3. Skeletal system
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Define skeletal system
Framework of cartilage and bones (organs) interrupted by joints
Why are bones classified as organs in the body?
Bones are considered organs because they are made up of different types of tissues that work together to perform specific functions, such as support, protection, and movement.
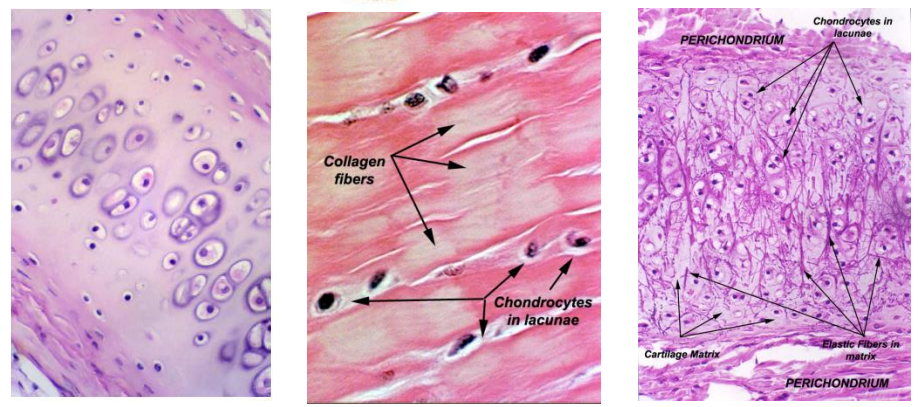
What are the three major types of cartilage, and how do they differ in structure?
Hyaline cartilage has fine fibers in a gel-like matrix (left picture)
Fibrocartilage contains large bundles of collagen (middle picture)
Elastic cartilage has a matrix of elastic fibers (right picture)
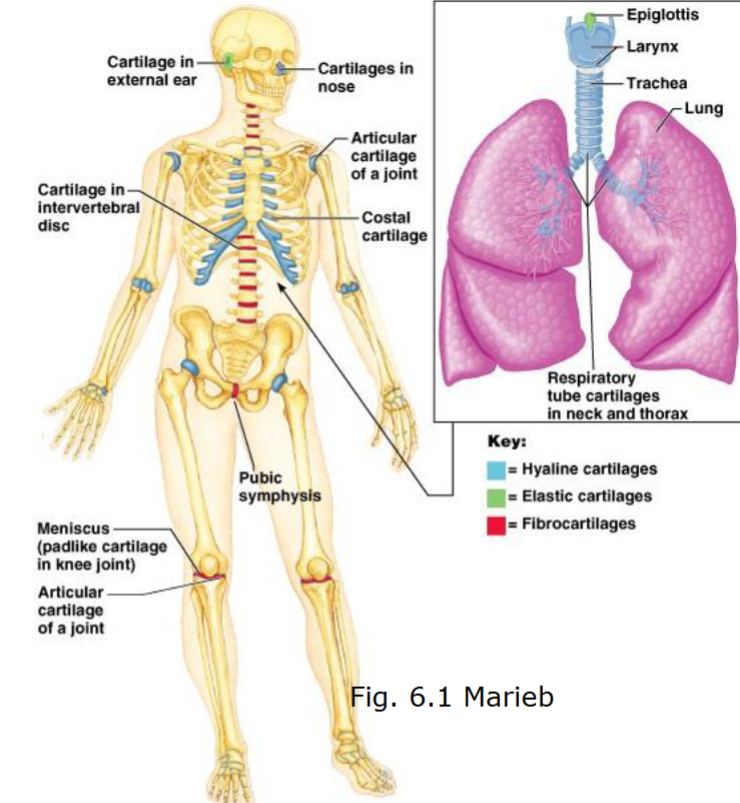
Which type of cartilage is most commonly found in the body, and where is it typically located?
Hyaline cartilage is the most common and is found in most joints (articulations)
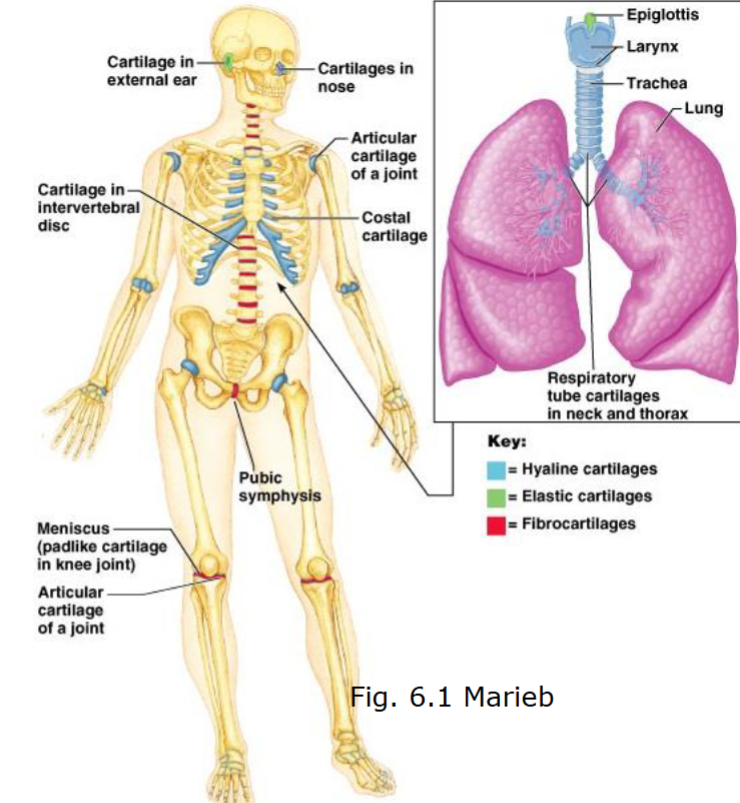
Where is elastic cartilage found, and what is its function?
Elastic cartilage is found in areas requiring flexibility, such as the epiglottis
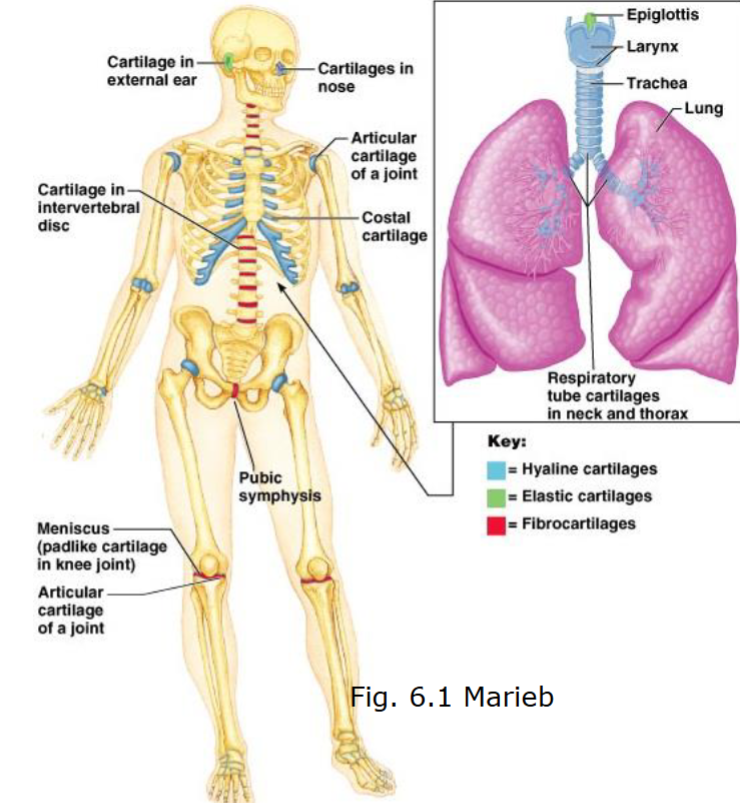
Where is fibrocartilage found, and what is its function?
The function of fibrocartilage is to resist compression and tension forces and can be found in e.g. anulus fibrosus
What are the main types of tissues that make up bones as organs?
Bones are made up of connective tissue (bone, cartilage, adipose, and blood), epithelial tissue (blood vessels), and nervous tissue (nerves).
How do bones contribute to the support of the body?
Bones provide a framework to support body weight and serve as attachment points for soft tissues.
In what way do bones assist with movement?
Bones act as a lever system that helps muscles generate a large range of movement.
Which parts of the skeleton provide protection for vital organs, and what specific organs do they protect?
The skull protects the brain, the rib cage protects the heart and lungs, the vertebral column protects the spinal cord, and the pelvis protects reproductive organs.
How do bones function in mineral storage, and which minerals are primarily stored?
Bones store calcium and phosphate, which can be released into the bloodstream when needed.
What role do bones play in blood cell production and energy storage?
Red and white blood cells are produced in the red bone marrow, and bones also store energy in the form of fat.
How does the hormone osteocalcin influence energy metabolism in the body?
Osteoblasts produce osteocalcin, which plays a role in energy metabolism by influencing bone production, regulating fat storage, and stimulating insulin production.
