Vitreo-Retinal-Choroidal Disease Review (Anatomy & Testing)
1/127
Earn XP
Description and Tags
Dr. Yacoub (Disease III)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
128 Terms
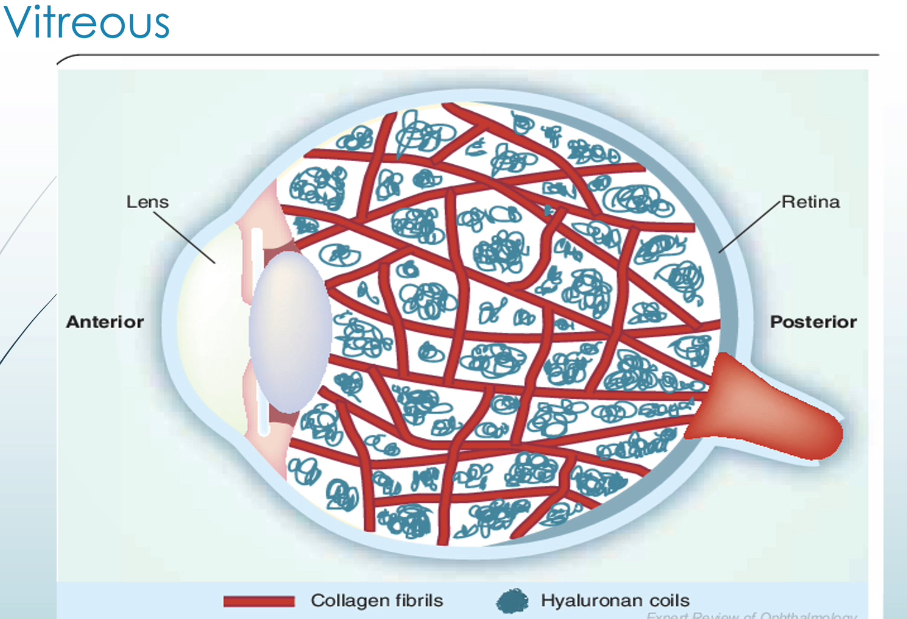
characteristics of vitreous
80% of the total volume of the eye
4g and 4ml in volume
composed of a matrix of type II collagen fibrils, hyaluronic acid, proteoglycans, glycoproteins, H2O
hyaluronic acid + collagen fibrils = gel-like consistency and transparency of vitreous
4 functions of vitreous
acts as shock absorber
maintains connection of neurosensory retina to RPE
stores and transfers nutrients to lens and retina
transmits and refracts light which helps focus light on retina
strongest vitreous attachment to weakest
strongest
vitreous base which is at ora serrata
optic nerve (vitreous inserts into glial peripapillary ring)
ILM in macula region
ILM over the retinal vasculature
ILM elsewhere
weakest
*posterior hyaloid face of vitreous attaches to the following from strongest to weakest
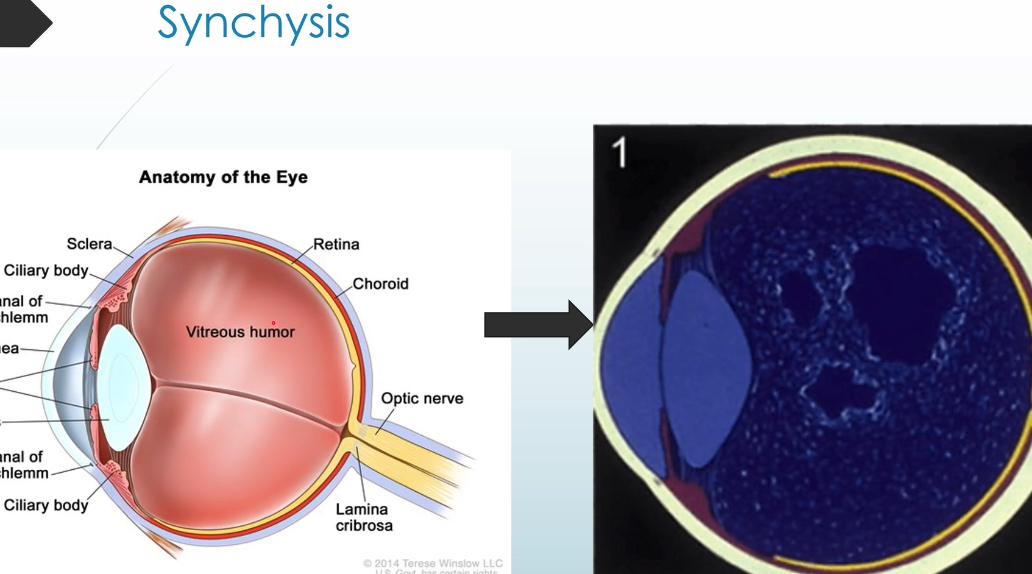
order of vitreous degeneration
synchysis → syneresis → PVD
define synchysis
liquefaction of the vitreous due to breakdown of hyaluronic acid
collagen fibrils disorganize and aggregate in clumps → floaters
water separates from collagen and forms pockets of water called lacunae
myopia, ocular inflammation, ocular trauma, retinal vascular disease, aphakia, and vitreous hemorrhage can accelerate snchysis
factors that accelerate synchysis of vitreous
myopia
ocular inflammation
ocular trauma
retinal vascular disease
aphakia
vitreous hemorrhage
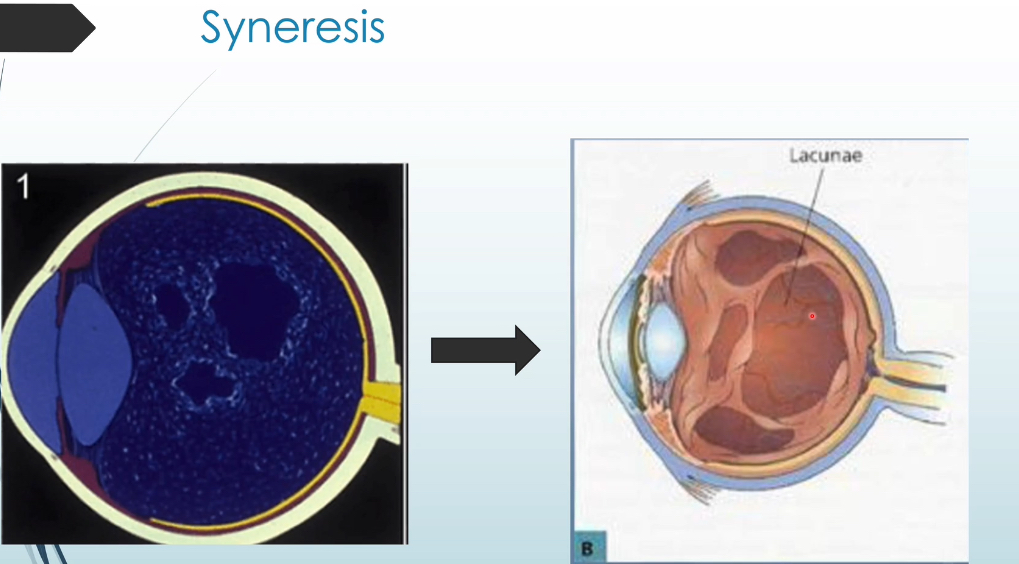
define syneresis
enlarging/coalescing lacunae → increase in weight of water centrally and anteriorly → disorganization of collagen fibrils → pulls/contracts vitreous → vitreous collapses and shrinks (syneresis)
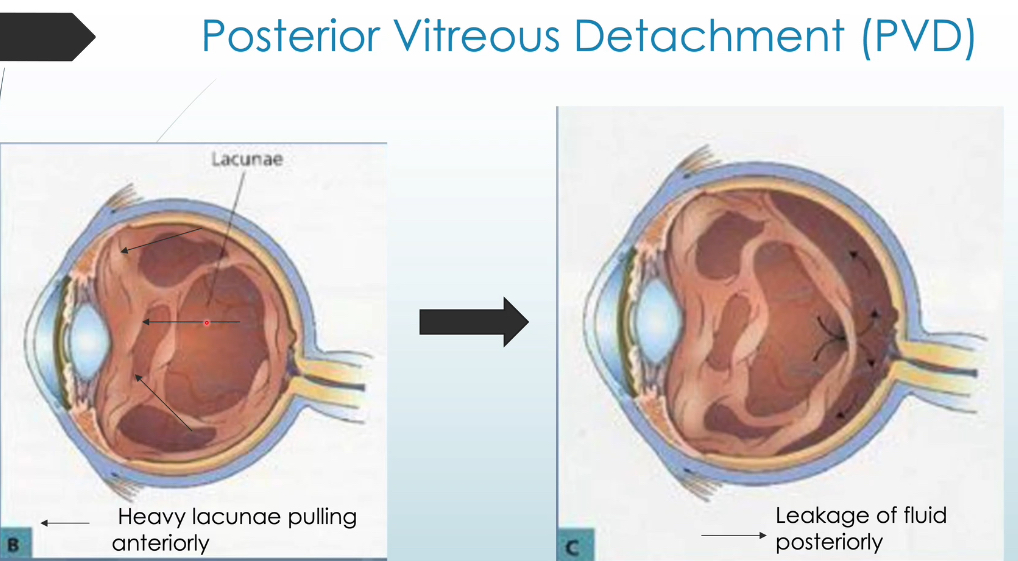
define posterior vitreous detachment (PVD)
contraction and shrinkage of vitreous → leakage of fluid thru breaks/thins in cortex → loss of attachment of retina and ON called PVD
about ___% of patients over age 65 develop a PVD
65%
stages of PVD
separation of posterior hyaloid face from perifovea with continued attachment to the fovea
complete separation of posterior hyaloid face from macula (including fovea)
extensive separation from retina with continued attachment to ON
complete PVD, no more adhesion to ON except vitreous base
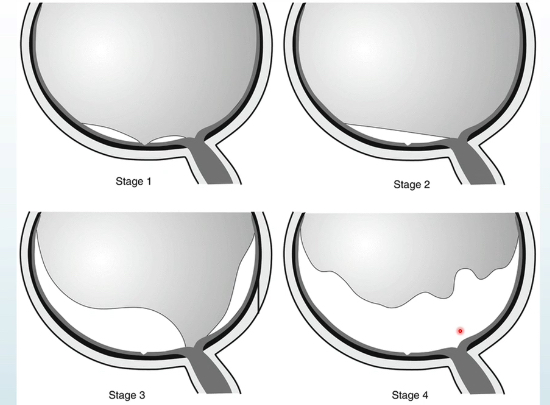
what will the posterior hyaloid face of vitreous still be attached to during stage 4 of PVD?
