AT 505 Ch.8 pt 2
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
primary headaches
Extremely common; headache is the pathology; no other condition causes it
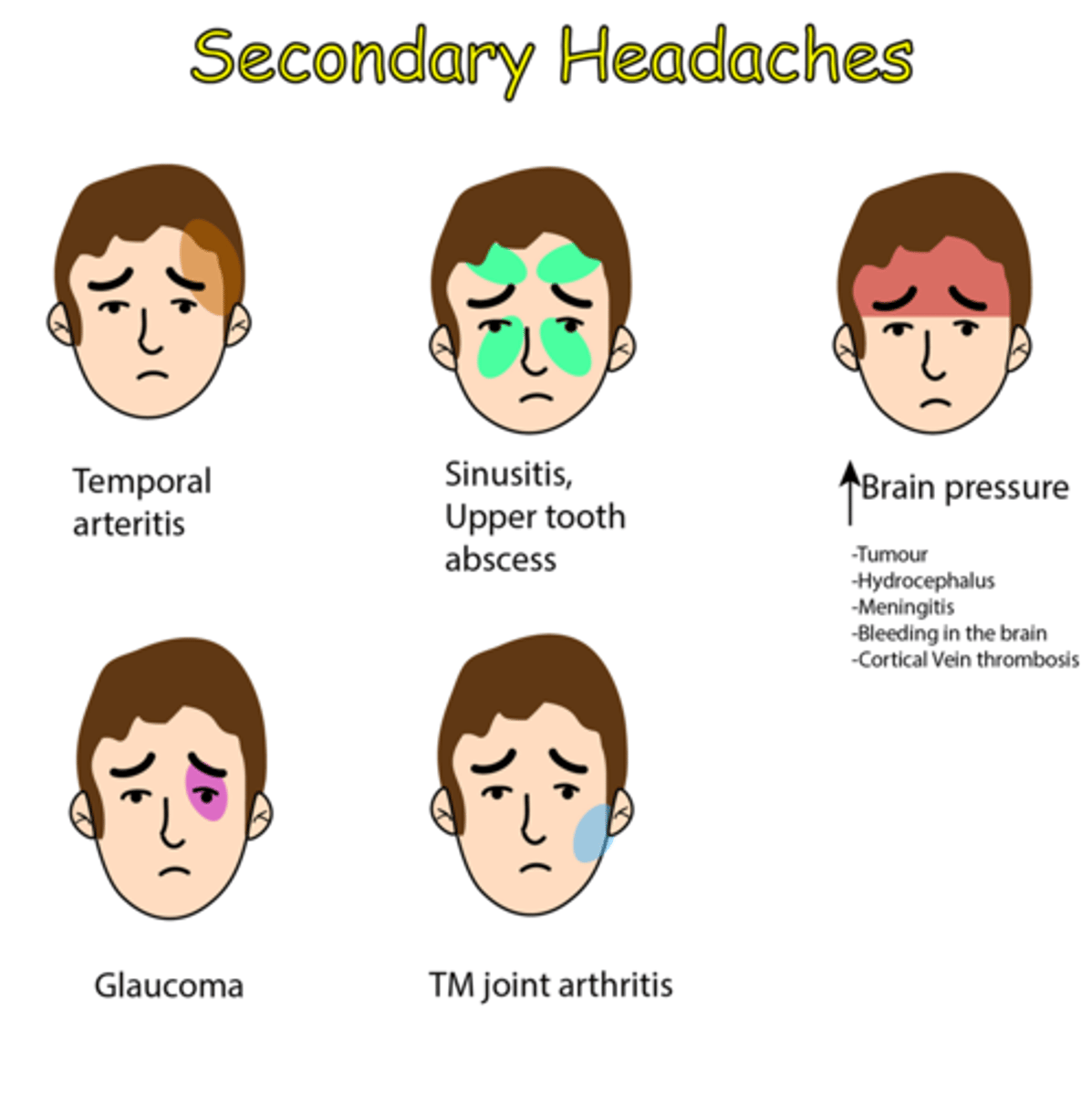
secondary headaches
Felt as a result or symptom of a different pathology (e.g., whiplash, environmental changes,TBI)
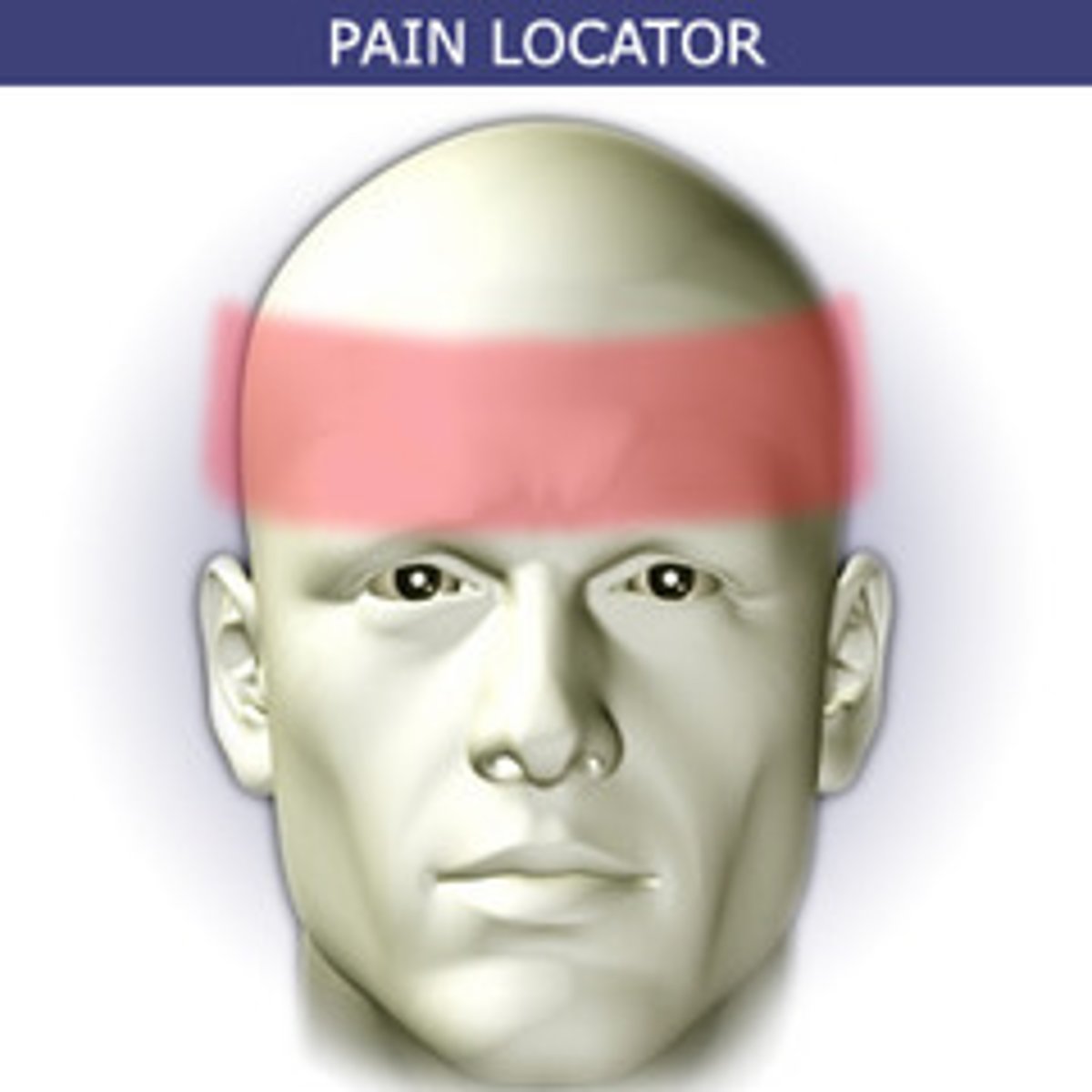
Tension headaches
Present as bilateral, mild to moderate pain; 15 or more tension headaches per month are deemed chronic tension headaches
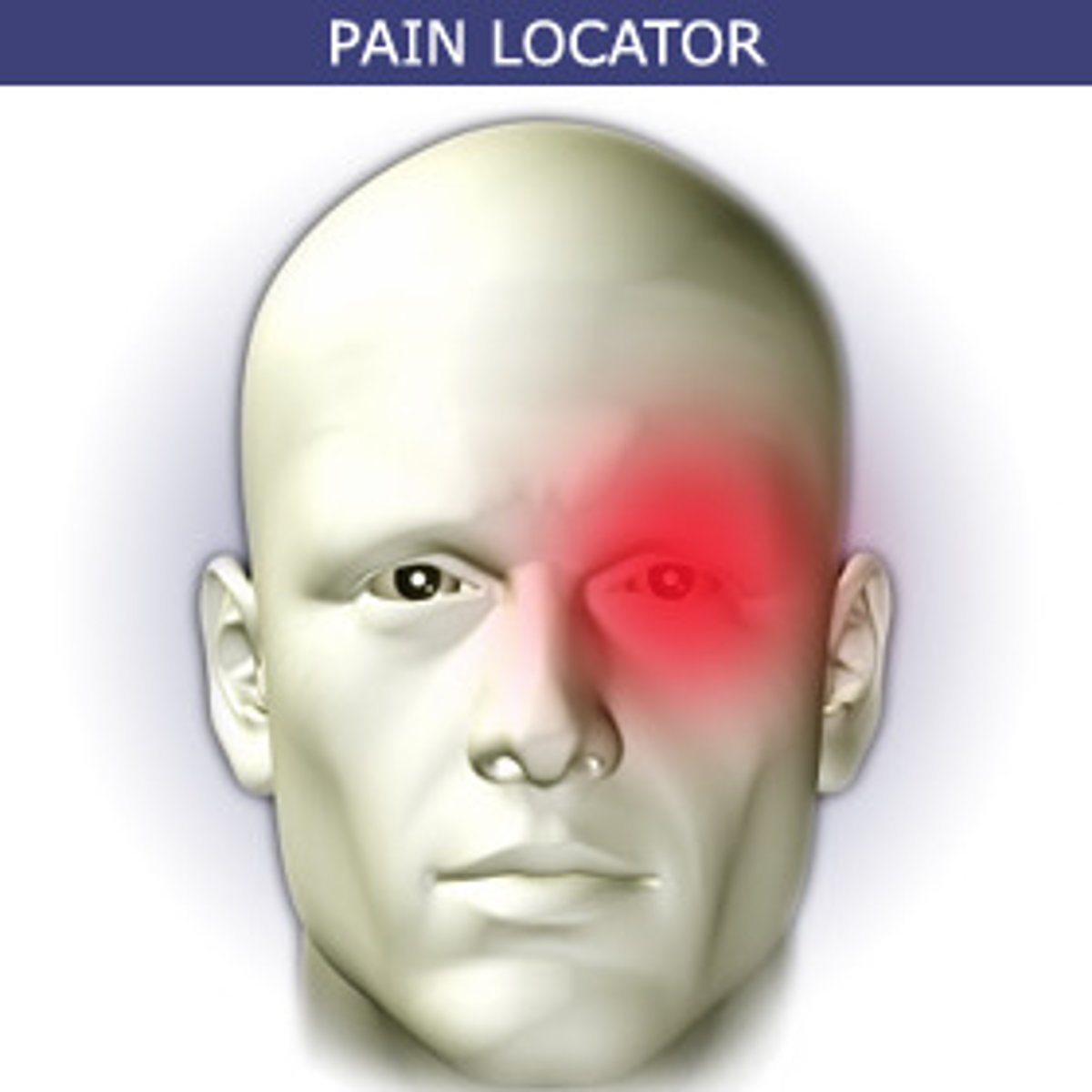
Trigeminal autonomic cephalalgias (cluster headache)
Present along the trigeminal nerve and result in autonomic nervous system symptoms,such as pain in the face, eye watering, or eye redness
migraines
Without aura, with aura, and chronic
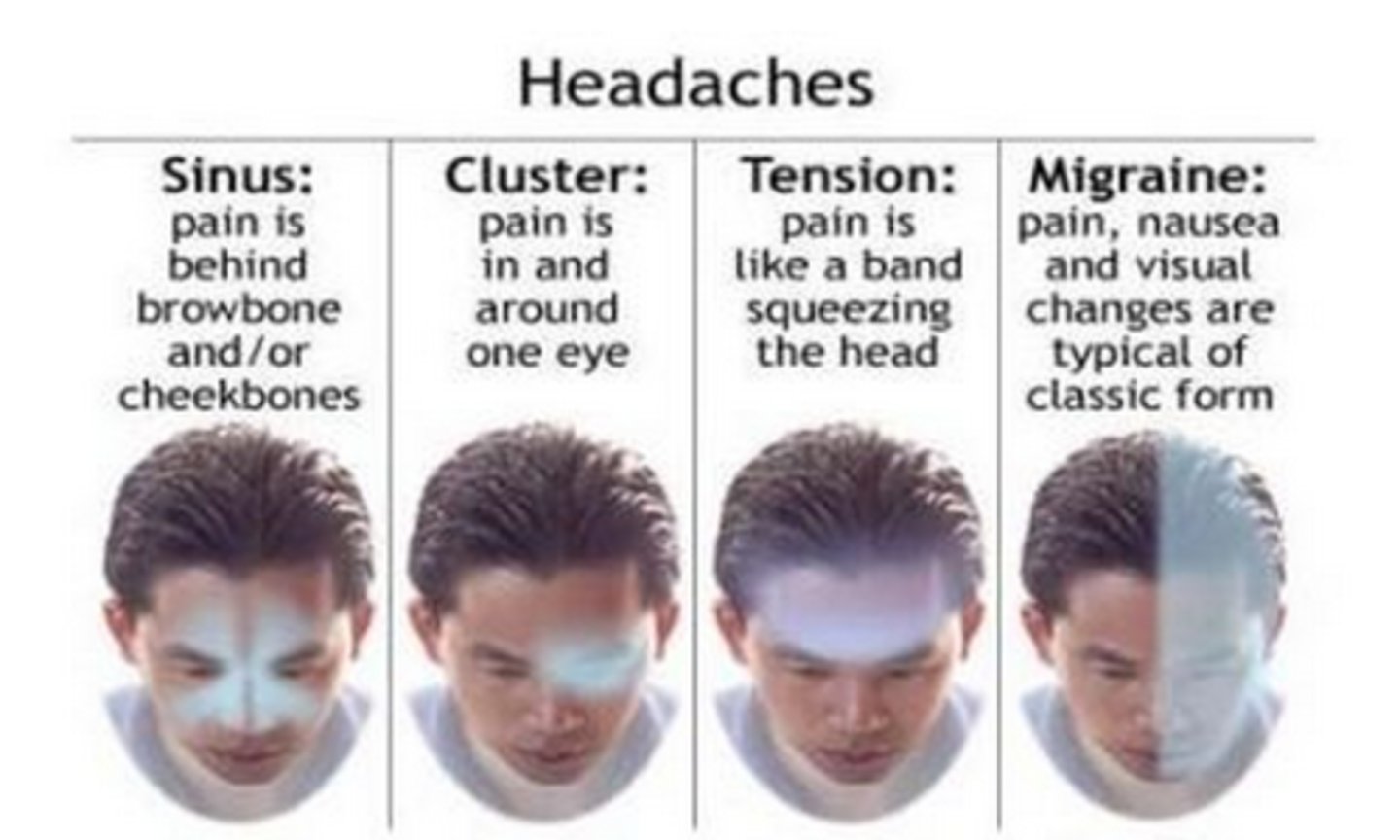
SInus headaches
pain is usually behind the forehead or cheekbones
SSNOOP
-To determine whether a headache warrants further evaluation
Systematic signs/symptoms
Systemic disease
Neurological signs/symptoms
