Objectives
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
129 Terms
Elective surgery
Planned in advance (e.g., cosmetic surgery, cataract removal).
Urgent Surgery
Needs to be performed soon but is not an emergency (e.g., gallbladder removal due to cholecystitis).

Emergency Surgery

Performed immediately to save life or prevent serious complications (e.g., appendectomy for ruptured appendix).
Minor Surgery

Low risk, minimal complications (e.g., skin biopsy, removal of warts).
Diagnostic

Confirms or determines a condition (e.g., biopsy).

Curative

Removes the cause of a condition (e.g., tumor removal).

Palliative

Relieves symptoms without curing (e.g., colostomy for bowel obstruction).

Reconstructive/Restorative

Restores function or appearance (e.g., plastic surgery after burns).

Transplant

Replaces malfunctioning organs (e.g., kidney transplant).
Cosmetic

Enhances appearance (e.g., rhinoplasty).
Preoperative Phase

Begins when the decision for surgery is made and ends when the patient is transferred to the operating room. It includes assessments, patient education, and preparation.
Intraoperative Phase

Starts when the patient enters the operating room and ends when they are transferred to the post-anesthesia care unit (PACU).
Postoperative Phase

Begins after surgery and continues until full recovery. It is divided into:
Immediate postoperative phase: Monitoring in PACU.
Intermediate postoperative phase: Hospital recovery.
Extended postoperative phase: Ongoing rehabilitation and home care.
Identify essential aspects of the pre-operative assessment.
Medical History: Chronic conditions (e.g., diabetes, hypertension), allergies, past surgeries.
Physical Examination: Vital signs, respiratory and cardiac status, hydration level.
Laboratory Tests: CBC, electrolytes, coagulation studies.
Medication Review: Blood thinners, insulin, steroids.
Psychosocial Assessment: Anxiety, coping mechanisms, support system.
Informed Consent: Ensuring the patient understands the procedure, risks, and benefits.
Preoperative Phase

Educate the patient on the procedure and expectations.
Ensure informed consent is obtained.
Complete physical and psychological assessments.
Intraoperative:

Maintain sterility and assist surgical team.
Monitor patient’s vital signs and anesthesia effects.
Postoperative:

Monitor for complications (bleeding, infection).
Manage pain and encourage early ambulation.
Educate on wound care and follow-up.
Describe essential preoperative teaching including; pain control, leg exercises, coughing and deep breathing exercises.
Pain Control: Explain pain management options (analgesics, PCA pump).
Leg Exercises: Prevent deep vein thrombosis (ankle pumps, leg raises).
Coughing & Deep Breathing: Prevent respiratory complications like pneumonia (incentive spirometry, splinting the incision with a pillow).
Describe essential aspects of preparing a person for surgery, including skin preparation
Fasting (NPO Status): Usually 6-8 hours before surgery.
Bowel Preparation: If required (e.g., for colorectal surgery).
Skin Preparation:
Cleansing with antiseptic solution (chlorhexidine or betadine).
Shaving (if required) using clippers to reduce infection risk.
Preoperative Medications: Sedatives, antibiotics, or anti-nausea drugs.
Marking of site to prevent wrong site surgery
Review the purpose of pre-operative medications and nursing considerations
Sedatives (e.g., benzodiazepines like midazolam): Reduce anxiety and induce relaxation.
Analgesics (e.g., opioids like morphine): Manage preoperative pain.
Anticholinergics (e.g., atropine): Reduce secretions to prevent aspiration.
Antiemetics (e.g., ondansetron, metoclopramide): Prevent nausea and vomiting.
Proton Pump Inhibitors (e.g., pantoprazole) or H2 Blockers (e.g., ranitidine): Reduce stomach acid and prevent aspiration pneumonia.
Antibiotics (e.g., cefazolin): Given prophylactically to reduce the risk of surgical site infections.
Nursing Considerations:
Verify the correct medication, dosage, and timing.
Assess for allergies and contraindications.
Educate the patient on medication effects.
Monitor vital signs for any adverse reactions.
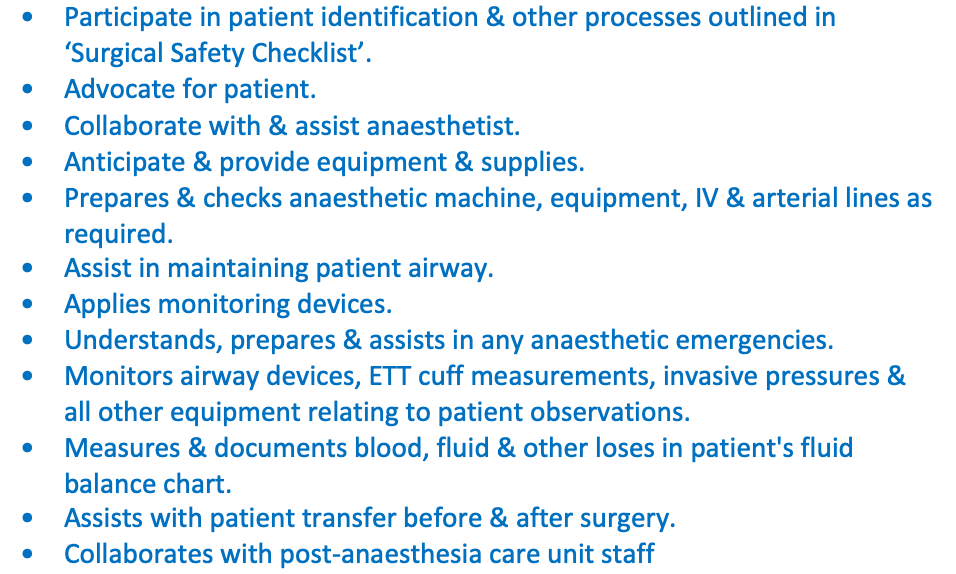
Anaesthetic Nurse
The anaesthetic nurse assists the anaesthetist in preparing and administering anaesthesia, ensuring patient safety during induction, maintenance, and recovery.
Participate in patient identification & other processes outlined in ‘Surgical Safety Checklist’.
Advocate for patient.
Collaborate with & assist anaesthetist.
Anticipate & provide equipment & supplies.
Prepares & checks anaesthetic machine, equipment, IV & arterial lines as required.
Assist in maintaining patient airway.
Applies monitoring devices.
Understands, prepares & assists in any anaesthetic emergencies.
Monitors airway devices, ETT cuff measurements, invasive pressures & all other equipment relating to patient observations.
Measures & documents blood, fluid & other loses in patient's fluid balance chart.
Assists with patient transfer before & after surgery.
Collaborates with post-anaesthesia care unit staff
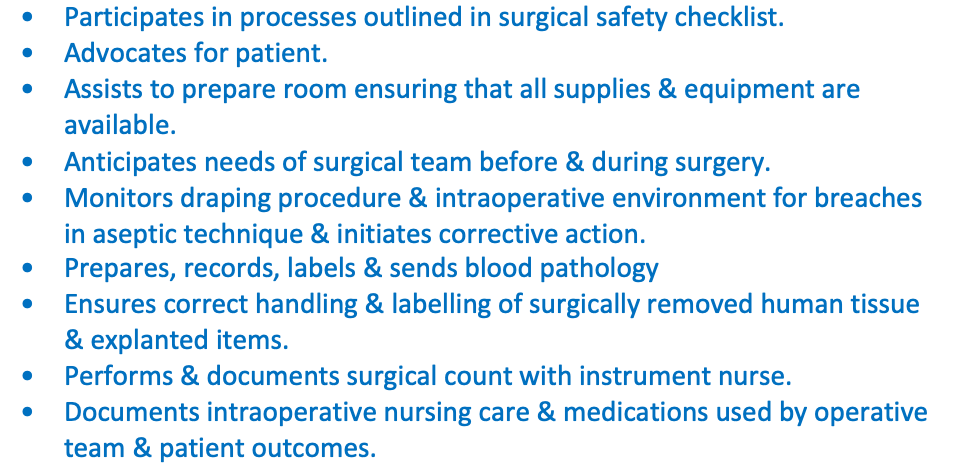
Circulating Nurse (Scout Nurse)
The circulating nurse works outside the sterile field, coordinating activities and ensuring a smooth surgical process.

Participates in processes outlined in surgical safety checklist.
Advocates for patient.
Assists to prepare room ensuring that all supplies & equipment are available.
Anticipates needs of surgical team before & during surgery.
Monitors draping procedure & intraoperative environment for breaches in aseptic technique & initiates corrective action.
Prepares, records, labels & sends blood pathology
Ensures correct handling & labelling of surgically removed human tissue & explanted items.
Performs & documents surgical count with instrument nurse.
Documents intraoperative nursing care & medications used by operative team & patient outcomes.
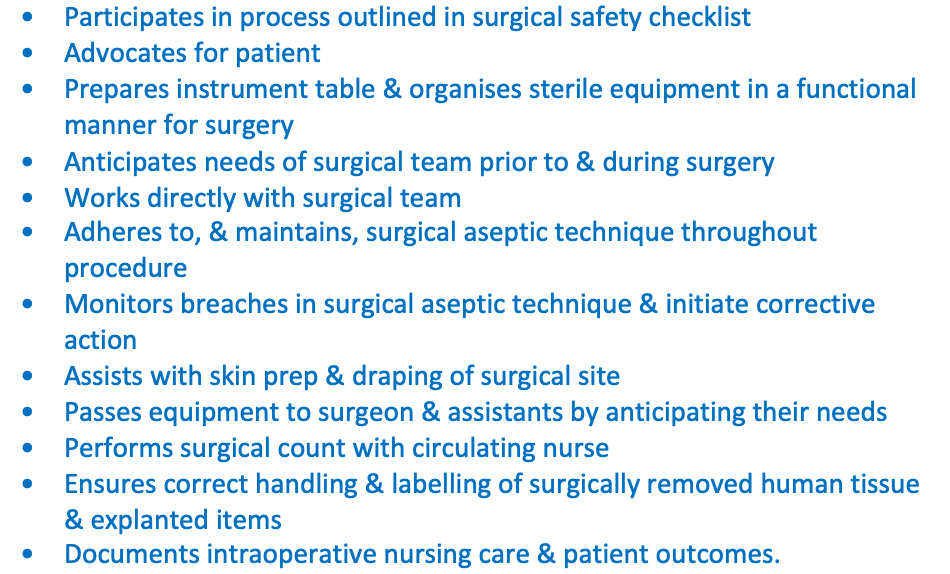
Instrument nurse (Scrub nurse)

