VM 577 Midterm Part I
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
If the hypothalamus releases corticotropin-releasing hormone (CRH), which of the following hormone would be released from the anterior pituitary?
a) Adrenocorticotropic hormone
b) Antidiurectic hormone
c) Growth Hormone
d) Prolactin
A.
Which of the following hormones is not secreted by the Anterior Pituitary?
a) Growth hormone
b) Thyroid-stimulating hormone
c) Follicle-stimulating hormone
d) Oxytocin
D.
What two endocrine glands are important in regulating blood calcium levels?
a) Adrenal gland & Pancreas
b) Parathyroid gland & Anterior Pituitary
c) Hypothalamus & Posterior Pituitary
d) Thyroid gland & Parathyroid gland
D.
What two hormones are important in glucose homeostasis?
a) FSH & LH
b) Glucagon & Insulin
c) Triiodothyronine & Thyroxine
d) Prolactin & Thyroid stimulating hormone
B.
Hormones may consist of all of the following except:
a) Carbohydrates
b) Steroids
c) Proteins
d) Amines
A.
You are presented with a 7-year-old spayed female mixed breed dog (37 kg) with the following history:
1-day history of progressive labored breathing and tachypnea/dyspnea
2-month history of polyuria/polydipsia (PU/PD) and polyphagia
On physical exam:
Mild pot-bellied appearance
Bilateral truncal alopecia
Crackles auscultated over all lung fields
A thoracic CT reveals:
A large partially occlusive thrombus in the main pulmonary artery
Diffuse pulmonary interstitial to alveolar infiltrates
Considering the patient's clinical presentation and imaging findings, what is the most appropriate next step in your diagnostic plan?
Stabilize patient → Delay testing for hyperadrenocorticism (HAC)
What would happen if you administer synthetic ACTH (Cosyntropin) to a healthy dog?
A. Cortisol levels would increase
B. Cortisol levels would decrease
C. Cortisol levels would remain unchanged
A.
What would happen if you administer synthetic ACTH (Cosyntropin) to a dog with naturally occurring Cushing’s disease?
A. Cortisol levels would increase
B. Cortisol levels would decrease
C. Cortisol levels would remain unchanged
A.
What would happen if you administer dexamethasone to a healthy dog?
A. Endogenous cortisol levels would increase
B. Endogenous cortisol levels would decrease
C. Endogenous cortisol levels would remain unchanged
B.
What would happen if you administer dexamethasone to a dog with Cushing’s disease?
A. Endogenous cortisol levels would increase
B. Endogenous cortisol levels would decrease
C. Endogenous cortisol levels would remain unchanged
C.
What is the clinical value of the UCCR? What patient population would you use this test in?
A. A negative result rules out HAC. This test should be used in those with low-moderate index of suspicion.
B. A positive result confirms HAC. This test should be used in those with high index of suspicion.
C. A negative result rules out HAC. This test should be used in those with high index of suspicion.
D. A positive result confirms HAC. This test should be used in those with low index of suspicion.
A.
Which of the following is the preferred diagnostic test for HAC?
A. ACTH Stim test
B. Low Dose Dex Suppresion Test
C. UCCR
D. Endogenous ACTH
B.
What would be the expected findings on abdominal ultrasound in PDH?
A. Two mildly-moderately enlarged adrenal glands
B. Two normal sized adrenal glands
C. Two small adrenal glands
D. One enlarged gland and one normal gland
A. AND B. (upper end of normal)
What would be the expected findings in ADH?
A. Two normal sized adrenal glands
B. One enlarged gland and one normal gland
C. One enlarged gland and one small gland
D. Two enlarged adrenal glands
C.
Interpretation - LDDST:
• 0 hr: 91 nmol/L (15-115 nmol/L)
• 4 hr: 72 nmol/L (< 30 nmol/L)
• 8 hr: 99 nmol/L (< 30 nmol/L)
A. This dog has HAC
B. This dog does not have HAC
C. This dog has PDH
D. This dog has ADH
A.
Interpretation - LDDST:
• 0 hr: 125 nmol/L (15-115 nmol/L)
• 4 hr: 38 nmol/L (< 30 nmol/L)
• 8 hr: 108 nmol/L (< 30 nmol/L)
• Endogenous ACTH: 24 pmol/L (10-48 pmol/L)
A. This dog has HAC
B. This dog does not have HAC
C. This dog has PDH
D. This dog has ADH
C.
