Depressive Disorders (Chapter 14)
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
88 Terms
What is the diagnostic criteria for major depressive disorder?
History of one or more major depressive episodes
No history of manic or hypomanic episodes
Symptoms interfere with social or occupational functioning
May include psychotic features
What is the significance on major depressive disorder diagnosis requirements?
Patients must have one or more major depressive episodes → This can be difficult for patients! They have to go through this several times before they can get on medication
What are the subtypes of major depressive subtypes?
Psychotic features
Melancholic features: sad, somber
Atypical features: don’t act themselves
Catatonic features: staring blankly like a zombie
Postpartum onset:
Seasonal features (seasonal affective disorder (SAD)): prominent in Alaska because of light!)
Proposed subtypes of major depressive disorder
Premenstrual dysphoric disorder
Mixed anxiety depression
Recurrent brief depression
Minor depression
Dysthymic disorder
Chronic depressive syndrome
Present for most of the day
More days than not
At least present for 2 years
Epidemiology of depression
Leading cause of disability in the United States and around the world
Children and adolescents
Older adults (mainly due to isolation, can’t do what they used to)
Comorbidity
Etiology of major depressive disorder
Biological factors
Genetic (runs in the family like most other mental illnesses)
Biochemical: alterations in hormonal regulation (Diathesis stress model)
Psychological factors
Cognitive theory
Learned helplessness
Nursing process: assessment
Self-assessment:
Unrealistic expectations of self: feeling what the patient is feeling
Assess suicide potential (usually take anger or negative feelings and bring it inward to self, so not as often a homicidal risk)
Other areas to assess
Thought process
Mood
Feelings
Physical behavior
Communication
Religious beliefs and spirituality
Which question would be a priority when assessing for symptoms of major depression?
a. Tell me about any special powers you believe you have
b. You look really sad. Have you ever thought of harming yourself?
c. Your family says you never stop. How much sleep do you get?
d. Do you ever find that you don’t remember where you’ve been or what you’ve done?
B: Suicide risk is a critical concern in depression assessment:
Asking about suicidal thoughts is essential to identify potential self-harm behaviors and provide necessary support.
What is always the highest priority for the nursing assessment of someone with depression?
Risk for suicide! Safety is always the highest priority.
3 phases of treatment:
Acute phase (6-12 weeks)
Continuation phase (4-9 months), when meds start to work
Maintenance phase (1 year or more), starting to see positive results
Basic level interventions
Counseling and communication
Health teaching and health promotion
Promotion of self-care activities
Milieu therapy
What is the BEST kind of therapy for depression?
Cognitive behavioral therapy
The therapist educates the patient to become their OWN therapis and work through their problems
What is the second-best kind of therapy for depression?
Group therapy
The patient identifies good and bad coping mechanisms and can relate to the other group members
Advanced practice interventions
Psychotherapy:
Cognitive behavioral therapy (CBT)
Interpersonal therapy (IT)
Time-limited focused psychotherapy
Behavior therapy
Group therapy
What kind of antidepressants are the first-line therapy for depression?
Selective Serotonin Reuptake Inhibitors (SSRI)
Indications
Adverse reactions
Potential toxic effects
Sometimes the best to use in conjunction with drugs like Abilify, which is normally for Schizophrenia; very small amount with SSRI will enhance the SSRi and will get better relief!
Tricyclic antidepressants (TCAs)
Neurotransmitter effects
Indications:
Adverse effects:
Contraindications:
Monoamine oxidase inhibitors
Neurotransmitter effects:
Indications:
Adverse/toxic effects:
Interactions:
Drugs
Food: smoked cheese, smoked salmon, smoked meats, avocado
Contraindications:
Can lead to serotonin syndrome → seizures!!
What are some of the other treatments for depression?
Electroconvulsive therapy (ECT) - only do this if NOTHING ELSE WORKS!!! AFFECTS THE HEART
Transcranial magnetic stimulation
Light therapy
St. John’s Wort
Exercise- THE BEST! 🙂 Release endorphins!