vitreous base
if you see a ___, you can assume the pt had a PVD
weiss ring
if the retina is transparent, what gives the retina its reddish color?
the color seen is due to the combo of the retinal pigment epithelium, choroid, and choroidal vasculature
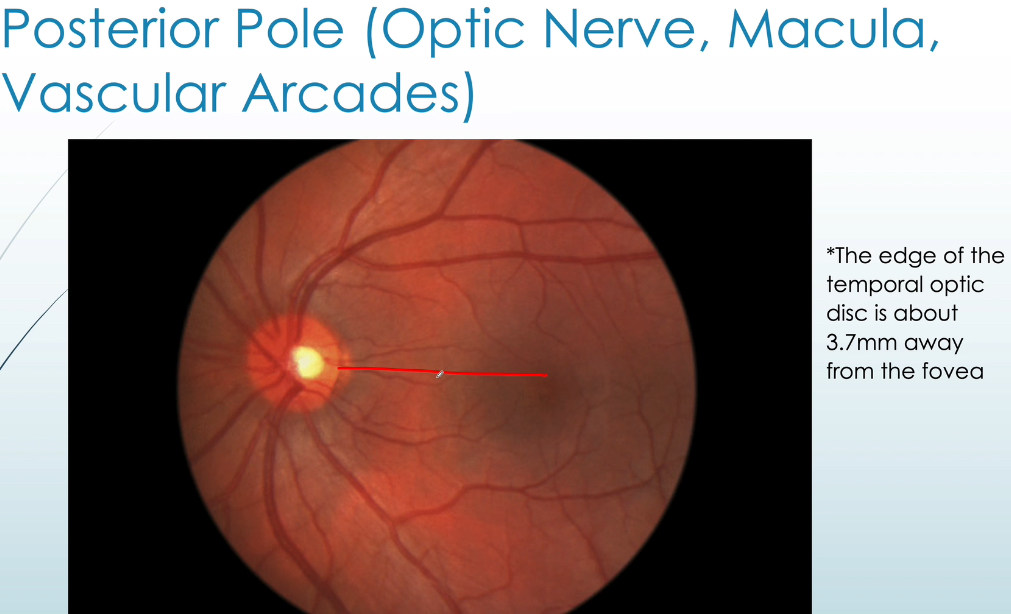
the retina is thickest in the ____ and thins out as the retina goes further out in periphery
macular region
the ora serrata is considered the ____ limit of the neural retina
anterior limit
the retina extends from optic dish in both directions up until the ora serrata
the edge of the temporal optic disc is about ___ away from the fovea
3.7 mm away from fovea
majority of rods are found in ____ and cones are found in ____
rods → peripheral retina
cones → posterior pole
the short ciliary nerves arises from the ____ and long ciliary nerves arises from the ____
short ciliary nerves → ciliary ganglion
long ciliary nerves → nasocilliary branch of CN V1
the SCN transmits _____ and LCN transmits ____
SCN → sensory (nasocilliary br of CN V1), sympathetic, and parasympathetic (CN III and VII)
LCN → sensory (nasocilliary br of CN V1), sympathetic info to → conj, cornea, CB, dilator muscle in iris
layers of retina from inner to outer
inner (vitreous)
ILM
RNFL
GCL
IPL
INL
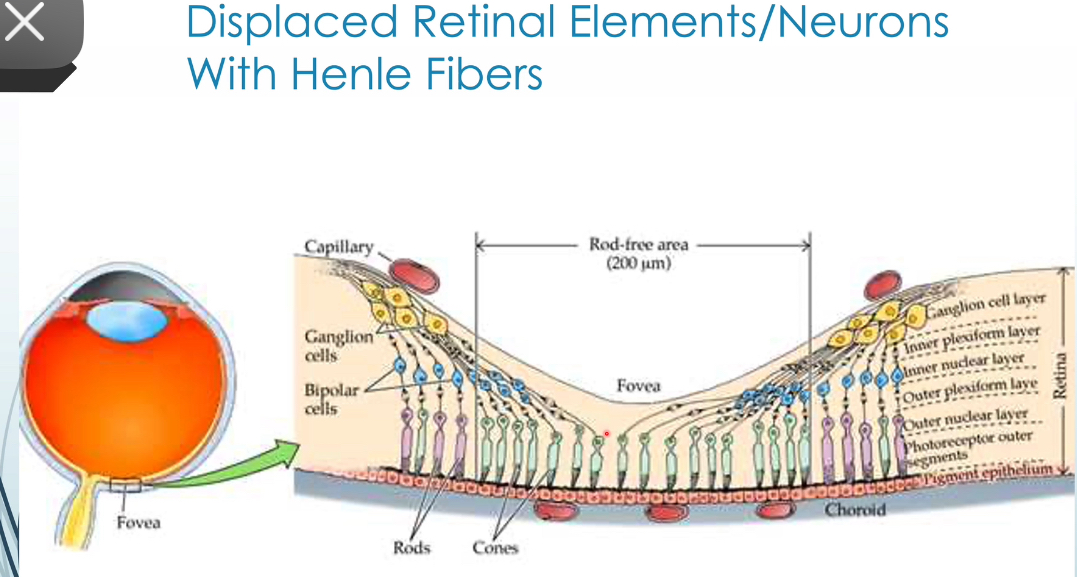
OPL (aka Henle fiber layer)
ONL
ELM
photoreceptor layer
myoid zone, ellipsoid zone, outer segments of PR
interdigitation zone (IDZ) between PR and RPE
RPE
bruch membrane
outer (choroid)
T/F: Bruch’s membrane has strong adhesion to RPE and RPE has weak adhesion to photoreceptor layer
true
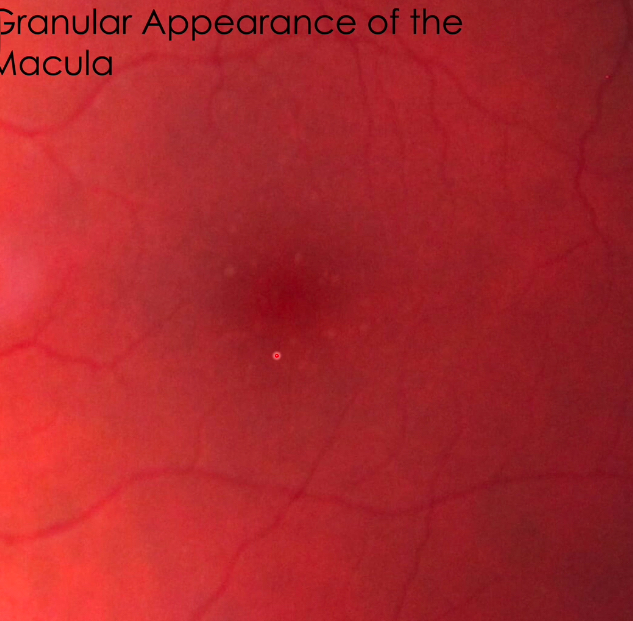
why does the macula normally have a granular appearance?
