Unit 5 - Electrical Stimulation for muscle contraction, functional activity, and biofeedback
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
Neuro Muscular Electrical Stimulation (NMES)
Induce contraction of skeletal muscles
Neuro Muscular Electrical Stimulation (NMES)
purpose
Muscle strengthening
Disuse atrophy
Spasm or spasticity reduction
Edema reduction
Improve range of movement
Voluntary contraction
Progressive recruitment of muscle
fibersSlow, typically small, motor units
followed by fast, typically large, motor
units.Asynchronous motor unit recruitment
patterns
NMES contraction
Recruitment is in a nonselective
manner, both small and large motor
units are recruited regardless of the
physiological principles.The recruitment of the motor units
occurs in a spatially fixed and
temporally synchronous pattern
TETANY
the point where further increases in frequency do not produce increases in force production
Types of Current
Russian Current
Low Voltage Pulsed Current
Muscle strengthening
Muscle mass takes several weeks
Non-muscle mass effects include:
Increase of number of motor units recruited
Increase in the frequency of motor units recruited
Increase the motor recruitment in a more synchronized manner
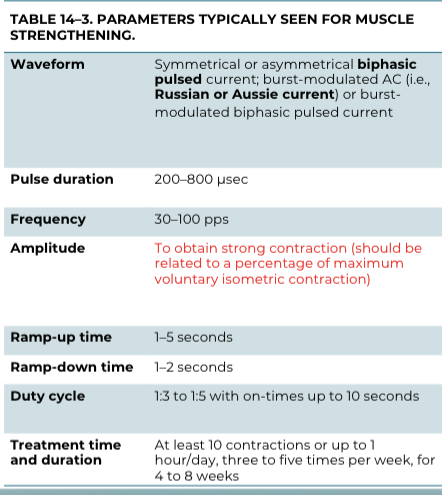
NMES parameters for muscle strengthening
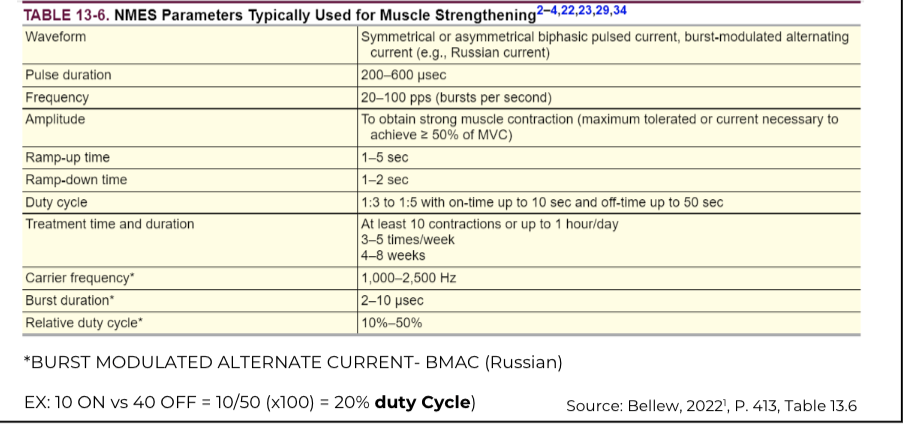
STIMULATION Parameters Considerations
Muscle strength: the highest pulse duration and amplitude tolerated by the patient should be used.
The frequency should be adjusted to achieve a smooth, forceful contraction above 30 pulses per second (pps or Hz).
Higher stimulation frequencies (pps or Hz) such as 100 Hz or above, may generate greater muscle fatigue
STIMULATION Parameters Considerations
Avoiding fatigue:
reducing the frequency,
increasing the rest time between
contractions.
Ramp time:
Shorter times are recommended.
1 or 2 seconds are ideal.
Intensity:
contractions near maximal tolerance
50 to 70% of the MVC of the opposite limb are common in studies reporting increased strength following NMES
Motor Recruitment and Intensity
NMES recruits muscle fibers located deep within the muscle
Electrical Muscle Stimulation Applied to Denervated Muscle
Electrical stimulation (ES) activates muscle fibers by depolarizing the sarcolemma
and not via peripheral motor nerves. NMES is for innervated muscle.
