Pediatric Endocrine Disorders
1/14
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
The Endocrine System is…
Composed of glands, tissues, or clusters of cells that produce and release hormones.
Influences all physiological effects:
Growth and development
Metabolic processes related to fluid and electrolyte balance and energy production
Sexual maturation and reproduction
The body’s response to stress
Anterior Pituitary Disorders
Growth Hormone Deficiency:
Physical Signs:
Poor growth
Short stature
Complications:
Altered carbohydrate, protein, and fat metabolism
Hypoglycemia
Glucose intolerance
Treatment:
Supplemental growth hormone
Regular visits to an endocrinologist for growth hormone injections until puberty.
Precocious Puberty:
Physical Signs:
Development of sexual characteristics before the usual age of puberty
Breast buds, pubic hair
More common in females and children with high adipose levels
Concerns:
Once a child enters puberty, especially females (menstruation), growth slows, leading to concerns about height velocity, bone, and organ maturation.
Treatment:
Education
Medications to slow secondary sexual development (may or may not be used depending on the child’s proximity to normal puberty)
Promote psychosocial well-being
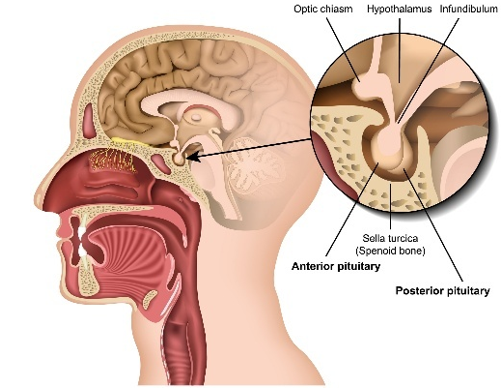
Posterior Pituitary Disorders
Diabetes Insipidus (DI):
Deficiency of ADH—losing more water.
Causes:
Tumor, genetics, or idiopathic
Pathophysiology:
Kidneys lose high amounts of water and retain sodium in the serum.
Physical Signs:
Polydipsia
Polyuria
Diagnostic Findings:
Specific gravity < 1.005
Elevated serum sodium
Treatment:
Low sodium/protein diet
Desmopressin Acetate (DDAVP)
Syndrome of Inappropriate Antidiuretic Hormone (SIADH):
Excess ADH—holding onto more water.
Physical Signs:
Decreased urine output
Weight gain
Diagnostic Findings:
Specific gravity > 1.030
Decreased serum sodium
Complications:
May have neurological symptoms as sodium levels decrease.
Risk for fluid overload.
Treatment:
Correct underlying disorder
Fluid restriction
Sodium chloride IV
Diabetes Insipidus vs SIADH (comparison)
Diabetes Insipidus (DI):
"High and dry"
Increased urination
Hypernatremia
Serum osmolality > 300 mOsm/kg
Urine specific gravity < 1.005
Decreased urine osmolality
Dehydration, thirst
VS
Syndrome of Inappropriate Antidiuretic Hormone (SIADH):
"Low and wet"
Decreased urination
Hyponatremia
Serum osmolality < 280 mOsm/kg
Urine specific gravity > 1.030
Increased urine osmolality
Fluid retention, weight gain, hypertension
Thyroid Disorders
Hyperthyroidism:
Hyperfunction of the thyroid gland (elevated T3 and T4).
Peaks during adolescence due to Graves’ disease.
Symptoms:
Nervousness/anxiety
Diarrhea
Heat intolerance
Weight loss
Smooth, velvety skin
Complications:
Thyroid storm
Treatment:
Antithyroid medications
Radioactive iodine therapy
Thyroidectomy
Hypothyroidism:
Malfunction of the thyroid gland.
Insufficient production of thyroid hormone (low T3 and T4).
Symptoms:
Tiredness/fatigue
Constipation
Weight gain
Dry, thick skin; edema of face, eyes, and hands
Decreased growth
Complications:
Intellectual disability
Short stature
Growth failure
Delayed physical maturation.
Treatment:
Thyroid replacement therapy (e.g., Synthroid)
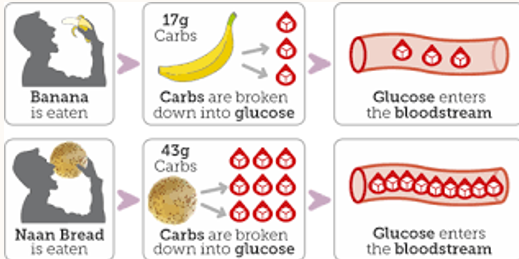
Types of Diabetes Mellitus
Impaired carbohydrate, protein, and lipid metabolism.
Type 1 Diabetes:
Caused by a deficiency of insulin secretion due to pancreatic beta-cell damage.
Type 2 Diabetes:
A consequence of insulin resistance that occurs at the level of skeletal muscle, liver, and adipose tissue, with varying degrees of beta-cell impairment.
Gestational Diabetes:
Diabetes that develops during pregnancy.