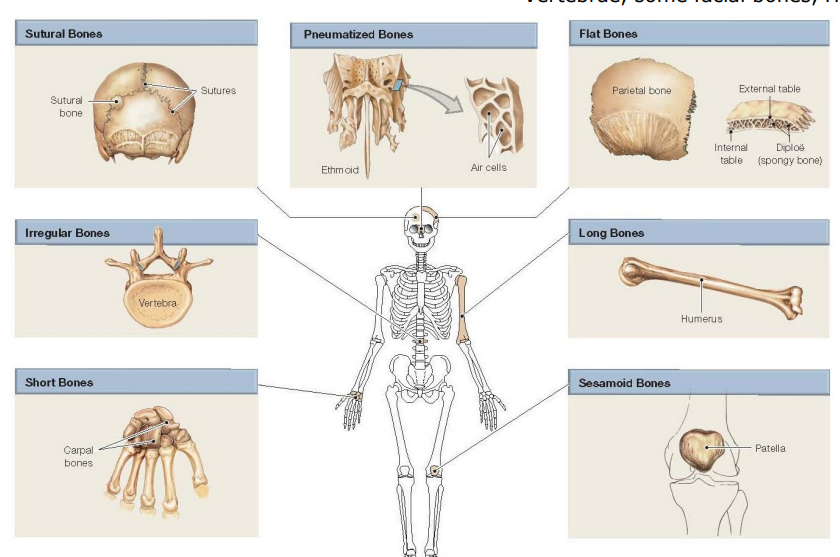
Bones can be classified according to shape, and what are the main categories?
Bones are classified into seven main categories based on shape: long bones, short bones, flat bones, sutural bones, pneumatized bones, irregular bones, and sesamoid bones.
What are flat bones, and where can they be found in the body?
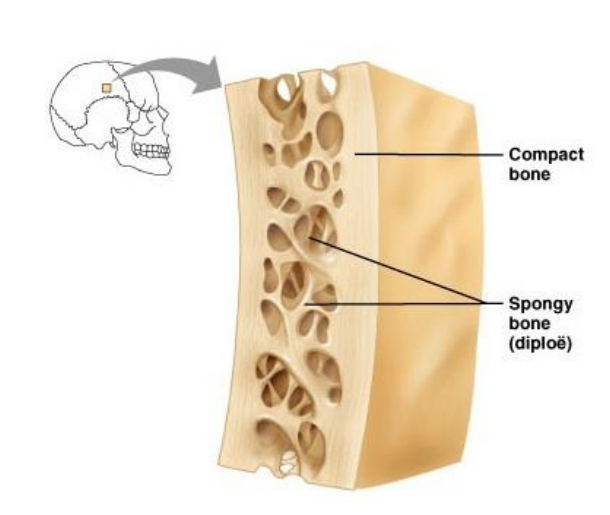
Flat bones consist of thin layers of compact bone surrounding spongy bone. Examples include the roof of the skull, ribs, sternum, and scapula.
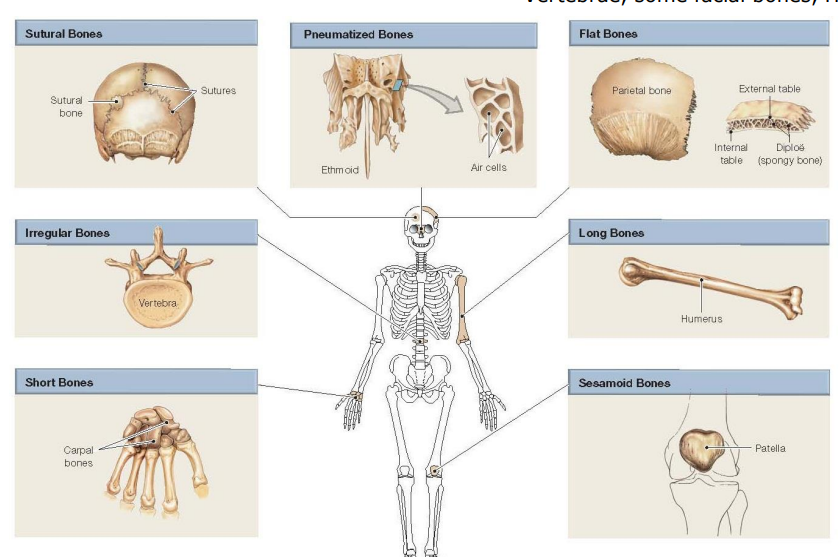
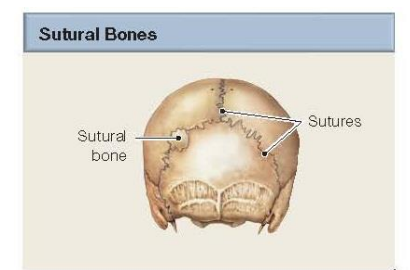
What are sutural bones?
Sutural bones consist of oddly shaped bones inserted between flat bones of skull. Structurally they are flat bones.
What are pneumatized bones, and can you provide an example?
Pneumatized bones are bones that are hollow or contain air pockets. An example of a pneumatized bone is the ethmoid bone found in the skull
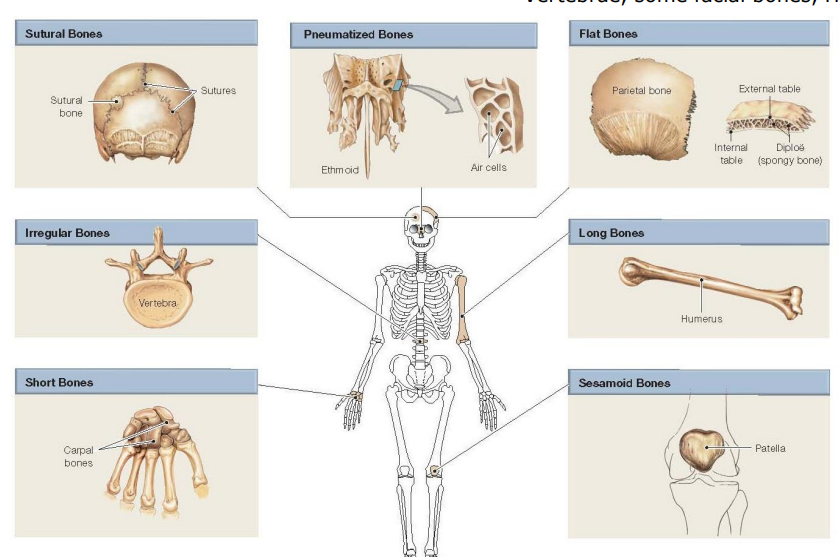
What are long bones, and where can they be found in the body?
Long bones have an elongated shape and are found in the limbs, such as the femur, humerus, and phalanges (fingers and toes).
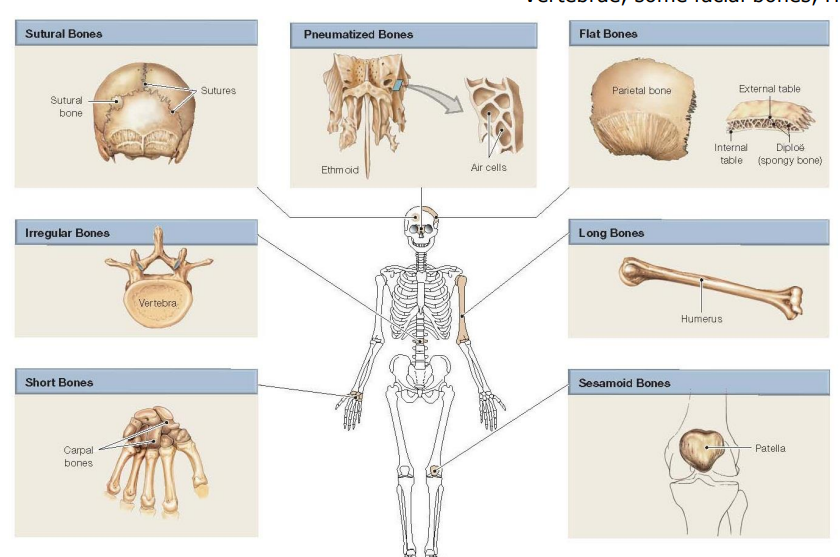
What are short bones, and where can they be found in the body?
Short bones are roughly box-shaped, with examples including the carpals (wrist bones) and tarsals (ankle bones).
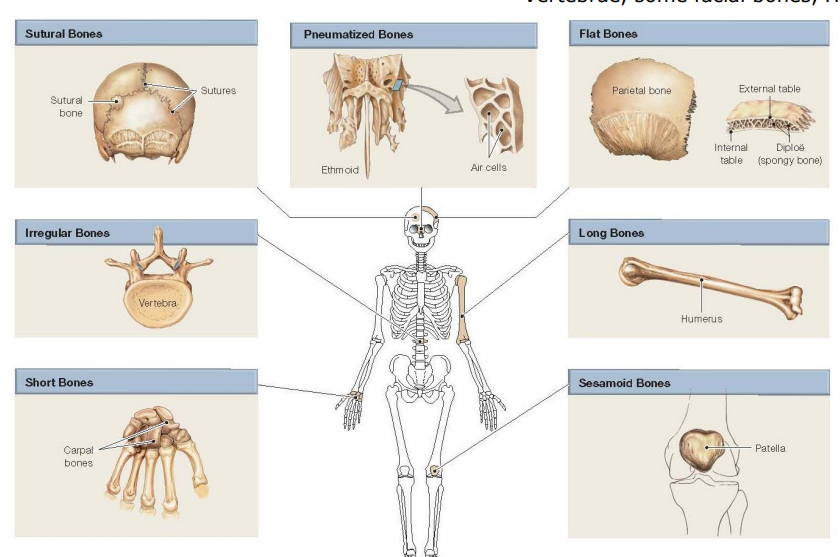
What are sesamoid bones, and where can they be found in the body?
