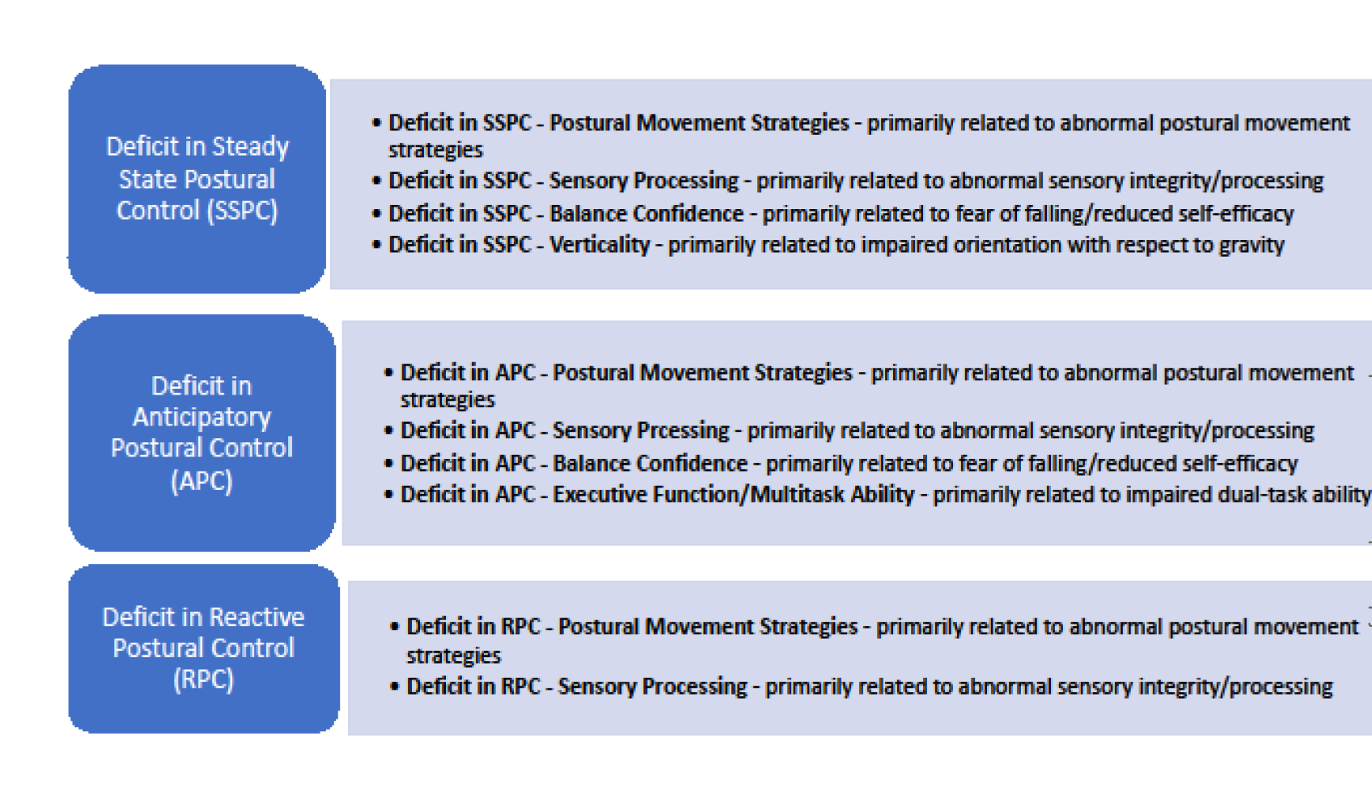
Movement system duagnoses for balance dysfunction
-There is no single existing framework that includes all relevant and current conceptual elements related to balance
-none of the frameworks sufficiently covered perceptually-based problems, nor were behaviorally based factors adequately represented in the framework
-ANPT arrived at a consensus to use a combination of frameworks and behavioral models
Conceptual elements
-Control strategies for balance (SSPC, APC, RPC)
-Underlying determinants of balance (MSK, neuromuscular, cognitive/mental function, behavioral factors)
Classification of balance dysfunction
-” key movement observation” is defined as deviations from typical movement performance that guide the detection of deficits in balance dysfunction
-Observation of 6 core tasks (maintenance of positions (sitting, standing), movement within positions (reach, grasp, and manipulate), movement between positions (sit-to-stand), and movement through the environment (step up/down, walk, and turn)
Observable movement constructs include
-alignment
-verticality
