RADT W3 Ch 19, 1, 2: Paralleling Technique, Radiation History and Biology
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
What are the 3 basic principles of the Paralleling Technique?
Film is placed parallel to the long axis of tooth being radiographed
Central Ray is directed perpendicular to film and long axis of tooth
Film holder must be used to keep film parallel to the long axis of tooth
How does Target-Film Distance (TFD) affect the radiograph?
Increased TFD = less magnification but more definition
Increased target-film distance (longer cone):
Reduces magnification
Increases image sharpness
Improves image quality
Short target-film distance:
More magnification and distortion
Less sharp image
Ideal: Use a longer distance (e.g. 16-inch cone) for better-quality radiographs.
What are some considerations for film selection?
Palate size
Torus
Floor of the mouth
Arch shape and size
Compare and contrast vertical angulation and horizontal angulation.
Vertical Angulation
Direction: Up and down; perpendicular to the film
Affects: Image length
Incorrect angulation: Foreshortening (too steep) or elongation (too shallow)
Critical in: Periapical radiographs
Horizontal Angulation
Direction: Side to side; open contacts
Affects: Overlapping of contacts
Incorrect angulation: Proximal/occlusal surfaces appear merged or unclear
Critical in: Bitewing radiographs
Key Difference:
Vertical = image height
Horizontal = contact clarity
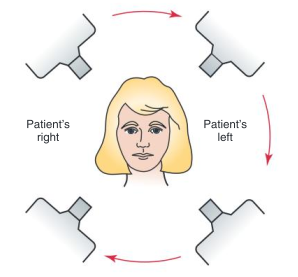
What is the suggested paralleling sequence for ANTERIOR exposure?
R Max. Canine → L Max. Canine
L. Mand. Canine → R Mand. Canine
When using size 2 film, how many exposures are required to cover all the Anterior teeth?
3 Max. exposures (2 canine, 1 incisors)
3 Mand. exposures (2 canine, 1 incisors)
When using size 1 film, how many exposures are required to cover all the Anterior teeth?
4 Max. exposures
3-4 Mand. exposures
What is the suggested paralleling sequence for POSTERIOR exposure?
Start: Q1 premolar → molar
Q3 premolar → molar
Q2 premolar → molar
Q4 premolar → molar
Total exposures: 4 max 4 mand
Due to the shallow nature of the palate, how do we adjust our technique to maintain parallelism between the film and the long axis of the teeth?
Use cotton roll under the bite block (you can use on both sides if required)

How are film placed when a client has bony growths (tori)?
Maxillary tori:
film should be placed on the far side of the torus; NOT on torus
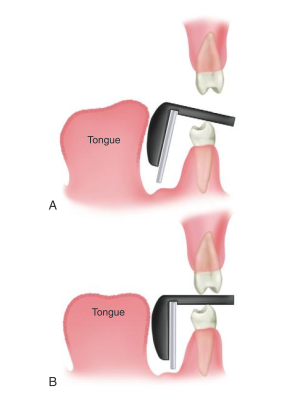
Mandibular tori:
film must be placed between the tori and the tongue
How should the film be placed for exposure in the Mandibular premolar region?
film is placed under the tongue to avoid impinging on muscle attachments
film is adjusted after the client closes down on the bite-block
What are the advantages and disadvantages of the paralleling technique?
Advantage:
Accuracy → minimal dimensional distortion if done correctly (good detail and definition)
Simple and easy to learn
Easy to standardize
Disadvantages:
Difficult film placement
Uncomfortable film-holding device for client
Who was the scientist that discovered xrays? What yr?
William C. Roentgen in 1895 → xrays are sometimes referred as Roentgen rays
Who was the scientist that exposed the early dental radiograph prototype?
Dr. Otto Walkoff
Dr. Edmund Kells was given the credit for what?
First intraoral radiograph made in 1896 on a living person in the US
What is the name of the company that manufactured the first pre-wrapped intraoral radiographic film?
Eastman Kodak Company
Who introduced the bisecting technique?
Weston Price in 1904
Who redefined the original bisecting technique and introduced the BITEWING technique in 1925?
Howard Riley Raper
What was Franklin W. McCormack’s contribution to radiation history?
Applied the paralleling technique in dental radiography during the 1920s.
Define Radiation
A form of energy carried by waves or stream of particles
Define X-Radiation
A high-energy radiation produced by the collision of a beam of electrons with a metal target in an x-ray tube.
Define X-Ray
A beam of energy that has the power to penetrate substances and record image shadows on photographic film.
→ often used to describe a radiograph which is incorrect. It is the beam.
Who is considered to be the father of panoramic radiography?
Yrjö Paatero (a Finnish dentist) is considered the father of panoramic radiography
Developed the technique in the 1940s–1950s
What is Radiation Biology?
The study of the effect of ionizing radiation on living tissue so that we can better understand the harmful effects of radiation.
Define Ionization
Ionization is produced through photoelectric effect or Compton scatter
How does radiation cause injury?
X-rays strike the client causing ionization. Ionization causes chemical changes at the celluilar level which then can cause biological damages.
How do free radical formation cause injury?
Unstable free radical will want to bind and recombine to regain stability which can create damaging compounds. (ex. H2O2 (hydrogen peroxide)
Unstable free radical will steal electrons from healthy stable atoms which can damage healthy cells/tissues/dna leading to disease/cancer
Free radicals form when x-ray photon ionizes water (primary component of living cells).
