Comprehensive Respiratory System: Functions, Anatomy, and Gas Exchange
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
What are the primary functions of the respiratory system?
Gas exchange, movement of air, protection of respiratory surfaces, production of sound, and detection of olfactory stimuli.
What is external respiration?
The exchange of O2 and CO2 between the interstitial fluid of the body and the external environment.
What are the three main processes involved in external respiration?
Pulmonary ventilation, gas diffusion, and transportation of gases.
What occurs during pulmonary ventilation?
The physical movement of air in and out of the lungs.
What is gas diffusion in the context of respiration?
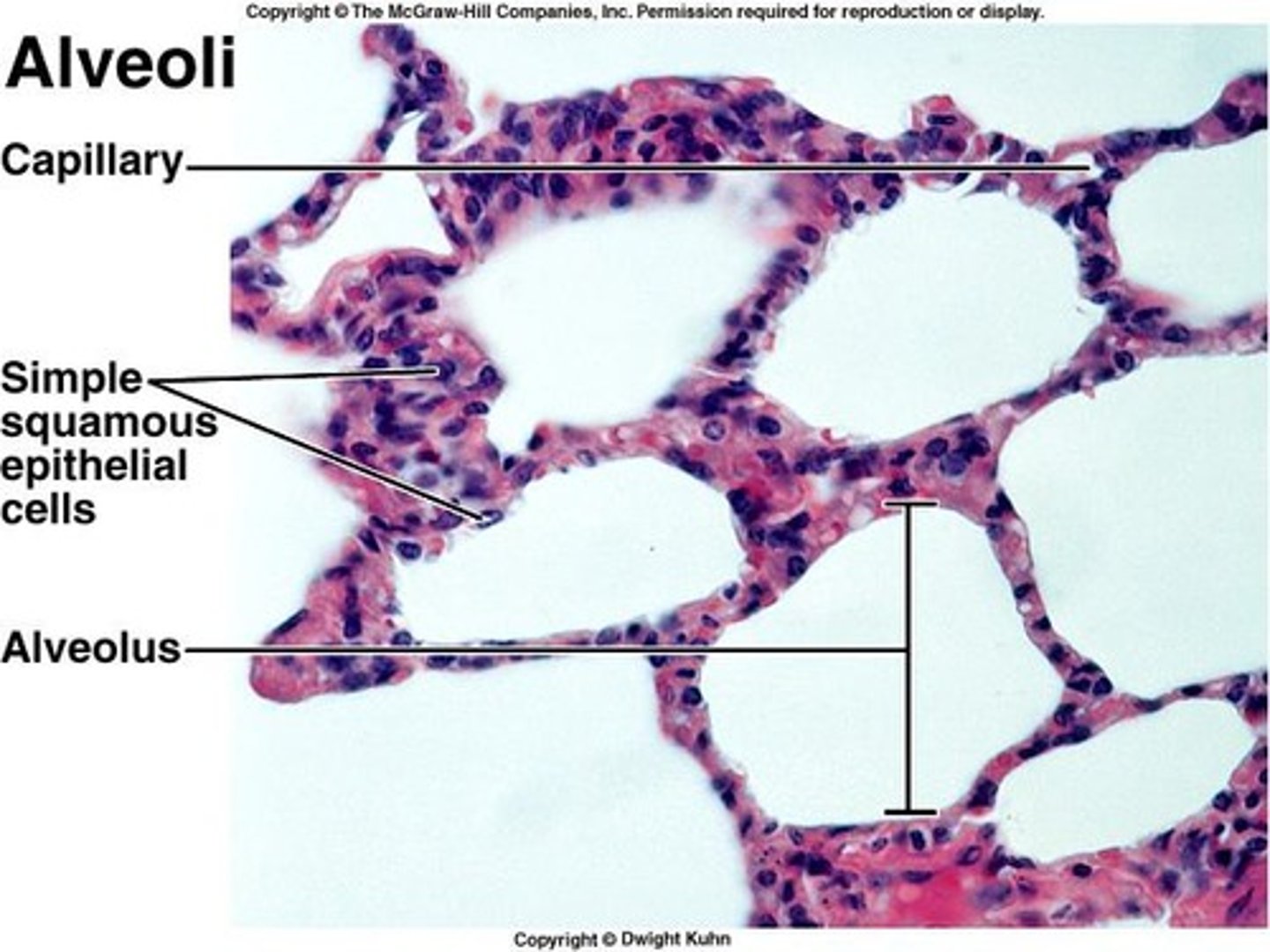
The exchange of gases across the pulmonary membranes between the alveoli and alveolar capillaries.
