Ischemic cardiovascular conditions & other vascular pathologies
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
ST elevation is associated with…
infarction
ST depression is associated with…
Ischemia
Prevalence of CAD among soldiers
-77.3% of 300 soldiers
-Mean age: 22.1
-In 10 men, complete obstruction of one or more coronary arteries was found
Anatomy of the coronary arteries
-Outer layer: adventitia
→provides support for the artey
→Houses the vessels that furnish the middle layer (vasa vasorum)
-Middle layer: media
→smooth muscle cells; resonsible for making laminal diameter adjustments based on required blood flow
-Inner layer: intima
Myocardial perfusion
-Perfusion is the blood flow/exchange at the capillary level in tissue
→adequate tissue perfusion: supply meets demand
→inefficient perfusion = ischemia (chronic ischemia can lead to infarction, dependent upon severity)
→Lack of perfusion = infarction
-Myocardial perfusion, like all muscle beds, occurs primarily during periods of muscle relaxation (diastole)
→allows time for perfusion to occur
Major determinants of myocardial blood flow
-diastolic BP is the major driving force moving into the myocardial tissue
-Resistance to flow is most commonly caused by atherosclerosis
→coronary arteries have collateral arteries (constant use and pressure increase their size and strength, connecting to the surrounding collateral arteries; creating a solid bypass around the blocked coronary artery)
atherosclerosis
-a disease that causes progressive hardening and narrowing of the coronary, cerebral, and peripheral arteries (occur in the intima and endothelial walls)
-Atherosclerotic plaque is composed of lipids and thrombus
Atherosclerosis: pathophysiology; “artherosis”
-Artherosis: build up of lipid blockages
-Clusters of monocytes have been found in areas where they accumuate lipids, combined together called foam cells
-first discussed lesion of atherosclerosis is a fatty streak (foam cells and smooth muscle cells)
-fatty streaks grow so large that the endothelium is stretched and begins to separate even further. endothelial separation exposes the intima even more (platelets bunch and a thrombus forms)
Atherosclerosis: pathophysiology; “sclerosis”
-a reduction in blood vessel compliance
-fatty streak lesions create scar tissue (increased collagen) and destruction of elastin
Vasospasm- Typical angina
-seen with exercise or activity (seen with myocardial O2 demand)
-result in ST segment depression (ischemia, decreased O2 demand)
Vasospasm- Prinzmetal angina (variant)
-seen at rest, typically in the early morning, not associated with exercise (seen without myocardial O2 demand)
-Results in ST-segment elevation
-Relieved by nitroglycerin or other vasodilators
-atherosclerosis believed to be main cause of(endothelial layer damage and lesion into smooth muscle, causing artery to spasm; spasm creates infarction, hence ECG appearance)
AHA research risk factors of heart and cardiovascular disease
-smoking
-physical inactivity
-obesity
-suboptimal diet
-HTN
-elevated serum cholesterol
-DM
-Fam hx
-age
-gender (men>females)
-stress
Risk factors: smoking
-15% all cardiovascular deaths
-Smoking decreases HDL’s
-Secondhand smoke has also been proven to be a factor in the development of cardiopulmonary disease
Risk factors: physical activity research from the CDC
-Lack of physical activity is the number one risk factor for developing chronic heart disease
