Lecture 10 - Cardiac Electrophysiology & EKG
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
Pathway of Blood
SVC + IVC → RA → Tricuspid valve → RV → Pulmonary valve → Pulmonary
trunk → R/L Pulmonary artery → Lungs → R/L Pulmonary veins →LA →
Mitral/Bicuspid valve → LV → Aorta → to the rest of the body
Two kinds of myocytes
Contractile cells: responsible for contraction
• Pacemaker cells: noncontractile cells that spontaneously depolarize
• Initiate depolarization of entire heart
• Do not need nervous system stimulation
Cardiac Muscle Contraction and Conducting System
Heart contracts as a unit
• All cardiomyocytes contract as unit, or none contract
• Contraction of all cardiac myocytes ensures effective pumping action
• Skeletal muscles contract independently
• Approximately 1% of cardiac cells do not function in contraction but have specialized features that are essential for normal heart excitation.
• These cells constitute a network known as the conducting system of the heart and are in electrical contact with the cardiac muscle cells via gap junctions.
• The conducting system initiates the heartbeat and helps spread an action potential rapidly throughout the heart
Mechanisms of Coordinated Hearbeat
Coordinated heartbeat is a function of:
• Presence of gap junctions
• Intrinsic cardiac conduction system
• Network of noncontractile (autorhythmic) cells
• Initiate and distribute impulses to coordinate depolarization and contraction of heart
Action potential initiation by pacemaker cells
Three parts of action potential
1. Pacemaker potential: K+ channels are closed, but slow Na+ channels are open, causing interior to become more positive
2. Depolarization: Ca2+ channels open (around −40 m V), allowing huge influx of Ca2+, leading to rising phase of action potential
3. Repolarization: K+ channels open, allowing efflux of K+, and cell becomes more negative
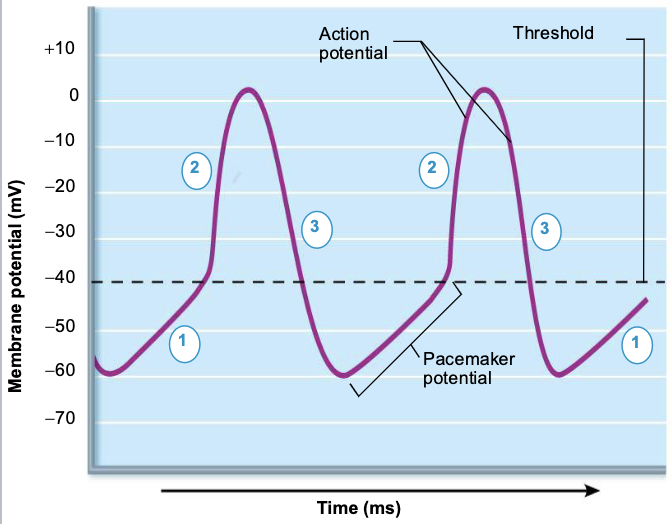
Pacemaker and Action Potentials of Pacemaker Cells
Pacemaker potential Slow depolarization is due to both opening of Na+ channels and closing of K+ channels. (*membrane potential not a flat line).
Depolarization The AP begins when the pacemaker potential reaches threshold. Depolarization is due to Ca2+ influx through Ca2+ channels.
Repolarization is due to Ca2+ channels inactivating and K+ channels opening. This allows K+ efflux, which brings the membrane potential back to its most negative voltage.
Sequence of excitation
Cardiac pacemaker cells pass impulses in ~0.22 seconds
1. Sinoatrial node →
2. Atrioventricular node →
3. Atrioventricular bundle →
4. Right and left bundle branches →
5. (Purkinje fibers)
Sequence of excitation (In depth)
Superior vena cava
Right atrium
1) The sinoatrial (SA) node (pacemaker) generates impulses.
Internodal pathway
2) The impulses pause (0.1 s) at the atrioventricular (AV) node.
3) The atrioventricular (AV) bundle connects the atria to the ventricles.
4) The bundle branches conduct the impulses through the interventricular septum.
5) Purkinje fibers depolarizes the contractile cells of both ventricles.