Onset sudden
Onset in individuals over 40 years
Previous headache pattern
Systematic signs/symptoms (Ssnoop)
Present with fever, malaise, lethargy - possible meningitis, encephalitis
Systemic disease (sSnoop)
Comorbidity of autoimmune disease - possible meningitis
Neurological signs/symptoms (ssNoop)
Present with decreased myotomes or dermatomes - possible transient ischemic attack,stroke, central nervous system infection
Onset sudden (ssnOop)
Complains of thunderclap headache - possible hemorrhage or epidural/subdural hematoma
Onset in individuals over 40 years (ssnoOp)
Present with pain local to temples - possible temporal arteritis
Previous headache pattern (ssnooP)
More/less frequent - possible change in primary condition, medical overuse headache
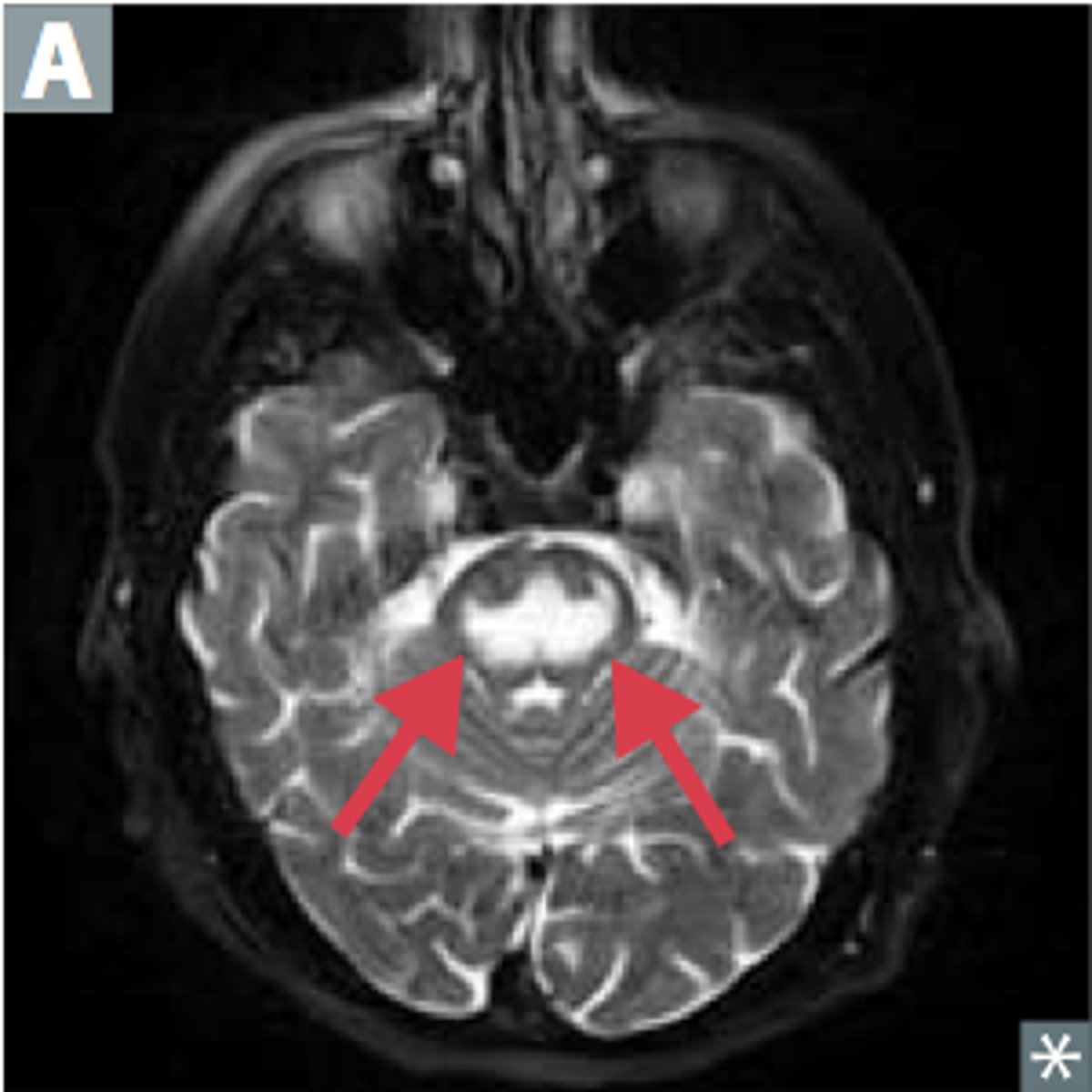
stroke
Neurovascular injury, the result of a cerebrovascular accident,where the brain cannot function due to a sudden vascular deficit
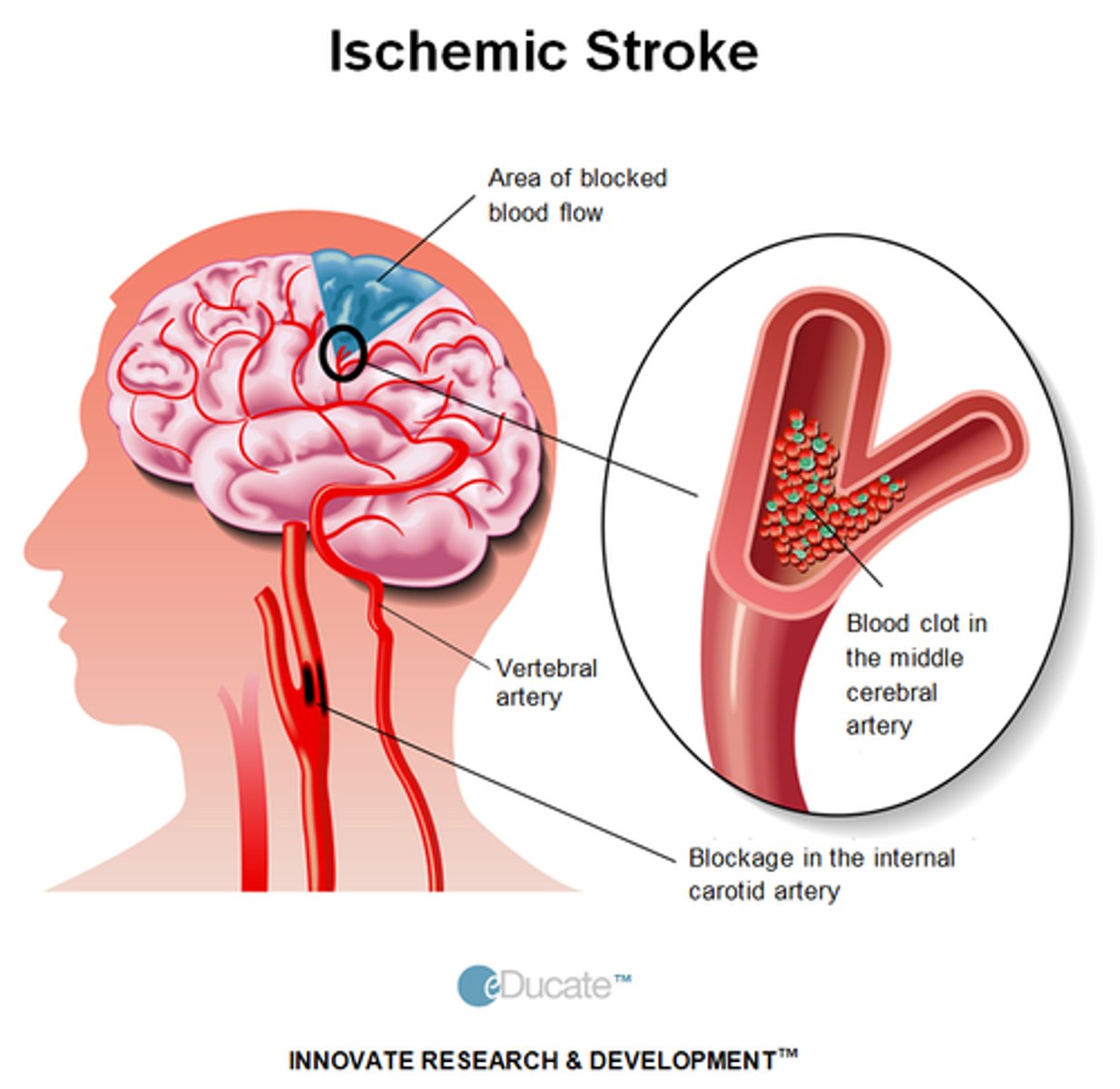
Ischemic strokes
