A&PII MODULE 3
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
myocardium
heart muscle
heart & generating blood pressure
heart/myocardium squeezes → blood pushed into arteries (from the chambers) → pressure builds up and pushes against the artery walls = blood pressure
heart & routing blood
right ventricle = pushes blood into the pulmonary arteries (to lungs)
left ventricle = pushes blood into the aorta (to the whole body)
right = respiratory
left = life
heart & ensuring one-way blood flow
valves prevent backflow during contractions
heart & regulating blood supply
heart adjusts cardiac output based on nerves/hormones
cardiac output
total volume of blood pumped by a ventricle per minute
all the squeezes in a minute
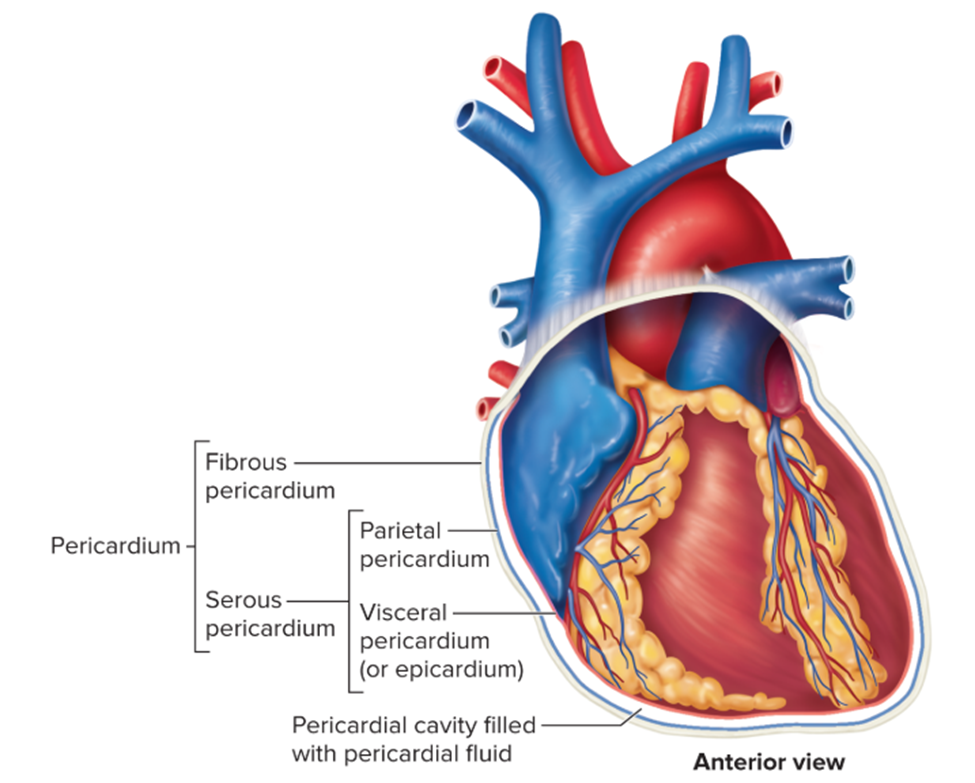
pericardium location
encloses the heart within the mediastinum
fibrous pericardium
tough outer layer that anchors the heart
fibrous = firm & fixed
serous pericardium
inner layer, delicate and produces lubrication fluid (fluid for friction-free beating)
serous = slippery & smooth
structure of serous pericardium
two layers:
parietal - lines fibrous pericardium
visceral - covers heart surface
pericardial cavity between layers contains pericardial fluid
location of the heart
in the mediastinum of the thoracic cavity
base of the heart
superior, flat, deep to sternum
where the great vessels attach
apex of the heart
inferior, pointy tip near diaphragm
what are the top chambers
atria
atria = Always on top (lightweight chambers)
what divides the top chambers
interatrial septum
what are the bottom chambers
ventricles
ventricles = Very strong bottom chambers
what divides the bottom chambers
interventricular septum
what valve separates the top right from bottom right side
Tricuspid (right AV) valve
TRI before you BI (Tricuspid on right, Bicuspid/Mitral on left)
what valve separates the top left from bottom left side
bicuspid/mitral (left AV) valve
TRI before you BI (Tricuspid on right, Bicuspid/Mitral on left)
what valve separates the right bottom chamber from the vessel leaving the heart
pulmonary valve / right semilunar valve (same thing)
RAP: Right Atrium = Pulmonary
What valve separates the left bottom chamber from the vessel leaving the heart?