What is internal respiration?
The absorption of O2 and release of CO2 by the cells.
Why is respiration at the alveolar membrane considered efficient?
Due to differences in partial pressures, small distances for gas exchange, lipid solubility of gases, large surface area of alveoli, and coordinated blood and air flow.
What happens to the diaphragm during inhalation?
It contracts and flattens, increasing the volume of the thoracic cavity and decreasing pressure.
What is the respiratory cycle?
A cycle of one breath in and one breath out.
How does the rib cage contribute to breathing?
Its upward movement increases depth and width, thus increasing thoracic volume.
What is the normal respiratory rate for adults?
12-18 breaths per minute.
What is minute respiration volume?
The amount of air that moves in and out of the lungs in one minute, calculated by multiplying tidal volume (TV) by respiratory rate (RR).
What is alveolar ventilation?
The amount of air that reaches the alveoli per minute.
Why is alveolar ventilation more important than minute respiration volume?
It indicates the rate of delivery of oxygen to the alveoli.
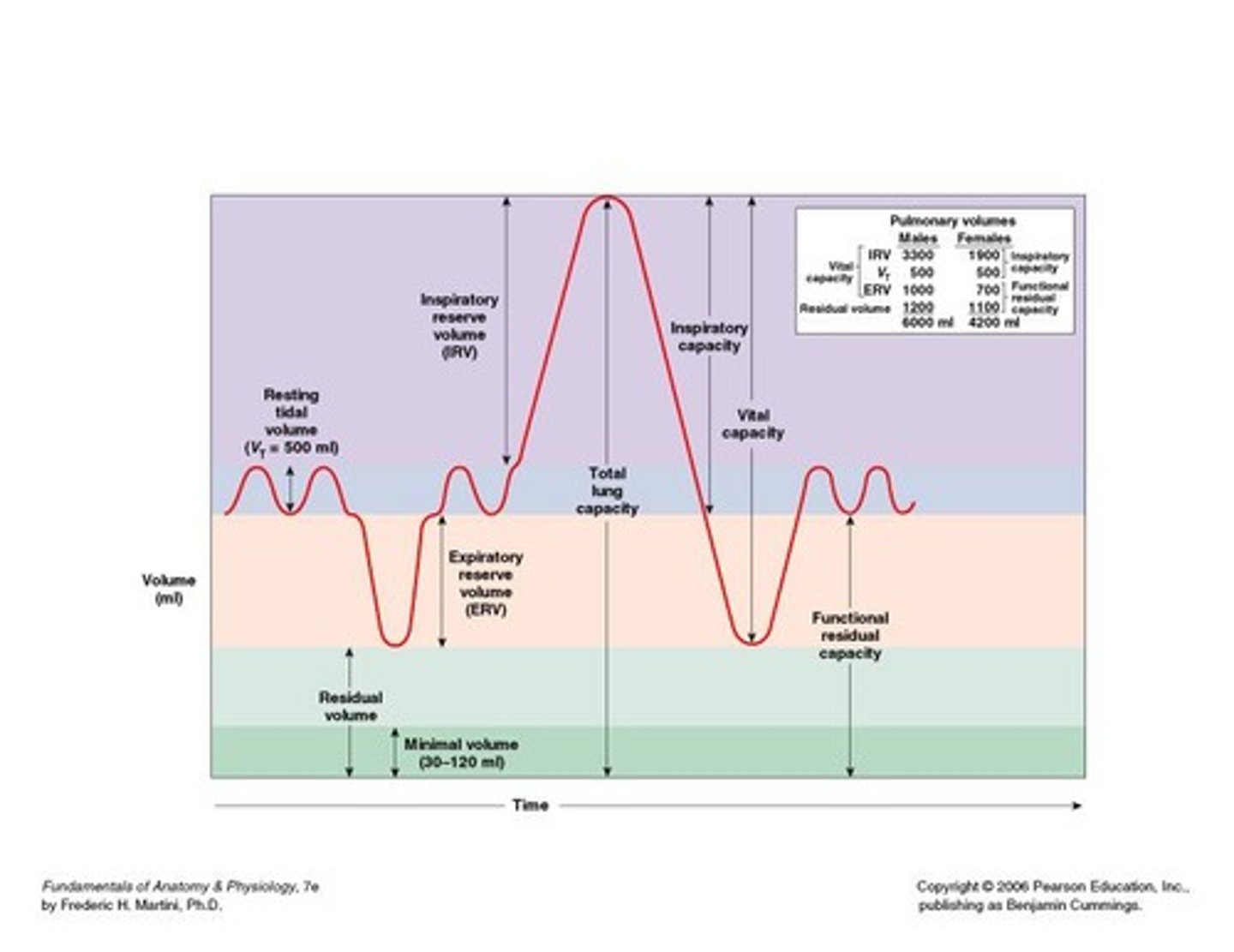
What is tidal volume (TV)?