→other factors include sedentary lifestyle (women>men); 60% americans do not recieve the min amount of exercise required daily; diabetic>non-diabetic
risk factors: body weight
-68% of pop is overweight or obese
-Several studies have associated obesity with the development of CHD (more prevalent if adipose is localized in the abdomen)
risk factors diet
-AHA recommends 4.5 cups of fruits&veggies/day; 2 servibgs fish/week, 3 servings whole grains/day, limiting sugar sweetened drinks to 36 oz/week or les, 1500mg sodium/day
Risk factors: chlesterol
-direct intake of cholesterol is not the principal influence on the level of cholesterol in the blood; instead its the intake of saturated fats which influence the lipoproteins most
-HDL: higher HDL levels help to fight and reduce the LDL levels
→HDL: <35m/dL is a risk factor
-Elevated triglycerides increase risk for CVD: >150 mg/dL
-The best predictor of risk is a total cholesterol to HDL ratio
→ A ratio greater than 4.5 increases the risk of an individual developing atherosclerosis
Values (total cholesterol, LDL, HDL, triglycerides, BP, fasting glucose)
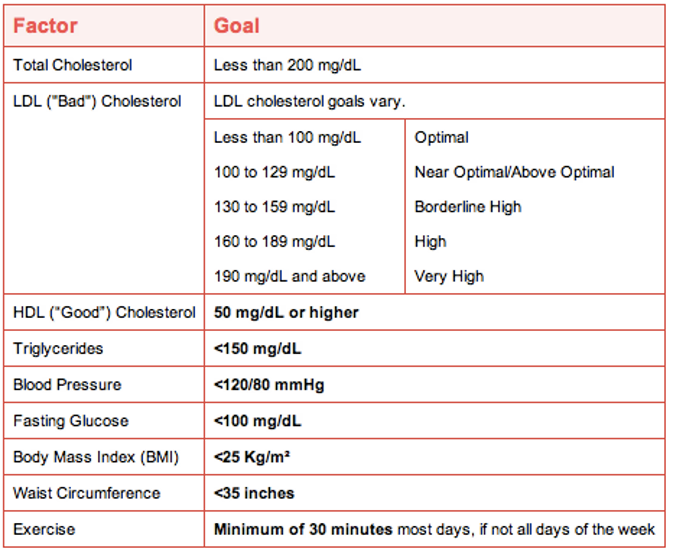
Risk factors: fasting blood glucose
-fasting glucose: should be less than 100 mg/dL (>100mg/dL=inc risk for heart disease)
-glucose hase proven to:
→decrease HDL production*
→Increase LDL production*
*all of which are factors for developing CVD
risk factors: family hx
-parent or sibling has been shown to affect the onset of CVD
-Hypercholesterolemia and HTN are highly genetic in nature
Risk factors: gender/age
-Gender
→men have more of a risk for having a MI
-research proves that once an individual has a MI, women have more risk for mortality (age/life expectancy related)
-Average age for initial MI
→Men 64.7
→Women 72.2
Risk factors stress
-increased stress stimulates sympathetic nervous system “fight or flight”
-increased levels of platelet secreted proteins
-increased risk for CVD
clinical presentation of chronic heart disease
-sudden cardiac death (ventricular tachycardia and ventricular fibrillation are usually the cause of sudden death; prompt AED utilization and/or immediate arrival to the ER are the only chance for survival)
-Chronic stable angina (chest pain resulting from inadequate O2 supply to myocardial tissue with activity; double product, or rate-pressure product (SBPxHR)) patients can correlate their functional levels as to when they do not adequately meet the O2 demand
-unstable angina (chest pain at rest) (acute MI)
Myocardial infarction S&S (most common warning signs of heart attack)
-uncomfortable pressure, pain squeezing in the center of the chest (prolonged)
-pain that spreads to the throat, back, neck, and arms
-chest discomfort with lightheadedness or dizziness
-pallor, nausea, sweating
-prolonged sxs not relieved by rest, nitroglycerin, or antacids
Myocardial infarction S&S: atypical, less common
-especially women
-unusual chest pain, stomach pain
-isolated right biceps pain
-flu-like manifestations
-breathlessness, dizziness
-unexplained intense anxiety, weakness or fatigue
-"tightness/pain along posterior bra strap region"
pathophysiology of ischemic heart disease (IHD) in women
women have:
-less obstructive CAD (vessel remodeling?)
-more plaque erosion and distal embolization
-higher incidences of inflammatory conditions (phlebitis? myocarditis?)