Disruptive mood dysregulation disorder
Symptoms of constant and severe irritability and anger
Diagnosis made between the ages of 6 and 18 with onset before age 10
Must exhibit symptoms in at least 2 of the following settings: home, school, and with peers:
More common in males than females
More common in children
If symptoms resemble major depressive disorder, antidepressants can be used
If manic episode occurs, bipolar disorder may be a possibility
CBT is essential
Persistent Depressive Disorder (Dysthymia)
Low-level depression occurs most of the day for the majority of days
Last at least 2 years in adults and 1 year in children and adolescents
Depressed mood with 2 of the following:
decreased appetite or overeating
Insomnia or hypersomnia
Low energy
Poor self esteem
Difficulty thinking
Hopelessness
Not severe enough to require hospitalization
“Always felt this way” and depression seems like nromal functioning
Early onset and chronic illness
More common in women
Common to go undiagnosed
Similar to major depressive disorder
Psychotherapy (CBT), antidepressants (SSRIs, SNRIs, TCAs)
Premenstrual dysphoric disorder
Cluster of symptoms that occur in the last week before the onset of a woman’s period
Severe enough symptoms to interfere with the ability to work or interact with others
S/s: mood swings, irritability, depression, anxiety, feeling overwhelmed, difficulty concentrating, lack of energy, overeating, bloating, weight gain, etc
Symptoms decrease with the onset of menstruation
Substance/medication-induced depressive disorder
Result of prolonged use of or withdrawal from drugs and alcohol
Depressive symptoms last longer than the length of physiological effects
Symptoms appear within one month of use
Once the substance is removed, depressive symptoms remit within a few days to several weeks
Depressive disorder due to another medical condition
Depression may be caused by another medical condition
May affect the body’s system or from long-term illness that causes ongoing pain
Cushings disease
Hypothyroidism
HIV
Arthritis
Back pain
Metabolic conditions
Diabetes
What is one of the most common psychiatric disorders?
Major Depressive Disorder
17 million adults in US (7% of the population)
Characterized by persistently depressed mood lasting for a minimum of two weeks
Length of a depressive episode maybe 5 to 6 months
May be chronic >2 years
Recurring episodes
Depression and the seasons (SAD)
Same diagnosis as major depressive disorder but with the addition of a seasonal pattern
2 seasonal depressive episodes during the same time period
Symptoms: hypersomnia, overeating, weight gain, and carbohydrates
More common in women 18-30 years old
Populations farthest from the equator most affect
What is bereavement exclusion
Clinicians were once advised against diagnosing a person with depression in the first two months following a signficant loss = bereavement exclusion
Normal mourning could be labeled pathological
A psychiatric diagnosis could result in a lifelong label
Unnecessary medications might be described
HOWEVER, things have changed and now someone can receive medication given in the first 2 months following the death of a loved one or other loss
What is the leading cause of disability worldwide?
Depression
More common in females
Most common in young adults (18-25)
Having two or more races or being white = higher rates of depression
7% of US adults
Psuedodementia
Psychomotor and cognitive slowing of depression may resemble a neurocognitive disorder, such as Alzheimer disease
Depressive syndromes frequently accompanies other psychiatric problems such as:
Schizophrenia
Substance use
Eating disorders
Borderline personality
Schizoaffective disorder
Combination of depression and anxiety is one of the most common psychiatric presentation
Risk factors for depression
Combination of biological, psychological, and cultural variables
Unlikely that there is a single cause of depression
female gender
ACEs
Stressful life events
first-degree family members with major depressive disorder
Neuroticism (negative personality trait)
Substance use, anxiety, personality disorders
Chronic medical conditions
Biological factors for depression
Genetic
Identical twins have a 50% chance of depression of the other has it
Multiple genes involved
Biochemical
CNS neurotransmitter abnormalites as result of genetic or enviroenmtnal factors, or other meci al condiiotns (cerebral infaraction, Parkinsons, hypothyroidism, AIDs, or drug use)
Serotonin and o
What main 2 neurotransmitters are responsible for mood?
