Glomerular Disease
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
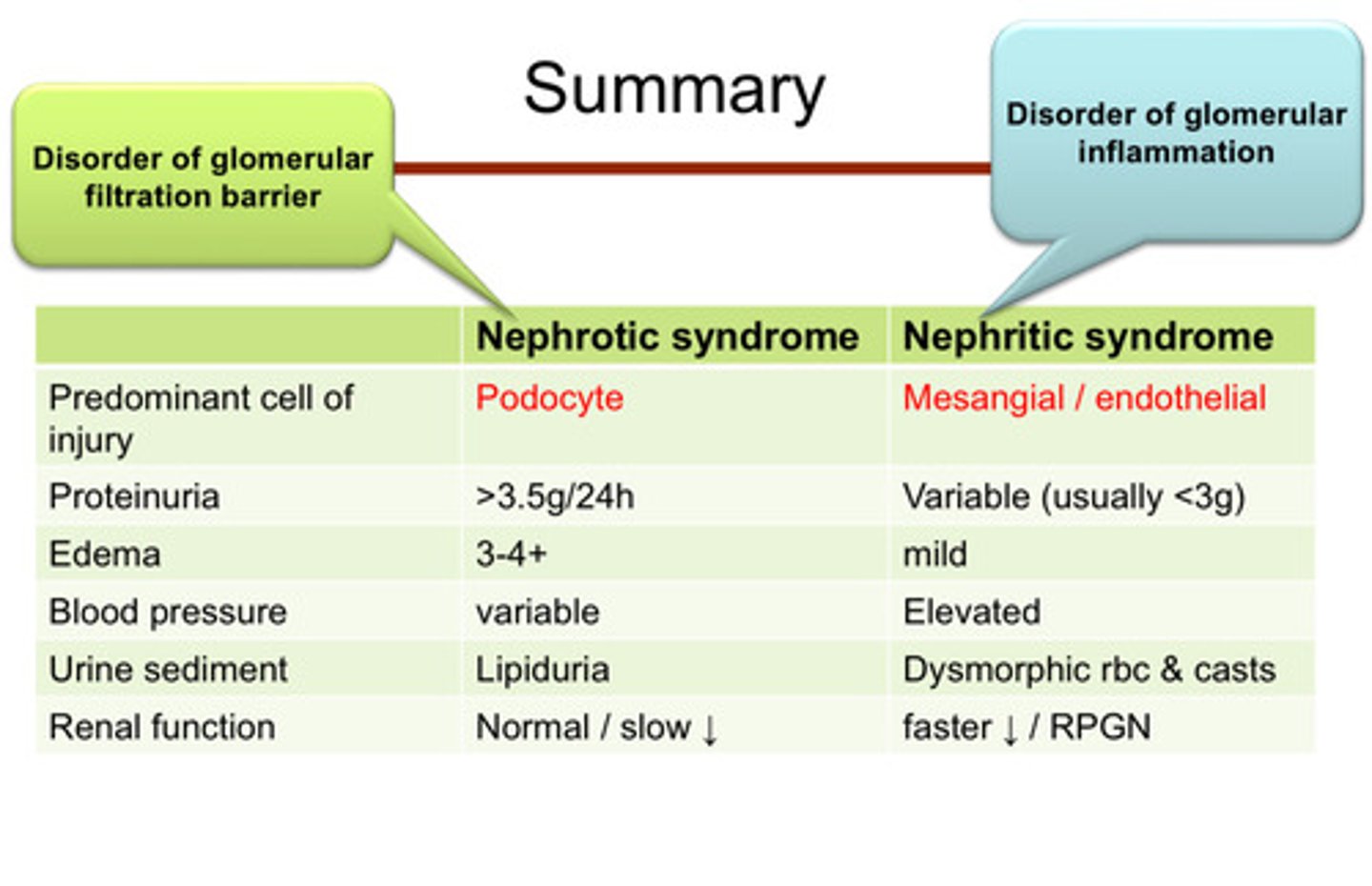
glomerular disease is categorized into what 2 kinds of syndromes?
nephrOtic syndrome and nephrItic syndrome
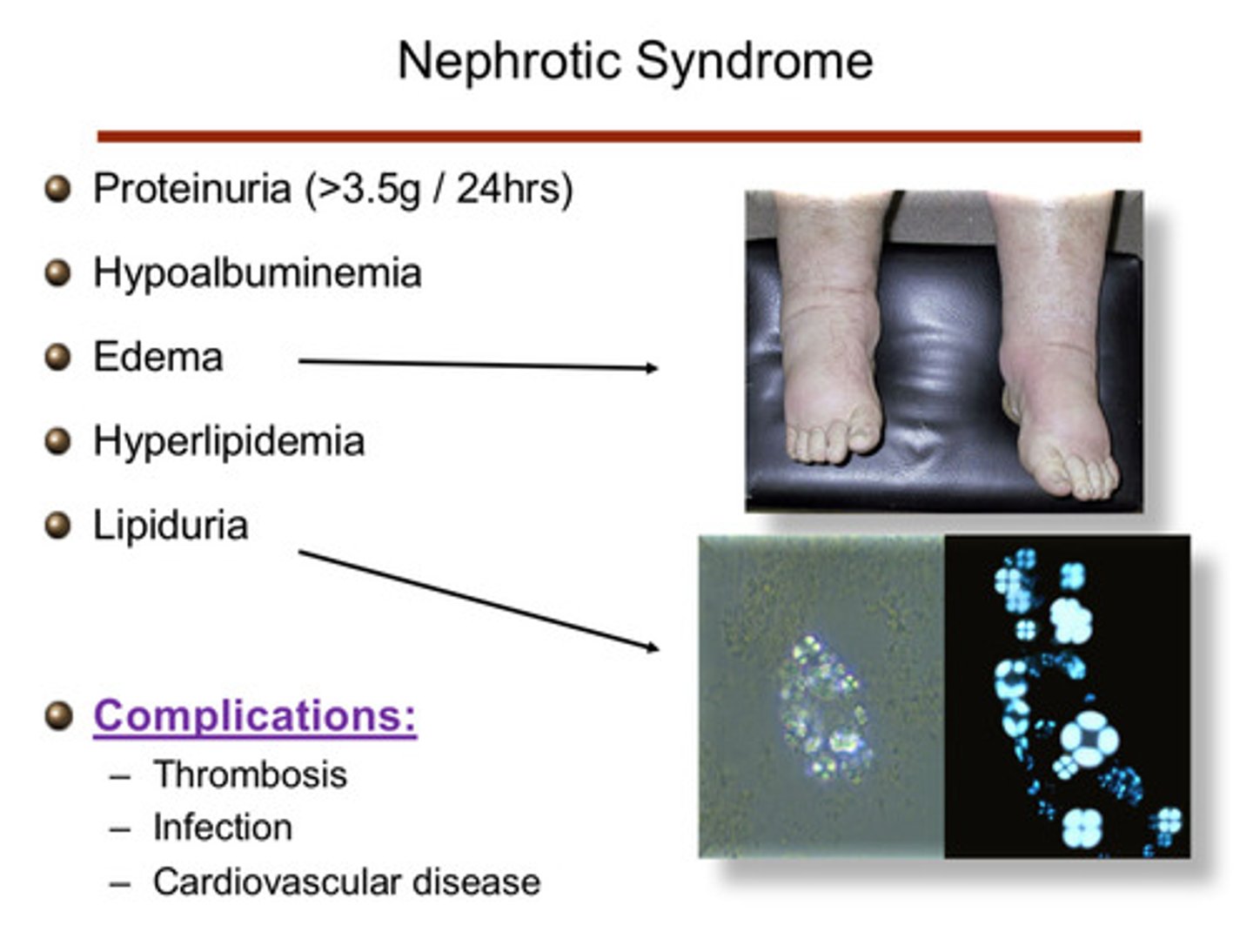
what are the characteristic features for nephrOtic syndrome? (note that it is a syndrome, not one disease) (5)
1) proteinuria (>3.5 g/24 hours)
2) hypoalbuminemia
3) edema
4) hyperlipidemia
5) lipiduria
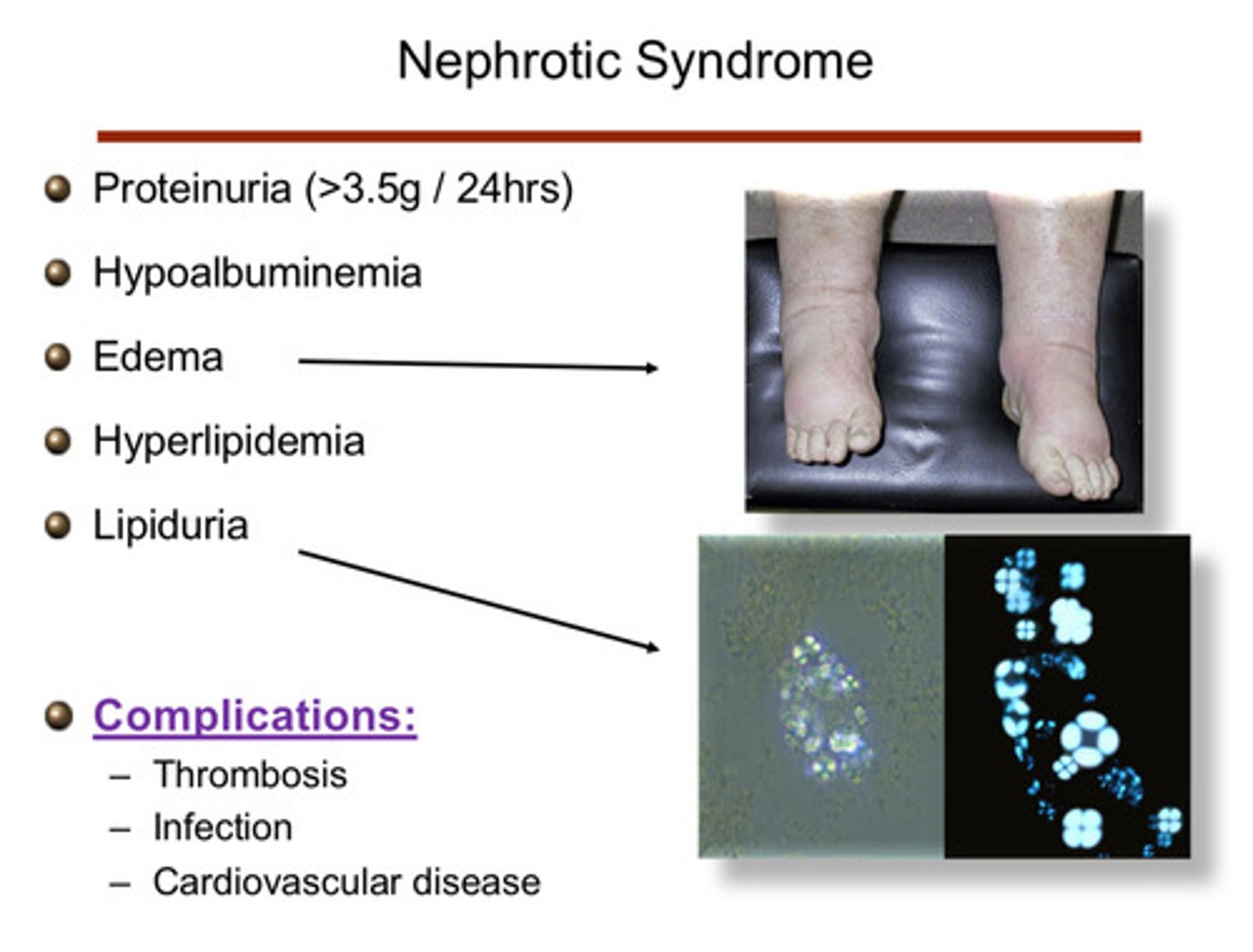
what are some complications of nephrOtic syndrome (3)
1) thrombosis
2) infection
3) CV disease
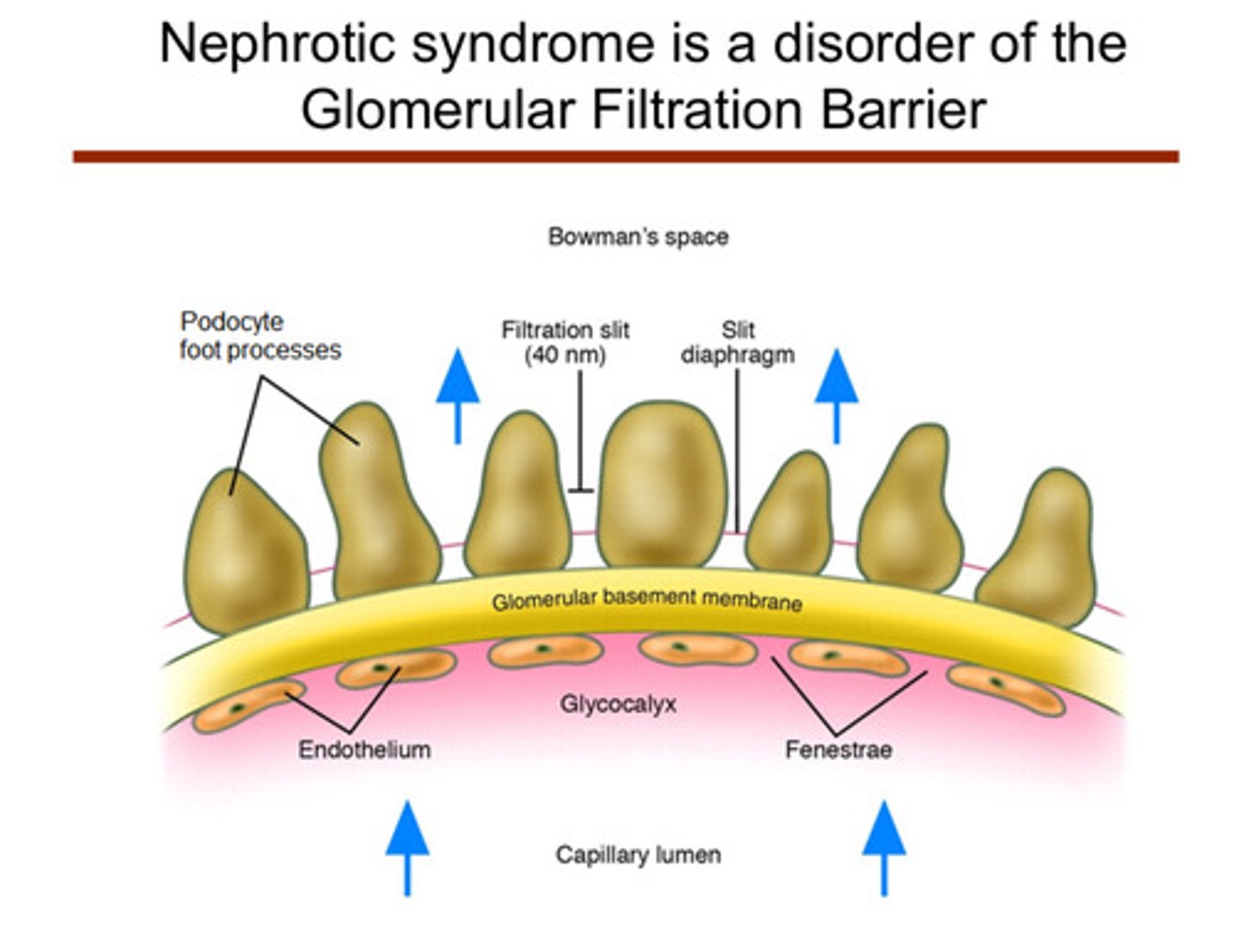