Factors that contribute to unstable angina (chest pain at rest)
-atherosclerotic plaque rupture in an already partially blocked artery (most common)
-dynamic obstruction (coronary vasocostriction (Printzmetal’s)
-tachycardia causing myocardial ischemia
Types of angina- other causes for chest pain: stable angina (effort angina)
develops with activity, relieved with rest or nitro (NTG)
Types of angina- other causes for chest pain: unstable angina (direct correlation to lack of O2 demand)
chest discomfort is increasing in intensity. does not respond to rest
Types of angina- other causes for chest pain: Prinzmetal angina (“Variant” angina; adequate O2, spasms cause issue)
chest discomfort associated with coronary spasm. occurs at rest. more likely in the morning or at night/while sleeping. responds to vasodilators such as nitroglycerine. more common in women and smokers
Types of angina- other causes for chest pain: pericarditis
pain at rest or activity- not relieved with rest or NTG. responds to anti-inflammatory meds. common post CABG
Types of angina- other causes for chest pain: pulmonary dx (pleuritis, pneumothorax)
Sharp in nature, which changes with breathing. decreased or abnormal breath sounds
Types of angina- other causes for chest pain: bronchospasm
induced by cold, extreme coughing relieved with bronchodilators
Types of angina- other causes for chest pain: vascular (PE)
constant, sudden onset, SOB
Types of angina- other causes for chest pain: GI
psptic ulcer, GERD, usualy related to food intake, relieved by antacids
Angina scale
-sed in rating subjective pain associated myocardial insufficiency
mild, barely noticeable
moderate, bothersome
moderately severe, very uncomfortable
most severe, or most intense pain ever experience
Provocative ergonovine testing
-Ergonovine is a medicine that vasoconstricts
-distinguishes angina between narrowing of arteries from plaque or vasospasm
-Indication for testing is (+) ECG and symptomatic for ischemia, but (-) angiography plaque
-Ergonvine is injected and agiograhy is performed
-Positive results: negative angiography first, with narrowing of the CA artery after ergonovine testing that reproduces the symptoms of angina for the patient. Immediately after, administration of a medical vasodilator is provided for safe means
STEMI
-ST elevation myocardial infarction, which happens as a result of a complete blockage in a coronary artery
-carries a great deal of risk, disability or death
-A MI occurs
Non-STEMI
-happens when a coronary artery is partially blocked, severely reducing blood flow
-non-stemi heart attack may occur
Tx of STEMI or Non-STEMI
-clot-busting medication
→fibrinolytic, thrombolysis
→most effective if given within 30 min of the attack
→negative effects: it poses a bleeding risk elsewhere
→all hospitals can do
-mechanical/surgical means
→stents, angioplasty, or similar methods to open the arteries, percutaneous coronary intervention (PCI)
→Non-PCI hospitals cannot meet the needs of STEMI patients, and often refer out to PCI hospitals (if a patient cannot get a PCI hospital within the golden 90-minute window, they will receive diltiazem-busting meds)
Crticial stenosis is defined as
-an occlusion >70%
-no intervention unless critical senosis is present
Calcium score test
-coronary calcium scan
-uses computerized tomography (CT) to detect calcium deposits in the coronary arteries of the heart
-higher coronary calcium score suggests you have a higher chance of significant narrowing in the coronary arteries and a higher risk of future heart attackM
MI CAUSES, OTHER THAN ATHEROSCLEROSIS
-trauma
-congenital
-metabolic disease
-other (vasospasm, electrolyte imbalance, stress, drugs (caffeine)
Type I-V MI
I: correlates to infarction with direct etiology linked to CAD
II: correlates to an infarction NOT linked to CAD (vasospasm; hypoxemia from COVID)(patient has demand ischemia first due to lack of O2 supply, not due to coronary artery blockage. Demand ischemia turns into infarction as it progressively worsens.