The amount of air that moves in or out of the lungs in a single, restful respiratory cycle (approximately 500 ml).
What is expiratory reserve volume (ERV)?
The amount of air you can forcefully exhale after a quiet respiratory cycle (approximately 1000 ml for males and 700 ml for females).
What is residual volume (RV)?
The amount of air that remains in the lungs at all times (approximately 1,200 ml for males and 1,100 ml for females).
What is minimal volume (MV)?
The amount of residual volume that cannot be measured but is believed to remain in the lungs even after collapse (30 to 120 ml).
What instrument is used to measure lung volumes and capacities?
A spirometer.
What is the significance of anatomic dead space in alveolar ventilation?
It is the volume of air in the conducting pathways that does not reach the alveoli.
What happens to thoracic cavity volume during expiration?
It decreases as the diaphragm relaxes, increasing pressure and forcing air out.
What is the relationship between respiratory rate and tidal volume in minute respiration volume?
Minute respiration volume is calculated by multiplying respiratory rate (RR) by tidal volume (TV).
What occurs when the pressure inside the lungs is less than atmospheric pressure?
Air enters the respiratory passages.
What is Inspiratory Reserve Volume (IRV)?
The amount of air that can be forcefully inhaled over and above Tidal Volume (approximately 3,300 ml for males and 1,900 ml for females).
How is Inspiratory Capacity calculated?
Inspiratory Capacity = Tidal Volume (TV) + Inspiratory Reserve Volume (IRV).
What is Functional Residual Capacity (FRC)?
The amount of air left in the lungs after a quiet respiratory cycle, calculated as Expiratory Reserve Volume (ERV) + Residual Volume (RV).
Define Vital Capacity (VC).
The maximum amount of air that can be moved into and out of the lungs in a single respiratory cycle, calculated as ERV + IRV + TV (approximately 4,800 ml for males and 3,400 ml for females).