• Embolisms and thrombosis
(MOI); brain is deprived of oxygen and glucose
• Risk factors: Dyslipidemia, diabetes, and smoking
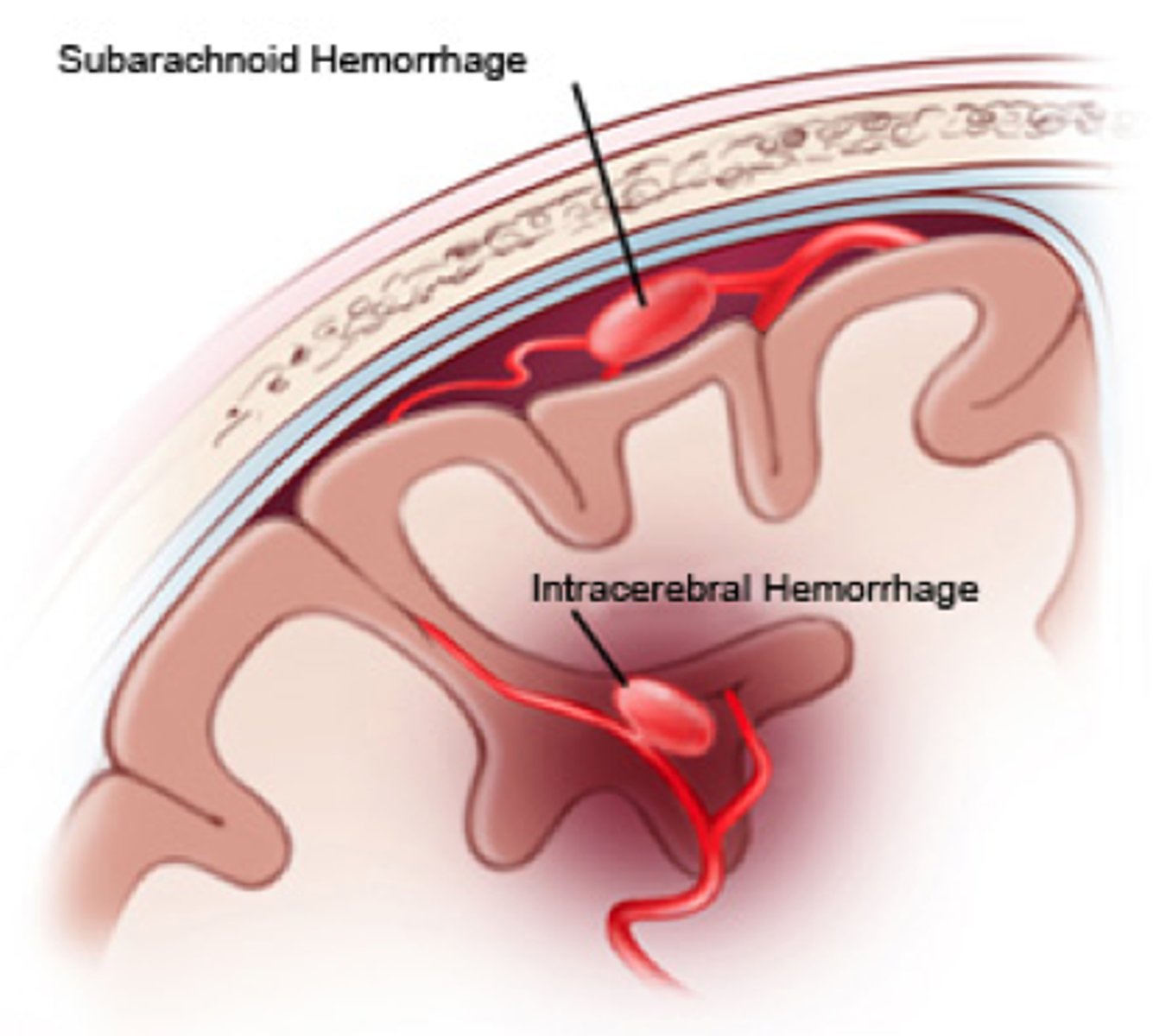
Hemorrhage strokes
• Weakened arterial vessels; ruptured blood vessel in the brain results in neural injury
• Risk factors: Drug use and exercise
immediate management for strokes
• Transport immediately to hospital with advanced stroke care
• FAST: Facial drop, Arm weakness, Speech difficulty, Time to call 9-1-1

general seizures
Including tonic-clonic, absence, and atonic seizures, affect both cerebral hemispheres and cause loss of awareness
focal onset seizure
Start in a specific area of the brain and can either occur with or without convulsions
unknown onset seizures
They are not witnessed, they occur during sleep, or the part of the brain involved is not known
sezuires typically last _______ minutes and can occur in clusters
3
Seizure clusters may last minutes to an hour; the longer durations result in poor outcomes for the patient.
