Histology: Salivary gland, Esophagus, and Stomach
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
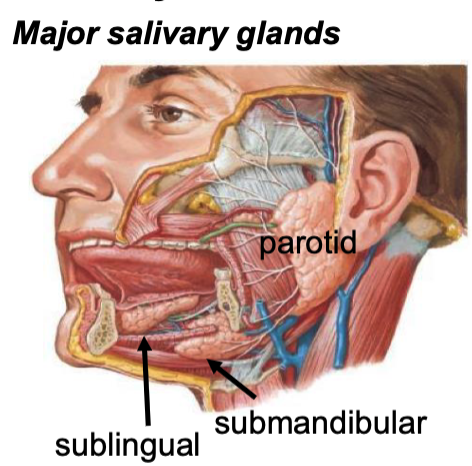
what are the major salivary glands?
parotid
submandibular
sublingual
(these are all duct systems)
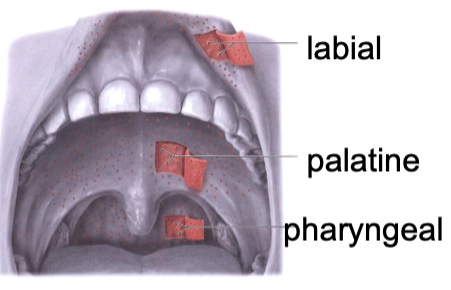
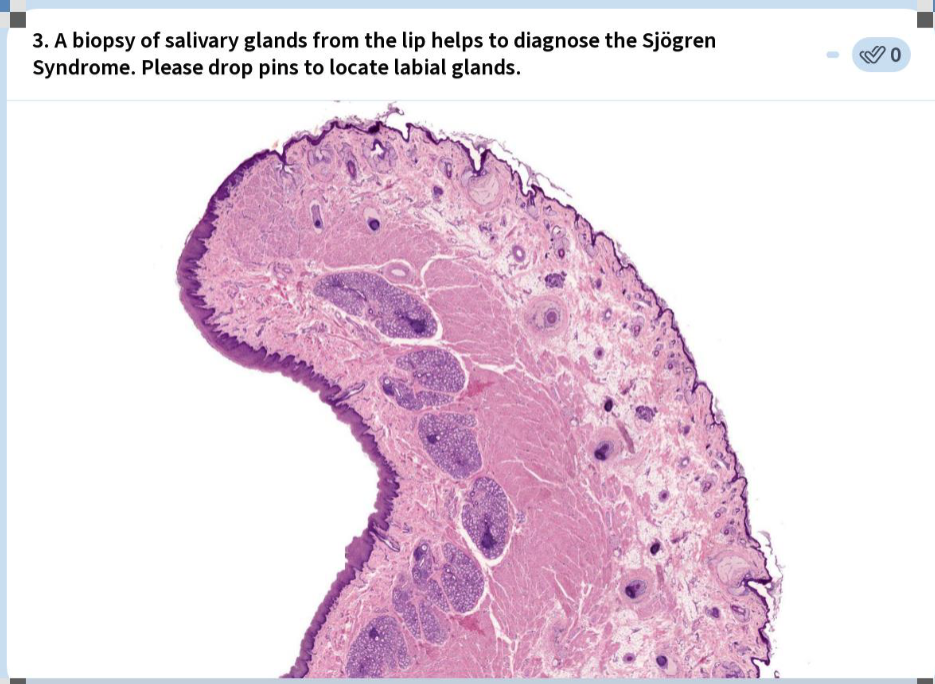
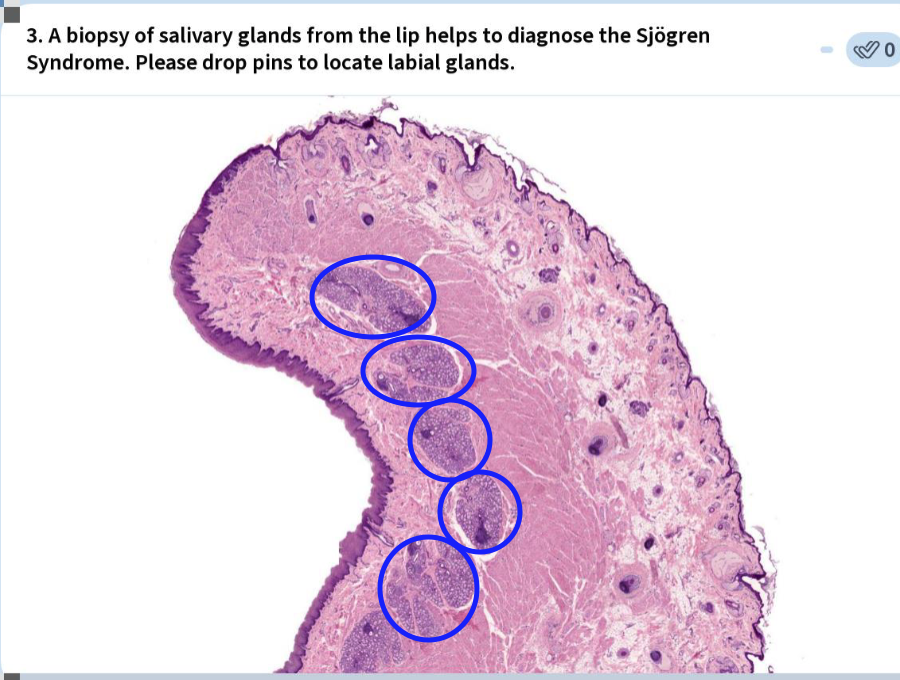
what are the minor salivary glands?
• Labial (lip)
• Buccal (cheek); molar
• Lingual (tongue)
• Palatine (hard and soft)
• Alveolar mucosa
• Floor of mouth
(short ducts or secrete directly into oral cavity)
what are components of saliva?
water (97-99%)
cells (lymphocytes, neutrophils, salivary corpuscles)
proteins/enzymes
mucin glycoproteins
electrolytes (Na+, K+, Ca++, HCO3-, PO43-, Cl-, F-)
% of mucous secretion are from minor glands
70%
% of saliva is from major glands. minor glands?
90+% from major glands; 5-10% from minor gl
we secrete ____ ml of saliva per day
1000
what are the functions of saliva?
protection, buffering
solubilize food molecules
moisten food
initiate digestion
control microbial flora
promote healing
how does saliva protect and buffer?
Moisten/lubricate oral mucosa, prevent drying, flush/cleanse/protect teeth, facilitate speech
Neutralization of acids, maintain pH
HCO3-
how does saliva initiate digestion?
enzymes like alpha-amylase, lipase, RNase, DNase
how does saliva promote healing?
epidermal growth factor (EGF)
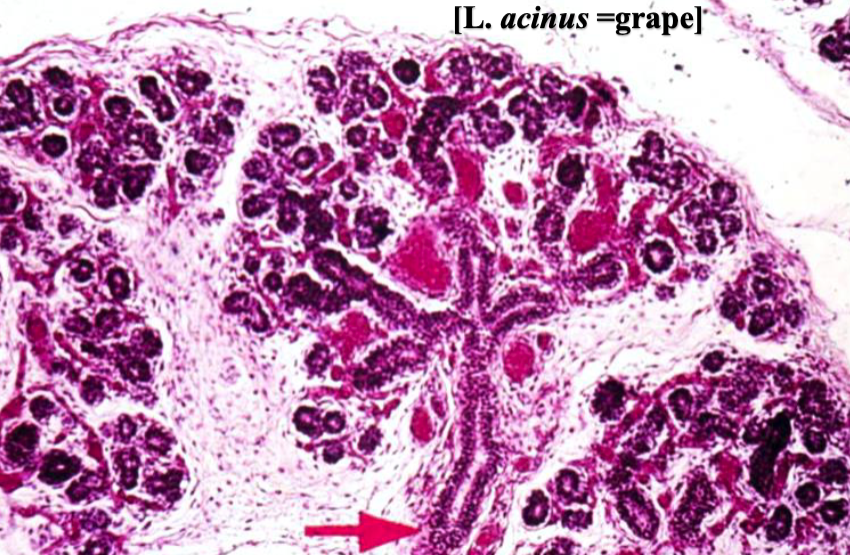
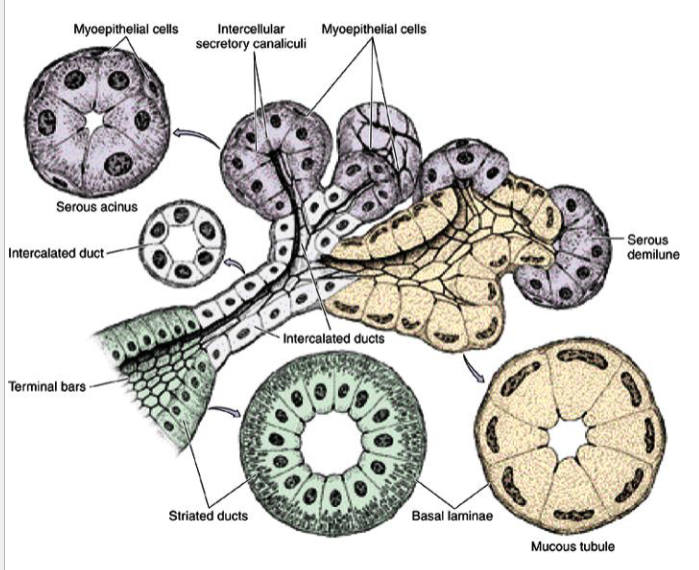
salivary gland
what are the components of salivary glands?
serous units
acinar
round nucleus toward base
mucous units
tubular
flattened nucleus
mixed units/cells
ducts
what do serous units secrete?
Watery fluid containing proteins
what do mucous units secrete?
