PHYS TOPIC 11 pt. 2
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
Blood Pressure
= hydrostatic P exerted by blood on wall of vessel (slinically on the walls of the arteries) results when F is opposed by R
systolic pressure = produced by vent. contraction against vascular restistance
diastolic pressure = produced by elastic arteries against vascular resistance (when vents. are relaxed)
what we measure in an artery: 120/80 - syst./diast.
pulse pressure = systolic - diastolic
mean arterial pressure (MAP) = regulated by the body i.e. what the body measures
= average of blood P through cardiac cycle BUT diastole us longer than systole, so;
MAP = diast P +1/3 pulse P
MAP Regulation
F= change in P/r, therefore change in P = F xR
change in P = F x R
MAP = cardiac output (HR x SV) X Total peripheral resistance (TPR) (= resistance in all arterioles)
chnage in P = MAP - venous P (P in veins ~ 0, therefore change in P = MAP)
MAP is regulated by controlling;
Cardiac Output
TPR (arteriolar radius)
Blood Volume (affects venous return which impacts SV; also MAP directly)
Extrinsic Regulation of MAP - Neural Control
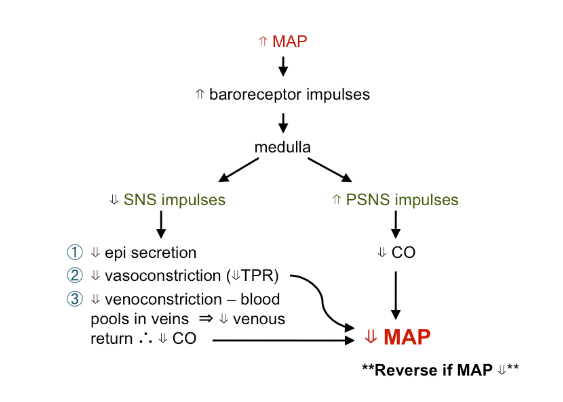
baroreceptor reflexes - short term changes e.g. standing
stretch receptors - monitor MAP in:
carotid sinus (brain bp)
aortic arch (systemic bp)
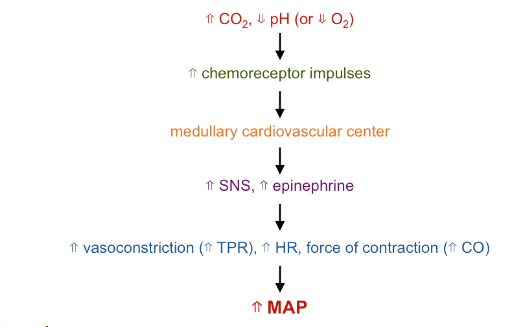
chemoreceptor reflexes
peripheral chemoreceptors - respond to pH, CO2, O2
found in aortic arch and carotid sinus (called “bodies”)
involved in regulation of respiration, but affect bp
Extrinsic Regulation of MAP - Hormonal Control
epi
incr. HR, force of contraction which results in incr CO2 = incr. MAP
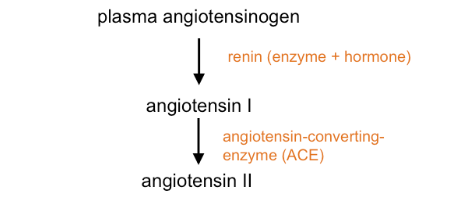
renin-angiotensin system:
angiotensin II causes:
incr. vasocons. and venocons. therefore incr. MAP
incr. aldosterone, ADH which act to incr. renal Na+, H2O absorption and incr. thirst which incr. blood volume = incr. MAP
atrial natriuretic peptide(ANP) causes:
decr. renin (therefore decrease angiotensin II) decrease aldosterone, ADH, all contribute to incr. urine production which will decrease blood volume
decrease vasoconstriction
so overall = decrease in MAP
Capillary Exchange
between blood and ISF
solutes enter and leave caps. by:
diffusion = major route (except brain)
CO2, O2, Ions, aa, glucose, hormones, etc.