Sesamoid bones are embedded within tendons (senor) and help protect them from stress, with the patella (kneecap) being a common example.
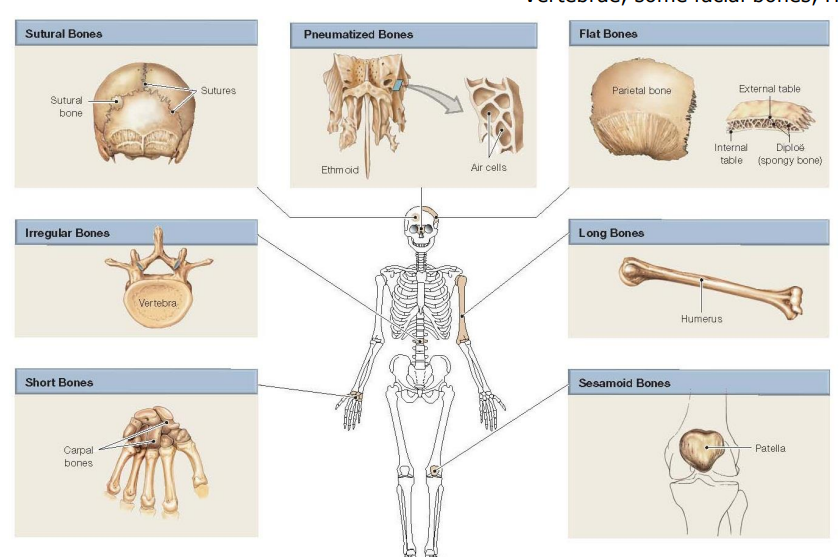
What are irregular bones, and where can they be found in the body?
Irregular bones have varied shapes that don’t fit into other categories, with examples including vertebrae, certain facial bones, and the calcaneus (heel bone).
What specific types of tissues are found in a typical long bone like the femur?
The femur is composed of connective tissue (bone tissue), cartilage (articular cartilage at the joints), adipose (fat) tissue (in the marrow), blood (within the bone and blood vessels), and nervous tissue (nerves associated with the bone).
What are the main differences in location between compact bone and spongy bone within a typical bone structure and what are their functions?
Compact bone is found in the external layer (cortex) of bones, providing strength and support
Spongy bone is located internally and consists of trabeculae. Spongy bone’s functions are to reduce weight of bones and support and protect red bone marrow
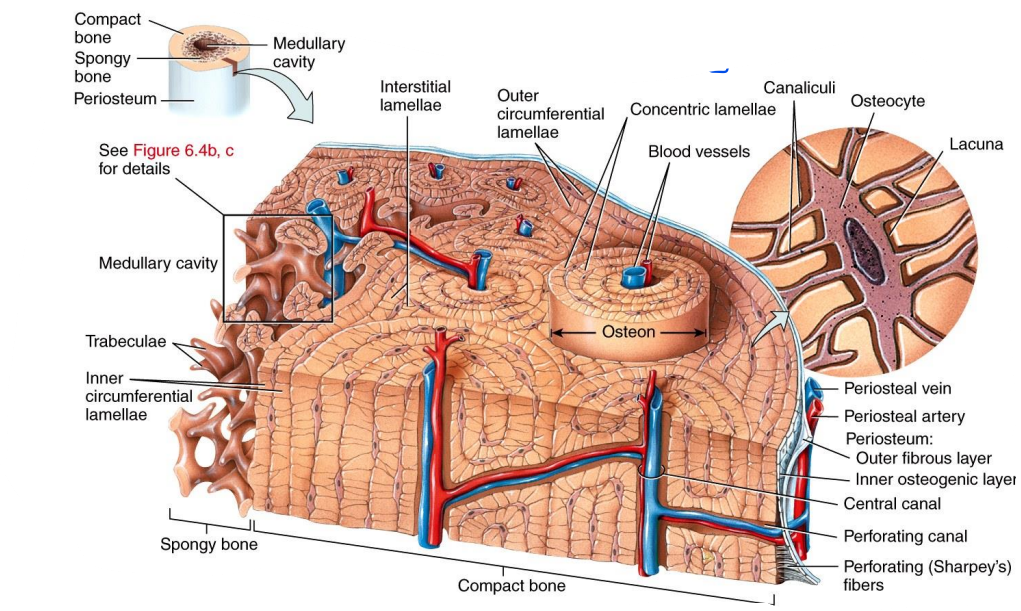
What is the basic structural unit of compact bone, and what are its key components?
The basic structural unit of compact bone is the osteon (or Haversian system), which consists of concentric lamellae (layers of bone matrix), a central canal (Haversian canal), canaliculi (small channels), and osteocytes (bone cells in lacunae).
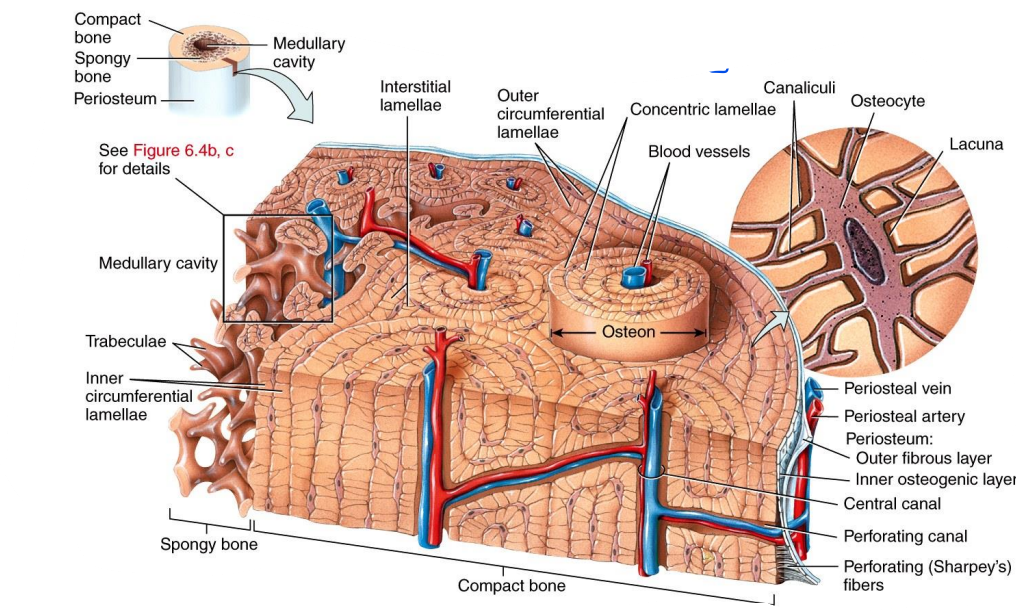
What is the microscopic structure of spongy bone?
The microscopic structure of spongy bone consists of trabeculae, which are thin, lattice-like plates that create a network.
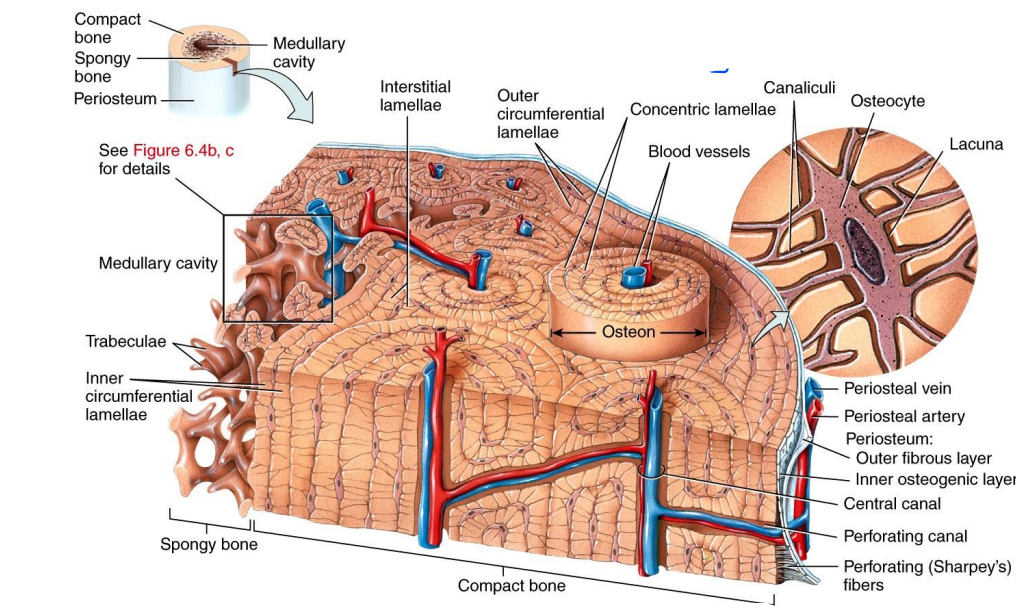
How are trabeculae organized in spongy bone to provide support while reducing weight?