Viscous fluid containing glycoproteins
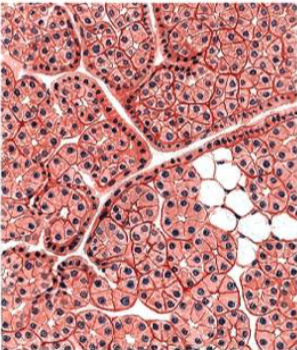
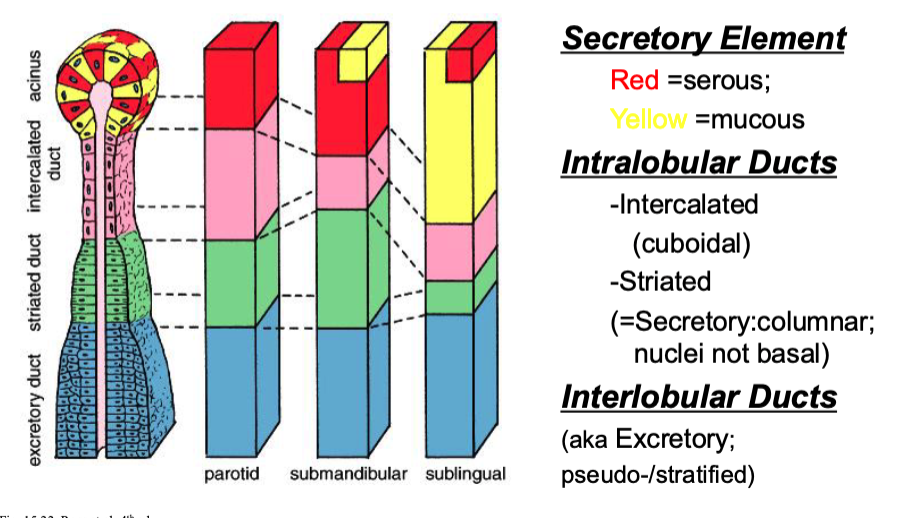
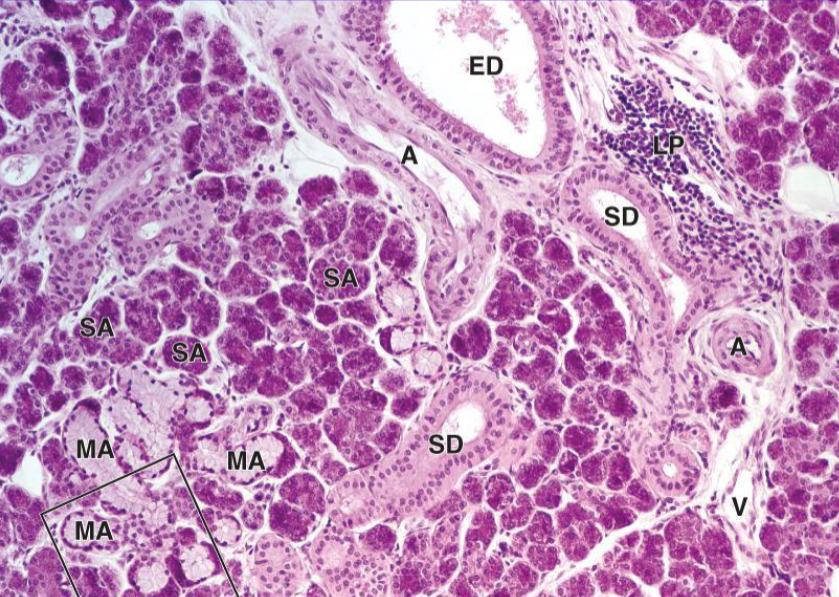
Parotid Gland
(Serous; mucous rare)
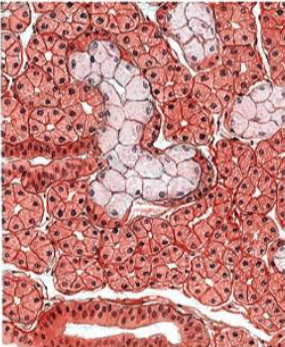
Submandibular Gland
(Serous>Mucous)
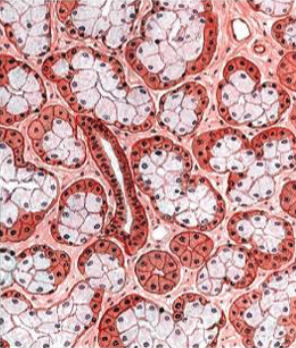
Sublingual Gland
(Mucous>Serous)
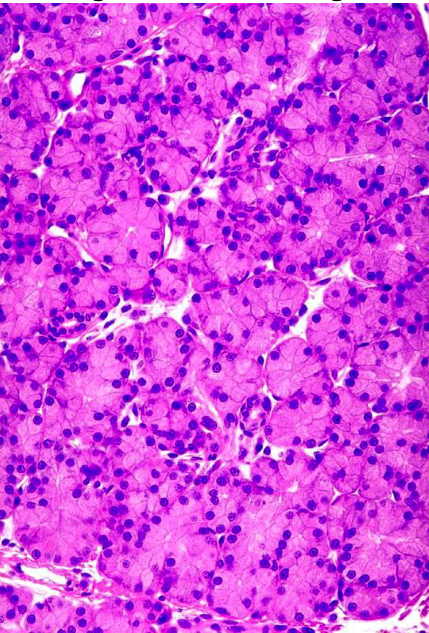
parotid
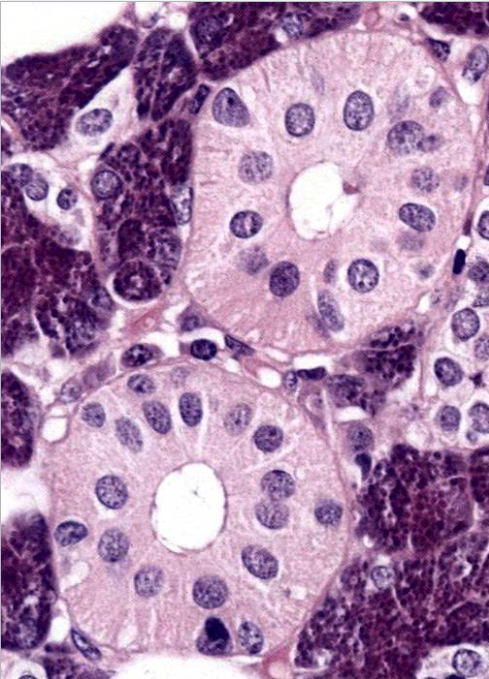
we know these are serous cells (dark staining, perfectly round nuclei)
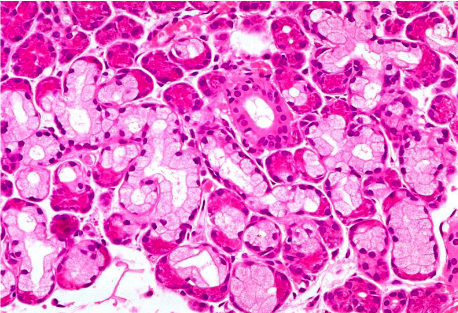
submandibular
darker staining + round nuclei = serous
lighter staining + flattened nuclei = mucous
more serous than mucous = submandibular
sublingual
darker staining + round nuclei = serous
lighter staining + flattened nuclei = mucous
more mucous than serous = sublingual
what are the ductal elements of salivary glands?
intralobular ducts
intercalated
striated
interlobular ducts (excretory)
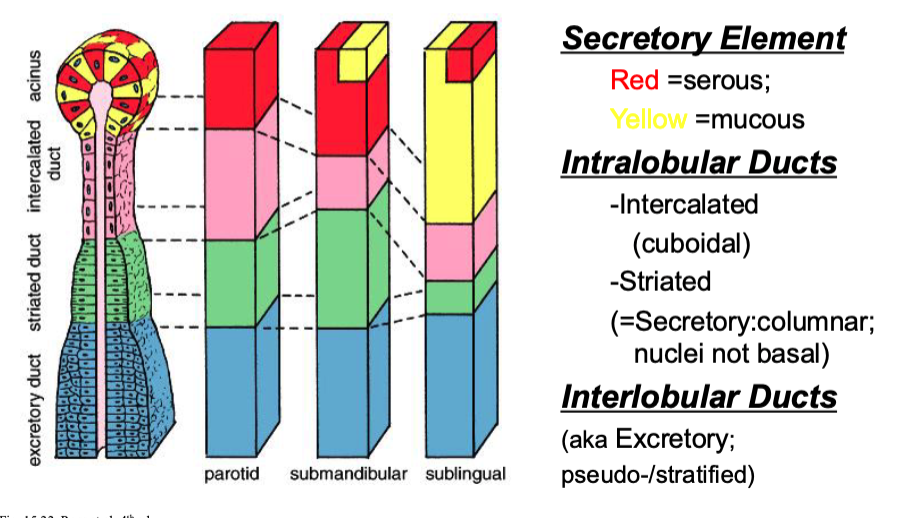
what kind of cells make up intercalated ducts?
cuboidal
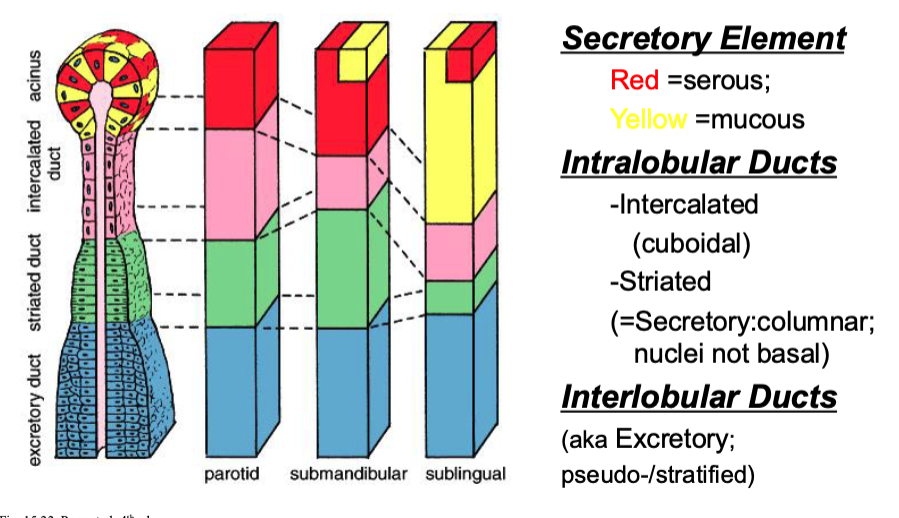
what kind of cells make up striated ducts?