ACTH Stim:
• 0 hr: 105 nmol/L (15-115 nmol/L)
• 1-hr post: 680 nmol/L (250-550 nmol/L)
• Abd u/s: (3-7 mm at cranial and caudal poles)
• Left adrenal: 9 mm (cranial) and 10 mm (caudal)
• Right adrenal 9 mm (cranial) and 8 mm (caudal)
A. This dog has HAC
B. This dog does not have HAC
C. This dog has PDH
D. This dog has ADH
C.
10 yr-old F/S terrier mix
PUPD
Alopecia
Increased ALP and CHOL
ACTH Stim: 0hr: 82 nmol/L (15-115 nmol/L)
1 hr post: 510 nmol/L (250-550 nmol/L)
What are your next steps?
A. Repeat ACTH stim in 2-3 days
B. Perform a LDDST in 2-3 days
C. Repeat ACTH stim in 1-2 months
D. Perform a LDDST in 1-2 months
D. → give it time
What complications would be expected to develop after the removal of the pituitary?
A. Hypothyroidism
B. Hypoadrenocorticism
C. Central diabetes insipidus (ADH deficiency)
D. More than one choice is correct
D. → hypot due to the loss of TSH, Addison’s due to the loss of ACTH, CDI could occur if pituitary stalk is damaged
What is the expected outcome of using radiation therapy for treatment of PDH?
A. Reductions in mass size and normalization of cortisol concentrations
B. No change in mass size, but normalization of cortisol concentrations
C. Reduction in mass size, but failure to normalize cortisol concentrations
D. No notable effect in most cases
C.
Which type of drug could effectively treat all cases of naturally occurring Cushing’s syndrome regardless of cause?
A. A drug that targets that hypothalamus and blocks hormone production
B. A drug that targets the anterior pituitary and blocks hormone production
C. A drug that targets the adrenal gland and blocks hormone production
D. A drug that blocks cortisol receptors on peripheral tissues throughout the body
D.
What drugs is needed for several weeks after surgical adrenalectomy?
A. Prednisone
B. Trilostane
C. Heparin/anticoagulant
D. Amlodipine
A.
You are managing a 12-year-old spayed female toy poodle (4.1 kg) previously diagnosed with pituitary-dependent hyperadrenocorticism (PDH) and treated with trilostane 5 mg PO q24h for the past 3 months.
History:
Panting has resolved
Polyphagia improved, but not fully normalized
PU/PD improved during the day, but still present at night
Physical Exam:
Mild pot-bellied appearance
Resolving alopecia
Otherwise normal
ACTH Stimulation Test Results:
Baseline cortisol: 59 nmol/L (RI: 50–180 nmol/L)
1-hour post-ACTH cortisol: 79 nmol/L (RI: 50–180 nmol/L)
How would you proceed?
A. increase the morning dose
B. Decrease the morning dose
C. Add an evening dose
D. Switch to an alternate therapy
C.
You are evaluating a 10-year-old spayed female mixed breed dog (8.8 kg) for a routine biannual wellness visit. She was diagnosed with suspected pituitary-dependent hyperadrenocorticism (PDH) one year ago and has been well-controlled on trilostane 10 mg PO q12h since that time.
History:
No complaints from the owners
No signs of PU/PD, polyphagia, or lethargy
Here for routine monitoring and wellness
Physical Exam:
Normal
Monitoring Test:
Pre-pill (trough) cortisol: 88 nmol/L
(Target range: 30–80 nmol/L)
How would you proceed?
A. Increase the dose
B. Decrease the dose
C. Add an evening dose
D. Keep the dose the same
D.
A 12-year-old NM Yorkshire Terrier (4 kg) has been receiving Trilostane at 5 mg BID for the management of PDH.
Target post-ACTH cortisol range 40–150 nmol/L.
In the first scenario, the dog presents with clinical signs of lethargy and anorexia.
Pre-ACTH cortisol concentration of 21 nmol/L
Post-ACTH cortisol concentration of 24 nmol/L.
In the second scenario, the dog is clinically normal
Pre-ACTH cortisol concentration of 21 nmol/L
Post-ACTH cortisol concentration of 24 nmol/L.
How should you proceed in each of these cases?
Stop Trilostane until dog is well, restart at lower dose
Do nothing ± could reduce dose
Which of the following dermatologic abnormalities occurs infrequently in dogs with Cushing's disease, but is highly suggestive of Cushing's disease when it does occur?
a. Pyoderma
b. Calcinosis circumscripta
c. Calcinosis cutis
d. Comedones
C.