true
seizure causes
• Congenital disorders, metabolic abnormalities, toxins, infections, and inflammatory conditions
• Hypoglycemia, hyponatremia, hypernatremia•
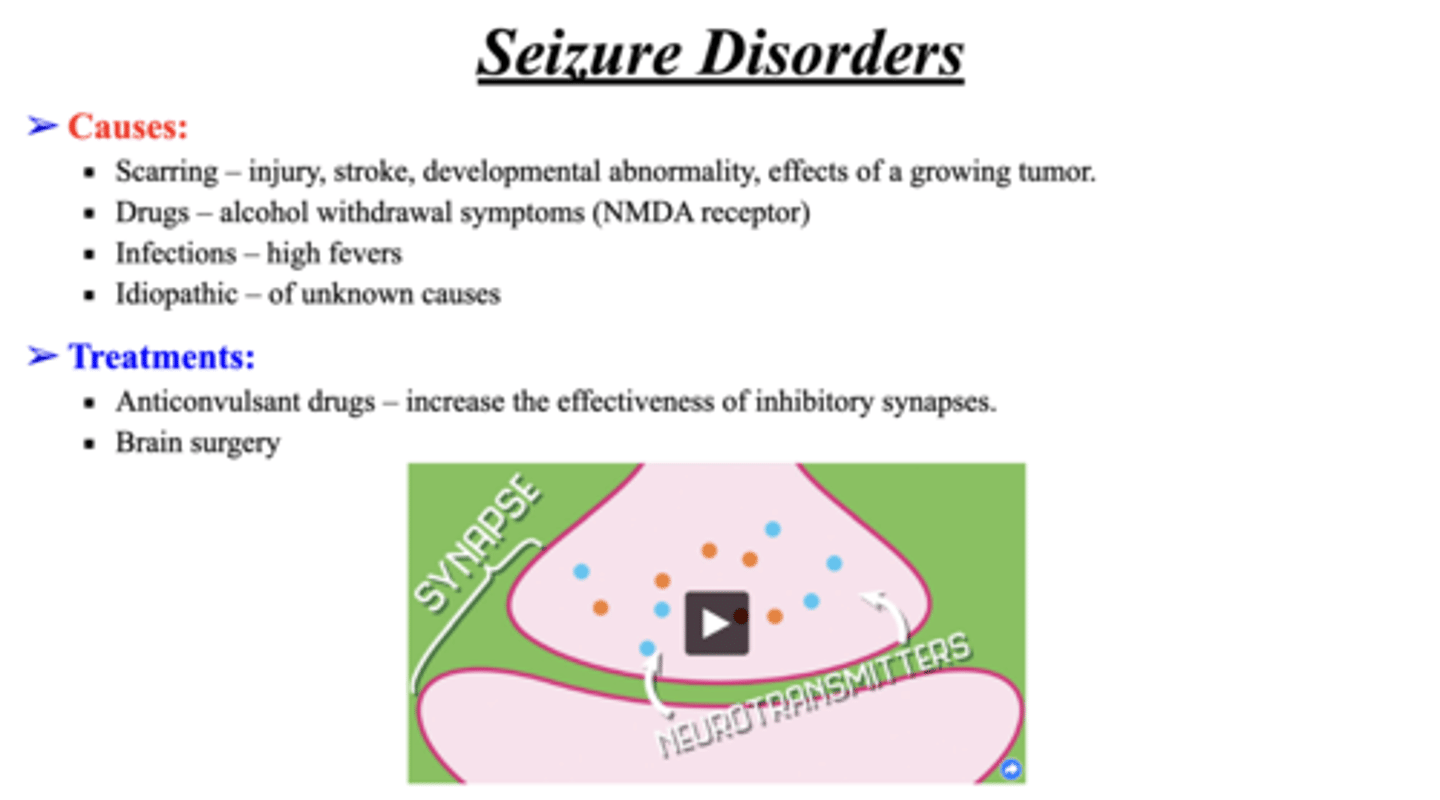
immediate management for seizures
Depends on cause and type of seizure, if physical convulsions protect patient from injury but do not restrain
• Hypoglycemic: Administer simple carbohydrate
If the patient has epilepsy and the seizure presents in the expected pattern, not advanced medical care is required
true
Immediate advanced medical care transport for seizures
• Does not have epilepsy
• Long-duration
• Frequent seizures
• Presentation change
Osmotic demyelination syndrome
Neurological damage to brain stem occurs if sodium levels rise to quickly
• Often result of hyponatremia
possible causes of altered mental status
Adrenal insufficiency, diabetic ketoacidosis,hypertensive emergency, hypoglycemia, hypothermia, myxedemacoma, orthostatic hypotension
risk factors of altered mental status
Heart failure or abnormal sinus rhythms
immediate management of altered mental status
Monitor vitals and activate EMS
• Assess body temperature, BP, blood glucose--differential diagnosis
overview of facial injuries
Always begin assessment with mental status and ABCDE
• Control bleeding with direct pressure and dressing
The Secondary survey to determine the presence of underlying injuries should follow the primary survey.
