Lab Diag- Blood chemistry/BMP
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
75 Terms
What is a BMP used to monitor?
Electrolyte balance, blood filtration/kidney function, and blood sugar levels
What are possible interferences you may see with a BMP?
Hemolytic (high K+, LDH, and AST), icteric (elevated bile), and lipemic (not fasting prior to collection) samples
What is assessed in a BMP?
Electrolytes (NA, K, Ca, Cl), blood glucose, total CO2 (bicarb), AGAP, BUN, and creatinine
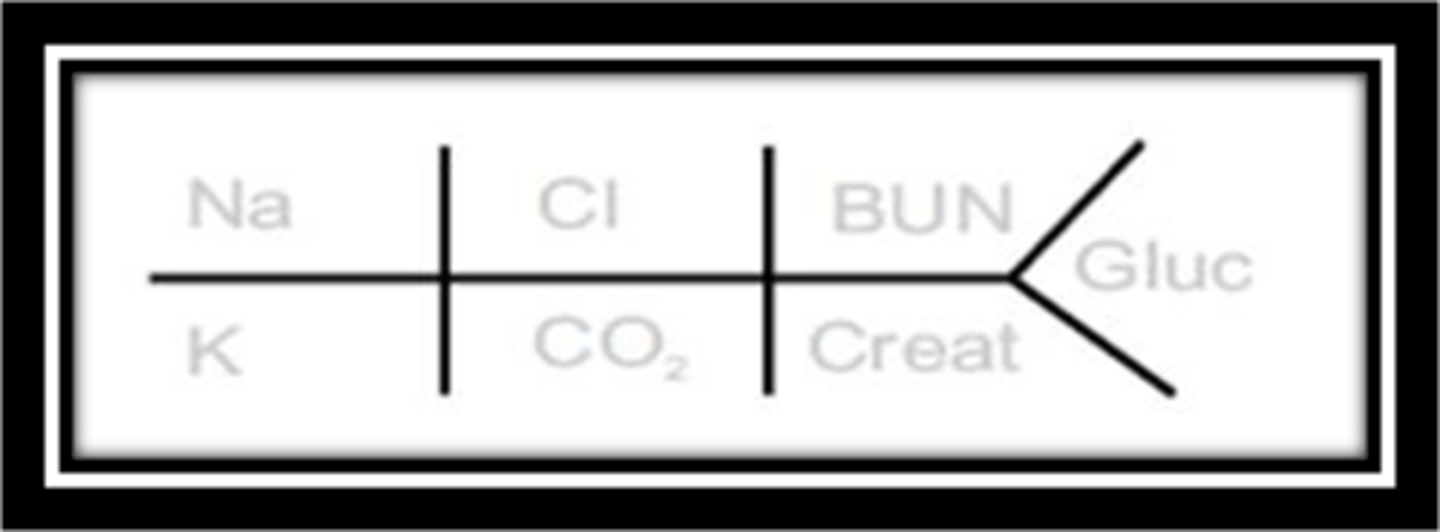
Fishbone of BMP
Mnemonic: Salty (NaCl) BUNs with Sugar (glucose)
For the denominators, they match with like ions such as Na on top and K on bottom bc they are both positive ions, CO2 under Cl bc negative ions, and creatinine under BUN bc related to kidneys
Where is sodium found in highest concentration?
In the extracellular fluid
Importance of sodium?
Maintains the osmotic pressure of cells, electrolyte balance, and maintaining the acid-base balance of the cells
What conditions might you see with hyponatremia?
severe polyuria, diarrhea, metabolic acidosis, Addison's disease (low aldosterone), and some renal tubular diseases (sodium absorbed in the kidney tubules)
What are possible signs and symptoms with hyponatremia?
Nausea, headaches, muscle cramps, and confusion
What are possible conditions associated with hypernatremia?
CHF, liver disease, renal disease, Cushing's syndrome (causes increased Na absorption by kidneys), severe dehydration (due to water loss, and certain brain injuries
Possible signs and symptoms with hypernatremia?
intense thirst, mucosal dryness, reduced urine output, and fatigue
What does osmolality measure?
Measures the total concentration of all ions and molecules present in a sample
What are major contributors to serum osmolality?
Sodium, glucose, and urea
Why is osmolality important and what brain structure controls it?
The hypothalamus responds to serum osmolality and it will decide whether to keep or release water
How does osmotic pressure work?
As osmolality of a solution increases, so does osmotic pressure (directly proportional).
A higher concentration of solutes = a greater force to draw water across a membrane into the solution.
What 3 processes regulate sodium?