within individual RPE cells, there’s unequal distribution of pigment → macula looks granular
most apparent at macula since RPE cells are most dense at the macula
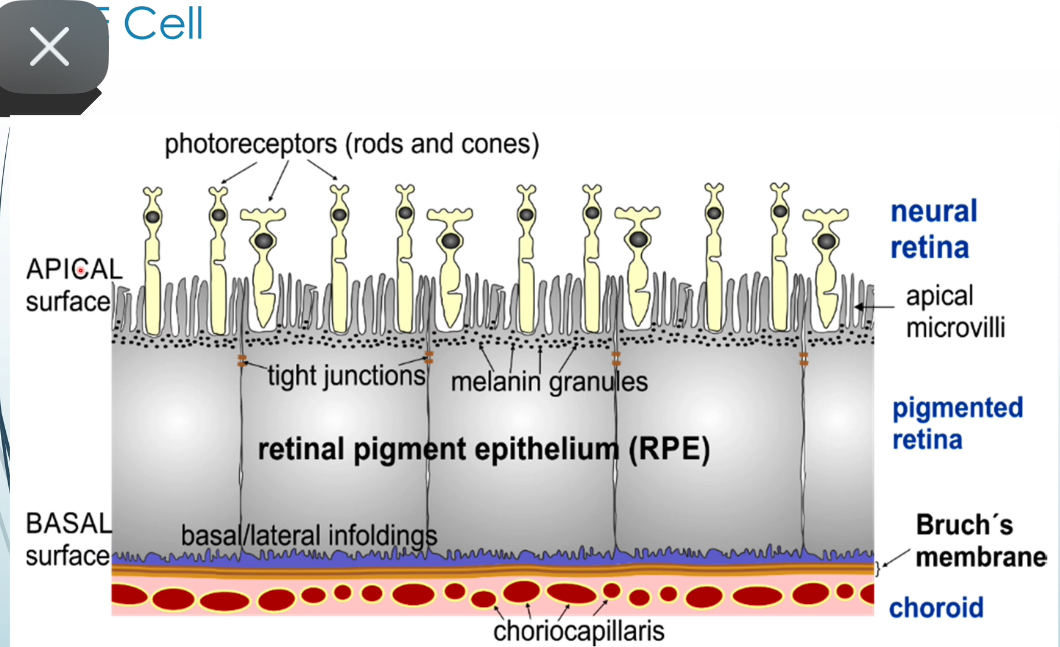
RPE cells are interlocked tightly by ___ and ____ which forms the outer blood-retina layer
zonula occludens (tight jxn) and zonula adherens (anchoring jxn)
what allows for the electrical coupling and low-resistance channel for flow of ions, metabolites, and nutrients from the choroid into the retina?
desmosomes and gap junctions are present throughout the RPE
the ____ surface of RPE cell is closest to Bruch’s membrane
basal surface
what are the reasons for RPE and photoreceptor attachment if there’s subretinal space there?
IOP
osmotic pressure
vitreous
apical microvilli of RPE
interphotoreceptor matrix (IPM) - GAGS and proteins make matrix ‘sticky’
keeps photoreceptor up against RPE
the potential space between RPE and PR is absent along the ___ and ____ which means that the retina is strongly attached in these areas
absent along the peripapillary ring around optic disc and ora serrata
functions of RPE
absorb scattered light (improve optical quality, decrease photo-oxidative stress)
control of fluid, nutrients, waste products
visual pigment (rhodopsin)
key for visual cycle
synthesis of signaling molecules (VEGF, TGF, PEDG, PDGF)
phagocytosis of photoreceptor waste
involved in regeneration and repair
stores vit A
synthesizes IPM
acts as the outer-blood retina barrier esp due to tight junctions found in the RPE
what is the interdigitation zone (IDZ)?
area where apices of RPE cells encase part of the cone outer segments as well as the rod outer segments
visible in post pole
part of subretinal space
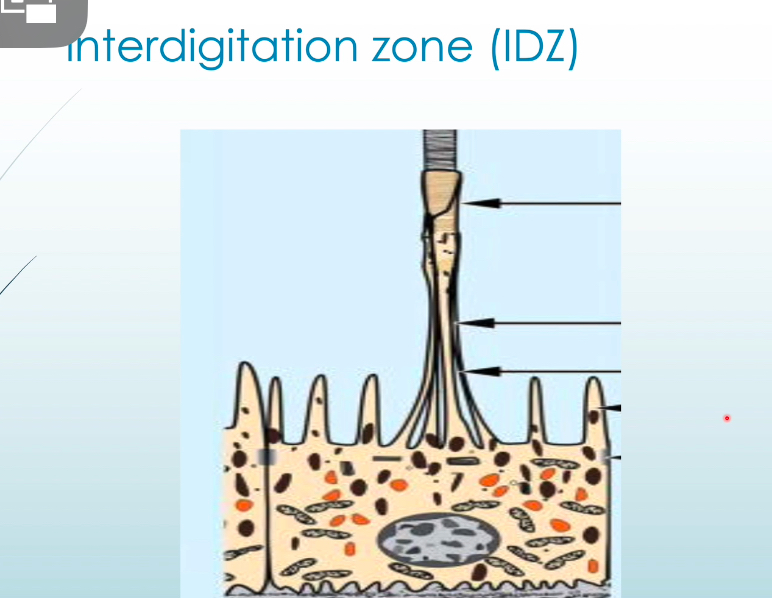
define verhoeff membrane?
anatomical structure that surrounds the apical portion of the RPE composed of the tight junctions between RPE cells
found in the interdigitation zone (IDZ)
there are about ____ total rods in retina and ____ total cones
120 million rods
6 million cones
T/F: no rods are found at the foveola, only cones
true
rod density is greatest concentrically ____ from the foveola
4.5 mm or 15 degrees from foveola
T/F: some photoreceptors are found at optic nerve
false - NO pr at optic nerve (blind spot)
characteristics of rods
40-60 microns
1 type of rod
rods tend to be longer and thinner than cones
rod outer segments are longer
rod spherules connect with bp cells, horizontal cells, and other rod spherules and cone pedicles
more active in dim (scotopic)
senses contrast, brightness, motion
characteristics of cones
40-50 microns long
cone outer segments shorter and may not reach RPE
microvilli from apical RPE reach and surround cone outer segments
exception: at the macula, cone outer segments have similar shape to rods
bright conditions (photopic)
cone pedicles connect with bp cells, horizontal cells, other rod spherules, cone pedicles
senses fine resolution, spatial resolution, color
which layer of retina acts as a metabolic barrier and prevents passage of large molecules and stabilizes the transducing portion of photoreceptors?
external limiting membrane (ELM)
ONL is thickest at ____ and thinnest at ____
thickest at foveola and fovea (50 microns thick)
thinnest just temporal to the optic nerve (22 microns)
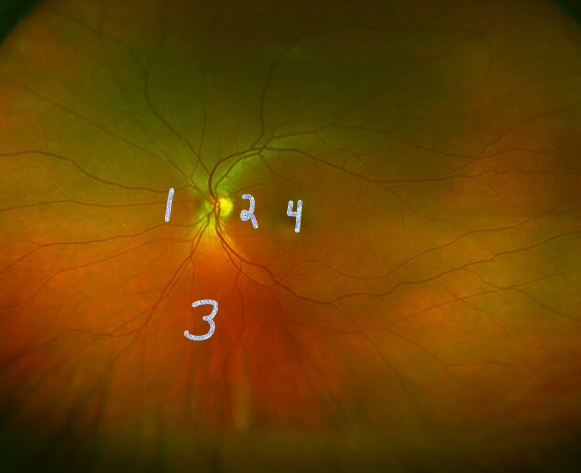
rank the thickness of ONL in the retina photo from thickest to thinnest
thickest 4, 1, 3, 2 thinnest
the synaptic junction between the photoreceptors and 2nd order neurons which include the bp cells and horizontal cells is called ____
outer plexiform layer (OPL)
in the fovea and esp at the foveola, there are no ____ because cone pedicles are displaced laterally (called the Henle layer)
no synaptic terminals bc cone pedicles are displaced laterally
the middle limiting membrane is composed of
desmosome-like attachments called synaptic densities that are found within the branching, interwoven bp dendrites and horizontal cells
in what layers can part of a photoreceptor be found in?