These trabeculae are organized along lines of stress, providing structural support while minimizing the overall weight of the bone.
How do osteocytes in lacunae receive nutrients, and what role does the endosteum play in this process?
Osteocytes in lacunae receive nutrients through diffusion from blood vessels located in the endosteum.
What is the composition of the extracellular matrix in bone tissue, and what are its main components?
The extracellular matrix in bone tissue is composed of 15% water, 30% collagen fibers, and 55% minerals, which include hydroxyapatite, calcium phosphate, magnesium, fluoride, potassium, and sulfate.
What does each component of the extracellular matrix provide to its overall functions?
Collagen fibres provide elasticity
Mineral salts provide rigidity
Collagen fibres provide an organic framework on which crystals can form. Allows bone to strong, somewhat flexible and highly resistant to shattering
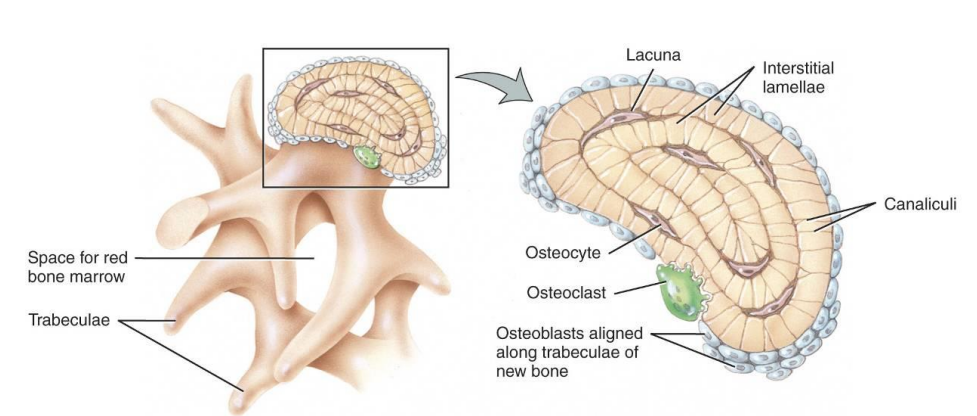
Name four cells that are present in bone tissue
Osteogenic (osteoprogenitor) cells
Osteoblasts
Osteocytes
Osteoclasts
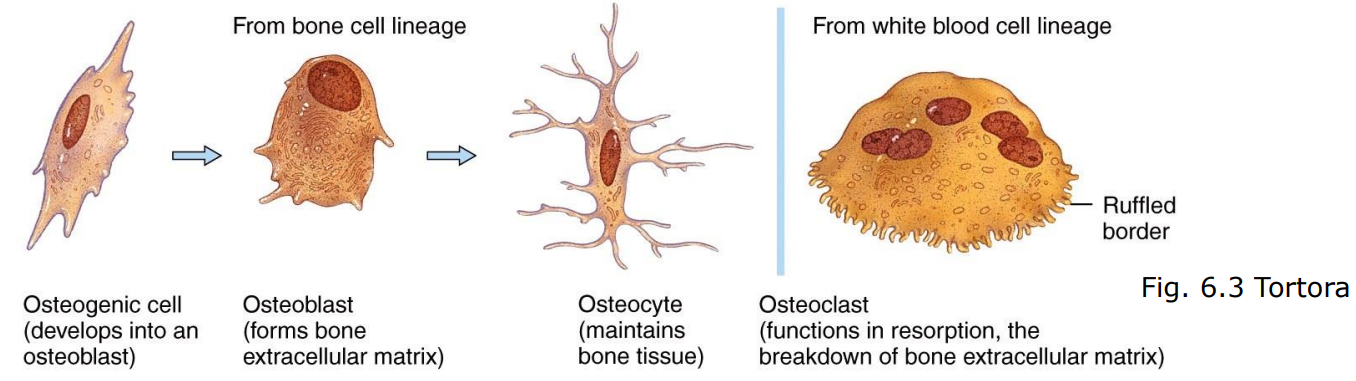
Describe the function of osteogenic (osteoprogenitor) cells in bone tissue and where they can be found
Osteogenic cells are unspecialized bone cells that can divide and differentiate into other bone cell types. They are found in the inner and outer lining of bones (endosteum and periosteum)
What are osteoblasts, and how do they contribute to the formation of bone?
Osteoblasts are bone-building cells that secrete collagen fibers and initiate the calcification process. They eventually surround themselves with the matrix they produce and differentiate into osteocytes.
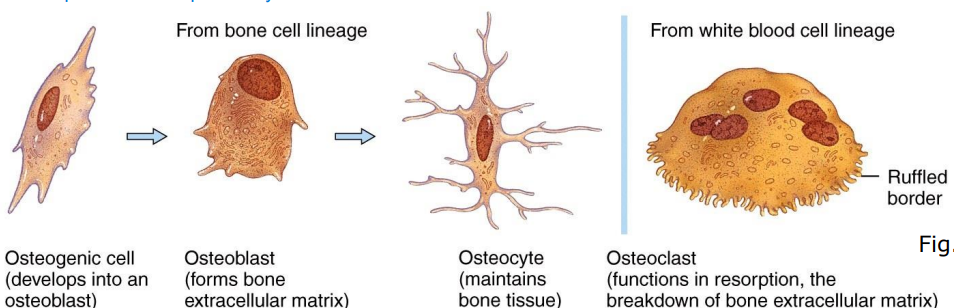
What is the main function of osteocytes in healthy bone tissue?
Osteocytes are the main cell type in healthy bone, responsible for the maintenance and metabolism of bone tissue
How do osteoclasts differ from other bone cells, and what is their role in bone tissue?
Osteoclasts are derived from white blood cells and are concentrated in the endosteum. They are active in bone growth and remodeling, as well as resorption, which helps regulate calcium levels by removing and recycling bone tissue.
How do bones withstand tension and compression forces, and what is the importance of aligning compact and spongy bone tissues along lines of stress?
Bones withstand tension and compression forces due to their unique structural composition and alignment. The alignment of compact and spongy bone tissues along lines of stress is crucial for optimizing their mechanical performance.
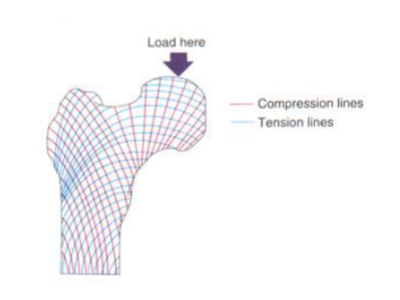
In what ways are compact and spongy bone tissues aligned to accommodate lines of stress?
Compact bone is thicker in areas subjected to greater forces, providing strength and support, while spongy bone is arranged in a mesh-like structure that aligns with lines of stress to better counteract multidirectional tension and compression forces.
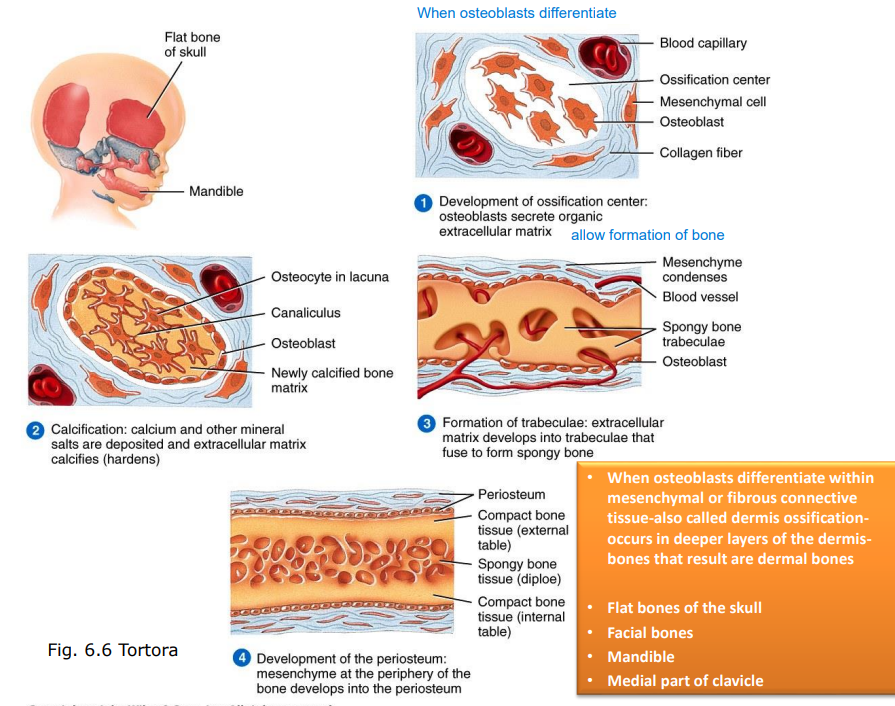
How does intramembranous ossification differ from endochondral ossification?
Intramembranous ossification occurs directly within fibrous connective tissue, leading to the formation of bone without a cartilage intermediate.