columnar
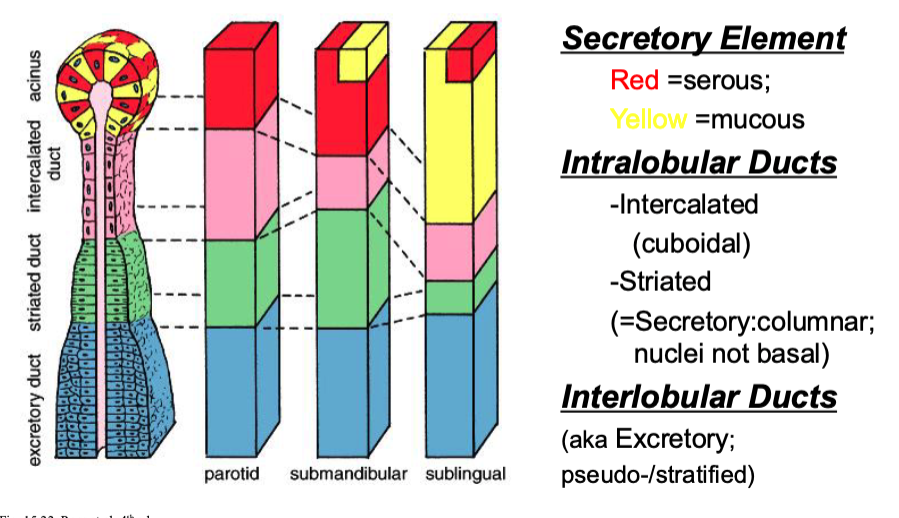
what kind of cells make up interlobular ducts?
pseudo-stratified
Striated ducts have eosinophilic cytoplasm due to large numbers of ______
mitochondria
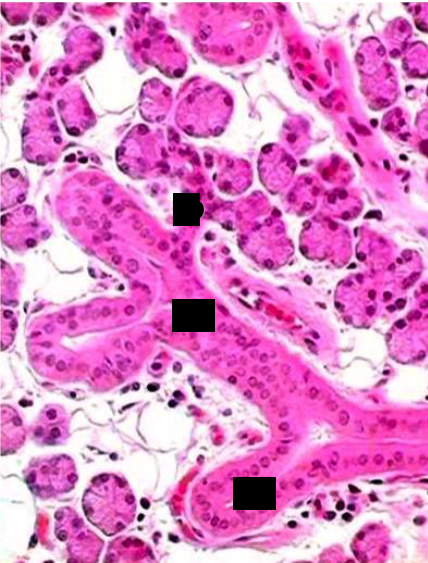
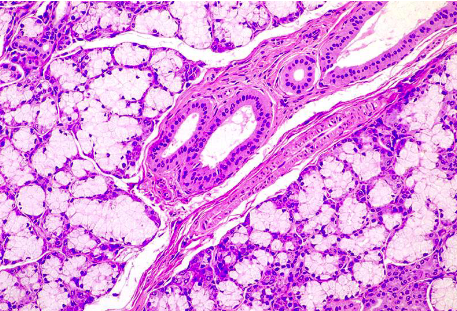
parotid gland (intercalated vs striated ducts)
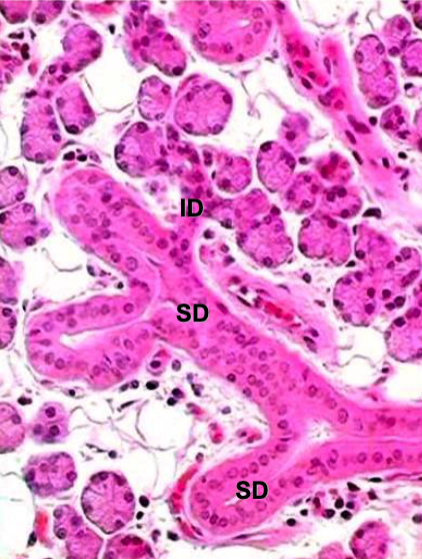
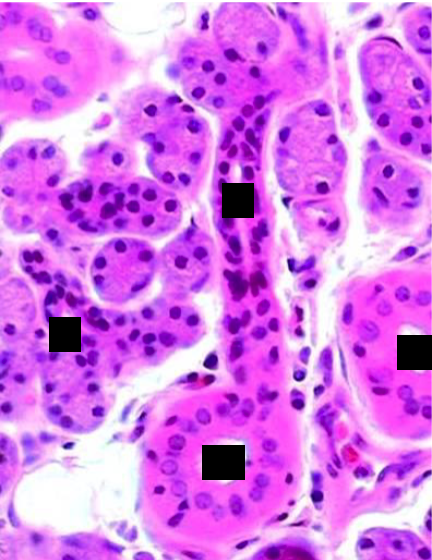
parotid gland (intercalated vs striated ducts)
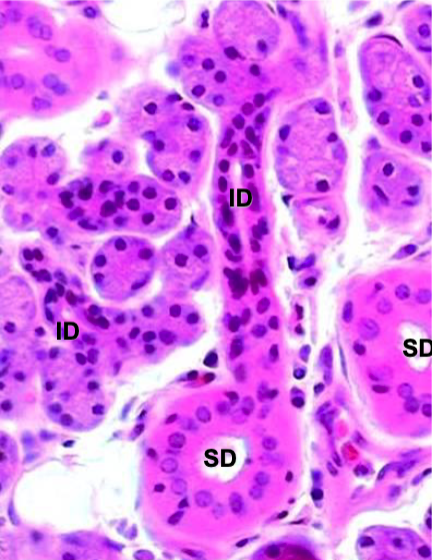
striated ducts (nuclei located closer to apical surface)
what is the funciton of striated ducts?
Na+ reabsorption; K+, HCO3- secretion; influenced by adrenal steroid aldosterone
what is the funciton of excretory ducts?
Transport saliva to the oral cavity, generally do not modify the saliva
what cells are responsible for salivation in response to visual/neurological stimulation (before we even put food in mouth)?
myoepithelial cells (located between secretory cells and basement membrane)
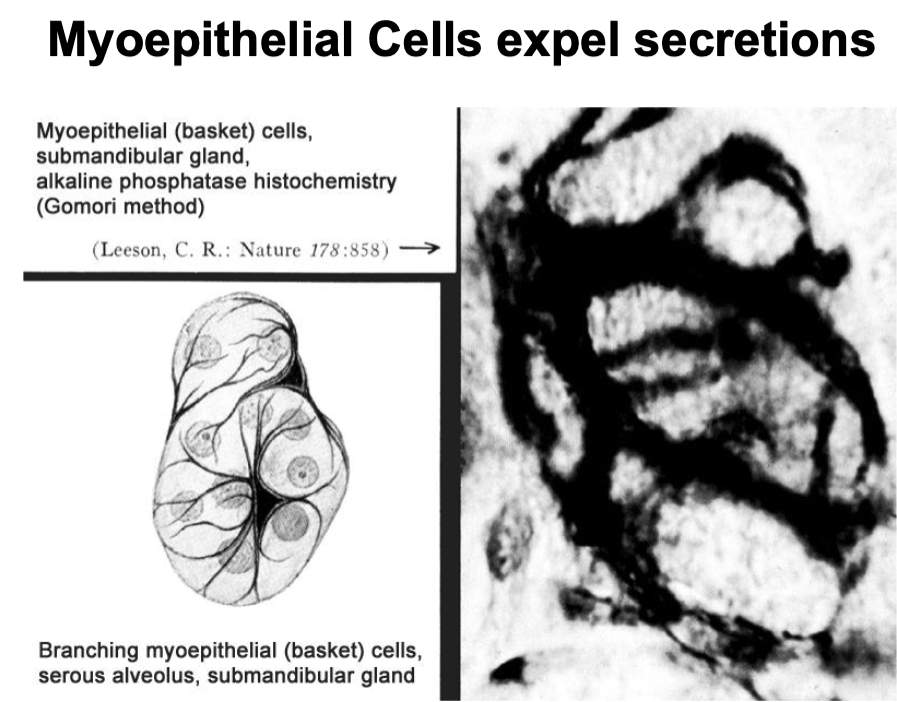
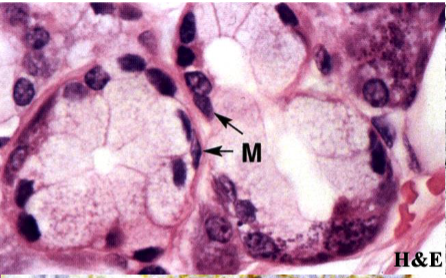
myoepithelial cells
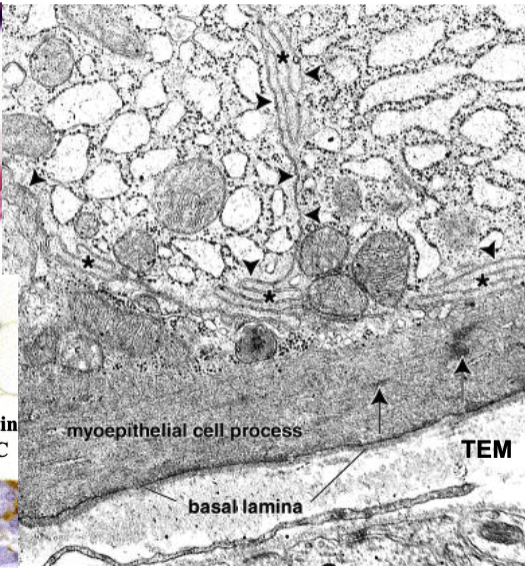
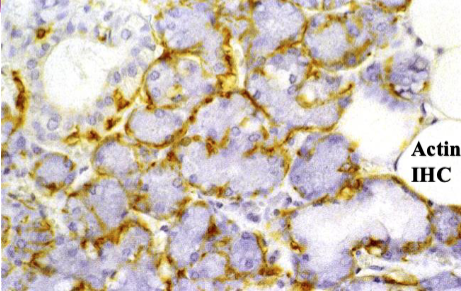
myoepithelial cells
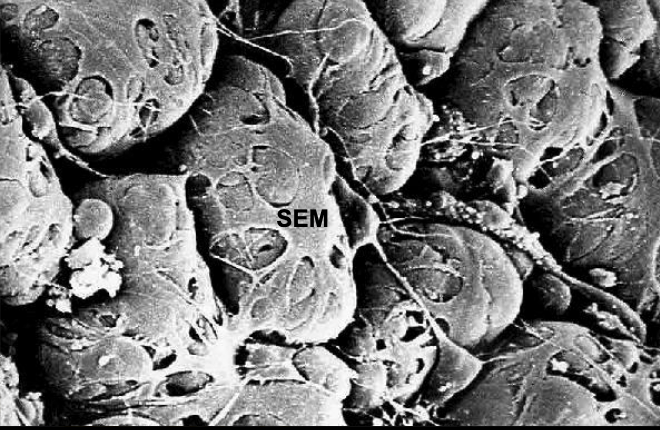