IDZ to OPL
what cells are found in the inner nuclear layer (INL)?
contains cell bodies of horizontal cells, bp cells, amacrine cells, interplexiform neurons, muller cells, displaced ganglion cells
what synapses occur in the inner plexiform layer (IPL)?
connections between axons of bp cells and dendrites of ganglion cells
synapses with amacrine cells
synapses between 2nd order and 3rd order neurons of the visual pathway
this layer disappears at the foveola
function of plexiform layers
prevent spread of fluid to other layers
IPL is stronger > than OPL
each ganglion cell is separated by
glial process of each muller cell
convergence of rods vs. cones
rods (75,000) → bp cells (500) → amacrine cells (250) → ganglion cells (1)
first, second, third, and fourth order neurons
cones (1-5) → bp cells (1-5) → ganglion cells (1)
first, second, third order neurons
function and types of neuroglial cells
provides structure, support, plays a role in neural tissue reaction to injury and infection
doesn’t participate in synaptic interactions and electrical signaling
muller cells, migroglial, astrocytes
muller cells project thick and thin processes in both directions to the ___ and ____
ILM and ELM (with microvilli extending into the sub-retinal space)
why macular edema greater at the foveal region of macula?
bc muller cells at macula are weak, few, and diagonally oriented
functions of muller cells
structural support to neuronal cell bodies
prevents mechanical deformation of retina
control homeostasis by regulating [K+] in retina
maintain extracellular pH by getting rid of metabolic waste as CO2 and ammonia
recycles glutamate, glycine, GABA
metabolizes, synthesizes, stores glycogen (fuels aerobic metabolism in neurons)
helps maintain inner blood-retina barrier
helps guide light directly to photoreceptors
which neuroglial cell increases in response to tissue inflammation and injury and phagocytize degenerating retinal neurons?
microglial cells
which neuroglial cells are almost entirely restricted to NFL and some of GCL?
astrocytes
functions of astrocytes
insulation and support to superficial retinal capillaries and nerve fibers
maintain inner blood-retina barrier
controls homeostasis by regulating concentration of [K+] in retina
metabolizes, synthesizes, stores glycogen
contributes to ILM
macula is ___ mm in diameter
fovea is ___ mm
foveola is ___ mm
macula = 5.5 mm
fovea = 1.5 mm (1 DD)
foveola = 0.35 mm
why does fovea have a dark appearance w a yellow hue?
high conc. of lutein and zeaxanthin (both xanthophylls) is found at fovea
xanthophylls tend to have a more yellow color
RPE cells are tallest, most dense/pigmented at fovea
choroidal capillary bed is thickest at fovea
macular pigment is located in OPL, muller cells, photoreceptor inner fibers, and rod outer segments
there is more lutein than zeaxanthin in the retina ____ while there’s more zeaxanthin than lutein at the ____
more lutein outside fovea
more zeaxanthin at the fovea
what layers of the retina are found at the foveola?
RPE/bruch complex
IDZ
outer segments of photoreceptors
ellipsoid zone
myoid zone
ELM
ONL
henle fiber layer
ILM
why is there a bump along the ellipsoid zone directly under the umbo?
RPE and IDZ are thicker, longer, and densely packed → pushing up the outer segments of photoreceptors → pushes up ellipsoid zone
cones are also more densely packed and rod-like in shape
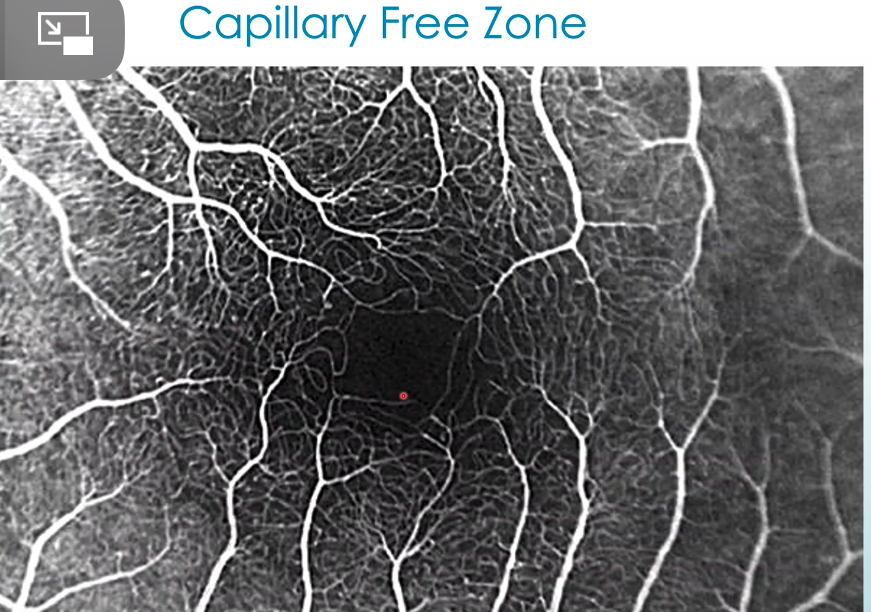
define capillary free zone
includes umbo, foveola, part of the fovea
lack of retinal blood vessels, which allows light to get to the photoreceptors without obstruction
choriocapillaris is found in retinal capillary free zone
at the ____, the orientation of retinal elements revert back to vertical orientation and henle fiber layer changes into OPL
perifovea
in the peripheral retina, RPE is continuous with ___ and ILM is continuous with ____
RPE continuous with outer pigmented epithelium of CB
ILM continuous with ILM of CB
T/F: choroidal thickness increases with age
false - it decreases with age
functions of choroid
vascular supply of outer retina
thermoregulation (maintain temp of the eye)
limits uncontrolled reflection of light
involved in VEGF production
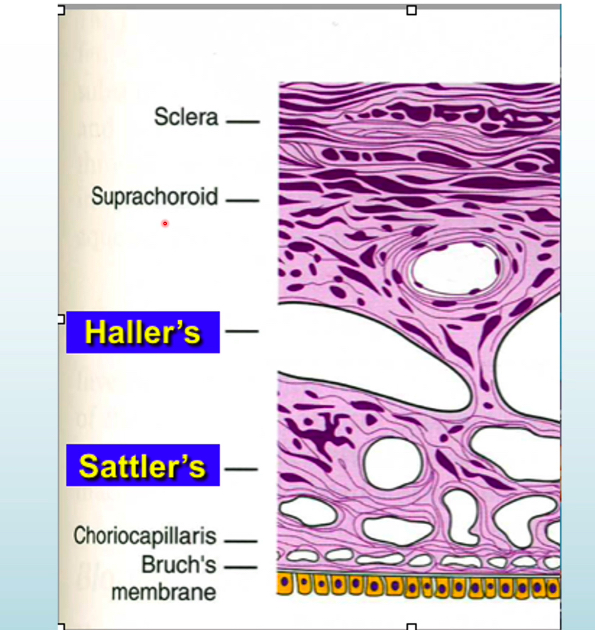
5 layers of the choroid
RPE
Bruch membrane (basal lamina)
choriocapillaris (stroma)
haller layer (stroma)
sattler layer (stroma)
suprachoroid (space in bw sclera and choroid)
sclera
in the inner retina, central retinal artery provides vascular supply to the inner retina via ____
in outer retina, choroidal capillary bed provides vascular supply to outer retina via ____
inner retina = perfusion
outer retina = diffusion
note: OPL has dual blood supply
4 types of retinal capillary plexues
superficial vascular complex (SVC)
radial peripapillary capillary plexus (RPCP) - NFL
superficial capillary plexus (SCP) - GCL, IPL
deep vascular complex (DVC)
intermediate/middle capillary plexus (ICP) - IPL, INL
deep capillary plexus (DCP) - INL, OPL
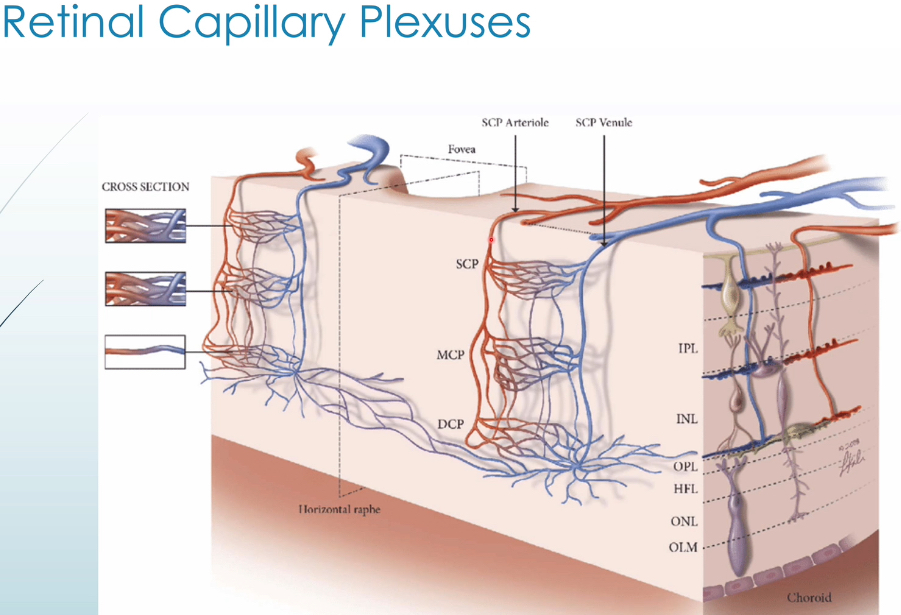
which plexuses are present in the peripapillary area? macula? central retina? periphery?
