2 - ANALYSIS OF OTHER BODY FLUIDS
1/403
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
404 Terms
Kidneys
two, bean-shaped, located on each side of the body
150
each kidney weighs approximately _ g and measures 12.5 cm x 6 cm 2.5 cm
Ureter
transports urine from the kidneys to the bladder
measures 25 cm long
Urinary Bladder
150
storage site for urine
when approximately _ mL urine accumulates, a nerve reflex is initiated
Urethra
transports urine outside the body
4 cm long in women and 24 cm long in men
Ancient Egyptians
History
Recorded urine observations in hieroglyphics (e.g., Edwin Smith Papyrus)
Egyptians and Babylonians
History
Practiced “taste testing” of urine to detect diabetes
Hindu Physicians
History
Noticed that “honey urine” attracted ants
Hippocrates
History
Uroscopy; developed humoral theory foundations; first documented the importance of sputum examination
Galen
History
Systematized the four humors/temperaments: sanguine (blood), choleric (yellow bile), phlegmatic (phlegm), melancholic (black bile)
Johannes de Ketham
History
Published Fasciculus Medicinae (1491), which featured the urine wheel (a large circle surrounded by thin-necked urine flasks, showing how the color and consistency of urine could be matched to a diagnosis)
Frederik Dekkers
History
Discovered albuminuria by boiling urine
Thomas Bryant
History
Wrote a book about “pisse prophets” (charlatans)
Thomas Addis
History
Introduced examination of urine sediment
Richard Bright
History
Introduced urinalysis as part of doctor’s routine patient examination
Ludwig Thudichum
History
Urochrome
Domenico Cotugno
History
Cerebrospinal fluid (CSF)
Ivan Følling
History
Phenylketonuria (PKU)
Archibald Garrod
History
Alkaptonuria
Frederick William Pavy
History
Orthostatic (cyclic) proteinuria
William Wollaston
History
Cystine calculi
Stanley Benedict
History
Benedict’s reagent
95-97
3-5
60
Urine Composition
_-_% water
_-_% solids (_ grams)
35
Urea
Urine Composition
3-5% solids (60 grams)
_ grams organic
_ (major)
Creatinine (2nd), hippuric acid, uric acid, CHO, pigments, fatty acids, mucins, enzymes, hormones
25
Chloride
Sodium chloride
Urine Composition
3-5% solids (60 grams)
_ grams inorganic
_ (major) > Sodium > Potassium
_ _ (principal salt)
Sulfate, phosphate, ammonium, magnesium, calcium
Random / Occasional / Single
Types of Urine Specimen
Collected at any time
Random / Occasional / Single
Types of Urine Specimen
For routine and qualitative urinalysis
5
Types of Urine Specimen
Random / Occasional / Single
Ideal for cytology studies (ONLY IF with prior hydration and exercise _ minutes before collection!)
First morning
Types of Urine Specimen
Ideal specimen for routine urinalysis, pregnancy testing (hCG), and evaluation of orthostatic proteinuria
First morning
Types of Urine Specimen
Often preferred for cytology studies / cytodiagnostic urine testing
First morning
Types of Urine Specimen
Most concentrated and most acidic (allows well preservation of cells and casts)
First morning
Types of Urine Specimen
Patient should empty their bladder before going to sleep, and collect the first morning urine specimen immediately upon rising
Second morning / Fasting
2-hour post-prandial
Glucose tolerance
Fractional specimen
Types of Urine Specimen
Specimens for Glucose Monitoring (4)
Second morning / Fasting
Types of Urine Specimen
Specimens for Glucose Monitoring
2nd voided urine after a period of fasting
Second morning / Fasting
Types of Urine Specimen
Specimens for Glucose Monitoring
For glucose determination
2-hour post-prandial
Types of Urine Specimen
Specimens for Glucose Monitoring
For diabetic screening or monitoring
2-hour post-prandial
Types of Urine Specimen
Specimens for Glucose Monitoring
Preferred for glucose
Glucose tolerance
Types of Urine Specimen
Specimens for Glucose Monitoring
Optional with blood samples in glucose tolerance test
Fractional specimen
Types of Urine Specimen
Specimens for Glucose Monitoring
At least 2 voided collections
Fractional specimen
Types of Urine Specimen
Specimens for Glucose Monitoring
Series of blood and urine samples are collected at specific time intervals to compare concentration of a substance in urine with its concentration in the blood
Fractional specimen
Types of Urine Specimen
Specimens for Glucose Monitoring
Used in the diagnosis of diabetes
Midstream clean-catch
Catheterized
Suprapubic aspiration
Types of Urine Specimen
Sterile Specimens (3)
Midstream clean-catch
Types of Urine Specimen
Sterile Specimens
For routine screening and bacterial culture
Midstream clean-catch
Types of Urine Specimen
Sterile Specimens
Patient should carefully clean the tip of the penis (for males) or the opening of the urethra (for females) before collection