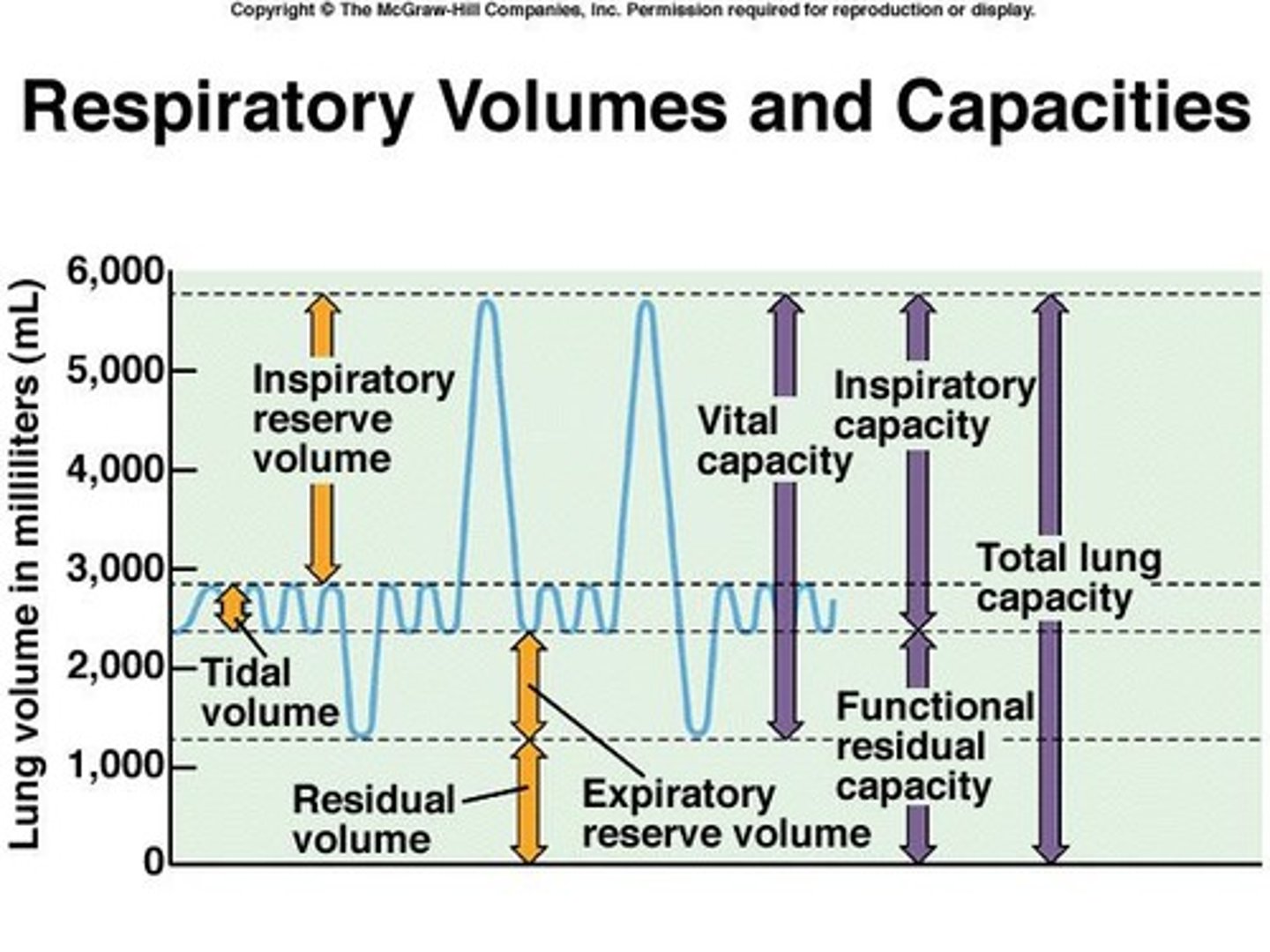
What is Total Lung Capacity?
The total volume of the lungs, calculated as Vital Capacity (VC) + Residual Volume (RV) (approximately 6,000 ml for men and 4,200 ml for women).
What are the functions of the respiratory system?
To facilitate gas exchange, regulate blood pH, and provide oxygen to the body while removing carbon dioxide.
Define pulmonary ventilation.
The movement of air into and out of the lungs.
What is gas diffusion?
The process by which gases move from areas of higher partial pressure to areas of lower partial pressure.
Why is respiration at the alveoli efficient?
Due to the large surface area and thin walls of the alveoli, which facilitate rapid gas exchange.
What happens to the diaphragm when it is at rest?
It is dome-shaped, creating a lower volume in the thoracic cavity.
What happens to the diaphragm when it is contracted?
It flattens, increasing the volume of the thoracic cavity and decreasing pressure, allowing air to flow in.
Define respiratory rate.
The number of breaths taken per minute.
What is Intrapulmonary Pressure?
The pressure in the respiratory tract at the alveoli, which decreases during inhalation and increases during exhalation.
What is Intrapleural Pressure?
The pressure in the space between the parietal and visceral pleura, averaging -4 mm Hg.
What is Boyle's Law?
For a fixed volume of gas, as the volume of a sealed container increases, the gas pressure decreases; pressure and volume are inversely proportional.
What is Dalton's Law?