peripapillary → RPCP, SCP, ICP, DCP
macula → SCP, ICP, DCP
central retina → SCP, ICP, DCP
periphery → SCP, DCP
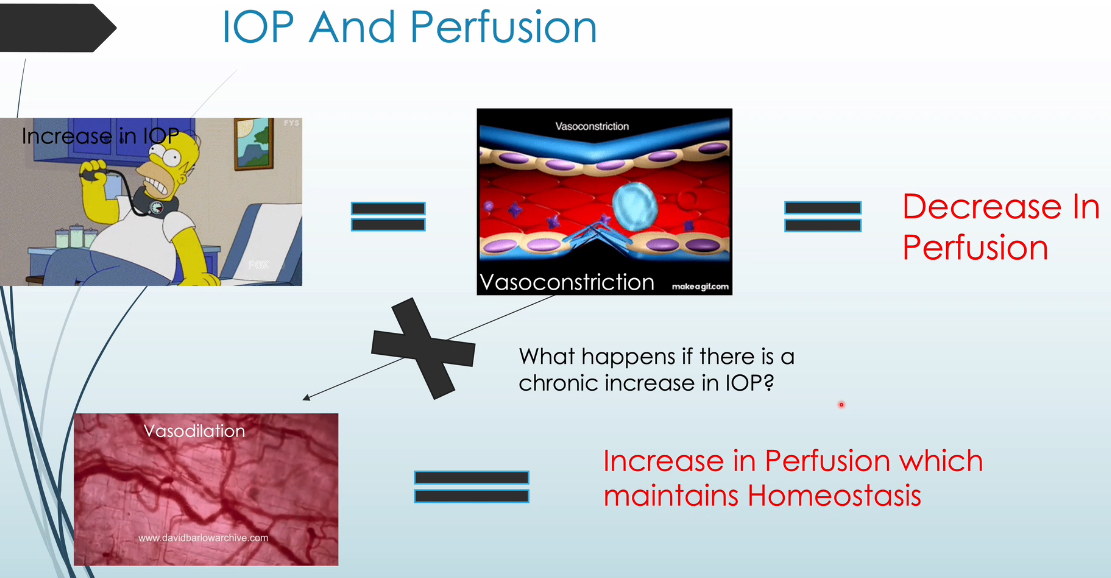
if IOP increases, what happens to the inner retina blood flow?
IOP increases → perfusion decreases due to constriction of arteries and arterioles → which dilate to keep homeostasis and maintain perfusion
in glaucoma, the arteries/arterioles can only autoregulate so much, ultimately arteries/arterioles will constrict → decrease in perfusion
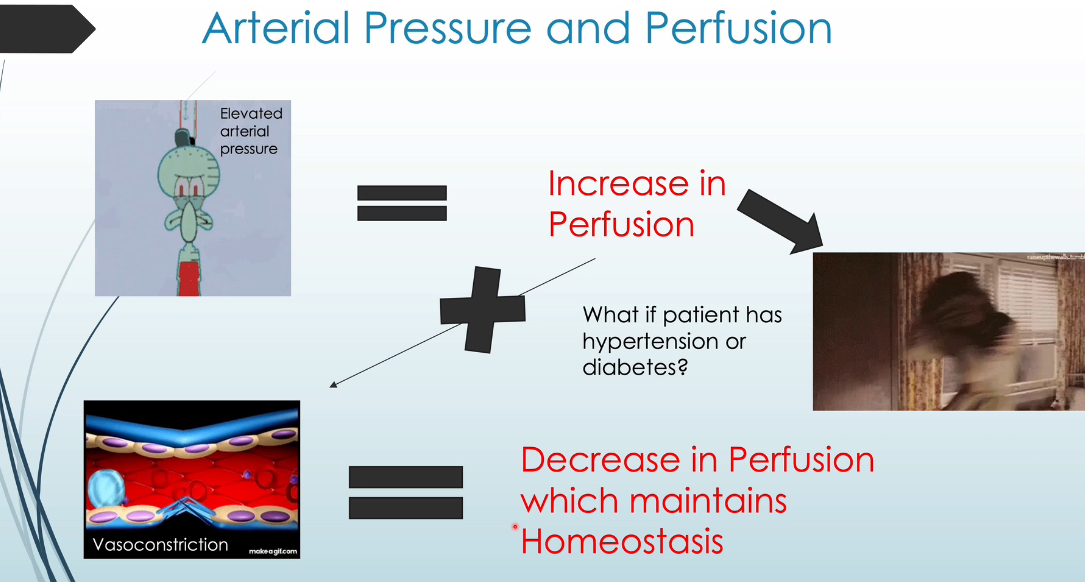
what happens to inner retinal blood flow if arterial pressure increases?
increase in arterial pressure → increase in perfusion → arteries/arterioles constrict to decrease perfusion and maintain homeostasis
retinal capillaries are dependent on autoregulation and perfusion that occurs in retinal arteries/arterioles
in HTN, arteries/arterioles can no longer autoregulate → retinal capillary damage
____ supplies the posterior choroid
____ supplies the anterior choroid
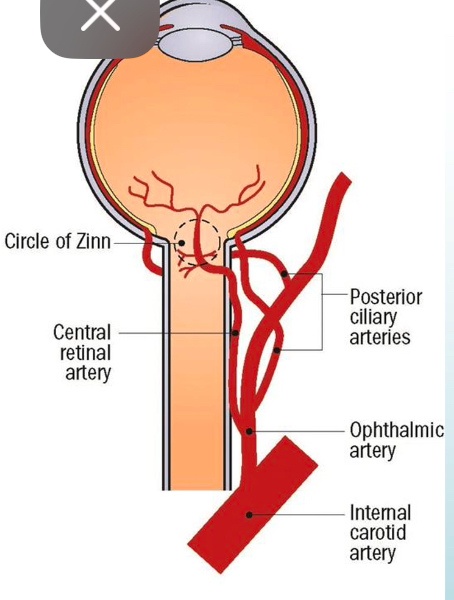
ophthalmic artery → short posterior ciliary arteries → posterior choroid → outer retina
ophthalmic artery → long posterior ciliary arteries → anterior choroid → CB and iris
haller vs. sattler layer vs. choriocapillaris
haller layer (outer choroid) = made up of large (“arteries”) non-fenestrated vessels
sattler layer (inner choroid) = made up of smaller (“arterioles”) non-fenestrated vessels
choriocapillaris (innermost choroid) = smaller (“capillaries”) fenestrated vessels directly up against Bruch membrane
since choroidal vessels aren’t able to autoregulate like retinal vasculature, it’s more dependent on ____
perfusion pressure
if you see a lesion on 78D lens, multiply by ____ to get the actl lesion size in mm. 90D? 60D?
