embryology-development of the heart
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
when does the development of separate blood vascular system start?
at the beginning of the third week
where does all of the components of the cardiovascular system develop from?
mesoderm
what are the two components of the cardiovascular system?
heart and blood vessels
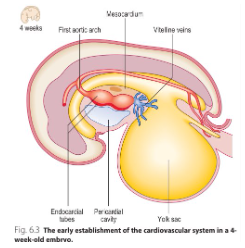
how does the heart develop?
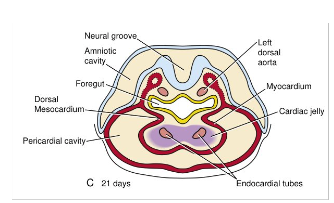
Heart develops from primitive heart tube, which forms from mesenchyme in the cardiogenic area of the embryo. Heart tube forms the endocardium of the heart. Splanchnic mesoderm surrounding the primitive heart tube forms myocardium and epicardium.
when does the primitive heart start beating?
21st-22nd day
when does blood begin to circulate within the embryo?
by the 24th day
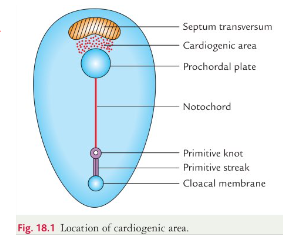
how does the cardiogenic area establish?
during week 3, cardiac progenitor cells develop cranial to the primitive streak- these cell migrate through the primitive streak cranially and form primitive heart field in the splanchnopleuric mesoderm by the end of the 3rd week
what induces vasculogenesis in the primary heart field ?
endoderm of primitive pharynx via secretion of vegf
how is the endocardium formed?
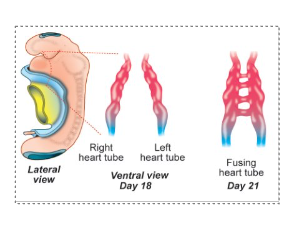
small vessels join to form two endothelial/endocardial heart tubes that give rise to endocardium
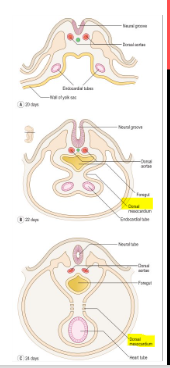
how is the heart tube formed?
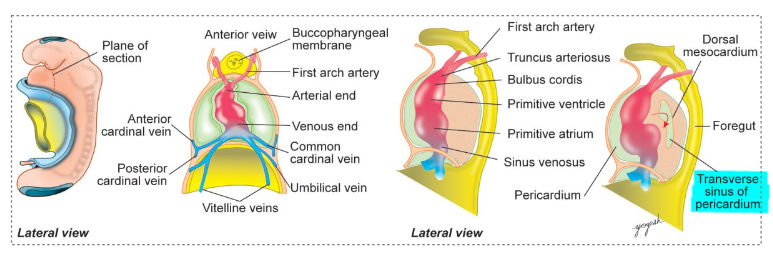
in the 3rd week embryo folding occurs- 2 endothelial heart tubes fuse and form a single heart tube- the ends of the heart tube remains bifurcatedwha
what is the cranial and caudal end called in the heart tube?
cranial- arterial end
caudal- venous end
what are the 5 dilatations that the heart tube forms?
cranial to caudal end:
Truncus arteriosus
Bulbus cordis
Primitive ventricle
Primitive atrium
Sinus venosus
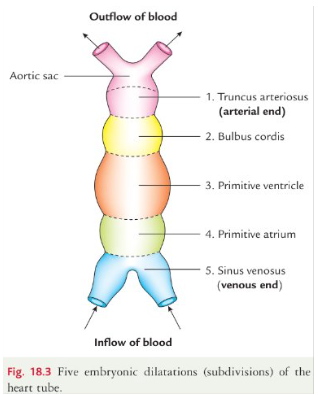
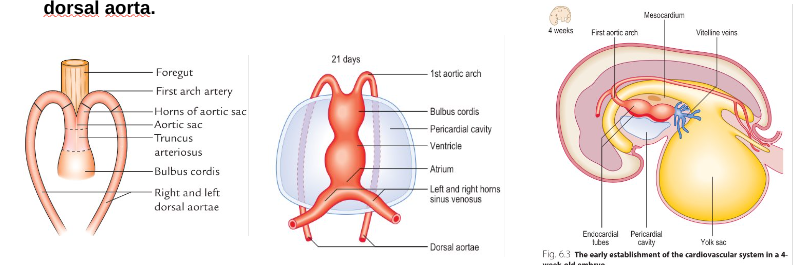
what is the truncus arteriosus?