Serotonin: a regulator of sleep, appetite, and libido (if deficient, can lead to low appetite, low sex drive, poor impulse control and irritability)
Norepinephrine: modulates attention and behavior, and is stimulated by stressful situations which may result in overuse and deficiency, which can cause apathy, reduced responsiveness, or slowed psychomotor activity
Depression may result from other dysregulations, such as glutamate and GABA. Stressful life events also can trigger depression, as it affects neurotransmitters like norepinephrine, serotonin and acetylcholine!
How do hormones affect depression?
Neurotransmitters and hormones have the same receptors and pathways in the mood area of the brain
People with depression have increased cortisol levels and elevated corticotropin-releasing hormone
Estradiol (form of estrogen) affects receptors sensitive to serotonin in the areas of the brain a
How does inflammation affect depression?
Inflammation may be the result of psychological injury as well
In young females with a history of adversity depression is accompanied by elevations in C-reactive protein and interleukin-6
Many people with major depression have elevated inflammatory biomarkers in the absence of physical illness
What is the diathesis stress model?
Considers the interplay between genetic and biological predisposition toward depression and life events
Physiological vulnerabilities, such as genetic and biological predisposition, biochemical makeup, and personality structure are all referred to as diathesis
The stress part refers of the life events that impact the individual’s vulnerabilities
Biochemically, psychosocial stressors and interpersonal events trigger neurophysical and neurochemical changes in the brain
Early trauma may lead to neuronal loss and lead to exaggerated stress responses
What is the cognitive theory?
The underlying assumption that a person’s thoughts will result in emotions
If someone looks at life in a positive way, they will experience positive emotions and vice versa
People may acquire a psychological predisposition to depression due to early life experiences, which contribute to negative, illogical and irrational thought process that are activated during times of stress
How do we screen for depression?
Beck Depression inventory
Hamilton Depression Scale
Geriatric Depression Scale
Patient Health Questionnaire
What is the most dangerous aspect of major depressive disorder? What should you ask the patient?
Preoccupation with death
Negativistic thoughts are referred to as suicidal ideation
May be mild and fleeting or persistent and involve a plan
Always evaluate for suicidal ideation
You said you are depressed. Tell me what that is like for you.
When you feel depressed, what sort of thoughts do you have?
Have you had thoughts of ending your life? Do you have any plans? Do you have the means to carry out your plan?
What are the key symptoms in depression
Depressed mood
Anhedonia (inability to feel pleasure)
Anxiety
Exaggeraton on percived faults anf ailures
Unable to recognize strengths and successes
Delusions congruent with negative mood
Feeling sof worthlessenss, hoplessness, guilt, anger, and helpenessess
Describe the relationship between pain and depression.
Depression and chronic pain are often seen together in primary care
Neurotransmitters and nerve pathways are shared
Acts in a vicious cycle
Two-way Interaction between pain and depression
Nursing assessment: Appearance
Poor grooming
Poor hygiene
Do not take pride in appearance
No eye contact
slumped or hunched, low head, and shoulders forward
Nursing assessment: Behavior
Anergia: abnormal lack of energy
Psychomotor agitation: pacing, nail biting, finger tapping
Vegetative signs of depression: alterations in activities necessary to support physical life and growth (eating, elimination, sleeping, and sex)
Sleep pattern disturbance is hallmark sign of depression (insomnia or hypersomnia)
Nursing assessment: Mood
Mood = general emotional state
Depressed mood evident for weeks
Nursing assessment: Feelings and emotions
Emotions/feelings = related to and flow from mod, more specific and can come and go quickly
Worthlessness
Guilt
Helplessness
Hopelessness
Anger
Suicidality
Anger and irritability (usually directed inward as self-destructive behaviors)
Anhedonia: inability to feel pleasure or happiness, disinterest in interaction with others resulting in insolation
Nursing assessment: Affect
Affect = outward representation of a person’s internal state and is objective finding based on the nurse’s assessment
Constricted affect (reduction in the range and intensity of normal expression)
Blunted (or shallow) affect is more severe and represents significant decrease in emotional reactivity
Flat affect is no or nearly no emotional expression or reactivity
Nursing assessment: Speech
Slow and softly
Monotone
Lack of spontaneity
Nursing assessment: Thought processes
Slow thinking
Poverty of though
Absent responses or slow responses
May be mute
Nursing assessment: Thought content and perceptions
In profound depression, psychotic features (delusions, hallucinations) may be present
May be mood congruent and focus on depressive themes
May hear critical voices
Psychosis increases the risk of suicide, self-harm and other-directed violence
Nursing assessment: Insight and judgment
Cannot problem solve
Poor judgment
Indecisiveness
Nursing assessment: Cognitive changes
Decreased ability to concentrate and decide
Deficits in short-term and working memeory
Issues with problem solving
Dysfunctions in processing speed
Dysfunction in auditory and visual processing
How do we screen older adults for depression?