Ocular Indicators of Closed Head Injury
Anisocoria (unequal pupil size; <3mm)
• Unequal movement
• Unequal alignment; differing directions
• Inability to follow finger motion
• Bleeding under conjunctiva that obscures the sclera (whiteportion)
• Protrusion or bulging
Corneal Abrasion and Foreign Objects in the Eye
Occur when the epithelium of the eye's surface
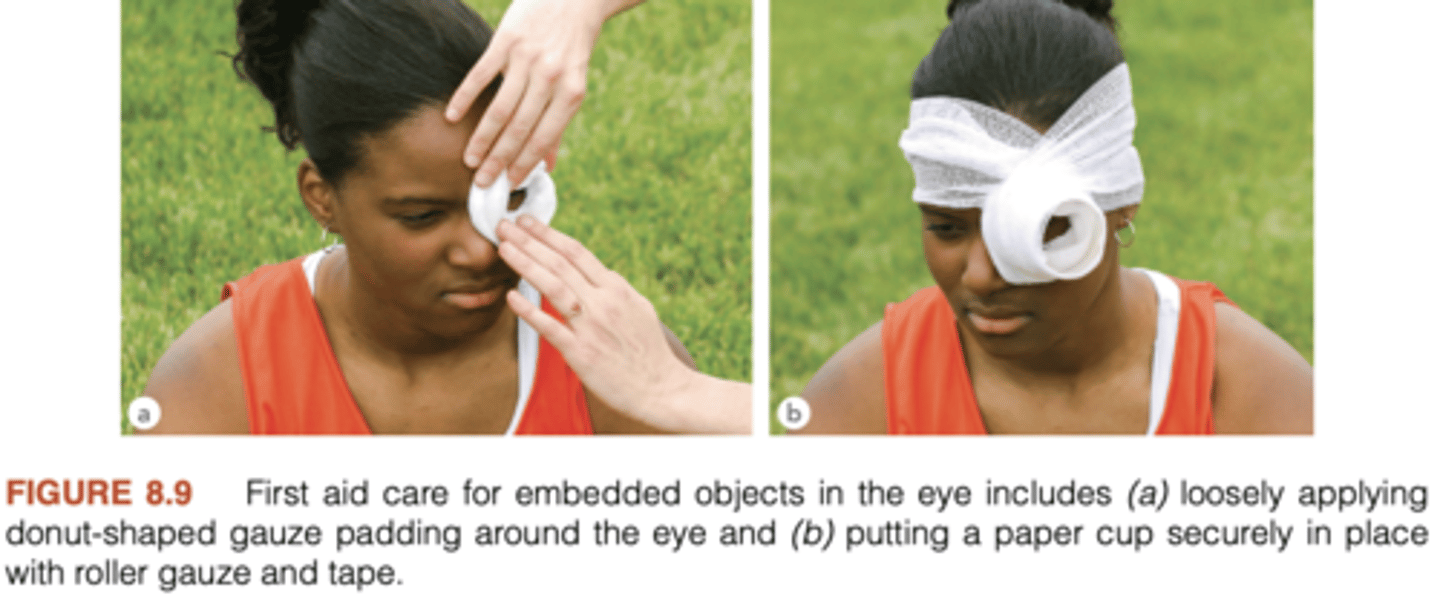
immediate management for corneal abrasions
• Irrigate eye (from nose outward)
• Assess extraocular motion, pupillary reaction, and visual acuity
• If impaled: Leave object, bandage, and cover with moist sterile dressing;transport immediately.
• If transporting, encourage the patient to lie supine and consider covering both eyes to avoid unnecessary movement
retinal detachment
Thin layer of tissue lining the back of the eye
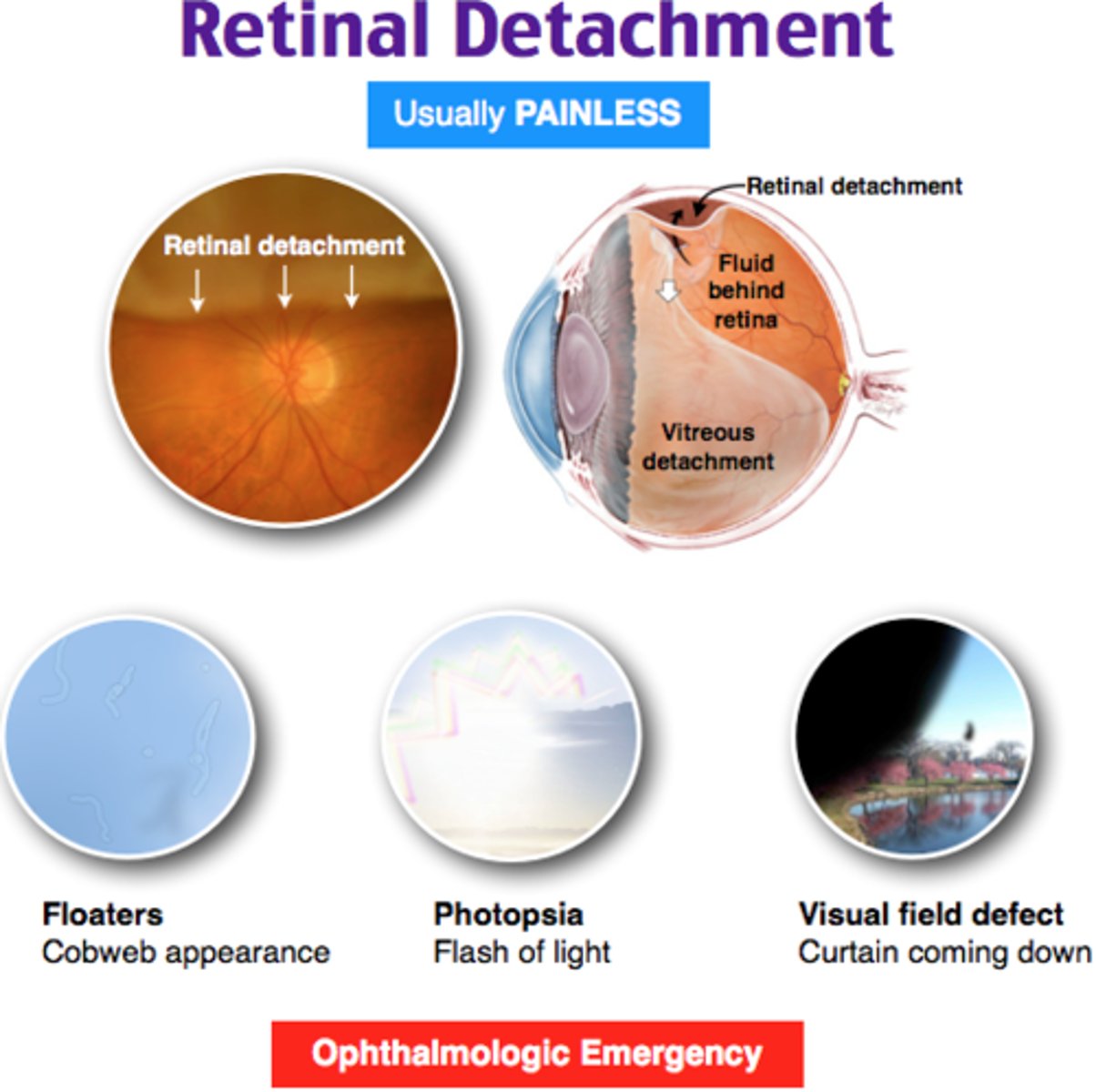
signs/symptoms of retinal detachment
• Shadow or curtain falling over visual field
• "Floaters" (e.g., dark spots or strands)
• Abnormal flashes of light (peripheral)
MOI of retinal detachment
blunt trauma
immediate management of retinal detachment
Refer to ophthalmologist•
Avoid pressure
Minimize eye movement
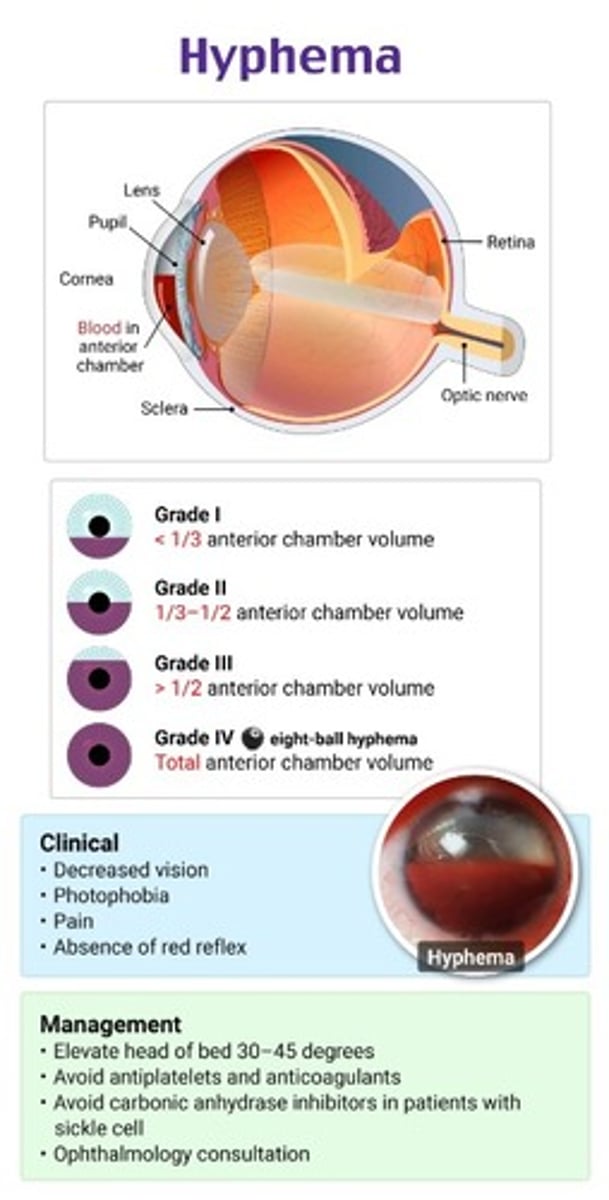
