Eval, Assess, Intervention, & Transfer Techniques
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
Factors impacting rehab
Comorbidities
Level of Amputation
●Cognitive Impairment
●Physical Conditioning
●Social Support
●Psychological Factors
role of PT in amputee rehab
Encouragement & education
● Positioning
● ROM, strength, sensory & balance assessment
● Residual limb care & desensitization
● Mobility & Gait (no hopping)
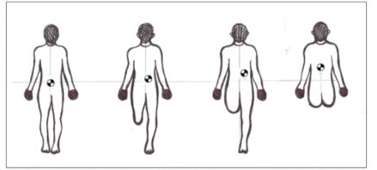
FUNCTIONAL BIOMECHANICS & POSTURE
Theoretical center point of human body presumed to be 2-4” below umbilicus. Dependent upon position of body & limbs.
COM
Front on & back off transfer approach is most often used for pts after
B LE Limb Loss, can be executed & practiced thru series of lateral weight shifts
Hip ROM assessment for transtibial amputation includes assessing what ROM?
extension
● assess in sidelying or Thomas Test position
Hip ROM assessment for transfemoral includes assessing extension via utilizing
sidelying or Thomas Test position
assess abduction/ adduction
*disposition to abductor tightness
strength assessment same as would in any eval, due to pain may be unable to apply resistance to surgical limb, so look at
Core strength, particularly important w/ this pop, is needed for bed mobility, transfers, & eventual gait/mvmt quality
sensation assessment of
light touch of sound limb & surgical limb
● Test proprioception of sound & surgical limbs at most distal jt
● Be sure to assess B LE
● Consider comorbidities including DM or PA
pain assessment post op is necessary. residual limb pain is pain felt in remaining tissue (expected sx after surgery) Can be caused by
poor prosthetic fit, bruising, rubbing
sensations felt in the part of the leg that is missing. NOT painful, may be lifelong
phantom sensation
pain felt in a portion of leg that is missing
■ Described as cramping, burning, tingling, sharp, shooting, electrical, squeezing, knifelike
■ Assess pain via 0-10 scale, FACES scale, word descriptions
phantom pain
○ Incidence of phantom pain 42.2-78.8%
for skin integrity assessment, measure girth to assess baseline for changes. Assess for skin impairments (wounds: surgical vs acquired)
○ Consider risk factors for skin breakdown. dressing type: Covered vs uncovered (pending physician orders). Education on need for
regular skin checks of both surgical & intact side. Utilization of mirror for visual assessment of difficult to visualize areas
what is method by which you control shape & edema of residual limb after amputation?
volume containment (residual limb shaping)
GOALS OF VOLUME CONTAINMENT:
Cylindrical Shape of residual limb
○ Better WBing surface
○ easiest to don prosthesis
● Reduce edema
○ Allow for prosthetic fit
○ decrease fluctuation in size of limb
METHODS OF VOLUME CONTAINMENT
Ace wrapping
● Stump shrinker
● Tubigrip
● Semi-rigid
● Rigid removable
● Rigid non-removable-IPORD
● Immediate post-op pylon-IPOP
What are advantages of ACE wrapping?
Inexpensive
○ Easily available
○ Easy to inspect wound
○ Excellent shaping & edema control
○ Easily modified to patient volume changes
What are disadvantages of ACE wrapping
Must be frequently reapplied
○ Difficult to teach to clinicians & pts
○ Requires 2 functional hands
○ Can be harmful when applied incorrectly
what are advantages of residual limb shrinker?
easy to don
○ easy to care for
○ easy to instruct pt & family
○ does not have to be re-applied
○ easy to view limb
what are disadvantages of residual limb shrinker?
not accessible outside clinics
○ expensive to replace
○ Contraindicated for sutures & sensitive skin (not used in phase 2)
○ loses effectiveness as limb shrinks
**Progress from wrapping to shrinker occurs when
sutures & staples are removed
what are some advantages of Tubigrip?
ease of application
○ easy to care for
○ easy to view limb
what are some disadvantages of Tubigrip?
not durable
○ increased cost
○ can roll & constrict
○ can cause window edema at end
○ difficult to purchase out of hospital
what is a gauze impregnated w/ calamine lotion or zinc oxide. Wrap onto residual limb w/o applying any tension tightens as it dries. This hardens into a semi-rigid cast.
Semi-Rigid Limb Shrinker: UNNA BOOT
what are some advantages of a Semi-Rigid Limb Shrinker: UNNA BOOT?
Good compression
○ Allows skin checks every 3 days
what are some disadvantages of a Semi-Rigid Limb Shrinker: UNNA BOOT?
Messy to apply
○ Can be expensive over time
○ Not easily applicable by a pt
what are some advantages of a rigid removeable?
Excellent edema control
○ easy to apply
○ skin is accessible
○ modified as limb shrinks-sock mgmt
○ Protection of residual limb against accidental trauma
what are some disadvantages of a rigid removeable?
time consuming to fabricate
○ skill to fabricate
○ donning can injure very fragile skin
○ Must closely monitor sock ply
what is a Rigid Cast above knee?
●1st cast changed 3 days
●Subsequent cast changes every 7 days, used in oncology realm
NON-REMOVABLE RIGID : IPORD
what are some advantages of a non-removable rigid: IPORD?
Best edema control
○ excellent wound protection
○ aids in contracture prevention
○ Increased pt confidence
what are some disadvantages of a non-removable rigid: IPORD?
Cannot view wound (not for disease pts)
○ Skill in fabricating
○ Heavy
○ Skin breakdown as limb shrinks
what has a connector, plyon, & foot are immediately attached to cast?
● Generally there is a protocol for WBing
○ Start at 20%
○ Progress
immediate post-op pylon: IPOP
what are some advantages of an immediate post-op pylon: IPOP?
● aids in contracture prevention
● Increased pt confidence
● Allows early WBing
● reduces phantom pain & edema control
● decreased hospital stay
what are some disadvantages of an immediate post-op pylon: IPOP?
Cannot view wound
● Skill in fabricating
● Heavy
● Skin breakdown as limb shrinks
● Risk of wound irritation
pt education regarding limb volume should include factors that impact limb volume such as
Water retention, Salt intake, Fluid intake, Activity Level
Pressure changes related to use of prosthesis
Gender- females have greater volume changes
Health Factors: Dialysis, medications, Lasix, PVD
Time since amputation
pt education regarding limb volume should include prognosis
7.3% volume decrease in 1st 3 months
35% after 5-6 months
Typically stabilize after that time
Transtibial limb loses 4-10% of volume in an 8 hour day, how much occurs in 1st 2 hrs?
90%, Prosthetic use may require more ply as day progresses due to volume loss
Residual Limb Wrapping compression must be worn up to
23 hrs per day; remove for hygiene & skin check
residual limb wrapping should progress to
residual limb shrinker when sutures & staples are removed
Interventions for residual limb volume control in addition to compression
Elevation & exercises (muscle pump)