Which of the following laboratory findings is consistent with Cushing's disease?
a. Hyponatremia
b. Azotemia
c. Thrombocytosis
d. Anemia
C.
Which of the following tests offers the greatest degree of specificity for a diagnosis of Cushing's disease?
a. ACTH stimulation test
b. Baseline cortisol concentration
c. Abdominal ultrasound
d. Low dose dexamethasone suppression test
A.
Which of the following statements concerning hyperadrenocorticism is TRUE?
a. Dogs with untreated Cushing's disease live longer than those with treated disease.
b. Adrenal-dependent forms are associated with a worse prognosis than pituitary dependent forms.
c. Expansion of pituitary tumors is the leading cause of death.
d. Most dogs with Cushing's disease die in < 1 year.
B.
T/F: The presence of an adrenal carcinoma is associated with a poorer prognoses than an adrenal adenoma
False
Which of the following is a common finding in cats with hyperaldosteronism?
a) hypocholesterolemia
b) hypercholesterolemia
c) hypertension
d) hypotension
C. → increased aldosterone → sodium/water retention → increased blood volume → increased blood pressure
Which age range of cats is most commonly affected with hyperaldosteronism?
a) young (1-4 years)
b) middle-aged (5-9 years)
c) old (>10 years)
C.
Which of the following breeds is predisposed to Addison’s disease?
a) Boxer
b) Boston terrier
c) Basenji
d) Standard poodle
D.
Which laboratory finding could be indicative of cortisol deficiency?
a) hypoglycemia
b) hyperkalemia
c) hypophosphatemia
d) hypercholesterolemia
A.
A 4 yr-old N/M dog is presented to a dialysis service because of AKI resulting from leptospirosis. The dog is anuric, azotemic, and severely hyperkalemic.
What would be the expected aldosterone concentrations?
A. Aldosterone levels would be normal
B. Aldosterone levels would be high
C. Aldosterone levels would be low
B.
A 7 yr-old F/S cat has Fanconi syndrome and is wasting potassium through her renal tubules. The cat is euvolemic, normotensive, and mildly hypokalemic.
What would be the expected aldosterone concentrations?
A. Aldosterone levels would be normal
B. Aldosterone levels would be high
C. Aldosterone levels would be low
C.
A 3 yr-old F/S cat was hit by a car. She has suffered severe blood loss and is hypovolemic and hypotensive on presentation.
What would be the expected aldosterone concentrations?
A. Aldosterone levels would be normal
B. Aldosterone levels would be high
C. Aldosterone levels would be low
B.
Primary drivers of aldosterone release are:
Hyperkalemia
RAAS
Biochemical markers for feline primary hyperaldosteronism
Hypokalemia
Metabolic alkalosis
Azotemia common
Increased CK
± Diabetes
Which of the following would be most suggestive of primary hyperaldosteronism in a 12 yr N/M DSH with systemic arterial hypertension?
Serum aldo RI: 100-400 pmol/L Serum K RI: 3.5-4.8 mmol/L
A. K: 4.2 mmol/L; aldo: 975 pmol/L
B. K: 2.7 mmol/L; aldo: 72 pmol/L
C. K: 5.1 mmol/L; aldo: >4300 pmol/L
D. K: 3.0 mmol/L; aldo: 2149 pmol/L
E. K: 4.4 mmol/L; aldo: 745 pmol/L
D.
In a hypokalemic cat, which of the following would be most suggestive of primary hyperaldosteronism?
A. High renin, high aldosterone, low ACTH
B. Low renin, high aldosterone, unaffected ACTH
C. High renin, high aldosterone, unaffected ACTH
D. Low renin, high aldosterone, low ACTH
E. Unaffected renin, high aldosterone, high
B.
Which of the following drugs have minimal affect on blood pressure?
A. Amlodipine
B. Spironolactone
C. Enalapril
D. Furosemide
C.
Which of the following statement about the serum Na:K ratio (normal, 29-37) is true:
A. > 95% of HA dog have a low Na:K ratio, hence an Na:K ratio > 29 can rule-out HA
B. Very few conditions cause a marked decrease in NA:K ratio, hence an Na:K ratio < 23 is diagnostic of HA
C. A decrease Na:K ratio is highly sensitive and specific for HA diagnosis and approaches the accuracy of ACTH stim testing.