Water intake in response to thirst (dictated by plasma osmolality), excretion of water, and regulation of blood volume
Where is potassium mostly found? What does it heavily influence?
intracellular fluid and it is an important influence on heart muscle activity and maintaining the acid-base balance of the cells
What conditions are associated with hypokalemia?
Prolonged vomiting/diarrhea and inadequate dietary intake.
Does the body have a mechanism to protect against excessive potassium loss?
No, even in times of potassium deficiency, the kidney will still excrete potassium
Possible signs and symptoms of hypokalemia?
muscle weakness and cramping, arrythmias, and weakened reflexes (potassium is important in regulating all excitable cell types)
We eat bananas for muscle cramps
Possible conditions associated with hyperkalemia?
kidney disfunction (cannot filter out K) and urinary obstruction (cannot pee out excessive K)
Possible sign and symptoms of hyperkalemia?
nausea, vomiting, muscle weakness, and arrythmias
Where are chloride ions mostly found?
Mostly in the serum/plasma, and also found in CSF, tissue fluid and urine. Important anion that counterbalances sodium, aids in osmotic pressure, and maintains electrical neutrality
What is chloride's relationship with bicarb?
A reciprocal relationship with bicarb.
When chloride decreases, bicarb goes up and vice versa.
What conditions are associated with hypochloremia?
Prolonged vomiting, chronic pyelonephritis, metabolic acidosis, and renal failure
Possible signs and symptoms from hypochloremia?
Fatigue, muscle cramps, nausea, and vomiting
Possible conditions associated with hyperchloremia?
dehydration, conditions causing decreased renal blood flow (CHF), and excessive dietary intake
Possible signs and symptoms of hyperchloremia?
Fatigue, thirst, nausea, vomiting, drowsiness, and lethargy
Where is bicarb mostly found and it's importance?
Major extracellular anion
Importance in gas exchange and maintaining acid-base balance
Where is bicarb usually filtered and do we find it in our urine?
Filtered by the kidney and little to no bicarb is found in urine as it is usually reabsorbed prior to excretion.
hypocapnia, hypocarbia
deficient level of carbon dioxide in the blood
hypercapnia, hypercarbia
excessive carbon dioxide in the blood
Difference in ionized calcium and serum calcium?
Ionized calcium is calcium readily available for reactions in the blood and is not bound to proteins or anions
Importance of calcium?
Essential for myocardial contraction, bone development, and coagulation cascade
Possible conditions associated with hypocalcemia?
Disorders of parathyroid hormone, vitamin D deficiency (it helps absorb Ca), low albumin (binds to serum Ca), hyperphosphatemia, CKD, and certain medications (calcium chelators and chemotherapy)
Possible signs and symptoms of hypocalcemia?
neuromuscular defects (involved in muscle contractions), paresthesias, cardiac irregularities, osteomalacia (softening of bones)
Conditions associated with hypercalcemia?
Increased intake, hyperparathyroidism, malignancy (bc of bone marrow), and certain medications (lithium, thiazide diuretics, etc)
Possible signs and symptoms of hypercalcemia?
Mild is usually asymptomatic but can result in fatigue, malaise, and weakness
What is an anion gap?
The difference between anions (Cl and bicarb) and cations (Na and K)
What is the anion gap used for?
to determine if patient has metabolic acidosis (too many anions make the blood acidic)
What does a decreased anion gap suggest?
May be to unmeasured ions or likely a potential lab error
What does an elevated anion gap suggest?
metabolic acidosis (diabetic ketoacidosis), lactic acidosis (think Sepsis), salicylate overdose (too much peptobismol), uremia, increased plasma proteins, etc.
High Anion Gap Metabolic Acidosis (HAGMA)
Why is kidney function important?
Important in balancing electrolytes.
CKD or renal failure highly increases a patient's risk of cardiovascular disease
How are nitrogen containing substances classified?
Protein substances containing nitrogen and non-protein substances (NPN) that consist of mostly urea
What is urea? What excretes it?
Urea is a waste product of protein metabolism and is made solely in the liver.
Urea is normally excreted through the kidneys
What may decreased renal function lead to?
increased urea, uric acid, and creatinine
Why can BUN sometimes not be as reliable in estimating renal function? (3 reasons)
1) Nonrenal factors affect levels
2) No significant change in BUN level until glomerular filtration rate (GFR) is decreased by at least 50%
3) Amount of urea determined by dietary protein and kidney function: low protein diet = urea levels may not accurately indicate kidney function
Causes for elevated BUN (azotemia)?
Mild to moderate increase in the plasma concentrations of nitrogen and other waste products in the blood when the kidney is impaired but not completely lost
Causes for elevated uremia?