In a mixture of gases, each gas contributes to the total pressure in proportion to its abundance.
What is Henry's Law?
At a given temperature, the amount of a particular gas in solution is directly proportional to its partial pressure.
What happens to the partial pressure of gases in the alveoli?
Blood in the pulmonary arteries has high PCO2 and low PO2; gas exchange occurs, resulting in blood leaving the lungs with a PO2 of about 100 mm Hg and a PCO2 of about 40 mm Hg.
What is the significance of the respiratory pump?
Cyclical changes in intrapleural pressure during inhalation and exhalation assist in venous return to the heart.
What does Henry's Law state about gas solubility?
Solubility of certain gases differs in different solutions.
Which gas has high solubility in body fluids?
Carbon dioxide (CO2) has high solubility, while nitrogen has very little.
How is dissolved gas content reported in solutions?
Dissolved gas content is reported as mL of gas/dL of solution.
What are the partial pressures of carbon dioxide, oxygen, and nitrogen in plasma?
CO2: 40 mm Hg, O2: 100 mm Hg, N2: 573 mm Hg.
What is the carbon dioxide content in the plasma of blood in the pulmonary vein?
About 2.62 mL/dL.
What is hemoglobin saturation?
The percentage of heme units (4 per Hb molecule) attached to oxygen at a given moment.
What happens to hemoglobin saturation when PO2 increases?
More oxygen binds to hemoglobin, increasing saturation.
What is the normal blood pH range?
7.35 - 7.45.
What effect does a decrease in pH have on hemoglobin?
Hemoglobin changes shape, releases more O2, and saturation decreases (Bohr Effect).
What is the role of carbonic anhydrase in CO2 transport?
It catalyzes the reaction CO2 + H2O ⇌ H2CO3 ⇌ H+ + HCO3-.
What is the chloride shift?
HCO3- moves into plasma and is exchanged for Cl-.