In contrast, endochondral ossification involves the formation of a cartilage model that is subsequently replaced by bone tissue.
What types of tissue comprises femur?
Bone tissue - both compact and spongy bone
Cartilage - articular cartilage at joints
Endosteum - thin membrane that lines the inner surface of the femur
Periosteum - dense layer of connective tissue that covers the outer surface of the femur
Medullary Cavity - hollow center of the femur contains yellow bone marrow
Red bone marrow is primarily found in the epiphyses (the ends) of the femur.
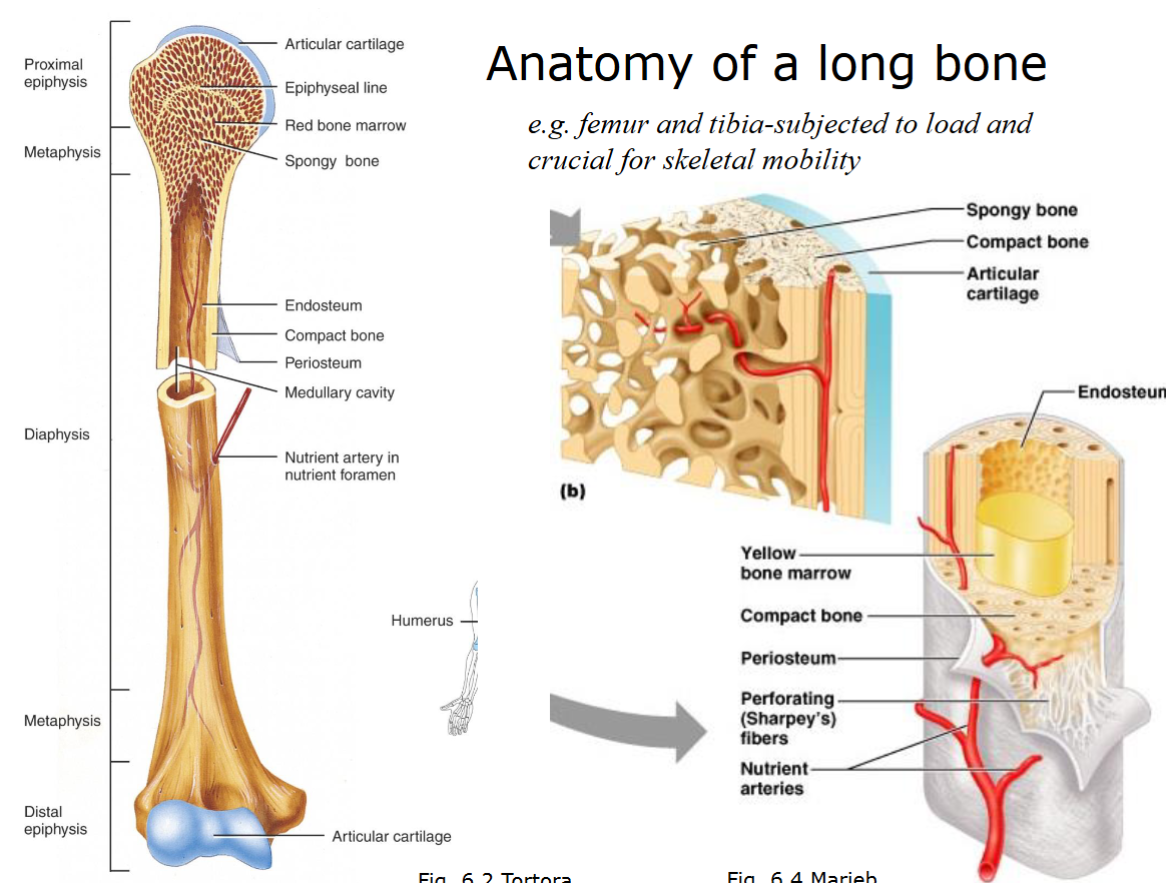
What are the main structural components of a typical long bone?
A typical long bone consists of the diaphysis (shaft), epiphyses (ends), metaphysis (wide portion of a long bone), medullary cavity (hollow space filled with yellow bone marrow), periosteum (outer covering), and nutrient arteries. The diaphysis is primarily composed of compact bone, while the epiphyses contain spongy bone and red bone marrow.
Describe the structure of flat bones and how it differs from long bones.
Flat bones consist of two outer layers of compact bone (external and internal tables) covered by the periosteum with a central layer of spongy bone known as diploë. Endosteum lines internal surface of the spongy bone.
Unlike long bones, flat bones do not have a medullary cavity; instead, red bone marrow is found within the spongy bone.
What is endosteum?
Single layer of osteoprogenitor cells
What is periosteum composed of?
Outer fibrous layer and inner cellular layer (osteoprogenitor cells).
What is the primary difference between intramembranous and endochondral ossification?
Intramembranous ossification forms bone directly from mesenchymal tissue, without a cartilage intermediate.
In contrast, endochondral ossification involves the formation of bone from a cartilage intermediate, generally, this intermediate cartilage is hyaline cartilage.
What types of bones are formed by intramembranous and endochondral ossification?
Intramembranous ossification is responsible for the formation of flat bones such as the skull, clavicle (collarbone), mandible (lower jaw) and facial bones.
Endochondral ossification forms long bones like the femur, tibia, and bones at the base of the skull
What are the key steps in intramembranous ossification?
Mesenchymal cells differentiate into osteoblasts, forming an ossification center.
Osteoblasts secrete organic exracellular matrix, which calcifies.
Formation of trabeculae: extracellular matrix develops into trabeculae that fuse to form spongy bone
Development of the periosteum:
Mesenchyme at the periphery of the bone develops into the periosteum
What are the key steps in endochondral ossification?
Mesenchymal cells differentiate into chondrocytes to form cartilage.
Cartilage calcifies and chondrocytes die. Cartilage is replaced by bone tissue.
Development of medullary cavity: Osteoclast breakdown bone to form medullary cavity
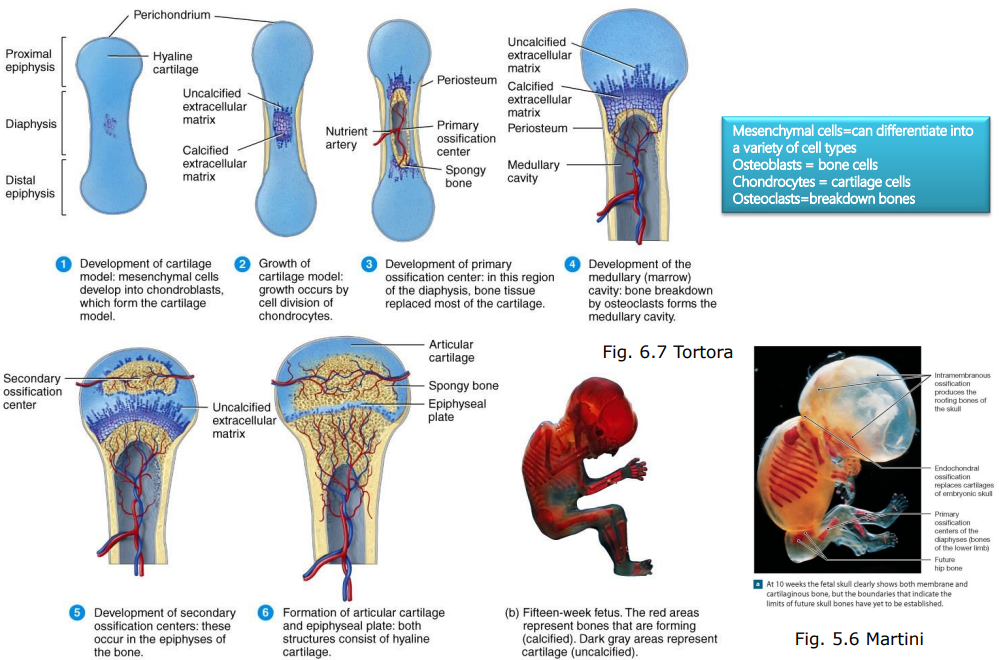
When do endochondral and intramembranous ossification typically stop?
Endochondral ossification stops around age 2, while intramembranous ossification continues until about 18 years in females and 21 years in males.
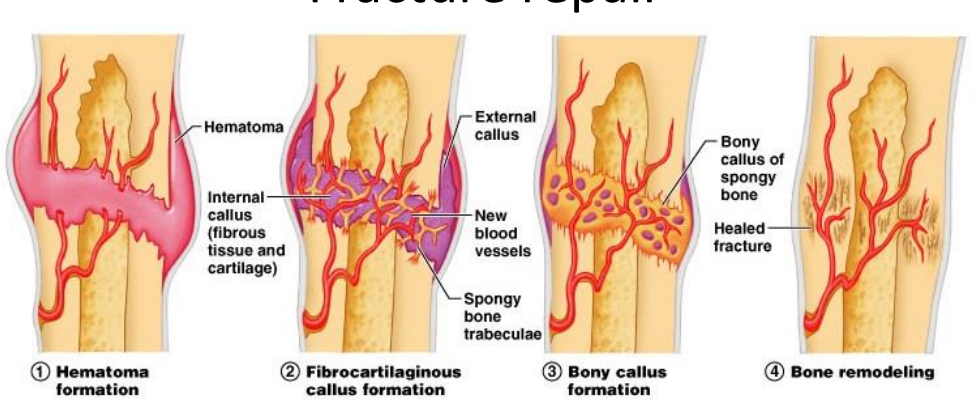
What are the main stages of bone fracture repair?