Left atrium
• Subendocardial conducting network
(Purkinje fibers)
Inter-ventricular septum
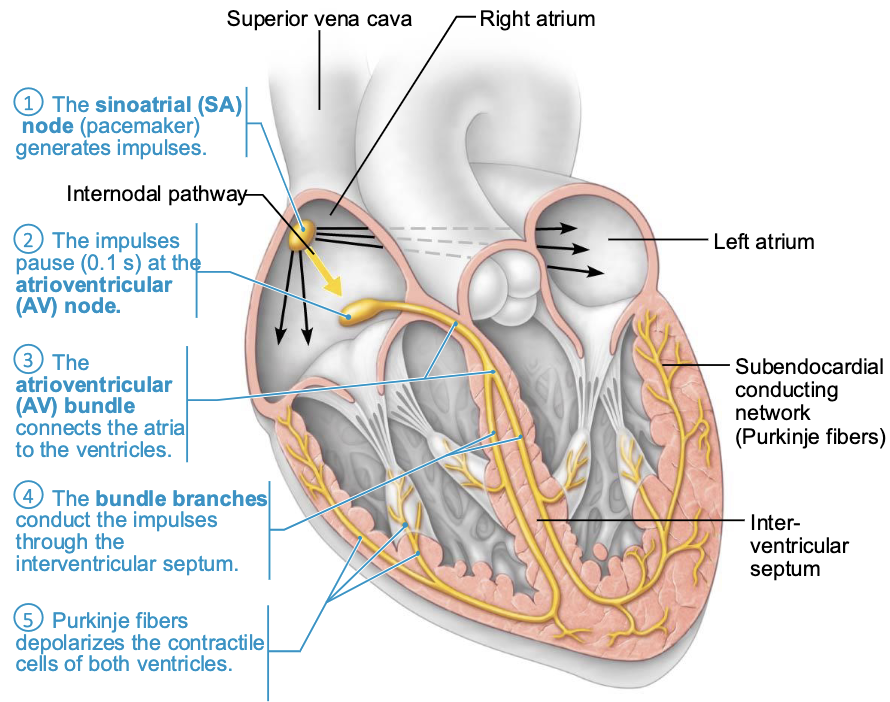
SA node (Pacemaker)
• Depolarizes faster than rest of myocardium
• Generates impulses about 75×/min. (sinus rhythm) → [100×/min. by extrinsic factors]
(AV) node
Delays impulses approx. 0.1 second (Allows atrial contraction prior to ventricular contraction)
(AV) bundle (bundle of His)
Only electrical connection between atria and ventricles
Right & left bundle branches
Carry impulses toward apex of heart
Purkinje fibers
Complete pathway through interventricular septum into apex and ventricular walls
• More elaborate on the left side of the heart
• AV bundle and Purkinje fibers depolarize 30×/minute in the absence of AV node input
• Process from initiation at SA node to complete contraction takes ~0.22 seconds
SA Node Dysfunction and Ectopic Pacemakers
Defective SA node may cause ectopic focus, an abnormal pacemaker that takes over pacing
• If AV node takes over, it sets junctional rhythm at 40–60 beats/min
• Extrasystole (premature contraction): ectopic focus of small region of heart that triggers impulse before SA node can, causing delay in next impulse
• Heart has longer time to fill, so next contraction is felt as thud as larger volume of blood is being pushed out
• Can be from excessive caffeine or nicotine
Heart Block and Pacemaker Intervention
If AV node is defective, may cause a heart block
• Few impulses (partial block) or no impulses (total block) reach ventricles
• Ventricles beat at their own intrinsic rate
• Too slow to maintain adequate circulation
• Treatment: artificial pacemaker (recouples atria and ventricles)
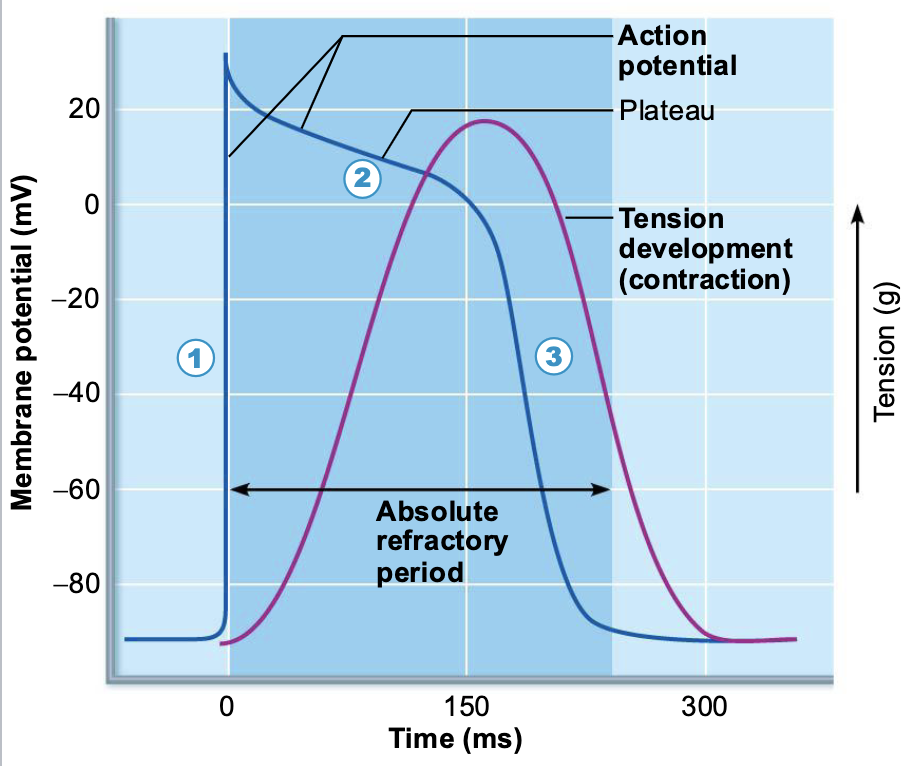
The Action Potential of Contractile Cardiac Muscle Cells
Depolarization is due to Na+ influx through fast voltage-gated Na+ channels. A positive feedback cycle rapidly opens many Na+ channels, reversing the membrane potential. Channel inactivation ends this phase.