represents the arterial end of the heart. cranially it is continuous with aortic sac having right and left horns. each horn of aortic sac, the 1st pharyngeal arch artery arises and becomes continuous with the dorsal aorta
what is the sinous venosus and what are the three veins of each horn?
unfused part forms two horns
each horn receives three veins from lateral to medial:
common cardinal vein from the body wall
umbilical vein from the placenta
vitelline vein from the yolk sac
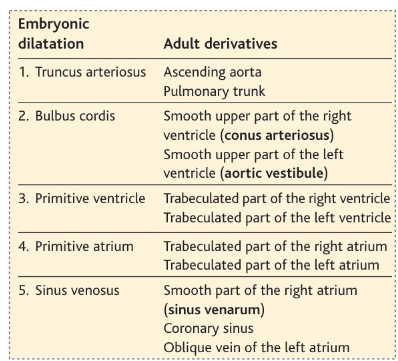
what are the derivatives of each dilatation of the heart tube?
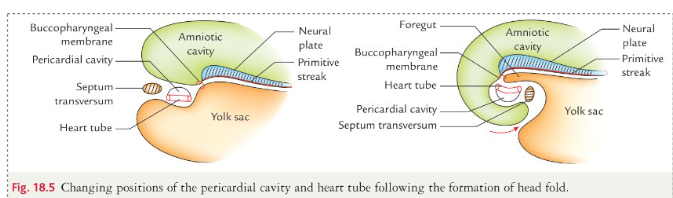
what is the position of the heart tube before and after formation of head fold?
before: heart tube lies in the floor of the pericardial cavity caudal to septum transversum
after: pericardial cavity and heart tube undergoes 180 degree rotation and the heart tube is lying of the roof of the pericardial activity
how does the intraembryonic cavity develop into the pericardial cavity?
Intraembryonic cavity over the heart fuse together later develops into the pericardial cavity and become located around the tube.
what is dorsal mesocardium formed and what happens when broken down?
Heart tube is suspended from dorsal wall of pericardial cavity by a fold of pericardium - dorsal mesocardium.
Soon, dorsal mesocardium breaks down, leaving the heart tube attached merely at the margins of the pericardium
where is the endothelial heart tube derived from and what does it form?
Endothelial heart tube is derived from the splanchnopleuric mesoderm.
Endothelial / endocardial heart tube forms the endocardium of the heart.
what is the myoepicardial mantle and how is it formed?
splanchnopleuric mesoderm of the pericardial cavity proliferates and becomes thick to form myoepicardial mantle, which invests the front and sides of the endothelial heart tube.
what separates the myoepicardial mantle from the heart tube?
a cellular gelatinous ct called cardiac jelly
what is the cardiac jelly?
an acellular matrix secreted by developing myocardium and is replaced by myocardium
what forms the endocardium of the heart?
endothelial heart tube
what forms the myocardium and the visceral layer of pericardium?
myoepicardial mantle
where is the parietal layer of pericardium derived from?
somatopleuric mesoderm
how are the bulboventricular loop formed?
bulbus cordis and primitive ventricle grow and form the bulboventricular loop
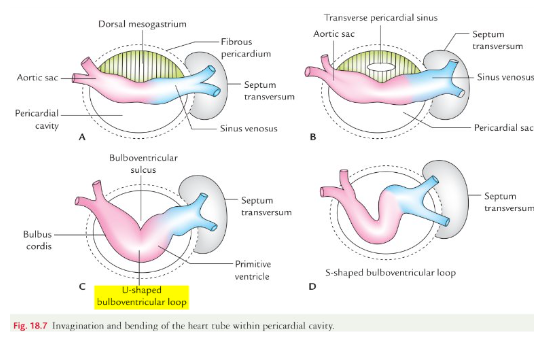
how is the transverse sinus formed?