III: we do not know what caused MI; patient passed away/could not get appropriate biomarkers for etiology; if autopsy performed later, then dx would change)
IV: MI due to PCI
V: MI due to CABG
medical management of acute coronary syndrome
-prompt recognition (receiving care within 60-90 minutes increases prognosis significantly)
-#1: repercussion, restoring blood flow to an organ, in this case t re-perfuse the heart (aspirin, anticoagulant therapy, improve O2 by administering O2, controle cardiac pain using nitrates, morphine, B-blockers to decrease demand on the heart)
-prevent complications to myocardial tissue
-decrease cardiac chest pain
complications with STEMI and non-STEMI
-Hypokinesis: reduction in the strength of contraction
-Akinesis: no contraction
-Dyskinesis: abnormal movement during contraction
Hyperkinesis is often seen in the non-infarcted areas and is thought to be due to increased sympathetic NS activity compensating for the infarcted tissue
left ventricular heart failure
-15-24% damage involvement of left ventricle
→stroke volume declines
→may or may not see S&S of heart failure (lower stroke volume leads to a lower aortic pressure and subsequently a reduction in coronary perfusion pressure)
-25-39% or more involvement
→S&S of heart failure are seen
-40% or more involvement
→most often death occurs
complications post-MI; if seen, will occur within first 24-48 hrs post MI
-ventricular tachycardia
-atrial flutter or fibrillation
-second or third degree atrioventricular (AV) blocks
-persistent sinus tachycardia (above 100 bpm_
-persistent systolic hypotension (below 90 mmHg)
-pulmonary edema
-persistent angina
-patients without complications post-MI have significantly lower morbidity rates.
-prolonged or complicated hospital course affects an individual’s activity progression due to the effects of inactivity or bed rest
Additional complications post-MI
-depression
-anxiety
ventricular remodeling
-Remodeling following an MI typically involves pathological changes in the left ventricle (deposition of collagen, leading to myocardial fibrosis)
-Over time, the infarct region becomes scar tissue (results in thinning of ventricular wall and dilation of the left ventricle; decline in cardiac function and reduced EF)
prognosis post-MI dependent on
-amount of complications
-infarct size
-presence of disease in other coronary arteries
-LEFT VENTRICLE FUNCTION (most important)
Myocardial infarctions
-results from prolonged myocardial ischemia)
-zone of infarction (necrosis, tissue death)
-zone of hypoxic injury (may return to normal if blood supply is restored)
-zone of ischemia (almost always will retuen to normal if blood supply is restored)