Geriatric Depression Scale - uses yes and no so it is easier to answer
3 phases of implementation of treatment for depression
Acute phase - 6 to 12 weeks, reduction if depressive symptoms and restoration of psychosocial and work function, may need hospitalization and medication or other biological treatments
Continuation phase: 4 to 9 months, directed at prevention of relapse through meds, education, and psychotherapy
Maintenance phase: 1 year plus, directed at prevention of further episodes
What is important to remember about conversing with patients with depression?
Silence is a good thing! Just sitting with them can be helpful
What is the prefrontal cortex responsible for?
Regulates role in executive functions and emotional control and memory
What is the limbic system responsible for?
Regulates activities such as emotions, physical and sexual drives, the stress response, and learning and memory
What is the anterior cingulate cortex responsible for?
Regulates heart rate and blood pressure, decision making, emotional regulation, error detection, preparation for tasks and executive functions
Imbalance of ______ contribute to depression
Neurotransmitters like serotonin and norepinephrine
What medications are used to treat depression?
Selective reuptake inhibitors (SSRIs)
Serotonin reuptake inhbitors (SNRIs)
Serotonin antagonists and reputake inhibitors (SARIs)
Norepinephrine dopamine reupake inhibitor (NDRI)
Noradrenergic and specific sertotonergic antidepresants (NaSSAs)
Ticyclic antepressants (TCAs)
Monamine oxidase inhibitors (MAOIs)
What do antidepressants help treat
Positively impact poor self-concept, social withdrawal, vegetative signs of depression, and activity level
Sleep disturbance
Appetite disturbance
Fatigue
Decreased sex drive
Psychomotor retardation or agitation
Impaired concentration
Anhedonism
What is the drawback to antidepressant drugs? What can we do if someone is acutely suicidal?
Improvements may take 1 to 3 weeks or longer → electroconvulsive therapy
May precipitate psychotic episode in a person with schizophrenia or manic episode with a patient with bipolar
How do SSRIs work?
Block the neuronal uptake of serotonin to increase the availability of serotonin in the synaptic cleft
SSRI side effects
Low side-effect profile compared to other antidepressants
Do not create anticholinergic effects, dry mouth, blurred viosn or urinary retention.