aortic valve / left semilunar valve
LAA: Left Atrium = Aorta
epicardium
epicardium = exterior
outermost / superficial layer covering the heart
Myocardium
Myocardium = Muscle
thick, muscular layer
contracts to pump blood
Myocardium & heart skeleton
Myocardium is anchored to the fibrous skeleton
→ structural support
→ electrical insulation between atria and ventricles
endocardium
deepest layer of the heart
lines inner chambers
simple squamous epithelium
pectinate muscles
atria muscle
internal ridges
crista terminalis
atria muscle
ridge separating pectinate muscles from smooth atrial wall
trabeculae carneae
ventricle muscle
internal ridges
papillary muscles
ventricle muscles
anchors chordae tendineae to prevent AV valve backflow
cardiac muscle physical appearance
cardiac muscle tissue = striations and branching fibers
is cardiac muscle voluntary or involuntary
involuntary
controlled by autonomic nervous system and intrinsic properties
auto-pilot
what structures connect adjacent cardiac muscle cells
intercalated disks
→ thick end-to-end connections
→ allow synchronized contraction
inside structures of intercalated disks
desmosomes: hold cells together so they don’t pull apart during contraction
gap junctions: pass electrical signals and ions so cells contract together
D = Durable anchor
G = Gateway for signals
What energy sources can cardiac muscle cells use to produce ATP?
Aerobic metabolism
use fatty acids, glucose, and lactate for ATP production
how does aerobic respiration benefit cardiac muscle function
ensures a continuous supply of energy for constant contraction
list in order the structures associated with the conduction system
Sally Always Buys Real Purple Mugs
SA node
AV node
Bundle of His
Right & Left branches
Purkinje fibers
Myocardium
Explain how the action potential moves through the conduction system and stimulated surrounding muscle
Sally And Bob Bring Pizza
SA node → AV node → Bundle of His → Bundle branches → Purkinje fibers
Action potential starts in SA node and spreads through the atria to the AV node, down the AV bundle and bundle branches, then through Purkinje fibers, which stimulate ventricular muscle to contract
autorhythmic
can self-stimulate contraction without external signals
automatic rhythm
where does a heartbeat originate
SA node = pacemaker of the heart
SA node = spark plug of the heart
Explain the channels and ions involved in the initiation of a heartbeat
Pacemaker potential: Na⁺ leaks into the SA node cells, depolarizing the membrane
Threshold reached: Voltage-gated Ca²⁺ channels open, causing rapid depolarization