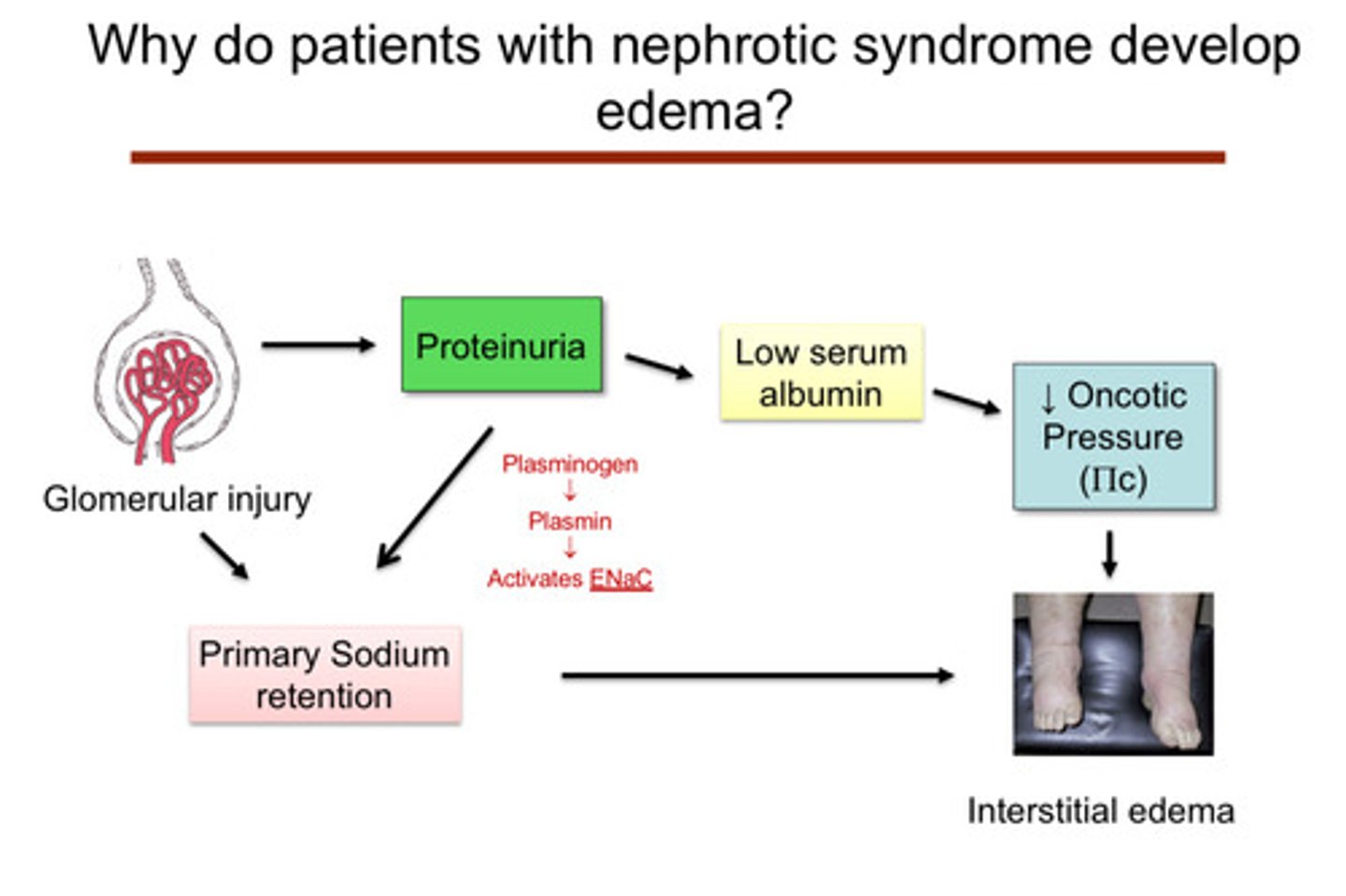
in general, what is the pathologic problem that leads to nephrotic syndrome
nephrotic syndrome is mainly a disorder of the glomerular filtration barrier
what are some things that glomerular injury can lead to in the context of nephrotic syndrome
glomerular injury can lead to:
1) proteinuria —> low serum albumin —> decreased oncotic pressure —> interstitial edema
2) proteinuria —> primary sodium retention via increased activation of ENaC by filtered plasminogen —> plasmin (not due to decreased effective arterial blood volume w activation of RAAS/SNS)
2) primary sodium retention —> interstitial edema