Plateau phase is due to Ca2+ influx through slow Ca2+ channels. This keeps the cell depolarized because most K+ channels are closed.
Repolarization is due to Ca2+ channels inactivating and K+ channels opening. This allows K* efflux, which brings the membrane potential back to its resting voltage.
Difference between contractile muscle fiber and skeletal muscle fiber contractions
• AP in skeletal muscle lasts 1–2 ms; in cardiac muscle, it lasts 200 ms
• Contraction in skeletal muscle lasts 15–100 ms; in cardiac contraction, it lasts over 200 ms
• Benefit of longer AP and contraction:
• Sustained contraction ensures efficient ejection of blood
Action Potentials of Contractile Cardiac Muscle Cells
Contractile muscle fibers make up bulk of heart muscle; responsible for pumping action
• Steps involved in AP:
• Depolarization opens fast voltage-gated Na+ channels; Na+ enters cell
• Positive feedback influx of Na+ causes rising phase of A P (from −90 mV to +30 mV)
• Depolarization by Na+ also opens slow Ca2+ channels
• At +30 mV, Na+ channels close, but slow Ca2+ channels remain open, prolonging depolarization → a plateau
• After about 200 ms, slow Ca2+ channels are closed, and voltage-gated K+ channels are open
• Rapid efflux of K+ repolarizes cell to RMP
• Ca2+ is pumped both back into SR and out of cell into extracellular space
P wave, QRS complex, T wave, P-R interval, S-T segment, Q-T interval, Electrocardiograph, Electrocardiogram
P wave: atrial depolarization initiated by SA node
• QRS complex: ventricular depolarization and atrial repolarization
• T wave: ventricular repolarization
P-R interval: beginning of atrial excitation to beginning of ventricular excitation
• S-T segment: entire ventricular myocardium depolarized
• Q-T interval: beginning of ventricular depolarization through ventricular repolarization
• Electrocardiograph: detect electrical currents generated by heart
• Electrocardiogram (ECG/EKG) is a graphic recording of electrical activity
• Composite of all action potentials at given time;
Electrocardiogram: Sequence of Electrical Events in the Heart
Atrial depolanzation, Initiated b le SA node, causes the P wave
With atrial depolarization complete, he impulse is delayed at the AV node.
Ventricular depolarization begins at apex, causing the QRS complex. Atrial repolarization occurs.
Ventricular depolarization is complete.
Ventricular repolarization begins at apex, causing the T wave.
Ventricular repolarization is complete.
ECG Abnormalities and Diagnostic Indicators
Changes in patterns or timing of ECG may reveal diseased or damaged heart, or problems with heart’s conduction system
• Problems that can be detected:
• Enlarged R waves may indicate enlarged ventricles
• Elevated or depressed S-T segment indicates cardiac ischemia
• Prolonged Q-T interval reveals a repolarization abnormality that increases risk of ventricular arrhythmias
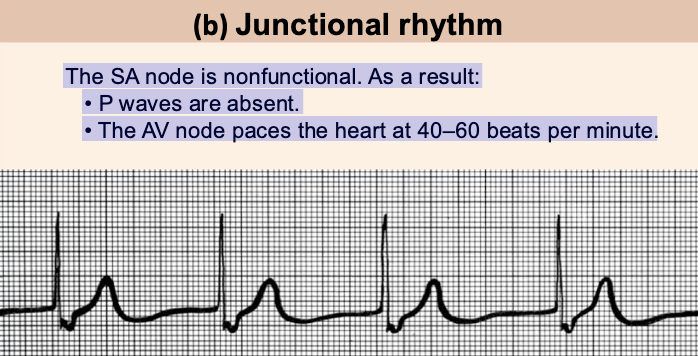
Junctional rhythm
The SA node is nonfunctional. As a result:
• P waves are absent.
• The AV node paces the heart at 40–60 beats per minute.
Ventricular fibrillation
Electrical activity is disorganized. Action potentials occur randomly throughout the ventricles.
• Results in chaotic, grossly abnormal ECG deflections.
• Seen in acute heart attack and after an electrical shock.