Sestambi vs. Thallium 201
-both radioactive dye that is injected IV. looks at how much cell death occurs post MI
-once injected, gamma camera take an image of myocardium 15-20 min post injection
-dye absorbs into healthy myocardium and not into necrotic tissue
-image again taken 4 hrs after to compare
→irreversible damage: area without uptake in both scans means tissue is permanently damaged
→reversible damage: area without uptake on first scan, however uptake occurs on 4 hours post scan, means damage is not permanent and intervention is necessary (stent, CABG)
-Sestambi vs Thallium 201
→Sestambi has higher Sn and Sp than thallium
→Sestambi more expensive
→Sestambi doesnt wash out like thallium so you can still reimage several hours later, wheras thallium you have to reinject 4 hrs later
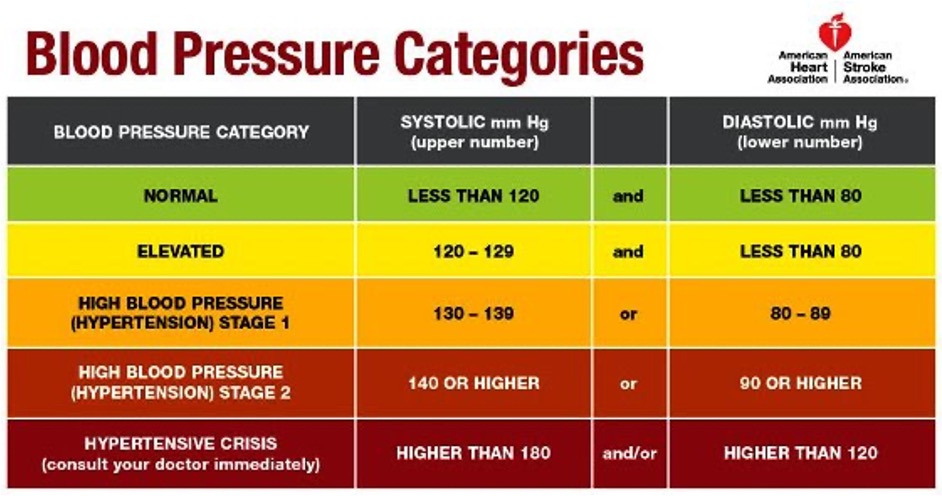
HTN
-primary vs secondary
→1*: 90-95%; aka essential HTN; genetics ,environment, stress, diet, etc
→2* other identifiable medical conditions resulting in HTN; renovascular or endocrine diseases
-Isolated systolic HTN (ISH)
→more sommon in elderly; artery stiffness, diabetes
→SBP is >140, DBP is normal
BP category values
HTN has ___ causes, making it ___ to treat or stabilize
many, difficult
Hypertensive heart disease
-HTN produces pressure overload on left ventricle
→causes hypertrophy and hardening of the myocardium (places more pressure on left atrium to contract harder- compensating for the lack of pump from the left ventricle)
-Now, left atrial hypertrophy develops
→O2 to the coronary arteries by way of the coronary sinus is decreased (predisposition for myocardial ischemia, a-fib, and ventricular dysrhythmias)
-with inadequate filling times in the left ventricle, cardiac stroke volume, cardiac stroke volume and cardiac output is decreased causing decreased supply to peripheral tissue
-eventually will lead to heart failure
Tx for HTN
-goals of antihypertensive therapy is to normalize BP both at rest and activity
-PreHTN stage: mod lifestyle, exercise, limit sodium and alcohol intake, stop smoking, weight reduction (wich will also help dex DM onset and hyperlipidemia)
-Stage 1 HTN: diuretics, vasodilators, B-blockers, ACE inhibitors, etc.
-Stage 2 HTN: use of 2 or more drug combinations
Cerebrovascular disease
-CVA is defined as a transient ischemic attack, if sxs resolve completely in 24 hours
-Patients with TIA have a higher chance of CVA in 90 days, with many CVAs occurring within the next 2 days following TIA
peripheral arterial disease (PAD)
-clot forms in vessels of the extremities, usually the LE’s, and gets stuck in the vessel wall (aneurysm). If the vessel breaks, hemorrhage occurs.