The scrub nurse works within the sterile field, directly assisting the surgeon by handling surgical instruments.
Participates in process outlined in surgical safety checklist
Advocates for patient
Prepares instrument table & organises sterile equipment in a functional manner for surgery
Anticipates needs of surgical team prior to & during surgery
Works directly with surgical team
Adheres to, & maintains, surgical aseptic technique throughout procedure
Monitors breaches in surgical aseptic technique & initiate corrective action
Assists with skin prep & draping of surgical site
Passes equipment to surgeon & assistants by anticipating their needs
Performs surgical count with circulating nurse
Ensures correct handling & labelling of surgically removed human tissue & explanted items
Documents intraoperative nursing care & patient outcomes.
Safety and risk management requirements
Maintain a sterile field and aseptic technique.
Prevent surgical site infections through proper hand hygiene and sterile draping.
Ensure correct patient positioning to prevent pressure injuries.
Perform surgical time-outs to confirm patient identity, procedure, and site.
Specific pre-, intra- and post-operative communication for patients
Preoperative: Educate the patient, answer questions, obtain informed consent.
Intraoperative: Communicate with the surgical team, document findings, and monitor the patient’s condition.
Postoperative: Provide handover to PACU staff, ensure smooth transition to recovery.
Differentiate between each type of anaesthesia and their purposes
General Anaesthesia: Induces unconsciousness and complete muscle relaxation (e.g., for major surgeries like open-heart surgery).
Regional Anaesthesia: Blocks sensation in a specific area while the patient remains conscious (e.g., epidural for childbirth).
Local Anaesthesia: Numbs a small area for minor procedures (e.g., lidocaine injection for suturing).
Identify potential post-anaesthesia complications and develop management strategies
Respiratory Issues: Airway obstruction, hypoxia.
Cardiovascular Instability: Hypotension, arrhythmias.
Nausea and Vomiting: Common with general anaesthesia.
Delayed Awakening: Due to prolonged drug effects.
Management Strategies:
Monitor vital signs and oxygenation.
Provide antiemetics and IV fluids.
Ensure airway patency and assist with ventilation if needed.
Examine equipment used in airway management including endotracheal tubes (ETT), laryngeal mask airway (LMA), oropharyngeal and nasopharyngeal airway adjuncts.
Endotracheal Tube (ETT): Inserted into the trachea for mechanical ventilation.
Laryngeal Mask Airway (LMA): Sits over the larynx to maintain an open airway.
Oropharyngeal Airway (OPA): Prevents airway obstruction by keeping the tongue from blocking the throat.
Nasopharyngeal Airway (NPA): Inserted through the nostril to maintain airway patency.
Discuss common respiratory surgical/procedural interventions for airway disruption.
Tracheostomy: Creating an opening in the trachea for long-term ventilation.
Acute airway obstruction is a medical emergency-insertion of a tracheostomy or similar airway may be required
Tracheostomy—a surgically created stoma (opening) in trachea, performed to establish an airway:
Bypassing an upper airway obstruction.
Facilitating secretion removal.
Allowing for long-term mechanical ventilation.
Immediate post-anaesthetic phase assessment A-E

A(irway): Patency & adequacy
B(reathing): Adequacy of ventilation/oxygenation
Arterial oxygen saturation
Adequacy of ventilation (CO2 increase- no adequate breath)
Respiratory rate, rhythm, depth
Use of accessory muscles (neck, diaphragm, positioning, abdominal muscles-rib)
Air entry & breath sounds
C(irculation): Adequacy of circulation
Heart rate & rhythm
Peripheral pulses amplitude & equality
Blood pressure
Capillary filling time (capp. refill) & skin warmth
Fluid status
Intake & output (estimated blood loss from surgery) (urine output anything less then 30ml concerning)
IV infusions
Signs of dehydration/fluid overload
D(isability): Neurological function
Level of consciousness (AVPU +/- GCS) (check with baseline)
Presence of protective reflexes (e.g. gag, cough, swallow)
Duration of emergence form unconsciousness
Ability to move extremities/limb power
Blood glucose
Pain
E(xposure):
Condition of operative site
Status of dressing
Drainage (type, amount, colour)
Drains
Patency
Type
Suction on/off
Body temperature
Postoperative care- lifespan and other considerations

Children:
Infants & young children- may not state their pain levels-can use other signs-crying, fussiness, increased heart rate & BP, agitation (FLACC-face, legs, arms, cry, consolability)
Good pain control help facilitate healing process & recovery
Some PACU’s have parents in area when child is waking & stable-calms both child & can reduce parent anxiety
Older adults
Have less efficient reserves –can take longer to recover –more fatigue & weakness post op (less elasticity)
Patients with dementia-increase in confusion & agitation- safety risk-calm & reassuring attitude important
Follow up phone calls if outpatient surgery useful for check on patient condition & if patient understood post op instructions/care
Bariatric patients- Increased risk for:
Airway obstruction-fat deposits in neck
Atelectasis –increased pressure on diaphragm from excess abdominal tissue
Difficulty clearing anaesthetic medications from system-pain control more complex (as it sits in the fat cells)
Thromboembolism
Pressure areas
Other issues to consider:
Diabetes Mellitus –healing impaired
Impaired vision or hearing (back on pt so they are more orientated)
Peripheral vascular disease-healing impaired
Previous cerebrovascular accident (CVA/Stroke)
Smoking, alcohol, drugs (resistance to normal doses)
This week’s focus is on the immediate postoperative phase in the PACU, and considers:
Close monitoring of patient is critical for safety- Unobstructed view of all patients
Situational awareness important- need for recognizing deterioration & acting quickly
Patient unable to protect themselves from environmental stimuli- reliant on nurse depending on level of consciousness =1:1 care for unconscious patients
Use of side rails
High risk of sudden deterioration
Observations 5-15 minutely
Continuous SpO2 +/- ECG (continuously monitoring)
Clinical reasoning (CR Cycle) helps identify & consider cues to predict & then intervene when needed
Knowing how to communicate issues accurately & timely is important
Pneumonia

Inflammation of alveoli
Causes: infection, toxins, irritants causing inflammation. Immobility & impaired ventilation results in lung collapse with growth of lung pathogens
Signs: increased temperature, cough –productive-with blood, purulent sputum, dyspneoa, chest pain
Preventative management: Deep breathing & coughing, early moving in bed & ambulation
Atelectasis (lung collapse)

Alveoli collapse & not ventilated!
Causes: mucus plugs causing blockage in bronchial airways, decreased lung expansion, analgesics, immobility
Signs: Dyspneoa, tachypnoea, tachycardia; diaphoresis, anxiety; pleural pain, decreased chest wall movement; dull or absent breath sounds; decreased oxygen saturation (SpO2)
Preventative management: Deep breathing & coughing, early moving in bed & ambulation
Pulmonary Embolism (PE)

Blood clot that has moved to lungs blocking a pulmonary artery, thus obstructing blood flow to a portion of lung
Causes: Stasis of venous blood from immobility, venous injury from fractures or during surgery, use of oral contraceptives high in oestrogen, pre-existing coagulation or circulatory disorder
Signs: Sudden chest pain, shortness of breath, cyanosis, shock (tachycardia, low blood pressure)
Preventative management: Turning, ambulation, anti-embolic stockings, sequential compression device (SCD)-promotes venous blood flow
Pneumothorax
occurs when air leaks into the space between the lung and the chest wall. This air accumulation puts pressure on the lung, causing it to partially or fully collapse
Hemothorax
is a condition where blood collects in the pleural space, the area between the lung and the chest wall
Chest drains are inserted following:

cardiothoracic surgery;
after chest trauma;
following a spontaneous pneumothorax;
or from any conditions resulting in accumulation of content in pleural space.
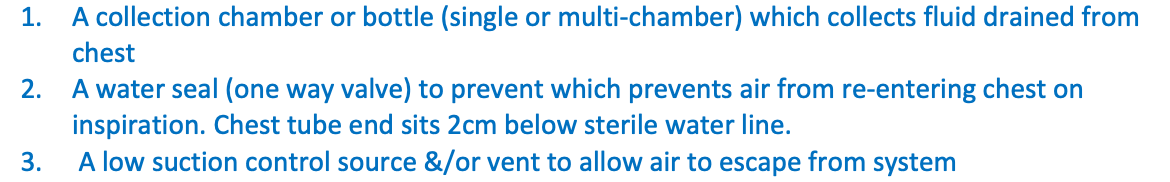
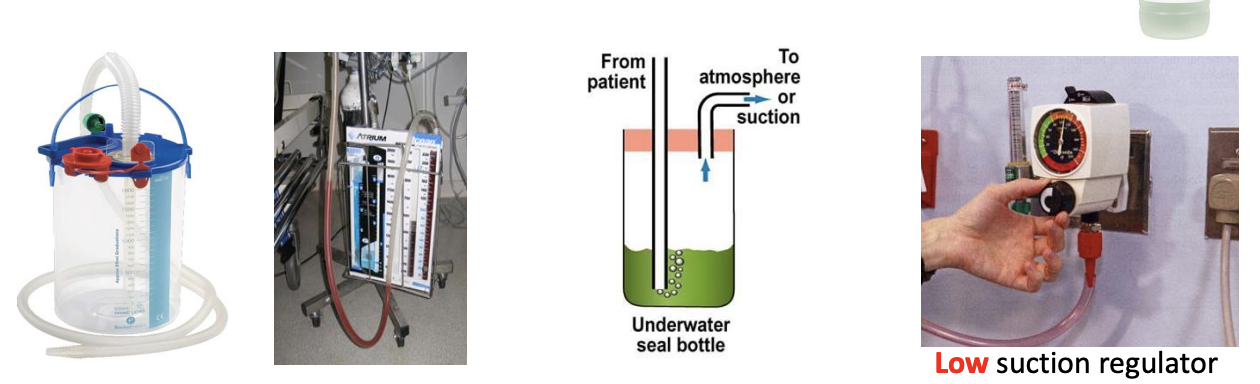
Chest drainage systems have 3 main components:

A collection chamber or bottle (single or multi-chamber) which collects fluid drained from chest
A water seal (one way valve) to prevent which prevents air from re-entering chest on inspiration. Chest tube end sits 2cm below sterile water line.
A low suction control source &/or vent to allow air to escape from system
Non-invasive ventilation (NIV)- NIV