hyphema
Bleeding into the anterior chamber of the eye, and can cause difficulty with visualizing the iris
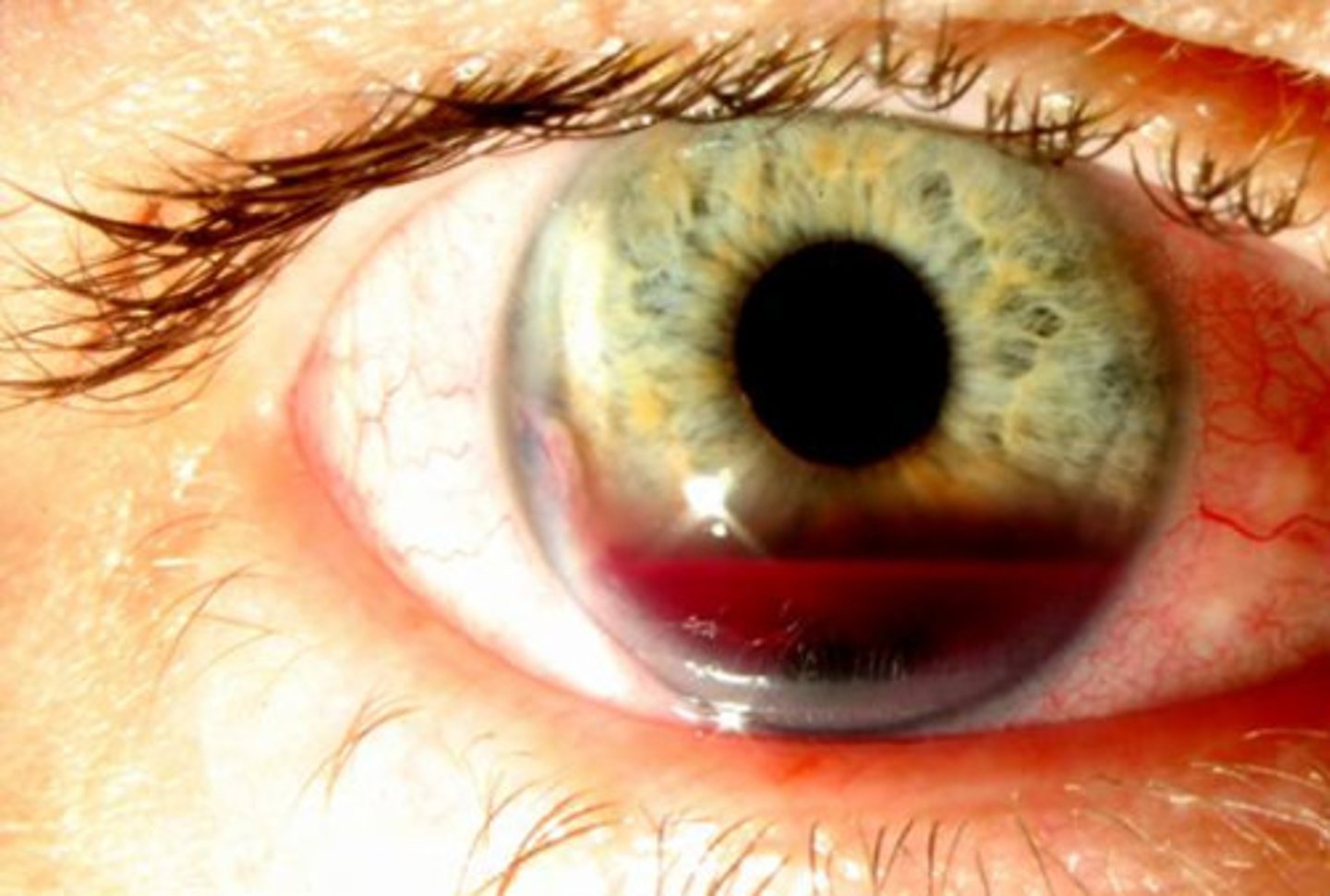
MOI of hyphema
Blunt trauma to eye or orbital socket fractures
signs and symptoms of hyphema
• Pain and discomfort
• Visual sign of blood in eye
•Cloudy or blurry vision
Tympanic Membrane Rupture
Occurs when the thin tissue separating the ear canal from the eardrum is torn
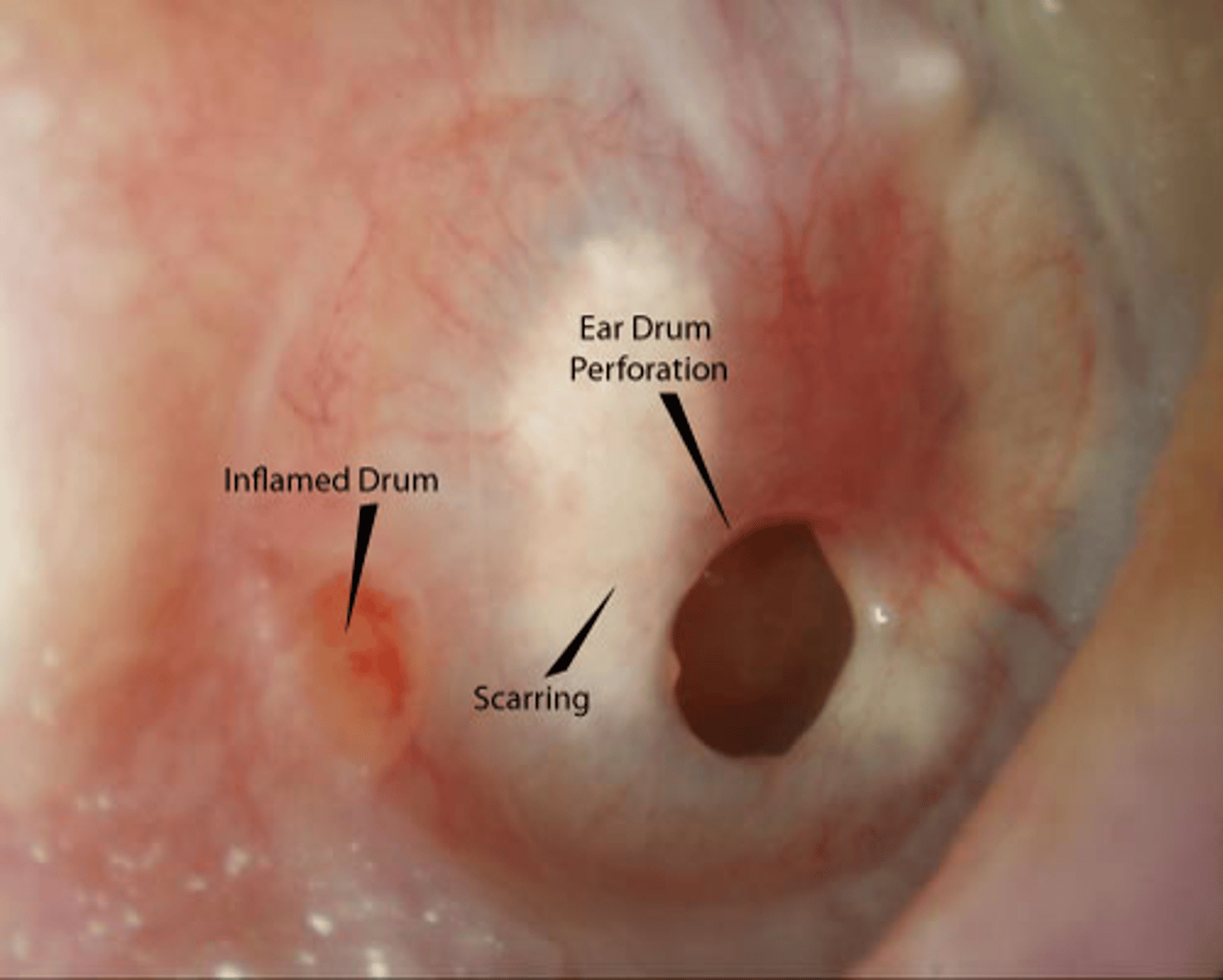
MOI of Tympanic Membrane Rupture
Blunt trauma to ear
risks of Tympanic Membrane Rupture
• Wrestling and boxing participation
• Current ear infection
• Previous history of rupture
• Ear surgery for tubes in canal
• Scuba diving
• Traumatic ear injury•
Insertion of objects (cotton swab)
signs and symptoms of Tympanic Membrane Rupture
• Pain following a popping sensation
• Hearing loss
• Tinnitus
• Dizziness•
Presence of fluid (e.g., watery pus or blood) in the canal
immediate care for tympanic membrane rupture
• Referral to determine surgical need and care
• Antibiotics often administered•
Over-the-counter eardrops
• Avoid blowing nose
most common facial fractures
margin orbital fractures

4-18% of sport fractures are
facial fractures
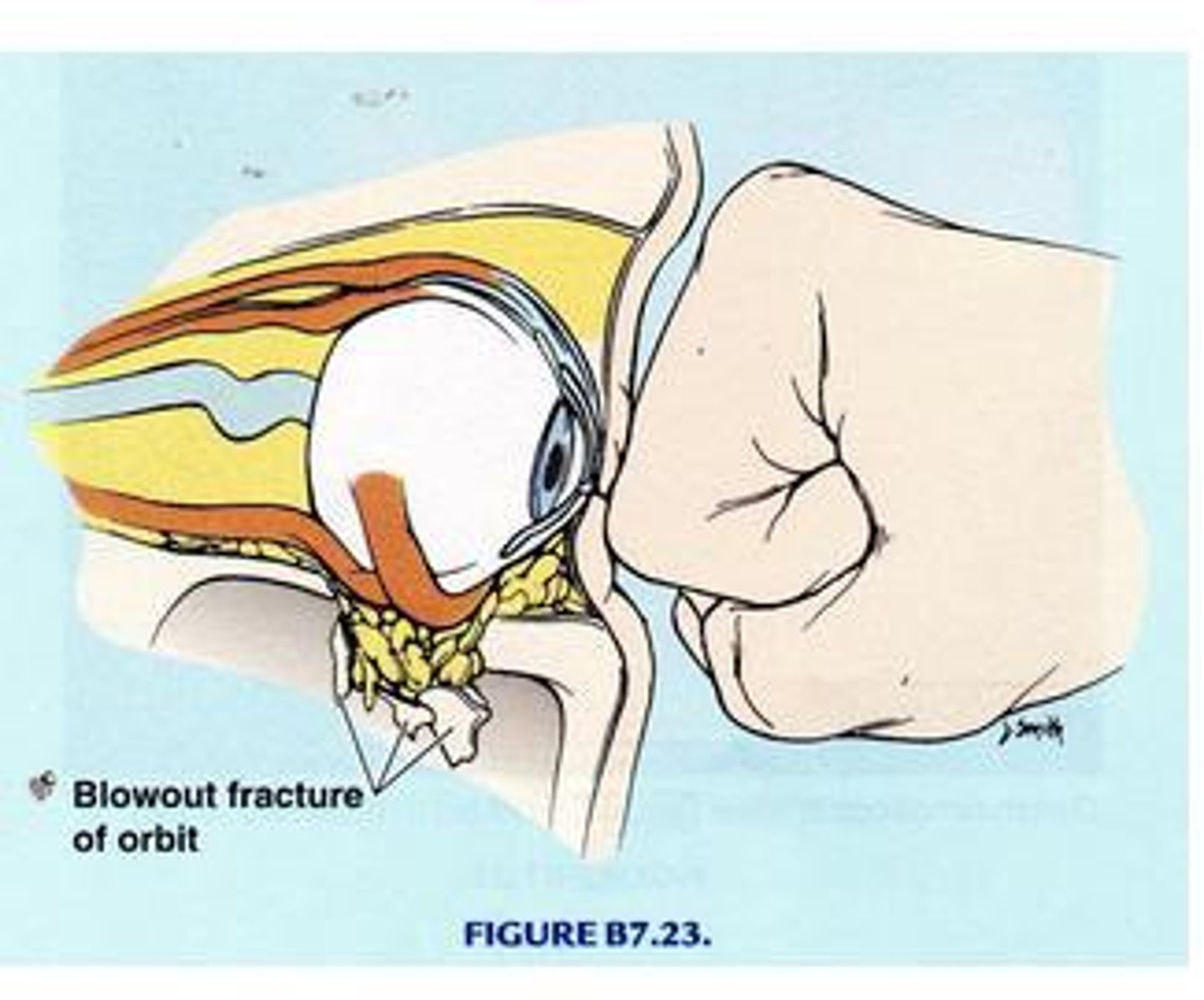