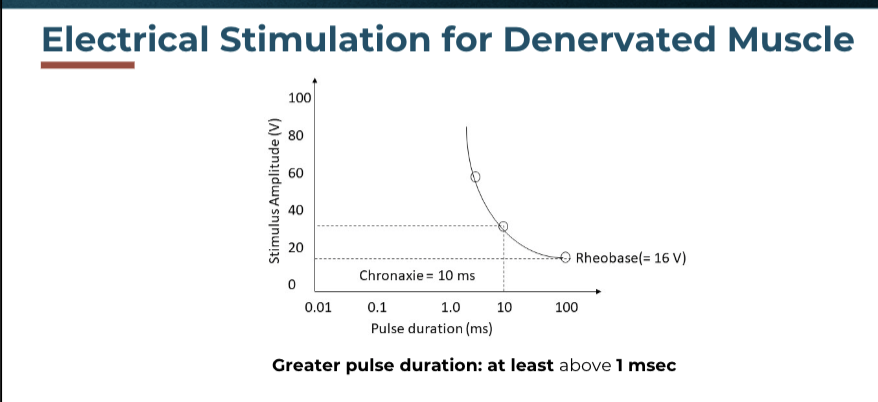
NMES on denervated muscle parameters:
Long pulse duration
Greater amplitude of stimulation,
Different waveform (direct current, greater risk of skin burns)
nmes contraindication
Electrodes should not be placed over:
The trunk or heart region in patients with demand-type pacemakers or implantable cardioverter defibrillators (ICDs)
The pelvic, abdominal, lumbar, or hip region in pregnant women
Carotid bodies
Phrenic nerve or urinary bladder stimulators
Areas of known peripheral vascular disease, including arterial or venous thrombosis or thrombophlebitis
The phrenic nerve, eyes, or gonads
Areas of active osteomyelitis
Areas of hemorrhage
nmes precautions
Without intact sensation. An exception to this is when using a low amplitude current for wound healing.
Who are unable to communicate, as they may be incapable of accurately providing feedback regarding the stimulation.
With compromised mental ability or lack of cognition, as they may be unable to understand directions.
With cardiac dysfunction, including uncontrolled hypertension, hypotension, or irregular heart rate or rhythm.
With epilepsy or other seizure disorders
Electrotherapy should be used with caution over neoplasms (active or previous).
Electrodes should not be placed over:
Compromised skin (except if treating for wound/tissue repair).
Tissues vulnerable to hemorrhage or hematoma.
Cervical (i.e., neck) or craniofacial regions in patients with a history of cerebrovascular accidents or seizures.
Do not use ES devices within approximately 5 yards of diathermy units or other sources of electromagnetic radiation
NMES and FES in patients with Neurological conditions
Neuromuscular electrical stimulation (NMES)
Electrical stimulation used to activate intended
muscles via intact motor neurons.
Functional Electrical Stimulation (FES) is the use of
NMES to promote functional activities
NMES in Patients with Neurological Conditions
indications:
Muscle Strengthening
Increase range of motion
Decrease spasticity
Decrease Urinary incontinence
Special considerations and rationale for using E. Stim in neurological patients.
Muscle innervation – Nerves should be intact
Strength – MMT to determine the muscle to treat and reassess
Range of motion – Limited ROM limit functional outcomes, E. Stim. may be used first to gain ROM.
Sensation – Decreased sensation requires frequent monitoring.
Pain – Determine if the E. Stim. will be beneficial in presence of pain
Spasticity – It could be impacted by E. Stim.
Function – Treat and assess using functional activities.
Cognitive status – Precaution/Safety to use E. Stim.
Caregiver assistance – Assistance for E. Stim. at home.
Other treatments – It may impact the patient outcome assessment
NMES for Muscle Strengthening
scientific evidence:
Stroke
Cerebral Palsy
Spinal cord injury
Multiple sclerosis
e-stim for increasing ROM
Stimulation of the antagonist’s muscle to
stretch the agonist-tight muscle
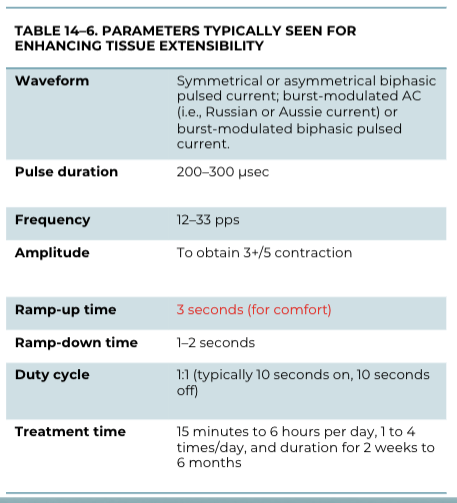
NMES and FES for Wrist Extension
Considerations for Using NMES to Increase ROM
Parameters should be set to follow the stretching principles: low load and prolonged application.