Non-invasive: Delivered via face or nasal masks or nasal cannulae (HFNC)
Positive pressure ventilation: air “forced” into patient’s airway, as opposed to natural breathing whereby air enters under negative pressure (diaphragm drops, drop in intrathoracic pressure)
Can only be delivered to patient who is breathing spontaneously & able to protect airway e.g. able to clear secretions. (NIV pt is awake)
NIV- Complications:

Hypotension (increased intrathoracic pressure)
Pulmonary barotrauma
Gastric distension (increased risk of aspiration)
Air leaks
Mask/tube discomfort
Pressure injuries (face & occiput)
Eye irritation
NIV- Nursing care:

Close observation (1:1 or 1:2 ratio typically)
High dependency area (PACU, CCU, HDU or ICU setting)
Hourly observation (at minimum)
May require NGT (aspiration risk)
Communication & reassurance
Planned breaks (oral & eye care, meals, pressure area care)
Airway Management:

Ensure airway patency (e.g., suctioning secretions, positioning).
Use airway adjuncts like oral or nasal airways if needed.
Be prepared for reintubation in severe cases.
Prevention and Early Detection of Complications NIV:

Frequent respiratory assessments (rate, depth, effort, breath sounds).
Monitor for signs of respiratory distress (cyanosis, tachypnea, use of accessory muscles).
Encourage early ambulation and repositioning to reduce the risk of atelectasis and PE.
NIV Pain Management:

Adequate pain control (opioids, NSAIDs, regional anesthesia) to allow effective breathing.
Encourage splinting of the incision while coughing or deep breathing to reduce discomfort.
High Flow Nasal Cannula/Prongs (HFNC/HFNP)- NIV

Supplemental oxygen delivered under a high flow
Settings:
Flow: Litres of gas per minute delivered (gas = air & O2)
20 – 60L gas/min
FiO2: Between 21% - 100% FiO2
Benefits:
Generates PEEP in lower airways
Cannot control PEEP like in CPAP (can't measure it)
Decreases physiological dead space (improving ventilation)
Reduces respiratory effort
Therapy better tolerated by patients
Uses: Bridge between CPAP & Low Flow oxygen (step down/up)
Continuous Positive Airway Pressure (CPAP)- NIV
Gas delivered under constant positive pressure during inspiration & expiration
“Splints open” airways
Recruits collapsed alveoli
Two main settings:
Fraction of inspired oxygen (FiO2) = Between 21% - 100% oxygen
PEEP = Positive End Expiratory Pressure. Pressure remaining in lungs at end expiration. Typically set between 5 – 10cmH2O
Used for: post operative atelectasis, pulmonary oedema, Type 2 Respiratory Failure (hypercapnia) & COPD
Chronic Obstructive Pulmonary Disease (COPD)

COPD revision
A COPD exacerbation is characterized by dyspnea &/or cough & sputum that worsens over ≤14 days; it may be accompanied by tachypnea &/or tachycardia & is often associated with increased local & systemic inflammation caused by airway infection, pulmonary embolism, pollution, or other airway insult.
Management goals:
Reverse airflow limitation using short-acting inhaled bronchodilators & oral systemic glucocorticoids e.g. prednisone
Treat infection, which is implicated in most exacerbations-some patients require antibiotics
Exclude other causes for which additional therapy is needed (eg, pulmonary embolism)
Ensure appropriate oxygenation-target of 88 to 92 percent pulse oxygen saturation= preventing worsening of hypercapnia
Avoid intubation & mechanical ventilation: NIV is preferred. Hiflow nasal cannula can be used which can provide a low level of continuous positive airway pressure (CPAP)
Pharmacological Approaches for pain
Opioids (e.g., morphine, fentanyl) for moderate to severe pain.
Non-opioid analgesics (e.g., paracetamol, NSAIDs like ibuprofen) to reduce inflammation and opioid use.
Local anesthetics (e.g., nerve blocks, epidurals) for site-specific pain control.
Adjuvant medications (e.g., anticonvulsants like gabapentin, antidepressants like amitriptyline) for neuropathic pain.
Non-Pharmacological Approaches for pain
Cognitive-behavioral therapy (CBT)
Cold/heat application
Relaxation techniques, such as breathing exercises
Patient education about pain expectations and control
Management of pain
Regular pain assessments using validated scales (e.g., Numeric Rating Scale, Wong-Baker Faces Scale)
Adjusting plans based on patient-specific factors (age, comorbidities, type of surgery)
Potential Complications of Post-operative Pain Management
Opioid-Related Complications:
Respiratory depression
Nausea and vomiting
Constipation
Opioid tolerance and dependency
Sedation and confusion (especially in elderly patients)
NSAID-Related Complications:
Gastrointestinal bleeding
Renal impairment
Cardiovascular risks (e.g., hypertension, heart failure exacerbation)
Local Anesthetic Complications:
Local anesthetic systemic toxicity (LAST)
Nerve damage
Infection at injection sites
Inadequate Pain Control:
Delayed mobilization, increasing the risk of:
Deep vein thrombosis (DVT)
Pulmonary embolism (PE)
Pneumonia
Poor wound healing
Chronic post-surgical pain development
Psychological Impact:
Increased anxiety and fear
Depression
Post-traumatic stress symptoms
Schedule 8
otherwise known as Controlled Drugs, are substances & preparations for therapeutic use which have high potential for abuse & addiction.
All drugs that are schedule 8 must be approved by health department at time of writing a prescription for that drug; prescriptions must be written by hand & not printed.
Schedule 4 Restricted (S4R)

These schedule 4 medicines are liable to abuse & may cause dependence. These medicines may be targeted for unauthorised use or diversion into illicit activities. These medications require more stringent storage & recording policies to allow more rigid monitoring & increase accountability of all health care providers.
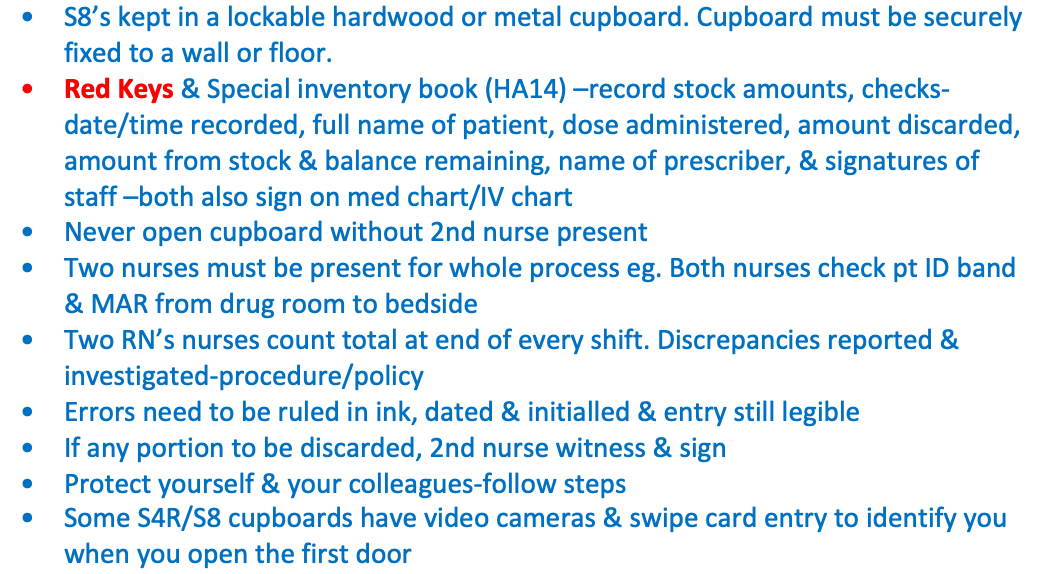
Schedule 8 care
S8’s kept in a lockable hardwood or metal cupboard. Cupboard must be securely fixed to a wall or floor.
Red Keys & Special inventory book (HA14) –record stock amounts, checks-date/time recorded, full name of patient, dose administered, amount discarded, amount from stock & balance remaining, name of prescriber, & signatures of staff –both also sign on med chart/IV chart
Never open cupboard without 2nd nurse present
Two nurses must be present for whole process eg. Both nurses check pt ID band & MAR from drug room to bedside
Two RN’s nurses count total at end of every shift. Discrepancies reported & investigated-procedure/policy
Errors need to be ruled in ink, dated & initialled & entry still legible
If any portion to be discarded, 2nd nurse witness & sign
Protect yourself & your colleagues-follow steps
Some S4R/S8 cupboards have video cameras & swipe card entry to identify you when you open the first door
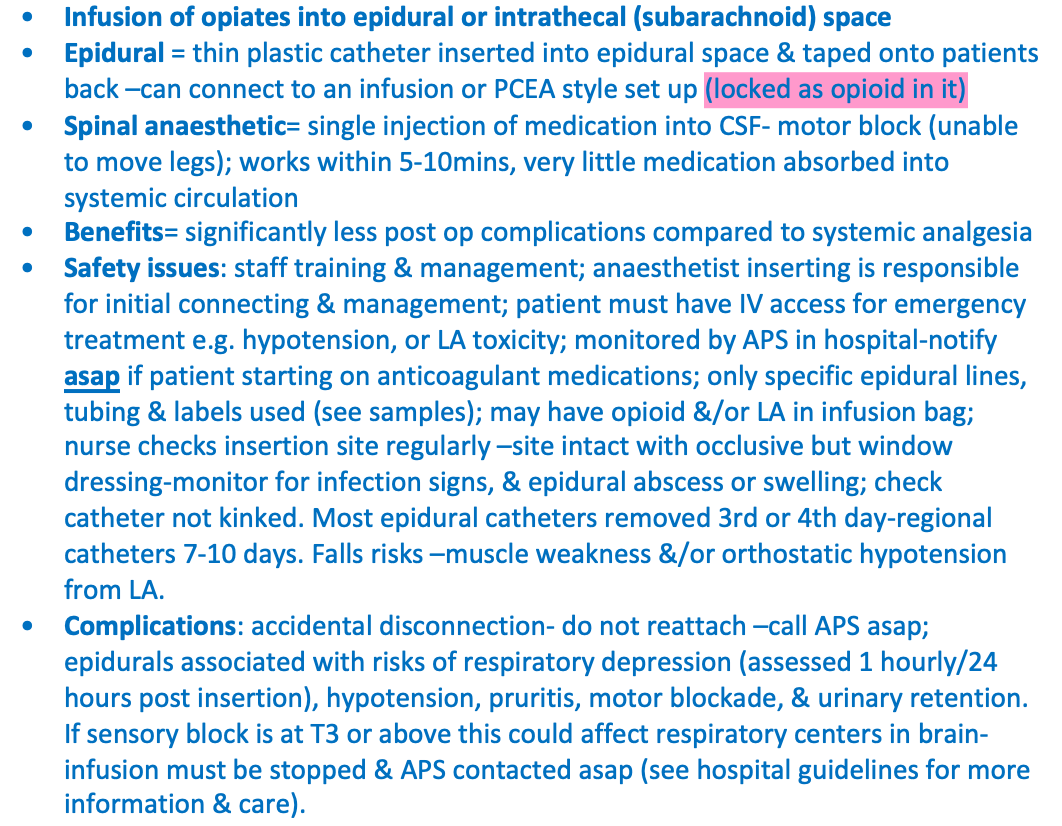
Epidural and spinal care – management and care