myoepithelial cells
what are the functions of myoepithelial cells
support, contraction, antiangiogenesis, tumor suppressor activity, barrier against invasive epithelial neoplasms
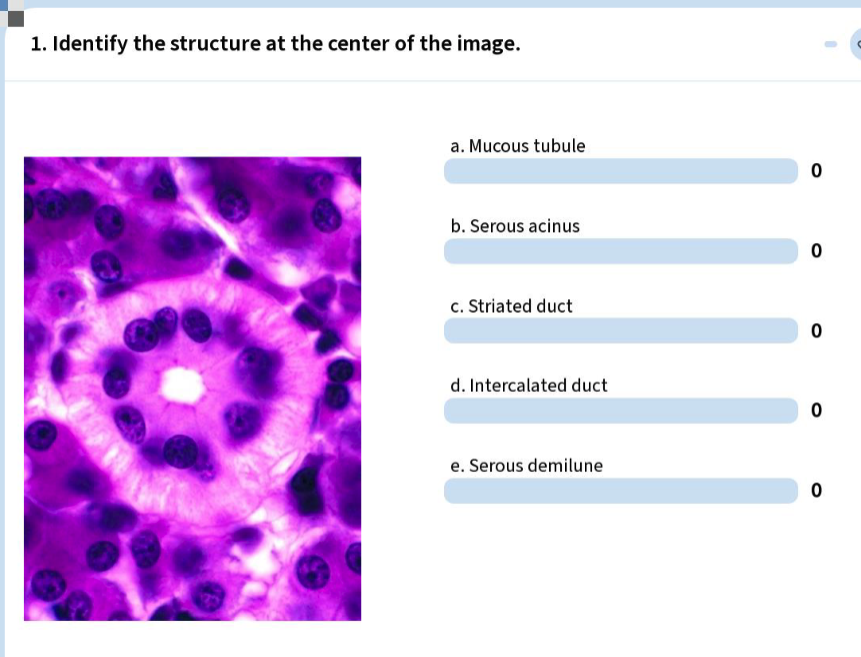
C) striated duct
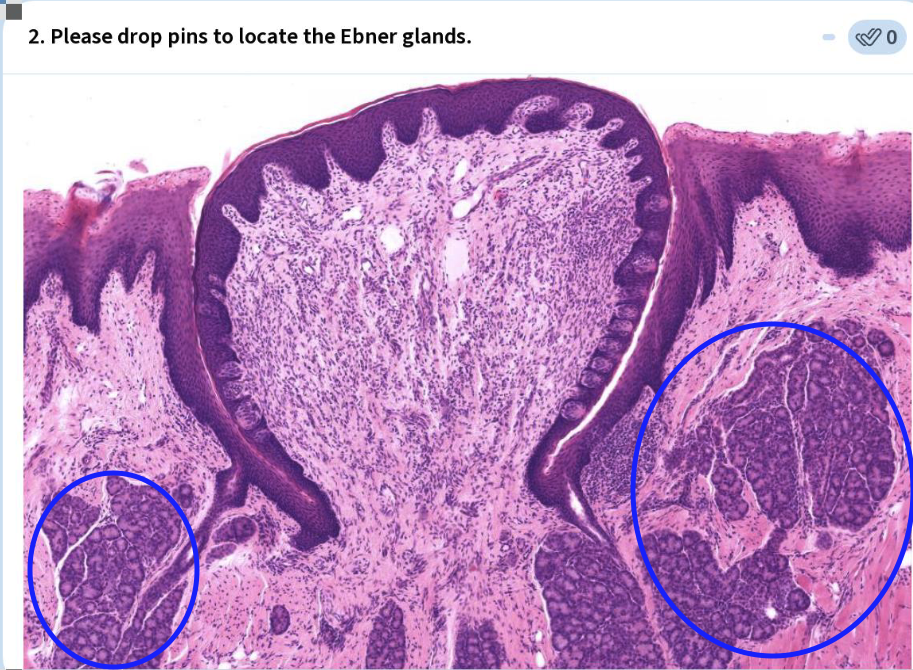
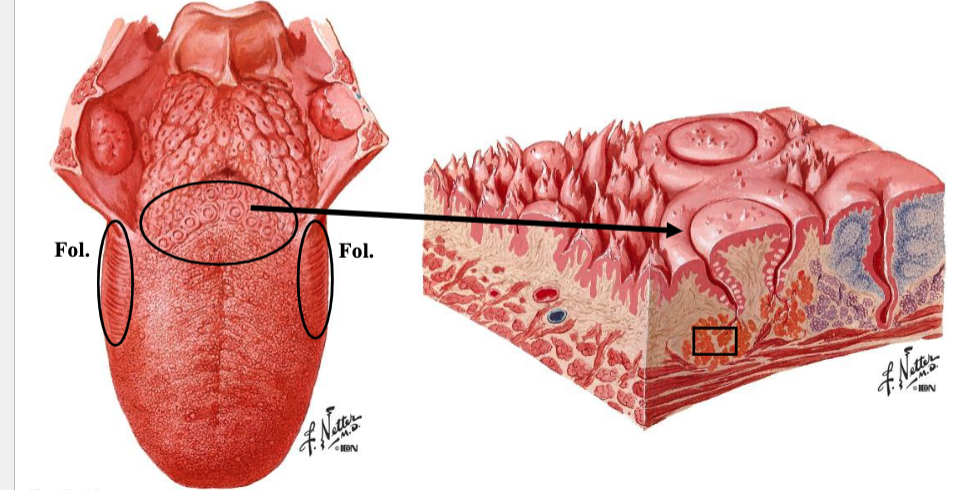
what type of glands are the minor salivary glands?
mixed (mucous > serous) OR mucous
except gustatory/Ebner glands are serous
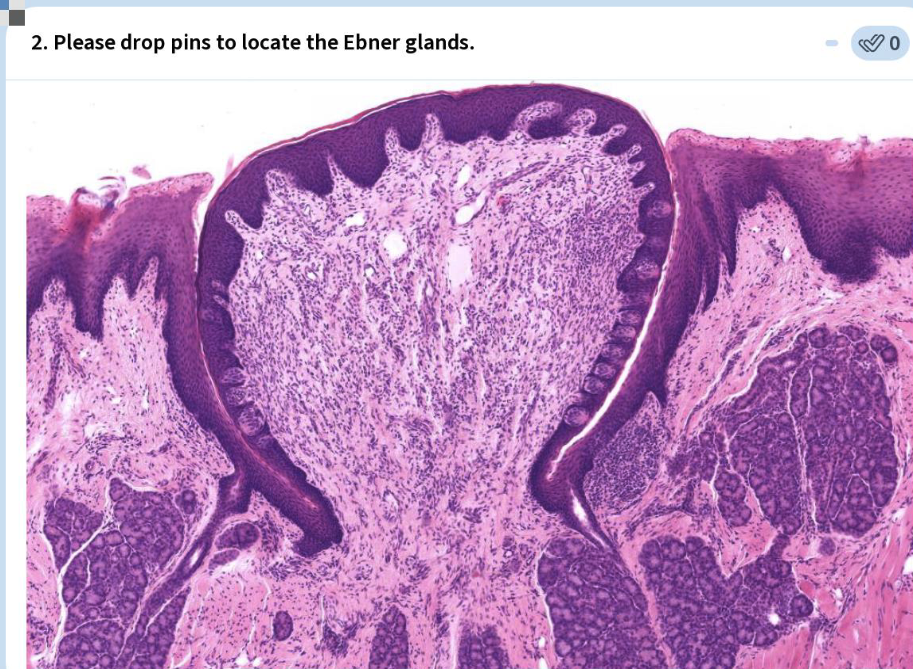
what type of fluid is secreted from Ebner glands?
serous only
where are Ebner glands located?
near vallate and foliate papillae
what Chronic autoimmune disorder affects salivary & lacrimal glands leading to xerostomia & dry eyes, respectively?
Sjögren Syndrome
what is the 3rd most common autoimmune disease next to RA & lupus?
Sjögren Syndrome
t/f: there is a cure for Sjogren’s syndrome
false.
• Mild symptoms to severe disease
• Currently no cure, but treatment may help
what is sialoithiasis?
formation of calculi or mineralized concretions that may block a salivary duct
what condition may lead to periodic pain in ducts or gland as well as swelling of gland due to obstruction of duct by mineralized concretions?