many diseases can cause nephrotic syndrome, both systemic diseases and diseases of the kidney itself. what are some systemic diseases that can lead to nephrotic syndrome (3)
1) diabetes
2) amyloid
3) lupus
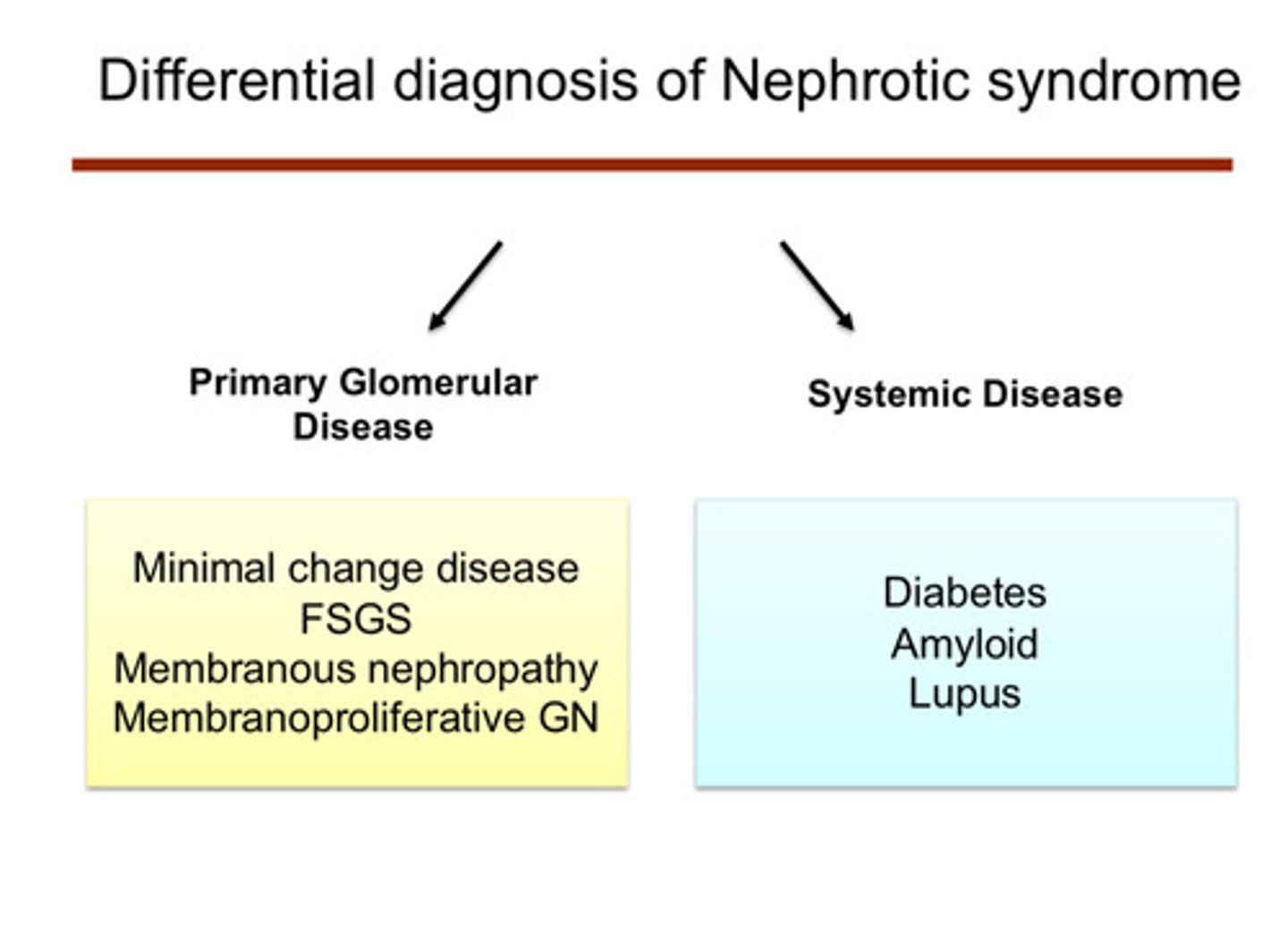
many diseases can cause nephrotic syndrome, both systemic diseases and diseases of the kidney itself. what are some glomerular diseases that can lead to nephrotic syndrome (4)
1) minimal change disease
2) FSGS (focal and segmental glomerulosclerosis)
3) membranous nephropathy
4) membranoproliferative glomerulonephritis
what is the most common cause of nephrotic syndrome?
diabetic kidney disease!