Repolarization: K⁺ channels open, letting K⁺ exit the cell, returning it to the resting state
→ cycle repeats automatically, generating the rhythmic heartbeat
Na sneaks in → Ca sparks → K exits → heartbeat restarts
pacemaker potential vs action potential in cardiac muscle
pacemaker potential: gradual depolarization to threshold, not a full action potential
action potential: rapid depolarization → plateau → repolarization (longer duration)
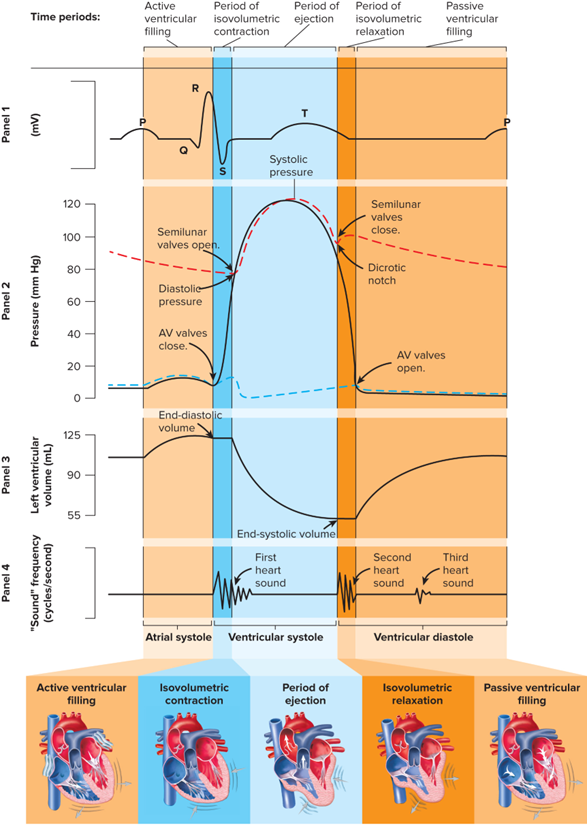
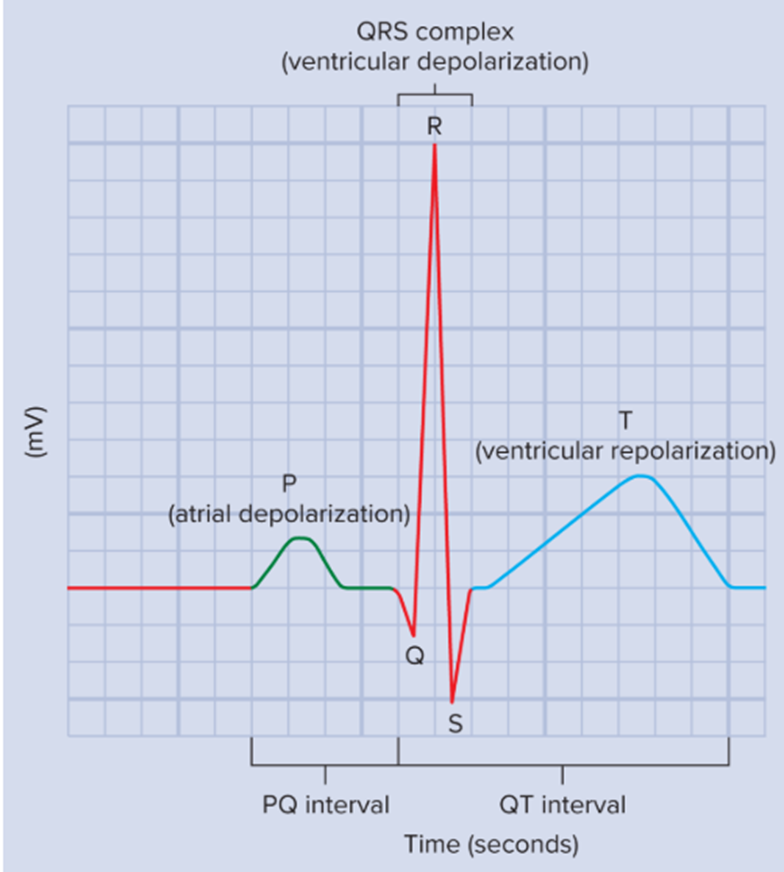
major component of the ECG
P wave: atrial depolarization
- atria depolarize → atria contract → push blood into ventricles
QRS complex: ventricular depolarization
- ventricles depolarize → ventricles contract → blood pumped out
T wave: ventricular repolarization
- ventricles repolarize → ventricles relax → heart resets for next cycle
P = Push Atria
QRS = Squeeze ventricles
T = Take a break
cardiac cycle
one full heartbeat (atria + ventricles contract and relax to move blood)
systole
contraction
South Carolina/Sweet Caroline
diastole
relaxation
Phases of the cardiac cycle
P.A.C.E.R
Passive
Active
Contract
Eject
Relax
Passive Ventricular Filling (1st phase)
atria: relaxed
ventricles: relaxed
blood flow: from atria to ventricles naturally
ECG: between T & next P wave
Active Ventricular filling (2nd phase)
atria: contract
ventricles: relaxed
blood flow: atria push remaining blood into ventricles
ECG: P wave (atrial depolarization)
Isovolumetric Contraction (3rd phase)
atria: relaxed
ventricles: contract
blood flow: all valves closed; pressure rises but no blood leaves
ECG: start of QRS (ventricular depolarization)
Ejection (4th phase)
atria: relaxed
ventricles: contract
blood flow: semilunar valves open; ventricles push blood out to aorta/pulmonary trunk
ECG: QRS continues
Isovolumetric Relaxation (5th phase)
atria: relaxed
ventricles: relaxed
blood flow: all valves closed; ventricles relax
ECG: T wave (ventricular repolarization)
heart sounds
S1 = AV valves close (at start of ventricular contraction) (LUB)
S2 = Semilunar valves close (at end of ventricular contraction) (DUB)
intrinsic vs extrinsic control of heart rhythm
intrinsic: heart’s own properties / inside job (SA node)
extrinsic: external control (nerves/hormones)
preload & heart rhythm
preload: the amount of blood in ventricle before contraction
increases stroke volume: more preload → more stretch of heart muscle → stronger contraction → higher stroke volume
more stretch = more squeeze
stroke volume
the amount of blood pumped out of a ventricle with each beat