D. A decreased Na:K ratio lacks the sensitivity or specificity to be useful as a stand-alone diagnostic test
D.
Which of the following disease cause a low Na:K ratio? Select all that apply
A. Whipworm infestation
B. Hookworm infestation
C. Acute kidney injury
D. Cushing’s
E. Addison’s
A. C. E
T/F: Diabetes is a very common sequela of Cushing’s in a cat
True
What is the clinical value of a baseline cortisol in testing for Addison’s?
A. Highly sensitive and can be used for screening dogs with low-moderate index of suspicion.
B. Highly specific and can be used to confirm a diagnosis in an ICU setting.
C. Moderate sensitivity and specificity useful for confirming disease in dogs with classic signs
D. They have no clinical value
A.
What effect will dexamethasone have on the ACTH stimulation test in a patient with suspect Addison’s disease when given BEFORE testing?
A. It will have no effect as dexamethasone does not cross-react with the cortisol assay.
B. It will suppress both the baseline and 1-hr post samples, therefore the test is of no value.
C. It will suppress the baseline sample, but the 1 hr post will be unaffected
D. It will increase both the baseline and 1 hr post samples
C. dexamethasone may suppress endogenous ACTH, lowering the baseline, but the 1-hour post sample reflects exogenous ACTH stimulation, and will not be affected by dexamethasone → can trust 1 hr post for Addison’s
Acute management of Addisonian’ crisis includes:
Correct hypovolemia/hypotension
Correct electrolyte abnormalities
Correct acid-base disturbances
Hormone replacement
GI supportive care
How high does potassium have to be before appreciating ECG abnormalities?
~6.5
T/F: The vast majority of Addisonians do no need anything other than fluid therapy initially to address their hyperkalemia
True
Hydrocortisone is routinely used to treat Addison’s disease in humans, but prednisone is routinely used to treat Addison’s in dogs. Why?
A. Prednisone is cheap and readily available.
B. Prednisone has both glucocorticoid and mineralocorticoid properties.
C. Dogs are unable to absorb hydrocortisone
A.
How should you monitor the efficacy of glucocorticoid replacement in Addison treatment?
A. ACTH stimulation testing
B. LDDST
C. Endogenous ACTH levels
D. Clinical signs
E. Routine labwork
D.
What would ACTH levels would be expected in a dog with untreated Addison’s disease?
Highly elevated → low cortisol, loss of negative feedback to pituitary = elevated ACTH
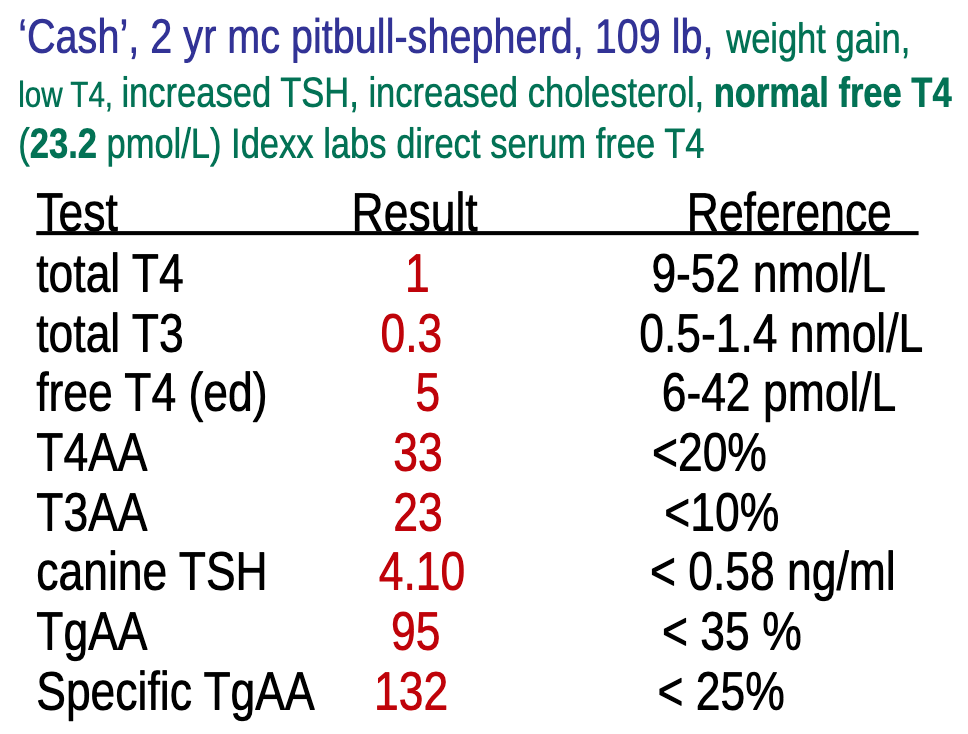
Which of the following test result is the most accurate in confirming the diagnosis of hypothyroidism in this patient?