Infusion of opiates into epidural or intrathecal (subarachnoid) space
Epidural = thin plastic catheter inserted into epidural space & taped onto patients back –can connect to an infusion or PCEA style set up (locked as opioid in it)
Spinal anaesthetic= single injection of medication into CSF- motor block (unable to move legs); works within 5-10mins, very little medication absorbed into systemic circulation
Benefits= significantly less post op complications compared to systemic analgesia
Safety issues: staff training & management; anaesthetist inserting is responsible for initial connecting & management; patient must have IV access for emergency treatment e.g. hypotension, or LA toxicity; monitored by APS in hospital-notify asap if patient starting on anticoagulant medications; only specific epidural lines, tubing & labels used (see samples); may have opioid &/or LA in infusion bag; nurse checks insertion site regularly –site intact with occlusive but window dressing-monitor for infection signs, & epidural abscess or swelling; check catheter not kinked. Most epidural catheters removed 3rd or 4th day-regional catheters 7-10 days. Falls risks –muscle weakness &/or orthostatic hypotension from LA.
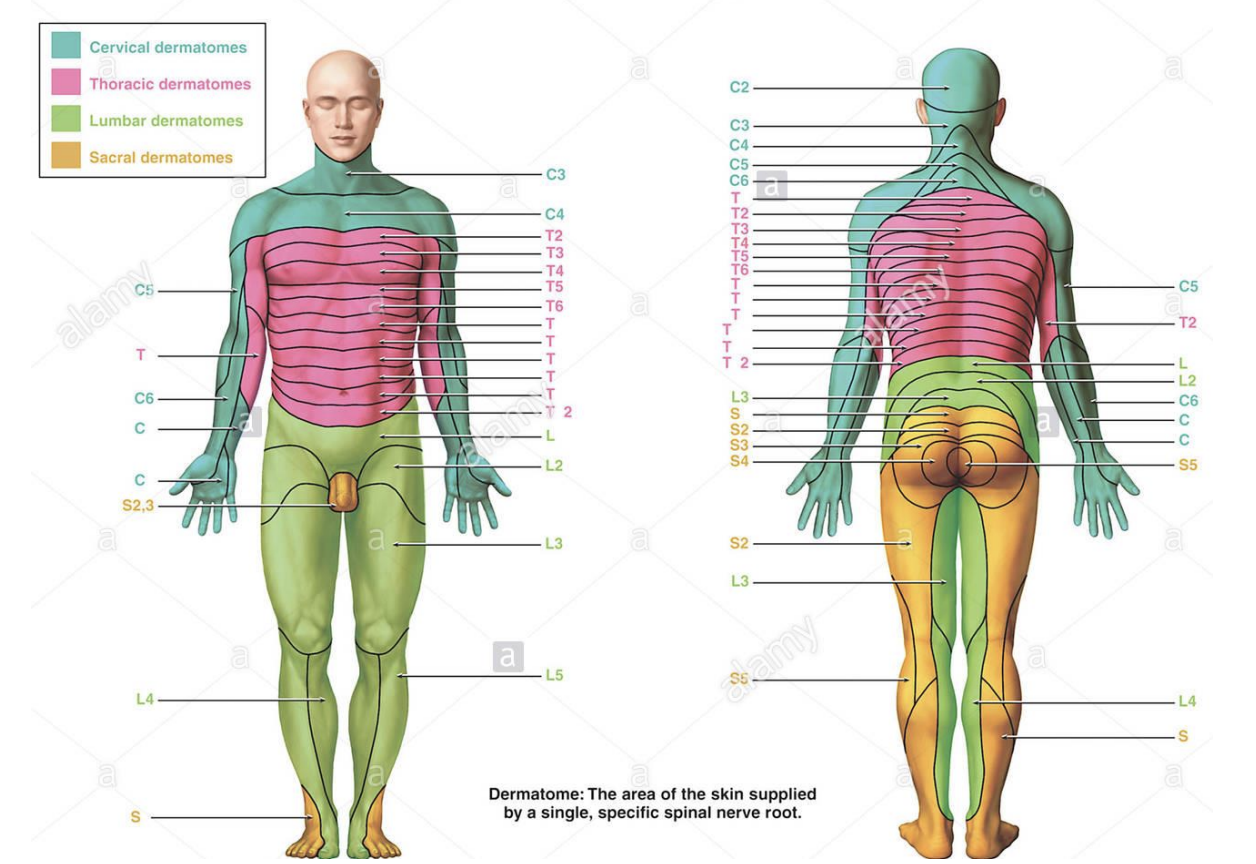
Complications: accidental disconnection- do not reattach –call APS asap; epidurals associated with risks of respiratory depression (assessed 1 hourly/24 hours post insertion), hypotension, pruritis, motor blockade, & urinary retention. If sensory block is at T3 or above this could affect respiratory centers in brain- infusion must be stopped & APS contacted asap (see hospital guidelines for more information & care).
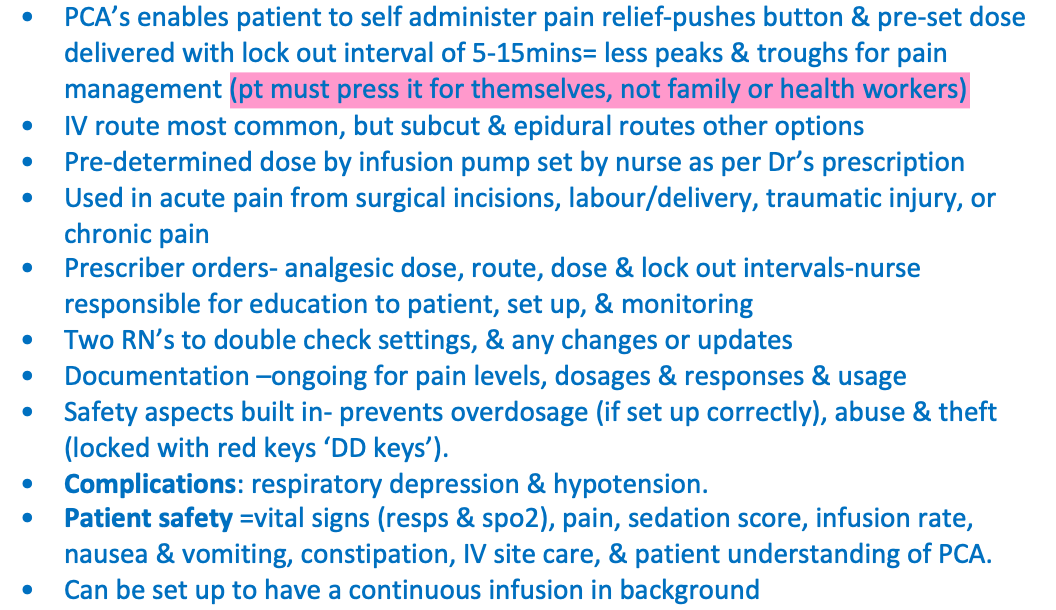
PCA care and management

PCA’s enables patient to self administer pain relief-pushes button & pre-set dose delivered with lock out interval of 5-15mins= less peaks & troughs for pain management (pt must press it for themselves, not family or health workers)
IV route most common, but subcut & epidural routes other options
Pre-determined dose by infusion pump set by nurse as per Dr’s prescription
Used in acute pain from surgical incisions, labour/delivery, traumatic injury, or chronic pain
Prescriber orders- analgesic dose, route, dose & lock out intervals-nurse responsible for education to patient, set up, & monitoring
Two RN’s to double check settings, & any changes or updates
Documentation –ongoing for pain levels, dosages & responses & usage
Safety aspects built in- prevents overdosage (if set up correctly), abuse & theft (locked with red keys ‘DD keys’).
Complications: respiratory depression & hypotension.
Patient safety =vital signs (resps & spo2), pain, sedation score, infusion rate, nausea & vomiting, constipation, IV site care, & patient understanding of PCA.
Can be set up to have a continuous infusion in background
Describe the Nursing management and assessment of post-operative emergence delirium.
Acute confusion which occurs during recovery from general anaesthetic
Usually short-term & may resolve within minutes
Common in paediatric populations & older patients
Initial management of emergence delirium &/or agitation includes:
Reassurance & reorientation.
Treatment of acute pain.
Treatment of other discomfort (bladder distention, hypothermia).
Laboratory testing to determine if hypoxemia, hypercarbia, hypoglycemia, or electrolyte imbalances are present.
Consideration of effects of certain residual anaesthetic agents
Explore Post-Operative Cognitive Dysfunction.
New cognitive deficits that appear immediately postoperatively
Not well understood thus far & requires further research
Suspected to have an inflammatory process resulting in cognitive dysfunction
Clinical observational studies show that POCD arises more frequently after extensive surgery under general anaesthesia, after secondary surgery, & when there are postoperative complications.
Discuss potential contributors and complications associated with delayed emergence
Lack of consciousness 20-30 minutes after last administration of anaesthetic-related medications
Contributing factors:
Hepatic or renal insufficiency
Age & weight
Body temperature
Medication length of action
Postoperative factors influencing urinary and renal function
Pathological conditions & types of renal failure-
Surgical procedures
Patient assessment questions
Bladder scanning and residual urine
Postoperative renal and urinary complications