usually between endothelial cells
Vesicular transport - large proteins (antibodies)
occurs via transcytosis
= endothelial from blood into cell, then exocytosis from endothelial cell into ISF
mediated transport - requires a memb. carrier protein
important mainly in brain
Capillary Exchange - Fluid
(h2) enters (absorption) or leaves (filtration) capillaries by:
osmosis
bulk flow - due to pressure differences
4 pressures involved
blood hydrostatic P (BHP) = blood pressure
blood osmotic P (BOP) - mainly due to plasma proteins
ISF hydrostatic pressure (IFHP) = 0mmHg
ISF osmotic pressure (IFOP) - mainly due to ISF proteins
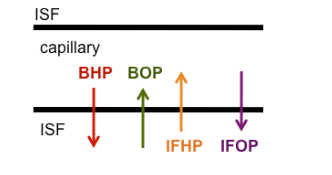
Net Filtration Pressure (NFP)
sum of hydrostatic and osmotic pressures acting on the capillary
in the body:
90% of filtered fluid reabsorbed to blood
10% enters lymph
therefore ISF volume remains relatively constant
clinical apps. Edema
= accumulation of fluid in the tissue (ISF) causing swelling
due to:
high BP
leakage of plasma proteins into ISF → inflammation (incr. IFOP)
decr. plasma proteins (malnutrition, burns) (decr. BOP)
obstruction of lymph vessels - elephantiasis, surgery
Circulatory Shock
inadequate flood flow (decr. O2, nutrients to cells)
types:
hypovolemic shock
vascular shock
Circulatory Shock Types
hypovolemic:
decrease blood volume
due to: blood loss, severe burns, diarrhea, vomiting
vascular shock:
blood vol. normal, but vessels expanded
due to: systemic vasodilation of blood vessels = decr. bp
examples:
anaphylactic shock- allergic reactions
due to lot of histamine released from mast cells
septic shock
due to bacterial toxins
cardiogenic shock
pump failure = decr. CO
heart cannot sustain blood flow
Stages of Shock
compensatory
progressive
irreversible
Compensatory Shock Stage
mechanisms can restore homeostasis by themselves
involves:
baroreceptors
chemoreceptors
ischemia (lack of O2) of medulla
all trigger SNS:
incr. HR, generalized vasoconstriction (except to heart, brains) = incr. BP
decr. blood flow to kidneys tiggers renin release - get angiotensin II, aldosterone and ADH release which causes: vasoconstriction; incr. Na+ and H2O retention (to maintain blood volume) , incr. Thirst
Progressive Shock Stage
mechanisms inadequate to restore homeostasis - requires intervention
decr. CO, decr. BP in cardiac circ. which will decr. cardiac activity
decr. blood to brain will decr. the ability of the brains to exert cardiovascular control
damage to viscera due to decr. blood flow, especially kidneys (can lead to renal failure)
Irreversible Shock Stage
decr. CP = too little blood to heart = decr. CO
self-perpetuating cycle - leads to death
Blood Contains
plasma
H2O
proteins
electrolytes (ions)
other solutes
formed elements
RBCs
WBCs
platelets
Plasma
H2O (90.5%)
transport medium and carries heat
proteins (7%)
albumins (58%)
globulins (38%)
fibrinogen (4%)
functions
produce osmotic pressure (especially albumins), buffer pH (7.35-7.45) - keep it from changing
α, β globulins - transport lipids, metal ions, hormones
(gamma) globulins = antibodies
clot formation
electrolytes (ions)
functions: memb. excitability, buffers (HCO3)
other solutes
nutrients, wastes, gases, hormones
Formed Elements in Blood
Red Blood cells
white blood cells
platelets
Red Blood Cells
functions:
transport - O2 on iron of heme; CO2 on globin
buffer - globin binds to H+ reversibly
carbonic anhydrase (CA) - important for CO2 transport in blood
hemoglobin:
hb= 4 hemes +4 globins (protein)
1 Fe/heme, therefore 4 Fe/Hb
broken down by macrophages into:
heme
Fe removed and stored (liver, muscle, spleen)
from stores (or diet) = bone marrow cells make heme → RBCs
non iron portion → bilirubin→ excreted in bile from liver
globin
converted to amino acids - recycled
NOTE RBCs → no nuclei/mitochondria → anaerobic resp. only
White Blood Cells
granulocytes
neutrophils
phagocytic
1st to enter infected area
eosinophils
attack parasites
break down chemicals released in allergic reactions
basophils
secrete histamine (increases inflammation)
secrete heparin (inhibits local clotting)
agranulocytes
monocytes
enter tissues, enlarge to become phagocytic macrophanges
lymphocytes
T lymphocytes - Helper T (TH) + cytotoxic T (CTLs) lymphocytes
B lymphocytes - when activated give rise to plasma cells - secrete antibodies
natural killer cells - attack foreign cells, abnormal cells (non specific)
Platelets
cell fragments from megakaryocytes
functions:
form platelet plug - prevents excess blood loss
contain granules = coagulation factors (proteins/chemicals involved in clotting)
Hemostasis
process of stopping bleeding
involves:
vascular spasm
platelet plug formation
clot formation
clot retraction
fibrinolysis
thrombus = a stationary clot in undamaged vessel
embolus = free floating clot
hemophilia = clotting abnormal/absent
about 83% Type A - lack clotting factor VIII
Hemostasis Vascular Spasm
= vasoconstriction of damaged arteries, arterioles - decr. blood flow (minutes to hours)
Hemostasis Platelet Plug Formation
platelets stick to damaged blood vessel, release chemicals (factors) which:
cause more platelets to stick (+ feedback)
promote clotting
begin healing
neighbouring healthy endothelial cells release a chemical preventing spread of plug
plug formation requires a prostaglandin - inhibited by aspirin
Hemostasis Clot Formation
3 stages:
production of prothrombin activator by:
extrinsic pathway - uses factors released by damaged tissues
intrinsic pathway - uses factors contained in blood → usually both occur together - require Ca²+, tissue, platelet and/or plasma factors
prothrombin converted to thrombin (using activator)
fibrinogen converted to fibrin (using thrombin, Ca²+)
thrombin - + feedback to incr. its own formation
NOTE: ~2 doz. factors involved
from diet, liver (plasma proteins), damaged tissue, platelets
e.g. vit. K required for synthesis of 4 factors
Hemostasis Clot Retraction and Repair
retraction - blood vessel edges pull together
repair - fibroblasts form new CT, new endo. cells repair lining
Hemostasis Fibrinolysis
clot dissolution
fibrin digesting enzyme = plasmin
phagocytes then remove clot in clumps
plasminogen —→ (using factors) —→ plasmin (breaks down clot)