Free T4 by ED
Archie, a 1-year-old neutered male French Bulldog (10 kg), presents with intense pruritus, crusting dermatitis, and a history of recurrent pyoderma with resistant Staphylococcus. He is currently being treated with Simparica Trio, Apoquel, and trimethoprim-sulfamethoxazole. A routine thyroid panel shows a low total T4.
What is the most likely explanation for Archie’s low T4 level?
Drug-induced suppression of thryoid peroxidase enzyme from trimethoprim-sulfamethoxazole
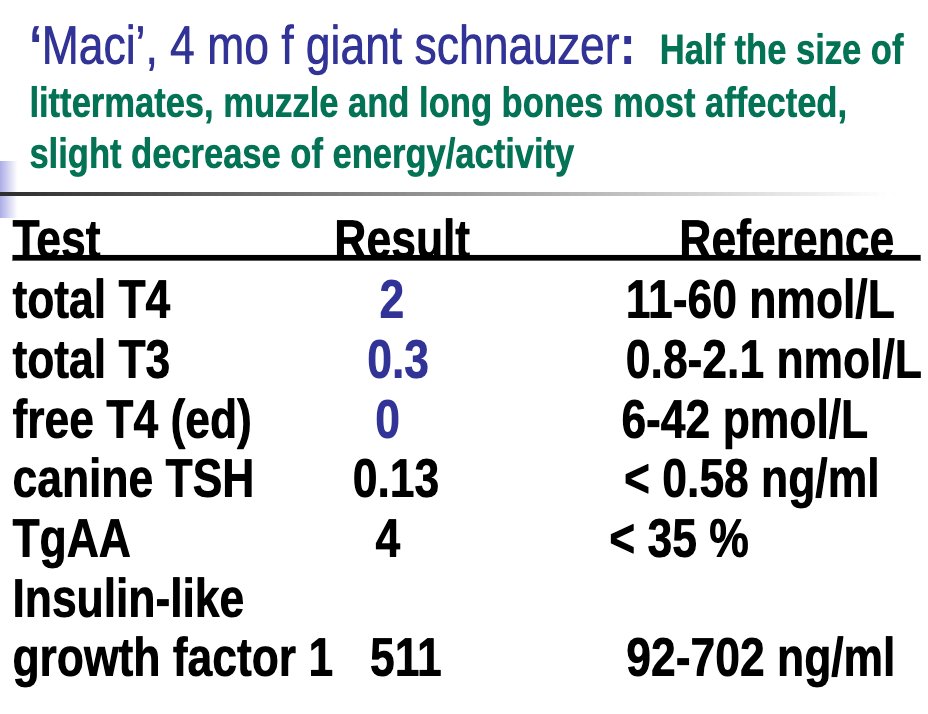
What would you tell her owner regarding these results?
Congenital Hypothyroidism
Which of the following is true regarding hyperthyroidism in cats?
A. A total t4 alone is sufficient to confirm a ddx in most cases
B. Thyroid hormones must be interpreted in conjunction with TSH when diagnosing hyperthyroidism in cats
C. Total and free T4 levels should always be checked together when testing for hyperthyroidism
D. A total T3 has the highest sensitivity but lowest specificity among the thyroid hormones
A.
What is your approach to equivocal test results in a high-normal T4 result in a cat?
A. Refer for nuclear scintigraphy study
B. Perform a complete thyroid profile now
C. Wait 2-3 months and assess a total T4 again
D. Wait 2-3 months and assess a complete thyroid profile
E. Perform dynamic thyroid function testing in 2-3 months
D.
Which of the exam findings is most commonly observed in cats with hyperthyroidism?
A. Panting
B. Palpable goiter
C. Carciac murmur
D. Hair coat abnormalities/seborrhea
B.
What is the most appropriate next step for a 17-year-old cat treated with I-131 for hyperthyroidism, now showing low TT4, high TSH, azotemia, and isosthenuria?