mesocardium connective bulboventricular loop disappear to form a gap
how is the s- shaped loop formed?
as primitive atrium and sinus venosus get freed from septum transversum, they come lie in the pericardial cavity dorso-cranial to the primitive ventricle
how is a single chamber formed in an adult heart?
bulbus cordis and primitive ventricle are separated by bulboventricular sulcus that later disappears and blublus cordis and ventricle fuse
how is a defect caused in cardiac looping?
caused by a defect in the dynein arm of microtubules and results in karatagener syndrome with situs inversus and dextrocardia
what is situs inversus and dextrocardia?
Situs inversus – rare, genetic condition in which some or all major visceral organs are positioned opposite from their normal position. Dextrocardia – abnormal orientation of the heart in which the apex is located to the right aspect of the mediastinum rather than the left.
what are the four chambers of the heart partitioned by?
Atrioventricular septum
Interatrial septum
Interventricular septum
Aorticopulmonary septum.
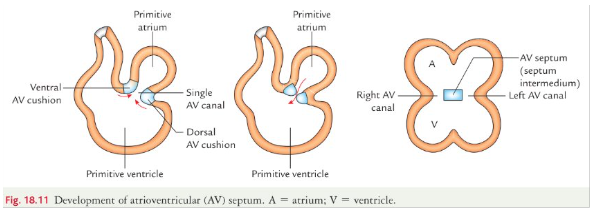
what are endocardial cushions and how are they formed?
at the end of the 4th week two swellings of mesenchymal tissue appear from wall of the canal
how is the atrioventricular septum formed?
neural crest cells migrate into the cushions to grow and the cushions fuse to form av septum and the septum intermedium divides the av into the right and left av canal
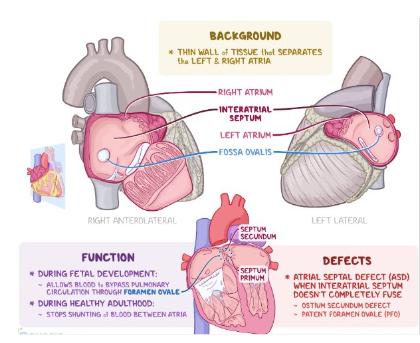
what is the interatrial septum?
divides the primitive atrium into the left and right atria- it is formed by two septa- septum primum and septum secundum
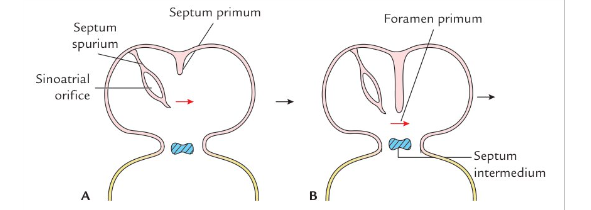
how is the interatrial septum formed?
At the end of 4th week, the septum primum starts developing from the roof of the primitive atrial chamber.- crescent shaped
It grows downward towards septum intermedium (AV septum).
The gap between the lower edge of septum primum and septum intermedium is foramen primum.
how is the second septum secundum formed?
As septum primum fuses with AV septum the upper part of septum primum breaks down.
The foramen thus formed is called foramen secundum (ostium secundum).
A second crescent-shaped septum secundum now arises from the roof of primitive atrial chamber immediately to the right of septum primum.
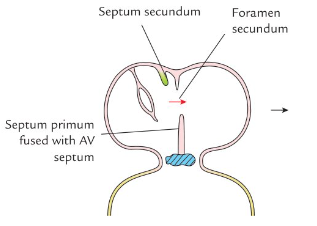
what are the two main components that make up the interatrial septum?
septum primum that forms the lower part of inter-atrial septum
septum secundum that forms the upper part of interatrial septum.
when does the foramen ovale close?
usually 6 months- a year after the birth of the baby
how does the foramen ovale closed?