Seen with end stage renal failure (worse than impairment)
When would a decreased BUN be clinically significant?
If liver damage is suspected and in pregnancy you may see lower than normal urea levels
What is prerenal azotemia?
-Before it reaches kidneys
-Result of decreased blood flow to the kidney causing decreased GFR.
Kidneys are otherwise functioning normally
Causes for prerenal azotemia?
dehydration, shock, diminished blood volume (hemorrhage), CHF, increased protein breakdown (fever, stress, severe burns)
What is renal azotemia?
-Once it reaches kidneys
Results from diminished GFR as a consequence of intrinsic renal disease
Possible causes for renal azotemia?
glomerulonephritis, polycystic kidney disease, autoimmune conditions
What is postrenal azotemia?
-After it reaches kidneys
-Usually will need both kidneys to be obstructed
-Results from any obstruction in which urea ends up reabsorbed into circulation
Serum creatinine clearance
-creatinine is a waste product of muscle breakdown that occurs at a constant rate
-provides a mean to determine the glomerular filtration rate of the kidney
-Must obtain both 24 hour urine collection and blood sample collected about 12 hours into urine collection period
is BUN or creatinine a better indicator of renal function?
Creatinine considered a better single test for renal function than urea as it is not as influenced by protein intake, degree of hydration, and protein metabolism.
What may elevated creatinine levels suggest?
Renal disease since excretion is impaired
Why is an accurate estimated Glomerular Filtration Rate (eGFR) important?
-Detecting the onset of renal insufficiency
-Adjusting drug dosages
-Evaluating therapies for patients with CKD (when to begin dialysis, transplant eligibility)
What is the BUN to creatinine ratio used for? (BUN:Cr)
-Helps to determine cause of azotemia
Low BUN/Creatinine Ratio
acute tubular necrosis (inside kidney), low protein intake, starvation, severe liver disease
elevated BUN and creatinine (depending with normal Cr or elevated Cr values)
-Normal Cr values: tissue breakdown, prerenal azotemia, high protein intake
-Elevate Cr: postrenal obstruction, prerenal azotemia associated with renal disease
Causes for hypoglycemia?
too much exogenous insulin (most common), pancreatic malignancy, glycogen-storage disease, additional endocrine abnormalities
Can be life threatening
Causes for hyperglycemia?
diabetes (most common), traumatic brain injury, fever, certain liver diseases, various endocrine abnormalities, stress
Where is magnesium usually found and its importance?
-Second most abundant intracellular ion found mainly in bone and muscle with small amount in serum and RBC
-Importance in cardiovascular metabolic, and neuromuscular disorders
Conditions associated with Hypomagnesemia?
-Most commonly seen in ICU patients
-Can be seen in diuretic use, patients on digitalis Digoxin-antiarrhythmic), diarrhea, vomiting, malabsorption, and alcoholism
-can result in cardiac arrhythmias, neuromuscular hyperexcitability (seizures)
What conditions can be seen with hypermagnesemia?
-Seen less frequently because it will likely have to reach 10 mg/dL until we see symptoms
-Seen in renal failure and increased intake of magnesium containing medications
-Can result in decreased deep tendon reflexes and apnea.
What regulates phosphate levels?
-Serum concentration primarily determined by kidneys (urinary excretion increased by PTH)
- Also regulated by PTH, vitamin D (increases absorption) , and growth hormone (decreases renal excretion)
Conditions associated with hypophosphatemia?
refeeding syndrome (giving starving people food to quickly), alcohol use disorders, decreased intestinal absorption, chronic diarrhea, and some medications (antacids, diuretics)
Possible signs and symptoms of hypophosphatemia?
muscle weakness, acute respiratory failure (phosphate needed for diaphragm function), tissue hypoxia, and confusion
Conditions associated with hyperphosphatemia?
acute phosphate load (release of intracellular ions resulting from marked tissue breakdown such as tumor lysis syndrome, ingesting large amounts of exogenous sources (laxatives containing phosphate), and kidney disease
Possible signs and symptoms with hyperphosphatemia?
tetany (severe muscle spasms), seizures, and hypotension
What is uric acid and where is it produced?
-End product of protein metabolism
-Produced in the liver
What can elevated uric acid indicate?
-Increased protein breakdown
-Renal disease
What conditions are associated with hypouricemia?
-Rare
-Decreased uric acid production, certain medications, renal disease, AIDS, increased clearance, malignancy
What conditions are associated with hyperuricemia?
obesity, diet, alcohol, some genetic conditions, renal disease, dehydration, and certain medications
-May result in gout, kidney stones, and CKD.