blood pumped per beat
single squeeze
sympathetic nervous activity & heart rhythm
increases heart rate
increases contractility
Sympathetic = Speeds up
contractility
the strength of ventricular contraction
how hard the heart squeezes
Parasympathetic nervous activity & heart rhythm
decreases heart rate (via vagus nerve)
Parasympathetic = Pumps down
Epinephrine/Norepinephrine & heart rhythm
increases heart rate, contractility, stroke volume
pulmonary circulation
transports blood from the right ventricle to the lungs for gas exchange (blood gets oxygen) and then returns it to the left atrium
right → lungs → left
systemic circulation
transports blood from the left ventricle to the body tissues to supply oxygen and nutrients, then returns deoxygenated blood to the right atrium
Left → Body → Right
coronary circulation
part of the systemic pathway
heart feeds itself from the aorta
1) arteries bring oxygen-rich blood to the myocardium
2) veins remove deoxygenated blood from the heart and drain it into the coronary sinus (which empties into the right atrium)
Pulmonary arteries + veins VS systemic arteries + veins
pulmonary:
arteries carry deoxygenated blood
veins carry oxygenated blood
systemic:
arteries carry oxygenated blood
veins carry deoxygenated blood
Pulmonary is flipped, systemic is standard
A blood cell is returning to the heart from the lungs. List in order the chambers, valves, and vessels the cell will pass through
1) Oxygenated blood returning from lungs
2) Pulmonary veins
3) Left atrium
4) Left ventricle
5) Aorta
6) Brain
7) Systemic veins
8) Right atrium
9) Right ventricle
10) Pulmonary trunk
11) Lungs
if a heart murmur involves the aortic valve, how would this impact circulation
aorta leaks → weak systemic flow
backflow into the left ventricle will decrease systemic circulation
if a heart murmur involves the mitral valve, how would this impact circulation
left atrium backflow → poor ventricular filling
from sitting to standing, how is heart rate affected
standing up = HR increases to fight gravity & maintain blood flow
calcium channel blockers
calcium channel blockers = less Ca²⁺ in = slower, weaker beat = lower BP
AV (atrioventricular) valves
betwwen atria and ventricles
right : tricuspid
left : bicuspid/mitral
TRI before you BI (Tricuspid on right, Bicuspid/Mitral on left)
prevent blood from flowing back into atria when ventricles contract
Semilunar valves
between ventricles and arteries leaving the heart
right : pulmonary
left : aortic
prevent blood from flowing back into ventricles after its ejected