Catheterized
Types of Urine Specimen
Sterile Specimens
May be urethral or ureteral
Catheterized
Types of Urine Specimen
Sterile Specimens
For bacterial culture
Suprapubic aspiration
Types of Urine Specimen
Sterile Specimens
Abdominal wall is punctured, and urine is directly aspirated from the bladder
Suprapubic aspiration
Types of Urine Specimen
Sterile Specimens
For anaerobic bacterial culture and urine cytology
Pediatric specimen
Types of Urine Specimen
Use of soft, clear plastic bag with adhesive
Pediatric specimen
Types of Urine Specimen
Sterile specimen obtained by catheterization or suprapubic aspiration
Pediatric specimen
Types of Urine Specimen
Urine collected from diaper is not recommended for testing
Three-glass collection
Types of Urine Specimen
For prostatic infection (1)
First portion of voided urine
Middle portion of voided urine
Urine after prostatic massage
Types of Urine Specimen
Three-glass collection
1st glass:
2nd glass:
3rd glass:
1st, 3rd
Prostatitis
Types of Urine Specimen
Three-glass collection
Examine the _ and _ specimen microscopically, then compare the no. of WBCs and bacteria
If the no. of WBCs and bacteria in the 3rd specimen is 10x greater than that of the 1st specimen = _
Invalid
Types of Urine Specimen
Three-glass collection
_ _ = control for bladder and kidney infection
If control is (+) for WBCs and bacteria = the results from the 3rd specimen are considered = _
Four-glass collection (Stamey-Meares Test)
Types of Urine Specimen
For prostatic infection (2)
Initial voided urine
Midstream urine
Expressed prostatic secretions
Post-prostatic massage urine
Types of Urine Specimen
Four-glass collection (Stamey-Meares Test)
VB1
VB2
EPS
VB3
Types of Urine Specimen
Four-glass collection (Stamey-Meares Test)
_____________ = tests for urethral infection or inflammation
_____________ = tests for urinary bladder infection
_____________ = tests for prostate infection or inflammation (>10-20 white blood cells per high-power field = ABNORMAL)
24-hour
12-hour
4-hour
Afternoon (2-4 PM)
Types of Urine Specimen
Timed Specimens (4)
24-hour
Types of Urine Specimen
Timed Specimens (4)
At start time, patient empties their bladder into the toilet → then, all urine passed after that is collected
24-hour
Types of Urine Specimen
Timed Specimens (4)
At end time, patient empties their bladder into the collection container
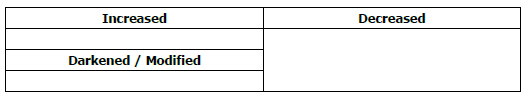
INCREASED
Types of Urine Specimen
Timed Specimens (4)
Addition of urine before the start of 24-hour collection period causes FALSE-_ results
DECREASED
Types of Urine Specimen
Timed Specimens (4)
Failure to include urine at the end of 24-hour collection period causes FALSE-_ results
Schistosoma haematobium
Types of Urine Specimen
Timed Specimens (4)
24-hour
For detection of _ _
preservative
Types of Urine Specimen
Timed Specimens (4)
24-hour
Requires _
3 L
Types of Urine Specimen
Timed Specimens (4)
24-hour
Containers should hold up to _ L and may be colored to protect light sensitive analytes
12-hour
Types of Urine Specimen
Timed Specimens (4)
For Addis count
4-hour
Types of Urine Specimen
Timed Specimens (4)
For ___________________ determination
Urine remains in bladder for at least 4 hours before voiding
Afternoon (2-4 PM)
Types of Urine Specimen
Timed Specimens (4)
For urobilinogen determination
chain of custody
Types of Urine Specimen
Drug specimen collection
Process providing documentation of proper sample ID from the time of collection to the receipt of laboratory results:
30-45 mL
Types of Urine Specimen
Drug specimen collection
Required urine volume:
Types of Urine Specimen
Drug specimen collection
Container capacity:
32.5-37.7 C
Types of Urine Specimen
Drug specimen collection
Temperature:
Types of Urine Specimen
Drug specimen collection
Added to the toilet water reservoir to prevent specimen adulteration:
>9
<1.005
Types of Urine Specimen
Drug specimen collection
pH _, S.G. _: possibly adulterated
wide
4
Types of Urine Specimen
Urine containers should:
have a _ base (to prevent spillage)
have an opening of at least _ cm (to allow easy and accurate urine collection)
be made of clear, disposable, single-use material
culture
Types of Urine Specimen
When both routine UA and culture are requested, the _ should be performed first
2 hours
30 minutes
Specimen Integrity
Following collection, urine specimens should be delivered to the laboratory promptly and tested within _ _ OR ideally within _ _
voided
Specimen Integrity
Physical, chemical, and microscopic characteristics of a urine specimen begin to change as soon as the urine is _
Specimen Integrity
Urine Preservatives
An ideal preservative (bactericidal, inhibits urease, preserves elements, and causes no interference) does not exist!