blowout fractures
orbital floor fractures
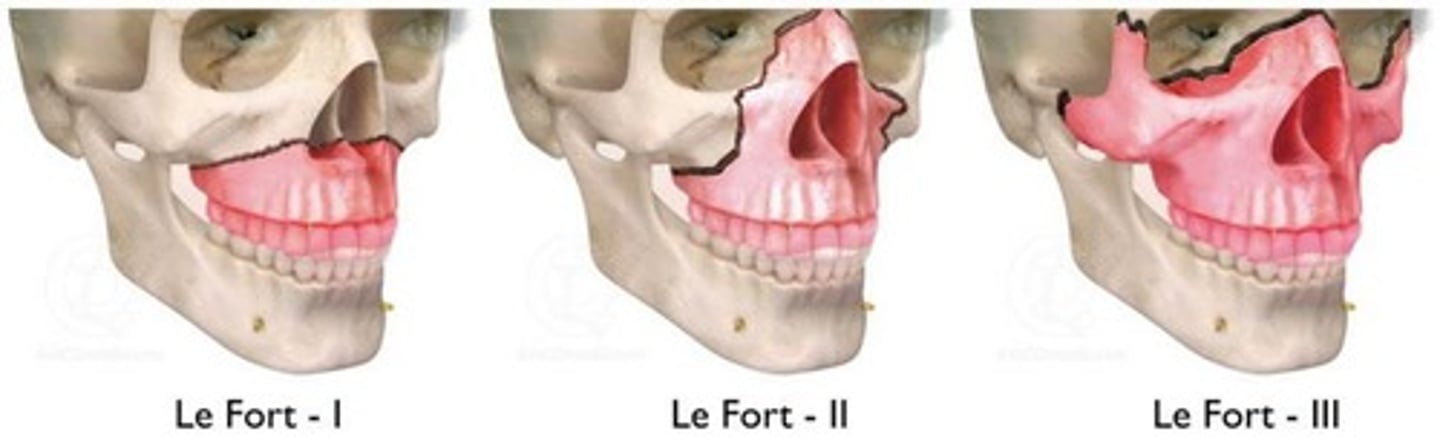
Maxillary fractures
Le Fort fractures types I-III
Mandibular fractures
Typically occur at or just below to the condyle and present with malocclusion
Facial fractures may be associated with head and cervical spine injuries
true
facial fracture risks
Sport participation with high-velocity projectiles followed by motorcycle accidents.
signs and symptoms of facial fractures
• Difficulty breathing and/or speaking
• Blurred or double vision
• Numbness
• Pain
• Malocclusion
• Blow-out fracture: Difficulty or inability to look upward
immediate management of facial fractures
• Place in a seated position unless suspected cervical spine injury
• Assess airway, circulation
• Address bleeding and transport if necessary
Type 1 Le Fort Fracutres
Fractures occur in the maxilla and separate the teeth from the upper face
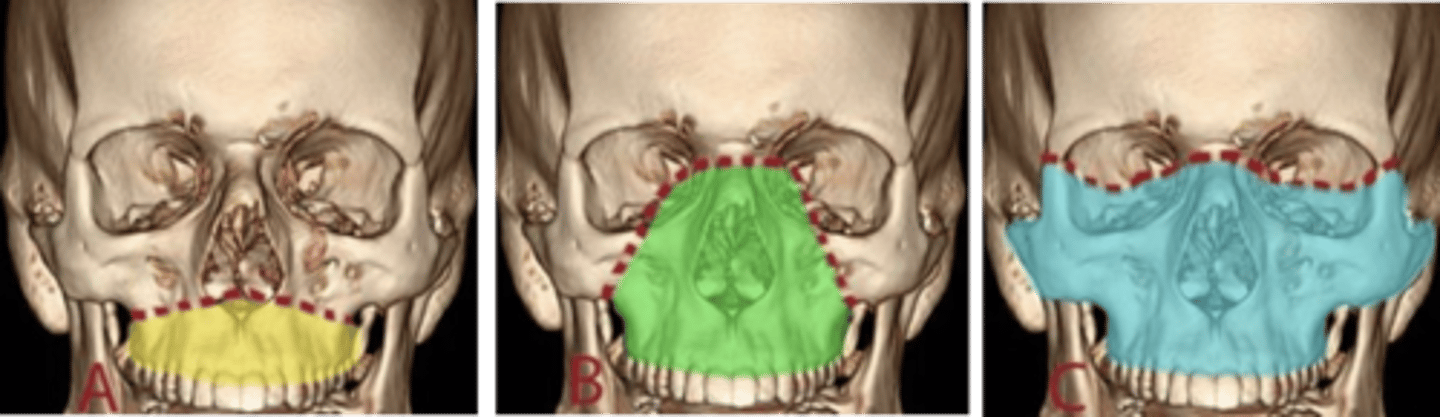
Type 2 Le Fort Fracutres
Fractures are pyramidal in nature, affecting the upper teeth, maxillary sinuses, inferior orbital rim, and nasal bones
Type 3 Le Fort Fracutres
Fractures include the nasofrontal suture, maxillofrontal suture, orbital wall,and zygomatic arch.