Secondary Diabetes:
Occurs as a result of certain conditions such as:
Cystic fibrosis
Glucocorticoid use (e.g., Cushing syndrome)
Infections
Autoimmune syndromes
Genetic syndromes (e.g., Down syndrome, Klinefelter syndrome, Turner syndrome)

Type 1 Diabetes
Deficiency of insulin secretion due to pancreatic β-cell damage.
Autoimmune in nature.
Onset usually in younger children.
DKA (Diabetic Ketoacidosis) is more likely in Type 1.
Sometimes has a genetic predisposition.
Affects all ethnic groups.
Signs & Symptoms:
Polyuria
Polydipsia
Polyphagia
Weight loss
Abdominal cramping/nausea/vomiting
Headache/fatigue/blurred vision
*School-aged child will present with, sudden night time enuresis (wetting the bed)*
Diagnostics:
Glucosuria (glucose in the urine)
Ketonuria (ketones in the urine)
Hemoglobin A1C (reflects average blood glucose over 3 months)
Serum Glucose > 200 mg/dL
Random Glucose > 200 mg/dL accompanied by typical symptoms of diabetes
Honeymoon Phase
Some people with type 1 diabetes experience a "honeymoon" period where the body produces enough insulin to lower blood glucose levels.
This phase typically occurs after starting insulin therapy, and you may not need to manage blood glucose as actively.
The honeymoon phase can last from 1 week to 1 year.
It does not mean that the diabetes is gone, and the pancreas will eventually be unable to produce enough insulin. Without treatment, symptoms will return.
Diabetic Ketoacidosis (DKA)
If diabetes (especially type 1) goes unrecognized or inadequately treated, diabetic ketoacidosis (DKA) or fat catabolism can develop.
This occurs when there is a deficiency or ineffectiveness of insulin, causing the body to use fat instead of glucose for energy.
Signs & Symptoms: MEDICAL EMERGENCY
Anorexia
Nausea/vomiting
Lethargy
Stupor
Altered level of consciousness/Confusion
Decreased skin turgor
Abdominal pain
Kussmaul respirations and air hunger
Fruity (sweet-smelling) or acetone breath odor
Presence of ketones and glucose in urine and blood
Tachycardia & Tachypnea
Metabolic acidosis
Alterations in potassium (K+)
Severe insulin deficiency
Serum glucose > 300 mg/dL (usually 400 to 800 mg/dL)
If left untreated, coma and death may occur.
Diagnostic Values for DKA:
Hyperglycemia: Serum glucose > 300 mg/dL (typically 400-800 mg/dL)
Acidosis: pH <7.3, HCO3- <15 mEq/L
Interventions:
Fluid Therapy:
Initial 20 mL/kg bolus of 0.9% normal saline over 1 to 2 hours.
Hypertonic solution to reduce the risk of cerebral edema.
Continuous IV fluid replacement.
EKG Monitoring.
Frequent V/S and physical assessment. (neuro checks)
Monitoring Urine Output.
Frequent blood glucose checks, potassium, and sodium levels.
Continuous insulin drip (IV Regular insulin).
Don’t drop blood glucose too quickly to avoid cerebral edema. Blood glucose should not fall more than 100 mg/dL per hour.
Types of Insulin
Rapid-Acting Insulin
Long-Acting Insulin
Intermediate-Acting Insulin
Insulin Pumps
Sliding Scales
Diabetes Mellitus: Nursing Assessment
Regulating Glucose Control and A1C Levels:
Target A1C for children should be <7.5%.
Monitor and Manage Complications:
Regular monitoring for potential complications such as diabetic retinopathy, nephropathy, neuropathy, and cardiovascular issues.
Education:
Provide ongoing education about diabetes management, nutrition, insulin administration, and recognizing signs of complications.
Support the Child and Family:
Offer emotional and psychological support to help cope with the challenges of managing diabetes.
Type 2 Diabetes
Not autoimmune
Onset usually in adolescents
DKA less likely but still possible
Usually linked to a family history
Affects Disproportionate Ethnic Groups:
Native-American
African-American
Latino
Asian/Pacific Islander
Signs & Symptoms:
Polyuria
Polydipsia
Polyphagia
Obesity
Hypertension
Dyslipidemia
Goals for Diabetes Mellitus Management
Achieve normal growth and development.
Promote optimal serum glucose control:
Near normal A1C.
Prevent hypoglycemia.
Prevent complications:
Both in the hospital and long-term.
Promote adjustment to the disease:
Address age-related changes and considerations.

Diabetes Mellitus: Diet & Exercise
Diet: Low in saturated fats and concentrated carbohydrates.
Identifying: Carbs, fats, and proteins.
Carb counting.
Meal plan: 3 meals per day + snacks for consistency.
Encourage regular exercise.
Age-appropriate sports.
Age-Related Considerations of Diabetes Mellitus
Infant:
Educate the family, watch for extreme fluctuations in serum glucose. (they’re growing fast!)
Toddlers:
Picky eaters, temper tantrums, emphasize routine.
Preschoolers:
May begin to participate, increasing awareness of diabetes.
School-Age:
Socialization, more participation in diabetes management.
Adolescent:
Body image concerns, independence, peer acceptance, maintain consistency.