-Occlusions may break off and get lodged into smaller vessels distally, causing ischemia to the tissue of the extremity beyond the occlusion
-Complete obstruction to the tissue will cause necrosis and possibly the loss of the limb
Exercise and PAD
-individuals with PAD are unable to produce the normal increases peripheral blood flow essential for enhanced oxygen supply to exercising muscles (inadequate O2 supply causes ischemia, which then causes lactic acid to build which accumulates in the muscle causing extreme pain, “intermittent claudication”
-catch 22: patients with intermittent claudication have extreme paun with exercise (walking)
→causes patient to not want to exercise due to increased pain
-Exercising will help increase blood flow to the LEs, thus reducing the progression of PAD
PAD subjective grading
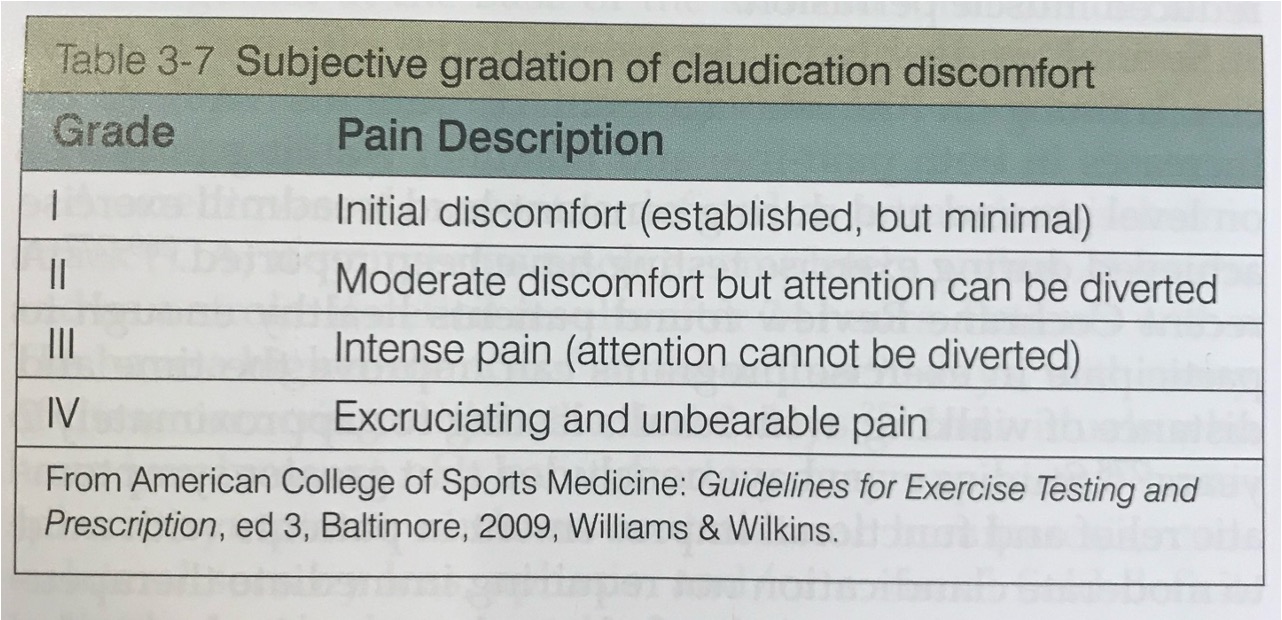
PT guidelines with PAD subjective grading
I: Okay to increase intensity
II: keep going, maintain current intensity
III:decrease intensity or stop and rest
IV: definitely stop and rest
Exercise recommendations for pts with PAD
-perform exercise intervals of 1-5 minutes, alternating with rest
-increase the length of exercise and decrease the length of rest over time (most convenient and functional mode of exercise is waking)
-longer warm-up required in colder environments bc of peripheral vasoconstriction
-sensory exam should be performed prior to any exercise rx given, due to possibility of peripheral neuropathy (monofilament testing)
-footwear and foot hygiene should be emphasized, especially for those with known peripheral neuropathy
venous insufficiency
-walls of veins are thinner and less rigid than that of artery walls
-one-way valves become outstretched, losing function (muscle action acts as a pump to also assist venous flow back to the heart)
-sxs include dull aches, heaviness, swelling, cramping, itching, tingling
-result is venous pooling
-chronic venous pooling leads to venous insufficiency
Chronic venous insufficiency leads to
-skin changes
→hemosiderin staining: RBC leak out of the veins into surrounding tissue. when the RBC break down, iron leaks into the area leaving a rust brown pigment
-venous wounds
→larger than arterial wounds, red in color, irregular borders, moderate to severe exudate, usually seen in the lower 1/3 leg
Venous thromboletic disease
-Virchow’s triad: one or more of three main categories thought to cause a VTE
→hyper coagulability: certain CA’s, hormonal therapy, inherited clotting disorders (factor 5 Leiden mutations)
→Venous stasis: blood flow at a rest (travel, paralysis, bed rest)
→Endothelial injury: surgery, trauma
VTE: Signs of PE
-SOB, pleural chest pain, decrease O2 satuiration, tachycardia
-Dx: V/Q scan, CXR, CT of chest, MRI of chest