What is the primary function of the respiratory bronchioles?
Gas exchange begins here.
What are the two main types of lung diseases?
Restrictive lung disease and obstructive lung disease.
What characterizes restrictive lung disease?
Decreased lung compliance, increased effort to expand lungs, and hypoxemia.
What is atelectasis?
Collapse of the lung.
What is the primary characteristic of obstructive lung disease?
Airway obstruction that is worse on expiration.
What is chronic bronchitis?
Excessive mucus production with a chronic cough lasting at least 3 months for 2 consecutive years.
What is emphysema?
Abnormal, persistent enlargement of gas exchange airways with loss of elasticity.
What is the function of the epiglottis?
Diverts food into the esophagus and prevents it from entering the trachea.
What is the glottis?
The triangular slit between the vocal cords.
What is the role of goblet cells in the respiratory system?
They produce mucus to trap foreign particles and pathogens.
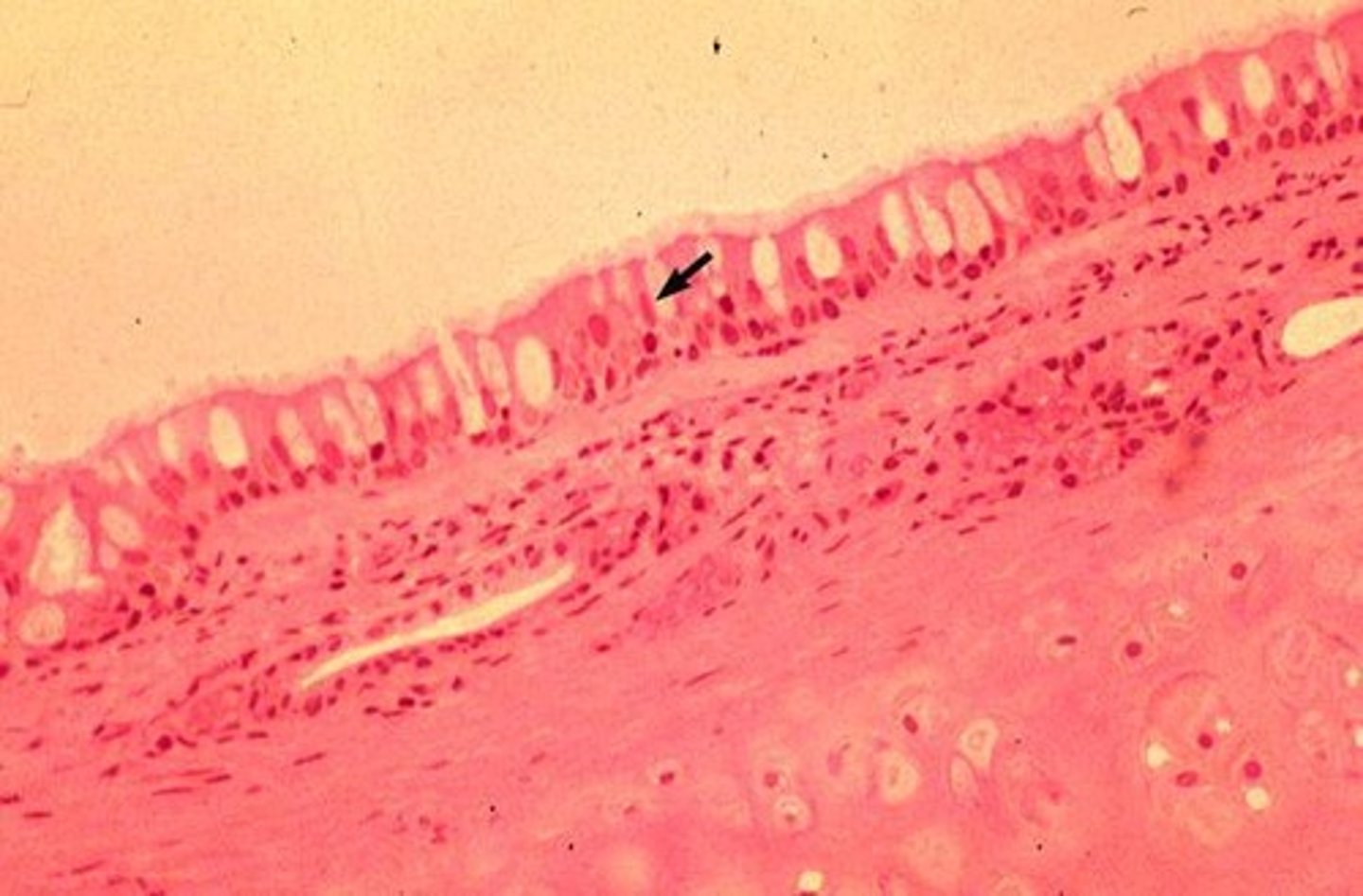
What is the mucus escalator?
Cilia sweep mucus toward the pharynx or esophagus to be expectorated or swallowed.
What is the primary source of ACE (angiotensin-converting enzyme)?
Alveolar capillaries.
What happens during hypercapnia?
Increased CO2 levels lead to increased respiratory rate and depth.
What is the function of type I pneumocytes?
They cover the majority of the alveoli and are the sites of gas exchange.
What is the function of type II pneumocytes?
They produce surfactant, which reduces surface tension in the lungs.
What is the cardiac notch?
A space in the left lung that accommodates the heart.
What is the primary function of the alveoli?
Gas exchange occurs via alveolar capillaries.
What is the role of surfactant in the lungs?
It lubricates the alveoli and prevents them from collapsing.