BUT they mat cause:
agitation
Anxiety
Sleeo distubrnace
Tremor
Sexual dysfunction
Tension headache
Autonomuc reactions (dry mouth, sweating, weight chance, nausea, loos bowel movements)
Indications for SSRIs
First line treatment for depression
Help with OCD and panic disorer
Can helpw tih prenmenttural dsysphric disorder and bulimia
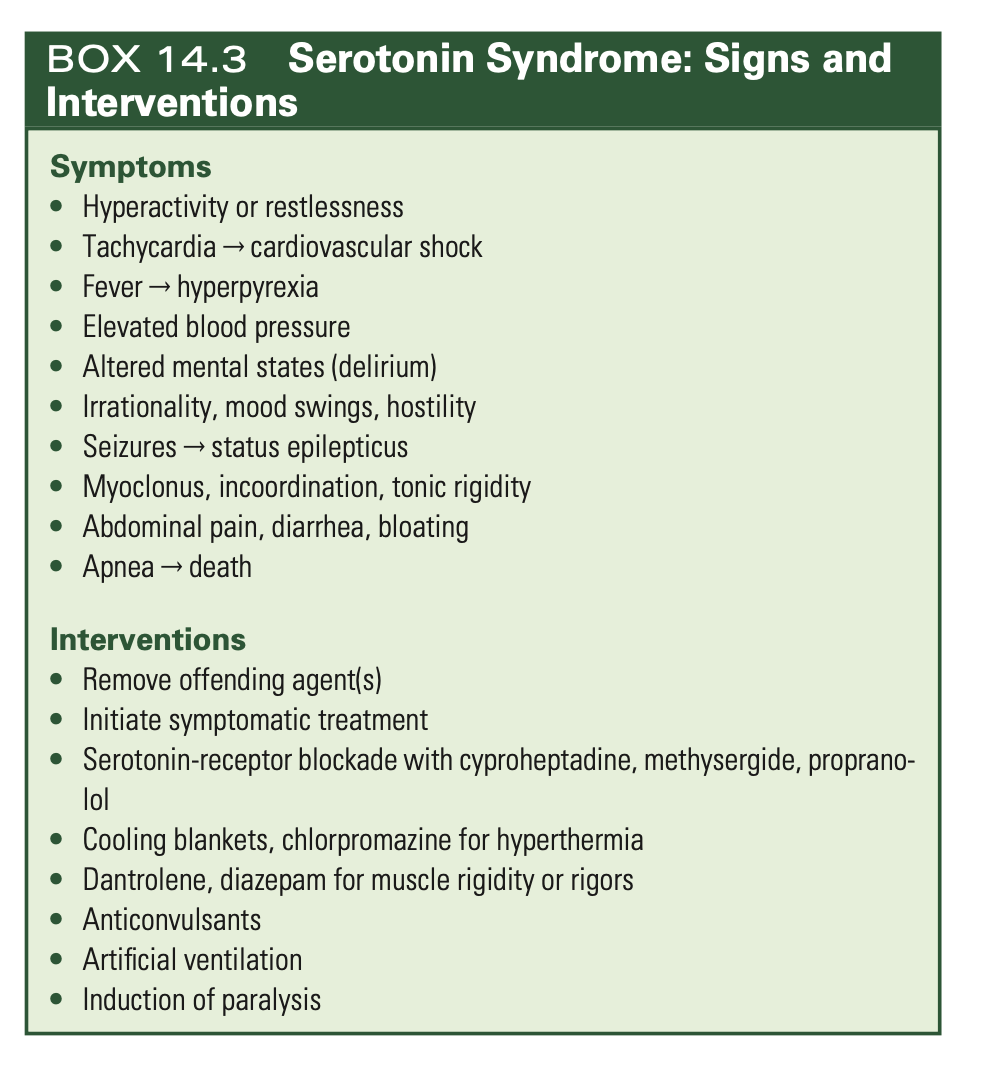
Poteitnial toxic effects of SSRIs
Serotonin syndrome
Overactivation of central serotonin receptors
Symptoms:
abdominal pain
Diarrhea
Sweating
Fever
Tachycardia
Elevated BO
Altered mental state (delirium)
Myoclonus (muscle spasm)
Increased motor activity
Irritability
Mood change
May lead to hyperpyrexia (HGIH FEVER), cardiovascular shock, DEATH
HIGHEST RISK IF administered with monoamine oxidase inhibitors (MAOI). Patient should discontinue SSRIs before starting MAOIs.
Serotonin norepinphrine inhibitors
Inibit the reuptake of serotonin and norepinephine
Similar affects of SSSRIs but not tolerated as well
May increase BP
Action of tricyclic antidepressants
Inhibit the reuptake of norpepinephrine and serotonin and parkinsonain symtoms
Followed by CNS depression
Used caustiously in suicidal patients
Tricyclic antidepressant contraindications
People who have recently had an MI, narrow-angle glaucoma, hx of seizures, pregnancy
How do monoamine oxidase inhibitors work?