Altered urine production
Urinary retention post op
Altered urine production

Normal function= 5-6 times a day, 1500ml or less output Abnormal= Revise terms & causes-prereading see table 51.3 in text
Oliguria (less than 30mls an hr), Anuria (lack of urine production), Polyuria (Litres more of urine than normal- due to diabetes, new medications, pituitary tumour, increased fluids), Frequency/Nocturia (urination in night), Urgency, Enuresis (involuntary), Retention
Urinary retention post op

Patients must void within 8 hours post op –report to medical staff
Anaesthetics depress bladder tone- resolves around 6-8 hours post op; note surgery type affecting urinary function if delays
Strict Fluid balance –input/output post op important-usually 2 days
Interventions: IDC may be required if retention persists if techniques aren’t successful- such as positioning (male-standing/female-sitting), running water, ensuring fluid intake, ambulation
Goal should be to seek help in the team prior to MET criteria
Infants & children factors affecting voiding

UTI’s common –can affect kidneys, bladder or both-if frequent- needs Dr review;
Teaching perineal hygiene important-Girls- wipe front to back, cotton underwear
Taught to go asap when sensation to void is felt
Older adults factors affecting voiding

Older women-UTI’s- can lead to incontinence, confusion, & falls; Menopause -decreased oestrogen=decreased perineal tone & bladder support –stress incontinence, leakage on exertion, & UTI’s
Older men-enlarged prostate-incomplete emptying of bladder=urinary retention & overflow dribbling of urine (take longer to empty their bladder & stop start, cultural change, functional incontinent)
Other issues to consider affecting voiding
Sex reassignment surgery=changes to urethra- longer term issues –stress incontinence, overactive bladder, & reduced blood flow
Note genital mutilation or obstetric fistulas (recurrent UTI’s, leakage) in some populations
Overactive bladder –sudden urge to void-from nerve damage from diabetes, stroke, injury, or surgery
Functional incontinence= from impaired mobility –joint & bone pain-surgery & neuromuscular issues –difficult to get to bathroom
Cognitive impairments- Dementia
Pathological conditions & types of renal failure-

Pre-renal – haemorrhage, dehydration, burns, shock, low intravascular volume
Intra Renal – nephrotoxic agents (gentamicin), transfusion reactions, diseases of glomeruli, renal neoplasms, systemic disease (DM), infections, hereditary (polycystic kidney disease)
Post-renal – obstruction (calculi -stones, clots, tumours),
Surgical procedures

Post cystoscopy –inflammation
Bleeding post op-risk of clots
Spinal anaesthetics –decrease awareness to void
Abdo surgery- structures adjacent to urinary system-swelling & affecting voiding e.g. uterus
Prevention of urinary tract infections

More common in women; nosocomial occurs in healthcare & mostly related to IDC insertion; Most UTIs caused by bacteria common to intestinal environment (e.g. Escherichia coli)- This GI bacteria can move into urethra following urethral trauma, irritation, & manipulation. See readings for preventative measures
Urinary sheaths- used for managing incontinence (less risk for UTI than IDC)
Suprapubic catheter (other options)- Dr inserts surgically through abdominal wall into bladder with LA & with closed drainage system; temporary or long term; maintenance of drainage tube –can become blocked easily; dressing care at site of insertion
Key points and nursing care

Strict aseptic technique
If resistance felt on insertion- STOP & seek help
Document post insertion-sticker in notes
Encourage fluids
Perineal care
Long term IDC
Strict FBC
Care of clients with bladder irrigations

Bladder Irrigation; continuous or intermittent; closed or open
Indications- to prevent blood clots & mucous occluding catheter eg. post genitourinary surgery; to instil medication
Medical order
Strict Aseptic technique
Warm irrigating fluids
Strict FBC
Monitor & assess drainage- observations 30 minutely
Bladder scans pre/prior to installation of fluid
Review sample hospital policies
Renal failure: Peritoneal Dialysis

Dialysis = fluids & molecules pass through a semi-permeable membrane with osmosis
Peritoneal dialysis (PD)- dialysis solution is instilled into abdominal cavity through a catheter, allowed to rest there while fluid & molecules exchange & then removed through catheter.
In PD peritoneal membrane acts as semipermeable membrane.
Peritoneal dialysis facilitates removal of waste products & excess fluid from bloodstream
process uses a specialised solution called dialysate, which is administered into peritoneal cavity
peritoneal cavity is then drained via gravity into a wastage bag for disposal
Performed at regular intervals until function returns or forever
Complications:
Exit-site infection
Peritonitis
Hernias-abdo wall from volume pressure of fluid
Lower back problems
Bleeding
Pulmonary complications-fluid shifts
Renal failure: Haemodialysis

Person’s blood flows through vascular catheters, passes by dialysis solution in an external machine & then returns to person.
It is used to correct fluid & electrolyte imbalances & to remove waste products in kidney failure. It can also be used to treat medication overdoses.
In HD an artificial membrane (usually made of cellulose-based or synthetic materials) is used as semipermeable membrane & is in contact with patient's blood.
Haemodialysis Types of access:
Arteriovenous fistulas & grafts (never take a blood pressure or blood tests or insert IV in this arm; has a ‘thrill’ vibration on palpation, & ‘bruit’ sound)
Temporary vascular access-Dialysis catheter (VasCath)
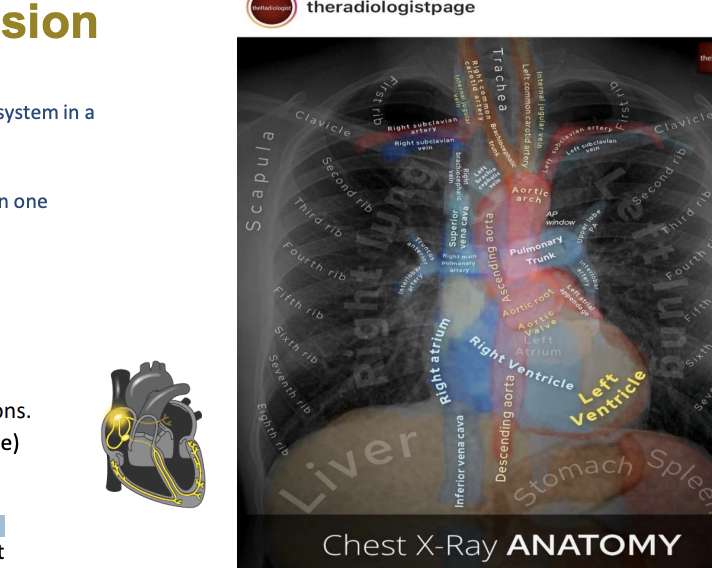
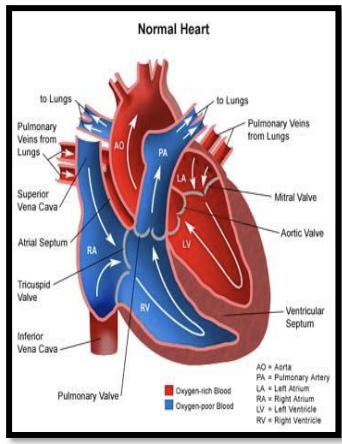
Cardiac physiology

What is Cardiac Output (CO)?
Amount of blood heart pumps through circulatory system in a minute.
What is Stroke Volume?
amount of blood put out by left ventricle of heart in one contraction.
CO = SV x HR
Heart rate

Influenced by autonomic nervous system (e.g. ‘Fight or flight’); blood pressure; hormones (thyroid); & medications.
Heart rates >150bpm cause inadequate filling time (diastole) thus a HR increases CO; if SV stays same.
Chronotropic effects (chrono= time) are those that change heart rate (SA node). Positive chronotropes >HR, whilst negative chronotropes <HR.
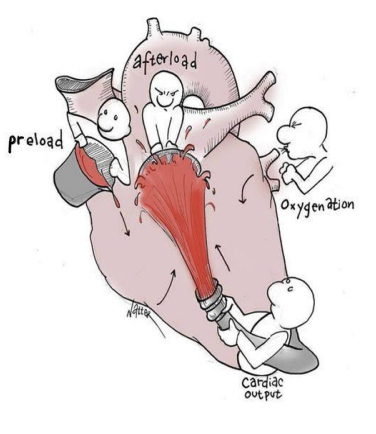
Stroke volume is determined by three factors

Preload: filling pressure of heart at end of diastole (volume circulating into atria/ventricles . Low preload-blood transfusions. High preload- furosemide)
Contractility: Inotropic state of heart-strength of contraction. Influenced by autonomic nervous system & medications. Positive inotropic drugs >contractility whilst negative inotropic drugs (force of heart)
Afterload: Pressure against which heart must work to eject blood during systole (resistance of ventricle must overcome to pump blood out into aorta & pulmonary artery)
Hypovolaemia

Inadequate circulating blood volume
Causes: Fluid deficit, haemorrhage
Signs: Tachycardia, decreased urine output, decreased blood pressure
Preventative management: Early detection of signs; fluid &/or blood replacement
Hypovolaemic shock

Inadequate tissue perfusion resulting from markedly reduced circulating blood volume
Causes: Severe hypovolaemia from fluid deficit or haemorrhage
Signs: Rapid weak pulse, dyspnoea, tachypnoea; restlessness & anxiety; urine output less than 30 mL/hr; decreased blood pressure; cool, clammy skin, thirst, pallor
Preventative management: Maintain blood volume through adequate fluid replacement, prevent haemorrhage; early detection of signs
Haemorrhage

Internal or External bleeding
Causes: Disruption of sutures, insecure sutures, insecure ligation of blood vessels
Signs: Overt bleeding (dressings saturated with bright blood; bright, free-flowing blood in drains or chest tubes), increased pain, increasing abdominal girth, swelling or bruising around incision
Preventative management: Early detection of signs
Thrombophlebitis

Inflammation of veins, usually of legs & associated with a blood clot
Causes: Slowed venous blood flow due to immobility or prolonged sitting; trauma to vein, resulting in inflammation & increased blood coagulability
Signs: Aching, cramping pain; affected area is swollen, red & hot to touch; vein feels hard; discomfort in calf when foot is dorsiflexed or when person walks (Homans’ sign)
Preventative management: Early ambulation, leg exercises, anti-embolic stockings, SCDs, adequate fluid intake
Thrombus