78D → 1.2x
90D → 1.33x
60D → 1x
whatever you see on SL, that’s the measurement. no conversion
benefits of scleral depression
useful in detection, evaluation, differentiation of peripheral retinal anomalies, degenerations, holes, tears, detachments
ID retinal breaks/tears
enhances contrast between intact retina and retinal break
better visualize sub-retinal fluid as it moves around w scleral depression
indications for scleral depression
symptoms of flashes/floaters
hx of trauma
high myopia
aphakia
evidence of retinal break
vitreous hemorrhage
preretinal hemorrhage
pigment floating in vitreous (Shafer sign)
suspected pars planitis
RD
on optos, the red free filter is for looking at the ____ and the green free filter is used for looking at the ____
red free → retina
green free → choroid
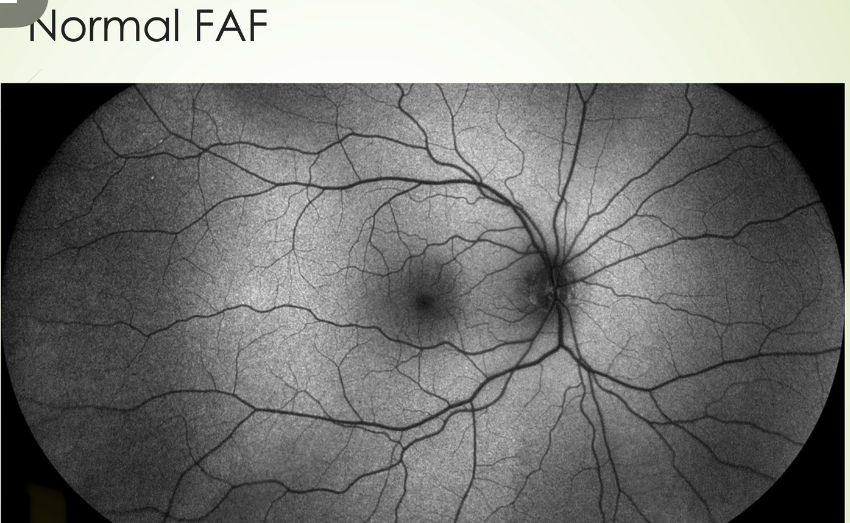
why does the retina normally have a slight glow on FAF?
25% of RPE cell is composed of lipofuscin
lipofuscin: when photoreceptors shed their outer sesgments, RPE ingests it thru phagocytosis which are then stored in liposomes → lipofuscin
loss of RPE cells = decrease in autofluorescence
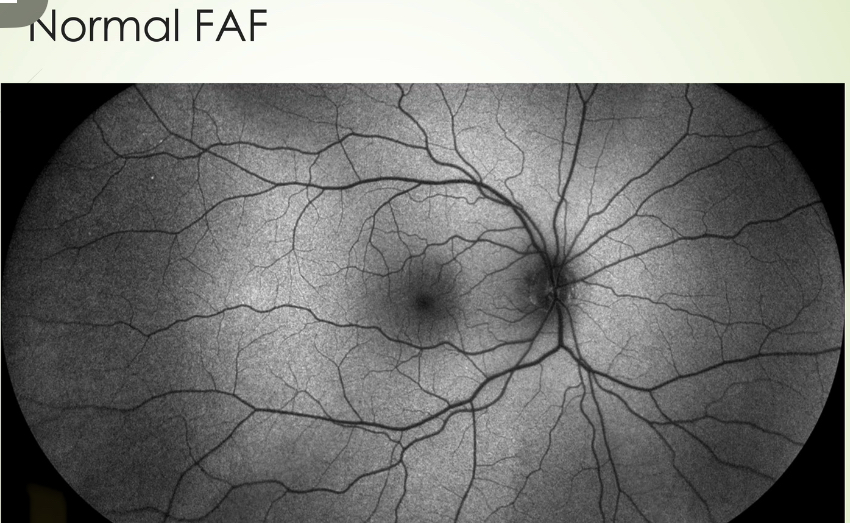
why does the ON and blood vessels show up as dark on FAF normally?
the ON and blood vessels don’t have RPE and thus, no lipofuscin
why does the fovea show up as dark normally?
due to the high concentration of light-absorbing xanthophyll pigment (blocks any underlying lipofuscin)
define iso-autofluorescence
normally expected autofluorescence (AF)
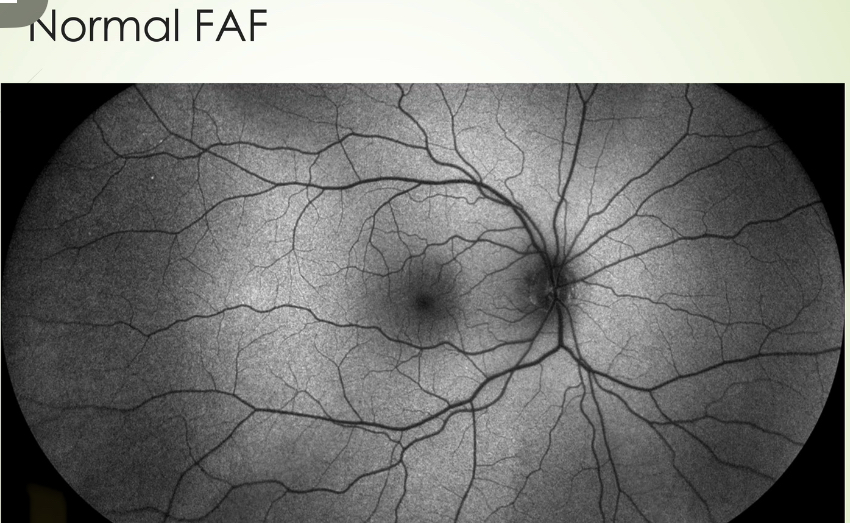
increase in autofluorescence (AF) shows up as ____ than normal
decrease in AF shows up as ____ than normal on FAF
increase in AF = brighter than normal
decrease in AF = darker than normal
purpose of fluorescein angiography (FA)
highlights ON, retina, choroidal circulation (although indocyanine green chorioangiography or ICG images choroidal circulation better)
useful in detection of subclinical retinal/choroidal/ON changes secondary to vascular conditions
aids in treatment decisions
guides retinal laser therapy
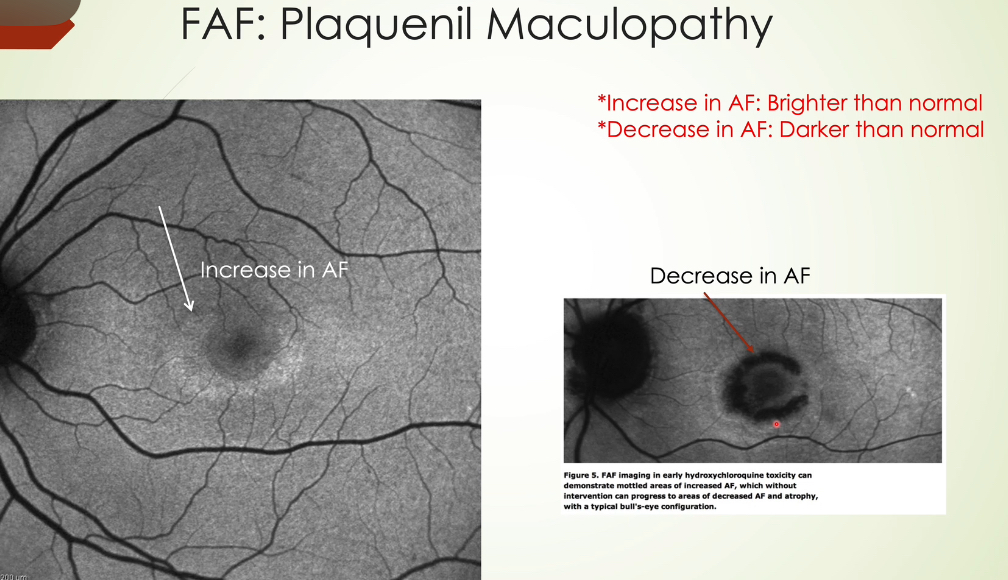
how does fluorescein travel/flow after injection in FA?