Sialolithiasis
what is the condition characterized by dryness of mucous membrane of mouth resulting from reduction (hyposalivation) or absence (asialism) of saliva?
Xerostomia
what are some causes of Xerostomia?
infections
side effects of medications, chemotherapy & radiotherapy;
autoimmune diseases (e.g., Sjögren syndrome);
endocrine disorders (e.g., diabetes); anxiety
xerostomia places patients at risk for…?
tooth decay, opportunistic oral infections (bacterial, fungal), gum disease
t/f: xerostomia is a relatively common condition that affects more females than males.
true
what is the acute infectious disease that causes inflammation and swelling of the parotid gland [parotitis =inflammation of the parotid gland] with occasional involvement of other salivary glands?
mumps (epidemic parotitis)
what is the cause of mumps?
contagious infection by mumps virus
t/f: mumps is typically a childhood disease, although adults may be affected.
true
what is metastatic mumps?
may involve other organs (e.g., testes, ovaries, breasts, meninges)
Presentation: 13yr w/ 2d history of facial swelling on lt side; pain w/out fever or ear discharge; recently began tuba
Physical exam shows swelling of left cheek w tenderness on palation
Lab results show serum amylase 3x the normal amount.
What is the condition?
pneumoparotid
(CT shows air in left parotid gland and duct)
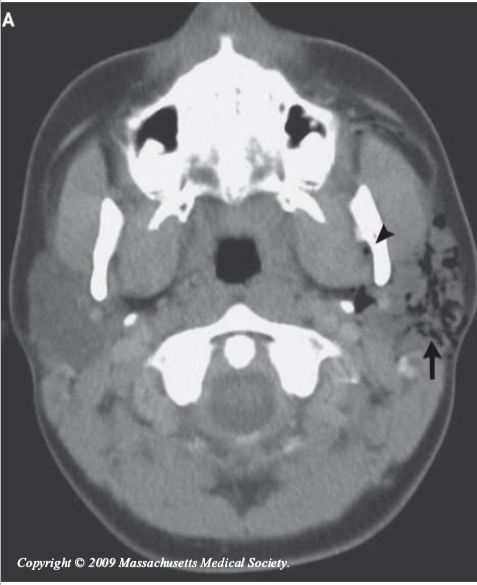
what is the treatment for pneumoparotid?
parotid massage = foamy secretions from duct
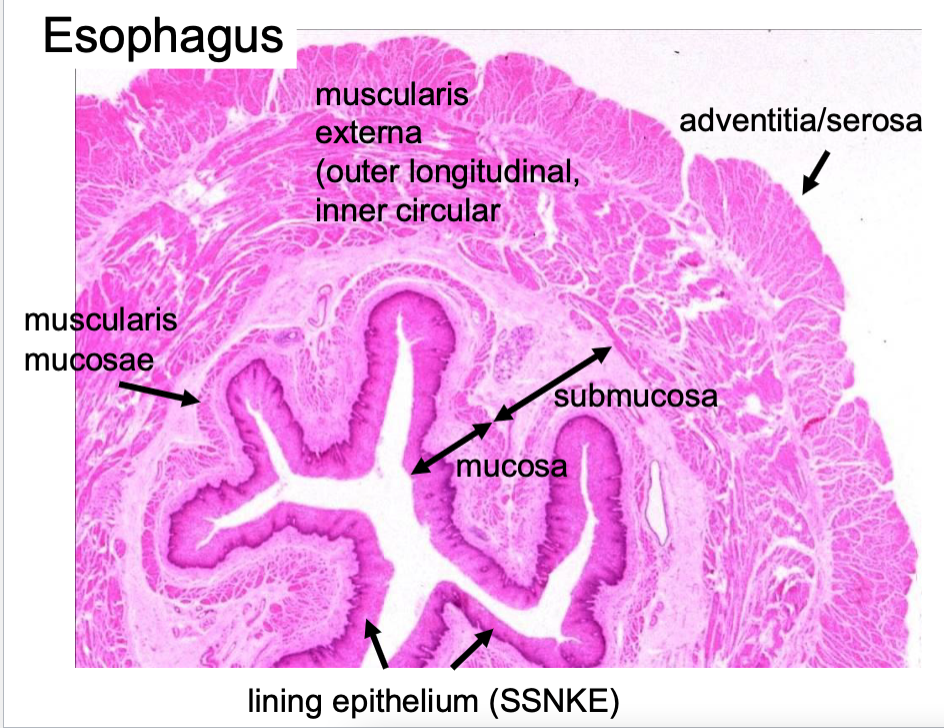
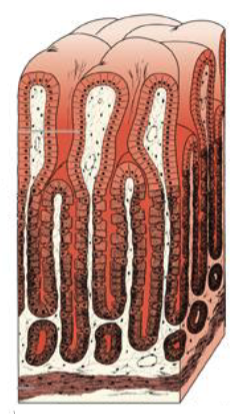
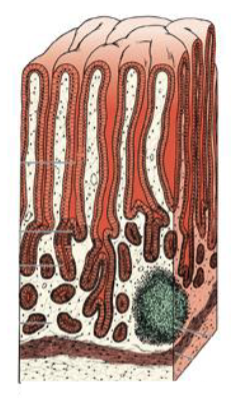
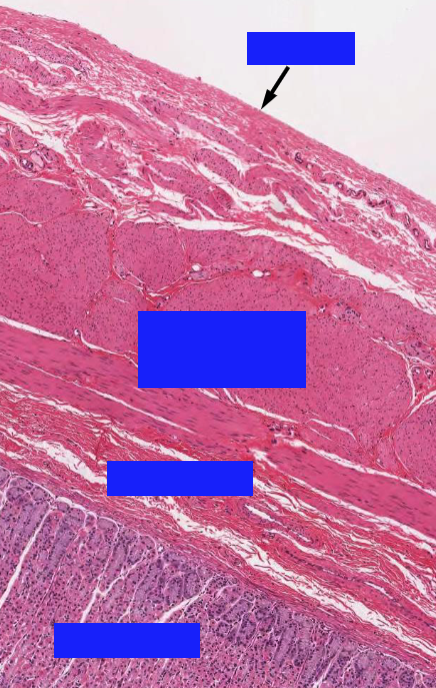
what are the layers of the GI lining?

what is the Muscular tube connecting pharynx to stomach?
esophagus
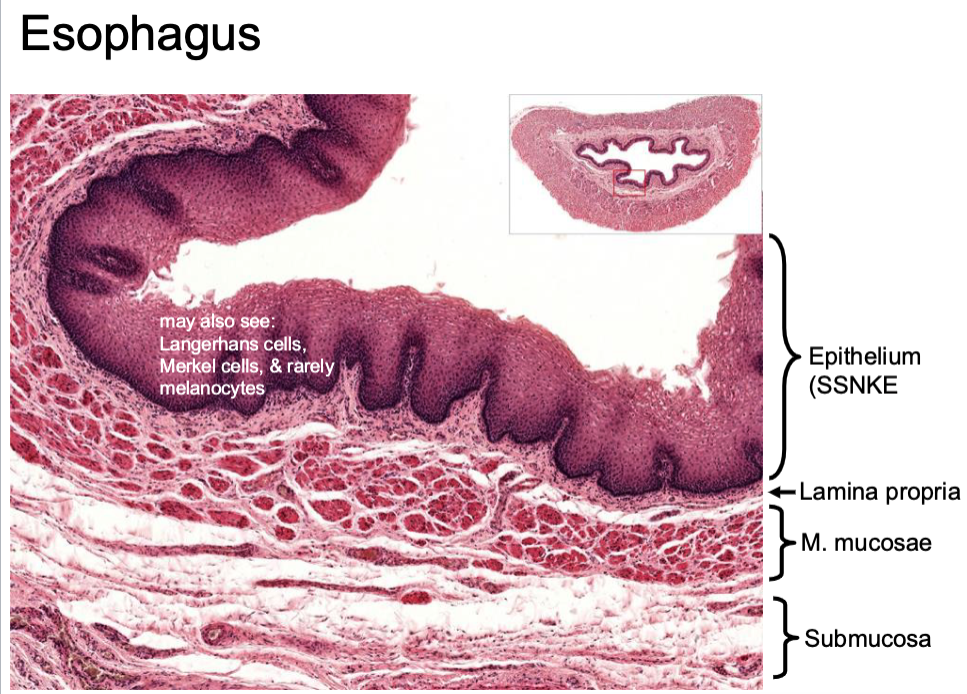
what are the layers of the mucosa?
epithelium
lamina propria
muscularis mucosae
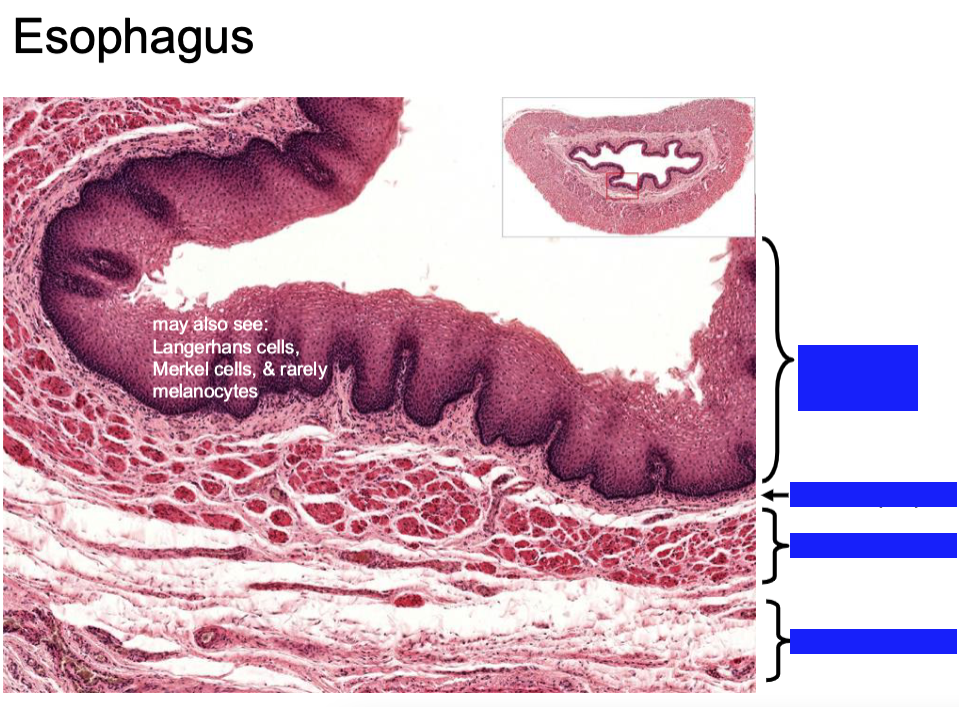
what are the layers of the esophageal mucosal lining?