Monoamine oxidase is responsible for inactivating monamine neutrotransmitters such as norepinipehrine, serotnin, dopamine and tyramine → fewer amines get inactvated → increased mood-elevating neurotrasmitters
Indications for MAOIs
Third line antidepressants
Significant drug reactions and dietary restrictirions
Common adverse reactions for MAOIs
Orthostatic hypotension
Weight gain
Edema
Change in cardiac rate and rhtyhm
Constipation
Urianry heistance
Sexual dysfunction
Vertigo
Overacitivty
Muscle twitching
Hypomanic and manic behacior
Insomnia
Weakesess
Fatigue
Toxic effects of MAOIs
Inability ti break down tyramine
At risk if people eat tyramine rich foods → risk for hypertensive crisis!!! CVA, intracranial hemorrhage, and death
MONITOR BLOOD PESSURE DURING TREATMENT AND D NOT EAT FOODS WITH TYRAMINE
Early signs of MAOI toxicity
Irritability
Anxiety
Flushing
Sweai=ting
Severe headache
Later signs of MAOI toxicity
Anxiety
restlessness
Fever
Seizures
Coma
death
Treatment for MAOI toxicity hypertensive crisis
Gastric lavage and chacoal
Treat purexia with hypothemic blankets or ice packs
Fluid therapy
Short-acting antihypertenive agent
Intravenous benzos for anxiety and agitation and seixure control
Contraindications for MAOIs
Cerebrovascular disease
Hypertension
Congestive heart failure
Liver disease
Consumption of foods containing tyramine
Certain medications
Surgery in past 10 days
Age <16
What is St. johns wort?