Hematoma formation: Blood leaks from broken blood vessels, leading to the formation of a hematoma (blood clot).
Fibrocartilaginous callus formation: A few days after the fracture, new blood vessels form across the hematoma, and fibrocartilage begins to form.
Bony callus formation: Around 1.5 weeks after the fracture, trabeculae of spongy bone begin to form, and the callus solidifies within two months.
Bone remodeling: Over the following months, compact bone is formed, and excess bone material is removed as the bone remodels along lines of stress.
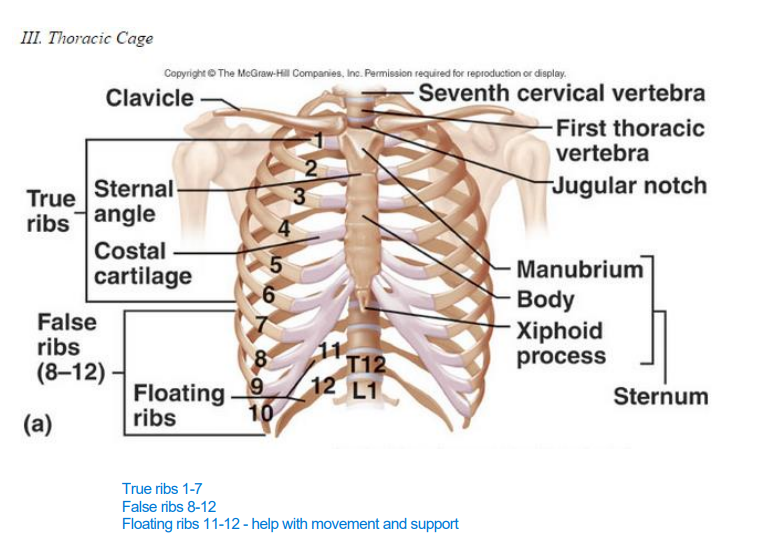
What bones are included in the axial skeleton, and what is its main function?
The axial skeleton consists of the skull, vertebral column, and thoracic cage (including ribs and sternum). Its primary functions are to protect the brain, spinal cord, and vital organs in the thoracic cavity, support body weight, and maintain postur
What bones are part of the appendicular skeleton, and what is its primary function?
The appendicular skeleton includes the bones of the upper and lower limbs and the girdles (pectoral and pelvic) that attach them to the axial skeleton. The appendicular skeleton's primary role is to facilitate movement
How does the vertebral column contribute to body function and movement?
The vertebral column supports body weight, protects the spinal cord, and allows for movement and flexibility. Its curvature provides shock absorption, and intervertebral discs cushion between vertebrae, permitting limited motion
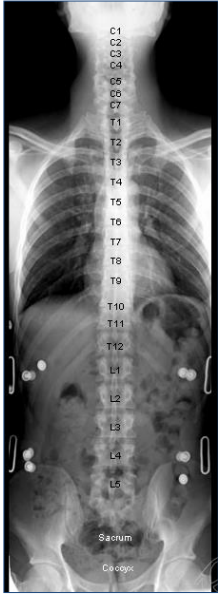
How is the vertebral column divided, and how does each region differ?
The vertebral column is divided into five regions:
Cervical (7 vertebrae, C1-C7): located in the neck, responsible for supporting the head and allowing neck movement. Greatest range of movement
Thoracic (12 vertebrae, T1-T12): provide attachment for ribs, providing stability and protecting the thoracic organs. Greatest degree of rotation-due to location of articular facets
Lumbar (5 vertebrae, L1-L5): supports much of the upper body's weight and is located in the lower back.
Sacrum (5 fused vertebrae): forms the posterior part of the pelvic girdle.
Coccyx (4 fused vertebrae): commonly referred to as the tailbone, it provides attachment for ligaments and muscles of the pelvic floor. Stabilise the sitting person
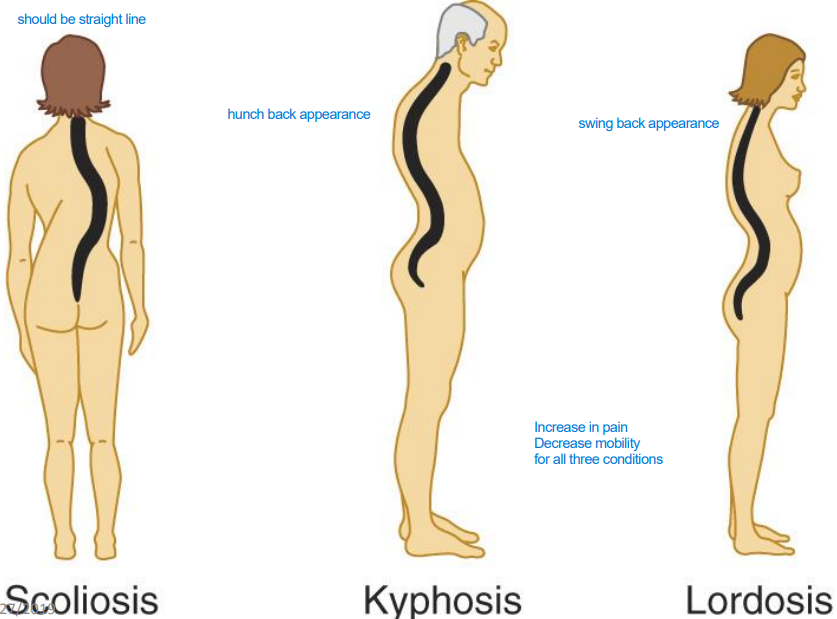
What clinical significance do the vertebral curvatures hold?
Normal vertebral curvatures help distribute body weight and maintain balance. Abnormal curvatures, such as scoliosis (lateral curve), kyphosis (hunchback), and lordosis (swayback), can lead to pain, decreased mobility, and may require medical intervention
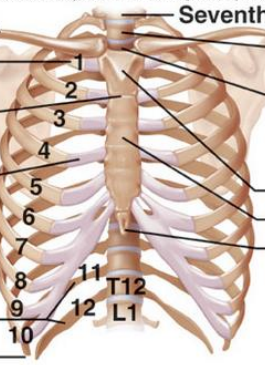
What is the difference between true ribs, false ribs, and floating ribs?
True ribs (1-7): These are directly attached to the sternum via costal cartilage.
False ribs (8-10): These are indirectly attached to the sternum through the cartilage of the ribs above them.
Floating ribs (11-12): These do not attach to the sternum at all, and instead terminate in the posterior abdominal wall
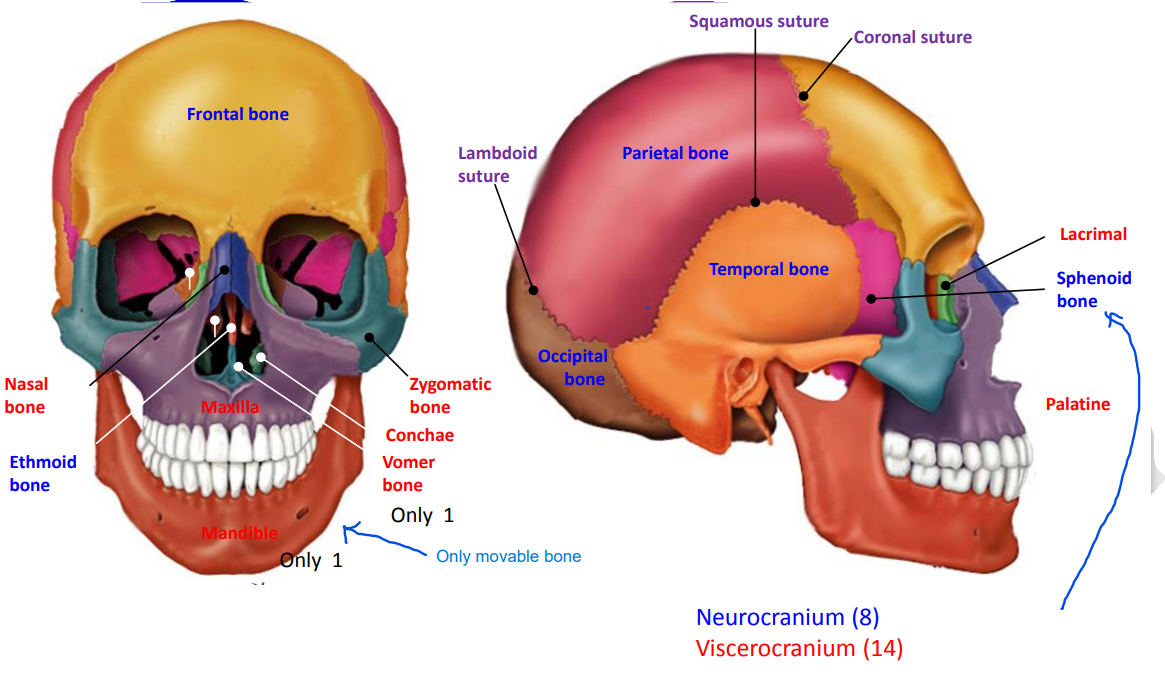
What is the difference between the neurocranium and the viscerocranium?