Blood clot attached to wall of vein or artery (most commonly leg veins)
Causes: As for thrombophlebitis for venous thrombi; disruption or inflammation of arterial wall for arterial thrombi
Signs: Venous: same as thrombophlebitis
Arterial: pain & pallor of affected extremity; decreased or absent peripheral pulses
Preventative management: Venous: same as thrombophlebitis Arterial: maintain prescribed position; early detection of detection of signs
Embolus

Foreign body or clot that has moved from its site of formation to another area of body (e.g. lungs, heart or brain)
Causes: Venous or arterial thrombus; broken intravenous catheter, fat or amniotic fluid
Signs: In venous system, usually becomes a pulmonary embolus (see pulmonary embolism); signs of arterial emboli may depend on location
Preventative management: Turning, ambulation, leg exercises, SCDs; careful maintenance of IV catheters
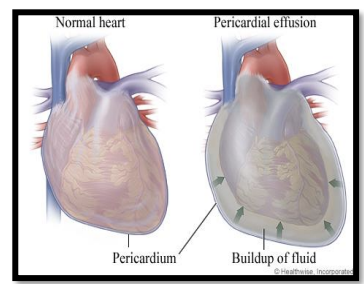
Cardiac tamponade

is a clinical syndrome caused by accumulation of fluid in pericardial space, resulting in reduced ventricular filling & subsequent hemodynamic compromise (squashes heart)
Condition is a medical emergency, complication of which include profound shock, multi organ failure & death.
Signs:
Tachypnea
Tachycardia
Elevated jugular venous pressure (JVP) & CVP
Confusion
Decreased urine output
Hypotension
Peripheral cyanosis
Management:
Urgent medical review
Drainage/evacuation of fluid from pericardial space
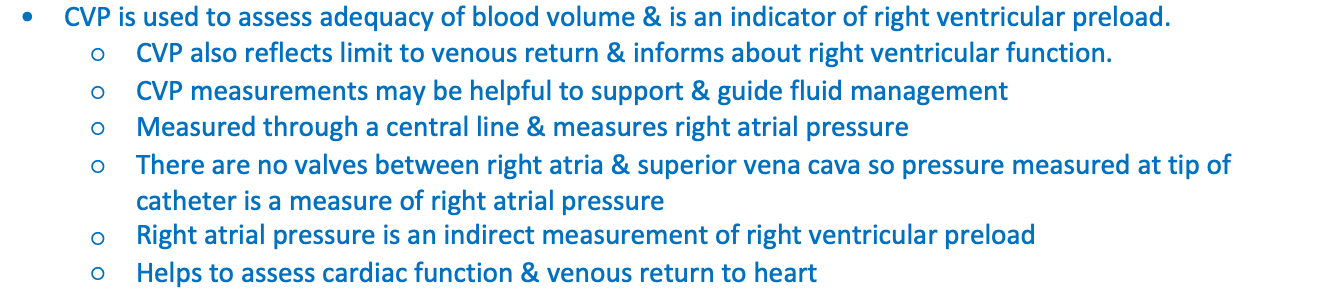
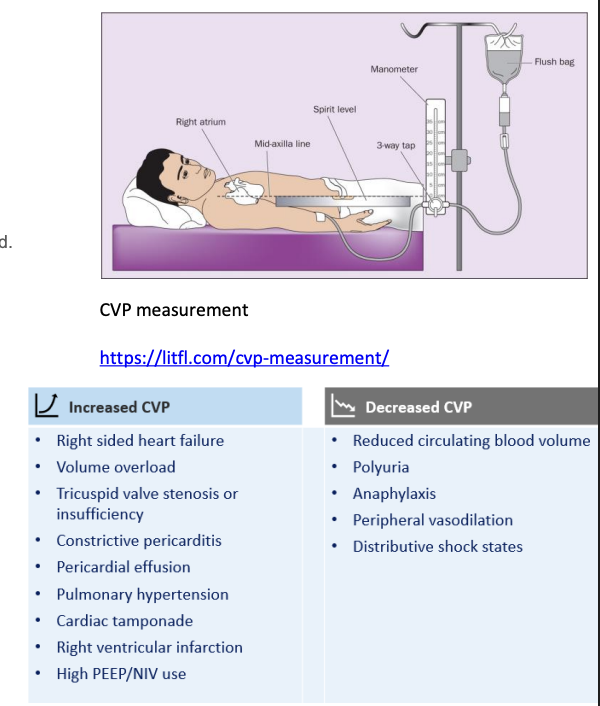
Why measure CVP:

CVP is used to assess adequacy of blood volume & is an indicator of right ventricular preload.
CVP also reflects limit to venous return & informs about right ventricular function.
CVP measurements may be helpful to support & guide fluid management
Measured through a central line & measures right atrial pressure
There are no valves between right atria & superior vena cava so pressure measured at tip of catheter is a measure of right atrial pressure
Right atrial pressure is an indirect measurement of right ventricular preload
Helps to assess cardiac function & venous return to heart
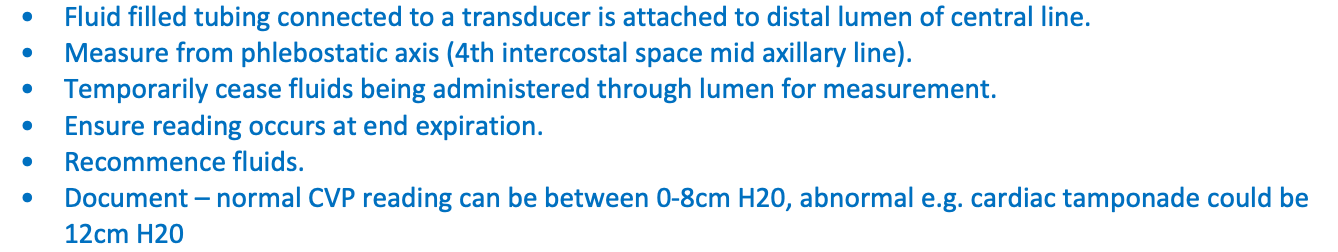
Measuring CVP:

Fluid filled tubing connected to a transducer is attached to distal lumen of central line.
Measure from phlebostatic axis (4th intercostal space mid axillary line).
Temporarily cease fluids being administered through lumen for measurement.
Ensure reading occurs at end expiration.
Recommence fluids.
Document – normal CVP reading can be between 0-8cm H20, abnormal e.g. cardiac tamponade could be 12cm H20
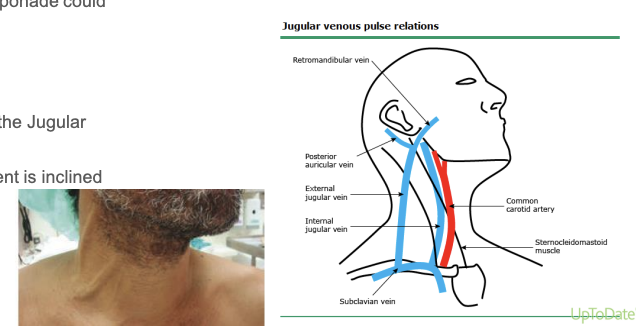
Jugular Venous Pressure (JVP):

Non-invasive evaluation of central venous pressure (CVP) can be achieved by assessing Jugular Venous Pressure (JVP)
Elevated CVP will present clinically as a pulsation of internal jugular vein when a patient is inclined at 45 degrees; however, it can be noted in an upright patient in severe cases.
Elevated JVP readings can indicate heart failure & fluid overload needing diuresis
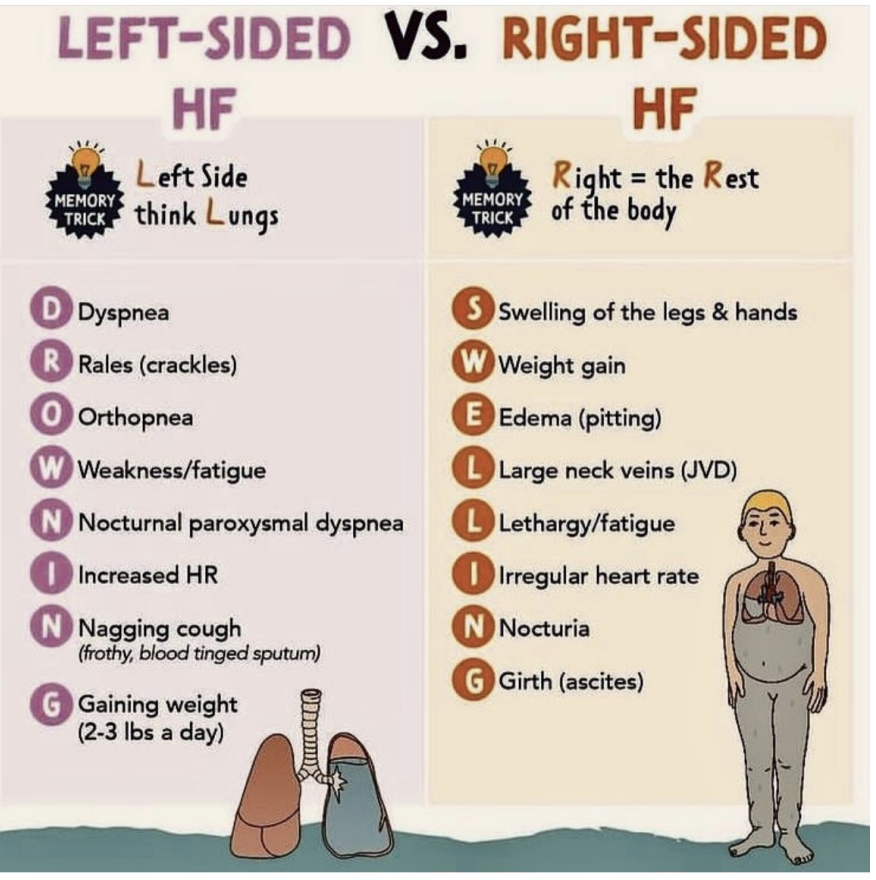
Discuss complex perfusion dysfunction and nursing management for patients with heart failure.