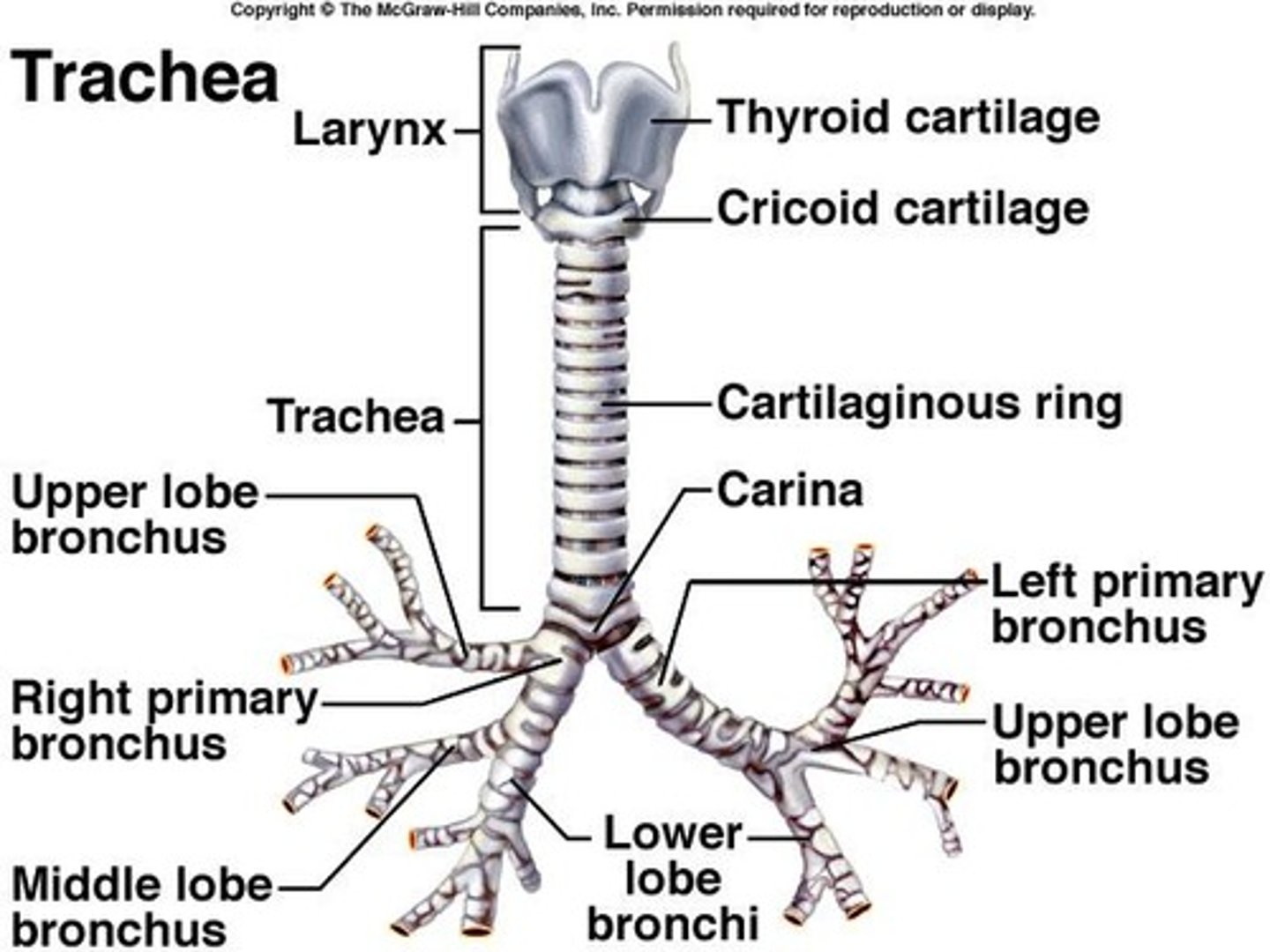
What is the structure of the trachea?
A cylindrical tube lined with pseudostratified columnar epithelium and incomplete rings of hyaline cartilage.
What are the three parts of the pharynx?
Nasopharynx, oropharynx, laryngopharynx.
What is the function of the larynx?
It prevents foreign objects from entering the trachea and houses the vocal cords.
What is the primary function of the respiratory defense system?
To filter, warm, and humidify air before it reaches the alveoli.
What is the significance of the pleural cavity?
It contains serous fluid that decreases friction and holds the pleural membranes together.
What is the role of alveolar macrophages?
They attack particles trapped in the liquid covering the alveoli.
What happens when temperature increases in relation to hemoglobin?
Hemoglobin releases more oxygen in response to increased metabolism.
What is the effect of increased 2-3 BPG in red blood cells?
It leads to the release of oxygen by hemoglobin.
What is the relationship between exercise and hemoglobin's oxygen release?
Increased exercise raises temperature and BPG levels, facilitating oxygen delivery to tissues.
What is the main difference between fetal hemoglobin and adult hemoglobin?
Fetal hemoglobin has a higher affinity for oxygen than adult hemoglobin.