SSNKE (epithelium)
lamina propria
muscularis mucosae
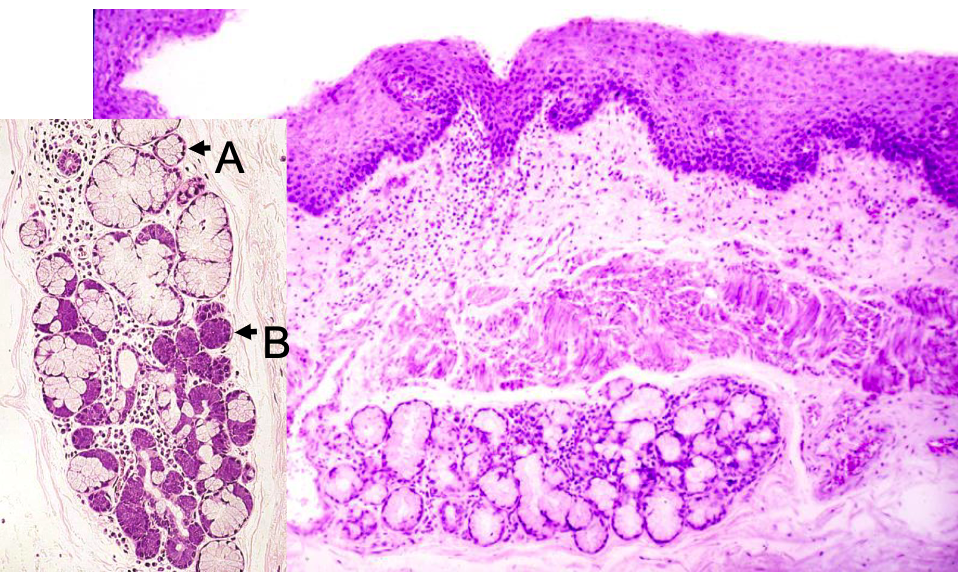
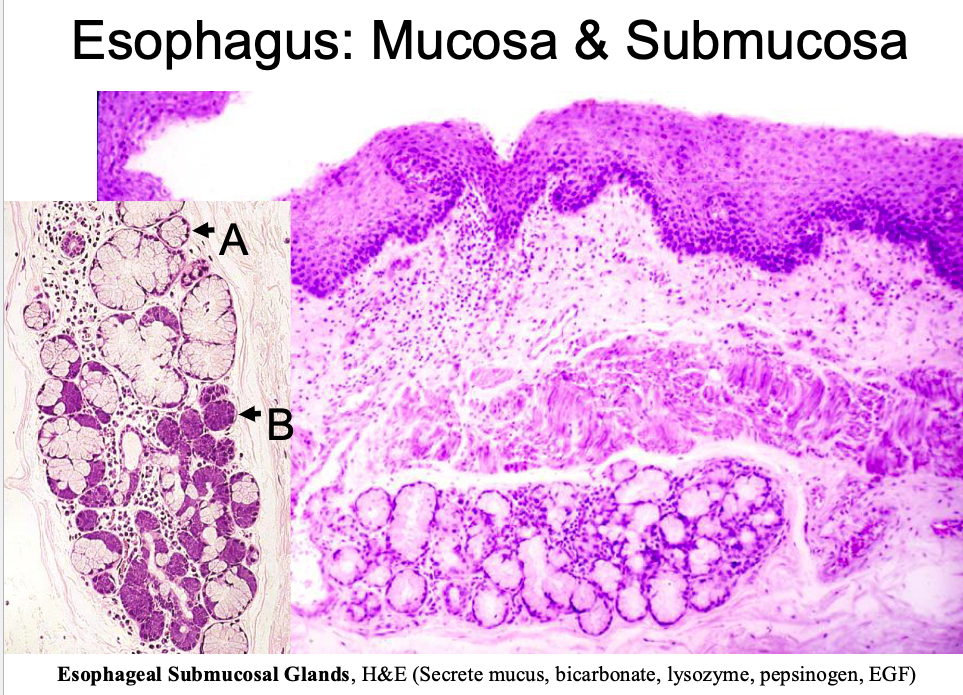
what are the components of esophageal submucosa?
loose CT
esophageal glands (*only esophagus and duodenum have submucosal glands)
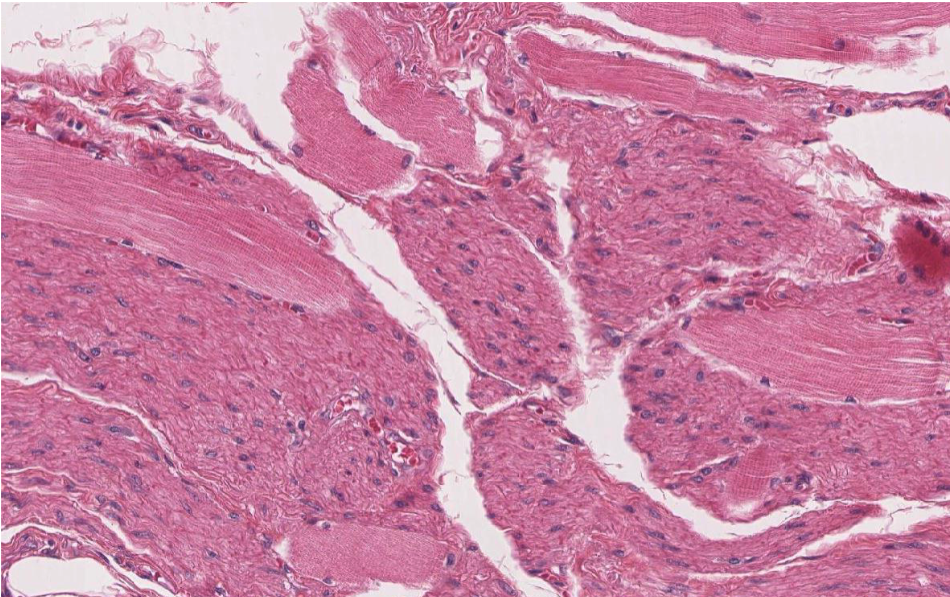
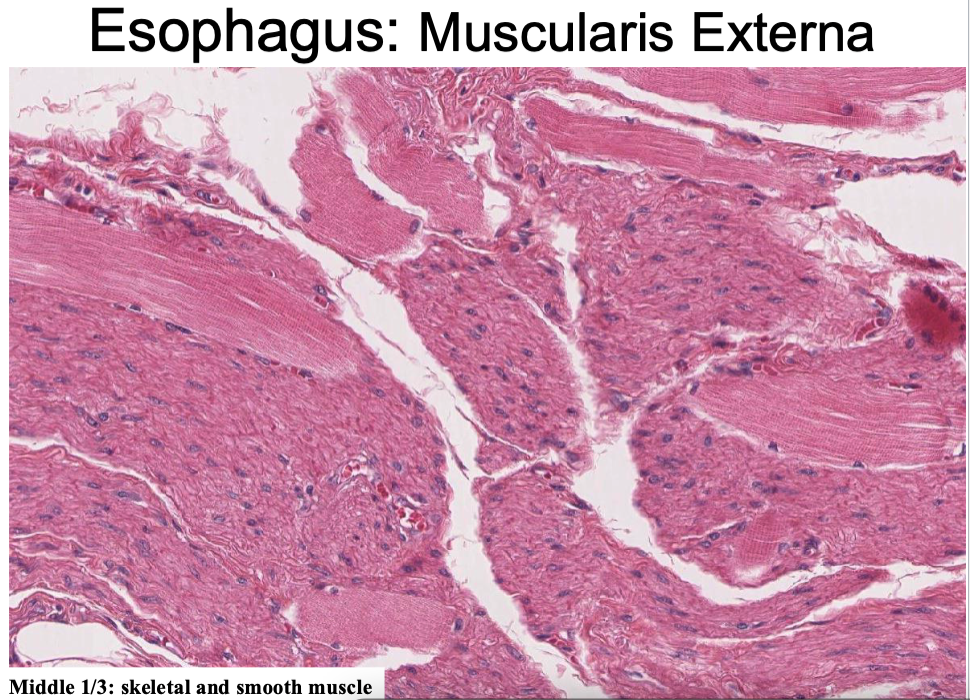
what kind of muscle is found in the esophageal muscularis externa?
inner circular/outer longitudinal
upper 1/3 = skeletal muscle
middle 1/3 = skeletal/smooth mixed
lower 1/3 = smooth muscle
where is the esophageal adventitia located?
thorax
where is the esophageal serosa located?