Flower processed into tea or tablets, increases serotonin, norepinephirne and dpamine effects on the brain resulting in antidpressant effects
Risks for ECT
Seozure
Hupertension
Congestive heart failure
Cardiac arrhythmias
Increased cerebtal oxygen, blood flow and ICP
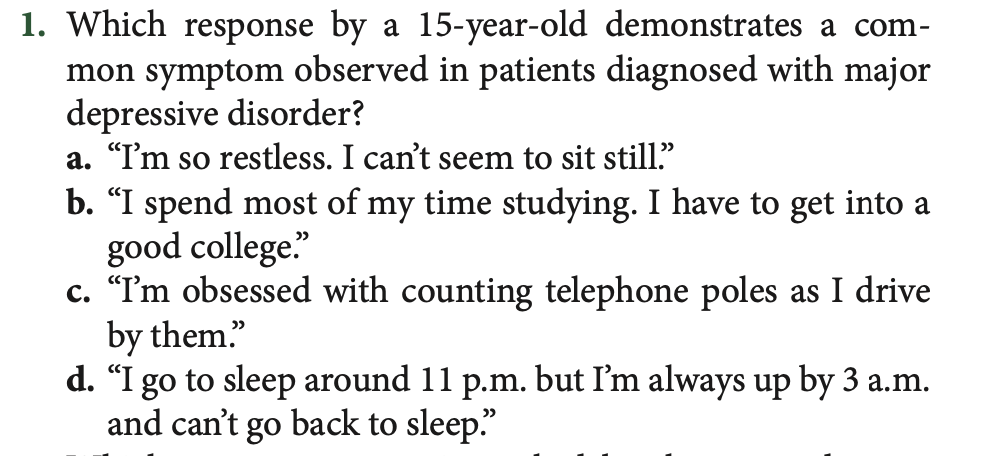
CORRECT ANSWER: D
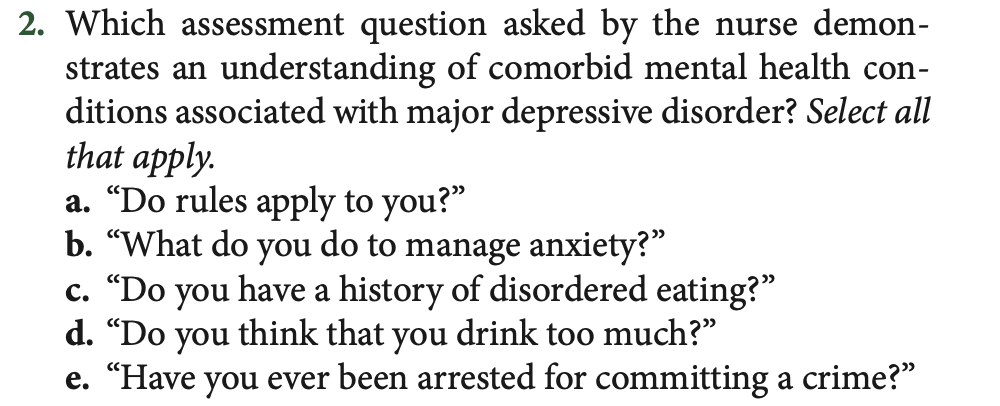
CORRECT ANSWER: B, C, D
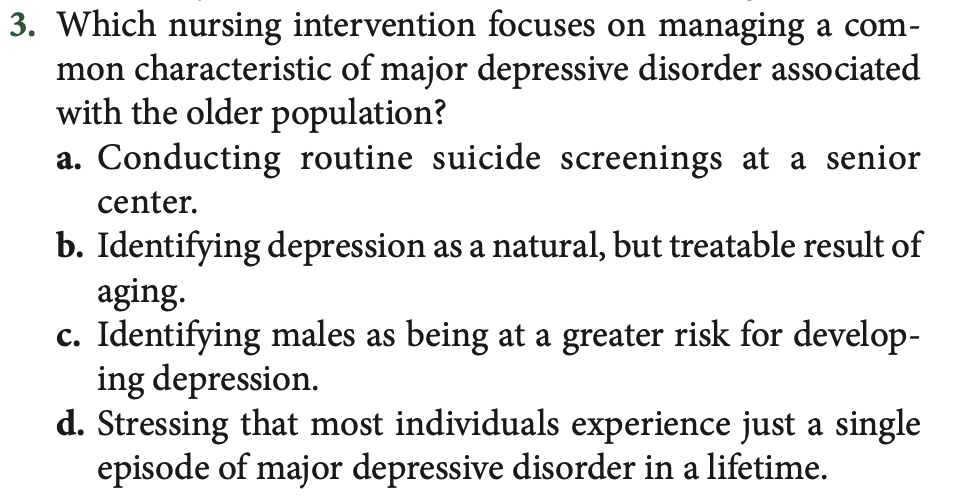
CORRECT ANSWER: A
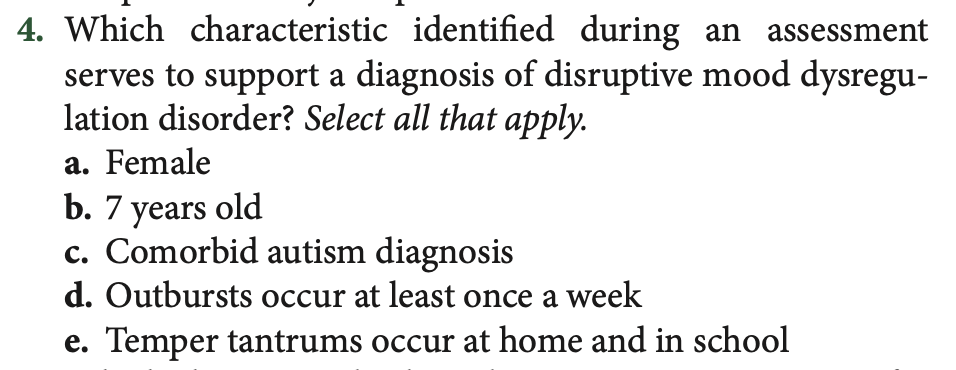
CORRECT ANSWER: B, C, E
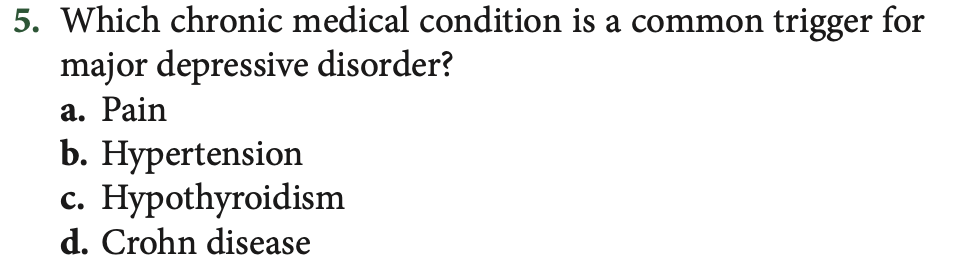
CORRECT ANSWER: A
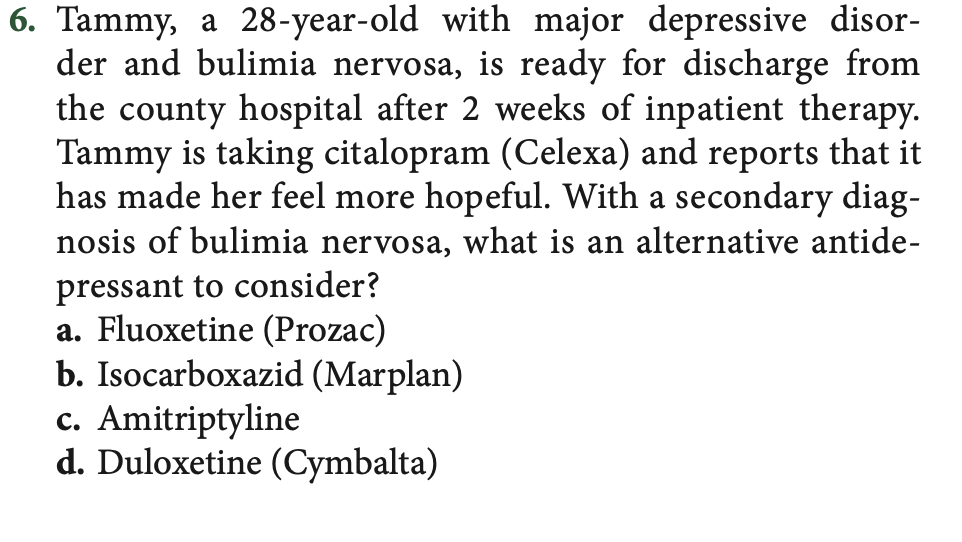
CORRECT ANSWER: A
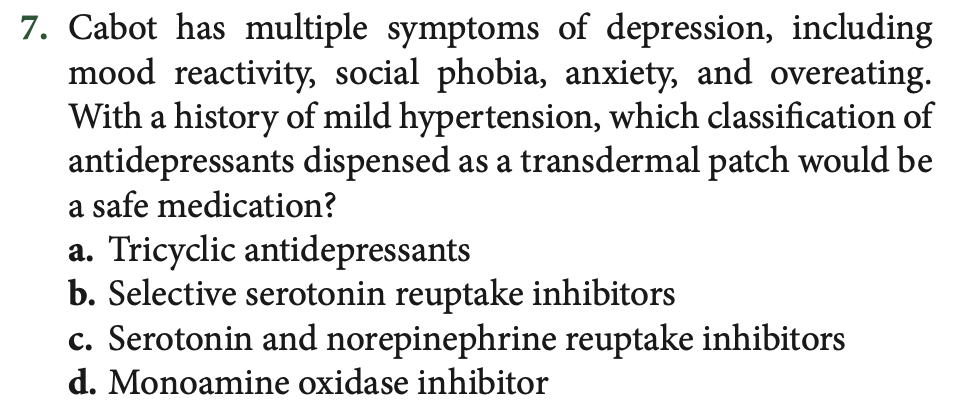
CORRECT ANSWER: D
CORRECT ANSWER: C
CORRECT ANSWER: B
CORRECT ANSWER: A