internal carotid artery → ophthalmic artery → central retinal artery → retina
internal carotid artery → ophthalmic artery → short posterior ciliary arteries → choroid + cilioretinal artery → artery
phases of a fluorescein angiography (FA)
choroidal flush → arterial phase → arteriovenous or laminar venous phase → complete venous phase → late phase
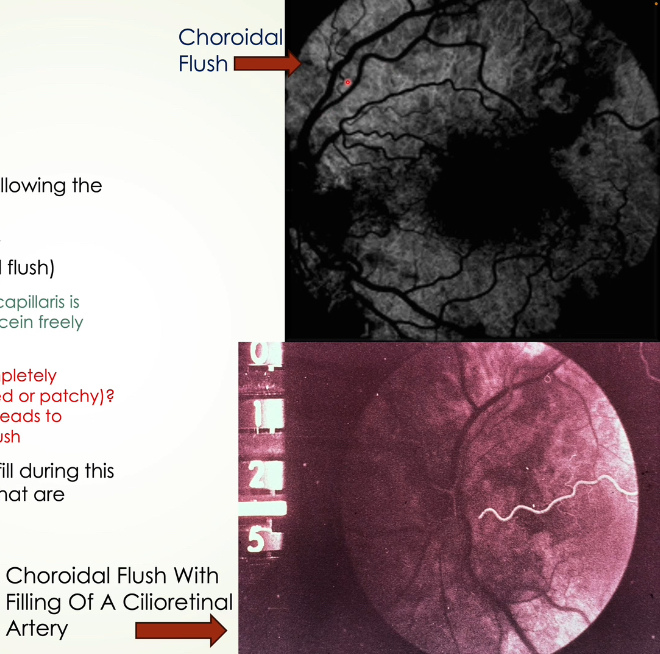
describe the choroidal flush phase of FA (1)
occurs 10 sec after injection
filling of the choroid is patchy hyperfluorescent (choroidal flush)
bc choriocapillaris is fenestrated and fluorescein freely leaks out
patchy due to various pigment levels in RPE so variable blockage of choroidal flush
cilioretinal artery + areas of retina perfused by cilioretinal artery will fill in this stage
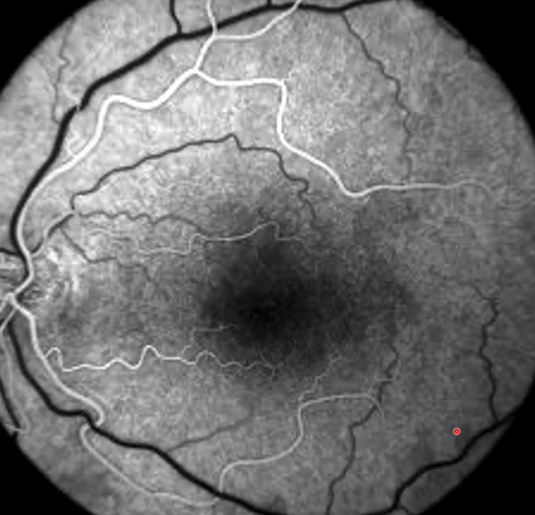
describe arterial phase of FA (2)
occurs 1-3 seconds following choroidal flush stage
arteries/arterioles fill with fluorescein
veins remain dark
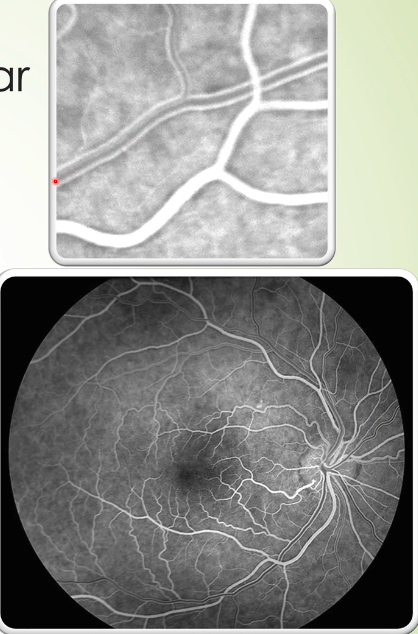
describe the arteriovenous or laminar venous phase of FA (3)
occurs 1-2 seconds following arterial phase
fluorescein spreads to capillaries and to postcapillary venules/veins
only the walls of venules/veins fluoesce while lumen remains dark
due to high density of erythrocytes in central lumen of venules/veins that prevent dye from filling centrally at first
describe the complete venous phase of FA (4)
occurs 1-2 seconds following arterial after arteriovenous or laminar venous phase
best stage to see perifoveal capillary network and foveal avascular zone
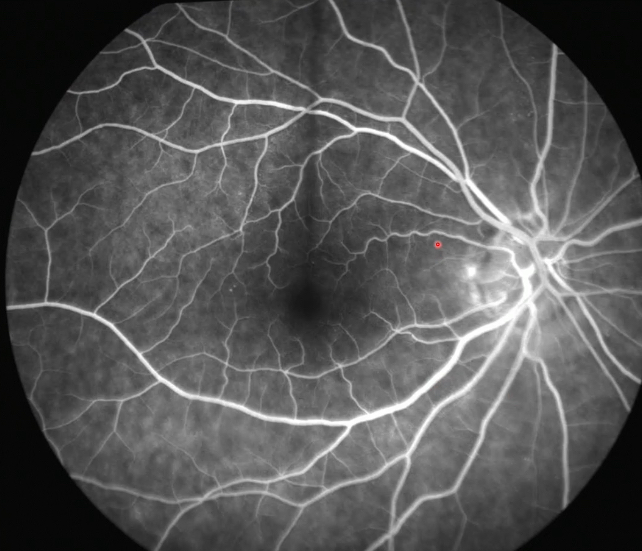
maximum vasculature fluorescence typically occurs at ___ after injection (best contrast between areas of hyperfluorescence and hypofluorescence)
25-30 seconds
after 30-45 sec, dye begins the recirculate and brightness starts to diminish as it makes a first pass thru kidneys
at 30 min, fluorescein is usually gone
describe late phase of FA (5)
5 min mark after injection and lasts until 20 min after injection
normal arterioles/arteries and venules/veins will almost be empty of fluorescein
any retinal leakage becomes more apparent
margins of ON remain hyperfluorescent (due to staining) as dye adheres to peripapillary choroidal plexus which supplies the prelaminar area of ON
staining of sclera or Bruch membrane may be seen
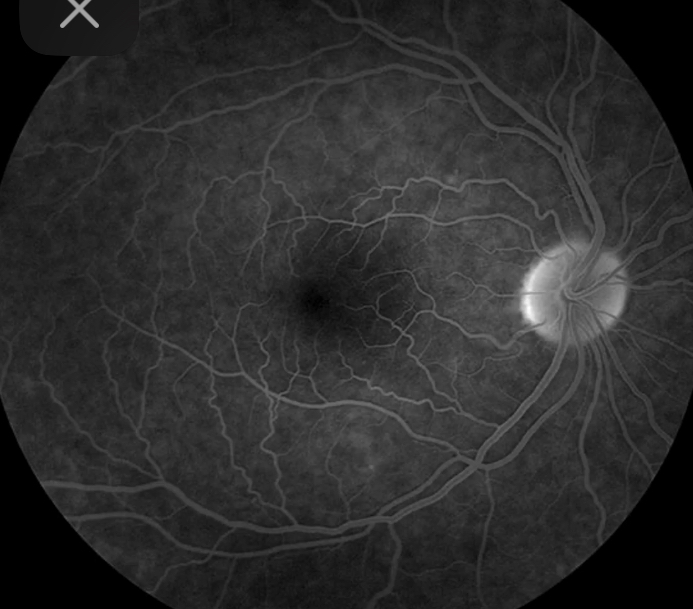
why is the macula (esp at fovea and foveola) normally darker on FA?