-stability
-symmetry
-speed
-amplitude
-smoothness
-sequencing
-timing
accuracy
-sx provacation
Regression/progression
task changes (BOS, speed, perturbation, cognitive demand)
-Environmental changes (surface type or height, cueing, physical assistance, external support, environmental inputs)
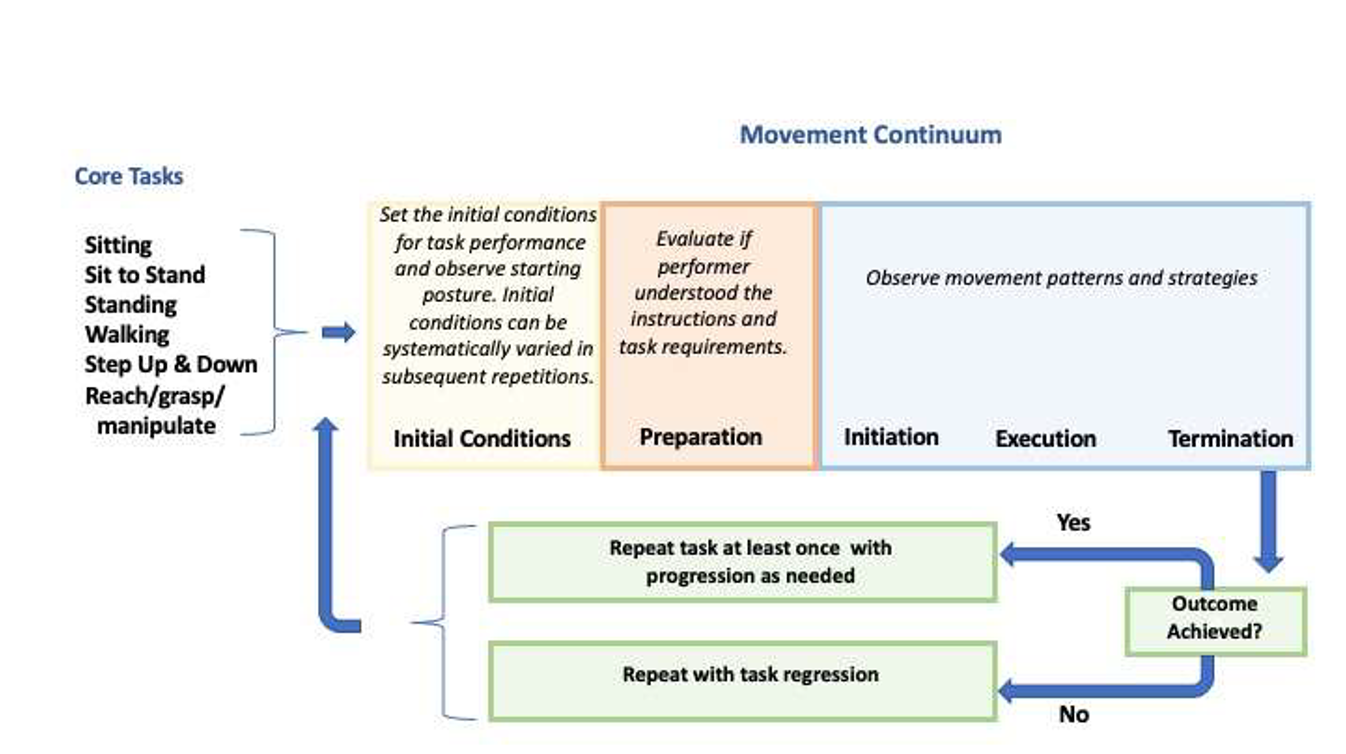
Movement analysis of tasks
Movement system diagnoses for balance (3 diagnostic labels and each has subcategories)
Summary of balance exam
-Begin at the functional/task level (use skillful observations to guide your approach)
-select appropriate tests and measures to refine your differential diagnosis of balance (remember to consider patient-related factors (age, dx, functional level), test-related factors (psychometric/clinimetric properties), and resource-related factors (skill&level of training required, time/space availability, equipment))
-use a systems approach to conduct a comprehensive exam nd determine a PT diagnosis (functional level (activities and participation), impairment level (body structure/function), diagnostic level (movement system dx)