A. No treatment, recheck thyroid and kidney values in 2-3 months
B. Initiate treatment for hypothyroidism and recommend a renal diet
C. Initiate treatment for hypothyroidism, no dietary change
D. No treatment for hypothyroidism, but recommend a renal diet
B.
T/F: Measuring Thyroglobulin Autoantibodies has high sensitivity and specificity for hypothyroidism
FALSE: for thyroiditis
What is the most reliable diagnostic criterion for hypothyroidism when interpreting thyroid test results in dogs?
Combination of low thyroid hormone levels and elevated TSH
In a case study investigating spontaneous primary hypothyroidism in adult cats aged 3.5-11 years, what was identified as the most likely underlying cause?
A. Iodine deficiency
B. Environmental goitrogen
C. Congenital dyshormonogenesis
D. End-stage lymphocytic thyroiditis
C.
Which of the following offers the greatest specificity for a diagnosis of hypothyroidism in dogs?
a) TSH
b) Total T4
c) Thyroglobulin Autoantibodies
d) Total T3
A. → Thyroid fails to produce T4 → no negative feedback → TSH rises. Not a sensitive test!
Which of the following is a well-recognized and common clinical sign of hypothyroidism in dogs?
A. Aggression
B. Vomiting
C. Lethargy
D. Seizures
C.
Which percentage of geriatric cats are estimated to have hyperthyroidism in the USA?
A. 1%
B. 5%
C. 10%
D. 25%
C.
Which of the following is the most common physical exam finding in cats with hyperthyroidism?
A. Enlarged kidneys
B. Diffuse alopecia
C. Palpable goiter
D. Malodorous breath
C.
When treating Cushing’s, what is usually the first clinical sign to resolve?
PUPD
A 3 year old F/S Labrador retriever presents for evaluation of vomiting and anorexia. The dog was not currently receiving any medications nor had she within recent months. A baseline cortisol was performed and the result was 12 nmol/L (Reference interval, 15-115 nmol/L). What is your interpretation of this result?
A. This test should not have been performed in a sick dog
B. Cushing’s disease has been excluded as a possibility
C. She has Addison’s disease and treatment should be initiated
D. Addison’s disease has not been ruled-out and further testing is necessary
D.
An 11 yr-old N/M Boston Terrier has been appropriately diagnosed with Cushing’s disease and presents to your hospital for differentiation of pituitary vs. adrenal dependent forms of disease. You measure an endogenous ACTH concentration and the result is within the reference interval, but at the high-end of normal. What is your interpretation?
A. This dog has PDH
B. This dog has ADH
C. This is an equivocal result and further testing is necessary
A.
In the absence of any clinical information, what would be your interpretation of the following low-dose dexamethasone suppression test results? Reference intervals are in ( ).
Baseline: 99 nmol/L (RI, 15-115 nmol/L)
4-hr: 88 nmol/L (RI, < 30 nmol/L)
8-hr: 90 nmol/L (RI, < 30 nmol/L
A. Results are suggesting of Cushing’s
B. Result are suggestive of ADH
C. Results are suggestive of PDH
D. Results are not suggestive of Cushing’s
A.
Which test is used most commonly to monitor the effectiveness of medical therapy for Cushing's disease?
A. Low dose dex suppression test
B. ACTH stimulation test
C. Urine cortisol to creatinine ratio
D. Endogenous ACTH concentration
B.
Which of the following would be MOST supportive of a diagnosis of ADH?
A. High endogenous ACTH
B. Low endogenous ACTH
C. Normal endogenous ACTH
B.
Which of the following would be MOST supportive of a diagnosis of PDH?
A. High endogenous ACTH
B. Low endogenous ACTH
C. Normal endogenous ACTH
A.
What are the 5 most common clinical signs seen in Cushing’s disease?
PU
PD
Polyphagia
Pot bellied appearance
Panting
A dog with Cushing’s disease has a USG of 1.014 and no signs of lower urinary tract disease. What should you do next?
A. No further testing needed
B. Start antibiotics empirically
C. Recommend a urine culture
D. Repeat urinalysis in 2 weeks
C.
What is the most characteristic chemistry panel abnormality in dogs with Cushing’s disease?
A. Elevated ALT > ALP
B. Decreased cholesterol
C. Mild azotemia
D. Increased ALP due to steroid-induced isoenzyme production
D.