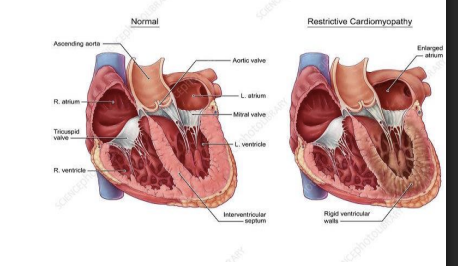
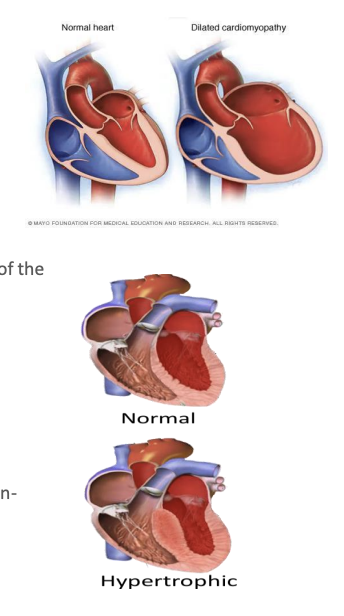
Cardiomyopathy (CMP)
Dilated CMP
Hypertrophic CMP
Restrictive CMP
Heart Failure
Left side heart failure
Right-sided heart failure
Management options and nursing care:
Treatment of underlying cause
Nitrates
Beta adrenergic blockers antiarrhythmics
ACE inhibitiors
Diuretics
Ventricular assist device
Implantable cardioverter/defibrillator
Surgical – Heart Transplantation
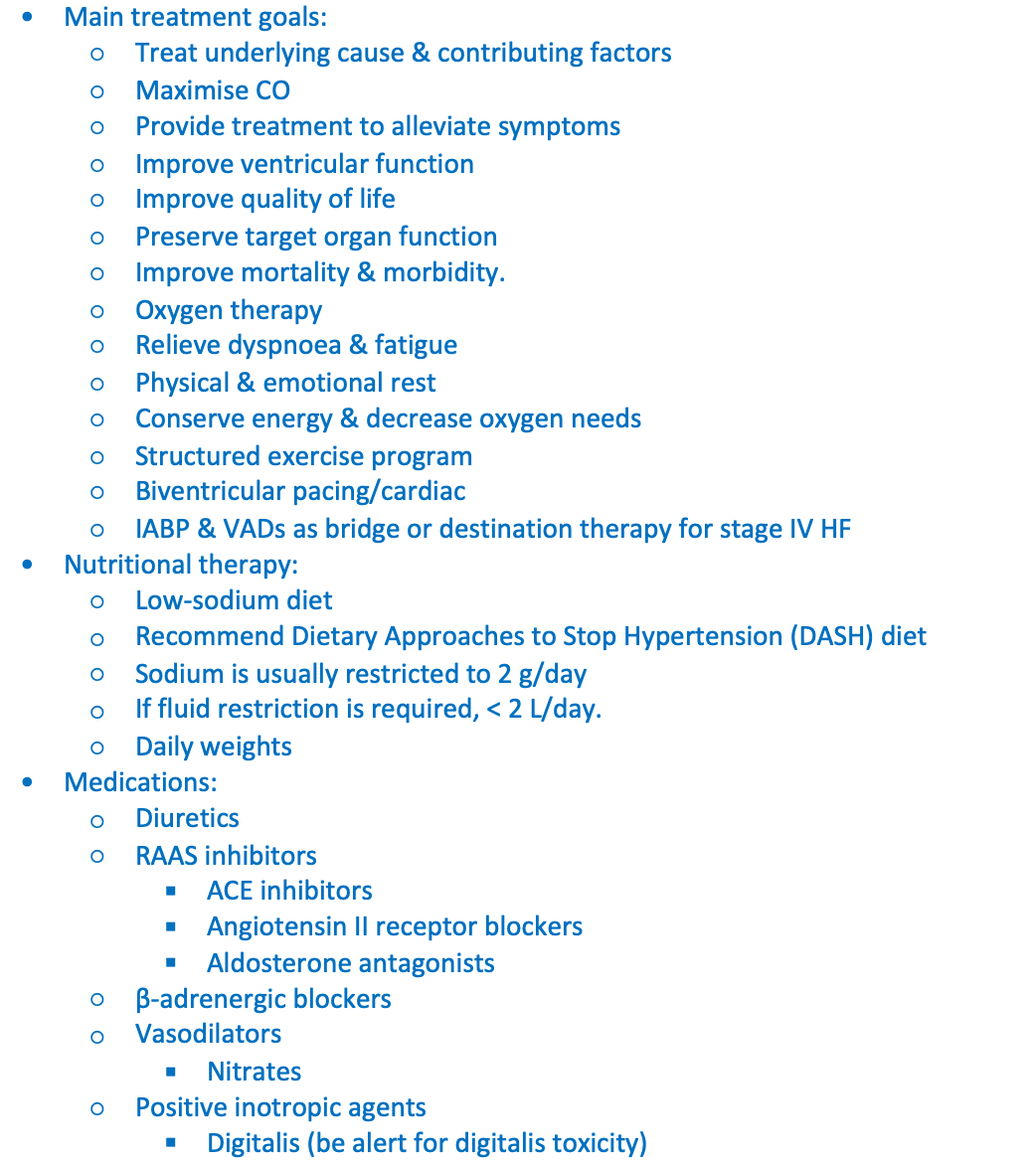
Management of heart failure:

Main treatment goals:
Treat underlying cause & contributing factors
Maximise CO
Provide treatment to alleviate symptoms
Improve ventricular function
Improve quality of life
Preserve target organ function
Improve mortality & morbidity.
Oxygen therapy
Relieve dyspnoea & fatigue
Physical & emotional rest
Conserve energy & decrease oxygen needs
Structured exercise program
Biventricular pacing/cardiac
IABP & VADs as bridge or destination therapy for stage IV HF
Nutritional therapy:
Low-sodium diet
Recommend Dietary Approaches to Stop Hypertension (DASH) diet
Sodium is usually restricted to 2 g/day
If fluid restriction is required, < 2 L/day.
Daily weights
Medications:
Diuretics
RAAS inhibitors
ACE inhibitors
Angiotensin II receptor blockers
Aldosterone antagonists
β-adrenergic blockers
Vasodilators
Nitrates
Positive inotropic agents
Digitalis (be alert for digitalis toxicity)
Tetralogy of Fallot
complex congenital heart defect that consists of four anatomical abnormalities:
Ventricular septal defect (VSD): A hole between the right and left ventricles.
Pulmonary stenosis: Narrowing of the pulmonary valve and artery, reducing blood flow to the lungs.
Overriding aorta: The aorta is positioned above the VSD, receiving blood from both ventricles.
Right ventricular hypertrophy: Thickening of the right ventricle muscle due to increased workload.
Clinical Features
Cyanosis: Bluish skin, lips, and nails due to low oxygen levels.
"Tet spells": Sudden episodes of deep blue skin, nails, and lips after crying, feeding, or agitation (caused by a sudden drop in oxygen).
Poor feeding and growth (failure to thrive).
Clubbing: Enlargement of fingers and toes.
Murmurs: Heart murmurs heard during auscultation.
Blood transfusion indications:

Blood loss (trauma, surgery, haemorrhage)
Severe anaemia
Replacement of fluid & protein
Restoration of oncotic pressure
Replacement essential clotting factors
Blood grouping and matching:

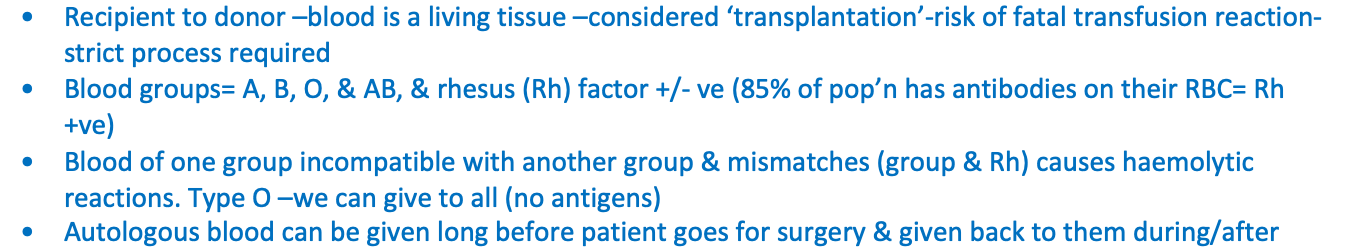
Recipient to donor –blood is a living tissue –considered ‘transplantation’-risk of fatal transfusion reaction-strict process required
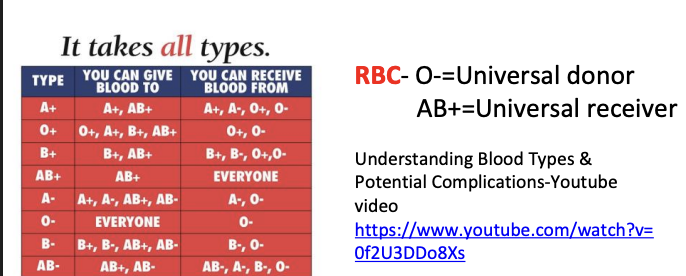
Blood groups= A, B, O, & AB, & rhesus (Rh) factor +/- ve (85% of pop’n has antibodies on their RBC= Rh +ve)
Blood of one group incompatible with another group & mismatches (group & Rh) causes haemolytic reactions. Type O –we can give to all (no antigens)
Autologous blood can be given long before patient goes for surgery & given back to them during/after
Before requesting issue of a blood product or collecting the blood product, clinical staff must check the following:

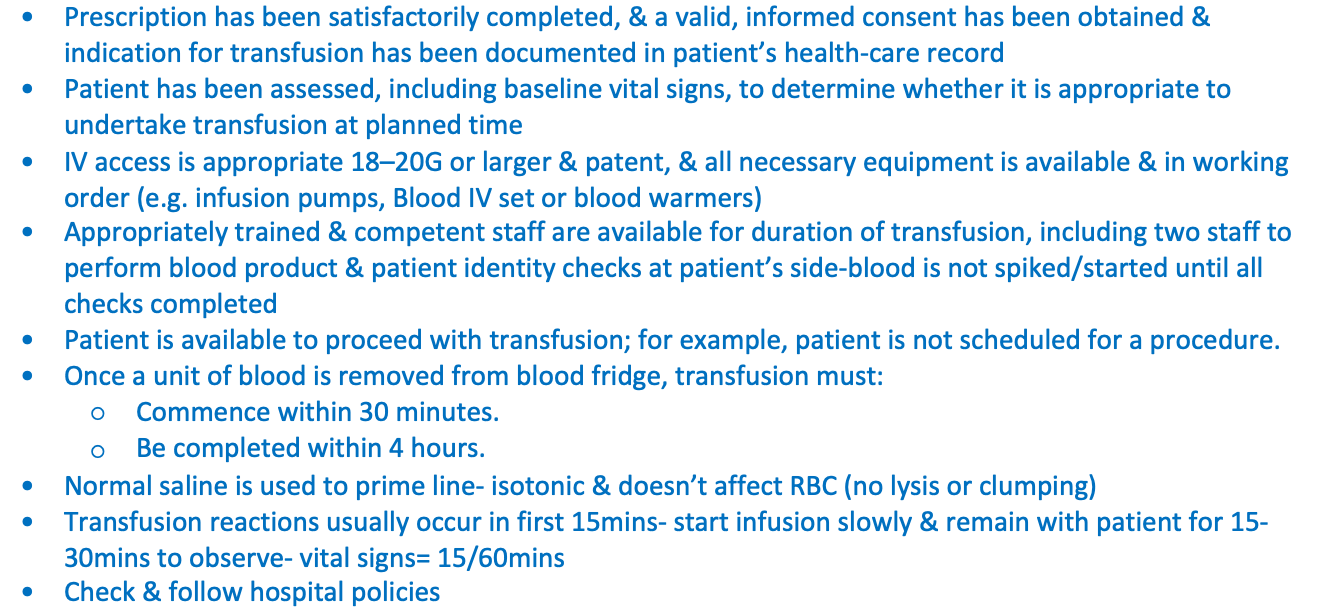
Prescription has been satisfactorily completed, & a valid, informed consent has been obtained & indication for transfusion has been documented in patient’s health-care record
Patient has been assessed, including baseline vital signs, to determine whether it is appropriate to undertake transfusion at planned time
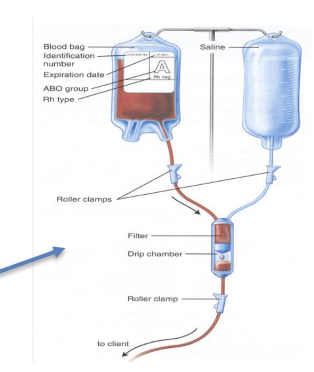
IV access is appropriate 18–20G or larger & patent, & all necessary equipment is available & in working order (e.g. infusion pumps, Blood IV set or blood warmers)
Appropriately trained & competent staff are available for duration of transfusion, including two staff to perform blood product & patient identity checks at patient’s side-blood is not spiked/started until all checks completed
Patient is available to proceed with transfusion; for example, patient is not scheduled for a procedure.
Once a unit of blood is removed from blood fridge, transfusion must:
Commence within 30 minutes.
Be completed within 4 hours.
Normal saline is used to prime line- isotonic & doesn’t affect RBC (no lysis or clumping)
Transfusion reactions usually occur in first 15mins- start infusion slowly & remain with patient for 15- 30mins to observe- vital signs= 15/60mins
Check & follow hospital policies
Reactions - refer to hosp clinical practice guidelines

Clinical Signs | Nursing Intervention |
| (incompatibility) Stop transfusion & ring for RMO! Monitor obs & FBC, urinalysis. Check blood pack & paperwork for discrepancies. Send remaining blood & lines to lab. Infuse NaCl with new lines. CALL MET if meets criteria. Document! (incident report, Progress notes) |
|
|
Febrile Reaction: Febrile, chills, warm, flushed skin, headache, anxiety, muscle pain. | (incompatibility) Stop transfusion & ring for RMO! Give antipyretics as ordered. Keep vein open with normal saline. |
Fluid overload/circulatory overload: Dyspnoea, chest pain, anxiety, diaphoresis, blood tinged sputum, fine crackles on auscultation of the chest | Stop transfusion Notify medical staff-frequent obs, check medication chart for frusemide to be given between units, FBC, nursing care as per fluid overload |
Discuss nursing management of post operative patients undergoing gastrointestinal surgery

Nursing management:
Post op movement/activity/mobilisation –often improves return of gastrointestinal function- from ‘gas cramps’-abdominal distension & loss of bowel sounds –slowed GI function from surgery or handling of bowel in surgery
Fluids- IV post op- patients often dehydrated- NBM, fluid loss during surgery, renal retention of sodium & water from stress. Strict FBC important post op- IV continues until fluids by mouth to maintain FBC
FBC includes all intake (e.g. IV, blood, volume expanders, oral, & enteral fluids) & output (drainage, stoma, vomitus, NGT output, bladder irrigations & urine). Note drainage changes- e.g. new bleeding, bile- may detect abnormality- e.g. breakdown of anastomosis
PONV- note factors = anaesthetic, opioids, hypotension, abdo surgery, female more likely, non-smoker, history of migraines or previous PONV (post-operative nausea & vomiting)
Antiemetics- 5-HT3 receptor antagonist (Serotonin) is first line of choice e.g. ondansetron. Dopamine antagonists- metoclopramide. H1 antihistamines can be used- promethazine, hyoscine can be used in vestibular disturbances such as motion sickness
Oral fluids used cautiously post op-to reduce risk of lung injury (aspiration)-ice chips used first- then sips of h20-avoid straw (more air into stomach), then clear fluids, then normal diet in steps. Chewing gum may help- but with caution, crackers
Diet –high protein= (tissue repair & healing), high carbohydrate (energy & vitamins C & D for tissue formation)-may need dietitian support for supplementary drinks or feeding
NGT – used to decompress stomach post GI surgery (prevents abdo distension), & may prevent PONV- remains insitu until peristalsis returns (bowel sounds & tolerating diet)-note if on straight drainage vs stopper
Bowel care- sluggish post op due to: fasting, dehydration, medications, bowel manipulation. If bowel sounds, & flatus returns –positive sign of peristalsis – oral intake could resume (if medical staff approve). May take 2-3 days before normal bowel function returns for patient. Note pain with incisions- patient may be reluctant to bear down with bowel motion with pain- management important-splinting wound, bowel care=stool softeners, laxatives (glycerin suppositories), microlax enemas if needed
Some diagnostic procedures (colonoscopy, sigmoidoscopy) require bowel cleansing & fasting e.g. golytely, glycoprep, Movicol, or picolax prior to procedure-some of these also used for faecal impaction…
Post op nausea & vomiting (PONV

Negative effects can include: wound dehiscence, oesophageal rupture, aspiration, dehydration, increased intracranial pressure (when you Valsalva blood goes into your brain), & pneumothorax.
Causes: Pain, abdominal distension, ingesting food or fluids before return of peristalsis, certain medications, anxiety
Signs: Complaints of feeling sick to the stomach, retching or gagging
Preventative management: IV fluids until peristalsis returns (bowel sound); then clear fluids, full fluids & regular diet; anti-emetic drugs if ordered; analgesics for pain
Constipation

Infrequent or no stool passage for abnormal length of time (e.g. within 48 hours after solid diet started)
Causes: Lack of dietary roughage, analgesics (decreased intestinal motility), immobility
Signs: Absence of stool elimination, abdominal distension & discomfort
Preventative management: Adequate fluid intake, high fibre diet, early ambulation
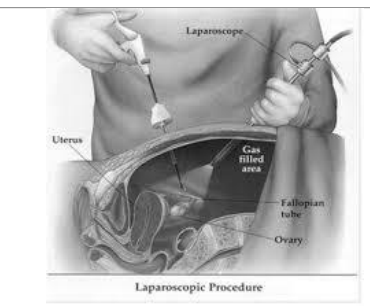
Abdominal distension (gas)

Retention of gases within intestines. Note some abdominal procedures e.g. laparoscopy instills CO2 into abdo to expand & to visualize structures (insufflation)-can also irritate phrenic nerve – referred pain in shoulder & chest
Causes: Slowed motility of intestines due to handling of bowel during surgery & effects of anaesthetic
Signs: Obvious abdominal distension, abdominal discomfort (gas pains), absence of bowel sounds
Preventative management: Early ambulation; avoid using a straw, provide ice chips or water at room temperature
Paralytic ileus

Intestinal obstruction characterized by lack of peristaltic activity
Causes: Handling bowel during surgery, anaesthetic, electrolyte imbalance, wound infection
Signs: Abdominal pain & distension; constipation; absent bowel sounds; vomiting-note could be bile looking or if severe- faecal, can be noted on Xray
Preventative management: Treat underlying causes, assess bowel sounds frequently & carefully –auscultation, assess for signs of abdominal distension above, NGT to decompress abdo distension

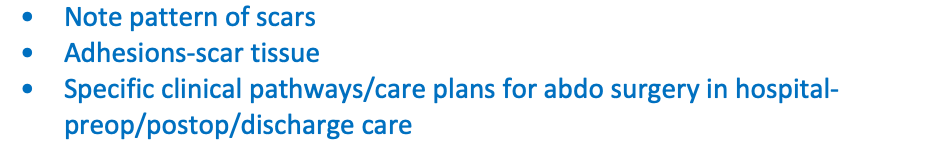
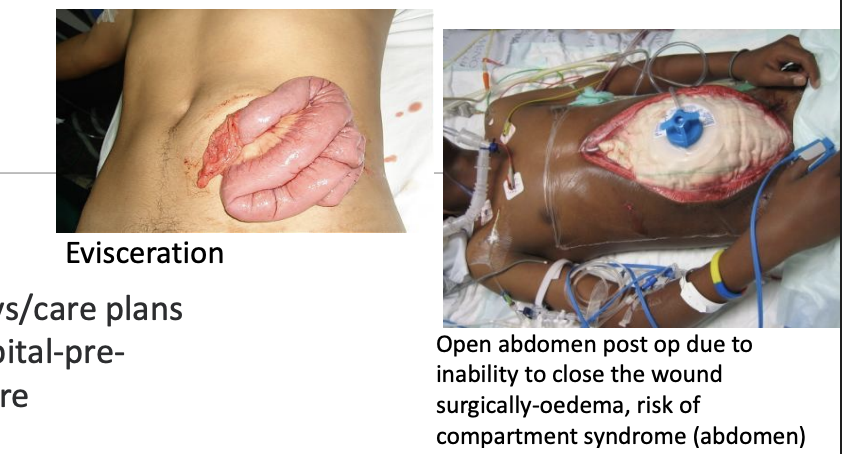
Abdominal Surgery

Note pattern of scars
Adhesions-scar tissue
Specific clinical pathways/care plans for abdo surgery in hospital-preop/postop/discharge care