abdominal cavity
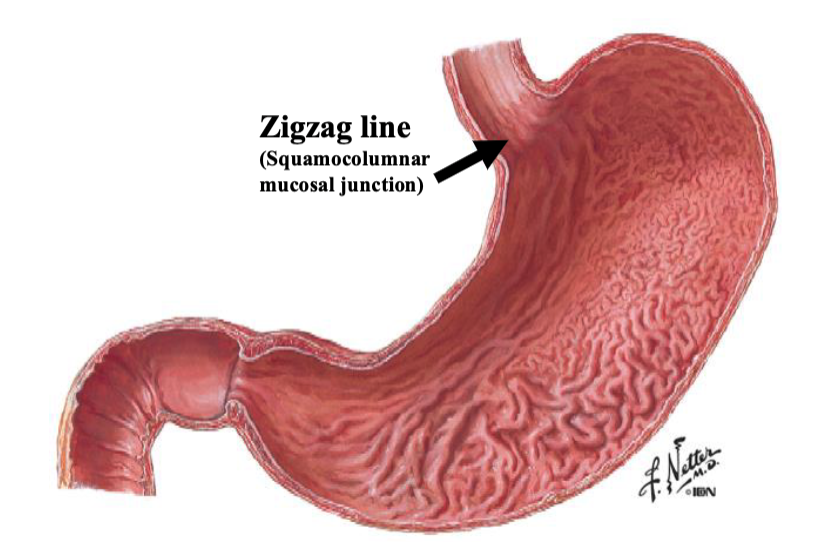
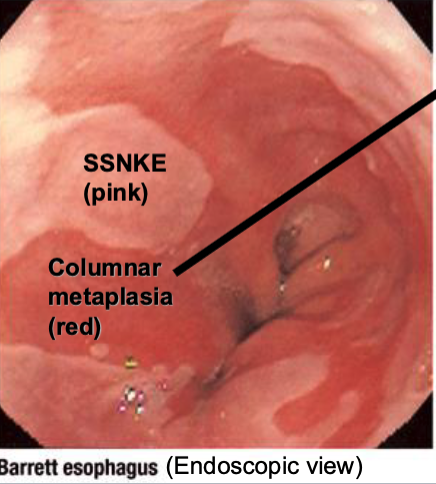
what is the zigzag line in the stomach?
squamocolumnar mucosal junction (area where the esophagus's normal squamous mucosa transitions to the columnar mucosa of the stomach)
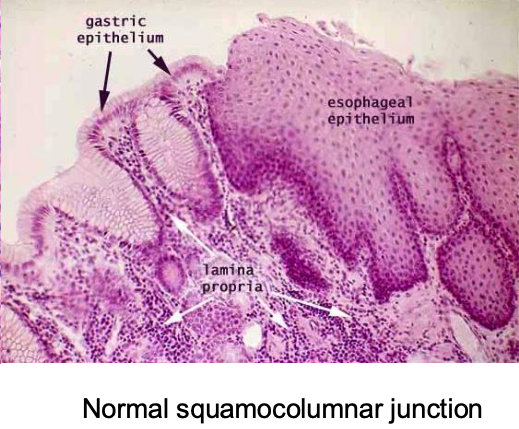
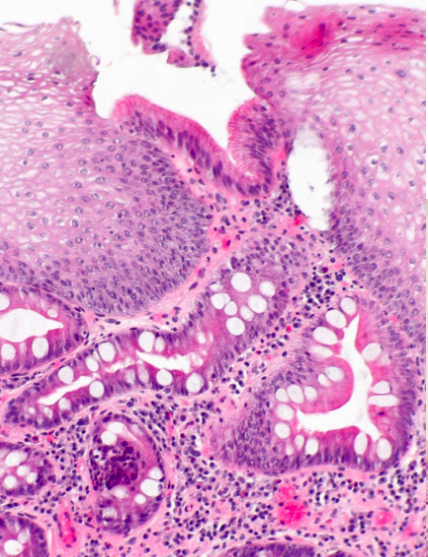
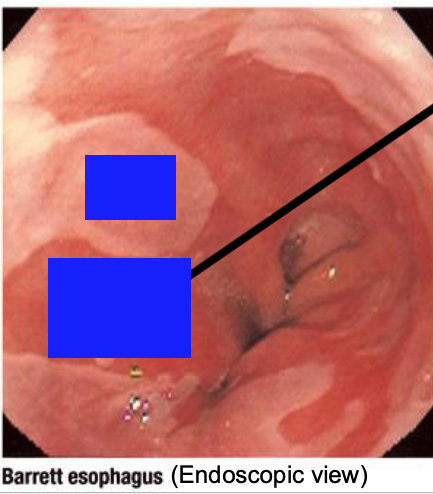
what is Barrett’s esophagus?
Abnormal squamocolumnar junction -metaplasia (to gastric or intestinal mucosa)
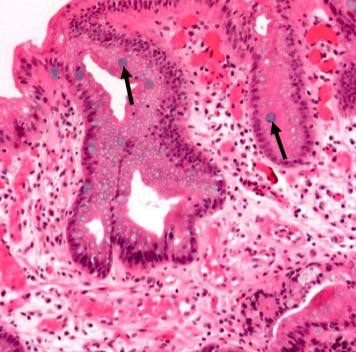
Short arrows: goblet cell mucins stained with alcian blue
b
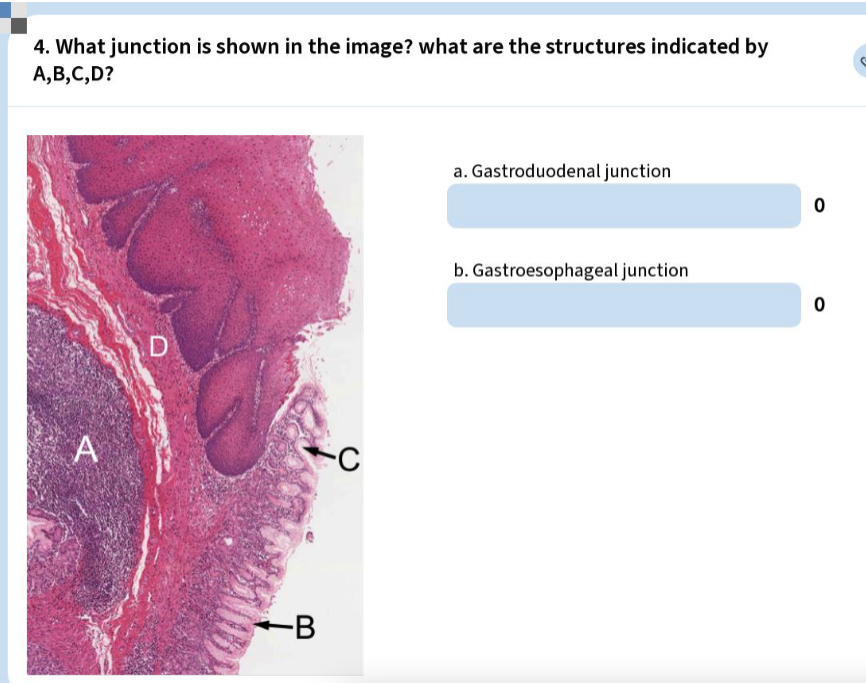
A=MALT (mucosa associated lymphoid tissue)
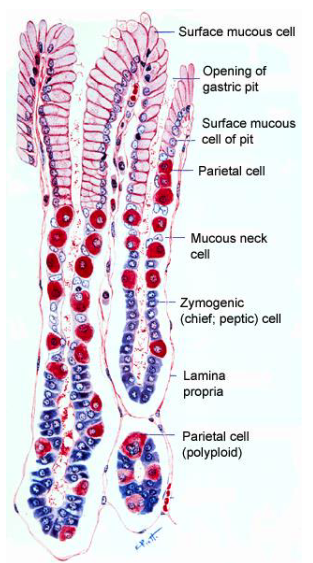
B=surface mucous cells,
C=gastric pit
D=muscularis mucosa
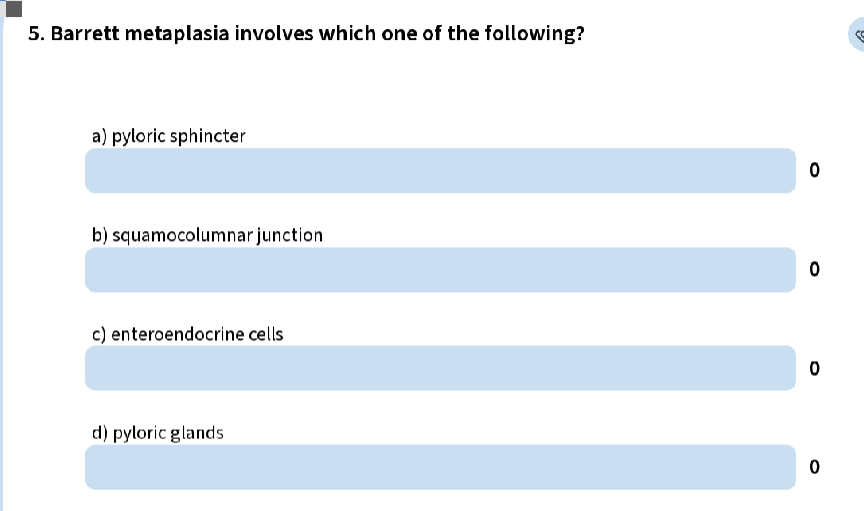
B) squamocolumnar junction
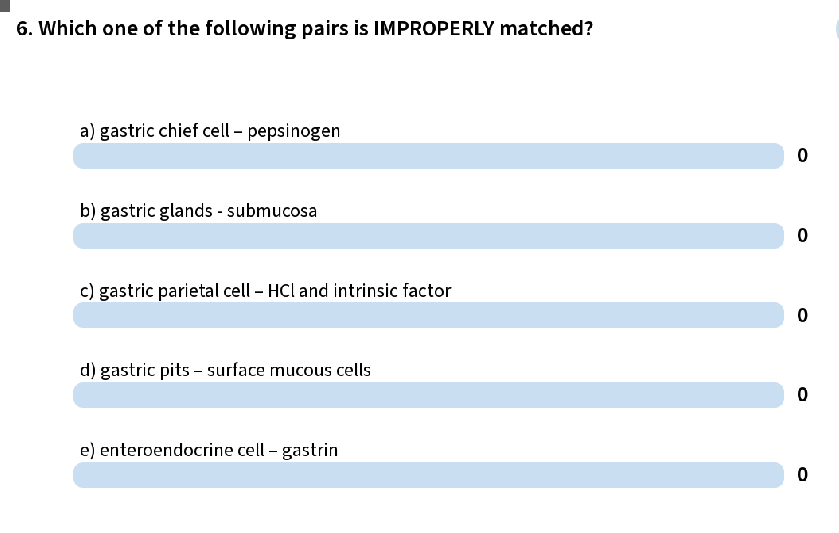
b (gastric glands are in the mucosa)
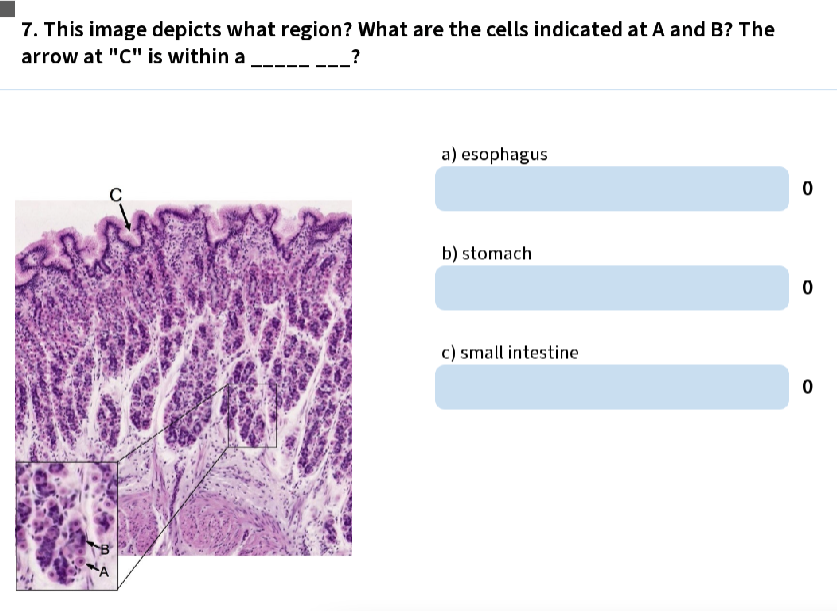
b, A=parietal, B=Chief, C=gastric pit
are there submucosal glands in the stomach?