The preservative should be chosen based on the specific needs of the test
Refrigeration
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Preservative of choice for routine urinalysis Prevents bacterial growth for 24 hours | Does not interfere with chemical tests | Raises SG by hydrometer Precipitates amorphous phosphates and urates |
Thymol
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | - | Preserves glucose and sediments well | Interferes with acid precipitation test for protein (SSA) |
Boric acid
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Keeps pH about 6.0 Bacteriostatic at 18 g/L For culture transport, C&S | Preserves protein and formed elements well Does not interfere with routine analyses other than pH | May precipitate crystals when used in large amounts Interferes with drug and hormone analyses |
Formalin (Formaldehyde)
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Rinse specimen container with formalin to preserve cells and casts Preservative of choice for Addis count | Excellent sediment preservative | Acts as a reducing agent (interferes with chemical tests for glucose, blood, leukocytes, and copper reduction) |
Toluene (Toluol)
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Best all-around preservative Ideal preservative for steroids | Does not interfere with routine tests | Floats on urine surface Clings to pipettes and testing materials |
Sodium fluoride
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | May use sodium benzoate instead of fluoride for reagent strip testing | Anti-glycolytic agent (prevents glycolysis) Good preservative for drug analysis | Inhibits reagent strip tests for glucose, blood & leukocytes |
Phenol
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Use 1 drop/ounce of specimen Used for transportation of urine specimen | Does not interfere with routine tests | Causes an odor change |
Commercial preservative tablets
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Check tablet composition to determine possible effects on desired tests | Convenient when refrigeration not possible Have controlled concentration to minimize interference | May contain one or more of the preservatives including sodium fluoride |
Saccomanno fixative
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Used for cytology studies (50 mL urine) | Preserves cellular elements | - |
Urine collection kits
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Contains collection cup, C&S preservative tube or UA tube | - | - |
Gray C&S tube
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Preservative is boric acid and may not be used for UA | Sample stable at room temperature for 48 hours Preserves bacteria | Decreases pH Do not use if urine is below minimum fill line |
Yellow plain UA tube
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | No preservative (plain) Round or conical bottom | Use on automated instruments | Must refrigerate within 2 hours |
Cherry red / yellow top tube
URINE PRESERVATIVES | |||
Preservatives | Description | Advantages | Disadvantages |
_ | Preservative is sodium propionate Conical bottom | Stable for 72 hours at room temperature Instrument compatible | Bilirubin and urobilinogen may be decreased if specimen is exposed to light and left at room temperature |
Physical Examination of Urine
Urine Volume
Normal urine output (24 hours): _________________ (Average: 1,200-1,500 mL)
Night urine output: _________________
Day : Night ratio: _________________
Container capacity (UA): _________________
Required for routine UA: _________________ (Average: 12 mL)
Polyuria
URINE VOLUME TERMINOLOGIES | ||
Definition | Causes | |
Increased urine volume = >2.5 L/day (adults) = 2.5-3.0 mL/kg/day (children) | Increased fluid intake Diuretics, nervousness Diabetes mellitus Diabetes insipidus | |
Oliguria
URINE VOLUME TERMINOLOGIES | ||
Definition | Causes | |
Decreased urine volume = <400 mL/day (adults) = <0.5 mL/kg/hour (children) = <1 mL/kg/hour (infants) | Dehydration Renal diseases Renal calculi or tumor | |
Anuria
URINE VOLUME TERMINOLOGIES | ||
Definition | Causes | |
Complete cessation of urine flow = <100 mL/day | Complete obstruction (stones, tumors) Toxic agents Decreased renal blood flow | |
Nocturia
URINE VOLUME TERMINOLOGIES | ||
Definition | Causes | |
Excretion of more than 500 mL of urine at night = S.G. <1.018 | Pregnancy Renal diseases, bladder stones Prostate enlargement | |
Diuresis
URINE VOLUME TERMINOLOGIES | ||
Definition | Causes | |
Any increase in urine excretion | Excessive water intake Diuretic therapy Hormonal imbalance Renal dysfunction Drug ingestion | |