Why is hypercholesterolemia a common finding in dogs with Cushing’s disease?
Increased hepatic synthesis of cholesterol due to excess cortisol
For which of the following diseases would you expect a stress leukogram with thrombocytosis as part of the CBC findings?
A) Addison’s
B) Cushing’s disease
C) Vit D toxicosis
D) Primary hyperparathyroidism
B.
Which of the following Low Dose Dexamethasone Suppression Test patterns is most consistent with pituitary-dependent hyperadrenocorticism (PDH) in a dog?
A) 4-hour: normal, 8-hour: suppressed below reference range
B) 4-hour: no suppression, 8-hour: no suppression
C) 4-hour: suppressed, 8-hour: rebound to baseline
D) 4-hour: suppressed, 8-hour: suppressed
C. → pituitary initially responds to dexamethasone but then resumes ACTH secretion, leading to a rise in cortisol at 8 hours.
Approximately 90% of cats with hyperadrenocorticism (Cushing’s disease) will also have which concurrent clinical diagnoses?
Insulin-resistant diabetes mellitus
What is the treatment of choice for dogs with ADH?
Adrenalectomy
A 13-year-old cat presents with cervical ventroflexion, hind limb weakness, and persistent hypokalemia. Abdominal palpation reveals a firm mass near the kidney. Which of the following best explains how increased aldosterone contributes to the observed clinical signs?
A) Promotes sodium excretion, leading to dehydration and neuromuscular dysfunction
B) Increases potassium excretion, resulting in muscle weakness and cervical ventroflexion
C) Stimulates insulin secretion, leading to muscle tremors and hypoglycemia
D) Causes direct skeletal muscle damage through cortisol overproduction
B.
Aldosterone __________ renal sodium reabsorption and potassium __________
increases
excretion
Chemistry findings for a cat with hyperaldosteronism
Hypokalemia
Increased CK
Metabolic alkalosis
Azotemia
What is the most common etiology of primary hyperaldosteronism in cats?
Unilateral adrenocortical neoplasia
What is the treatment of choice for a cat with hyperaldosterodism?
A. Amlodipine
B. Spironolactone
C. Enalapril
D. Furosemide
B.
Which of the following is a key limitation when interpreting plasma aldosterone concentration (PAC) in cats suspected of having hyperaldosteronism?
A) It is unreliable in the presence of hypokalemia
B) Elevated levels are specific for adrenal tumors
C) Normal reference ranges vary widely among cats
D) Aldosterone secretion is not influenced by the RAAS system
C.
What three major body systems are primarily affected by Addison’s disease?
GI
Urinary
Cardiovascular
CBC findings for Addison’s disease
Absence of stress leukogram
Erythrocytosis
Non-regenerative anemia
T/F: Elevated liver enzymes would be mildly elevated due to hypovolemia in Addison’s disease
True
Gold standard test for Addison’s disease and the expected result
ACTH stimulation test → pre and post < 55 nmol/L
What is the steroid dose for:
Anti-inflammatory
Physiologic dose
Immunosuppresion
0.5-1.0 mg/kg
0.1-0.3 mg/kg
1-2 mg/kg
What are two mineralocorticoids use for long-term management of Addison’s
DOCP: mineralocorticoid only
Fludrocortisone: mineralocorticoid and glucocorticoid
What dosing approach for DOCP is supported by anecdotal experience at MSU for medium to large breed dogs with Addison’s disease?
Start at a lower dose (0.25–1.5 mg/kg) to minimize cost and reduce risk of excess mineralocorticoid effects
Addison’s disease commonly causes which of the following cardiac abnormalities?
A) Bradycardia
B) Tachycardia
C) Normal sinus rhythm
D) Tall-tented T-waves
A.
Secondary hypothyroidism is a defect in the ________ while tertiary hypothyroidism is a defect in the ________
pituitary
hypothalamus
Which of the following would NOT be a clinical sign from hypothyroidism?
A. Nasal alopecia
B. Bradycardia
C. Ataxia
D. Prolonged parturition
E. Heat intolerance
E.
Which of the following laboratory abnormalities is most commonly associated with hypothyroidism in dogs?
A) Hypochromic, microcytic anemia
B) Decreased cholesterol and triglyceride levels
C) Normocytic, normochromic anemia and hyperlipidemia
D) Marked elevation in ALT and AST
C.
Which dog breed is known to have naturally lower T4 levels that are considered normal?
Greyhound