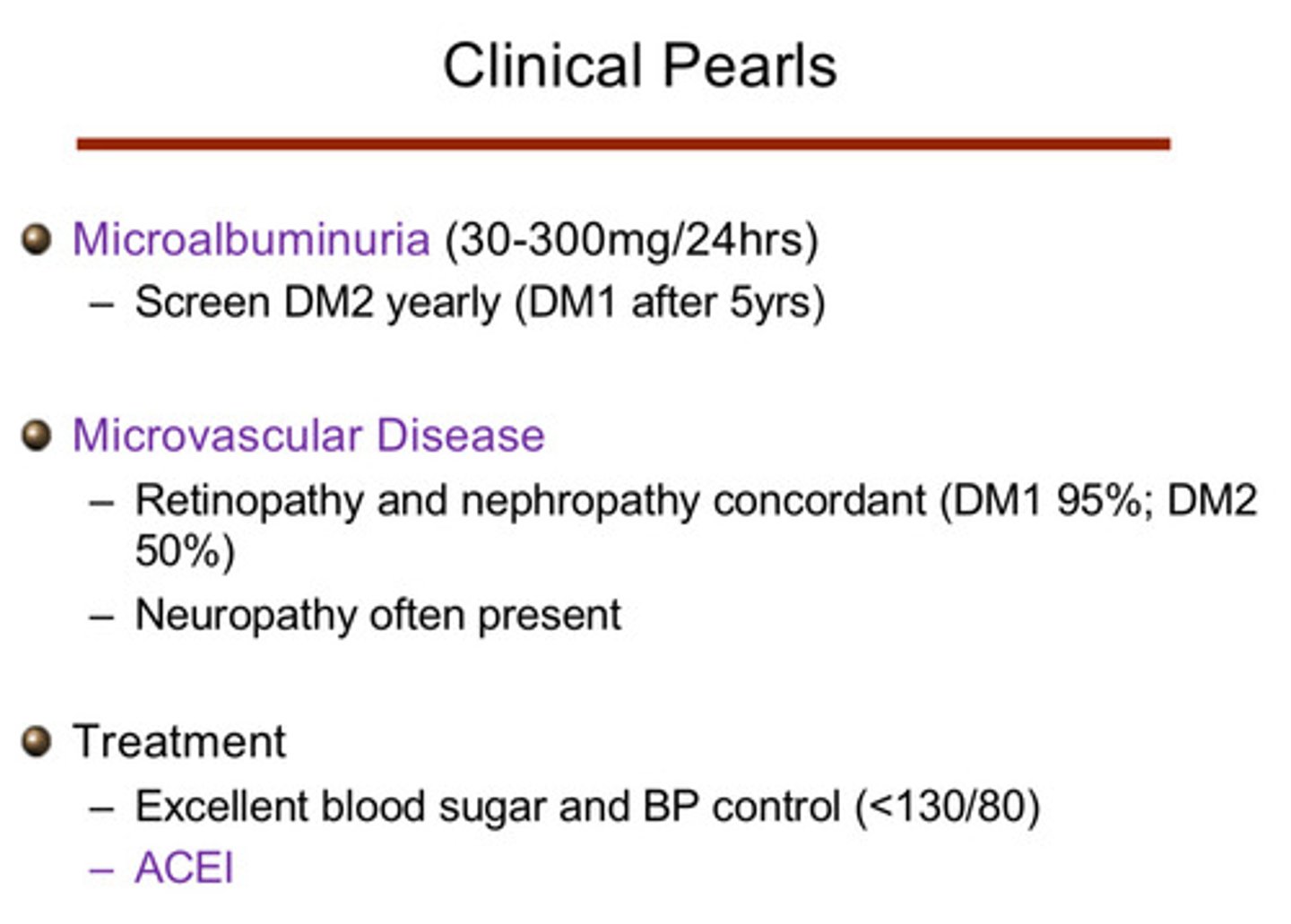
how can we screen to catch diabetic nephropathy in the early stage?
1) we can screen for microalbuminuria (30-300 mg/24 hours): screen DM2 pts yearly, screen DM1 pts after 5 years
2) we can check for microvascular disease: retinopathy and nephropathy are concordant (DM1 95%, DM2 50%); neuropathy is also often present
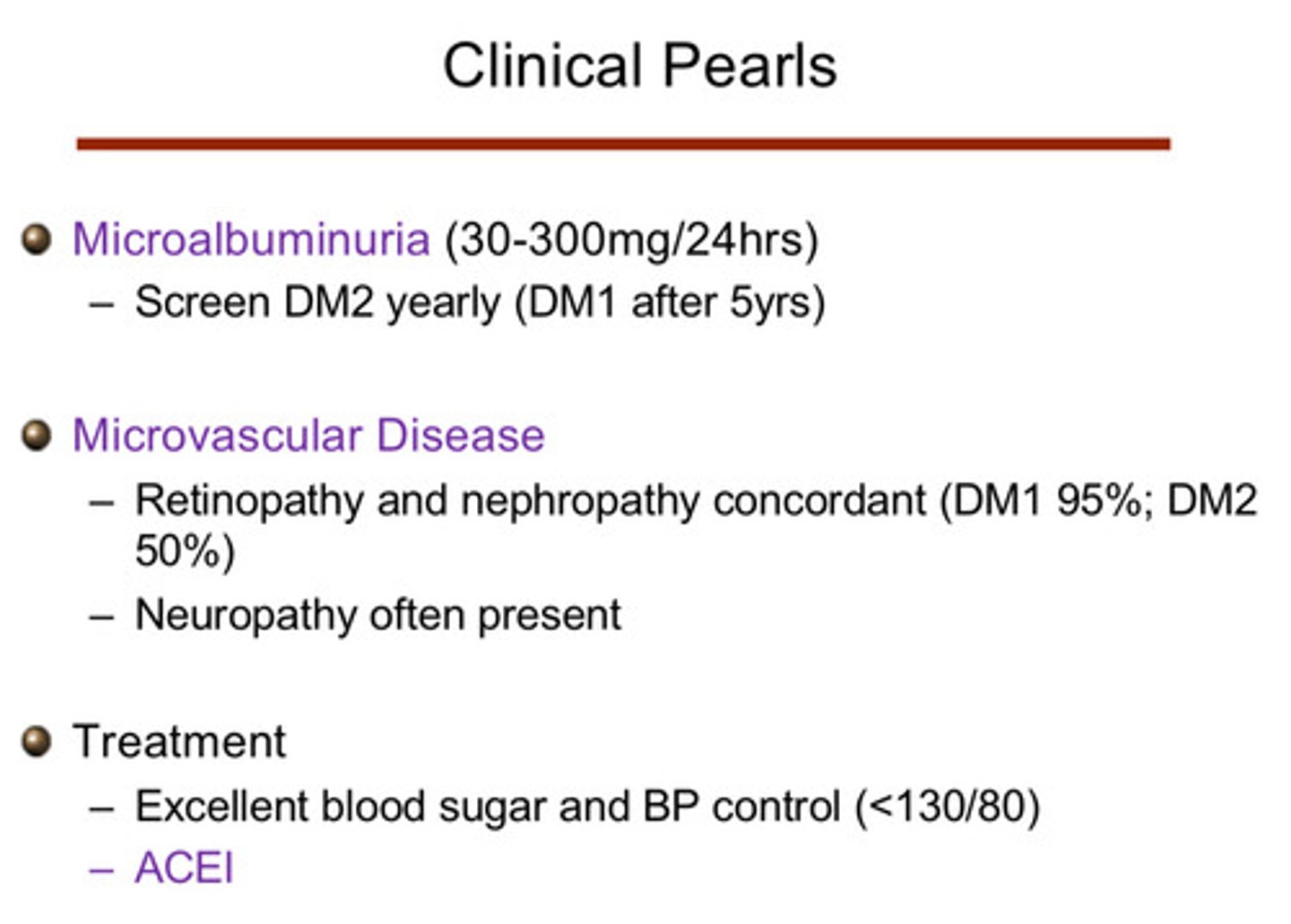
what interventions can help prevent or slow diabetic nephropathy?