RPE cells are larger with more melanin in foveal region
high conc. of xanthophyll pigment in foveal region
xanthophyll pigment absorbs excitatory light from the camera
no retinal vasculature and retinal capillaries in this area (FAZ)
reasons for hypofluorescence?
hypofluorescence: reduction or absence of normal fluorescence (darkness)
blockage: obscuration of normal brightness due to overlying material
ex: intraretinal hemorrhages, preretinal hemorrhages, exudates, CWS, choroidal nevus, CHRPE without lacunae
filling defect: occurs due to reduced perfusion
ex: CRAO, retinal capillary dropout, choroidal non-perfusion, optic atrophy
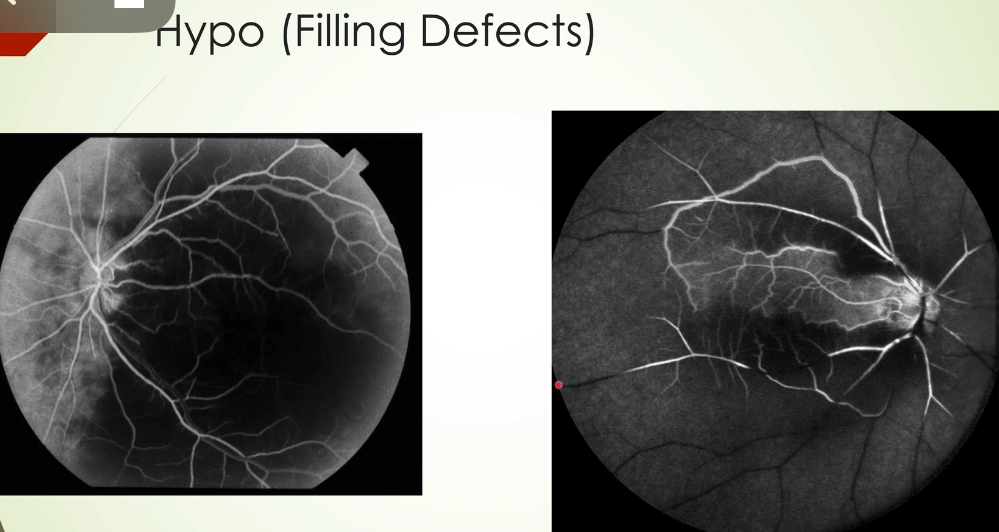
blockage vs. filling defect
both cause hypofluorescence
blockage: obscuration of normal brightness due to overlying material
ex: intraretinal hemorrhages, preretinal hemorrhages, exudates, CWS, choroidal nevus, CHRPE without lacunae
filling defect: occurs due to reduced perfusion
ex: CRAO, retinal capillary dropout, choroidal non-perfusion, optic atrophy
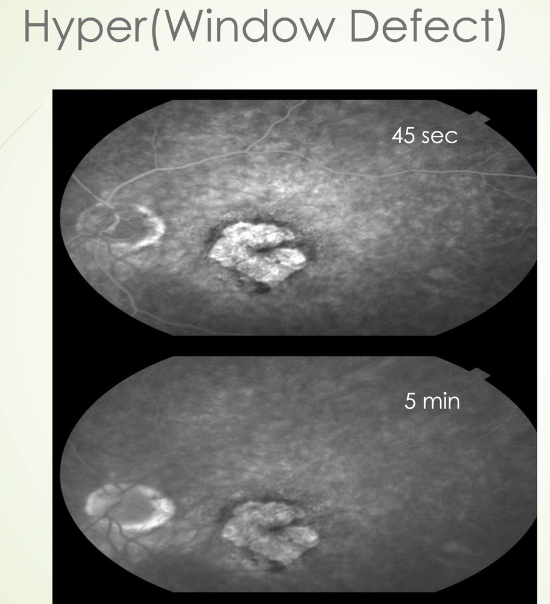
reasons for hyperfluorescence
hyperfluorescence: increase in normal fluorescence (bright)
window defect: defect in RPE
leakage: occurs in extracellular space
staining: fluorescein binds to tissue/accumulates within
pooling: leakage that occurs in confined or potential space
define window defect (hyperfluorescence) in FA
defect in RPE allows transillumination of choroidal flush
initially bright before arteries fill (most noticeable in choroidal flush stage)
stays the same size and brightness until late stage where it starts to lose its brightness
margins always distinct
ex: RPE window defects, geographic atrophy, CHRPE with lacunae
describe leakage (hyperfluorescence) in FA
leakage occurring in extracellular space
hyperfluorescence that appears early and progressively enlarges and gets brighter with less distinct margins as time goes on
see leakage well at 5 min mark
ex: mac edema, retinal neo, choroidal neovascular membrane
subfoveal, juxtafoveal, extrafoveal leakage
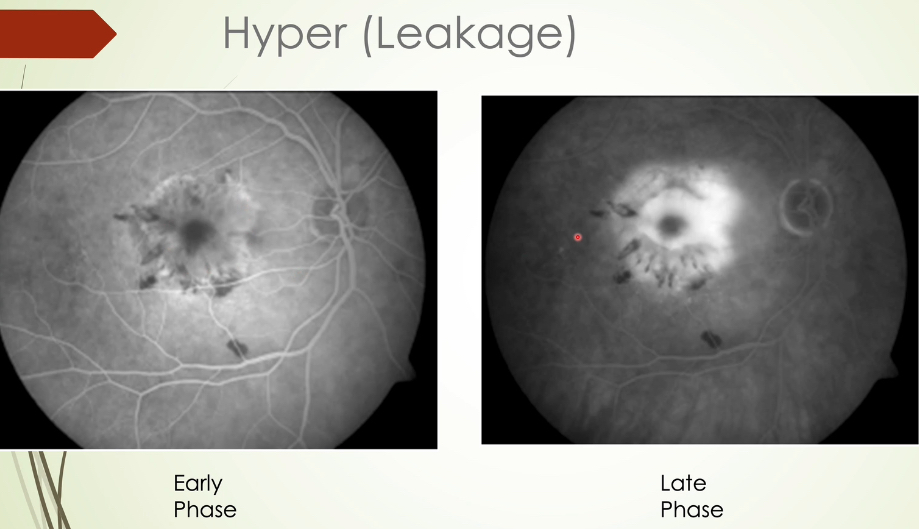
subfoveal vs. juxtafoveal vs. extrafoveal leakage in FA
subfoveal: under the fovea
juxtafoveal: leaking <200 microns from foveal center
extrafoveal: leaking ≥200 microns from foveal center
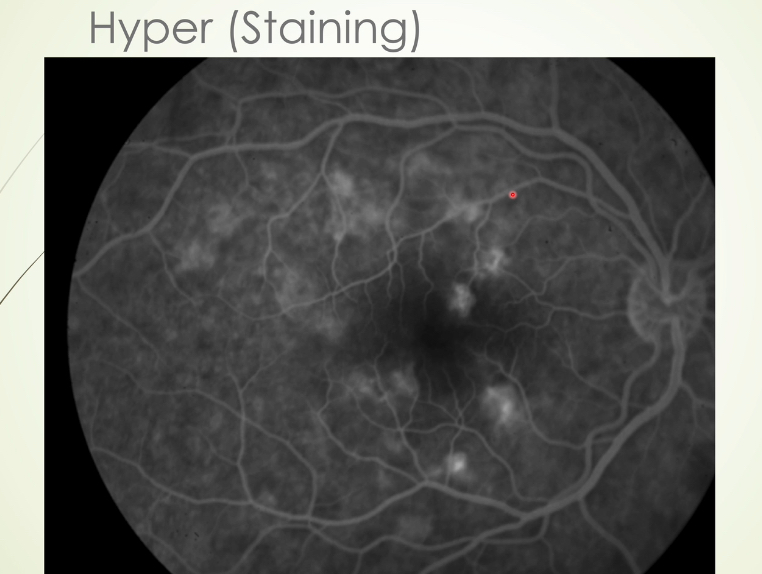
describe staining (hyperfluorescence) in FA
occurs when fluorescein binds with tissue or accumulates within tissue
hyperfluorescence gradually gets brighter (not as bright as leakage) in later stages but stays about the same size
typically seen after 2 min
ex: drusen, fibrotic tissue