VTE: Signs of DVT
-ipsilateral swelling, palpable cord/knot, redness, increased warmth to touch
-Dx: Homans sign (bad), Wells (use in clinic), venous doppler U/S
Padua prediction score for VTE
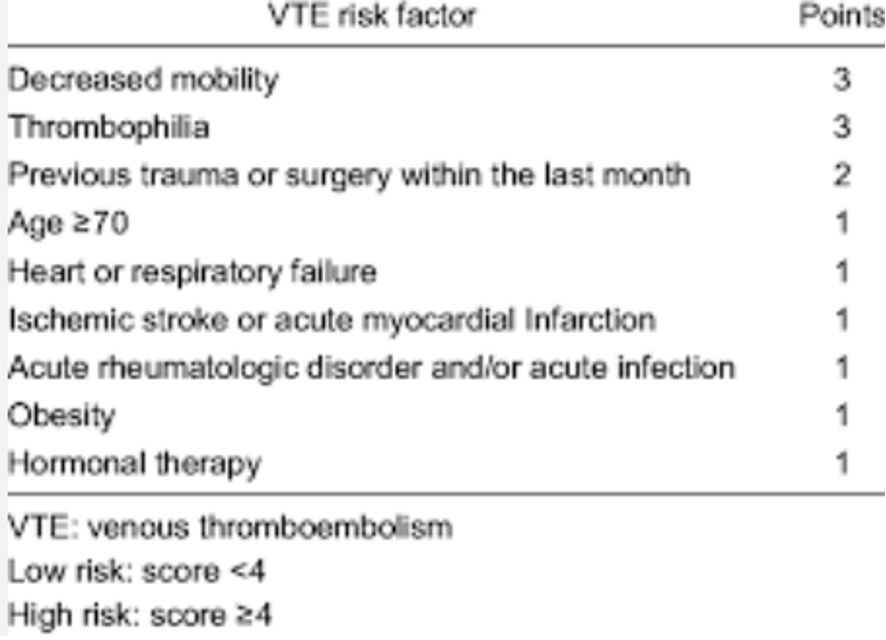
Padua prediction score for VTE facts
-standardized tool used to assess the risk for VTW
-11 Q’s
-Scores of 4 or more are considered high
-Scores less than 4 are considered low risk
-Wells’ clinical prediction rule is for LE DVT
Post thrombotic syndrome
-permanent damage to the valves of the veins and reflux of blood in the venous system
-causes venous HTN
-risk factors for developing
→inc age, inc BMI, thrombophilia, recurrent DVT events
-S&S
→chronic aching pain, intractable edema, limb heaviness, leg ulcers
Renal artery disease
-renal artery stenosis results from atherosclerosis of renal artery. it is associated with increased cardiovascular events and mortality
-if a pt has severe kidney failure and RAD and receiving dialysis tx: 56% 2 yr survival rate; 18% 5 yr survival rate; 5% 10 yr survival rate A
Aortic aneurysm
-aorta is the largest artery in the body: divided into thoracic and abdominal (diaphragm boundary)
-an aneurysm in the aortic wall is described as being 50% greater than that of normal size (>3 cm is considered aneurysmal in adults)
-AAA
→infrarenal aneurysms: most common. formed below the renal arteries
-suprarenal aneurysms: uncommon. formed between the levels of the diaphragm and renal arteries
-can be unilateral (sacclular aneurysm) or bilateral (fusiform aneurysm)
AAA S&S
-pulsating mass in abdoment
-bruit heard over swollen area in abdomen
-abdominal, back or flank pain
Special considerationf for cardiac rehab for pts with CVD
-submax exercise is performed by PT,s. very rarely do PTs perform maximal exercise testing
→submax exercise testing shoulder never exceed 6 METS
→MET is a ratio of your working metabolic rate relative to your resting metabolic rate. it’s one way to describe the intensity of an exercise or any activity
-Pts CVD
→HR max=220-age
→Target HR [(220-age) x 0.6] to [(220-age)x0.8]
-Gold standard (pts c CVD) = use sxs limited max HR from exercise tesing, multiply by 60-80%
→pts max HR was 158 bpm during exercise testing
-?[t HR range for CR = 158×0.6 - 158×0.8 (94.8-126.4)
Hemodynamic stability guidelines: interventions for patients
-HR 60-100 bpm
-SBP >80mmHg and <180mmHg
-DBP <110mmHg
-MAP 70-110 mmHg
-SPO2 >90%
-RR 12-18rpm
It is common for PTs to work with patients outside these parameters, especially the ICU patients who have complex cardiovascular and pulmonary dx; close communication with medical team and documentation key when working with pts outside these parameters