The neurocranium protects the brain, while the viscerocranium, or facial skeleton, supports the face and houses the cavities for sensory organs.
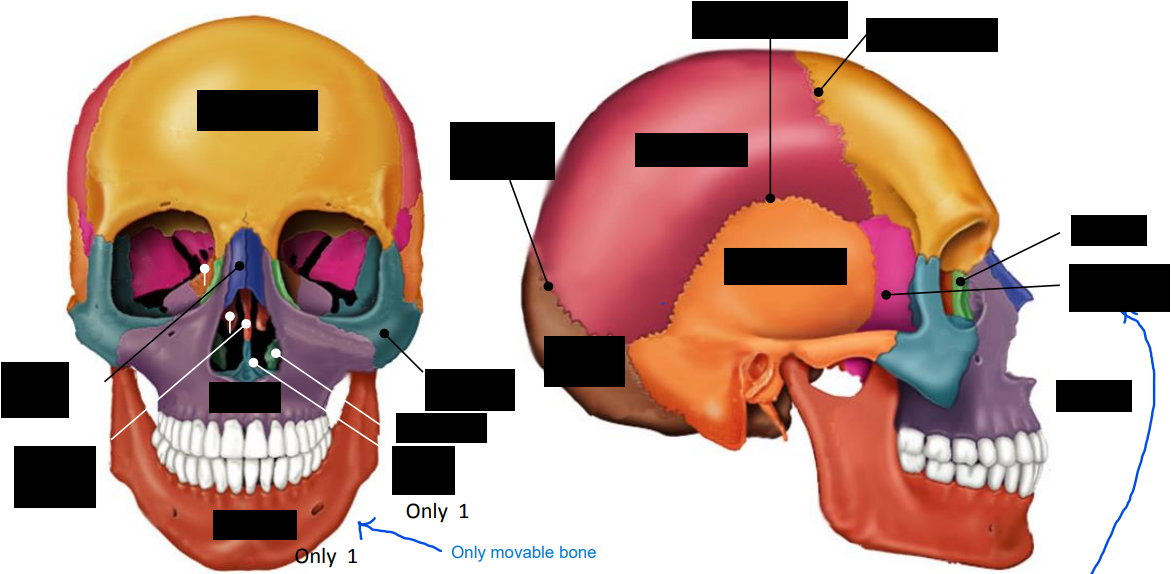
How many bones are found in the viscerocranium, and what are they?
The viscerocranium consists of 14 bones: nasal bones (2), maxillae (2), zygomatic bones (2), palatine bones (2), lacrimal bones (2), inferior nasal conchae (2), vomer (1), and mandible (1). purposegames.com
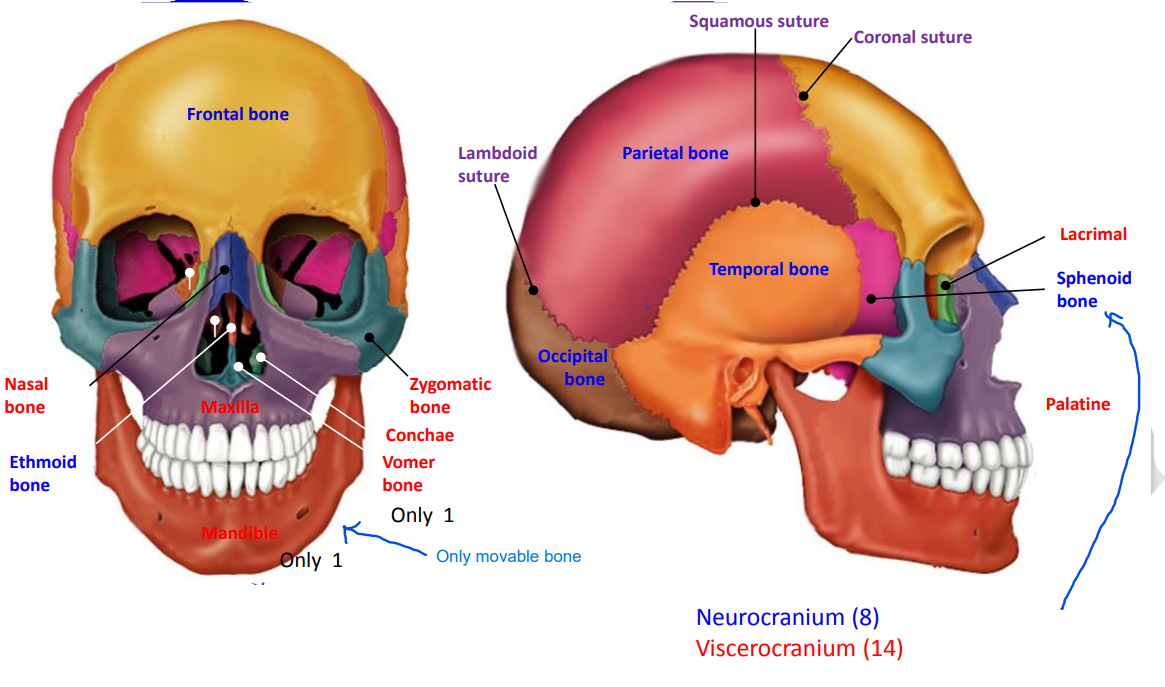
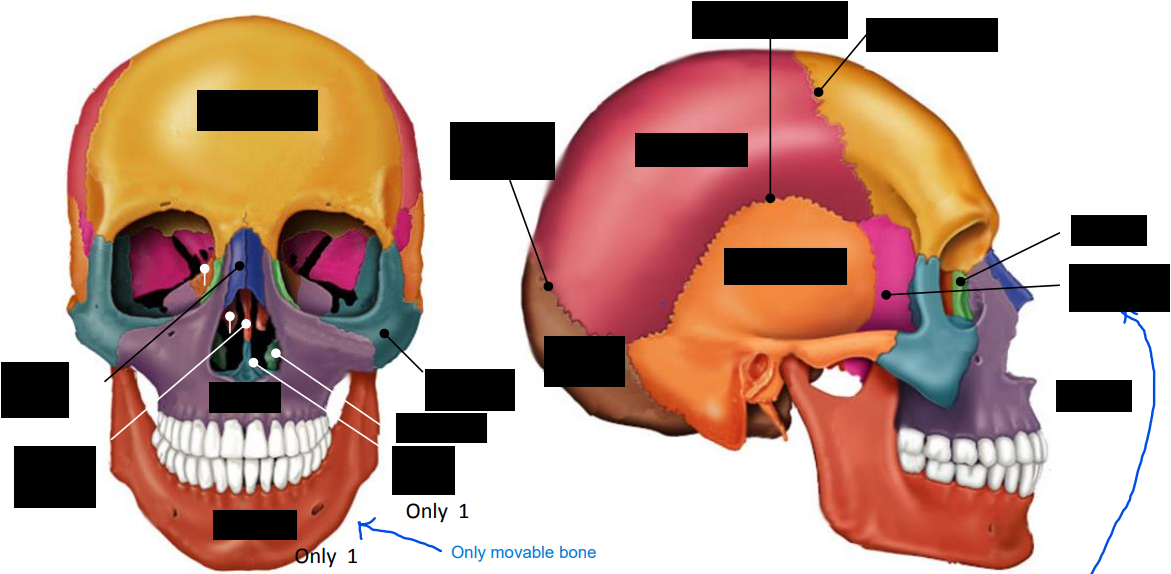
How many bones make up the neurocranium, and can you list them?
The neurocranium is made up of 8 bones: the frontal bone, parietal bones (2), temporal bones (2), occipital bone, sphenoid bone, and ethmoid bone.
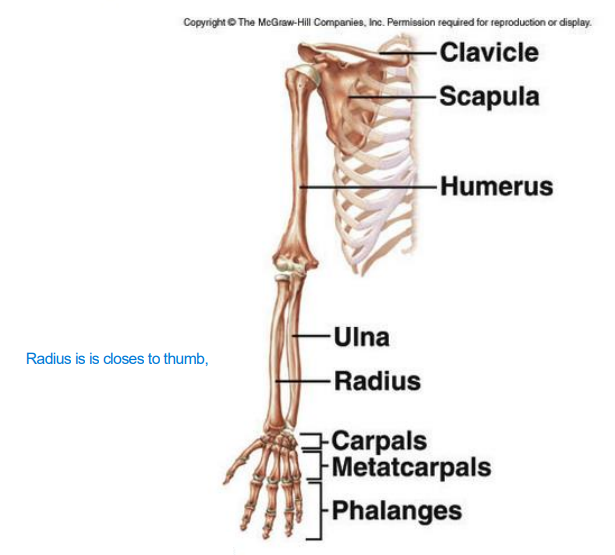
What are names of bones in upper limb and pectoral girdle?