After birth LA receives blood from lungs and pressure within it becomes greater than the RA.
As the pressure of blood in the LA increases, it pushes the septum primum to the right.
It comes in opposition with septum secundum and foramen ovale is closed - blood is prevented from flowing from the LA to the RA.
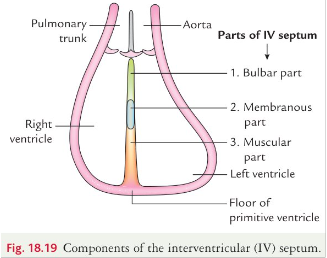
when does the interventricular septum begin development and when does it close completely?
the interventricular septum begins in week 4 and is usually completed by the end of week 7.
IV septum will develop and close by week 8 without any shunting between the ventricles.
what are the 3 parts of the iv septum?
all three parts are from three different sources
muscular part
bulbar part
membranous part
how is the aorticoplumonary septum formed?
neural crest and endocardial cells migrate to form truncal ridges and bulbar ridges and these spiral to form the ap septum
ap fuses and rotates 180 degrees dividing the outflow tract into the aorta and pulmonary trunk
what is the embyonic origin for the development of semilunar valves?
endocardial cushions of outflow tract
what is the embyonic origin for the development of av valves?
fused endocardial cushions of av canal
what is cogenital heart defects and what are they caused by?
CHDs are caused by the disruption of the normal sequence of cardiac morphogenesis.
CHDs may lead to the formation of shunts between the right and left heart chambers, allowing blood to flow along the pressure gradient from high pressure to low pressure.
Shunts are classified according to the direction of the blood flow as: left-to-right or right-to-left
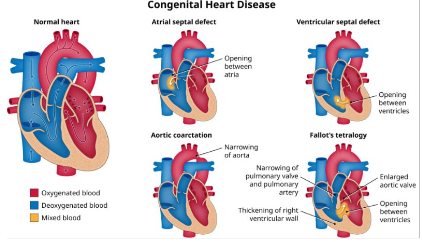
what are two left to right shunt defects?
Oxygenated blood from the lungs is shunted back into the pulmonary circulation via an atrial septal defect, ventricular septal defect, or patent ductus arteriosus pulmonary hypertension
Right ventricular pressure overload → right sided heart hypertrophy and heart failure but no cyanosis
what is a right-to-left shunt defect?
blood flows from the right to the left heart via a shunt → deoxygenated blood entering the systemic circulation → cyanosis
what are examples of congenital heart defects and what are they commonly caused by?
risk factors:
teratogens, genetic abnormalities, premature birth, asphyxia during delivery, rubella infection during pregnancy
acyanotic congenital heart defects:
Ventricular septal defect (VSD)
Atrial septal defect (ASD)
Patent foramen ovale
Patent ductus arteriousus (PDA)
Coarctation of the aorta
Endocardial cushion defect
Pulmonary valve stenosis
what are acyanotic heart defects?
Congenital cardiac malformations that affect the atrial or ventricular walls, heart valves, or large blood vessels.
Acyanotic heart defects are pathophysiologically characterized by a left-to-right shunt, which causes pulmonary hypertension and right heart hypertrophy.
Infants may be asymptomatic or present with exercise intolerance, failure to thrive, and symptoms of heart failure.
Acyanotic heart defects requiring treatment are repaired via catheter procedures or surgery.
what are cyanotic heart defects general clinical features?
right-to-left-shunt
“Blue babies”: pale gray or blue skin color caused by cyanosis
Feeding problems and failure to thrive
Exertional dyspnea, tachypnea, and fatigue
Hypoxemia
Symptoms of heart failure
Nail clubbing may occur later in life.
what are some examples of cyanotic heart defects?
Tetralogy of Fallot
Transposition of the great vessels (TGV)
Tricuspid valve atresia
Ebstein anomaly
Total anomalous pulmonary venous return (TAPVR)
Persistent truncus arteriosus
Hypoplastic left heart syndrome (HLHS)