1) excellent blood sugar and BP control (<130/80)
2) ACEI
what are the injuries that happen to the glomerulus with diabetes? (3)
injury to vessels unifies pathology of diabetic injury:
1) repeated bouts of capillary injury and remodeling leads to formation of Kimmelstiel-Wilson nodules (these are characteristic of diabetes)
2) arteriolar hyalinosis (small vessels) and arteriosclerosis (large vessels) are also typical
3) thickening of glomerular and tubular basement membranes can be seen via electron microscopy
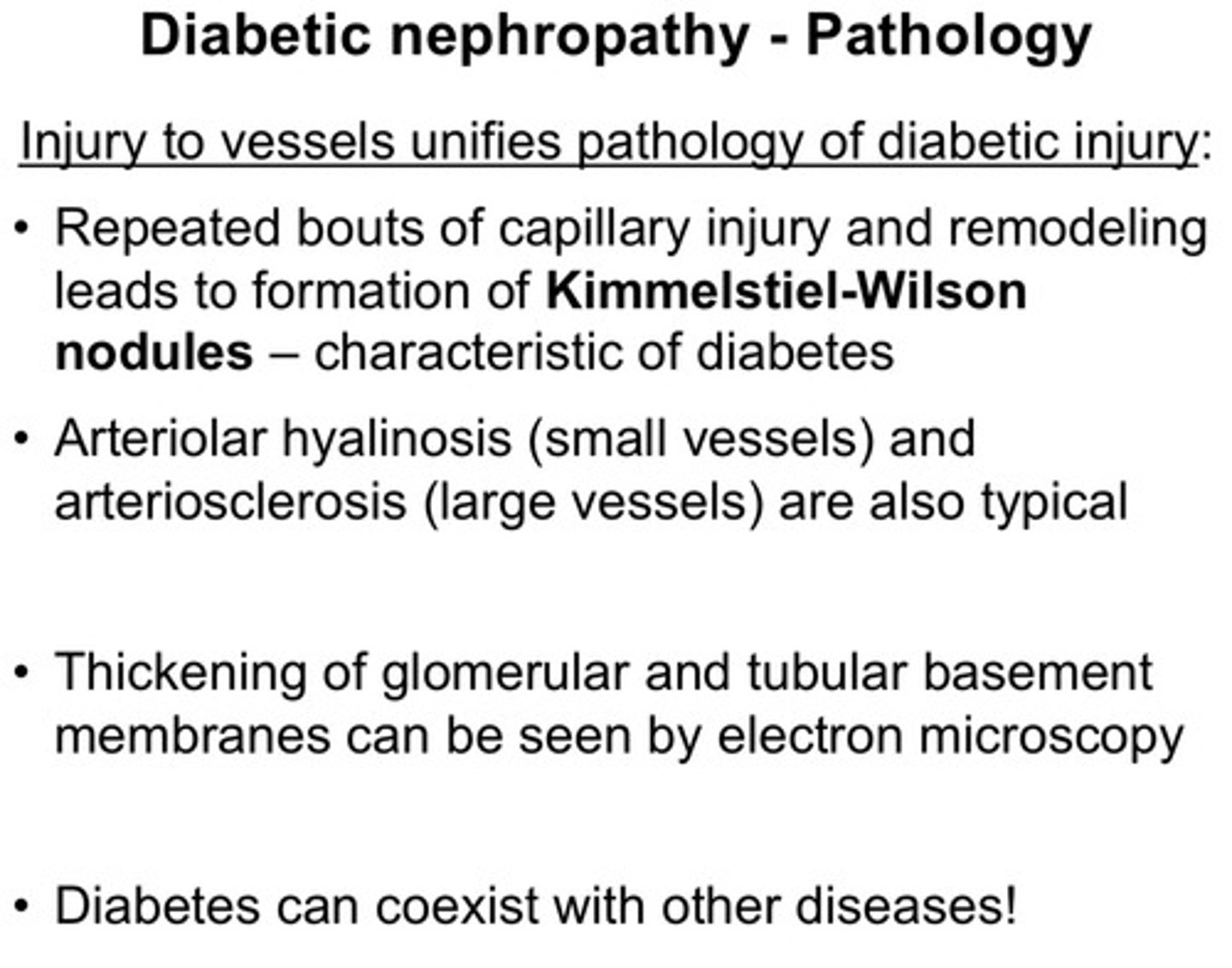
note that diabetes can coexist with ?
other diseases!
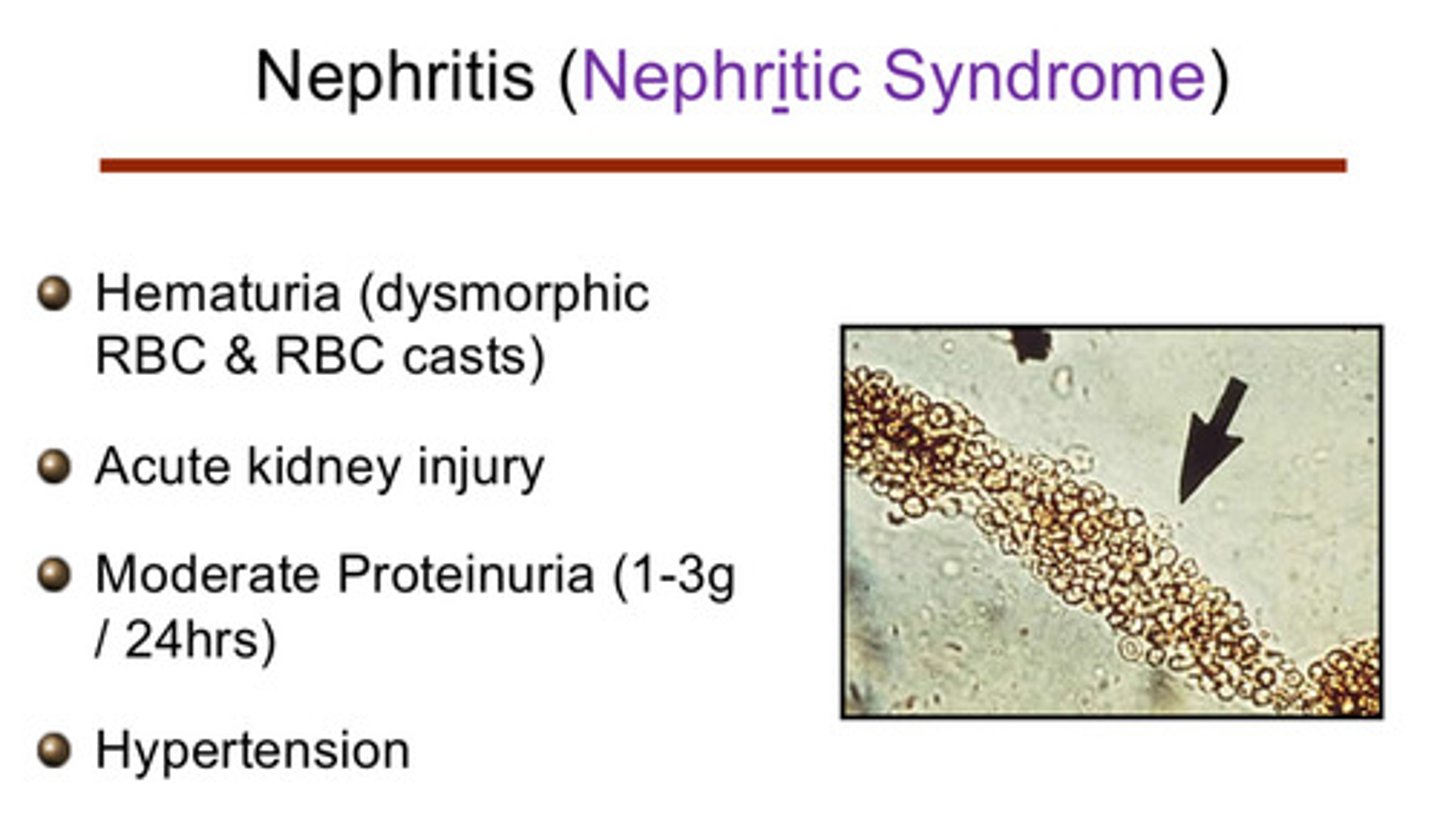
what are the characteristic findings for nephritic syndrome? (4)
1) hematuria (dysmorphic RBC and RBC casts)
2) acute kidney injury
3) moderate proteinuria (1-3 g/24 hours)
4) hypertension
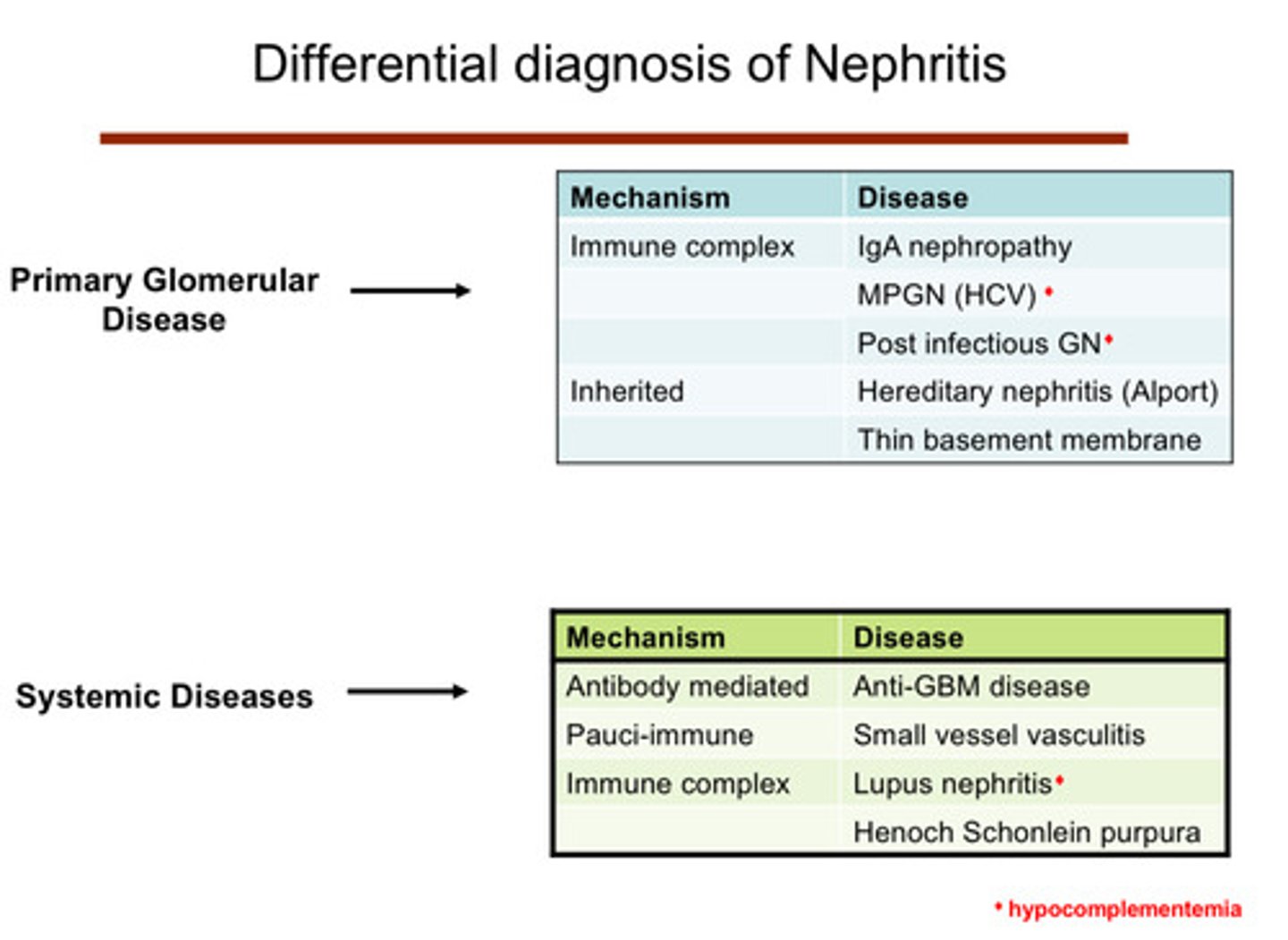
what are some systemic diseases that lead to nephritic syndromes and what are their associated mechanisms of pathology (4)
1) anti-GBM disease (anti-glomerular basement membrane): antibody mediated mechanism
2) small vessel vasculitis: pauci-immune mechanism
3) lupus nephritis (hypocomplementemia): immune complex mechanism