Water ionization = Hydrogen + hydroxyl free radicals.
Free radicals are uncharged atoms/molecules that exist with a single unpaired eletron in its outer shell making the atom unstable and highly reactive.
What is the Direct Radiation Theory?
The theory that cell damage occurs as a direct result of ionizing radiation targeting critical areas.
Ex. Xray photon directly striking DNA cell causing injury to irradiated organism
Occurs infrequently but is more severe damage (most xray photons just pass through cells and cause little damage)
What is the Indirect Radiation Theory?
The theory that x-ray photons are being absorbed within the cell causing “toxins” therefore damaging the cell.
Ex. Free radicals combine to form toxins causing cellular dysfunction and biological injury
Occurs frequently because of the high water content in the cells (70-80%)
What is the Dose-Response-Curve?
The correlation between the response and damage of tissues with the dose or amount of radiation received.
Graph showing the relationship between radiation dose and biological effect
Helps determine how much damage occurs at different exposure levels
Explain the Threshold Curve
A type of Dose-Response curve that indicates that below a certain level (threshold) no response is evident.
Explain the Linear Curve
A type of Dose-Response Curve that indicates that the response (injury) is proportional to the dose.
Explain the Linear Non-Threshold curve.
A type of Dose-Response Curve that indicates that a response is seen at any dose.
Define Stochastic
randomly determined; having a random probability distribution or pattern that may be analysed statistically but may not be predicted precisely.
Define Stochastic effects in relation to radiation injury.
Defn: Stochastic effects are random biological injuries caused by radiation. The severity of stochastic effects is not dependent on the magnitude of the absorbed dose (there is no threshold). These effects are believed to result from ionizing radiation damaging chromosomes—potentially leading to conditions such as cancer.
Define Non-Stochastic effects in relation to radiation injury.
Defn: Non-stochastic effects are biological injuries caused by radiation that have a threshold dose. The severity of non-stochastic effects increases with the magnitude of the absorbed dose. These effects occur only when exposure exceeds a certain level and often result from extensive cell damage or death. (ex. erythema (redness), hair loss, cataracts, infertility)
What is Latent Period?
The time that elapses between exposure and observable clinical signs.
More radiation = faster the dose rate = shorter latent period
Basically a measure for how quickly clinical signs appear
Define Injury period
Injury period follows latent period in which cellular damage may be the result of the duration of exposure.
Define Recovery Period
Recovery period is the phase following the latent and injury periods of radiation exposure during which cells repair sublethal damage.
Damaged tissues may heal partially or fully (not all cellular radiation are permanent)
Depends on radiation dose, tissue type, and cell turnover rate
Some injuries may be permanent or cumulative if repair is incomplete
damage that remains unrepaired accumulates in the tissues which then can lead to cancer, cataracts, birth defects
What are the 5 factors that contribute to severity of Radiation Injury
Total dose → how much radiation received/being absorbed by cells
Dose Rate → the rate at which exposure to radiation occurs (cells take time to heal)
Area Exposed → larger area, more injury
Cell Sensitivity → some cell types are more sensitive
Age → younger individuals more susceptible; elderly have thinner body tissue and less capable of repair
What types of cells are Radiosensitive? are Radioresistant?
Radiosensitive → small lymphocyte, bone marrow, reproductive cells
Radioresistant → muscles, nerve, mature bone
What is the difference between short-term and long-term effects in relation to Radiation?
Short-term = large amounts of radiation over short period of time
Long-term = small amounts of radiation repeated over long period of time (dentistry risk)
What is Background Radiation?
Naturally occurring background radiation that emits from radioactive materials present in the earth and air. (i.e potassium, uranium)
What are the OLD units of measurement for Radiation? (3)
Roentgen (R) - exposure
Radiation Absorbed Dose (RAD)
Radiation Equivalent (in Man) = rem
What are the NEW units of measurement for Radiation? (3)
Coulombs/kg (C/kg)
Gray (Gy)
Sievert (Sv)
What does Roentgen (Coulomb) measure?
Measure the energy produced by gamma radiation in a cubic centimetre of air AKA measures radiation exposure
Abbrev. R or mR (milli)
What does Radiation Absorbed Dose - RAD (Gray) measure?
Amount of energy absorbed by tissue
amount of radiation energy transferred to some mass of material (i.e. humans)
1 R of gamma radiation exposure = 1 Rad of Absorbed dose.
What does Roentgen Equivalent Man - REM (Sievert) measure?
Unit that relates the dose of any radiation to the biological effects of that dose
Measures the biological effect of ionizing radiation on human tissue.
Used to assess radiation risk to health
Gamma rays/beta particles → 1 RAD of exposure = 1 REM of dose
What are the 4 critical organs at risk when performing Dental Radiography?
Thyroid Gland
Bone Marrow
Skin
Eyes
What are the 4 variables that contributes to the quantity of xray exposure to clients.
Film speed → faster films reduces absorbed dose by 60%
Collimation → Rectangular shape instead of round reduced absorbed dose by 60-70%
Technique → Long cone paralleling and longer TFD reduces skin dose
Exposure → Higher kVp reduces skin dose. (high kvp=more penetrating=less absorbed)