Parameters should be set to minimize fatigue due to longer application goal: low frequency and amplitude
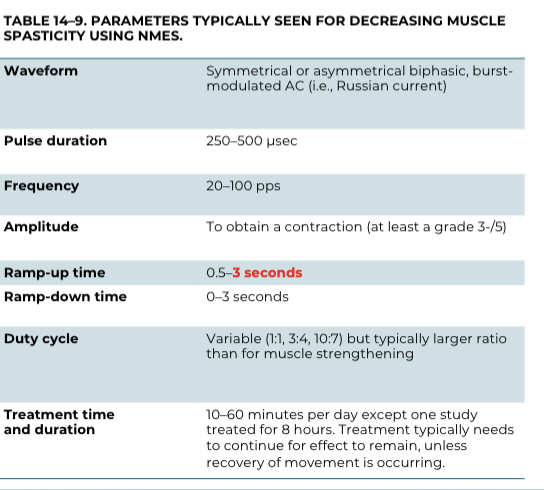
nmes - Decrease spasticity
Applied in the antagonist of the agonist spastic muscle – reciprocal inhibition.
ORApplied directly to the spastic muscle by fatiguing the muscle or by providing recurrent inhibition by Renshaw cells
Functional Electrical Stimulation (FES)
Most common Indications
Shoulder subluxation
Upper-extremity function
Foot drop
Gait
UE and LE Cycling
fes for shoulder subluxation
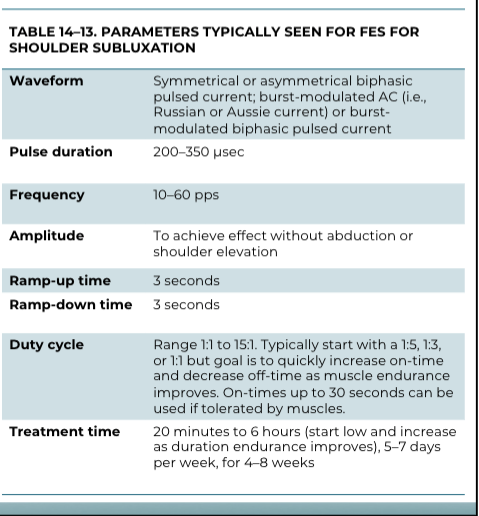
FES: Upper-extremity function
patients
Patients: stroke, traumatic brain injury (TBI), CP, and SCI.
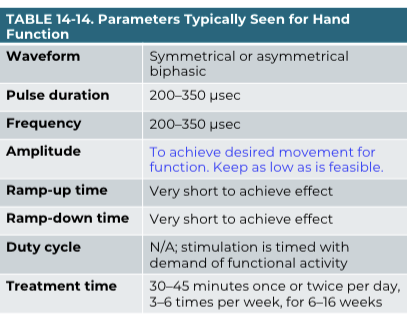
FES: Upper-extremity function
indications:
Indications: spasticity, ROM, motor function, and functional abilities
FES: Upper-extremity function
parameters:
FES for Foot Drop and Gait
Researchers in the Clinical Center's Rehabilitation Medicine Department (RMD) are studying an electrical stimulation device designed for children with cerebral palsy who suffer from foot drop and tripping when walking.
The WalkAide device stimulates the muscle that lifts up the ankle and the foot on the lower leg.
In addition to its success in gait improvement, the RMD team found that electrical stimulation reversed some of the leg muscle wasting caused by the disorder and, in several patients, preserve and increased muscle strength
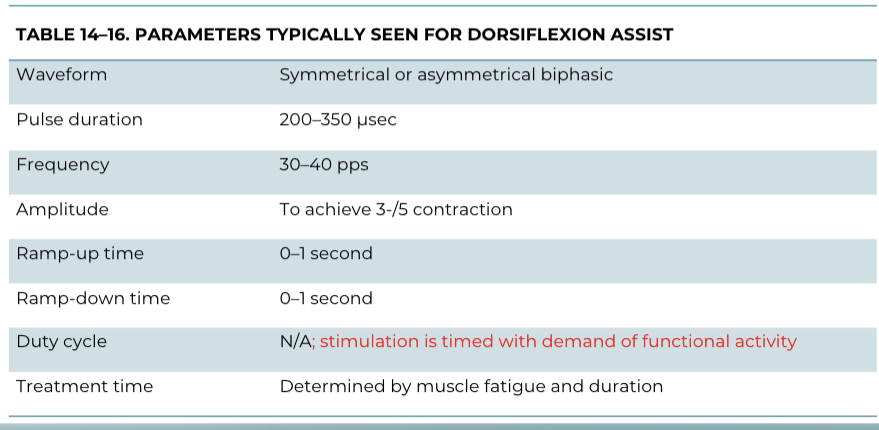
FES for Foot Drop and Gait
parameters:
Assist Dorsiflexion Electrodes Placement

General Application and Monitoring Information for NMES and FES
Instruct the patient:
Purpose and procedure.