4) henoch schonlein purpura: immune complex mechanism
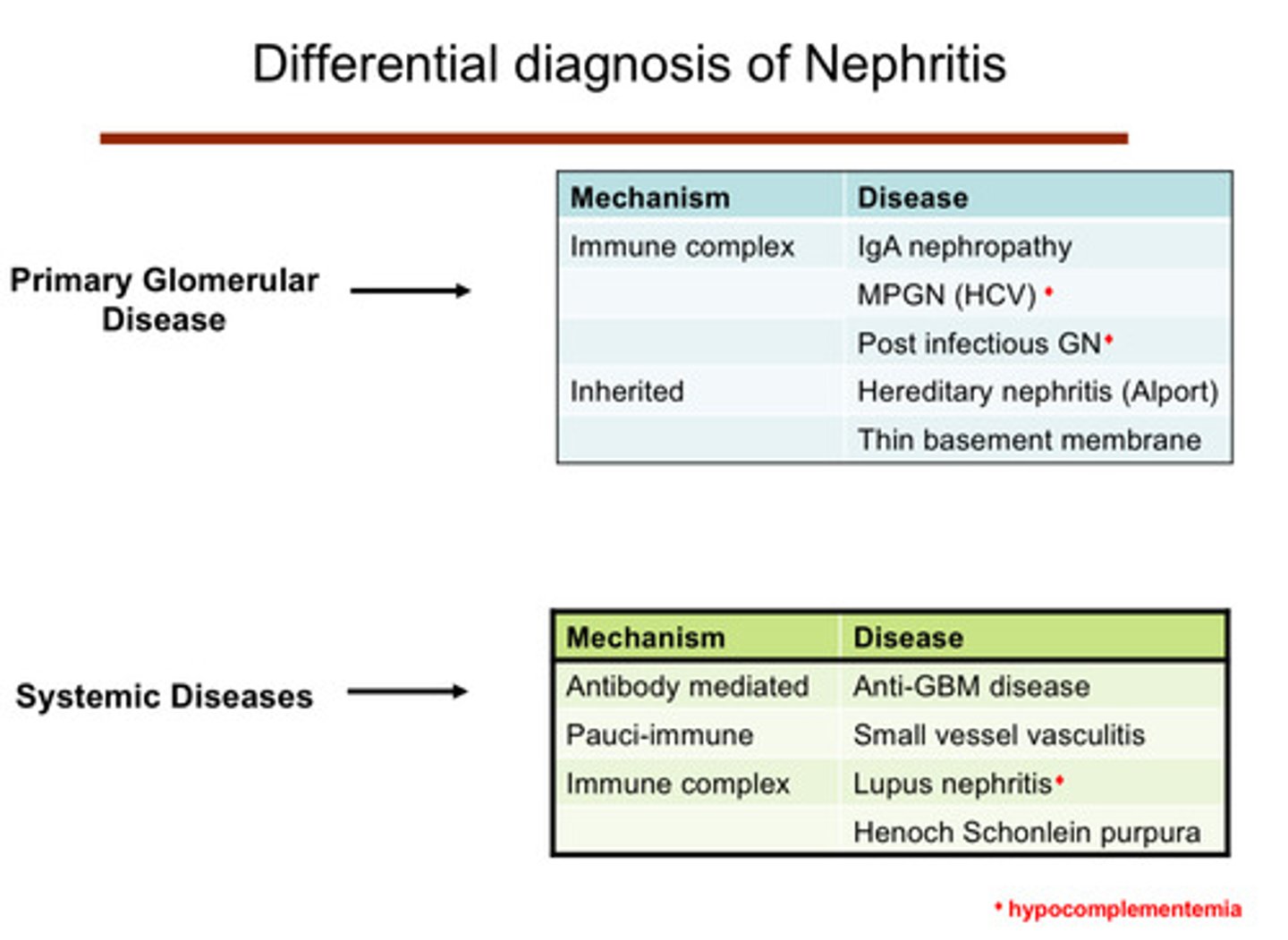
what are some glomerular diseases that lead to nephritic syndromes and what are their associated mechanisms of pathology (5)
1) IgA nephropathy: immune complex mechanism
2) membranoproliferative glomerulonephritis (MPGN): associated w Hep C virus; immune complex mechanism
3) post infectious glomerulonephritis: immune complex mechanism
4) hereditary nephritis (alport): inherited mechanism
5) thin basement membrane: inherited mechanism
what are the 5 immune complex mediated nephritic syndromes
1) IgA nephropathy
2) MPGN
3) post infectious GN
4) lupus nephritis
5) henoch schonlein purpura
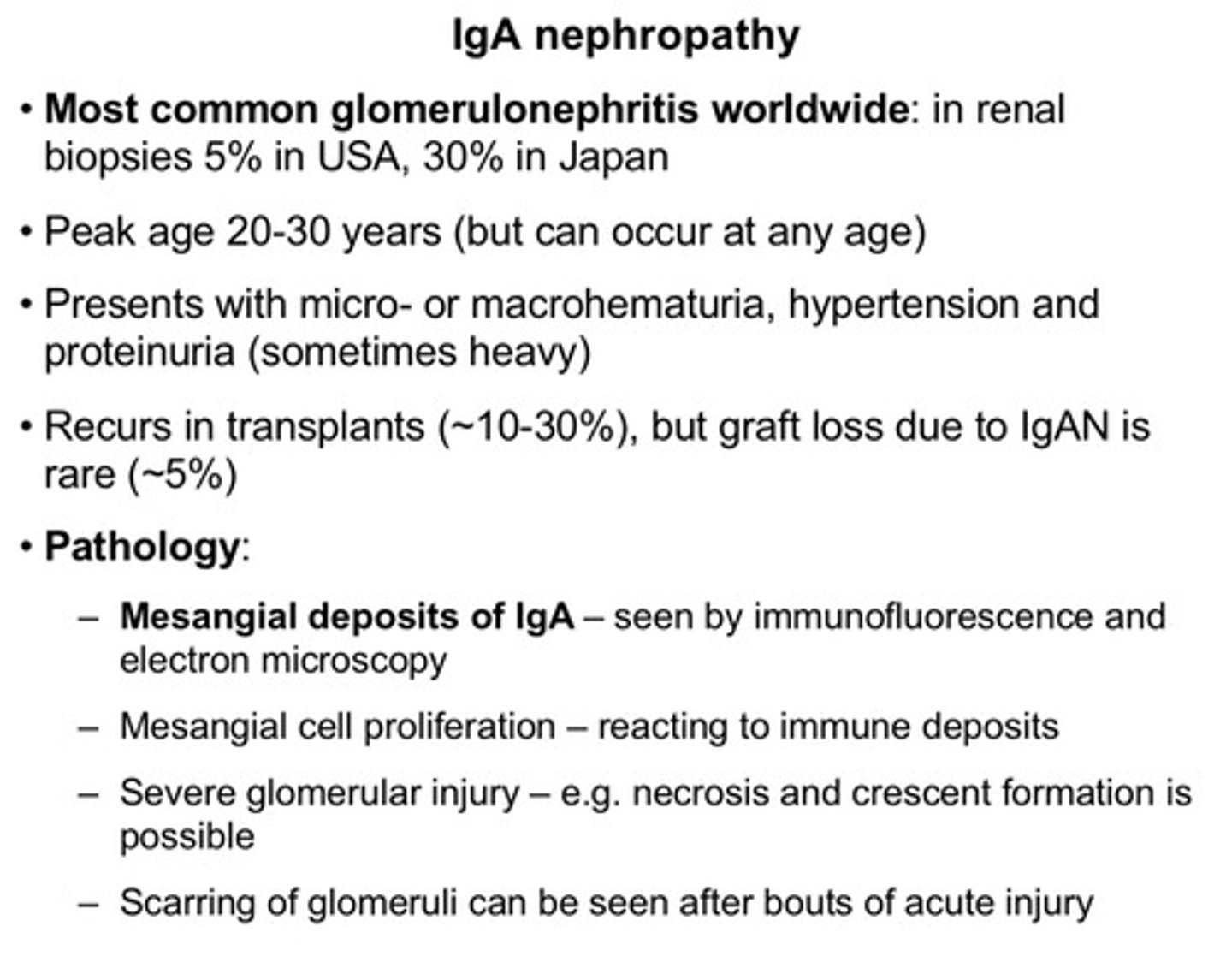
what are the clinical features of this immune complex mediated nephritic syndrome: IgA nephropathy
1) most common glomerulonephritis worldwide
2) peak age 20-30 yrs (but can occur at any age)
3) presents with micro- or macrohematuria, hypertension, and proteinuria (sometimes heavy)
4) recurs in transplants (10-30%), but graft loss due to IgA nephropathy is rare (5%)