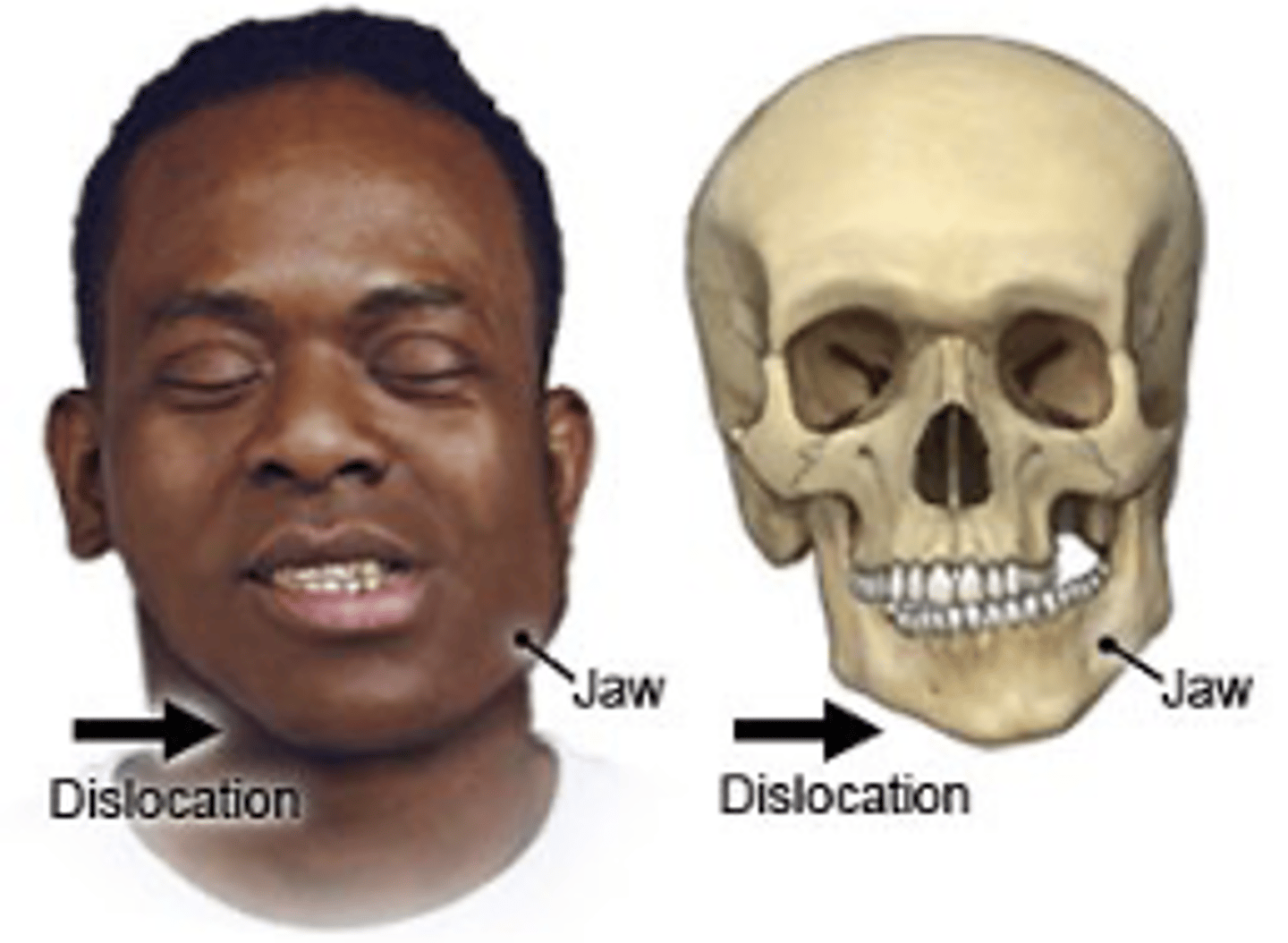
Temporomandibular Joint (TMJ) Dislocation
• Can be unilateral or bilateral as well as chronic or acute
.• Dislocation involves the disarticulation of the mandibular condyle and the temporal bone
.• Anterior dislocation is most common
risk factors of Temporomandibular Joint (TMJ) Dislocation
• Capsular or ligamentous laxity•
Muscle spasm•
Facial dystonia•
Forceful contractions of the face, jaw, and/or tongue causing difficulty in opening and closing the mouth and often affecting chewing and speech.
• Marfan syndrome
signs and symptoms of Temporomandibular Joint (TMJ) Dislocation
• Inability to close mouth (open lock)•
Pain
• Drooling
• Speaking difficulty
immediate management of Temporomandibular Joint (TMJ) Dislocation
• Referral for treatment
• Place index fingers into mouth on the interior border of the mandible, and press outward•
Pain and movement: Mandible fracture
• Pain only at TMJ: Possible dislocation
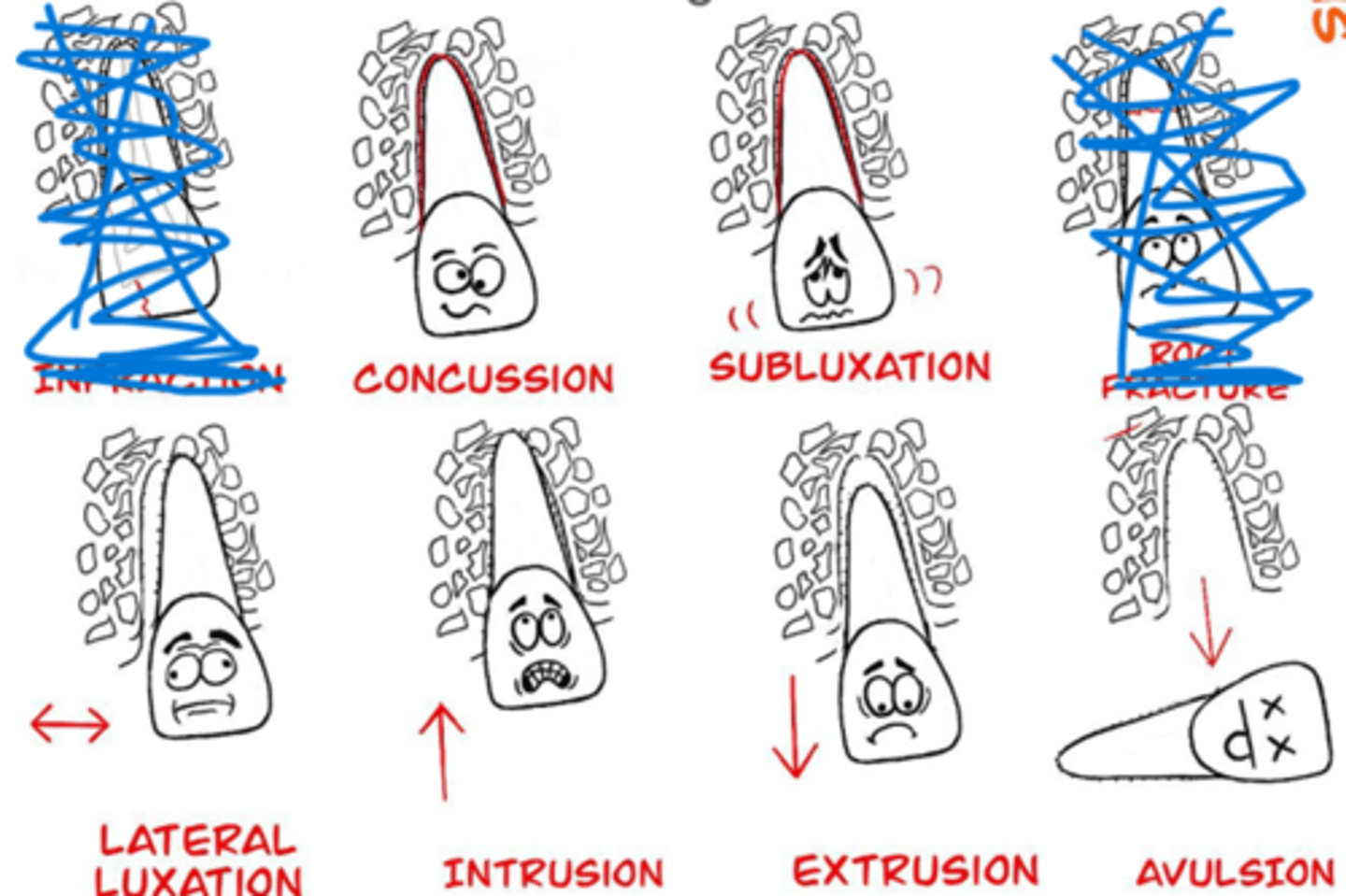
Immediate management depends on dental injury; referral within 24 hours or less almost always required
true
dental Injury categories
Tooth fractures
• Root fractures
• Tooth displacement
Laryngeal Injuries
Occur to the voice box (larynx), the upper portion of the airway
MOI of laryngeal injuries
• High-impact trauma
• Blunt or penetrating neck trauma
• Low-impact trauma
• Abrasions, edema, or contusion
Laryngeal Injuries, Signs and symptoms
- hoarseness
- stridor
- dyspnea
- hemoptysis
- dysphonia
- respiratory distress
- anterior neck tenderness
- subcutaneous emphysema
Most common long-term complication is dysphonia withhoarseness, poor vocal control, and voice fatigue
true
immediate management of laryngeal injuries
• Maintain an patent airway (jaw-thrust) and refer for advanced medical care
• If airway good, evaluate cervical spine
• Apply ice if soft tissue injury
• Recommend vocal rest, humidified air, soft foods, and clear liquids