no
what type of muscles make up the muscularis externa of the stomach?
inner oblique (limited); middle circular; outer longitudinal (limited)
what are the stomach mucosal glands?
cardial gastric glands
gastric glands proper
pyloric glands
which type of stomach mucosal gland is this:
short pits; short glands
Cells: mucous, stem, enteroendocrine, occasional parietal
Short segment: <4mm
Cardial gastric glands
which type of stomach mucosal gland is this:
short pits; long glands
Cells: mucous neck, stem, parietal, zymogenic chief, enteroendocrine
Gastric glands proper (fundic glands)
which type of stomach mucosal gland is this:
long pits; short glands
Cells: mucous, stem, enteroendocrine, occasional parietal
Pyloric glands
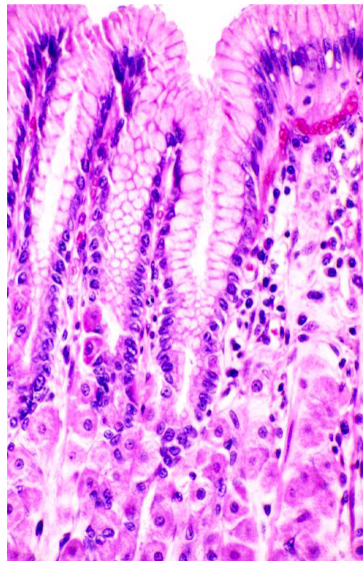
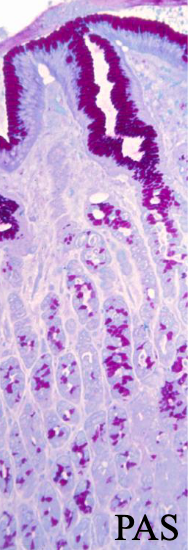
Stomach: Surface Mucous Cells
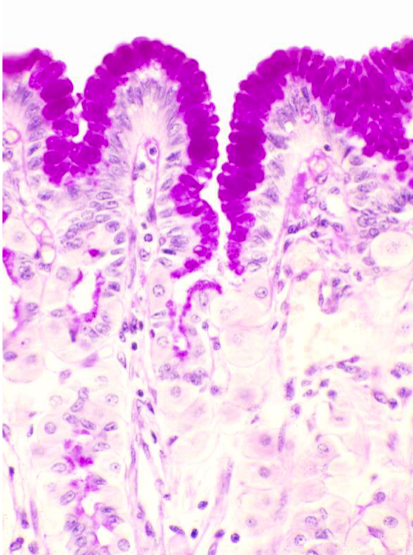
Stomach: Surface Mucous Cells
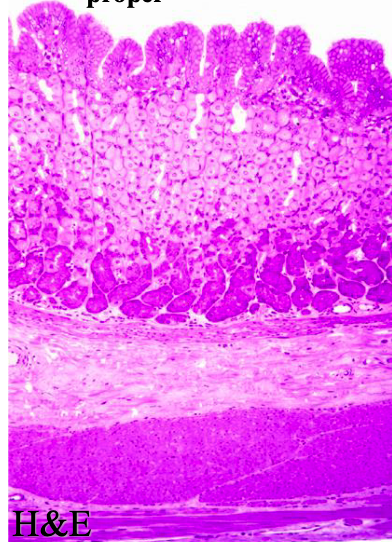
Gastric glands proper
Mucous neck cells (fundus)
________ deficiency can lead to decreased rbc development (pernicious anemia)
Vitamin B12
which stomch cells secrete HCl an intrinsic factor which helps with vit B12 absorption in gut?
parietal
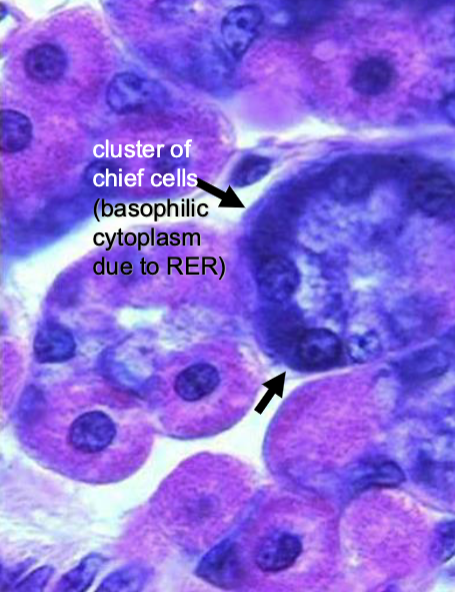
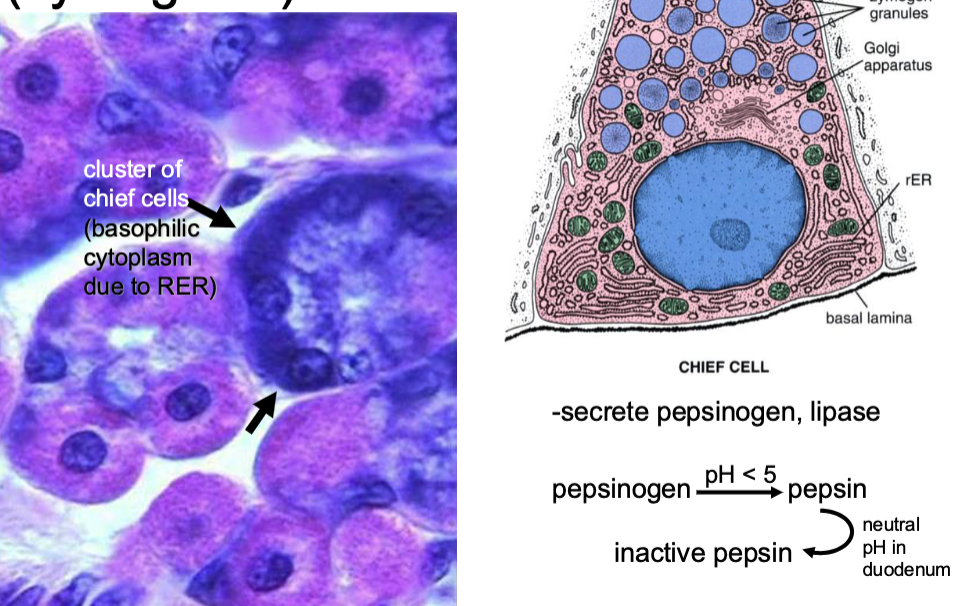
which stomach cells secrete pepsinogen and lipase?
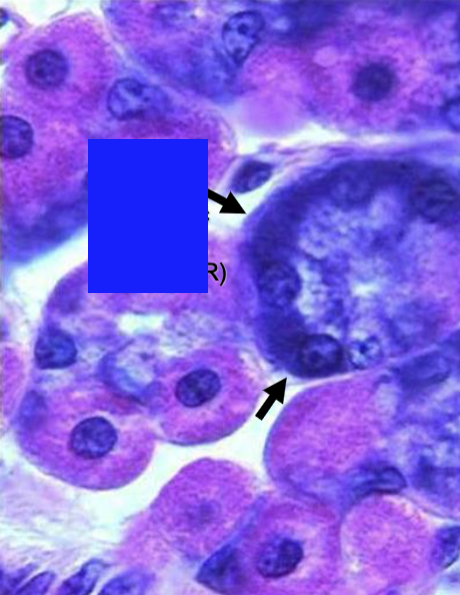
chief (zymogenic) cells

which stomch cells are eosinophilic due to abundant mitochondria/
parietal cells