5) pathology wise: we can see mesangial deposits of IgA, mesangial cell proliferation (reacting to immune deposits), severe glomerular injury (eg: necrosis or crescent formation), scarring of glomeruli can be seen after bouts of acute injury
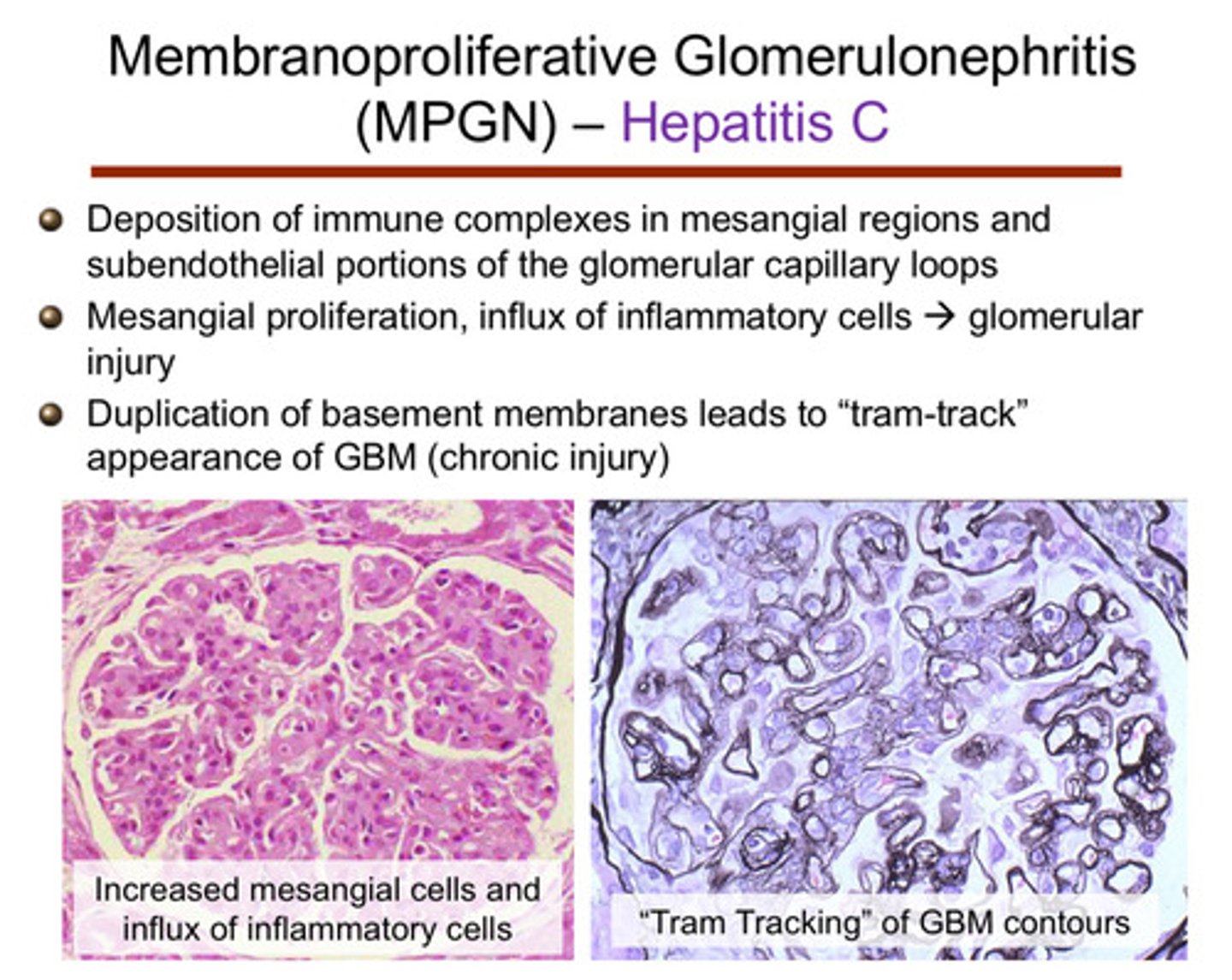
what are the clinical features of this immune complex mediated nephritic syndrome: MPGN
1) deposition of immune complexes in mesangial region and subendothelial portions of the glomerular capillary loops
2) mesangial proliferation, influx of inflammatory cells —> glomerular injury
3) duplication of basement membrane leads to a "tram-track" appearance of the glomerular basement membrane (chronic injury)
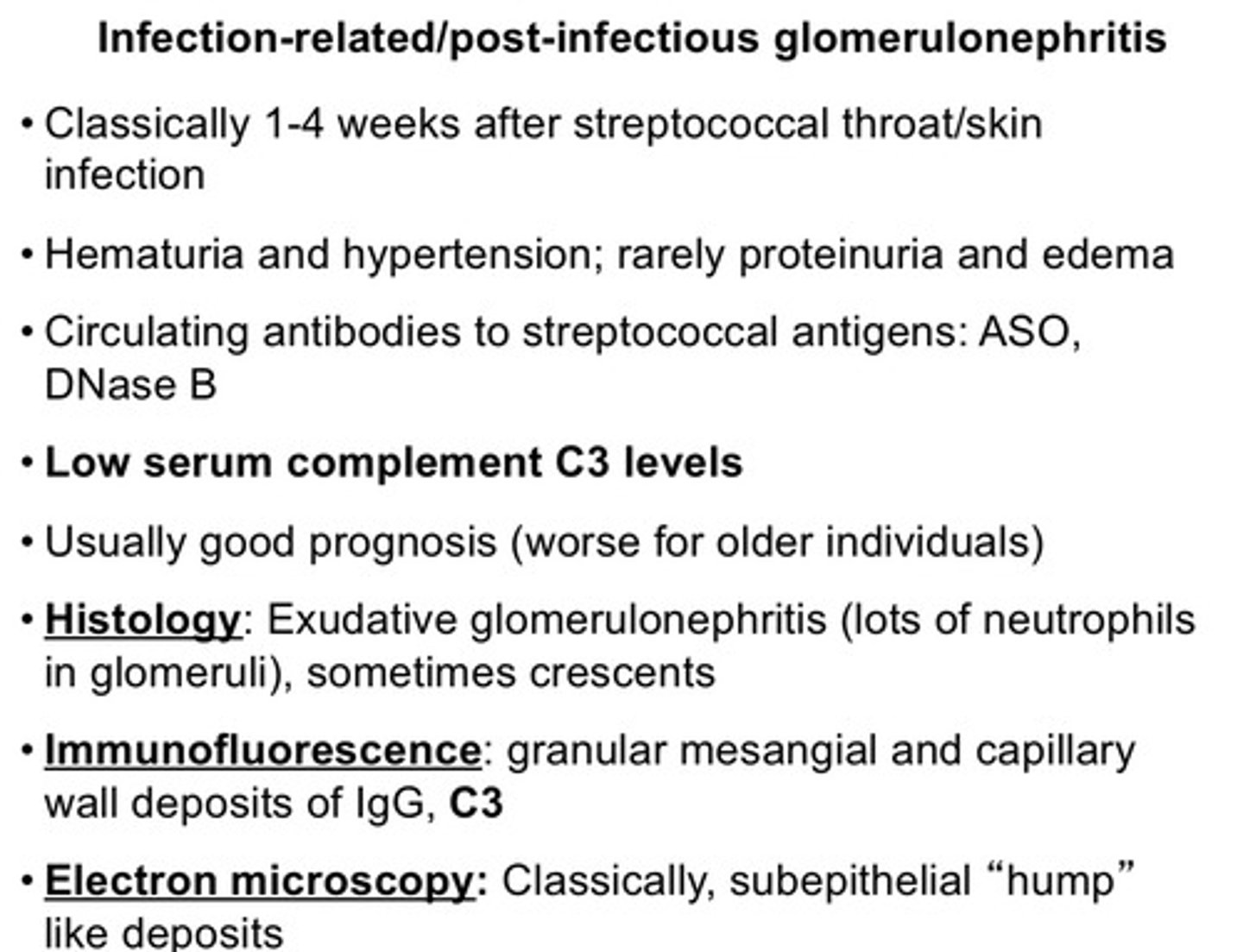
what are the clinical features of this immune complex mediated nephritic syndrome: post infectious GN
1) classically 1-4 weeks after streptococcal throat/skin infection
2) hematuria and hypertension; rarely proteinuria and edema
3) circulating antibodies to streptococcal antigens: ASO, DNase B
4) low serum complement C3 levels
5) usually good prognosis (worse for older individuals)
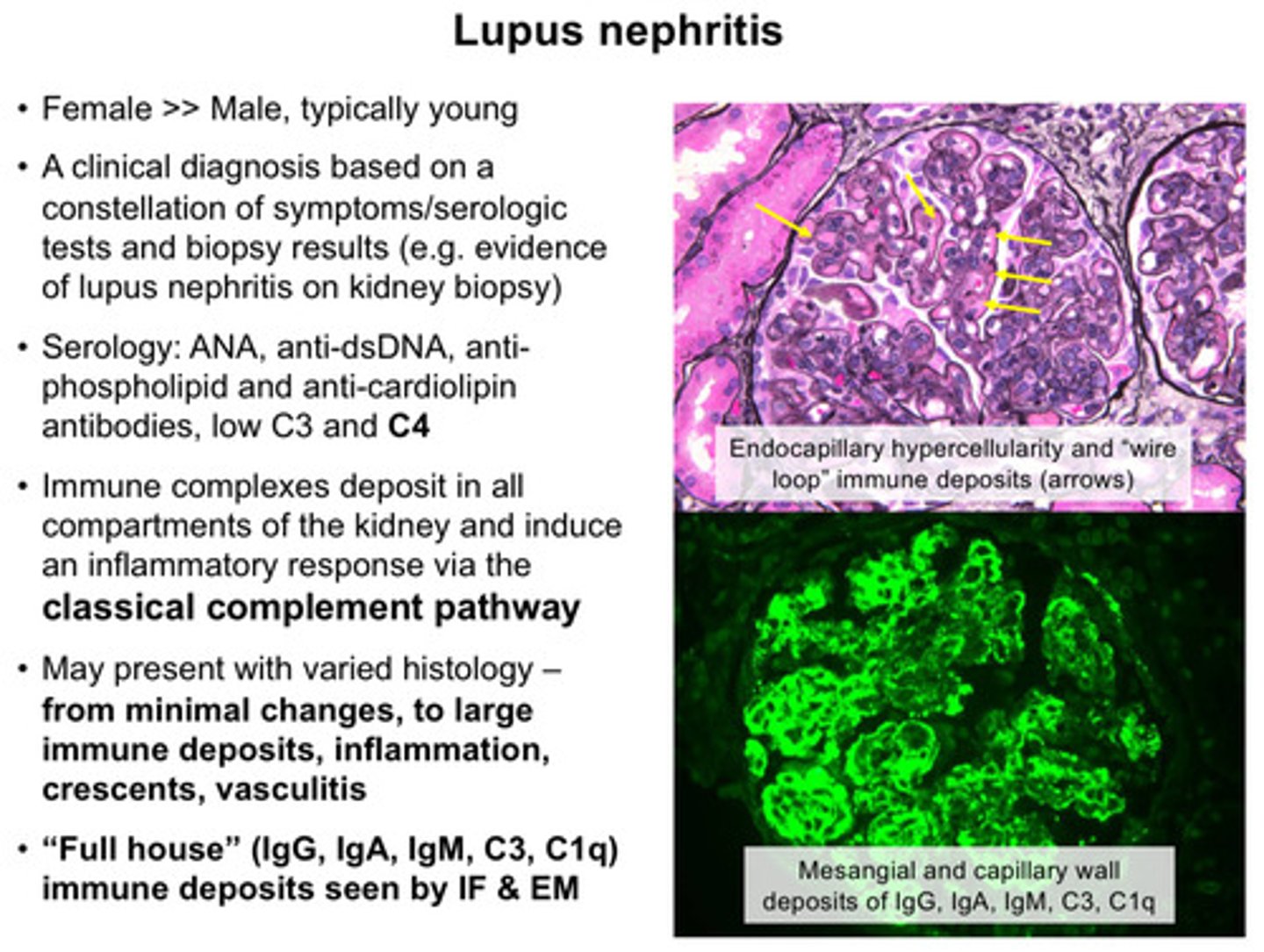
what are the clinical features of this immune complex mediated nephritic syndrome: lupus nephritis
1) female > male; typically young
2) clinical diagnosis is based on a constellation of symptoms/serologic tests and biopsy results (eg: evidence of lupus nephritis on kidney biopsy)
3) serology: ANA, anti-dsDNA, antiphospholipid and anti-cardiolipin antibodies, low C3 and C4
4) immune complexes deposit in all compartments of kidney and induce an inflammatory response via the classical complement pathway
5) may present with varied histology: from minimal changes, to large immune deposits, inflammation, crescents, vasculitis
what is RPGN?
a clinical syndrome (subcategory of nephritis) that is characterized by rapid loss of kidney function over days to weeks, typically with evidence of glomerular injury (also defined by presence of crescent formation in most glomeruli on kidney biopsy)
RPGN often presents with lung involvement, called what?
pulmonary renal syndrome
what are the general characteristics of RPGN
1) rapidly declining kidney function (rising serum creatinine, reduced GFR)
2) oliguria or anuria
3) hematuria
4) proteinuria (usually non-nephrotic range)
5) hypertension, edema, fever, malaise, weight loss, myalgias
6) hemoptysis (coughing up blood)
7) skin rash (purpuric)
summary points/differences between nephrotic and nephritic syndrome