explain the anticipated sensation and effect of the stimulation.
explain that you need a strong muscle
Make a familiarization session to familiarize the patient with the electrical stimulation sensation.
E. Stim in Kids - you must distract them with a game, video, or other activity
Pre-inspection:
Intact skin and sensation
Treatment monitoring:
Monitor the patient’s response to treatment
Adjust the amplitude if needed
Obtain patient feedback regarding the sensation and strengthening of muscle contractions.
Patients with cognitive deficits need additional supervision, removing and adding the electrodes once or twice during treatment to check the skin may be required.
Post-inspection:
Inspect the skin after removing the electrodes
Make sure there is no skin irritation ormadverse effects.
Slight redness is normal and may disappear in 24 hours.
Biofeedback
EMG:
1. EMG biofeedback provides information about the muscle activity that the patient
and clinician can use to increase or decrease the future activity of a treated muscle.
2. EMG feedback does not deliver any electrical current to the patient as in other forms of electrotherapy; instead, it detects the electrical activity generated by muscles that are used for therapeutic purposes
Most biofeedback equipment devices provide
visual and auditory feedback
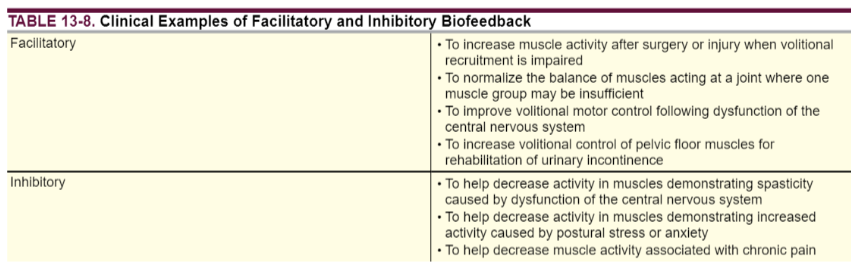
Biofeedback indications
EMG biofeedback can be used to facilitate or Inhibit muscle contraction
Electrode Type and Electrode Placement Considerations for EMG Biofeedback
Electrode used for biofeedback are like those used for electrical stimulation, such as disposable adhesive electrodes.
The muscle fibers that will be detected are those close to the electrodes.
The wider the electrode placement, the larger the volume of muscle is detected.
Electrodes close to each other are used to inhibit the muscles that are “very active.” For activating muscles in which their volitional activity is decreased, wider electrode placement is recommended.
The muscles should be partially innervated there are no contraindications to using EMG biofeedback since no electrical stimulation is not delivered
Sensitivity
the ability to detect the electrical activity associated with muscle contraction
Typical devices used for EMG biofeedback offer
sensitivity settings (sometimes called gain) of 1, 10, 100, or 1,000 microvolts (μV).
Sensitivity and gain are
inversely related, such that the gain setting is the lowest at the highest sensitivity
Recording and Displaying the EMG Signal
example:
Example, at the lowest gain setting of 1 μV, the sensitivity is greatest, capable of detecting as little as 1 μV of change in muscle activity. In contrast, a high gain setting of 1,000 μV is much less sensitive and can only detect changes of 1,000 μV.
The sensitivity of a biofeedback device is set depending on the need for amplification and the clinical goals. Less sensitivity is needed when muscle activity is very high. More sensitivity is needed when volitional muscle activity is low
Example: Quadriceps facilitation biofeedback
Post-surgery of ACL reconstruction
First days after surgery: HIGH sensitivity (gain of 1 μV): the machine will detect minimum muscle contractions.
Few weeks after surgery: LOW sensitivity (gain of 500 μV): the patient must produce stronger contractions to be sensed by the device