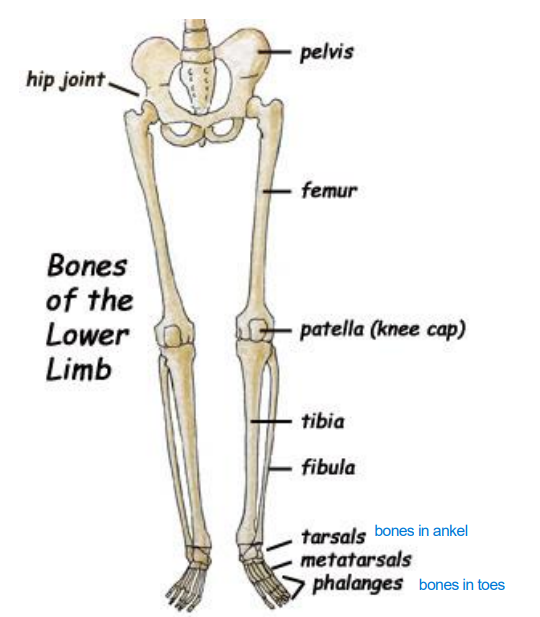
What are names of bones in lower limb and pelvic girdle?
tibia closes to big toe
fibula
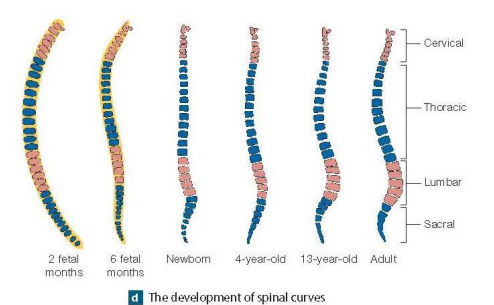
What are the four curvatures of the adult vertebral column?
The adult vertebral column has four curvatures: two primary curvatures (thoracic and sacral) that are present at birth, and two secondary curvatures (cervical (babies can’t lift their heads) and lumbar) that develop later as the child grows and begins to hold its head up and walk.
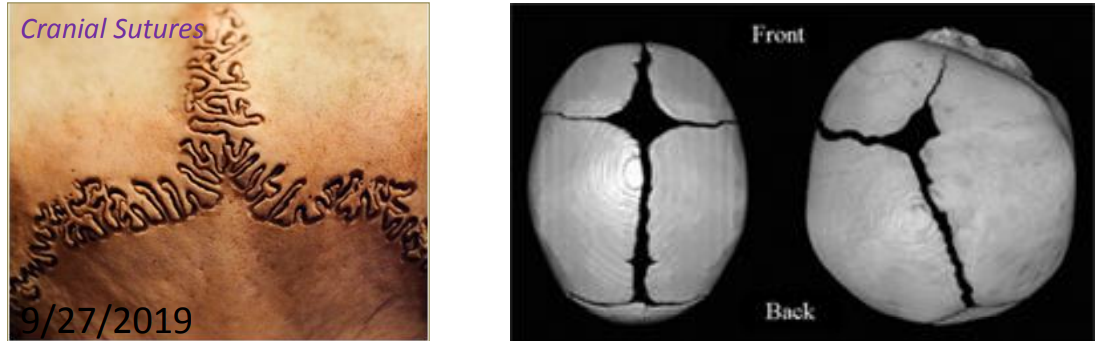
What are cranial sutures, and what role do they play in the skull in adults versus newborns?
Cranial sutures are thin layers of dense fibrous connective tissue found between the bones of the skull. In adults, they appear as seams connecting the skull bones, while in newborns, they consist of linear attachments of fibrous tissue and fontanelles, allowing for skull flexibility during birth and growth.
What are the implications of a cervical spine fracture above the C4 vertebra?
A cervical spine fracture above the C4 vertebra can cause paralysis of the diaphragm, which may lead to sudden death due to respiratory failure.
What is the expected outcome of a spinal fracture at the cervical level below C4?
A fracture at the cervical level below C4 may result in quadriplegia, characterized by the loss of motor and sensory function in all four limbs.
How does a fracture in the thoracic region affect the body?
A fracture in the thoracic region may result in paraplegia, which is the loss of function in the lower extremities while typically preserving arm function.
What are the potential effects of lumbar region fractures?
Fractures in the lumbar region can lead to variable sensory and motor loss in the lower extremities, which may affect mobility and function depending on the severity of the injury.
What are the special features of the first two cervical vertebrae (C1 and C2)?
C1 (the atlas) and C2 (the axis) are specialized to accommodate the skull. The atlas supports the head and allows for the nodding motion, while the axis has a peg-like projection called the odontoid process (or dens) that enables the head to rotate.
What is the shape and surface characteristics of the vertebral body?
The vertebral body is short and square-shaped, with a concave superior surface that interfaces with the vertebra above and a convex inferior surface that interfaces with the vertebra below.
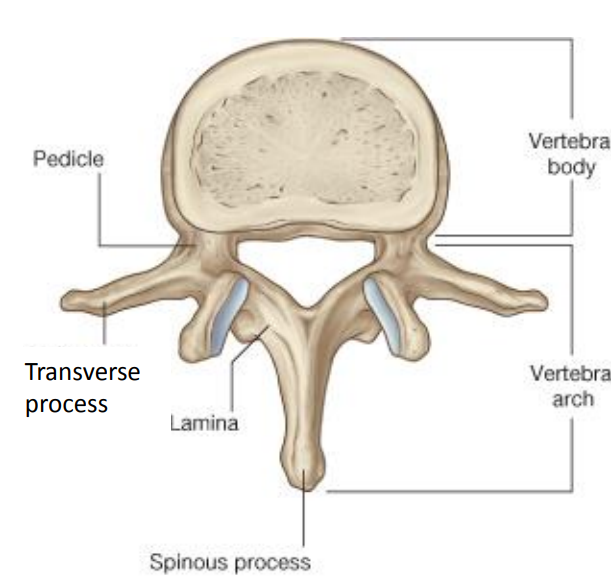
What is the shape of the vertebral arch?
The vertebral arch is typically described as having a triangular shape
How many processes does a typical vertebra have, and what are their functions?
A typical vertebra has seven processes: two transverse processes for muscle attachment and movement, one spinous process felt through the skin for muscle attachment and movement, and four articular processes that restrict movement.
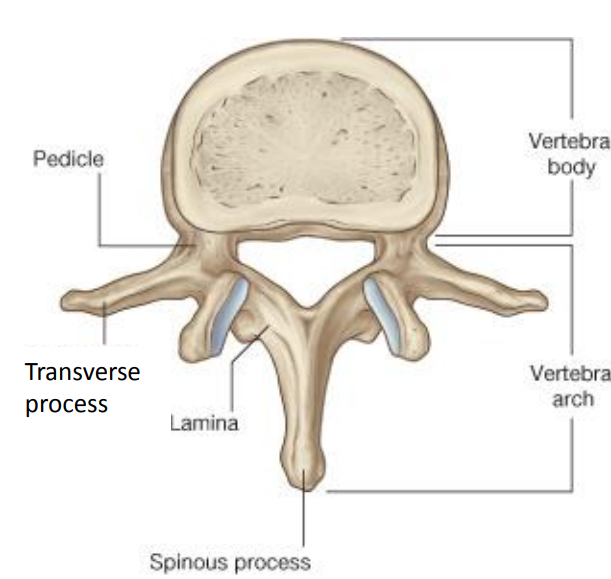
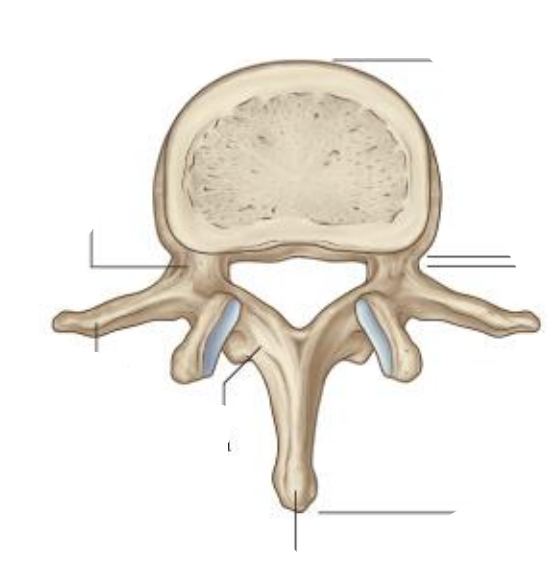
Where are pedicles and laminae located vertebral?
The pedicles are the lateral walls of the vertebral arch. The laminae form the posterior walls of the arch.
How do the thicknesses of intervertebral discs vary along the vertebral column?
The intervertebral discs are thinnest in the cervical region and progressively become thicker towards the lumbar region.
What are the two main components of an intervertebral disc, and what are their functions?
The two main components are the nucleus pulposus, which is a soft, pulpy, elastic material that acts as a shock absorber, and the anulus fibrosus, which is a concentric ring of fibrous tissue and fibrocartilage that provides structural support.
What does a "slipped disc" refer to, and what causes this condition?
A "slipped disc" is a misleading term that describes a tear in the anulus fibrosus. This tear allows the nucleus pulposus to bulge out, which may put pressure on spinal nerves, leading to pain.
How does disc dehydration affect height, particularly in older adults?
Disc dehydration can contribute to a loss of height in individuals, accounting for as much as 1.8 cm in men. This thinning of discs with age is a factor in the height loss commonly observed in the elderly.